Abstract
Background
Dissection involving patent arterial duct (PDA) extending to main pulmonary artery (MPA) is an extremely rare condition.
Case summary
We report a case of complex dissection involving PDA extending to MPA, in a child with vein of Galen malformation. This was surgically corrected under deep hypothermic circulatory arrest, and we describe the pathophysiology and surgical rationale in this report.
Discussion
Management of intracardiac lesion in the presence of intracranial arterio-venous malformations such as vein of Galen is very difficult, and employing deep hypothermic circulatory arrest allows one to manage cerebral protection while offering the visualization of intracardiac anatomy more effectively.
Keywords: Case report, Patent arterial duct, Main pulmonary artery dissection, Vein of Galen malformation
Learning points
Spontaneous dissection of patent arterial duct (PDA) is extremely rare, and often seen with other pre-existing conditions or any traumatic interventions in children.
Strong suspicion of infective endocarditis is important for clinical management of dissected PDA.
Early surgery is important to help with the haemodynamic management of such a condition, and also to avoid catastrophic spontaneous rupture of either the pulmonary artery or the dilated duct.
Deep hypothermic circulatory arrest is of vital use in such a situation, in order to allow for a bloodless field and for surgical exposure, thereby optimal surgical procedure is carried out.
Introduction
Spontaneous pulmonary artery dissection is an extremely rare condition.1 Reports of dissected pulmonary artery secondary to infective endocarditis are available. Origin of such a dissection from patent arterial duct (PDA) in a neonate has not been reported previously. We report such a condition, where there was a dissected PDA with extension into main pulmonary artery (MPA), which was treated surgically. Informed consent has been obtained from the parents to report this exceptional case report as part of publication.
Timeline
| On admission | Initial diagnosis of vein of Galen malformation |
| In the first 2 weeks of hospital admission | Neuro-radiological intervention of arterio-venous malformations to vein of Galen malformation |
| On 15th day in hospital | Echocardiographic diagnosis of patent arterial duct (PDA) diagnosis |
| On 18th day in hospital | Further evaluation with computerized tomographic scan of chest with contrast and delineation of anatomy with further echocardiography |
| On 20th day | Joint cardiology and cardiothoracic surgery conference discussion to make management decision |
| On 24th day | Surgical procedure to correct PDA dissection |
| On 27th day | Extubation in cardiac intensive care unit, and assessment proving normal neurological assessment |
| On Days 26 and 28 (for maintenance of chronology, is mentioned here as combined event) | Post-operative echocardiography confirming corrected lesion, with normal flow across pulmonary artery |
Case presentation
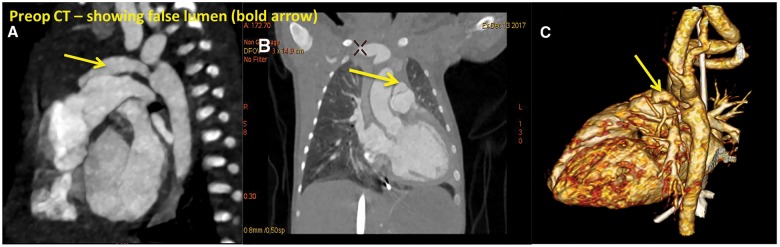
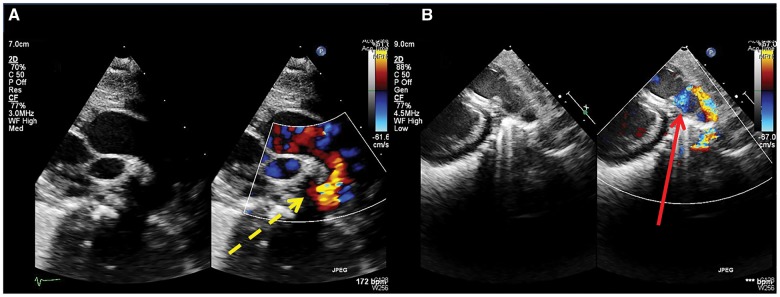
A 20-day-old neonate was evaluated by echocardiography following a neuro-radiological intervention to vein of Galen malformation, whereby coil occlusion of arterio-venous malformations (AVMs) was done. Clinical examination showed mild pectus deformity of chest. There were occasional tachypnoeic features, but no obvious signs of cardiac failure. The heart sounds were normal, with no audible murmurs at this stage. Echocardiography demonstrated PDA and confirmed an additional lumen inside PDA, shunting from aorta to MPA, just proximal to the pulmonary valve. Clinically the child was asymptomatic, but had features of hyperdynamic circulation with palpable pericardial thrill. Further evaluation was done with a contrast-enhanced computerized tomographic (CT) scan. This confirmed a dissected PDA with evidence of both true and false lumen (Figure 1) with dilated MPA. The exit point of this dissection into MPA was not clear on the scan. Bacterial cultures were repeatedly negative to explain any possibility of infective source for this. Despite this, we kept the possibility of infection higher in our consideration, thereby warranting repeated evaluation to seek infective markers and kept the child under antibiotic cover.
Figure 1.
Preoperative computerized tomographic scan showing (A): contrast filled false lumen from the aortic end (B): cross-sectional view of main pulmonary artery with true and false lumens (C): reconstructed image showing similar appearance.
Based on an unquantified risk of rupture from any literature evidence, surgery was decided with aim to ligate the PDA, obliterate the false lumen, and repair the MPA. Furthermore, on discussion, it was felt that any interventional approach would risk placing a larger device within the duct and potentially compromise pulmonary valve because of its proximity.
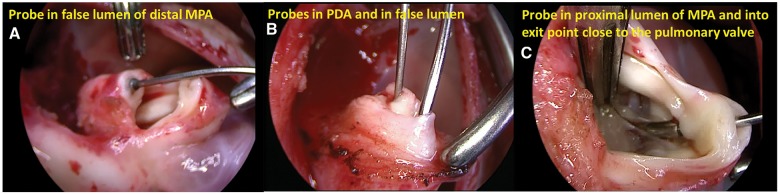
Surgery was carried under cardiopulmonary bypass, with deep hypothermic circulatory arrest at 18°. Neurological monitoring was with near-infrared spectroscopy and using pH strategy for better cerebrovascular control. External appearance showed bosselated appearance of MPA and a large PDA. Once circulation was stopped, division of PDA in its midpoint confirmed two lumens—one small true and another false lumen. The MPA was opened distal to pulmonary valve, and false lumen was additionally confirmed. The extent of false lumen towards the pulmonary valve, thereby showing the exit point near the valve is shown in Figure 2.
Figure 2.
(A) Probe inside false lumen of distal main pulmonary artery; (B) divided arterial duct with probes in true and false lumens; (C) proximal extent of dissection with probe at exit point near pulmonary valve.
Figure 3.
Echocardiographic images showing (A) pre-neurointervention with a small ductal ampulla (dotted line) at aortic end; (B) preoperative image showing false lumen of the duct with flow into main pulmonary artery (solid line) via exit point.
The exit point was closed using 7/0 polypropylene suture. The false lumen on either side of transected pulmonary artery was sutured using similar 7/0 polypropylene sutures. The divided PDA was secured, and MPA was closed. Weaning from bypass was smooth. The child was extubated in 3 days with a normal neurological assessment and post-operative echocardiography confirms normal flow across pulmonary artery with no evidence of any false lumen.
Discussion
Spontaneous dissection of pulmonary artery or PDA is an extremely rare condition. While there are individual reports of dissected pulmonary artery, reports on dissected PDA are scanty. These dissections are thought to be secondary to primary pulmonary hypertension or in association with conditions such as vascular inflammatory disease, aorto-pulmonary fistulas, connective tissue disease, or catheter-induced vessel injury.1
Some of these conditions predispose to a weak arterial wall. Associated abnormal hydrodynamics, in the presence of extensive AVMs, as seen in our child, with vein of Galen malformation may increase the risk of intimal damage, thereby inducing intimal rupture leading to dissection.2
Traumatic dissections can occur in arterial tree in small children in the presence of abnormal haemodynamics.3,4 The traumatic event is related to any instrumentation, including catheterization, as in our case. But the timing of origin and site of dissection away from the end of PDA make this unlikely to be the cause in our case. The entry point of dissection was in the PDA itself away from aortic wall.
Infective endocarditis can potentially weaken specific area of arterial tree. Bacterial cultures in our child were negative to explain such an origin. Despite this, the possibility remained high in our consideration, thereby warranting repeated evaluation and antibiotic cover. Shi et al.5 further reports that while infective endocarditis can help begin the process of dissection, PDA might also contribute to the progression even in the absence of pulmonary hypertension.
Considering the unquantified risk of rupture in a small child, surgery was offered. Catheter-based interventions would potentially be difficult in this situation. Surgical strategy depends on the comorbidities and deep hypothermic arrest would allow us to inspect the anatomy clearly.
With a paucity of report, management depends entirely on the haemodynamic status on the child. With a successful early result, we suggest surgical intervention on dissected PDA with dissection into MPA.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Malm CJ, Ternstrom L, Jorgensen K, Dellgren G.. Pulmonary artery dissection in a patient with undiagnosed pulmonary hypertension—a case report and review of literature. Heart Lung 2015;44:453–457. [DOI] [PubMed] [Google Scholar]
- 2. McElhinney DB, Halbach VV, Silverman NH, Dowd CF, Hanley FL.. Congenital cardiac anomalies with vein of Galen malformations in infants. Arch Dis Child 1998;78:548–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zamorano MMB. Dissection and rupture of the pulmonary artery associated with patent ductus arteriosus: report of a case. Rev Bras Cir Cardiovasc 1987;2:139–144. [Google Scholar]
- 4. Cui Y, Yu J, Nie Z, Shi H.. A rare case of aortic dissection with concomitant pulmonary artery dissection extending through a patent ductus arteriosus. J Vasc Interv Radiol 2015;26:1084–1086. [DOI] [PubMed] [Google Scholar]
- 5. Shi X, Wang X, Wang C, Zhou K, Li Y, Hua Y.. A rare case of pulmonary artery dissection associated with infective endocarditis. Medicine 2016;95:e3358. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.