Abstract
The study examined how ‘transition readiness’ skills develop from relationship processes with parents, friends, and healthcare providers. During their senior year of high school and one year later, participants (N = 217) with type 1 diabetes completed measures of transition readiness skills (Self-Management; Self-Advocacy), adherence, HbA1c, and relationships with providers (patient-centered communication), parents (monitoring/knowledge), and friends (knowledge/helpfulness) surrounding diabetes. Self-Management skills increased across time. Higher friend knowledge/helpfulness during emerging adulthood was associated with increased Self-Management skills. Adherence improved when relationships with providers and friends matched transition readiness skills, indicating that these relationships may facilitate transition skills in early emerging adulthood.
Emerging adulthood is considered a high risk time for type 1 diabetes, as diabetes care and glycemic control is especially poor compared to other ages (Miller et al., 2015). Diabetes management relies heavily on individuals’ adherence to daily self-care behaviors, such as checking blood glucose many times per day, adjusting and administering insulin, and monitoring and adjusting food intake (e.g. Iannotti et al., 2014). Emerging adults with type 1 diabetes also assume more responsibility for their daily self-care as they move from pediatric to adult care (Hanna et al., 2013; Weissberg-Benchell, Wolpert, & Anderson, 2007) concurrently with other normative changes (e.g. attending college, moving away from home and entering the workforce) (Arnett, 2000). As a result, researchers have sought to better understand this transitional process (Sheehan, While, & Coyne, 2015; Van Staa, Van Der Stege, Jedeloo, Moll, & Hilberink, 2011) and identify specific skills that are associated with successful illness management during this high risk time (Peters & Laffel, 2011). ‘Transition readiness’ skills (e.g. managing medications and interacting independently with healthcare providers) refer to specific skills believed to help prepare emerging adults for successful independent diabetes management in the context of the transfer to adult care, beyond other self-care behaviors (Schwartz et al., 2014).
Despite the posited importance of transition readiness skills (Peters & Laffel, 2011), no data are available as to what factors contribute to their development or whether these skills change across late adolescence into early emerging adulthood. Although cross-sectional age differences suggest transition readiness skills increase between adolescence and emerging adulthood (Sawicki et al., 2011), consistent with the idea that adolescents assume greater independent responsibility for their diabetes care behaviors, it is largely unknown whether transition readiness skills change within person during this period. Similarly, there is little evidence as to whether transition readiness skills prospectively predict health outcomes during early emerging adulthood (Schwartz et al., 2014). Only one study has looked at this issue, indicating that feeling ‘ready’ for the transfer to adult care was not associated with diabetes outcomes after transfer (Garvey et al., 2012). As evidence of the importance of examining transition readiness skills, the American Diabetes Association (ADA) recommends including individuals’ diabetes-related capabilities in the transfer to adult care (Peters & Laffel, 2011). Further, it is possible that those who transfer to adult care with lower transition readiness skills may experience the poorest of outcomes. In both new and existing relationships with healthcare providers, emerging adults are expected to navigate their health needs more independently than at younger ages (e.g. Monaghan, et al., 2013; Weissberg-Benchell et al., 2007). It is currently unknown whether transition readiness skills are utilized in the transfer to adult care or how they are associated with health outcomes after transfer.
Like other self-care skills, transition readiness skills do not develop in a social vacuum (e.g. Modi et al., 2012). Other people, including parents, diabetes healthcare providers, and friends, may foster or interfere with the development of transition readiness skills, much as they foster or interfere with good adherence behaviors. However, different relationship figures may influence illness through different relationship processes. For example, across childhood and adolescence, high parental involvement is associated with better adherence and metabolic control (King, Berg, Butner, Butler, & Wiebe, 2014). Parents who are more knowledgeable and engage in higher levels of monitoring of their adolescent’s diabetes activities may provide the scaffold for adolescents to learn to be good advocates for themselves in the healthcare setting and take responsibility for tasks previously completed by parents (e.g., filling prescriptions, dealing with insurance companies). Healthcare providers foster better adherence and diabetes outcomes when they provide patient-centered care and open communication (Croom et al., 2011; Monaghan, Hilliard, Sweenie, & Riekert, 2013) and this may extend to the fostering of transition readiness skills. Finally, friend knowledge of and involvement in daily management may also influence adherence and diabetes outcomes (e,g, Palladino & Helgeson, 2012).
By early emerging adulthood, not only does the need for increased independence in self-care become more pressing, but existing relationships also are changing. Parents become less involved or in the know about their children’s diabetes management (King et al., 2014). Peers may become more knowledgeable, involved and supportive surrounding diabetes (Pendley et al., 2002), although whether such peer support is beneficial for diabetes outcomes is unclear (Palladino & Helgeson, 2012). Moreover, emerging adults begin to leave their pediatric providers and embark in new relationships with adult care providers (e.g. (Weissberg-Benchell et al., 2007). Although these relationship processes are associated with other aspects of self-care in adolescence, it is currently unknown whether they are associated with the development of transition readiness skills.
The fit between the involvement of relationships and transition readiness skills may be especially important in understanding changes in adherence and metabolic control across the transition out of high school. For instance, higher parental involvement is especially beneficial for adolescents with low perceived competence to complete diabetes tasks (Palmer et al., 2009; Wiebe et al., 2014). As friends may become utilized more in diabetes management during emerging adulthood, knowledgeable friend involvement may serve to compensate for low transition readiness skills. In addition, mismatches between relationship processes and transition readiness skills may be especially challenging. For example, emerging adults may endeavor to advocate for themselves in the presence of a healthcare provider who is not perceived to be open to such advocacy. Examining these potential mismatches during a sensitive time for diabetes management may provide an avenue for ensuring better diabetes outcomes.
The present study examined transition readiness skills prospectively from the senior year of high school to one year later. First, we examined how transition readiness skills changed across this time period. Second, we explored how relationship processes with diabetes healthcare providers, parents, and friends across time were associated with the development of transition readiness skills in early emerging adulthood and whether relationship processes moderated the associations between transition readiness skills and glycemic control and adherence. We predicted that 1) transition readiness skills would increase after the senior year of high school; 2) greater patient-centered communication with diabetes healthcare providers, greater knowledge/monitoring from parents, and greater knowledge/helpfulness from friends would relate to higher transition readiness skills initially and increases across time; and 3) greater transition readiness skills would support good diabetes management and outcomes across early emerging adulthood, but perceptions of others’ involvement in and knowledge of typical diabetes management would moderate these associations. In addition to the above main aims, we examined whether transition readiness skills were associated with diabetes outcomes differently for individuals who transferred to adult care compared with those who had not, independent of relationship processes.
Participants and Methods
Research Design
As part of a multisite, multi-year study on diabetes management in emerging adulthood, late adolescents from pediatric endocrinology clinics in two Southwestern United States cities participated in a longitudinal study. Both clinics generally transferred patients to adult care at age 18, although this varied across individual providers and patients. Participants were eligible if they were in their senior year of high school, had been diagnosed with type 1 diabetes for at least one year, and spoke English as their primary language (Author’s Citation). Participants completed measures through online surveys and HbA1c assay kits at both time points.
Of 504 eligible participants approached, 247 enrolled, 242 completed Time 1 measures, and 217 (88% of the initial sample) completed Time 2 measures. Analyses were run on participants who completed both Time 1 and Time 2 measures (n = 217). Reasons for nonparticipation included lack of interest (33%) and being too busy (34%). Of the 25 participants who completed measures at Time 1 but did not complete measures at Time 2: 5 (20%) officially withdrew after contact with the study team at Time 2; 3 (12%) officially withdrew after contact with the study team at a later assessment; 9 (36%) remained in the study and completed study measures at a later assessment; and, 8 (32%) were lost to follow-up but did not officially withdraw from the study. No differences emerged on Time 1 transition readiness skills or adherence between participants who did versus did not complete Time 2, but completers had significantly lower Time 1 HbA1c values (M = 8.19% vs 9.25%, 66 mmol vs 78 mmol; t(238) = 3.08, p < .01; Mdiff = 1.06, 95% CI = [.31, 1.74]). The study was approved by the appropriate Institutional Review Boards. Parents provided informed consent and participants provided assent or consent. Participants providing only assent provided consent one year later.
At Time 1, participants’ (N = 217) average age was 17.77 (SD = .40), 64.5% were female, average time since diagnosis was 7.39 years (SD = 3.82), 42.6% were on an insulin pump, and average HbA1c was 8.2% (SD = 1.62; 66 mmol/mol, SD = 17.71). Of the participants who reported both race and ethnicity, 76.5% identified as non-Hispanic White/Caucasian, 5.4% identified as non-Hispanic Black/African American, 13.2% identified as Hispanic, and 7.4% identified as either Asian, Native Hawaiian/Pacific Islander, Native American, or more than one race. Socioeconomic status was approximated via mother’s education level at Time 1: 13.8% of mothers reported having a secondary school education or less, 42.6% having some college or a vocational degree, and 43.7% having a bachelor’s degree or higher.
At Time 2, participants’ average age was 18.81 (SD = .40) and 46.0% used an insulin pump. Most participants reported receiving routine care for their diabetes (80.5%). Independent of regular routine care, the majority of participants also reported receiving a diabetes check-up within the previous 6 months (89.3%) and only 1.4% had not received a diabetes check-up in the past year. Few participants reported any diabetes-related emergency room visits (9.3%) or hospitalizations (7.5%) in the previous six months. About half of participants stated they had transferred to adult care (53.3%).
Transition Readiness Skills
Participants completed a shortened 15-item version of the Transition Readiness Assessment Questionnaire (TRAQ). We selected items that loaded most highly, at least .50, on each subscale (Sawicki et al., 2011) to reduce participant burden. The shortened TRAQ was comprised of two subscales: Self-Management (11 items, e.g., “Do you order your medications before they run out?”) and Self-Advocacy (4 items, e.g., “Do you answer questions that are asked by the doctor, nurse, or clinic staff?”). Items measured participants’ independence in performing behaviors for illness management. Item responses included: 1 (“I do not know how to do this”), 2 (“I do not know how but I want to learn how to do this”), 3 (“I am learning to do this), 4 (“I am starting to do this”), and 5 (“I always do this when I need to”).
The structure of the shortened TRAQ was similar to the original measure (Sawicki et al., 2011) in that a two-factor solution emerged using a principal components analysis. Two items did not load strongly on either factor and were removed. A principal components analysis on the remaining 13 items yielded the same two factor solution accounting for 54.93% of the variance with good overall reliability (ɑ = .88), and good to acceptable subscale reliability (Self-Management ɑ = .91; Self-Advocacy ɑ = .64) at Time 1. Subscale reliability increased at Time 2 (Self-Management ɑ = .92; Self-Advocacy ɑ = .71).
Provider, Parent, and Friend Relationships
Participants completed measures to assess diabetes-specific components of their own perceptions of aspects of their relationships with their main diabetes care provider, parents, and friends.
The Health Care Climate Questionnaire – Short Form assessed participants’ perceived patient-centered communication with their providers. Items consisted of aspects of the patient-provider relationship that reflect patient-centered care (e.g. “My doctor encourages me to ask questions about managing my diabetes”). This measure consisted of 5-items, on a scale from 1 (“strongly disagree”) to 5 (“strongly agree”). Items were averaged to create an overall score which had good reliability (Time 1 ɑ = .91; Time 2 ɑ = .92).
To assess perceptions of parental involvement in diabetes care, participants completed the Parental Monitoring Scale (Berg et al., 2008). The Parental Monitoring Scale (Berg et al., 2008) measured participants’ reports of their mothers’ and fathers’ knowledge about their everyday diabetes management. This 7-item measure assessed how much participants’ mothers and fathers “really know” about their current diabetes self-management (e.g. “How much does your mother/father REALLY know how much insulin you have given yourself?”) on a scale from 1 (“doesn’t know”) to 5 (“knows everything”). Questions were asked separately for perceptions of mother and father involvement and were averaged separately for mothers (Time 1 ɑ = .94; Time 2 ɑ = .94) and fathers (Time 1 ɑ = .96; Time 2 ɑ = .95).
Friend knowledge/helpfulness for diabetes was assessed using an average score of three items created for this study: whether the friends they spend the most time with: “know I have diabetes;” “are helpful in providing support for my diabetes;” and, “know what to do when I have an emergency with my diabetes.” The friend knowledge/helpfulness sought to assess how much friends may be involved in everyday diabetes care and participants’ perceptions of whether their friends were helpful in providing diabetes-related support. Each item was rated on a scale from 1 (“strongly disagree”) to 5 (“strongly agree”). A principal components analysis yielded a one component solution, accounting for 67.46% of the variance. Reliability was moderate at Time 1 (ɑ = .64) but stronger at Time 2 (ɑ = .76).
Diabetes Management and Transfer to Adult Care.
Glycemic control was measured using dried blood spot HbA1c Assay Kits provided and processed by CoreMedica Laboratories, accredited by the College of American Pathologists. Blood samples were obtained in lab at Time 1 and through mail-in kits at Time 2. This approach was chosen over obtaining HbA1c from medical records to ensure that the same procedures were used across time periods (even as participants changed providers across time) and that HbA1c could be obtained from all participants (as poor clinic attendance is common in this age group, e.g. Sheehan et al., 2015).
Adherence was assessed using the Diabetes Behavior Rating Scale (DBRS) (Iannotti et al., 2006), which consisted of 37 items, rated on a scale from 1 (“never”) to 5 (“always”), regarding how often they engaged in various diabetes management behaviors during the past week. The DBRS had good reliability for both pump (Time 1 ɑ = .84; Time 2 ɑ = .87) and non-pump users (Time 1 ɑ = .83; Time 2 ɑ = .83).
At Time 2 only, participants indicated whether they had switched from their pediatric diabetes provider to an adult provider in the past year (yes or no).
Analysis
All analyses were run using SPSS Version 23 (IBM Corp., 2013) and all statistical tests used a designated value of p < .05 to determine significance of findings. We first examined correlations of study variables. Next, we assessed changes in transition readiness skills from Time 1 to Time 2 using paired-samples t-tests. Third, we ran a series of multiple regression analyses. Gender was entered as a covariate on step 1 of all regression models, as males had lower Time 2 Self-Advocacy scores in our sample (t(125.90) = 2.25, p = .03; Mdiff = .22, 95% CI = [.03, .40]), consistent with other findings of gender differences in transition skills (Sawicki et al., 2011). Years since diagnosis also was included on step 1 of all models as a covariate, as it is a known predictor of HbA1c (Clements et al., 2014).
All regression models assessed residualized change, such that Time 2 variables were examined in predicting outcomes after those same Time 1 variables were entered into the model. Multicollinearity was assessed for all variables. No variable exceeded current conventions of VIF > 6 (observed range VIF = 1.00 to 4.16). The first set of multiple regressions assessed diabetes-specific relationship processes across relationships (i.e., provider, parents, and/or friends) and whether processes at Time 1 and Time 2 (controlling for Time 1) were associated with changes in transition readiness skills across time. A second set of multiple regressions addressed whether transition readiness skills were associated with changes in HbA1c or adherence and whether relationship processes moderated the associations between transition readiness skills and HbA1c or adherence.
First, we examined whether Time 1 transition readiness skills along with relationship processes predicted changes in adherence and HbA1c from Time 1 to Time 2. All predictor variables and covariates were grand-mean centered in all models. Interaction terms were created using centered Time 1 patient-centered communication, mother knowledge, father knowledge, or friend knowledge/helpfulness times centered Time 1 Self-Management and Time 1 Self-Advocacy skills. Covariates (i.e. gender, time since diagnosis, and Time 1 outcome variables) were entered on Step 1. Centered Time 1 patient-centered communication, mother knowledge, father knowledge or friend knowledge/helpfulness were entered on Step 2, along with centered Time 1 Self-Management skills and Time 1 Self-Advocacy skills. For the patient-centered communication regression model only, participants’ transfer status also was entered on Step 2 to control for the influence of any change in diabetes providers. Interaction terms were entered on Step 3 (Time 1 relationship variable X Time 1 Self-Management skills and Time 1 relationship variable X Time 1 Self-Advocacy skills). For all analyses that yielded significant interactions, simple slopes were tested and the interaction graphed using Dawson’s unstandardized two-way interaction utility for Microsoft Excel (Dawson, n.d.).
Finally, as roughly half of our sample moved out of pediatric care by Time 2 and the transfer to adult care may be a pivotal milestone for emerging adults with diabetes, a third set of multiple regressions examined whether transferring to adult care moderated the relationship between transition readiness skills and diabetes outcomes. Centered covariates were entered on Step 1. Centered Time 1 Self-Management skills and Time 1 Self-Advocacy skills and uncentered transfer status were entered on Step 2. Time 1 Self-Management skills by Transfer Status and Time 1 Self-Advocacy skills by Transfer Status were entered on Step 3.
Results
Preliminary Analyses
Descriptive statistics and correlations of study variables are found in Table 1. Transition readiness skills were generally associated with relationship variables, suggesting that higher levels of provider communication, parent knowledge/monitoring, and friend knowledge/helpfulness were associated with higher transition readiness skills. Higher transition readiness skills also correlated with better adherence; however, only greater Self-Advocacy skills were associated with lower HbA1c.
Table 1.
Correlations and Descriptives for Predictor and Outcome Variables
| Time 1 |
||||||||
| Time 1 Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | M (SD) |
| 1. Self-Management | --- | --- | --- | --- | --- | --- | --- | 3.03 (.99) |
| 2. Self-Advocacy | .16* | --- | --- | --- | --- | --- | --- | 4.41 (.63) |
| 3. Patient-Centered Communication | -.01 | .15* | --- | --- | --- | --- | --- | 4.06 (.85) |
| 4. Mother Knowledge | .16** | .25*** | .23** | --- | --- | --- | --- | 3.24 (1.03) |
| 5. Father Knowledge | .21** | .22** | .08 | .59*** | --- | --- | --- | 2.71 (1.14) |
| 6. Friend Knowledge/Helpfulness | .32*** | .35*** | .09 | .37*** | .47*** | --- | --- | 4.07 (.73) |
| 7. HbA1c | -.02 | -.20** | -.14* | -.14+ | -.14* | .05 | --- | 8.19 (1.62) |
| 8. Adherence | .20** | .39*** | .26*** | .43*** | .35*** | .36*** | -.22** | .61 (.12) |
| Time 2 |
||||||||
| Time 2 Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | M (SD) |
| 1. Self-Management | --- | --- | --- | --- | --- | --- | --- | 3.64 (.95) |
| 2. Self-Advocacy | .36*** | --- | --- | --- | --- | --- | --- | 4.45 (.63) |
| 3. Patient-Centered Communication | .09 | .12 | --- | --- | --- | --- | --- | 4.01 (.86) |
| 4. Mother Knowledge | .09 | .21** | .15* | --- | --- | --- | --- | 2.80 (1.12) |
| 5. Father Knowledge | .17* | .19* | .07 | .68*** | --- | --- | --- | 2.28 (1.02) |
| 6. Friend Knowledge/Helpfulness | .24** | .21** | .29*** | .20*** | .25** | --- | --- | 3.95 (.93) |
| 7. HbA1c | .04 | -.14* | -.09 | -.07 | -.02 | -.16* | --- | 8.95 (1.91) |
| 8. Adherence | .22** | .35*** | .26*** | .41*** | .37*** | .24*** | -.25** | .59 (.13) |
Note. p < .06.
p < .05.
p < .01.
p < .001.
HbA1c is listed in NGSP units. In IFCC units, mean HbA1c is 66 mmol/mol (SD = 17.71) at Time 1 and 74 mmol/mol (SD = 20.88) at Time 2.
Change in Transition Readiness Skills
A paired-samples t-test revealed a significant increase in Self-Management skills from Time 1 to Time 2 (t(190) = 8.75, p < .001; Mdiff = .60, 95% CI = [.47, .74]), but no change in the mean of Self-Advocacy skills (t(200) = 1.00, p = .32; Mdiff = .05, 95% CI = [−.05, .15]). Increases were evident in all Self-Management items across time indicating participants on average moved from reporting “I’m learning how to do this” toward the “I’m starting to do this” stage of skill mastery. For Self-Advocacy items, participants reported high competence at Time 1, with little change occurring over the subsequent year.
Relationships and Change in Transition Readiness
To examine how relationship processes, initially and one year out of high school, were associated with changes in transition readiness skills, two multiple regression analyses were conducted (see Table 2). For Self-Management skills, Time 1 relationship variables were not associated with changes in Self-Management, but some Time 2 relationship variables were significant. Specifically, Time 2 patient-centered communication and friend knowledge/helpfulness, controlling for Time 1, were both significantly associated with increases in Self-Management skills. Time 1 mother knowledge was associated with greater increases in Self-Advocacy skills, whereas Time 1 patient-centered communication trended towards a negative association with changes in Self-Advocacy, though failed to reach statistical significance (p = .05). Time 2 mother and father knowledge, friend knowledge/helpfulness, and patient-centered communication were not significantly associated with changes in Self-Advocacy.
Table 2.
Predicting Change in Transition Readiness from Change in Relationship Factors
| Time 2 Self-Management |
Time 2 Self-Advocacy |
|||||
|---|---|---|---|---|---|---|
| R2Δ | βin | 95% CI | R2Δ | βin | 95% CI | |
| Step 1 | .21*** | .19*** | ||||
| Gender | -.01 | [−.33, .28] | -.23** | [−.50, −.08] | ||
| Years Since Diagnosis | -.03 | [−.04, .03] | .10 | [−.01, .04] | ||
| Time 1 Self-Management | .44*** | [.24, .53] | .09 | [−.05, .15] | ||
| Time 1 Self-Advocacy | .05 | [−.18, .33] | .31*** | [.15, .50] | ||
| Step 2 | .02 | .07* | ||||
| Time 1 Patient-Centered Communication | -.12 | [−.31, .06] | -.17+ | [−.25, .00] | ||
| Time 1 Mother Knowledge | .05 | [−.15, .23] | .25* | [.02, .27] | ||
| Time 1 Father Knowledge | -.05 | [−.29, .09] | -.02 | [−.12, .10] | ||
| Time 1 Friend Knowledge/Helpfulness | .10 | [−.25, .24] | .04 | [−.14, .20] | ||
| Step 3 | .13** | .02 | ||||
| Time 2 Patient-Centered Communication | .23** | [.06, .42] | .11 | [−.05, .21] | ||
| Time 2 Mother Knowledge | -.03 | [−.28, .24] | -.04 | [−.21, .17] | ||
| Time 2 Father Knowledge | .16 | [−.11, .39] | .13 | [−.10, .26] | ||
| Time 2 Friend Knowledge/Helpfulness | .22* | [.03, .40] | .01 | [−.13, .14] | ||
Note. p < .06.
p < .05.
p < .01.
p < .001 Males coded as 0 and females coded as 1.
Transition Readiness Skills Moderated by Social Relationships in Relation to Diabetes Outcomes
Regressions were conducted to examine whether transition readiness skills at Time 1 were moderated by relationship processes in predicting changes in adherence or HbA1c. No main effects emerged for Time 1 Self-Management skills or Time 1 Self-Advocacy skills on either HbA1c or adherence. Thus, transition skills at Time 1 did not predict changes in either adherence or HbA1c across this one year period.
Two moderations were found in predicting adherence (see Table 3). A significant Time 1 Self-Advocacy by Time 1 patient-centered communication interaction revealed that higher Self-Advocacy skills were associated with better adherence among individuals who reported higher patient-centered communication but were associated with lower adherence among individuals who reported lower levels of patient-centered communication (see Figure 1). Testing of simple slopes indicated that the slope of the line was significant for participants high in patient-centered communication at + 1 SD above the mean (t = 2.74, p = .01; Cohen’s d = .40, 95% CI = [.06,.34]) and for participants low in patient-centered communication at – 1 SD below the mean (t = −2.11, p = .04; Cohen’s d = −.31, 95% CI = [.01,.30]).
Table 3.
Predicting Adherence from Baseline Transition Readiness and Interactions with Patient-Centered Communication and Friend Knowledge/Support
| Time 2 Adherence |
Time 2 Adherence |
||||||
|---|---|---|---|---|---|---|---|
| R2Δ | βin | 95% CI | R2Δ | βin | 95% CI | ||
| Step 1 | .49*** | Step 1 | .45*** | ||||
| -Gender | .08 | [−.01, .05] | -Gender | .07 | [−.01, .05] | ||
| -Years Since Diagnosis | .05 | [−.00, .01] | -Years Since Diagnosis | .03 | [−.00, .01] | ||
| -Time 1 Adherence | .70*** | [.61, .82] | -Time 1 Adherence | .67*** | [.57, .81] | ||
| Step 2 | .01 | Step 2 | .03* | ||||
| -Time 1 Self-Management | .02 | [−.01, .02] | -Time 1 Self-Management | -.04 | [−.02, .01] | ||
| -Time 1 Self-Advocacy | -.06 | [−.04, .01] | -Time 1 Self-Advocacy | -.11 | [−.05, .01] | ||
| -Time 1 PCC | -.04 | [−.02, .01] | -Time 1 Friend K/H | .20** | [.01, .06] | ||
| -Time 2 Transfer Status | .03 | [−.03, .03] | |||||
| Step 3 | .02* | Step 3 | .02 | ||||
| -T1 SM * T1 PCC | -.08 | [−.03, .00] | -T1 SM * T1 Friend K/H | -.13* | [−.04, −.00++] | ||
| -T1 SA * T1 PCC | .12* | [.00+, .06] | -T1 SA * T1 Friend K/H | .01 | [−.03, .04] | ||
Note. All variables grand mean centered. T1 SM = Time 1 Self-Management. T1 SA = Time 1 Self-Advocacy. PCC = Patient-Centered Communication. Friend K/H = Friend Knowledge/Helpfulness.
95% CI = .003.
95% CI = −.001.
p < .05.
p < .01.
p < .001.
Figure 1.
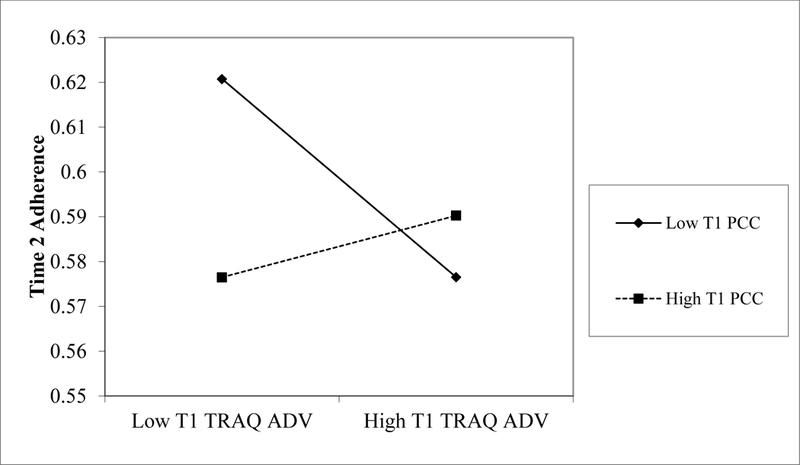
Plot of interaction between Time 1 Self-Advocacy by Time 1 Patient-Centered Communication on Time 2 Adherence Controlling for Time 1 Adherence.
The Time 1 Self-Management by Time 1 friend knowledge/helpfulness interaction was also significant, indicating that lower Self-Management skills were associated with better adherence among individuals who reported higher levels of friend knowledge/helpfulness (see Figure 2). Testing of simple slopes indicated that, the slope of the line was only statistically different from zero for participants high in friend knowledge/support at +1 SD above the mean (t = −2.28, p = .02; Cohen’s d = −.36, 95% CI = [.02,.34]), but failed to reach statistical significance for participants low in friend knowledge/support at −1 SD below the mean (t = 1.87, p = .06; Cohen’s d = .30, 95% CI = [−.01,.31]).
Figure 2.
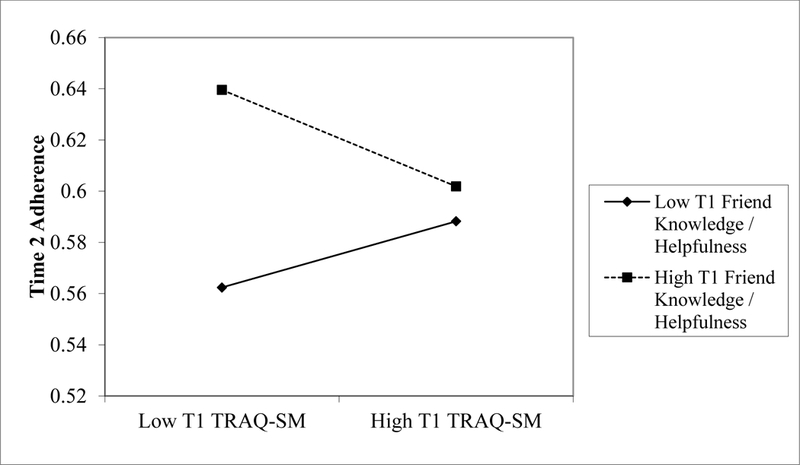
Plot of interaction between Time 1 Self-Management by Time 1 Friend Knowledge/Helpfulness on Time 2 Adherence Controlling for Time 1 Adherence.
Transfer to Adult Care with Transition Readiness Skills and Diabetes Outcomes
A separate set of regressions examined whether transition readiness skills were associated with different outcomes based on whether participants transferred to adult care. Again, transition readiness skills at Time 1 were not associated with changes in HbA1c or adherence. Additionally, no main effect emerged for transferring from pediatric to adult care on HbA1c or adherence. No significant interactions emerged between transition readiness skills and transfer status.
Discussion
As participants entered emerging adulthood they became more proficient in transition readiness skills, but these changes were localized to Self-Management skills. These longitudinal findings build on cross-sectional findings of Sawicki and colleagues (Sawicki et al., 2011), which indicated that older age was associated with higher Self-Management skills but not with Self-Advocacy skills in a sample of participants with chronic illness aged 16 to 26. Although participants in the present sample became more capable of independent diabetes care and managing their diabetes in relation to the healthcare system, even by Time 2, participants were not engaging in transition readiness behaviors entirely independently. Instead, participants moved toward the “starting to do this” level of proficiency. This suggests that the development of transition readiness skills is an ongoing process that continues through early emerging adulthood.
Diabetes-specific relationship processes appeared to be important for the development of transition readiness skills in young emerging adults. Similar to research on the benefits of parental involvement (King et al., 2014) and patient-centered communication or care (Croom et al., 2011; Monaghan et al., 2013) for diabetes management, relationship processes were associated with greater transition readiness skills at Time 1. These results suggest that greater perceived involvement by parents and better perceived communication with diabetes care providers may be helpful as adolescents develop transition readiness skills. As relationship dynamics are changing in early emerging adulthood (Hanna et al., 2014; King et al., 2014), we also found that the way in which these relationship processes were associated with the development of transition readiness skills differed depending on whether they were assessed in late adolescence versus one year later. Our results suggest that higher levels of patient-centered communication and friend knowledge/helpfulness were particularly important for increased Self-Management transition readiness skills after the senior year of high school.
Although main effects of transition readiness skills on diabetes outcomes were not evident, associations were moderated by relationship processes. For example, when there was a mismatch between Self-Advocacy skills and perceived patient-centered communication adherence seemed to suffer. Self-Advocacy skills were associated with better adherence among those with higher patient-centered communication, but lower adherence among those with low patient centered communication. When patient-provider relationships embodied a communication style that fit with patients’ ability to independently advocate for themselves adherence was best. When individuals felt that they were able to advocate for themselves but did not perceive their provider as receptive or focused on high patient-centered communication, adherence suffered.
Changes in adherence were also affected by the fit between Self-Management skills and friend relationship processes, but potentially in more of a compensatory fashion. Adherence was highest when low Self-Management skills occurred in the context of high friend knowledge and helpfulness. These results suggest that friends may actually help bridge the gap for individuals who may be lagging behind in their transition readiness skills. However, this benefit may not extend to individuals who are already high in Self-Management skills as measured via transition readiness skills. Although the slope for low friend knowledge/helpfulness failed to reach statistical significance and any interpretation should be taken with caution, individuals with high Self-Management skills but low friend knowledge/helpfulness also approach a similar level of adherence as individuals with high friend knowledge/helpfulness. It may be that individuals with high Self-Management transition readiness skills are actually functioning more independently and may regress more toward a ‘fair enough’ level of adherence instead of benefitting further from their friend relationships.
Taken together, these results indicate that transition readiness skills alone may not predict diabetes management outcomes at this time in early emerging adulthood. There are several possibilities as to why. First, our participants were only one year out of high school and becoming independent in diabetes care is a gradual process (Peters & Laffel, 2011). This is supported by the fact that our sample of emerging adults were only starting to engage in the transition skills involved with Self-Management by Time 2. Second, the first year after high school may be a particularly challenging time with many other developmentally normative factors to consider (e.g., moving out of the home, entering the workforce, beginning college) that are likely associated with diabetes outcomes (Hanna, Weaver, Stump, Guthrie, & Oruche, 2014). Moreover, an important consideration for future research is that general life skills accompany these changes in living or employment situations (e.g., learning how to cook healthily, time management skills to allow for blood glucose testing, responsible use of alcohol). These additional skills undoubtedly influence diabetes management and our measure of transition readiness did not include such life skills, nor do these measures generally include such skills (Schwartz et al., 2014). Transition readiness measures may be missing an important consideration for explaining health outcomes for emerging adults with diabetes or any chronic illness that infiltrates many aspects of daily living. It is important to note that the typical age of transfer to adult care is at age 18 and often occurs regardless of patients’ readiness to assume the responsibilities of care in an adult-like manner. Our results suggest that there are no differences in terms of transition readiness skills between individuals who remained in pediatric care compared to those who moved to adult care. A more individualized plan for transfer to adult care may help to ensure more success for individuals moving out of the pediatric care system.
Though the results of this study show how transition readiness skills change and how changing relationships are associated with the development of these skills, there are limitations to consider. First, a shortened version of the TRAQ was used to reduce participant burden. Although factor analysis and reliability indicated this shortened version was similar to the original measure, our lack of findings for Self-Advocacy skills may be due in part to the limited number of items included from that subscale. Thus, replication of these results with the full TRAQ is warranted. Second, although the TRAQ is regarded as a particularly strong measure of transition readiness (Schwartz et al., 2014), it was created for use with many chronic health conditions. Supplementing the TRAQ with diabetes-specific measures in future research may be beneficial, as there may be unique ways that individuals with diabetes are expected to manage their illness and interact with the healthcare system (e.g. more or less frequent visits to clinics to assess glycemic control compared to other chronic illnesses like asthma or cystic fibrosis). Third, all of the measures (with the exception of HbA1c) were based on self-report. The results would be strengthened by supplementing these measures with observational measures, particularly of adherence and transition readiness skills. Finally, the results may not generalize to other samples (e.g. those with poorer glycemic control), as there was some bias in the sample that remained in the study. Those who completed measures at Time 2 had better glycemic control than those who did not. Moreover, some measures had limited variability, with few participants reporting low levels of patient-centered communication and friend knowledge/helpfulness.
Implications for Practice
These results provide insight as to how and which social relationships may aid in fostering, or undermining, independence in diabetes management at a time of transition. Moreover, these results also support current concerns that emerging adults are still developing skills for independent diabetes care in early emerging adulthood when they are expected to move from pediatric to adult care (Peters & Laffel, 2011). A focus on improving independence in broad illness management skills without accounting for relationship processes may not result in positive outcomes for all individuals. Further, types of involvement from other people that do not reflect participants’ views of their own abilities may lead to worse adherence. Yet, there are likely other normative developmental factors, such as more general life skills, to consider for optimal diabetes outcomes in emerging adulthood, in addition to specific transition readiness skills. In order to optimize illness outcomes in this high risk group (Weissberg-Benchell, Wolpert, & Anderson, 2007), future research examining issues surrounding the transfer to adult care may benefit from a broadened focus beyond how transition skills may improve adherence to include perceptions of other people’s involvement and also developmental issues in emerging adulthood related to self-care success.
References
- Arnett JJ (2000). Emerging adulthood. A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469–480. 10.1037/0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- Berg CA, Butler JM, Osborn P, King G, Palmer DL, Butner J, … Wiebe DJ (2008). Role of parental monitoring in metabolic control of type 1 diabetes. Diabetes Care, 31(4), 678–683. 10.2337/dc07-1678 [DOI] [PubMed] [Google Scholar]
- Clements MA, Lind M, Raman S, Patton SR, Lipska KJ, Fridlington AG, … Kosiborod M (2014). Age at diagnosis predicts deterioration in glycaemic control among children and adolescents with type 1 diabetes. BMJ Open Diabetes Research & Care, 2(1), e000039 10.1136/bmjdrc-2014-000039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croom A, Wiebe DJ, Berg CA, Lindsay R, Donaldson D, Foster C, … Swinyard MT (2011). Adolescent and parent perceptions of patient-centered communication while managing type 1 diabetes. Journal of Pediatric Psychology, 36(2), 206–215. 10.1093/jpepsy/jsq072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson J (n.d.) Interpreting interaction effects: Two-way interactions. Retrieved from: http://www.jeremydawson.co.uk/slopes.htm
- Garvey KC, Wolpert HA, Rhodes ET, Laffel LM, Kleinman K, Beste MG, … Finkelstein JA (2012). Health care transition in patients with type 1 diabetes: Young adult experiences and relationship to glycemic control. Diabetes Care, 35(8), 1716–1722. 10.2337/dc11-2434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna KM, Weaver MT, Stump TE, Guthrie D, & Oruche UM (2014). Emerging adults with type 1 diabetes during the first year post-high school: Perceptions of parental behaviors. Emerging Adulthood, 2(2), 128–137. 10.1177/2167696813512621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna KM, Weaver MT, Stump TE, Slaven JE, Fortenberry JD, & DiMeglio LA (2013). Readiness for living independently among emerging adults with type 1 diabetes. The Diabetes Educator, 39(1), 92–9. 10.1177/0145721712465341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iannotti RJ, Nansel TR, Schneider S, Haynie DL, Simons-Morton B, Sobel DO, … Clark L (2006). Assessing regimen adherence of adolescents with type 1 diabetes. Diabetes Care, 29(10), 2263–2267. 10.2337/dc06-0685 [DOI] [PubMed] [Google Scholar]
- Corp IBM. (2013). IBM SPSS Statistics for Windows. Armonk, NY: IBM Corp. [Google Scholar]
- King PS, Berg CA, Butner J, Butler JM, & Wiebe DJ (2014). Longitudinal trajectories of parental involvement in type 1 diabetes and adolescents’ adherence. Health Psychology, 33(5), 424–432. 10.1037/a0032804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller KM, Foster NC, Beck RW, Bergenstal RM, DuBose SN, DiMeglio LA, … Tamborlane WV (2015). Current state of type 1 diabetes treatment in the U.S.: Updated data from the T1D Exchange Clinic Registry. Diabetes Care, 38(6), 971–978. 10.2337/dc15-0078 [DOI] [PubMed] [Google Scholar]
- Modi AC, Pai AL, Hommel KA, Hood KK, Cortina S, Hilliard ME, … & Drotar D (2012). Pediatric self-management: a framework for research, practice, and policy. Pediatrics, 129(2), e473–e485. 10.1542/peds.2011-1635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monaghan M, Hilliard M, Sweenie R, & Riekert K (2013). Transition readiness in adolescents and emerging adults with diabetes: The role of patient-provider communication. Current Diabetes Reports, 13(6), 900–908. 10.1016/j.biotechadv.2011.08.021.Secreted [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palladino DK, & Helgeson VS (2012). Friends or foes? A review of peer influence on self-care and glycemic control in adolescents with type 1 diabetes. Journal of Pediatric Psychology, 37(5), 591–603. 10.1093/jpepsy/jss009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer DL, Berg CA, Butler J, Fortenberry K, Murray M, Lindsay R, … Wiebe DJ (2009). Mothers’, fathers’, and children’s perceptions of parental diabetes responsibility in adolescence: Examining the roles of age, pubertal status, and efficacy. Journal of Pediatric Psychology, 34(2), 195–204. 10.1093/jpepsy/jsn073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pendley JS, Kasmen LJ, Miller DL, Donze J, Swenson C, & Reeves G (2002). Peer and family support in children and adolescents with type 1 diabetes. Journal of Pediatric Psychology, 27(5), 429–438. [DOI] [PubMed] [Google Scholar]
- Peters A, & Laffel L (2011). Diabetes care for emerging adults: Recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care, 34(11), 2477–2485. 10.2337/dc11-1723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawicki GS, Lukens-Bull K, Yin X, Demars N, Huang IC, Livingood W, … Wood D (2011). Measuring the transition readiness of youth with special healthcare needs: Validation of the TRAQ - Transition readiness assessment questionnaire. Journal of Pediatric Psychology, 36(2), 160–171. 10.1093/jpepsy/jsp128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz LA, Daniel LC, Brumley LD, Barakat LP, Wesley KM, & Tuchman LK (2014). Measures of readiness to transition to adult health care for youth with chronic physical health conditions: A systematic review and recommendations for measurement testing and development. Journal of Pediatric Psychology, 39(6), 588–601. 10.1093/jpepsy/jsu028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan AM, While AE, & Coyne I (2015). The experiences and impact of transition from child to adult healthcare services for young people with type 1 diabetes: A systematic review. Diabetic Medicine, 32, 440–458. 10.1111/dme.12639 [DOI] [PubMed] [Google Scholar]
- Van Staa A, Van Der Stege HA, Jedeloo S, Moll HA, & Hilberink SR (2011). Readiness to transfer to adult care of adolescents with chronic conditions: Exploration of associated factors. Journal of Adolescent Health, 48(3), 295–302. 10.1016/j.jadohealth.2010.07.009 [DOI] [PubMed] [Google Scholar]
- Weissberg-Benchell J, Wolpert H, & Anderson BJ (2007). Transitioning from pediatric to adult care: A new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care, 30(10), 2441–2446. 10.2337/dc07-1249.Abbreviations [DOI] [PubMed] [Google Scholar]
- Wiebe DJ, Chow CM, Palmer DL, Butner J, Butler JM, Osborn P, & Berg CA (2014). Developmental processes associated with longitudinal declines in parental responsibility and adherence to type 1 diabetesmanagement across adolescence. Journal of Pediatric Psychology, 39(5), 532–541. 10.1093/jpepsy/jsu006 [DOI] [PMC free article] [PubMed] [Google Scholar]


