Abstract
Purpose: This study examines the associations between discrimination experiences (types and locations) and care postponement among trans-feminine individuals in the United States.
Methods: This secondary, cross-sectional study utilized a subset of the data from the National Transgender Discrimination Survey (n = 2248), specifically for trans-feminine individuals. In this analysis, we examined the relationship between discrimination and primary care postponement.
Results: Twenty-six percent (26.25%) of the study sample reported delaying preventive care due to fear of discrimination; 23.98%–46.66% of respondents reported past experiences of discrimination (setting dependent). Discrimination in health and non-health settings and different types of discrimination—being denied services, verbally harassed, or physically assaulted—were all significantly associated with delaying care; respondents reporting discrimination were up to 20 times more likely to postpone care. While discrimination at a health location had the strongest association with care postponement (adjusted odds ratio = 9.65, confidence interval = 7.60–12.24), discrimination in all non-health-related locations was also important. Individuals reporting discrimination in greater numbers of locations and multiple types of discrimination were more likely to postpone care.
Conclusion: To promote preventive care-seeking, these results affirm the importance of interventions that promote discrimination-free environments for gender minorities.
Keywords: : discrimination, gender minority, preventive care, transgender
Introduction
Transgender* individuals, especially trans-feminine individuals,† experience an array of health disparities compared to their cisgender counterparts. For example, the highest rates of new HIV cases in the United States are among transgender individuals, particularly transgender women.1 A 2013 report found that 22% of transgender women in the United States were living with HIV, making transgender women among the populations most affected by HIV in the United States.2 An earlier meta-analysis found that 27.7% of transgender women tested positive for HIV, whereas only 11.8% self-reported a positive diagnosis,3 indicating that many HIV-positive transgender women are unaware of their HIV status. Approximately half of transgender individuals with HIV are African American.4 Furthermore, in the United States, more than half of HIV testing events in 2009–2011 among transgender people occurred at non-healthcare facilities (55%),5 indicating both potential barriers to accessing preventive care services in healthcare settings and the unique role that non-healthcare facilities play in providing resources in accessible formats.
Many studies utilizing convenience samples indicate that transgender populations, especially transgender women,‡ are affected disproportionately by various forms of violence, including sexual assault, physical abuse, and assault in one's home.6–8 These reports show that the majority of transgender individuals are living with the aftermath of trauma and the fear of possible repeat victimization. Transgender individuals who have endured physical and/or sexual violence are significantly more likely than those who have not had such experiences to report a history of single and multiple suicide attempts, alcohol abuse, and illicit substance use.9 Furthermore, transgender individuals have been found to have a high prevalence of clinical depression (44.1%) and anxiety (33.2%), with slightly higher rates for transgender women.10 While the direct outcomes of violence, such as injury, are a recognized public health concern, the longer-term associations of violence, such as mental health correlates, could be mitigated with preventive care and warrant public health attention. It is important to note that, while population-level data for transgender populations are limited, due to a historic resistance to include survey items that measure gender minorities, many studies using convenience samples have provided rich data about transgender health.11–13
Preventive care, or any form of primary care, often depends upon a relationship with a healthcare provider.14 However, transgender individuals report high levels of discrimination and problematic interactions with healthcare providers, for example, refusal of services, being treated harshly or with aggressive language, and being addressed and treated in a manner incongruent with their gender identity.13,15 Several studies show that transgender men are more likely to report unequal treatment, whereas transgender women are more likely to report treatment refusal.6,13,16 Transgender individuals frequently do not access healthcare, due, in part, to these histories of negative interactions, resulting in both short- and long-term adverse health outcomes.11,17,18 Even those who do access routine care may avoid particular screenings that exacerbate their gender dysphoria, such as cervical and breast examinations or prostate examinations, especially where there is poor provider training around these issues.
Inequalities arising from discrimination in one setting can shape expectations of poor treatment in other settings. Accordingly, members of minority groups may develop negative attitudes toward services in response to past incidents of discrimination.19 Mistrust or fear of the medical establishment, especially when reinforced by perceived mistreatment across various institutions and/or individual discriminatory experiences at the hands of providers, has the potential to impact healthcare access and health-seeking behavior. Empirical evidence demonstrates this for racial minorities,20 and the same may be true for transgender individuals. The results of trans-negative attitudes, the experience of discrimination based on having a gender identity or expression that varies from the sex assigned at birth, constitute an access barrier to healthcare, both in general primary care14,21,22 and in specialized areas such as mental health,23 substance abuse treatment,24 and HIV.12,25
Despite the multiple health disparities experienced by trans-feminine people and the barriers experienced in receiving optimal healthcare, little is known about how these individuals seek, engage in, and experience healthcare.17 Although a link between discrimination and care-seeking behavior has been established, many of these studies have looked at race-based discrimination.26,27 The goal of this research was to determine how experiences of discrimination in both healthcare and non-healthcare settings are associated with postponement of preventive care in a U.S.-based sample of trans-feminine individuals. This subsample was examined because, when transgender data are available by gender identity and expression, trans-feminine people are shown to have the greatest burden of health disparities, as illustrated by the HIV disparity data noted previously.§ We also examine how the impact of cumulative experiences of stigma and discrimination ([1] multiple types of stigma, e.g., verbal harassment or physical assault, and [2] in multiple locations, e.g., doctor's office or government agency) in non-health public spaces are associated with delaying preventive care.
Methods
Study design and sample
This secondary, cross-sectional study utilized data from the National Transgender Discrimination Survey (NTDS), a population-based survey collected in 2008 through a research partnership between the National Center for Transgender Equality and the National Gay and Lesbian Task Force.13 The final survey sample included 6456 respondents from all 50 U.S. states, the District of Columbia, Puerto Rico, Guam, and the U.S. Virgin Islands. The data were collected by convenience sampling, utilizing online and paper formats of the 70-item survey.
The online survey was distributed through direct contact with more than 800 transgender-led or transgender-serving community-based organizations in the United States, as well as to participants recruited through 150 active online community listservs. The vast majority (n = 6021; 93%) of respondents completed the survey online, through a URL established at Pennsylvania State University. In addition, the paper survey was distributed to organizations serving hard-to-reach populations—including rural, homeless, and low-income transgender and gender-nonconforming individuals—and was completed by 435 respondents (7%). To reach respondents whose economic vulnerability, housing insecurity, or literacy level might pose particular barriers to participation, workers in homeless shelters, legal aid clinics, mobile health clinics, and other service settings hosted “survey parties.” The survey was available in English and Spanish.
The NTDS inclusion criteria defined “transgender” broadly to include “those who transition from one gender to another (transsexuals), and those who may not, including genderqueer people, cross-dressers, the androgynous, and those whose gender non-conformity is a part of their identity.”13 The NTDS study analyzed cross-dressers and gender-nonconforming people separately from male-to-female and female-to-male transgender respondents.13 For our analysis, we restricted inclusion to participants who reported being assigned male at birth and, for the question regarding current primary gender identity, indicated a response of (1) “Female/Woman,” (2) “part time as one gender, part time as another,” or (3) a “gender not listed here, please specify,” where the NTDS staff determined that the write-in response could appropriately be recoded into the existing categories. This study population will hereafter be referred to as “trans-feminine individuals.” There is an assumption made here that those people in our sample identifying part time as one gender and part time as another have some identification with femininity. This reduced the dataset to 3446 individuals.
The second inclusion criterion limited the sample to those respondents who replied to all key variables: (1) postponement of care (yes or no; those reporting “not applicable” were excluded) (n = 2731) and (2) denied care, verbal harassment, or physical assault (n = 2248). A total of 2248 individuals were included in this analysis. All analyses were conducted in STATA version 14 (StataCorp LLC, College Station, TX). The Tulane University School of Public Health and Tropical Medicine Institutional Review Board approved the protocol for this secondary analysis.
Measures
Independent variables
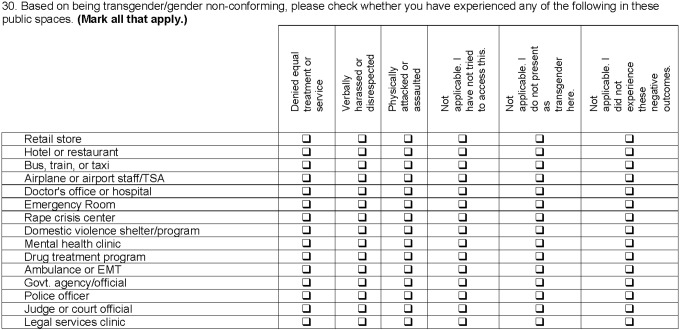
The main exposures of interest are self-reported experiences of discrimination based on gender identity or expression. Discrimination experiences were assessed for 15 public spaces, including health, transportation, commercial, and civic spaces. The survey item is presented in Figure 1.13 Separate variables were constructed to capture experiences of discrimination in non-health public spaces. In an effort to most appropriately conceptualize cumulative discrimination, exploratory factor analysis (EFA) and principal components analysis were conducted. Analyses examined discrimination cumulatively as well as separately by discrimination type (e.g., verbal harassment, physical assault, or denial of services) and locations where discrimination occurred (e.g., doctor's office or government agency). Formal qualitative analyses, namely pile sorts, were used to further conceptualize ways of grouping locations, as described below.
FIG. 1.
Survey item assessing stigma and discrimination experiences in various locations. National Transgender Discrimination Survey. Reproduced with permission from the National Center for Transgender Equality and the National LGBTQ Task Force.13
Discrimination type variables included binary variables (yes/no), noting the following: (1) discrimination in any setting; (2) denial of equal care in any setting; (3) verbal harassment in any setting; (4) and physical assault in any setting. Categorical variables were also created to examine the number of experiences (0 = no discrimination, 1 = experienced at least one type, 2 = experienced two types, and 3 = experienced three types). An additional categorical variable was created with various combinations of discrimination (i.e., verbal harassment, denial of services, or both).
The 15 locations where discrimination occurred were combined into location categories, using 2 approaches along underlying dimensions. EFA on locations indicated a grouping based on health-related locations, including medical and social health (doctor's office or hospital; emergency room; rape crisis center; domestic violence shelter/program; mental health clinic; drug treatment program; and ambulance or emergency medical technicians). As literature on conceptualizing discrimination locations is limited, and intuitive grouping of these locations was challenging, pile sort analysis was conducted with 12 adults recruited purposively and analyzed using Anthropac (Analytic Technologies, Lexington, KY).28 A three-dimensional solution for the items yielded a stress level of = 0.004 for the proximity matrix. Data suggested grouping locations as follows: transportation (bus, train, or taxi; airplane or airport staff), commercial (retail store; hotel or restaurant), and civic spaces (government agency/official; police officer; judge or court official; and legal services clinic). Binary variables (yes/no) were created to indicate whether an experience of discrimination occurred in one of these location categories. Count variables were created for health spaces, non-health spaces, and all spaces. For the above-mentioned variables, all respondents indicated that they had attended at least one of the spaces as transgender or gender nonconforming, and there were no missing data.
Dependent variable
The primary outcome of interest was postponement of preventive care, assessed by survey response to the question, “Because you are transgender/gender nonconforming, have you postponed or not tried to get checkups or other preventive medical care because of disrespect or discrimination from doctors or other healthcare providers?” Response options for each scenario included (1) yes; (2) no; and (3) not applicable. Five hundred and ninety (26%) respondents reported “yes” to this prompt. Respondents who reported “not applicable” (14%) were not included in the sample, as mentioned previously.
Potential confounders
Potential confounders are mainly social in nature, and were obtained by self-report at enrollment in the study. Potential confounders were as follows: race, education, age, income, insurance status, outness, and relationship status. Reisner et al. found that existing NTDS research indicates that different survey modes reach transgender respondents with vastly different health and life experiences,29 a potential confounder as well as a potential effect modifier. Many of the characteristics highlighted as different in the Reisner study29 were controlled for in this study (e.g., race, income, and educational attainment).
Statistical analyses
All statistical analyses were performed using STATA version 14. Univariate, bivariate, and multivariate analyses were conducted. Bivariate analyses assessed the unadjusted relationship between independent variables, potential moderators, and potential confounders with the outcome variable. Variables significant at the bivariate level with Pearson's chi-square tests (p ≤ 0.10), with both (1) discrimination experiences and (2) postponement of preventive care, were considered for inclusion in the multivariable model as well as those variables with theoretical relevance based on literature review and researcher knowledge of the subject. Propensity score analyses were conducted to examine potential exchangeability between exposure groups30 (propensity for having experienced any discrimination vs. no discrimination experiences) and indicated balance between groups; therefore, analyses advanced without matching.
Multivariate logistic regression was used to examine the association between discrimination and postponement of preventive care, adjusting for confounders. Odds ratios and 95% confidence intervals (CIs) were utilized to evaluate strength and magnitude of association. Moderation by gender identity was tested with two-way interaction terms in the model. Moderation by survey implementation was also examined, but no significant interaction was detected.
Results
Respondent characteristics are presented in Table 1, overall and by postponement of care. Twenty-six percent (26.25%) reported delaying preventive care due to fear of discrimination. Reports of discrimination in the various locations varied between 24% and 47%, with 23.98% indicating discrimination in transportation spaces, 41.19% in a civic location, and 46.66% in a commercial location. Respondents who reported postponement of preventive care were significantly different from those who did not report postponement on all characteristics.
Table 1.
Distribution of Trans-Feminine Individuals: National Transgender Discrimination Survey, 2008–2009
| Postponed preventive care based on discrimination | ||||||
|---|---|---|---|---|---|---|
| Total | Yes | No | ||||
| Key variables and covariables of interest | N | % | n 590 | % 26.25 | n 1658 | % 73.75 |
| Discrimination by location*** | ||||||
| Health location | 876 | 38.97 | 457 | 52.17 | 419 | 47.83 |
| Commercial location | 1049 | 46.66 | 407 | 38.8 | 642 | 61.2 |
| Transportation location | 539 | 23.98 | 267 | 49.54 | 272 | 50.46 |
| Civic location | 926 | 41.19 | 406 | 43.84 | 520 | 56.16 |
| Education** | ||||||
| High school or less | 274 | 12.19 | 81 | 29.56 | 193 | 70.44 |
| Some college | 996 | 44.31 | 283 | 28.41 | 713 | 71.59 |
| College degree | 531 | 23.62 | 112 | 21.09 | 419 | 78.91 |
| Graduate degree | 443 | 19.71 | 113 | 25.51 | 330 | 74.49 |
| Health insurance*** | ||||||
| Insured private | 1246 | 55.43 | 279 | 22.39 | 967 | 77.61 |
| Insured public | 534 | 23.75 | 148 | 27.72 | 386 | 72.28 |
| Uninsured | 432 | 19.22 | 149 | 34.49 | 283 | 65.51 |
| Income*** | ||||||
| <$20,000 | 562 | 25 | 211 | 37.54 | 351 | 62.46 |
| $20,000 to $49,999 | 681 | 30.29 | 174 | 25.55 | 507 | 74.45 |
| $50,000+ | 969 | 43.1 | 195 | 20.12 | 774 | 79.88 |
| Age*** | ||||||
| 18–24 | 226 | 10.05 | 77 | 34.07 | 149 | 65.93 |
| 25–44 | 947 | 42.13 | 300 | 31.68 | 647 | 68.32 |
| 45–54 | 564 | 25.09 | 133 | 23.58 | 431 | 76.42 |
| 55+ | 469 | 20.86 | 72 | 15.35 | 397 | 84.65 |
| Race/ethnicity*** | ||||||
| White | 1756 | 78.11 | 424 | 24.15 | 1332 | 75.85 |
| People of color | 482 | 21.44 | 164 | 34.02 | 318 | 65.98 |
| Out with healthcare providers* | ||||||
| None | 144 | 6.41 | 32 | 22.22 | 112 | 77.78 |
| Few/some | 707 | 31.45 | 207 | 29.28 | 500 | 70.72 |
| Most/all | 1361 | 60.54 | 341 | 25.06 | 1020 | 74.94 |
| Relationship status*** | ||||||
| Single | 712 | 31.67 | 206 | 28.93 | 506 | 71.07 |
| Partnered | 399 | 17.75 | 125 | 31.33 | 274 | 68.67 |
| Married/civil union | 572 | 25.44 | 127 | 22.2 | 445 | 77.8 |
| Separated/divorced/widowed | 561 | 24.96 | 130 | 23.17 | 431 | 76.83 |
p ≤ 0.10; **p ≤ 0.05; *** p ≤ 0.01. P value is based on Pearson's chi-square tests.
Results of the analysis based on the location categories in which the discrimination occurred are presented in Table 2. The categories were as follows: health, transportation, commercial, and civic spaces. Discrimination experience in any of the location categories was significantly associated with postponement of preventive care (Models A–E). Apart from discrimination in a health location, which had the strongest association, discrimination in all non-health-related locations was significantly associated with a more than threefold likelihood of care postponement (adjusted odds ratio [aOR] range from 3.27 to 4.16). Furthermore, as the number of health, non-health, and all combined discrimination locations increased, so too did the likelihood of postponement (results not shown). Differences in postponement of preventive care also differed by income, age, and disclosure, with less postponement among those with higher incomes, those 55 years of age and older, and those who reported being generally “out.” This remained consistent across the models.
Table 2.
Association Between Location of Discrimination Experience and Postponement of Preventive Care, Logistic Regression, N = 2090
| Model A | Model B | Model C | Model D | Model E | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| No discrimination (Ref.) | 1 | 1 | 1 | 1 | 1 | |||||
| Any location | 7.23 | 5.18–10.11 | ||||||||
| Health location | 9.65 | 7.60–12.24 | ||||||||
| Commercial location | 3.27 | 2.64–4.06 | ||||||||
| Transportation location | 3.59 | 2.86–4.51 | ||||||||
| Civic location | 4.16 | 3.33–5.18 | ||||||||
| Pseudo R2 | 0.1261 | 0.2165 | 0.0977 | 0.0964 | 0.1165 | |||||
| Pearson chi-square | 1070.51 | 1081.6 | 1092.51 | 1031 | 1083.21 | |||||
| Hosmer-Lemeshow chi-square | 5.46 | 5.42 | 6.98 | 7.1 | 9.21 | |||||
Models controlled for education, income, insurance status, age, race, relationship status, and out with healthcare provider.
aOR, adjusted odds ratio; CI, confidence interval.
Results of discrimination type (in any location) on care postponement are presented in Table 3. Respondents who indicated they had been denied services, verbally harassed, or physically assaulted were significantly more likely to postpone care. Cumulative discrimination experiences were strongly associated with postponement of care-seeking for preventive health in a dose–response manner. Individuals who experienced any type of discrimination were significantly more likely to postpone preventive care (aOR = 7.23; 95% CI = 5.18–10.11).
Table 3.
Association Between Type of Discrimination Experience and Postponement of Care, Logistic Regression, N = 2090
| Model A | Model B | Model C | Model D | Model E | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| No discrimination (Ref.) | 1 | 1 | 1 | 1 | 1 | |||||
| Any discrimination | 7.23 | 5.18–10.11 | ||||||||
| Denied services | 4.78 | 3.82–6.00 | ||||||||
| Verbally harassed | 3.78 | 3.00–4.77 | ||||||||
| Physically assaulted | 3.32 | 2.37–4.64 | ||||||||
| Any one type | 4.21 | 2.94–6.04 | ||||||||
| Any two types | 10.67 | 7.46–15.27 | ||||||||
| All three types | 20.51 | 12.68–33.19 | ||||||||
| Pseudo R2 | 0.1261 | 0.1311 | 0.1037 | 0.0661 | 0.164 | |||||
| Pearson chi-square | 1070.51 | 1088.38 | 1134.3 | 1003.7 | 1305.7 | |||||
| Hosmer-Lemeshow chi-square | 5.46 | 10.33 | 15.52 | 5.95 | 3.32 | |||||
Models controlled for education, income, insurance status, age, race, relationship status, and out with healthcare provider.
Discussion
This study explored the association between discrimination in multiple locations and across various types of discrimination and postponement of preventive care in a U.S.-based sample of trans-feminine individuals. Discrimination experiences both in and outside healthcare settings influenced health-seeking behavior, as did varying types of discrimination. As expected, the cumulative effect of experiencing discrimination in multiple locations and multiple types of discrimination had the largest impact.
Although data comparison is difficult because standardization for constructing gender minority categories or collecting data on discrimination and health does not yet exist, we attempt to put our findings in relation to similar research. The findings of this study reveal higher rates of overall lifetime discrimination in a health setting (38.97%) among trans-feminine people than other studies reporting findings on a wider umbrella of gender minority individuals.13 NTDS findings report that 24% of all respondents experienced denial of equal treatment in doctor's offices and hospitals in their lifetime, with female-to-male respondents reporting higher rates than their male-to-female counterparts (subsample percentages not available).13 In addition, 28% of all respondents reported verbal harassment in a doctor's office, emergency room, or other medical setting.13 These results suggest that our study population may bear a higher burden of medical discrimination than other gender minority subgroups. The report of the 2015 U.S. Transgender Survey (USTS) reported that in the past year, 33% of respondents (including all groups under a transgender umbrella) experienced at least one negative experience with a doctor or other healthcare provider related to being transgender.6 However, in the USTS, transgender men (42%) were more likely to report negative experiences than transgender women (36%) and nonbinary respondents (24%).6
A 2010 Lambda Legal study reported that 70% of all transgender and gender-nonconforming respondents had experienced at least one type of discrimination in a healthcare setting, with transgender respondents being four to seven times more likely than gender-nonconforming respondents to experience discrimination based on their gender identity.15 The rate of discrimination in the Lambda legal study is much higher than our findings, perhaps because the Lambda Legal study included more possible types of discrimination than the NTDS and did not provide subanalysis by gender identities that matched our study population.15 Furthermore, the Lambda Legal study was not limited to trans-feminine individuals, suggesting that it is other (non trans-feminine) individuals under a larger gender minority umbrella who may be experiencing more healthcare discrimination.15 However, selection bias may also be an explanation for differences across studies in that systematic differences in who agreed to participate in each study may also be related to experiences of discrimination. Gender minority subgroups face a variety of discrimination experiences that are uniquely influenced by sexism, trans-negative attitudes, misogyny, and other intersectional systems of oppression, perhaps explaining why discrimination rates may vary depending on the gender identity composition of the sample population. Our findings highlight a need to conduct further analyses based on gender expression and identity and work toward standardized ways of constructing gender minority subsamples and discrimination-related measurements.
Our results concerning the effects of discrimination show that 26.25% of trans-feminine individuals report postponing care due to discrimination concerns, which is similar to the 33% in the larger NTDS sample, with female-to-male transgender respondents reporting a higher frequency (48%) than male-to-female transgender respondents (27%).13 These findings align with data from the 2015 USTS, which did not focus specifically on preventive care, but found differences by gender identity, with transgender men (31%) being more likely to avoid care out of fear of discrimination than transgender women (22%) and nonbinary respondents (20%).6 These results also corroborate findings from race-based discrimination studies, such that discrimination in one setting can shape expectations of poor treatment in other settings.19 Furthermore, race-based findings that perceived discrimination can delay medical care-seeking26,27 are also confirmed in our study, which showed that discrimination in a non-health location is associated with care postponement (aOR 3.27–4.16 depending on location). Those race-based studies also show that perceived discrimination can erode adherence with medical treatment and trust in healthcare providers,26,31,32 which may also be true among trans-feminine individuals.
Research has shown that racial disparities in healthcare stem from institutionalized patterns of racial discrimination, in addition to overt discriminatory acts by healthcare providers.20 As the data in this study demonstrate, it is also possible that institutionalized trans-feminine-negative attitudes influence healthcare utilization negatively. Although the data from our trans-feminine sample differed from other studies in terms of the exact rates of health-related discrimination, we see that gender minority groups do face discrimination that impacts their health-seeking behavior. Broader efforts to diminish discrimination toward all transgender individuals in health systems and wider society, rather than only within client-provider interactions, could improve health outcomes for our study population and the transgender population at large. The influence of institutionalized trans-negative attitudes, and ways to mitigate its effect on health, should continue to be explored in disparities research and in the development of interventions.
High rates of employment discrimination, housing discrimination, and healthcare discrimination have been reported in various studies among transgender individuals,6,15,33,34 and corroborated in our study, with discrimination reports in this study in various locations ranging from 23.98% to 46.66%. Trans-negative attitudes have been shown to be associated with barriers to employment, sex work, incarceration, increased HIV vulnerability,35 lack of health insurance, inability to obtain needed healthcare, history of sexual and physical violence, substance use, and interpersonal resilience factors,11 as well as rejection from family and friends, and emotional distress.36 All of these negative outcomes are further associated with increased sexual risk-taking behavior and negative sexual health outcomes.35 Access to high-quality primary care could mitigate many of these social, physical, and mental health issues by intervening at an earlier stage and providing prevention and treatment services, or connecting patients to additional resources.
Access to primary healthcare is directly influenced by access to health insurance. As transgender individuals are likely to face employment discrimination,13 they are therefore less likely to have health insurance through an employer. In addition, many clients face insurance problems when the anatomy for which they require preventive services does not match that associated with their gender marker (i.e., prostate examinations for trans-feminine individuals). Insurance was controlled for, but did not prove significant in any of the study models.
Limitations
Despite important findings, this study has limitations, including the cross-sectional nature of the study and, therefore, lack of temporal associations. Furthermore, the use of a convenience sample strategy limits the overall generalizability to a larger population, although it is important to note that the geographic distribution of the sample largely mirrors that of the general U.S. population, and that a probability sample of transgender individuals, or any subsample, is impossible at this time with existing data and sampling frames. In addition, many of the survey questions were complex and included multiple components, which may have resulted in confusion and some response bias. Furthermore, the data were collected between 2008 and 2009, and experiences and behaviors may have shifted since that time.
The categorization of our study population assumes that those people identifying part time as one gender and part time as another, do in some way associate with femininity, and may be inaccurate. Therefore, some members of our population may not actually identify as trans feminine, which will complicate the interpretation of the findings. It is worth reiterating that standard definitions of gender minority subpopulations do not exist, making category construction complicated and data comparisons imperfect. Furthermore, few studies have collected such extensive data regarding discrimination among gender minorities. The 2015 USTS does collect similar data, but has not yet presented analysis on our specific study population.6 Nonetheless, this study has several strengths, including minimal missing data and exploration of a relatively unexamined area.
Conclusion
Our results indicate that reducing discrimination in the lives of trans-feminine individuals may reduce barriers to healthcare access and improve health. At the time that this article was being written, transgender discrimination and hate crimes specifically targeting trans-feminine individuals, and particularly those from racial and ethnic minority groups, were on the rise.37 Due to the questionable future of transgender-related nondiscrimination legislation,38 the ongoing battles for transgender bathroom access,39,40 and questions regarding the types of gender-affirming healthcare that will be covered by the Affordable Care Act or any insurance plan,41 it is paramount that we not only monitor experiences of discrimination but also begin to address the larger social determinants of such discrimination,42 if we aim to make any significant reductions in health disparities experienced by transgender individuals.
Acknowledgments
This study was supported by grants from the Health Resources & Services Administration Maternal and Child Health Epidemiology Doctoral Training Program (T03MC07649), NIH Drug Dependence Epidemiology Training Program, NIH/National Institute on Drug Abuse (T32DA007292), the National Institute on Alcohol Abuse and Alcoholism (P60AA009803), and Doctoral Scholarships from the Global Community Health and Behavioral Sciences Department at Tulane University. The authors would also like to thank the National Center for Transgender Equality and the National Gay and Lesbian Task Force, who collected the important data of the NTDS and so willingly shared the data with us.
Disclaimer
Preliminary findings from this study were presented in a poster session at the American Public Health Association Annual Meeting, Denver, CO, October 29 to November 2, 2016 and at the WPATH Graduate Student Research Symposium in Transgender Health: Philadelphia Trans-Health Conference, Friday, September 8, 2017.
Author Disclosure Statement
No financial conflicts of interest exist.
Transgender is a term “… for those people whose gender identity or expression is different than that typically associated with their assigned sex at birth, including transsexuals, androgynous people, cross-dressers, genderqueers, and other gender non-conforming people who identify as transgender. Some, but not all, of these individuals desire to transition gender; and some, but not all, desire medical changes to their bodies as part of this process.” (Grant et al.13)
Trans-feminine people are those who are assigned male at birth and identify full or part time as women.
Many articles do not explicitly define the construction of their transgender subpopulations. Therefore, it is difficult to find comparison data on trans-feminine individuals and data on transgender women, and the larger transgender umbrella group is presented in an effort to contextualize the study as effectively as possible.
It is important to note that the National Transgender Discrimination Survey report did not look specifically at the subsample in this study, and that trans-feminine and trans-masculine individuals might differ. We hope to compare these samples in future studies and contribute to the existing literature in this area of research.
References
- 1.Centers for Disease Control and Prevention. HIV and transgender communities. CDC Issue Brief. 2016. Available at www.cdc.gov/hiv/pdf/policies/cdc-hiv-transgender-brief.pdf Accessed October31, 2017
- 2.Baral SD, Poteat T, Stromdahl S, et al. : Worldwide burden of HIV in transgender women: A systematic review and meta-analysis. Lancet Infect Dis 2013;13:214–222 [DOI] [PubMed] [Google Scholar]
- 3.Herbst JH, Jacobs ED, Finlayson TJ, et al. : Estimating HIV prevalence and risk behaviors of transgender persons in the United States: A systematic review. AIDS Behav 2008;12:1–17 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. HIV among transgender people. 2017. Available at www.cdc.gov/hiv/pdf/group/gender/transgender/cdc-hiv-transgender-factsheet.pdf Accessed September7, 2017
- 5.Habarta N, Wang G, Mulatu MS, Larish N: HIV testing by transgender status at Centers for Disease Control and Prevention-funded sites in the United States, Puerto Rico, and US Virgin Islands, 2009–2011. Am J Public Health 2015;105:1917–1925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.James SE, Herman JL, Rankin S, et al. The Report of the 2015 U.S. Transgender Survey. 2016. Washington, DC, National Center for Transgender Equality [Google Scholar]
- 7.Stotzer RL: Violence against transgender people: A review of United States data. Aggress Violent Behav 2009;14:170–179 [Google Scholar]
- 8.Nemoto T, Bödeker B, Iwamoto M: Social support, exposure to violence and transphobia, and correlates of depression among male-to-female transgender women with a history of sex work. Am J Public Health 2011;101:1980–1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Testa RJ, Sciacca LM, Wang F, et al. : Effects of violence on transgender people. Prof Psychol Res Pract 2012;43:452–459 [Google Scholar]
- 10.Bockting WO, Miner MH, Swinburne Romine RE, et al. : Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health 2013;103:943–951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bradford J, Reisner SL, Honnold JA, Xavier J: Experiences of transgender-related discrimination and implications for health: Results from the Virginia Transgender Health Initiative Study. Am J Public Health 2013;103:1820–1829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kenagy GP: Transgender health: Findings from two needs assessment studies in Philadelphia. Health Soc Work 2005;30:19–26 [DOI] [PubMed] [Google Scholar]
- 13.Grant JM, Mottet LA, Tanis J, et al. Injustice at Every Turn: A Report of the National Transgender Discrimination Survey. 2011. Washington, DC, National Center for Transgender Equality and National Gay and Lesbian Task Force [Google Scholar]
- 14.Rachlin K, Green J, Lombardi E: Utilization of health care among female-to-male transgender individuals in the United States. J Homosex 2008;54:243–258 [DOI] [PubMed] [Google Scholar]
- 15.Lambda Legal. When Health Care Isn't Caring: Lambda Legal's Survey on Discrimination Against LGBT People and People Living with HIV. 2010. New York, Lambda Legal [Google Scholar]
- 16.Harrison-Quintana J, Grant JM, Rivera IG: Boxes of our own creation: A trans data collection wo/manifesto. TSQ 2015;2:166–174 [Google Scholar]
- 17.Roller CG, Sedlak C, Draucker CB: Navigating the system: How transgender individuals engage in health care services. J Nurs Scholarsh 2015;47:417–424 [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine (US) Committee on Lesbian, Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academies Press, 2011 [PubMed] [Google Scholar]
- 19.Blank RM, Dabady M, Citro CF, eds.: Measuring Racial Discrimination. Washington, DC: The National Academies Press, 2004 [Google Scholar]
- 20.Williams DR, Sternthal M: Understanding racial-ethnic disparities in health: Sociological contributions. J Health Soc Behav 2010;51(Suppl):S15–S27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bockting W, Robinson B, Benner A, Scheltema K: Patient satisfaction with transgender health services. J Sex Marital Ther 2004;30:277–294 [DOI] [PubMed] [Google Scholar]
- 22.Melendez RM, Pinto RM: HIV prevention and primary care for transgender women in a community-based clinic. J Assoc Nurses AIDS Care 2009;20:387–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Avery AM, Hellman RE, Sudderth LK: Satisfaction with mental health services among sexual minorities with major mental illness. Am J Public Health 2001;91:990–991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lombardi E: Substance use treatment experiences of transgender/transsexual men and women. J LGBT Health Res 2007;3:37–47 [DOI] [PubMed] [Google Scholar]
- 25.De Santis JP: HIV infection risk factors among male-to-female transgender persons: A review of the literature. J Assoc Nurses AIDS Care 2009;20:362–372 [DOI] [PubMed] [Google Scholar]
- 26.Casagrande SS, Gary TL, LaVeist TA, et al. : Perceived discrimination and adherence to medical care in a racially integrated community. J Gen Intern Med 2007;22:389–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee C, Ayers SL, Kronenfeld JJ: The association between perceived provider discrimination, healthcare utilization, and health status in racial and ethnic minorities. Ethn Dis 2009;19:330–337 [PMC free article] [PubMed] [Google Scholar]
- 28.Bernard HR: Research Methods in Anthropology: Qualitative and Quantitative Approaches. Lanham, MD: AltaMira Press, 2011 [Google Scholar]
- 29.Reisner SL, Conron K, Scout N, et al. : Comparing in-person and online survey respondents in the US National Transgender Discrimination Survey: Implications for transgender health research. LGBT Health 2014;1:98–106 [DOI] [PubMed] [Google Scholar]
- 30.Rosenbaum PR, Rubin DB: Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Statistic 1985;39:33–38 [Google Scholar]
- 31.Van Houtven CH, Voils CI, Oddone EZ, et al. : Perceived discrimination and reported delay of pharmacy prescriptions and medical tests. J Gen Intern Med 2005;20:578–583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Malley AS, Sheppard VB, Schwartz M, Mandelblatt J: The role of trust in use of preventive services among low-income African-American women. Prev Med 2004;38:777–785 [DOI] [PubMed] [Google Scholar]
- 33.Burgess D, Lee R, Tran A, van Ryn M: Effects of perceived discrimination on mental health and mental health services utilization among gay, lesbian, bisexual and transgender persons. J LGBT Health Res 2008;3:1–14 [DOI] [PubMed] [Google Scholar]
- 34.Clements-Nolle K, Marx R, Katz M: Attempted suicide among transgender persons: The influence of gender-based discrimination and victimization. J Homosex 2006;51:53–69 [DOI] [PubMed] [Google Scholar]
- 35.Gutierrez-Mock L, Thomas-Guess Y, Sevelius J, et al. T-SISTA: Resource Guide for Adapting SISTA for Transwomen of Color. 2009. San Francisco, CA, University of California, San Francisco: The Transitions Project [Google Scholar]
- 36.Hunt J, Moodie-Mills A: The Unfair Criminalization of Gay and Transgender Youth: An Overview of the Experiences of LGBT Youth in the Juvenile Justice System. Washington, DC: Center for American Progress, 2012 [Google Scholar]
- 37.Human Rights Campaign. Violence against the transgender community in 2016. Available at www.hrc.org/resources/violence-against-the-transgender-community-in-2016 Accessed October27, 2017
- 38.Trans Equality. Trump administration plan to roll back health care nondiscrimination regulation: Frequently asked questions. Available at https://transequality.org/1557-FAQ Accessed February2, 2018
- 39.Trans Equality. Transgender people and bathroom access. Available at https://transequality.org/issues/resources/transgender-people-and-bathroom-access Accessed February2, 2018
- 40.Understanding transgender access laws. The New York Times. 2017. Available at www.nytimes.com/2017/02/24/us/transgender-bathroom-law.html Accessed February2, 2018
- 41.Baker KE: The future of transgender coverage. N Engl J Med 2017;376:1801–1804 [DOI] [PubMed] [Google Scholar]
- 42.Jones CP: Systems of power, axes of inequity: Parallels, intersections, braiding the strands. Med Care 2014;52:S71–S75 [DOI] [PubMed] [Google Scholar]