Abstract
Background
Symptoms of insomnia have been widely identified as risk factors for health, including heart disease. Despite the expansive and growing literature on health concordance among coupled individuals, few studies have examined insomnia as a shared risk factor for heart disease among middle-aged and older couples.
Purpose
This study examined the association between insomnia and incident heart disease among couples. A dyadic modeling approach was employed to investigate the relationships between one’s own insomnia and partners’ insomnia for the risk of incident heart disease for each partner.
Methods
Data from the 2010, 2012, and 2014 Health and Retirement Study were utilized in a prospective research design (N = 3,221 couples). Actor-partner interdependence models were employed to estimate actor and partner effects of insomnia symptoms for incident heart disease over the 4 year observation period.
Results
Insomnia symptoms measured at baseline were related to an increased risk for heart disease for husbands, whereas for wives the association was attenuated after other health measures were controlled. Wives’ insomnia was related to an increased risk of incident heart disease for husbands but husbands’ insomnia was not related to wives’ risk of heart disease.
Conclusions
This study showed how subjective insomnia symptoms among middle-aged and older adults in intimate partnerships are associated with their heart disease risk. Further research is needed to verify the results with objective measures of sleep problems and heart disease.
Keywords: Cardiovascular disease, Couples, Dyadic models, Health and Retirement Study, Interdependence models
Among couples, wives’ insomnia symptoms were related to an increased risk of heart disease for their husbands but husbands’ insomnia symptoms were not related to wives’ risk of heart disease.
Introduction
Despite the extensive literature regarding spousal influences on health among coupled individuals, few studies examine wives’ and husbands’ insomnia as risk factors for well-being among couples [1]. Yet, sleep researchers encourage attention be paid to insomnia among couples, with a focus on the potential for spousal sleep problems to have consequences for one’s own health and overall well-being [2]. Results from such studies provide an opportunity to uncover one of the mechanisms through which cardiovascular health may be adversely affected by poor sleep; that is, one pathway through which risk of heart disease increases may be one’s partner’s sleep problems. To provide evidence for this possible mechanism, a dyadic modeling approach is required, whereby incident heart disease is estimated to be related to partner’s sleep problems, as well as one’s own sleep problems.
Symptoms of insomnia are defined on the basis of self-reported sleep complaints, such as difficulty initiating or maintaining sleep, early awakening, interrupted sleep, and nonrestorative sleep [3, 4]. Recent studies demonstrate that various dimensions of sleep—including specific sleep disorders, objectively measured sleep duration, sleep efficiency, and sleep architecture, as well as subjectively reported sleep quality and insomnia—are linked to a cluster of cardiovascular disease (CVD) risk factors, including obesity, hypertension, and diabetes, as well as mortality [5, 6]. Recent prospective population-based studies find evidence supporting the association between self-reported insomnia symptoms and CVD risk factors, with and without considering sleep duration or sleep-breathing problems [7, 8]. However, results from other studies of insomnia and CVD, such as myocardial infarction, stroke, and heart failure, are equivocal, especially regarding gender differences in these relationships [9–11].
The purpose of this study is to examine whether insomnia is associated with incident heart disease among a sample of middle-aged and older adult couples who are part of an intimate partner relationship. We adopt a dyadic modeling approach for coupled individuals [12], allowing for the investigation of each partner’s sleep problems in relation to the risk of heart disease. Using a population-based prospective study design, we examine data from the Health and Retirement Study (HRS), a large, nationally representative data source.
Insomnia Symptoms and Cardiovascular Health
Studies of the health consequences of sleep problems find that composite measures of insomnia symptoms, as well as specific symptoms, are associated with CVD risk factors and heart disease outcomes [11, 13]. Statistical associations between insomnia symptoms and hypertension are reported in cross-sectional studies [7]. Prospective studies also show that onset of disturbed sleep and persistent insomnia symptoms are associated with a higher risk of hypertension and dyslipidemia [14, 15]. Moreover, subjective insomnia symptoms, along with objectively measured short-sleep duration, are linked to increased risk of hypertension and diabetes [6, 16].
Although individual insomnia symptoms are associated with an increased risk of myocardial infarction or heart failure for respondents free of heart conditions at baseline [17, 18], difficulty falling asleep has the strongest association with CVD, including heart disease [13]. Also, having at least one insomnia symptom is associated with a significantly higher risk for the onset of a CVD event [19]. Furthermore, the concurrence of multiple insomnia symptoms may be associated with additive risk for CVD [8, 17]. The underlying biological mechanisms linking insomnia symptoms and CVD remain to be identified. However, researchers speculate that changes in metabolism and endocrine functions, as well as heightened levels of sympathetic activation, blood pressure, and inflammatory cytokines associated with troubled sleep, may explain the relationship [13, 20]. Poor sleep is also known to influence perceived stress [21, 22], physiological and affective stress reactivity [23], alcoholism [24], and physical activity [25], all of which are associated with cardiovascular health. One contribution of the present study is to examine whether spouse’s insomnia is associated with one’s own heart disease risk, a mechanism rarely studied in the past.
Health Concordance Among Couples
Persons in intimate relationships may have positive and negative effects on their partners’ psychological and physical health outcomes [1], indicating an interdependence between the partners for their well-being. This interdependence among spouses has been documented for CVD and its risk factors [26]. The quality of intimate relationships and coronary heart disease is linked to interpersonal psychosocial risks within couples [27]. The phenomenon of health concordance among couples is attributed to the quantity and quality of social support, shared economic resources, social control of health behaviors, and health-related lifestyles [28].
On the one hand, being married (or other intimate relationship) is often health-promoting and has protective effects for CVD and mortality [28, 29]. The health benefits associated with being married are often explained with reference to socioemotional support that enhances resilience to stress and physiological dysregulation. Additionally, spouses monitor each other’s health and health behaviors and their combined economic resources may provide access to better medical care [28]. Although both men and women may benefit from being married, the health benefits are particularly consistent for men [28].
On the other hand, being in a coupled-relationship is also related to increased risk for depression, obesity, diabetes, CVD, and mortality, among other maladies [1, 30]. Poor health outcomes arise in part when the relationship between partners is strained and of low quality, resulting in increased stress. The association between poor sleep and marital conflict is potentially reciprocal. When one partner has a health problem, that problem may influence the sleep and health of the other partner, even when that partner is otherwise healthy [1]. In general, examining concordance of health-partnered individuals, whether good or bad, is well-situated within the life course perspective because the life course perspective focuses on the importance of linked lives for health outcomes [31].
Gender, Sleep, and Cardiovascular Health
As noted above, recent studies of individuals indicate that the sleep environment represents a social condition with potential negative and positive health consequences [2, 32]. Sleep patterns and health outcomes among couples also invite gendered explanations for this phenomenon. Women’s sleep problems are associated with different life-stage responsibilities for family members, which vary by life course stage [33]. The emotional and psychological burden that women sometimes experience in their multiple social roles (caregiving for spouses, children, grandchildren, extended kin and friends, along with paid work) may give rise to an overwhelming sense of family responsibility, resulting in disturbed sleep [34]. Women also tend to react more strongly than men to relationship conflict [1].
Furthermore, clinical studies of sleep problems among couples provide evidence that specific sleep disorders, such as obstructive sleep apnea and loud snoring, are related to partner’s sleep problems, particularly for wives [2]. Women living with husbands who are heavy snorers more often report insomnia, daytime sleepiness, and fatigue [35]. Yet, women often find excuses for their partner’s snoring and place their own sleep subordinate to their husband’s sleep [36]. This may provide a partial explanation for gender differences in reporting insomnia symptoms, where sleep problems appear to be more prevalent among women compared with men [10].
In general, how such gender differences in sleep disorders may translate into heart disease is complex and not fully understood [13]. As noted earlier, marital benefits associated with health tend to favor men, in part, because women more often possess greater health-related knowledge than men, and are more likely to monitor their partner’s health as well as their own health [37]. When impaired daytime functioning, cognitive deficit, or elevated stress levels associated with sleep problems undermine wives’ spousal social control function, this may have implications for the spousal association between insomnia symptoms and heart disease. A study of couples suffering from psychological, spiritual, and physical illnesses and CVD shows that husbands whose wives report more suffering had higher CVD prevalence, whereas such a relationship was not found for wives in relation to their husbands’ suffering [30]. We expect that health benefits of marriage may diminish or no longer be present for husbands when wives experience poor sleep patterns. Thus, the negative health consequences of spouses sleep problems are expected to be greater for men than women.
Few quantitative studies with nationally representative data have investigated the association between insomnia and health, especially heart disease, among couples from a dyadic perspective (however, see Refs. 21 and 38). We employ a dyadic modeling approach to address the relationship between insomnia symptoms and heart disease in the context of couples bonded in marriage and other forms of intimate partnerships. The current study seeks to contribute to the scientific literature by examining the possibility that husbands’ and wives’ insomnia symptoms are associated with spouses’ risk of heart disease. We address three research questions:
(i) Is there a relationship between one’s own insomnia symptoms and risk for incident heart disease?
(ii) Is there a relationship between spouse’s insomnia symptoms and partner’s risk for incident heart disease?
(iii) Which specific symptoms of insomnia are related to incident heart disease for partnered women and men?
Methods
Data Source
This study utilized data from the biennial HRS, a longitudinal panel study of over 7,000 households in the USA. The HRS was initiated in 1992 with a cohort of individuals born between 1931 and 1941; subsequently, cohorts born earlier and later were added, comprising what is now a nationally representative sample of individuals aged 51 and older. In addition to relying on the publicly available data files provided by the University of Michigan, heart disease, household income, body mass index (BMI), and health behaviors (smoking, exercise, and alcohol consumption) were taken from a file constructed by the Rand Corporation.
In 2002, the HRS began collecting information on respondents’ insomnia symptoms, using four items including (not) feeling rested in the morning, trouble falling asleep, trouble waking up during the night, and trouble waking up too early; three of the four items (i.e., items other than “feeling rested in the morning”) were asked every other wave. We identified 2010 as baseline in this prospective design to examine all four items of insomnia symptoms included in the same wave and to take advantage of the most recent birth cohort added to the HRS sample in 2010. We followed respondents over two subsequent waves (i.e., 2012 and 2014) to track incident heart disease during each 2 yr observation period.
Study Sample
The HRS interviewed 22,034 respondents in 2010, 65 per cent of whom were identified as coupled or partnered (n = 14,238). In this report, we use the term “wives” and “husbands” to refer to respondents who were either married or part of a nonmarried couple. The analytic technique employed in this study can only be applied to “distinguishable” dyads [12]. Thus, we selected heterosexual couples living in the same household because same-sex couples were not uniquely identified in the HRS. Only self-respondents were retained (n = 11,838; dyads n = 5,919). Underweight respondents (BMI <18.5 kg/m2; n = 110) were excluded because their health conditions are considered to be different from individuals in other BMI groups [39]. Because the aim of the study was to examine the cross-spousal association between insomnia symptoms and heart disease incidence, we selected couples where both spouses were free from heart disease at baseline (n = 7,146; dyad n = 3,573). We then selected couples where both spouses provided information on physician diagnosed heart disease during the two subsequent waves (dyad n = 3,314); couples where either spouse was not interviewed in both 2012 and 2014 were excluded (dyad n = 259). Finally, we excluded about 2.8 per cent of the couples where either spouse had missing information on the study variables (dyad n = 93). The final sample included 3,221 couples. Compared with those in the study sample, individuals who were excluded were more likely to experience insomnia symptoms, as measured by not feeling rested in the morning (p < .05) and having trouble waking up too early (p < .01). Also, we excluded respondents who were older (p < .001), less educated (p < .001), and not working for pay (p < .001); these respondents were of normal weight (p < .01), had more depressive symptoms (p < .01) and chronic health conditions (p < .001), and engaged in less physical activity (p < .01).
Measures
Heart disease was assessed with respondents’ self-report of a physician’s diagnosis of these illnesses. Our analyses were based on the measure of heart disease provided in the RAND-constructed data file. Inconsistences and errors were corrected yielding a heart disease measure composed of multiple heart conditions. Once respondents indicated that a physician told them they had a heart condition, respondents were referred to as having heart disease from that point on. HRS respondents were asked at baseline (2010) and at two follow-up points (2012 and 2014), “Since we last talked to you, has a doctor told you that you had a heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems?” Thus, incident heart disease was defined as a new physician diagnosis during the 4 yr observation period. The incidence rate of heart disease at the end of the 4 yr period was 6.9 per cent (6.1% for wives, 7.7% for husbands; n = 444).
To assess insomnia symptoms, we employed items based on a modified version of the four-item Jenkins Sleep Problem Questionnaire [3, 4]. Respondents were asked how often they (i) had trouble falling asleep, (ii) had trouble with waking up during the night, (iii) had trouble with waking up too early and not being able to fall asleep again, and (iv) felt really rested when they woke up in the morning. Respondents rated the severity of the insomnia symptoms on a scale, including 0 (rarely or never), 1 (sometimes), and 2 (most of the time). The item for feeling rested in the morning was reverse-coded to establish consistency with the meaning of the other insomnia indicators. We created an index by summing responses for the four insomnia symptoms, with higher scores denoting more severe insomnia (range: 0–8). Studies using the modified Jenkins Questionnaire reported that these four items loaded into a single factor with the internal consistency of the scale falling within an acceptable range (α = 0.63–0.66) [4, 40, 41]. In our study sample, we estimated Cronbach’s alpha to be 0.65, which falls within a tolerable range for the insomnia index. No items measuring objective sleep problems were available in the three HRS waves employed in this study.
We also included covariates known to be associated with heart disease, including sociodemographic, other health characteristics, and health behaviors. All covariates were measured at baseline. Sociodemographic factors included age (in years), race, and ethnic status (non-Hispanic White (reference group), non-Hispanic Black, non-Hispanic other race group, and Hispanic), marital status (1 = married; 0 = non-marital cohabitation), years of education (0–17), annual household income (transformed by the natural log), and employment status (1 = working for pay; 0 = not working for pay). Health measures included an index of chronic conditions (a count of five relevant chronic health conditions available in the HRS, including high blood pressure or hypertension, diabetes, cancer, lung disease, and stroke; range = 0–5), BMI (1 = normal weight, BMI ≥ 18.5, and BMI < 24.9 kg/m2; 0 = obese or overweight, BMI ≥ 25 kg/m2; based on self-reported weight and height), and an abbreviated seven-item version of the Center for Epidemiological Studies-Depression (CES-D) scale, derived from the eight-item version of the scale included in the HRS minus an item related to sleep (i.e., sleep was restless; range = 0–7). Health behaviors included smoking (1 = current smoker; 0 = former or non-smoker), physical activity (1 = vigorous or moderate physical activity more than once a week; 0 = vigorous or moderate physical activity less than once a week), and alcohol consumption [42] (1 = more than 14 drinks/week for men and more than 7 drinks/week for women; 0 = others). All study variables were measured at the level of the individual, with the exception of marital status and household income, which were couple-level covariates.
Design and Analysis
The analyses for the relationship between insomnia and incident heart disease were based on the multilevel actor-partner interdependence model (APIM) framework, widely used to examine dyadic data [12]. We used generalized estimating equations (GEE) techniques, with an extension for logistic regression models (PROC GEMNOD [SAS Version 9.2] [12]). We employed a two-intercept model approach to estimate actor and partner effects for the relationships between insomnia and incident heart disease [12]. This approach provided a simultaneous estimation of the unique effects of one’s own (i.e., actor) and spousal (i.e., partner) insomnia symptoms for incident heart disease, accounting for the within-couple interdependence in the outcome measure. We estimated a series of APIM using a hierarchical inclusion of variables to evaluate whether actor and partner effects of insomnia symptoms were sensitive to the effects of specific sets of covariates. Model 1 included actor and partner effects of insomnia symptoms without covariates (i.e., unadjusted model); Model 2 introduced sociodemographic factors; and Models 3 and 4 introduced health characteristics and health behavior measures, respectively.
We first estimated multilevel models using the insomnia index to address the research questions (RQ) regarding the overall effects of one’s own (RQ 1) and partner’s (RQ 2) insomnia symptoms for incident heart disease. We then estimated models for each insomnia symptom indicator to evaluate whether heart disease incidence was associated with specific symptoms (RQ 3). Odds ratios (OR) and 95% confidence intervals (CI) are presented. Significance of estimates was determined using Wald χ2 tests [12].
Results
Study sample characteristics are presented in Table 1. Wives had a lower incidence of heart disease during the 4 yr study period and reported higher levels of insomnia compared with husbands. Wives also tended to be younger, had fewer chronic health conditions, reported more depressive symptoms, and were of normal weight compared with husbands. Compared with wives, a higher percentage of husbands reported working for pay, currently smoking, and were more frequently engaged in moderate to vigorous physical exercise. Wives and husbands did not show statistically significant differences in terms of race and ethnic group affiliation, education level, and alcohol consumption. Most of the couples were in a formal marriage, with a smaller proportion (8.3%) in a nonmarital cohabitation status.
Table 1.
Descriptive characteristics of the study sample
| Wives | Husbands | ||||
|---|---|---|---|---|---|
| M | (SD) | M | (SD) | t or χ2 | |
| Heart disease incidence (2012 or 2014)a, % | 6.09 | 7.70 | 6.54* | ||
| Insomnia symptoms (2010) | |||||
| Not feeling rested in the morningb | 0.63 | (0.74) | 0.53 | (0.71) | 29.46*** |
| Trouble falling asleepb | 0.69 | (0.72) | 0.41 | (0.63) | 273.31*** |
| Trouble waking up during nightb | 0.84 | (0.76) | 0.73 | (0.77) | 34.02*** |
| Trouble waking up too earlyb | 0.57 | (0.69) | 0.49 | (0.66) | 23.99*** |
| Insomnia Indexc | 2.72 | (2.07) | 2.15 | (1.89) | 133.73*** |
| Covariates (2010) | |||||
| Socio-demographic characteristics | |||||
| Age (range: 25–92) | 59.25 | (10.01) | 62.34 | (9.94) | 155.26*** |
| Race/ethnicity, % | |||||
| White (non-Hispanic) | 64.67 | 64.64 | 0.70 | ||
| Black (non-Hispanic) | 15.43 | 15.86 | |||
| Other Race (non-Hispanic) | 3.66 | 3.85 | |||
| Hispanic (any race) | 16.24 | 15.65 | |||
| Married, % | 91.68 | 91.68 | – | ||
| Education (years; range: 0–17) | 13.11 | (2.98) | 13.12 | (3.18) | 0.02 |
| Income (logged; range: 0–14.38) | 10.88 | (1.48) | 10.88 | (1.48) | – |
| Working for pay, % | 52.53 | 57.31 | 14.87*** | ||
| Health status | |||||
| Chronic conditionsd | 0.77 | (0.83) | 0.90 | (0.87) | 37.58*** |
| Normal weight, % | 29.77 | 19.68 | 88.09*** | ||
| Depressive symptomse | 0.96 | (1.63) | 0.78 | (1.41) | 21.42*** |
| Health behaviors | |||||
| Current smoker, % | 13.32 | 15.31 | 5.18* | ||
| Problem drinkingf, % | 7.70 | 8.26 | 0.69 | ||
| Moderate/vigorous physical activity weekly or more, % |
58.65 | 62.59 | 10.49** | ||
Dyad N = 3,221.
Group differences are tested using t tests for continuous variables and the chi-square statistics for categorical variables. All study variables measured at the level of the individual, with the exceptions of marital status and household income, which were measured at the couple level.
M mean; SD standard deviation.
aSelf-report of a doctor’s diagnosis of heart disease, including heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems.
bRated as 0 (rarely or never), 1 (sometimes), or 2 (most of the time).
cSummation of the four insomnia symptom items (range: 0–8).
dNumber of chronic health conditions diagnosed by a doctor (range: 0–5).
eSeven-item version of the Center for Epidemiological Studies-Depression scale (range: 0–7).
fMore than 14 drinks/week for men and more than 7 drinks/week for women.
*p < .05; **p < .01; ***p < .001.
Results from regression models examining the overall association between the insomnia symptom index and incident heart disease over the 4 yr follow-up (2012 and 2014) are presented in Table 2. The rows containing estimates of actor and partner effects of insomnia symptoms address the first research question: Is there a relationship between one’s own insomnia symptoms and risk for incident heart disease? In the unadjusted model (Model 1), actor effects of insomnia symptoms were associated with an increased likelihood of heart disease incidence for both wives and husbands. A one-unit increase in one’s own score on the index of insomnia symptoms was related to an increased likelihood of incident heart disease for wives (OR = 1.14, 95% CI = 1.06–1.23) and for husbands (OR = 1.15, 95% CI = 1.08–1.22). For husbands, the association between insomnia symptoms and incident heart disease remained statistically significant in all subsequent models (e.g., Model 4; OR = 1.12, 95% CI = 1.04–1.20). For wives, the association was not statistically significant after chronic health conditions, BMI, and number of depressive symptoms were introduced in Model 3 (OR = 1.06, 95% CI = 0.98–1.16). To evaluate the concordance of heart disease incidence within couples, we estimated intraclass correlation coefficients (ICC). The ICC’s for Models 1–4 ranged from 0.03 to 0.05, indicating a modest level of health concordance as measured by heart disease.
Table 2.
Dyadic models of insomnia symptoms and incident heart disease at 4 yr follow-up: odds ratios and 95% confidence intervals
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | + Sociodemographic | + Health status | + Health behavior | |||||
| Wives | Husbands | Wives | Husbands | Wives | Husbands | Wives | Husbands | |
| Insomnia symptoms indexa | ||||||||
| Actor effects | 1.14*** | 1.15*** | 1.13** | 1.15*** | 1.06 | 1.11** | 1.06 | 1.12** |
| [1.06, 1.23] | [1.08, 1.22] | [1.04, 1.22] | [1.07, 1.23] | [0.98, 1.16] | [1.04, 1.20] | [0.98, 1.16] | [1.04, 1.20] | |
| Partner effects | 1.04 | 1.07* | 1.04 | 1.08* | 1.03 | 1.07* | 1.03 | 1.07* |
| [0.97, 1.12] | [1.01, 1.14] | [0.97, 1.12] | [1.01, 1.15] | [0.96, 1.11] | [1.00, 1.15] | [0.95, 1.11] | [1.00, 1.14] | |
| Covariates | ||||||||
| Age | 1.02** | 1.04*** | 1.02* | 1.04*** | 1.03*** | 1.04*** | ||
| [1.01, 1.04] | [1.03, 1.06] | [1.01, 1.04] | [1.02, 1.06] | [1.01, 1.05] | [1.03, 1.06] | |||
| Race/Ethnicity (reference: White (non-Hispanic)) | ||||||||
| Black (non-Hispanic) | 1.00 | 0.69† | 0.83 | 0.62* | 0.78 | 0.60* | ||
| [0.64, 1.57] | [0.45, 1.06] | [0.52, 1.30] | [0.41, 0.95] | [0.49, 1.23] | [0.39, 0.92] | |||
| Other race (non-Hispanic) | 1.24 | 0.63 | 1.25 | 0.65 | 1.31 | 0.65 | ||
| [0.55, 2.79] | [0.28, 1.44] | [0.56, 2.82] | [0.28, 1.50] | [0.58, 2.95] | [0.28, 1.51] | |||
| Hispanic (any race) | 1.26 | 0.63* | 1.11 | 0.62* | 1.20 | 0.64 | ||
| [0.78, 2.03] | [0.39, 1.02] | [0.68, 1.81] | [0.38, 1.00] | [0.74, 1.93] | [0.40, 1.04] | |||
| Married | 0.94 | 1.15 | 1.00 | 1.13 | 1.05 | 1.14 | ||
| [0.56, 1.59] | [0.67, 1.98] | [0.59, 1.69] | [0.65, 1.95] | [0.62, 1.79] | [0.66, 1.96] | |||
| Education (years) | 0.97 | 0.96 | 0.98 | 0.97 | 0.99 | 0.97 | ||
| [0.92, 1.02] | [0.91, 1.01] | [0.93, 1.04] | [0.92, 1.02] | [0.94, 1.05] | [0.92, 1.02] | |||
| Income (logged) | 0.97 | 0.90† | 1.00 | 0.90* | 1.00 | 0.90* | ||
| [0.89, 1.06] | [0.83, 0.98] | [0.90, 1.11] | [0.83, 0.98] | [0.89, 1.12] | [0.83, 0.98] | |||
| Working for pay | 0.59** | 0.90 | 0.66* | 1.03 | 0.69* | 1.06 | ||
| [0.41, 0.84] | [0.66, 1.24] | [0.46, 0.94] | [0.75, 1.42] | [0.49, 0.98] | [0.77, 1.46] | |||
| Chronic conditionsb | 1.44*** | 1.36*** | 1.42*** | 1.38*** | ||||
| [1.22, 1.70] | [1.18, 1.58] | [1.20, 1.67] | [1.20, 1.60] | |||||
| Normal weight | 0.60* | 0.82 | 0.58** | 0.77 | ||||
| [0.41, 0.89] | [0.57, 1.18] | [0.39, 0.85] | [0.54, 1.12] | |||||
| Depressive symptomsc | 1.16*** | 1.07 | 1.15*** | 1.06 | ||||
| [1.07, 1.26] | [0.98, 1.18] | [1.06, 1.26] | [0.97, 1.17] | |||||
| Current smoker | 1.94*** | 1.65** | ||||||
| [1.31, 2.87] | [1.14, 2.39] | |||||||
| Problem drinkingd | 0.97 | 1.12 | ||||||
| [0.71, 1.33] | [0.85, 1.47] | |||||||
| Moderate/vigorous physical activity weekly or more | 0.66 | 0.74 | ||||||
| [0.32, 1.33] | [0.44, 1.24] | |||||||
Dyad N = 3,221.
aSummation of the four insomnia symptom items (range: 0–8).
bNumber of chronic health conditions diagnosed by a doctor (range: 0–5).
cSeven-item version of the Center for Epidemiological Studies-Depression scale (range: 0–7).
dMore than 14 drinks/week for men and more than 7 drinks/week for women.
† p < .10; * p < .05; ** p < .01; *** p < .001.
The second research question asked whether there is a relationship between spouse’s insomnia symptoms and partner’s risk for incident heart disease. We did not find a statistically significant relationship for husbands’ insomnia symptoms and wives’ heart disease risk. However, we found a statistically significant relationship between wives’ insomnia symptoms and husbands’ incident heart disease (Model 4; OR = 1.07, 95% CI = 1.00–1.14). That is, husbands whose wives reported higher levels of insomnia showed a higher likelihood of incident heart disease across all four models.
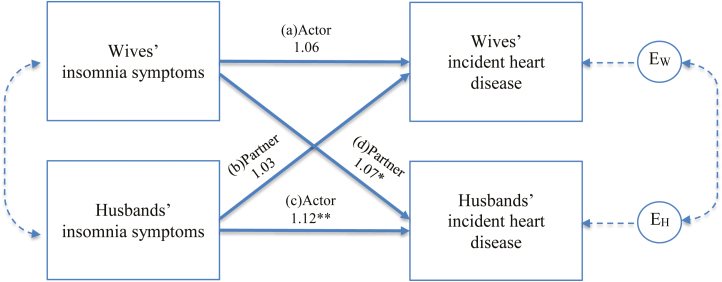
Note that the differences of actor or partner effects between husbands and wives found in our models do not indicate gender differences in the association between insomnia and CVD. We conducted a test for gender differences in our models based on the “interaction” modeling approach [12], finding no statistically significant differences between genders in respective actor or partner effects of insomnia (results available upon request). A summary of the findings for the relationships between the actor and partner effects of insomnia index and incident heart disease is presented in Fig. 1.
Fig 1.
Model of actor and partner effects of insomnia index (range: 0–8) on incident heart disease. EH and EW denote residuals for husband and wife outcomes, respectively. Solid arrows indicate paths of direct interest to the present study. Estimates are from the fully adjusted multilevel model. *p < .05; **p < .01.
Results from models examining the association between each of the four insomnia symptoms and incident heart disease are presented in Table 3. These results addressed the third research question regarding which specific symptoms of insomnia were related to incident heart disease for partnered women and men. For parsimony, only the estimates for the actor and partner effects of insomnia symptoms are reported in the table (results for the covariates were similar to those reported in Table 2 and are available upon request). The insomnia symptom most consistently associated with incident heart disease for both wives and husbands in the fully adjusted models was trouble falling asleep (Panel 2). In Model 4, self-reported trouble falling asleep was associated with an increase in the likelihood of heart disease incidence for wives (OR = 1.25, 95% CI = 1.01–1.56) and for husbands (OR = 1.39, 95% CI = 1.13–1.71). Furthermore, we found statistically significant partner effects of this symptom for husbands, but not wives. That is, husbands whose wives reported trouble falling asleep showed an increased likelihood of incident heart disease, over and above the effects of their own difficulties falling asleep and the covariates (Model 4; OR = 1.25, 95% CI = 1.04–1.50). One’s own symptoms of not feeling rested in the morning, trouble waking up during night, and trouble waking up too early also showed an association with incident heart disease in the unadjusted models, but these actor effects generally became statistically nonsignificant in the fully adjusted models (i.e., Models 4 of Panels 1, 2, and 4). An exception was for the effect of husbands’ reporting trouble waking up too early, which remained statistically significant in Model 4 (OR = 1.26, 95% CI = 1.04–1.53). Partner effects for the other three symptoms were not associated with actors’ incident heart disease.
Table 3.
Dyadic models of insomnia symptom indicators and incident heart disease at 4 yr follow-up: odds ratios and 95% confidence intervals
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | + Sociodemographic | + Health | + Health behavior | |||||
| Wives | Husbands | Wives | Husbands | Wives | Husbands | Wives | Husbands | |
| Panel 1: Not feeling rested in the morninga | ||||||||
| Actor effects | 1.30* | 1.14 | 1.37** | 1.21* | 1.17 | 1.12 | 1.16 | 1.12 |
| [1.06, 1.59] | [0.95, 1.35] | [1.11, 1.69] | [1.01, 1.44] | [0.93, 1.46] | [0.93, 1.34] | [0.92, 1.46] | [0.93, 1.34] | |
| Partner effects | 1.07 | 1.03 | 1.09 | 1.13 | 1.05 | 1.11 | 1.05 | 1.11 |
| [0.87, 1.32] | [0.86, 1.23] | [0.89, 1.34] | [0.94, 1.36] | [0.86, 1.29] | [0.92, 1.33] | [0.85, 1.29] | [0.92, 1.33] | |
| Panel 2: Trouble falling asleepa | ||||||||
| Actor effects | 1.53*** | 1.44*** | 1.43** | 1.48*** | 1.26* | 1.39** | 1.25* | 1.39** |
| [1.25, 1.86] | [1.20, 1.74] | [1.16, 1.77] | [1.21, 1.81] | [1.01, 1.57] | [1.13, 1.71] | [1.01, 1.56] | [1.13, 1.71] | |
| Partner effects | 0.99 | 1.29** | 0.99 | 1.28* | 0.97 | 1.25* | 0.95 | 1.25* |
| [0.79, 1.24] | [1.08, 1.53] | [0.79, 1.25] | [1.07, 1.54] | [0.76, 1.22] | [1.04, 1.51] | [0.75, 1.20] | [1.04, 1.50] | |
| Panel 3: Trouble waking up during nighta | ||||||||
| Actor effects | 1.21 | 1.32** | 1.14 | 1.21* | 1.03 | 1.13 | 1.05 | 1.14 |
| [0.99, 1.46] | [1.12, 1.56] | [0.93, 1.40] | [1.02, 1.44] | [0.84, 1.26] | [0.95, 1.35] | [0.86, 1.28] | [0.96, 1.36] | |
| Partner effects | 1.09 | 1.22* | 1.08 | 1.16† | 1.08 | 1.16 | 1.08 | 1.16 |
| [0.92, 1.31] | [1.03, 1.44] | [0.90, 1.30] | [0.97, 1.39] | [0.90, 1.30] | [0.97, 1.39] | [0.90, 1.30] | [0.97, 1.39] | |
| Panel 4: Trouble waking up too earlya | ||||||||
| Actor effects | 1.25* | 1.34** | 1.16 | 1.32** | 1.05 | 1.25* | 1.05 | 1.26* |
| [1.02, 1.54] | [1.12, 1.61] | [0.93, 1.44] | [1.09, 1.60] | [0.84, 1.31] | [1.02, 1.52] | [0.83, 1.31] | [1.04, 1.53] | |
| Partner effects | 1.17 | 1.12 | 1.16 | 1.11 | 1.12 | 1.10 | 1.11 | 1.09 |
| [0.95, 1.43] | [0.92, 1.36] | [0.94, 1.43] | [0.91, 1.36] | [0.91, 1.38] | [0.90, 1.34] | [0.90, 1.37] | [0.89, 1.34] | |
Dyad N = 3,221.
aRated as 0 (rarely or never), 1 (sometimes), or 2 (most of the time).
† p < .10; *p < .05; **p < .01; ***p < .001.
Discussion
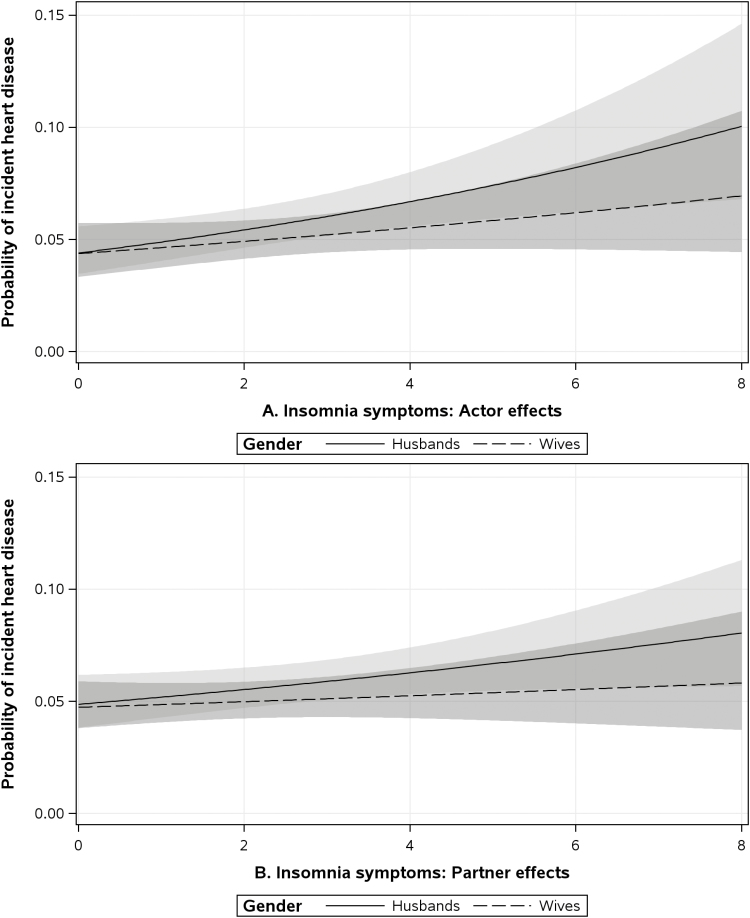
This study investigated the relationship between insomnia and incident heart disease among middle-aged and older adults who were married or in another type of intimate partnership. The central findings were that husbands’ insomnia symptoms were associated with an increased risk of incident heart disease for themselves and that wives’ insomnia symptoms were also related to incident heart disease for husbands; husbands’ insomnia symptoms were not related to wives’ incident heart disease (see Fig. 2 for a graphic representation of the actor and partner effects of insomnia index for incident heart disease found in this study). Trouble falling asleep was the most consistent insomnia symptom related to risk of heart disease, which is consistent with research summarized in a recent meta-analysis of the extant scientific literature [13].
Fig. 2.
Probability of incident heart disease (and 95% confidence intervals marked in grey) for husbands (solid line) and wives (dotted line) by varying levels of (A) actor effects and (B) partner effects of insomnia symptoms (index range: 0–8). The plots are based on estimated parameters from the fully adjusted multilevel model.
Most prior research on the relationship between insomnia and health focused on children and younger adults, with limited attention given to middle-aged and older adults. Even less effort has been given to investigating this question for couples at any stage of the adult life course. Our results were generally consistent with multiple population-based prospective studies of individuals that showed insomnia symptoms are associated with indicators of CVD [17, 19], and specifically, a moderate, yet statistically significant association between insomnia symptoms and heart disease was also found. Our results suggested a consistent actor effect for the relationship between insomnia and heart disease risk for husbands across our models, whereas the relationship for wives’ insomnia and their own heart disease risk was attenuated to statistical nonsignificance after baseline measures for chronic conditions, BMI, and depressive symptoms were controlled. The chronic health conditions index was associated with a strong and persistent risk of incident heart disease for both husbands and wives. Not only was the chronic health conditions index associated with an elevated heart disease risk, additional analyses showed that in models where hypertension at baseline was included as a covariate—one of the most important CVD risk factors—hypertension was also associated with heart disease for wives and husbands (results not shown).
On the other hand, our findings were somewhat different from previous research, where wives were found to be more vulnerable than husbands to the potential negative consequences of insomnia with respect to incident CVD events [17]. We are not aware of any studies that employed dyadic modeling by considering spouses’ sleep to examine the association between insomnia and cardiovascular health among middle-aged and older couples. Thus, it is not feasible to make a direct comparison of findings across studies with substantially different research designs.
Elevated cardiovascular risk in relation to insomnia among men was reported in some studies comparing men and women, and in other studies examining only men [43, 44]. Given that women consistently reported more insomnia symptoms compared with men, it could be that men tended to have sounder sleep patterns than women. However, for those men whose sleep was disturbed, the health consequences of insomnia symptoms may have been more severe. Conversely, a higher prevalence of insomnia symptoms for women may mean that troubled sleep was more accepted by women, or more under-reported by women. Hence, our measures of insomnia symptoms may not have captured fully the effects for incident heart disease. In addition, women have been shown to more actively cope with poor sleep than men, often through self-help behavioral strategies and medical therapies [45], potentially counterbalancing the negative health outcomes, such as heart disease risk, associated with higher rates of insomnia.
As noted above, our findings suggested that wives with insomnia did not have higher risk of heart disease after controlling for their chronic health conditions, depressive symptoms, and BMI—a result not found for husbands. Psychological distress and poor sleep have been closely tied in previous research [1]. Some evidence showed that insomnia and depression were reciprocally related and may have both independent and similar relationships with heart disease [46]. Also, obesity has been associated with both elevated cardiometabolic risk and sleep problems [47, 48]. As wives’ insomnia was found to have no actor effects in our full model, it is possible that the effects of wives’ poor sleep on heart disease operated indirectly through psychological distress, biological systems, and physiological problems [49].
Our findings also indicated that insomnia symptoms may have had adverse consequences for heart disease at the couple level. Over and above the effects of one’s own insomnia symptoms, partner’s insomnia symptoms were also associated with an elevated likelihood of incident heart disease for husbands only. This finding was consistent with recent research on the dyadic nature of couple’s sleep, psychological distress, and heart disease risk [21, 27]. We speculate that when wives suffered from insomnia symptoms, their ability to monitor and exert social control regarding their husband’s health may have been compromised. Another explanation may be located in a body of research on spousal suffering and cardiovascular outcomes [30, 50]. It may be that husbands were more likely to keep their poor health symptoms to themselves [45], whereas wives were more likely to share their concerns with their partners; this, in turn, may have served as a source of stress that had health consequences for husbands [30].
Inspection of the coefficients and confidence intervals suggest a small partner effect for the insomnia index, whereas the partner effect for trouble falling asleep was the only insomnia symptom indicator that reached statistical significance. This was not surprising given the complex mechanism through which one’s sleep problems were potentially linked to partner’s heart health. As we are not aware of methodological strategies that allow for appropriately estimating effect sizes in the dyadic analyses based on GEE models, we were not able to provide specific estimates of effect sizes.
“Trouble falling asleep” was the only insomnia indicator that showed significant actor and partner effects (“trouble waking up early” also had a statistically significant actor effect, albeit only for husbands). The significant relationship between the trouble falling asleep and one’s own CVD was consistent with other studies in the scientific literature [13]. The significant partner effect of trouble falling asleep found in this study adds to our understanding of the negative health effects associated with this specific insomnia indicator. Trouble falling sleep is an important marker of psychological stress that may be related to heightened activity of the sympathetic nervous system and it is particularly pertinent in the context of CVD and CVD-related mortality [44]. The link between trouble falling asleep and CVD may have cross-spousal ramifications via mechanisms of stress contagion and health concordance [26, 51]. Identifying this specific symptom as a risk factor for heart disease may help target interventions for individuals and their partners suffering from this particular complaint.
Further research is needed to expand on the analyses reported here, especially with respect to alternative mechanisms not related to spouse’s insomnia, through which insomnia may be related to heart disease among middle-aged and older adults. For example, research has shown that relationship quality among couples was related to heart disease [52], and that insomnia and other sleep problems were related to relationship quality [32, 53]. We engaged in an elaboration analysis to determine whether relationship quality mediated the relationship between insomnia and incident heart disease among middle-aged and older adult couples but found no evidence that relationship quality was a pathway for this association for either wives or husbands.
Limitations
This study had limitations, including the lack of clinical evaluations of sleep problems. Some researchers question the clinical value of self-reported insomnia symptoms [54]. Questions have been raised about findings linking insomnia to CVD from studies that did not control for sleep apnea or other objective sleep duration measures [55]. Other researchers have argued that specific symptoms were a useful proxy for the core dysregulation of insomnia [48], and that insomnia symptoms, as a whole, may serve as general indicators of sleep problems that have consequences for health [56]. We are not aware of any published study that makes direct comparisons between the modified Jenkins Sleep Questionnaire [3]—the measure employed in our research and many other studies—and other well-established sleep measures, such as the Insomnia Severity Index or the Pittsburgh Sleep Quality Index. Because of a lack of data on clinical sleep measures in the HRS, we were also unable to make comparisons between subjective and objective indicators of sleep problems.
Self-report of height and weight for the BMI measure and of ever being diagnosed with heart disease (CVD) by a physician are potential limitations of this research. Past research has shown that specific self-reported heart conditions may be misclassified or under-reported by respondents, but also that these self-reported conditions have acceptable validity when heart disease is more broadly defined, as is the case in the present study [57, 58]. Additionally, the prevalence estimates of heart disease and other chronic conditions obtained in the HRS were similar to those estimated from the National Health Interview Survey (NHIS), which is a principle source of health information of the noninstitutionalized civilian U.S. population [59]. The high correspondence of chronic health conditions measured in the two surveys (HRS and NHIS) lends confidence regarding the measurement properties of the heart conditions reported by respondents in the HRS. A related limitation is that we were not able to examine how insomnia may be related to specific heart conditions due to our reliance on the RAND heart disease variable. Future research should address this issue.
Causal statements about the relationships found for insomnia and incident heart disease were not possible due to likely omitted variable bias and selection bias based on mortality [60]. Implicated unobserved variables include underlying biological and physiological conditions that may be associated with both self-reported sleep problems and heart disease. Furthermore, mortality risk is not distributed evenly in the population, as the risk was higher for men than women. Because we restricted the study sample to married couples alive at each observation point, the results reported here may reflect healthy-survivor selection effects. Finally, it is reasonable to assume a reciprocal relationship between incident heart disease and insomnia symptoms. The data and statistical techniques available to us do not permit examination of the potential reciprocity between our key variables; future research should address this possibility.
The HRS data did not allow us to determine whether couples actually slept together. The National Sleep Foundation reported that three out of ten couples sleep in separate beds. Separate sleeping arrangements may increase with age [61]. If a significant portion of middle-aged and older adults in the HRS, in fact, did not share a bed, this could result in weaker findings regarding the association between insomnia and incident heart disease. Chen has argued convincingly that dyadic sleep measures reflect not only sleep behaviors, but more generally interdependence among spouses in daily life, including sharing similar wake and sleep hours and other lifestyle behaviors [21]. The fact that we found dyadic effects given that some fraction of the sample likely did not sleep together suggests that our results may underestimate the association between insomnia and incident heart disease.
We also acknowledge that the sampling criteria employed in this study yield a younger and healthier study sample, particularly for women, as individuals were excluded from the sample when their spouse had CVD at baseline. It is worth noting that such sample selection likely makes our estimates more conservative, given that women’s CVD events are likely under-reported in this study sample.
Conclusions and Contributions
This study contributed to the scientific literature by examining the relationship between insomnia symptoms and heart disease among middle-aged and older adult couples using a prospective design with a large, national population-based sample. The study laid a foundation for future work that should investigate other mechanisms through which insomnia is related to health among persons who are in intimate partnerships across the adult life course. These mechanisms may include biological, physical, and mental health conditions, along with environmental conditions and variation in overall social integration. The results of this study underscored the need to find effective therapies for sleep problems to improve overall well-being among middle-aged and older adults and their partners.
Acknowledgments
The HRS is funded by the National Institute of Aging in the USA (grant number NIA U01AG009740) and the Social Security Administration.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards The authors Shih, Han and Burr declare that they have no conflict of interest. All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national).
Ethical Approval The University of Michigan Institutional Review Board granted ethical approval for the HRS (9/20/90 through 10/18/2018).
Informed Consent Informed consent was obtained from all participants.
Author Contributions YCS conceived of the study; YCS, SHH and JAB designed the study; SHH conducted the statistical analysis and YCS wrote the first draft of the manuscript; YCS, SHH and JAB interpreted the results, revised the manuscript for important intellectual content, and approved of the final manuscript for submission. All authors had full access to all of the data (including statistical reports and tables) in the study and take full responsibility for the integrity of the data and accuracy of the statistical analysis.
References
- 1. Kiecolt-Glaser JK, Wilson SJ. Lovesick: how couples’ relationships influence health. Annu Rev Clin Psychol. 2017;13:421–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Troxel WM. It’s more than sex: exploring the dyadic nature of sleep and implications for health. Psychosom Med. 2010;72:578–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jenkins CD, Stanton BA, Niemcryk SJ, Rose RM. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988;41:313–321. [DOI] [PubMed] [Google Scholar]
- 4. Lee JH, Chopik WJ, Schiamberg LB. Longitudinal associations between marital quality and sleep quality in older adulthood. J Behav Med. 2017;40:821–831. [DOI] [PubMed] [Google Scholar]
- 5. St-Onge MP, Grandner MA, Brown D, et al. ; American Heart Association Obesity, Behavior Change, Diabetes, and Nutrition Committees of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; and Stroke Council. Sleep duration and quality: Impact on lifestyle behaviors and cardiometabolic health: A scientific statement from the American Heart Association. Circulation. 2016;134:e367–e386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. 2013;17:241–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mesas AE, Guallar-Castillón P, López-García E, et al. Sleep quality and the metabolic syndrome: the role of sleep duration and lifestyle. Diabetes Metab Res Rev. 2014;30:222–231. [DOI] [PubMed] [Google Scholar]
- 8. Phillips B, Mannino DM. Do insomnia complaints cause hypertension or cardiovascular disease?J Clin Sleep Med. 2007;3:489–494. [PMC free article] [PubMed] [Google Scholar]
- 9. Bonnet MH, Arand DL. Cardiovascular implications of poor sleep. Sleep Med Clin. 2007;2:529–538. [Google Scholar]
- 10. Jaussent I, Dauvilliers Y, Ancelin ML, et al. Insomnia symptoms in older adults: Associated factors and gender differences. Am J Geriatr Psychiatry. 2011;19:88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li M, Zhang XW, Hou WS, Tang ZY. Insomnia and risk of cardiovascular disease: A meta-analysis of cohort studies. Int J Cardiol. 2014;176:1044–1047. [DOI] [PubMed] [Google Scholar]
- 12. Loeys T, Cook W, De Smet O, Wietzker A, Buysse A. The actor-partner interdependence model for categorical dyadic data: A user-friendly guide to GEE. Pers Relatsh. 2014;21:225–241. [Google Scholar]
- 13. He Q, Zhang P, Li G, Dai H, Shi J. The association between insomnia symptoms and risk of cardio-cerebral vascular events: a meta-analysis of prospective cohort studies. Eur J Prev Cardiol. 2017;24:1071–1082. [DOI] [PubMed] [Google Scholar]
- 14. Clark AJ, Salo P, Lange T, et al. Onset of impaired sleep and cardiovascular disease risk factors: A longitudinal study. Sleep. 2016;39:1709–1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Suka M, Yoshida K, Sugimori H. Persistent insomnia is a predictor of hypertension in Japanese male workers. J Occup Health. 2003;45:344–350. [DOI] [PubMed] [Google Scholar]
- 16. Vgontzas AN, Liao D, Bixler EO, Chrousos GP, Vela-Bueno A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32:491–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Laugsand LE, Strand LB, Platou C, Vatten LJ, Janszky I. Insomnia and the risk of incident heart failure: a population study. Eur Heart J. 2014;35:1382–1393. [DOI] [PubMed] [Google Scholar]
- 18. Laugsand LE, Vatten LJ, Platou C, Janszky I. Insomnia and the risk of acute myocardial infarction: a population study. Circulation. 2011;124:2073–2081. [DOI] [PubMed] [Google Scholar]
- 19. Canivet C, Nilsson PM, Lindeberg SI, Karasek R, Östergren PO. Insomnia increases risk for cardiovascular events in women and in men with low socioeconomic status: a longitudinal, register-based study. J Psychosom Res. 2014;76:292–299. [DOI] [PubMed] [Google Scholar]
- 20. Motivala SJ. Sleep and inflammation: Psychoneuroimmunology in the context of cardiovascular disease. Ann Behav Med. 2011;42:141–152. [DOI] [PubMed] [Google Scholar]
- 21. Chen JH. Couples’ sleep and psychological distress: A dyadic perspective. J Gerontol B Psychol Sci Soc Sci. 2017;73:30–39. [DOI] [PubMed] [Google Scholar]
- 22. Sin NL, Almeida DM, Crain TL, Kossek EE, Berkman LF, Buxton OM. Bidirectional, temporal associations of sleep with positive events, affect, and stressors in daily life across a week. Ann Behav Med. 2017;51:402–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Williams PG, Cribbet MR, Rau HK, Gunn HE, Czajkowski LA. The effects of poor sleep on cognitive, affective, and physiological responses to a laboratory stressor. Ann Behav Med. 2013;46:40–51. [DOI] [PubMed] [Google Scholar]
- 24. Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: Results of the 1991 National Sleep Foundation Survey. I. Sleep. 1999;22 (Suppl 2):S347–S353. [PubMed] [Google Scholar]
- 25. Penev PD. Update on energy homeostasis and insufficient sleep. J Clin Endocrinol Metab. 2012;97:1792–1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Di Castelnuovo A, Quacquaruccio G, Donati MB, de Gaetano G, Iacoviello L. Spousal concordance for major coronary risk factors: a systematic review and meta-analysis. Am J Epidemiol. 2009;169:1–8. [DOI] [PubMed] [Google Scholar]
- 27. Smith TW, Baucom BRW. Intimate relationships, individual adjustment, and coronary heart disease: Implications of overlapping associations in psychosocial risk. Am Psychol. 2017;72:578–589. [DOI] [PubMed] [Google Scholar]
- 28. Rendall MS, Weden MM, Favreault MM, Waldron H. The protective effect of marriage for survival: a review and update. Demography. 2011;48:481–506. [DOI] [PubMed] [Google Scholar]
- 29. Manfredini R, De Giorgi A, Tiseo R, et al. Marital status, cardiovascular diseases, and cardiovascular risk factors: a review of the evidence. J Womens Health (Larchmt). 2017;26:624–632. [DOI] [PubMed] [Google Scholar]
- 30. Schulz R, Beach SR, Hebert RS, et al. Spousal suffering and partner’s depression and cardiovascular disease: the cardiovascular health study. Am J Geriatr Psychiatry. 2009;17:246–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Settersten RA. Age structuring and the rhythm of the life course. In: Mortimer JT, Shanahan MJ, eds. Handbook of the Life Course. Boston, MA: Springer; 2003. [Google Scholar]
- 32. Hasler BP, Troxel WM. Couples’ nighttime sleep efficiency and concordance: Evidence for bidirectional associations with daytime relationship functioning. Psychosom Med. 2010;72:794–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Walker RB, Luszcz MA, Hislop J, Moore V. A gendered lifecourse examination of sleep difficulties among older women. Ageing Soc. 2011;32:219–238. [Google Scholar]
- 34. Venn S, Arber S, Meadows R, Hislop J. The fourth shift: exploring the gendered nature of sleep disruption among couples with children. Br J Sociol. 2008;59:79–97. [DOI] [PubMed] [Google Scholar]
- 35. Ulfberg J, Carter N, Talbäck M, Edling C. Adverse health effects among women living with heavy snorers. Health Care Women Int. 2000;21:81–90. [DOI] [PubMed] [Google Scholar]
- 36. Venn S. ‘It’s okay for a man to snore’: the influence of gender on sleep disruption in couples. Sociol Res Online. 2007;12:1–14. [Google Scholar]
- 37. August KJ, Sorkin DH. Marital status and gender differences in managing a chronic illness: the function of health-related social control. Soc Sci Med. 2010;71:1831–1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Strawbridge WJ, Shema SJ, Roberts RE. Impact of spouses’ sleep problems on partners. Sleep. 2004;27:527–531. [DOI] [PubMed] [Google Scholar]
- 39. Ferraro KF, Su YP, Gretebeck RJ, Black DR, Badylak SF. Body mass index and disability in adulthood: a 20-year panel study. Am J Public Health. 2002;92:834–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chen JH, Waite L, Kurina LM, Thisted RA, McClintock M, Lauderdale DS. Insomnia symptoms and actigraph-estimated sleep characteristics in a nationally representative sample of older adults. J Gerontol A Biol Sci Med Sci. 2015;70:185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kim ES, Hershner SD, Strecher VJ. Purpose in life and incidence of sleep disturbances. J Behav Med. 2015;38: 590–597. [DOI] [PubMed] [Google Scholar]
- 42. Willenbring ML, Massey SH, Gardner MB. Helping patients who drink too much: An evidence-based guide for primary care clinicians. Am Fam Physician. 2009;80:44–50. [PubMed] [Google Scholar]
- 43. Elwood P, Hack M, Pickering J, Hughes J, Gallacher J. Sleep disturbance, stroke, and heart disease events: evidence from the Caerphilly cohort. J Epidemiol Community Health. 2006;60:69–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med. 2002;251:207–216. [DOI] [PubMed] [Google Scholar]
- 45. Venn S, Meadows R, Arber S. Gender differences in approaches to self-management of poor sleep in later life. Soc Sci Med. 2013;79:117–123. [DOI] [PubMed] [Google Scholar]
- 46. Mezick EJ, Hall M, Matthews KA. Are sleep and depression independent or overlapping risk factors for cardiometabolic disease?Sleep Med Rev. 2011;15:51–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33:414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Troxel WM, Buysse DJ, Matthews KA, et al. Sleep symptoms predict the development of the metabolic syndrome. Sleep. 2010;33:1633–1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Cappuccio FP, Miller MA, Lockley SW. The epidemiology of sleep and cardiovascular risk and disease. In: Cappuccio FP, Miller MA, Lockley SW, eds. Sleep, Health and Society: From Aetiology to Public Health. New York, NY: Oxford University Press; 2010. [Google Scholar]
- 50. Monin JK, Schulz R, Martire LM, Jennings JR, Lingler JH, Greenberg MS. Spouses’ cardiovascular reactivity to their partners’ suffering. J Gerontol B Psychol Sci Soc Sci. 2010;65B:195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Doerr JM, Nater UM, Ehlert U, Ditzen B. Co-variation of fatigue and psychobiological stress in couples’ everyday life. Psychoneuroendocrinology. 2018;92:135–141. [DOI] [PubMed] [Google Scholar]
- 52. De Vogli R, Chandola T, Marmot MG. Negative aspects of close relationships and heart disease. Arch Intern Med. 2007;167:1951–1957. [DOI] [PubMed] [Google Scholar]
- 53. Ailshire JA, Burgard SA. Family relationships and troubled sleep among U.S. adults: examining the influences of contact frequency and relationship quality. J Health Soc Behav. 2012;53:248–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Buysse DJ, Germain A, Moul DE. Diagnosis, epidemiology, and consequences of insomnia. Prim psychiatry. 2005;12:37–44. [Google Scholar]
- 55. Bonnet MH. Evidence for the pathophysiology of insomnia. Sleep. 2009;32:441–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Chen JH, Waite L, Kurina LM, Thisted RA, McClintock M, Lauderdale DS. Insomnia symptoms and actigraph-estimated sleep characteristics in a nationally representative sample of older adults. J Gerontol A Biol Sci Med Sci. 2015;70:185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lampe FC, Walker M, Lennon LT, Whincup PH, Ebrahim S. Validity of a self-reported history of doctor-diagnosed angina. J Clin Epidemiol. 1999;52:73–81. [DOI] [PubMed] [Google Scholar]
- 58. O’Donnell CJ, Glynn RJ, Field TS, et al. Misclassification and under-reporting of acute myocardial infarction by elderly persons: Implications for community-based observational studies and clinical trials. J Clin Epidemiol. 1999;52:745–751. [DOI] [PubMed] [Google Scholar]
- 59. Fisher GG, Faul JD, Weir DR, Wallace RB.. Documentation of Chrinoc Disease Measures in the Health and Retirement Study (HRS/AHEAD). 2005. HRS/AHEAD Documentation Report, DR-009. Available at https://hrs.isr.umich.edu/publications/biblio/5619. Accessibility verified April 22, 2018. [Google Scholar]
- 60. Helbig AK, Stöckl D, Heier M, Ladwig KH, Meisinger C. Symptoms of insomnia and sleep duration and their association with incident strokes: Findings from the population-based MONICA/KORA Augsburg cohort study. PLoS One. 2015;10:e0134480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Drake C, Kryger M, Phillips B.. 2005 Sleep in America Poll: Adult Sleep Habits and Styles. Washington, DC: National Sleep Foundation; 2005. [Google Scholar]