Abstract
Introduction:
Shifts in the health care delivery system have emphasized providing cost-efficient care. The operating room comprises a significant proportion of hospital costs. Analysis of practice variation in operating room supply use can provide insight into opportunities for cost reduction and improved efficiency without compromising outcomes.
Methods:
A retrospective review was conducted of urological procedures performed at the University of California San Francisco Medical Center from September 2012 through December 2015. Supply costs for individual cases were itemized and aggregated using the institution negotiated rate. Operative time was monetized. Supply cost was analyzed with multivariate mixed effects models evaluating surgeon experience and surgeon volume.
Results:
The majority of common urological procedures demonstrate significant variation among surgeons in supply, time and overall cost. Surgeon annual procedure specific volume was a significant predictor of lower cost in multivariate analysis of supply cost (p = 0.016) and correlated with a lower likelihood of the case supply cost being in the top quintile (p <0.001). Surgeon experience was not a significant predictor of absolute supply cost or being in the top quintile of supply cost.
Conclusions:
Significant variation exists among supply costs of high volume procedures. Higher surgeon procedure specific volume predicts lower operating room supply costs. Targeting procedures with variation for cost optimization via standardization could have a substantial impact on operating room costs and efficiency. The experience of high volume surgeons may be useful to guide optimal supply use given their comparatively lower costs.
Keywords: health care costs, cost-benefit analysis, cost control, operating rooms, urology
Health care costs are substantial and rising steeply. In 2013 health care spending totaled $2.9 trillion and comprised 17.4% of the gross domestic product.1 This has led to an increased emphasis on delivering high value care, with a focus on maximizing the cost-effectiveness of medical interventions by balancing monetary costs with quality of care and patient outcomes.2–4 The American Medical Association has called on physicians to be arbiters by making cost conscious clinical decisions.5 Several initiatives, such as Choosing Wisely®, focus on the reduction of unnecessary tests and procedures.6 The American College of Physicians and the Alliance for Academic Internal Medicine have developed a High Value Care Curriculum to train physicians about high value care.7 These programs have shown that changing physician behavior around medical costs requires providing physicians with knowledge and means to improve cost efficiency.8,9
The operating room represents a significant cost center in the hospital, estimated at up to 15% of hospital budgets.10,11 In the OR nearly 50% of the cost comes from surgical materials and supplies.12 Work to analyze operative supply and time costs in the OR is still in its infancy.13–17 One approach to determine where costs may be improved is to evaluate cost discrepancies caused by practice variation by providers performing the same procedures. This analysis offers a prime target for cost-effectiveness and supply cost optimization.
We identified variation in surgical case costs through the evaluation of surgical supply and time cost among common urological procedures performed by multiple surgeons at the same institution, and identify surgeon related predictors of high cost procedures. We hypothesized that significant variation in cost exists among surgeons performing the same procedure and this is driven by surgeon specific factors such as experience and volume.
Methods
We analyzed elective urological surgical procedures performed at University of California San Francisco Medical Center from September 2012 to December 2015, excluding cases that were incorrectly booked (91) or those that had multiple unrelated billed procedures (693). We performed descriptive analyses to identify overall costs, time and supply use for all cases during this period (7,610). We then selected the most common procedures in which at least 2 surgeons had performed the procedure at least twice (6,786). Institutional review board approval was obtained.
Surgeon data were de-identified. Years of experience since completion of residency and mean annual case specific volume per 10 cases per surgeon were calculated. We did not use fellowship training as a covariate as the majority of the surgeons were fellowship trained. Supply costs were determined as the institutional negotiated rate, reflecting the amount paid by the Medical Center for each item. Item selection for each procedure was entirely subject to surgeon discretion, as each surgeon selects the supplies s/he requires for the procedure. Disposable case supply costs were totaled for each case and averaged over all cases of that type for each provider to determine the cost of each item for that provider. Operative time was monetized at $69 per minute based on institutional guidance.
Median case supply cost, case duration cost and total cost by procedure were analyzed with one-way analysis of variance to identify variation among surgeons. Multivariate analysis of factors associated with case supply cost (provider experience and case specific volume per 10 cases) was conducted using a linear mixed effects regression model with the absolute supply cost as the outcome, controlling for procedure and case start time after 3 p.m. (change of shift) as fixed effects, and surgeon as a random effect. To ensure these results were not biased by cost outliers, a sensitivity analysis was performed using the same linear mixed effects model with supply cost normalized as a z-score.
An additional logistic mixed effects model using supply cost in the top quintile as the outcome, and controlling for procedure and case start time after 3 p.m. as fixed effects and surgeon as a random effect, was used to identify factors associated with being a high cost provider. Regression diagnostics were performed for all of these models. Analysis was conducted using R and p <0.05 was considered significant.18
Results
During this period 19 surgeons performed a mean of 2,500 cases per year (777 uniquely billed procedures, mean 107.5 ± 90.9 cases per surgeon per year). More than 84,000 supplies were used per year, costing $3.3 million per year. Overall 5,003 hours per year were spent in the OR (mean case duration 147 ± 101 minutes), contributing $20.7 million of OR time cost per year. Case duration variation did exist in most procedures, and the majority of procedures had significant supply cost variation (11/16) and total cost variation (15/16) among surgeons (table 1).
Table 1.
Procedure cost variation among surgeons with most frequent procedures performed by at least 2 surgeons
| Supply Cost ($) | Duration | Total Cost ($) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Operation | No. Cases | No. MDs | Median ± IQR | p Value | Median ± IQR Mins | Median ± IQR Cost ($) | p Value | Median ± IQR | p Value |
| Robotic assisted prostatectomy | 897 | 6 | 1,324 ± 315 | <0.01 | 241 ± 51 | 16,629 ± 3,519 | <0.01 | 18,167 ± 3,590 | <0.01 |
| Ureteroscopy for stone | 678 | 10 | 907 ± 495 | <0.01 | 87 ± 44 | 6,003 ± 3,036 | 0.55 | 6,856 ± 3,349 | 0.47 |
| Transurethral bladder tumor resection | 484 | 15 | 221 ± 437 | <0.01 | 67 ± 34 | 4,623 ± 2,346 | <0.01 | 5,023 ± 2,443 | <0.01 |
| Percutaneous nephrolithotomy | 409 | 6 | 2,041 ± 946 | 0.92 | 147 ± 65 | 10,143 ± 4,485 | <0.01 | 12,188 ± 5,117 | <0.01 |
| Transurethral prostate resection | 269 | 15 | 689 ± 502 | <0.01 | 124 ± 78 | 8,556 ± 5,348 | <0.01 | 9,598 ± 5,658 | <0.01 |
| Urethroplasty | 258 | 6 | 496 ± 116 | 0.09 | 170 ± 65 | 11,730 ± 4,468 | <0.01 | 12,235 ± 4,520 | <0.01 |
| Laparoscopic radical nephrectomy | 224 | 7 | 2,539 ± 1,838 | <0.01 | 222 ± 110 | 15,318 ± 7,607 | <0.01 | 18,375 ± 8,872 | <0.01 |
| Open partial nephrectomy | 158 | 7 | 837 ± 775 | <0.01 | 282 ± 73 | 19,424 ± 5,037 | <0.01 | 20,442 ± 5,210 | <0.01 |
| Ureteroscopy for tumor | 149 | 12 | 397 ± 442 | <0.01 | 72 ± 33 | 4,968 ± 2,243 | <0.01 | 5,522 ± 2,565 | <0.01 |
| Direct vision internal urethrotomy | 149 | 10 | 259 ± 163 | <0.01 | 51 ± 22 | 3,519 ± 1,484 | <0.01 | 3,823 ± 1,659 | <0.01 |
| Robotic partial nephrectomy | 146 | 4 | 2,506 ± 1,295 | <0.01 | 205 ± 62 | 14,111 ± 4,295 | <0.01 | 16,641 ± 5,055 | <0.01 |
| Inflatable penile prosthesis | 139 | 4 | 7,296 ± 393 | 0.17 | 155 ± 38 | 10,695 ± 2,622 | <0.01 | 18,126 ± 2,943 | <0.01 |
| Open cystectomy with conduit | 84 | 9 | 1,907 ± 815 | <0.01 | 416 ± 159 | 28,670 ± 10,988 | <0.01 | 30,599 ± 11,206 | <0.01 |
| Artificial urinary sphincter | 77 | 5 | 9,376 ± 585 | 0.80 | 125 ± 78 | 8,625 ± 5,382 | <0.01 | 17,918 ± 4,072 | <0.01 |
| Robotic cystectomy with conduit | 64 | 5 | 4,541 ± 1,836 | <0.01 | 413 ± 112 | 28,463 ± 7,694 | <0.01 | 33,457 ± 6,560 | <0.01 |
| Open cystectomy with neobladder | 31 | 4 | 1,757 ± 373 | 0.25 | 455 ± 127 | 31,395 ± 8,729 | <0.01 | 33,336 ± 9,214 | <0.01 |
Values rounded to nearest whole number.
One-way analysis of variance used as test of significant variation.
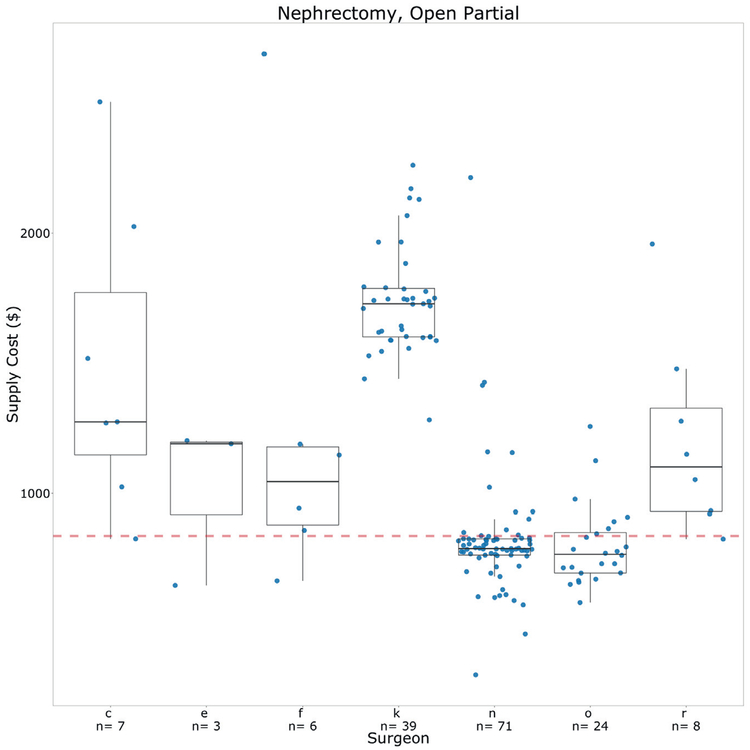
When specific procedures are broken down to evaluate the between-surgeon variation, a pattern of supply use and practice patterns can be visualized. We present open partial nephrectomy as an example of the variation that exists among surgeons (fig. 1). In this example surgeon n is high volume with a low median range and a narrow interquartile range, demonstrating lower cost and consistency in his/her practice. Conversely, surgeon k has a higher median cost but still maintains a fairly narrow interquartile range, which demonstrates a systematic difference in how these surgeons perform this procedure. Surgeon c demonstrates wider interquartile ranges, which could be due to this surgeon having less standardization in this procedure.
Figure 1.
Example of provider variation within open partial nephrectomy. Red broken line represents median supply cost. Surgeon median costs with interquartile range are shown as box plots. Each dot represents supply cost for individual case performed by that provider.
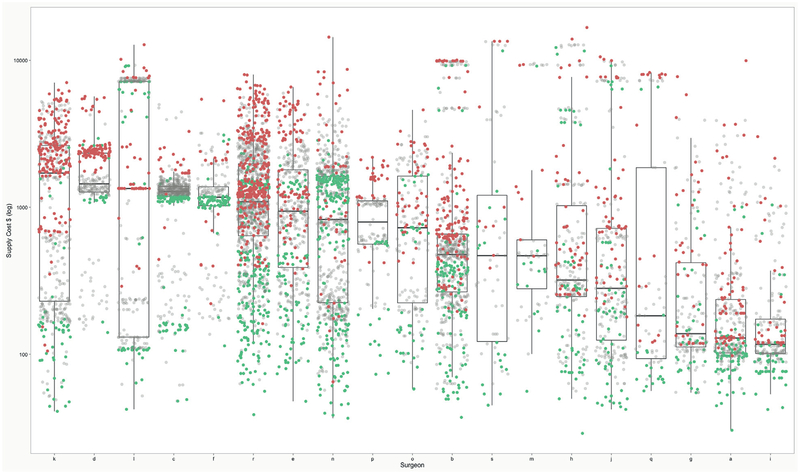
We also evaluated whether a surgeon’s cases were in the top cost quintile for each procedure. Figure 2 shows each case performed by every surgeon, where the dot color indicates whether each case was in the top, lowest or middle (2–4) quintiles of cost for that specific case type. For example, surgeon p performs some expensive procedures but even those higher cost procedures are generally in the lowest quintile of cost for that case. The overall median for each surgeon may be driven more by the case mix. Some surgeons may perform higher cost procedures (surgeons to the left of the graph) whereas other surgeons’ cases may be less expensive (to the right of the graph). Surgeon d demonstrates an interquartile range that is close to that surgeon’s median cost, which may be due to this surgeon’s practice consisting mostly of 1 type of procedure. As another example, surgeon v’s practice is dominated by 2 types of procedures, one that is higher cost and one that is lower cost. Surgeon v tends to be in the highest cost quintile for the more expensive procedure but in the lowest cost quintile for the less expensive procedure, demonstrating that just because a surgeon is cost-efficient in 1 surgery does not necessarily translate to cost efficiency to that surgeon’s other procedures. However, surgeon p demonstrates cost efficiency throughout the practice, given that low cost procedures and high cost procedures tend to be in the lowest cost quintiles for each specific case type.
Figure 2.
Distribution of supply cost by providers across all procedures. Providers listed in descending frequency of median supply cost across all procedures. Each dot represents single operation. Green dots represent cases in bottom supply cost quintile for that specific procedure, red dots represent cases in top supply cost quintile for that specific procedure and grey dots represent cases in middle 3 quintiles.
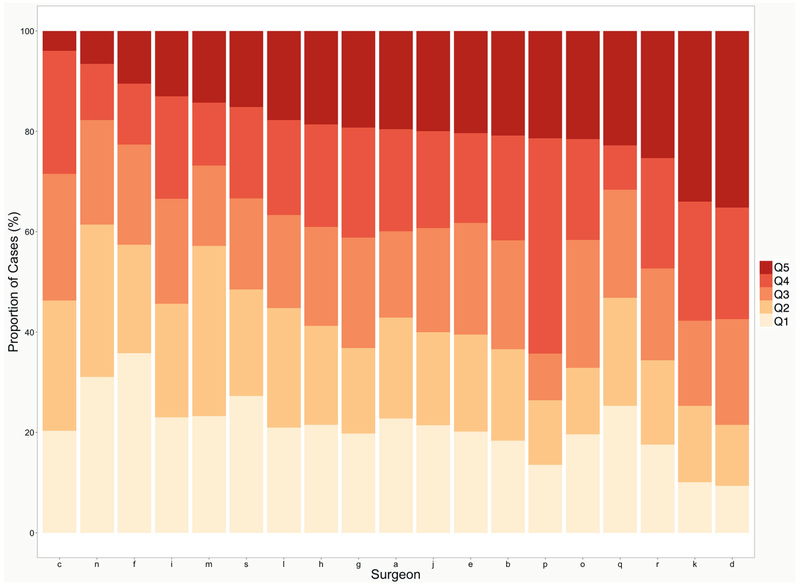
To understand cost efficiency by provider we further evaluated each surgeon’s cases by identifying the proportion of cases in each cost quintile for those specific procedures (fig. 3). Surgeons are listed in increasing order of proportion of top quintile cases. Ideally each surgeon would strive to have a higher proportion of cases in the lower quintiles and decrease the proportion of cases in the highest quintiles.
Figure 3.
Surgeon cases by supply cost quintile. Surgeons listed along x-axis in increasing order based on proportion of cases in top supply cost quintile. Shades represent proportion of each surgeon’s cases in each supply cost quintile.
To determine predictors of absolute case supply cost we performed a linear mixed effects multivariate analysis (table 2). For each additional 10 procedure specific cases that a surgeon performed per year the supply cost decreased by $12.66 (p = 0.016). Surgeon experience was not a significant predictor of supply cost (p = 0.149). A sensitivity analysis using normalized costs supported these findings (years of experience p = 0.056, procedure specific volume p = 0.007). In a logistic mixed effects model evaluating cases in the top quintile of case specific cost to determine predictors of high cost procedures, providers with a higher procedure specific volume were less likely to be in the top quintile of case specific cost (p <0.001) and years of experience since training was not a significant predictor.
Table 2.
Linear mixed effects multivariate analysis
| Absolute Supply Cost* | Top Quintile Supply Cost† | |||
|---|---|---|---|---|
| Covariate | Coefficient | p Value | OR | p Value |
| Yrs of experience | 5.56 | 0.149 | 1.007 | 0.571 |
| Procedure specific annual vol (per 10 cases) | −12.66 | 0.016 | 0.999 | <0.001 |
| Case start time after 3 p.m. | −53.20 | 0.046 | 0.761 | 0.003 |
Linear mixed effect regression of absolute supply cost controls for procedure type. Individual p values not shown.
Logistic mixed effect regression of top quintile of supply cost.
Discussion
Our analysis shows that supply and time costs for the most common procedures vary significantly among surgeons even at the same institution. Higher annual procedure specific surgeon volume was associated with decreased overall supply cost and a lower likelihood of a surgeon being in the top quintile of supply cost for a particular case. In other words, providers who perform more of a certain type of procedure are more incrementally cost-efficient but the years of surgeon experience since training were not associated with cost. This may be because higher volume surgeons know exactly which supplies are needed, and because they perform these procedures often the OR staff does not open unnecessary supplies. Alternatively, it could be a result of high volume surgeons having refined their techniques to use a more cost-efficient approach. This indicates that cost efficiency is a function of high volume and frequency, not cumulative experience, suggesting that having procedural specialists may improve cost efficiency.
Surgeon case supply cost variations are a result of differences in type and volume of supplies used during the operation. For example, the cost differences between various types of electrical coagulating energy sources such as LigaSure™ and Harmonic scalpel™ can be significant. The urologists at our institution use one of 3 instruments, namely a disposable corded onetime use instrument, a corded instrument that can be reprocessed by the manufacturer and a cordless onetime use instrument. The cordless instrument is 3 to 8 times more expensive than the corded device, representing a significant difference in cost and an imperceptible functional difference.
There is also room for improved cost efficiency with low cost but high volume items. Hem-o-lok® clips used for intraoperative hemostasis vary in cost based on clip size, with 5 mm clips costing twice as much as 10 mm clips at our institution. Often clip size is a function of surgeon preference rather than surgical necessity. A round surgical drain with a metal trocar, used in many procedures across disciplines, is 4 times more expensive than the same drain without a trocar. Of note, surgeons often cut off the trocar and discard it, preferring to use other techniques for drain placement, likely without understanding the expense of the item. Another example is the suture used to close fascia. A 36-inch #1 polydioxanone suture on a CTX needle costs a few dollars but that price increases to more than $100 if a blunt tip needle is used.
It is important to note that a certain amount of variation is expected within procedures due to patient characteristics. Patients undergoing surgery for nephrolithiasis, for example, have variable volumes of stone burden and variable complexity of stone location, which may result in the use of more, less or different supplies. With that in mind, there are procedures with significant supply cost variation which may be due to more than just underlying patient characteristics. The wide cost differential seen in open partial nephrectomy, for example, can be explained at least in part by the differential use of hemostatic agents, which are a relatively high cost item. A surgeon may use more expensive supplies such as these because the surgeon believes that they confer a benefit in time efficiency or patient outcomes and, thus, justify the costs. Because we have not evaluated clinical outcomes we cannot evaluate this possibility here.
Our results are a first step in identifying which procedures present opportunities for cost efficiency. It should also be noted that even a lack of variation in cost does not negate an opportunity for cost savings. Procedures that are performed by multiple surgeons using the same supplies and, thus, having similar costs may also be improved despite a lack of variation. The next step is a concerted effort among surgeons to decrease supply costs based on these results. Although surgeons believe that it is important to take cost into account when selecting supplies, many surgeons are unaware of supply costs. Educating surgeons about supply costs and the cost differential between similar items have been shown to be effective.14,19–21
Another method to achieve cost reductions may be to standardize supply use.22 Evaluation of the surgeons in the lower quintiles for each procedure could reveal a more cost-efficient approach that could determine a best practices supply set. Surgeons at an institution should consider collaborating to determine an optimal, standardized way of performing procedures that uses lower cost supplies without compromising outcomes. If standardization of supplies across surgeons could be achieved, this could lead to stocking lower cost alternatives, thereby reducing multiple alternatives of similar supplies to one common option, providing the hospital with better purchasing power and decreasing overall cost. One group analyzed cost differences in laparoscopic appendectomy and found a significant difference in disposable case costs.23 Using data such as ours, surgeons could engage in discussions about using less expensive alternatives or standardizing their supplies, which some have started doing.21
Even if surgeons are unable to agree on a standardized supply preference card, updating each surgeon’s preference card once s/he has learned about supply costs and alternatives may make a substantial difference in each surgeon’s median cost. Our data show that supply cost variation exists even within an individual surgeon’s procedure, as seen in the example of open partial nephrectomy. This may result from out-of-date preference cards, leading to unnecessary supplies being opened but never used, and represents a significant source of waste.24
There are several limitations to this study. The costs that we examined comprise supply costs from the OR only and do not reflect the overall cost of hospitalization, which is a significant contributor to a patient’s operative costs. In addition, these costs have not yet been linked to patient related predisposing factors, which might account for some of the variation, nor have they been linked to patient outcome data to understand if higher costs are justified by improved outcomes.
Our study also has many strengths. We were able to provide data on the relative cost of supplies, which remains poorly described in the literature. In addition, these data reflect real-world materials use and are supported by cost level data, not just charges. Our results identify procedures associated with significant variation that can be targeted for evaluation for further cost improvement. Future work will analyze individual procedures to better understand the drivers of variation and where cost savings measures may be implemented, with specific cost data on supplies used in these procedures. We will tie costs to predisposing factors and patient outcomes that will augment our understanding of value and whether higher operative costs are justified by case difficulty or better patient outcomes. Providing these data to surgeons in the form of anonymized case specific feedback may provide an opportunity to change surgeon practice patterns.
Conclusions
There are significant variations in operative and time costs among providers performing the same procedures, even at the same institution. Surgeons with higher case specific volume were shown to have lower costs and were less likely to fall into the top quintile of case specific costs. Although supply costs constitute a fraction of overall surgical costs, targeting high volume procedures with significant supply cost variability among providers for standardization could have a substantial impact on overall costs, and the experience of high volume surgeons may be used to guide supply use given their comparatively lower costs.
Abbreviation and Acronym
- OR
operating room
Footnotes
No direct or indirect commercial incentive associated with publishing this article.
The corresponding author certifies that, when applicable, a statement(s) has been included in the manuscript documenting institutional review board, ethics committee or ethical review board study approval; principles of Helsinki Declaration were followed in lieu of formal ethics committee approval; institutional animal care and use committee approval; all human subjects provided written informed consent with guarantees of confidentiality; IRB approved protocol number; animal approved project number.
Presented at annual meeting of American Urological Association, New Orleans, Louisiana, May 15–19, 2015.
References
- 1.Centers for Medicare and Medicaid Services: National Health Expenditures 2013 Highlights. CMS; 2013. Available at https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/highlights.pdf. [Google Scholar]
- 2.Qaseem A, Alguire P, Dallas P et al. : Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med 2012; 156: 147. [DOI] [PubMed] [Google Scholar]
- 3.Porter ME: What is value in health care? N Engl J Med 2010; 363: 2477. [DOI] [PubMed] [Google Scholar]
- 4.Curfman GD, Morrissey S and Drazen JM: High-value health care — a sustainable proposition. N Engl J Med 2013; 369: 1163. [Google Scholar]
- 5.Goold SD: Physician Stewardship of Health Care Resources. American Medical Association; 2012. [Google Scholar]
- 6.Levinson W, Kallewaard M, Bhatia RS et al. : ‘Choosing Wisely’: a growing international campaign. BMJ Qual Saf 2015; 24: 167. [DOI] [PubMed] [Google Scholar]
- 7.Smith CD, Alliance for Academic Internal Medicine–American College of Physicians High Value, Cost-Conscious Care Curriculum Development Committee: Teaching high-value, cost-conscious care to residents: the Alliance for Academic Internal Medicine–American College of Physicians Curriculum. Ann Intern Med 2012; 157: 284. [DOI] [PubMed] [Google Scholar]
- 8.Pines JM, Newman D, Pilgrim R et al. : Strategies for integrating cost-consciousness into acute care should focus on rewarding high-value care. Health Aff (Millwood) 2013; 32: 2157. [DOI] [PubMed] [Google Scholar]
- 9.Conway PH: Value-driven health care: implications for hospitals and hospitalists. J Hosp Med 2009; 4: 507. [DOI] [PubMed] [Google Scholar]
- 10.Rutter TW and Brown A: Rutter: Contemporary operating room management - Google Scholar. Advances in Anesthesia; 1994. [Google Scholar]
- 11.Jeon AA: A hospital administrator’s view of the operating room. J Clin Anesth 1995; 7: 585. [DOI] [PubMed] [Google Scholar]
- 12.Souhrada L: OR and materials: the yin and yang. Mater Manag Health Care 1999; 8: 18. [PubMed] [Google Scholar]
- 13.Keller DS, Champagne BJ, Reynolds HL Jr et al. : Cost-effectiveness of laparoscopy in rectal cancer. Dis Colon Rectum 2014; 57: 564. [DOI] [PubMed] [Google Scholar]
- 14.Gitelis M, Vigneswaran Y, Ujiki MB et al. : Educating surgeons on intraoperative disposable supply costs during laparoscopic cholecystectomy: a regional health system’s experience. Am J Surg 2015; 209: 488. [DOI] [PubMed] [Google Scholar]
- 15.Lukish J, Powell D, Morrow S et al. : Laparoscopic appendectomy in children: use of the endoloop vs the endostapler. Arch Surg 2007; 142: 58. [DOI] [PubMed] [Google Scholar]
- 16.Bedeir K, Mann A and Youssef Y: Robotic single-site versus laparoscopic cholecystectomy: Which is cheaper? A cost report and analysis. Surg Endosc 2016; 30: 267. [DOI] [PubMed] [Google Scholar]
- 17.Hall BL, Campbell DA Jr, Phillips LR et al. : Evaluating individual surgeons based on total hospital costs: evidence for variation in both total costs and volatility of costs. J Am Coll Surg 2006; 202: 565. [DOI] [PubMed] [Google Scholar]
- 18.R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2015. [Google Scholar]
- 19.Okike K, O’Toole RV, Pollak AN et al. : Survey finds few orthopedic surgeons know the costs of the devices they implant. Health Aff (Millwood) 2014; 33: 103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vigneswaran Y, Linn JG, Gitelis M et al. : Educating surgeons may allow for reduced intraoperative costs for inguinal herniorrhaphy. J Am Coll Surg 2015; 220: 1107. [DOI] [PubMed] [Google Scholar]
- 21.Gibbs BF, Guzzetta VJ and Furmanski D: Cost-effective carotid endarterectomy in community practice. Ann Vasc Surg 1995; 9: 423. [DOI] [PubMed] [Google Scholar]
- 22.Avansino JR, Goldin AB, Risley R et al. : Standardization of operative equipment reduces cost. J Pediatr Surg 2013; 48: 1843. [DOI] [PubMed] [Google Scholar]
- 23.Chu T, Chandhoke RA, Smith PC et al. : The impact of surgeon choice on the cost of performing laparoscopic appendectomy. Surg Endosc 2011; 25: 1187. [DOI] [PubMed] [Google Scholar]
- 24.Penn E, Yasso SF and Wei JL: Reducing disposable equipment waste for tonsillectomy and adenotonsillectomy cases. Otolaryngol Head Neck Surg 2012; 147: 615. [DOI] [PubMed] [Google Scholar]