Abstract
Introduction
Perivalvular abscess in native valve infective endocarditis (IE) is associated with significantly increased mortality.
Case description
Herein, we report a 29 year old Indian male who presented with culture negative IE with perivalvular abscess and severe mitral regurgitation requiring mitral valve replacement.
Discussion
Initial approach is very difficult in terms of when IE presents as culture negative. This case highlights the important role of echocardiography in the management of culture negative IE.
Keywords: Blood culture negative infective endocarditis, Mitral valve abscess, Mitral valve replacement, Case report
Learning points
In blood culture negative infective endocarditis, always involve the entire heart team and do not delay the surgical intervention if required. Long-term specific antibiotic treatment is vital in all such cases.
Echocardiography always plays an important role in the timely diagnosis and proper management of such cases.
Introduction
Endocarditis was first described by William Osler in 1885. In 1978, Mardelli et al.1 first described the role of echocardiography in detecting valvular abscess. The incidence of blood culture negative infective endocarditis (BCNIE), defined as evidence of endocarditis but without a causative organism being identified after three consecutive blood cultures, is between 2.5 and 31%.2,3 The most common reason for BCNIE is prior antibiotic use or a microorganism which is difficult to detect by conventional blood culture methods.4 In this setting, Dukes criteria is limited with greater reliance on clinical criteria which have high sensitivity but low specificity.5 Delay in diagnosis, amongst other factors, is likely contribute to higher in-hospital adverse events and mortality patients with BCNIE.6
Case report
We report a 29 year old Indian male who presented to our institution with complaints of fever, chills, rigors, fatigue, and shortness of breath (SOB) on minimal exertion for 10 days. He also reported a history of productive cough for 2 months and had been treated on multiple occasions with antibiotic therapy for these symptoms. He gave a history of prolonged antibiotic treatment on and off since 3 years. He denied tobacco, alcohol, or IV drug abuse. There were no symptoms of congestive heart failure. On examination he was alert and oriented. Blood pressure (BP) = 120/70 mmHg, heart rate (HR) = 105/minute, saturation = 98% on room air, temperature = 37.2°C, with pallor and clubbing. There was no skin rash, nor evidence of vascular or immunologic phenomena. On cardiac examination, an apical pan-systolic murmur with radiation to the axilla and a palpable thrill was present. Lung fields were clear bilaterally. A chest X-ray demonstrated mild cardiomegaly, but no pulmonary venous congestion, nor effusions. The resting electrocardiogram showed normal sinus rhythm, rate 80, PR 160 ms, QRS 80 ms, T inversion V1 and V2, and no other significant ST-T changes.
Timeline
| 20th April 2017 | C/o shortness of breath and productive cough on several course of antibiotics. |
| 12th June 2017 | Fever, Chills & rigor |
| 22nd June 2017 | Admitted to the hospital & confirmed the diagnosis of IE with mitral valve abscess by TEE. Started on IV ceftriaxone, gentamycin & vancomycin |
| 27th June 2017 | Surgical excision of abscess & closure done with bovine pericardium and mitral valve replacement with St.Jude mechanical valve performed |
| 6th July 2017 | After 2 weeks of IV gentamycin patient developed interstitial nephritis. Then he was kept on only IV ceftriaxone & vancomycin |
| 9th July 2017 | Follow-up TTE showed normally functioning mitral prosthesis with mild MR. It was decided to continue IV antibiotics for 4 more weeks |
| 1st Aug 2017 | Follow-up TTE was satisfactory |
| 10th Aug 2017 | Patient discharged |
Baseline laboratory investigations showed white blood cells (WBC) = 20.8 × 109/L (Ref. range 4–10 × 109/L), C-reactive protein (CRP) = 84.2 mg/L (Ref. range 0–8 mg/L), erythrocyte sedimentation rate (ESR) = 56 mm/h (Ref. range 0–15 mm/h), plasma lactic acid = 5.7 mmol/L (Ref. range 0.5–2.2 mmol/L). A Q-test for tuberculosis (TB) was positive; however, sputum samples for acid-fast bacilli (AFB) and polymerase chain reaction (PCR) of TB culture were negative. No growth was seen from three sets of blood culture after 5 days. Malaria and Brucella tests and Coxiella Brunetti (Q fever) antibodies were negative. Anti-nuclear antibody screen, anti-myeloperoxidase, and anti-proteinase-3 antibodies were negative. Aspergillus antigen was negative. Screening for mycoplasma immunoglobulin G (IgG) and IgM were negative. Urine culture showed no growth. Transthoracic echocardiography revealed a ruptured cyst-like structure attached to posterior mitral leaflet (PML) which communicated with the left atrium (LA) and left ventricle (LV). We initially suspected the presence of vegetation’s and later by transoesophageal echocardiography (TOE) we confirmed it as a cavity (Figure 1). Severe mitral and moderate aortic valve regurgitation was present. Left atrium was dilated and LV ejection fraction (EF) of 55–60% noted. A TOE demonstrated a large cavity (3.1 × 3.8 cm) involving the anterior wall of LA, LV, and PML extending from P2–P1–A1–A2. Communication of the cavity involving the anterior wall of LA, LV (Figure 2) along with moderate aortic regurgitation (AR) and severe mitral regurgitation (MR) was reconfirmed on this study. The non-contrast high-resolution computed tomography (HRCT) of the chest was performed to assess the lungs and it was normal. After consulting with the microbiology team, it was decided to keep the patient was on IV gentamycin, ceftriaxone, and vancomycin for 4–6 weeks.
Figure 1.
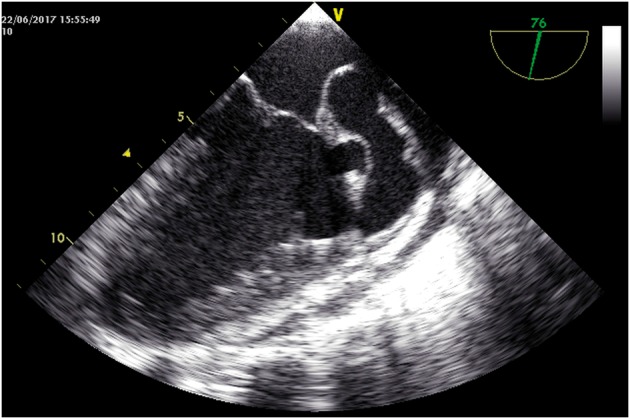
Transoesophageal echocardiography shows a cavity communicating between left atrium and left ventricle.
Figure 2.
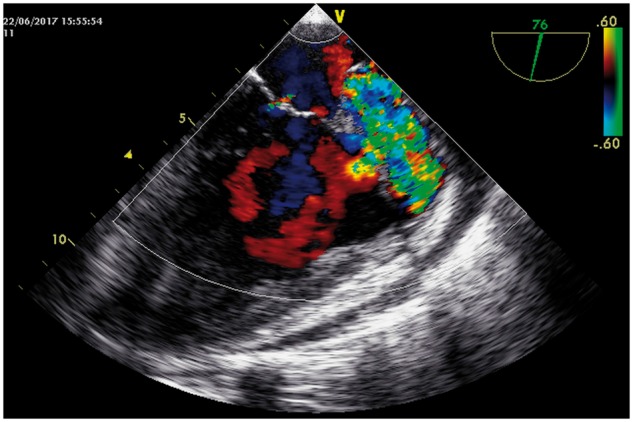
Transoesophageal echocardiography colour Doppler shows the flow through the cavity
Intraoperative findings were consistent with a cavity involving the PML P1 and P2, and anterior mitral leaflet A1 was seen along with a large perforated abscess cavity originating from left atrial appendage (LAA) affecting the mitral leaflets and extending to the left ventricle (Figure 3). Mitral annuloplasty and abscess closure with bovine pericardium was performed from LAA base to P1 and P2 to A1 annulus. Median sternotomy was performed. After establishment of heart lung machine (aortic and bicaval cannulation) antegrade cardioplegia was applied to achieve a cardiac stand still. Right atrium was opened and followed by transatrial septal opening. Localization of the abscess cavity communication LA and LV. Resection of the parts of AML, PML, and abscess cavity followed by the closure of the cavity with bovine pericardial patch from mid-left atrium (inlet of abscess cavity) to anterolateral papillary muscle of the LV (outlet of the fistula). Implantation of bileaflet mitral mechanical prosthetic valve (St. Jude mechanical valve 27 mm) was performed in the classical way along with fixation of pericardial patch.
Figure 3.
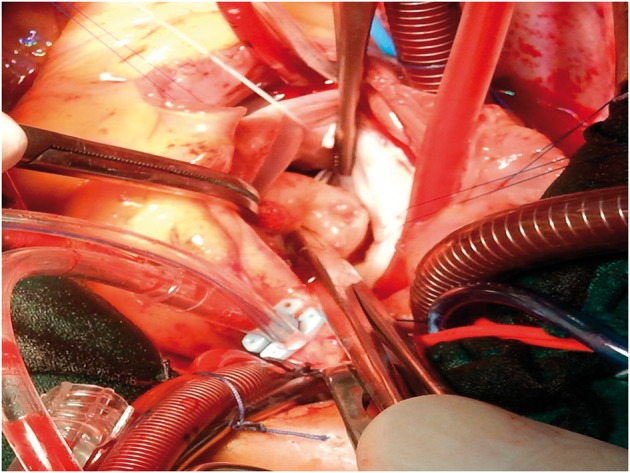
Intraoperative findings shows a abscess cavity originating from left atrial appendage affecting the mitral leaflets and extending to the left ventricle.
No further episodes of fever noted. Electrocardiogram showed junctional rhythm. Laboratory investigations showed WBC = 6.8 × 109/L (Ref. range 4–10 × 109/L), CRP = 14.6 mg/L (Ref. range 0–8 mg/L), ESR = 33 mm/h (Ref. range 0–15 mm/h), plasma lactic acid = 1.6 mmol/L (Ref. range 0.5–2.2 mmol/L), RF = 41 IU/mL (Ref. range 0–20 IU/mL), PCT = 0.44 ng/mL (Ref. range <0.5 ng/mL). Histopathology of tissue samples from mitral apparatus showed mild chronic inflammation without bacterial growth. Tongue swelling was noted and found to have Candida treated with mycostatin oral drops along with heavy growth of alpha-haemolytic streptococci, a normal mouth flora. Follow-up transthoracic echocardiography showed well-functioning mechanical mitral valve, mild MR, and mild systolic dysfunction EF = 40–45%. He was started on IV Ceftriaxone 2 g o.d., IV Gentamycin 80 mg b.i.d. and IV Vancomycin 1 g b.i.d. Patient improved remarkably and discharged after the completion of 6 weeks IV antibiotics.
There was a remarkable improvement on patient’s clinical symptoms. All inflammatory markers reduced markedly and the patient responded well to the surgical correction and antibiotic treatment. He developed interstitial nephritis after 2 weeks of IV gentamycin, hence it was decided to discontinue it and continued IV ceftriaxone and IV vancomycin for 6 weeks.
The patient was very much satisfied by the care given by the cardiology team from the day one. The heart team was activated to explain the procedure and outcomes prior to the surgery. An informed consent was taken prior to the procedure. The post-operative period was satisfactory. He responded to the medications and was happy about the sense of well-being. The cardiac rehabilitation team explained post-procedural routine and patient agreed to follow the instructions.
Discussion
Endocardial abscess in culture negative IE with involvement of the mitral valve, LA, and LV is rare and associated with high morbidity and mortality. Prompt diagnosis and treatment with timely intervention may diminish valve damage and retain the structural integrity of the valve.7 In our case, the diagnosis was prompt and immediate action was taken to replace mitral valve with resection of abscess cavity. Fever is infrequent in cases of BCNIE,8 and in fact our patient did not manifest prolonged episodes of fever. In most of the cases, CRP values give a clue regarding the progression of the disease. Patients with lower CRP levels have better prognosis with less chances of embolization.9 In our case, the CRP level was initially high but it came down quickly soon after the surgery. In BCNIE, Dukes criteria has limitations, and therefore careful echocardiographic evaluation (in particular TOE) plays an important role in the diagnosis and treatment of BCNIE.10 Specific and long-term antibiotic treatment is vital in all cases of culture negative IE.11 Although data on the optimal duration of antibiotic therapy is lacking, we believe antibiotic therapy should continue for a minimum of 6 weeks with adjustments made on the basis of clinical response and inflammatory markers such as ESR, CRP, PCT (see Supplementary Data). In our case, we continued antibiotics for 6 weeks until all inflammatory markers returned to baseline values. Almost 50% of IE cases requires surgical correction along with long-term antibiotic therapy.12 During surgical correction removal of the entire abscess cavity with debridement of tissues around the cavity is essential.13 Majority of the cases with perivalvular abscess with IE require valve replacement. In such cases proper debridement and antibiotic therapy plays a vital role for better results and to avoid further recurrence.14 Post-operative mortality remains high and ranges from 14% to 24%. In-hospital mortality remains same for both cases with culture positive and culture negative IE.15,16 In our case abscess closure, mitral annuloplasty with mitral valve replacement was performed along with 6 weeks of IV antibiotics.
Limitations
We could not perform blood culture for bartonella and legionella. Also serology study to rule out hydatid cyst was not performed in our laboratory at the time.
Conclusion
Echocardiography plays an important role in the timely diagnosis and management of BCNIE. Antibiotic therapy for a minimum 6 weeks seems most appropriate. However, the precise duration of antibiotic therapy for BCNIE is unknown due to lack of data in large numbers of patients.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1.Mardelli TJ, Ogawa S, Hubbard FE, Dreifus LS, Meixell LL. Cross-Sectional Echocardiographic Detection of Aortic Ring Abscess in Bacterial Endocarditis. Chest 1978;74:576–578. [DOI] [PubMed] [Google Scholar]
- 2. Raoult D, Casalta JP, Richet H, Khan M, Bernit E, Rovery C, Branger S, Gouriet F, Imbert G, Bothello E, Collart F, Habib G.. Contribution of systematic serological testing in diagnosis of infective endocarditis. J Clin Microbiol 2005;43:5238.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lamas CC, Eykyn SJ.. Blood culture negative endocarditis: analysis of 63 cases presenting over 25 years. Heart 2003;89:258–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kupferwasser LI, Darius H, Müller AM, Martin C, Mohr-Kahaly S, Erbel R, Meyer J.. Diagnosis of culture negative endocarditis: the role of the Duke criteria and the impact of transesophageal echocardiography. Am Heart J 2001;142:146–152. [DOI] [PubMed] [Google Scholar]
- 5. Kupferwasser LI, Bayer AS.. Update on culture-negative endocarditis. Curr Clin Top Infect Dis 2000;20:113–133. [PubMed] [Google Scholar]
- 6. Kupferwasser LI, Bayer AS.. Culture-negative endocarditis: etiology, diagnosis, management and therapy. Herz 2001;26:398–408. [DOI] [PubMed] [Google Scholar]
- 7. Miyazato A, Mitsutake K, Ohkusu K, Ezaki T, Tabata M, Uwabe K, Niinami H, Kawamura T, Tachi Y.. Comparative molecular and microbiological diagnosis of 19 infective endocarditis cases in which causative microbes were identified by PCR-based DNA sequencing from the excised heart valves. J Infect Chemother 2012;18:318–323. [DOI] [PubMed] [Google Scholar]
- 8. Zamorano J, Sanz J, Moreno R, Almerı´a C, Rodrigo J-L, Samedi M, Herrera D, Aubele A, Mataix L, Serra V, Sánchez-Harguindey L. Comparison of outcome in patients with culture-negative versus culture-positive active infective endocarditis. Am J Cardiol 2001;87:1423–1425. [DOI] [PubMed] [Google Scholar]
- 9. Zamorano J, Sanz J, Almería C, Rodrigo JL, Samedi M, Herrera D, Aubele A, Mataix L, Serra V, Moreno R, Sánchez-Harguindei L. Differences between endocarditis with true negative blood cultures and those with previous antibiotic treatment. J Heart Valve Dis 2003;12:256–260. [PubMed] [Google Scholar]
- 10. Erbel R, Rohmann S, Drexler M, Mohr-Kahaly S, Gerharz CD, Iversen S, Oelert H, Meyer J.. Improved diagnostic value of echocardiography in patients with infective endocarditis by transoesophageal approach. A prospective study. Eur Heart J 1988;9:43–53. [PubMed] [Google Scholar]
- 11. Oakley CM. The medical treatment of culture-negative infective endocarditis. Eur Heart J 1995;16 Suppl B:90–93. [DOI] [PubMed] [Google Scholar]
- 12. Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta J-P, Del Zotti F, Dulgheru R, El Khoury G, Erba PA, Iung B, Miro JM, Mulder BJ, Plonska-Gosciniak E, Price S, Roos-Hesselink J, Snygg-Martin U, Thuny F, Tornos Mas P, Vilacosta I, Zamorano JL.. 2015 ESC Guidelines for the management of infective endocarditis: the task force for the management of infective endocarditis of the European Society of Cardiology (ESC), Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015;36:3075–3128. [DOI] [PubMed] [Google Scholar]
- 13. Musci M, Hübler M, Amiri A, Stein J, Kosky S, Meyer R, Weng Y, Hetzer R.. Surgical treatment for active infective prosthetic valve endocarditis: 22-year single-centre experience. Eur J Cardiothorac Surg 2010;38:528–538. [DOI] [PubMed] [Google Scholar]
- 14. Piciché M, El Khoury G, D'udekem D'akoz Y, Noirhomme P.. Surgical repair for degenerative and rheumatic mitral valve disease. Operative and mid-term results. J Cardiovasc Surg (Torino) 2002;43:327–335. [PubMed] [Google Scholar]
- 15. Picichè M, Ranocchi F, Fiorani B, Bergonzini M, Feccia M, Montalto A, D'Alessandro C, Cottini M, Gherli R, Mariani B, Parisi G, Casali G, Luzi G, Pergolini A, Ferretti E, Giacopino F, Cattolica SL, Madaro L, Musumeci F. Surgical treatment of valvular infective endocarditis complicated by an abscess: a single center’s experience. Interv Cardiol J 2017;3:1. [Google Scholar]
- 16. WernerAndersson M, Olaison R, HogevikA LH.. 10-year survey of blood culture negative endocarditis in Sweden: aminoglycoside therapy is important for survival Scand. J Infect Dis 2008;40:279–285. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


