Abstract
Background
The prevalence of gambling disorder (GD) in women has increased, but, to date, few studies have explored the features of clinical GD subtypes in female samples.
Aims
The aim of this study is to identify empirical clusters based on clinical/sociodemographic variables in a sample of treatment-seeking women with GD.
Methods
Agglomerative hierarchical clustering was applied to a sample of n = 280 patients, using sociodemographic variables, psychopathology, and personality traits as indicators for the grouping procedure.
Results
Three mutually exclusive groups were obtained: (a) Cluster 1 (highly dysfunctional; n = 82, 29.3%) endorsed the highest levels in gambling severity, comorbid psychopathology, novelty seeking, harm avoidance, and self-transcendence, and the lowest scores in self-directedness and cooperativeness; (b) Cluster 2 (dysfunctional; n = 142, 50.7%) achieved medium mean scores in gambling severity and psychopathological symptoms; and (c) Cluster 3 (functional; n = 56, 20.0%) obtained the lowest mean scores in gambling severity and in psychopathology, and a personality profile characterized by low levels in novelty seeking, harm avoidance, and self-transcendence, and the highest levels in self-directedness and cooperativeness.
Discussion and conclusions
This study sheds light on the clinical heterogeneity of women suffering from GD. Identifying the differing features of women with GD is vital to developing prevention programs and personalized treatment protocols for this overlooked population.
Keywords: gambling disorder, personality traits, women, psychopathology, assessment
Introduction
Gambling disorder (GD) is defined by a persistent and recurrent maladaptive pattern of gambling behavior associated with impaired functioning in the personal, social, and occupational areas of patients’ lives (DSM-5; American Psychiatric Association [APA], 2013). In the European Union, lifetime prevalence for problematic gambling is 1.02% and 0.57% for GD (Binde, 2014; Goudriaan, 2014; Valleur, 2015).
Epidemiological and clinical research on GD have mainly been focused on males, since the prevalence of GD is significantly higher in men than women (Blanco, Hasin, Petry, Stinson, & Grant, 2006; Granero et al., 2009), around the ratio of 1:3 in samples of treatment-seeking patients (Crisp et al., 2004; Slutske, Blaszczynski, & Martin, 2009), and it is now suspected that this disorder might have been historically underdiagnosed in females (primarily because only a small percentage of women gamblers who develop subclinical or clinically relevant problem gambling issues seek treatment; Braun, Ludwig, Sleczka, Bühringer, & Kraus, 2014). These circumstances hinder the early identification of GD in women and the identification of GD phenotypes in female samples (Coriale, Ceccanti, De Filippis, Caravasso, & De Persis, 2015).
Some shared features have been found in men and women who met criteria for GD. A recent study with a large sample of n = 454 treatment-seeking problem gamblers did not find gender differences in conceptualizing latent constructs of problem gambling (Smith, Battersby, & Harvey, 2015). In this same line, a study carried out in a sample of respondents to the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; n = 43,093) was focused on Kendler’s model, a framework that considers the etiology of major depression as multifactorial and suggests an interrelation of the risk factors in the different stages of development (García-Rodríguez et al., 2014). Previous research in the same sample (NESARC; n = 43,093) had also concluded the validity of a higher-order externalizing factor comprising a three-factor model of common mental disorders (GD, alcohol and drug dependence, and antisocial personality traits) with good fit for men and women (Oleski, Cox, Clara, & Hills, 2011). However, this result should be interpreted with caution, since the best fit was also observed in women with GD when anxiety was loaded as an externalizing factor.
Regarding comorbidity, concurrent psychiatric conditions are fairly common in men and women who meet criteria for GD (Dowling et al., 2015; Ibáñez, Blanco, Moreryra, & Saiz-Ruiz, 2003; Lorains, Cowlishaw, & Thomas, 2011), with mood and anxiety disorders (Quigley et al., 2014), suicidal behaviors (Bischof et al., 2016), dysfunctional personality traits (del Pino-Gutiérrez et al., 2017), substance-use disorders (Cowlishaw, Merkouris, Chapman, & Radermacher, 2014; Di Nicola et al., 2015; Rash, Weinstock, & Petry, 2011), and behavioral addictions being the most prevalent (Granero et al., 2016; Jiménez-Murcia et al., 2013, 2015; Tackett et al., 2017).
A number of consistent differences between men and women in the pathogenesis of GD have been found (Fattore, Melis, Fadda, & Fratta, 2014; Grant & Kim, 2002; Jiménez-Murcia, Fernández-Aranda, Granero, & Menchón, 2014; Smith et al., 2015). First, demographic variables associated with female GD patients include older age since GD is diagnosed later in women, but the evolution of the disorder is also faster for females due to the “telescoping” phenomena (Grant, Odlaug, & Mooney, 2012; Shin et al., 2014; Slutske, Piasecki, Deutsch, Statham, & Martin, 2015). Second, regarding gambling activity preferences and motivations, males are more likely to prefer strategic games (such as cards or sports betting), whereas most female gamblers tend to prefer non-strategic games (such as bingo or slot machines) and gambling for reasons other than social reasons (women often use gambling behavior as a maladaptive coping mechanism to escape from negative mood states) (Grant, Chamberlain, Schreiber, & Odlaug, 2012; Hing, Russell, Tolchard, & Nower, 2016; Moragas et al., 2015). Third, considering personality and clinical profiles, female gamblers in clinical samples have endorsed lower mean scores in impulsivity and sensation seeking (Hodgins & Holub, 2015), lower risk of drug and/or alcohol abuse (Pilver, Libby, Hoff, & Potenza, 2013; Ronzitti, Lutri, Smith, Clerici, & Bowden-Jones, 2016; Tackett et al., 2017), lower prevalence of antisocial personality disorder (Echeburúa, González-Ortega, de Corral, & Polo-López, 2011), a higher lifetime prevalence for depressive–anxiety symptoms, and a greater likelihood of having a history of physical abuse and neglect (Dion, Cantinotti, Ross, & Collin-Vézina, 2015; Ronzitti et al., 2016). However, to date, no studies have examined how women are specifically grouped bearing in the aforementioned variables.
Studies examining the main predictors of the GD severity have also found different variables depending on the participants’ sex. While impulsivity, maladjustment in everyday life and age of onset for gambling are predictors for both men and women (Castrén et al., 2013; Granero et al., 2014; Mestre-Bach et al., 2016; Nower, Derevensky, & Gupta, 2004), there is evidence to suggest that additional relevant specific predictors for women include older age and low levels of family support (González-Ortega, Echeburúa, Corral, Polo-López, & Alberich, 2013; Ibáñez et al., 2003; Ladd & Petry, 2002).
Different studies have been carried out in order to conceptualize all these GD clinical characteristics through subtyping. The identification of different clinical subgroups allows, among other aspects, to improve existing therapeutic approaches (Milosevic & Ledgerwood, 2010). Some studies using cluster analysis in GD are based on money and time spent on gambling activities (Heiskanen & Toikka, 2016), the presence of GD-related criminal acts (Granero et al., 2015), favorite gambling activities (Challet-Bouju et al., 2015), or the affective motivations for gambling (Stewart, Zack, Collins, & Klein, 2008). Other researchers have opted to subject gamblers to personality tests and evaluations of their gambling practice in order to shed light on the commonly utilized pathway models of gambling behavior (Blaszczynski & Nower, 2002; Valleur et al., 2016). However, the dearth of studies examining these features exclusively in women is a shortcoming in GD research that must be addressed.
As such, the aim of this work was to identify distinct GD phenotypes in a large sample of women receiving outpatient treatment for GD through clustering analysis, using a wide set of variables including sociodemographic, psychopathological, and personality measures as indicators for grouping.
Methods
Participants and procedure
This study sample included women (n = 280) recruited from the Department of Psychiatry, at a University Hospital, between January 2005 and September 2015. All the women in our sample voluntarily sought treatment for GD and met DSM-IV-TR diagnostic criteria for GD (APA, 2000). All patient diagnoses were reassessed and recodified post hoc and only patients who met DSM-5 criteria for GD (APA, 2013) were included in our analysis. Additional exclusion criteria were having an intellectual disability or a severe mental disorder (schizophrenia or other psychotic disorders, bipolar disorder, etc.). Experienced psychologists and psychiatrists, with more than 20 years of clinical experience in the field of addictive disorders, conducted the two face-to-face clinical interviews. All the measures analyzed in this study correspond to the assessment conducted prior to the beginning of the treatment.
Measures
South Oaks Gambling Screen (SOGS; Lesieur & Blume, 1987)
This self-report, 20-item questionnaire discriminates between probable pathological, problem, and non-problem gamblers. The Spanish validation used in this work showed excellent internal consistency (α = .94) and test–retest reliability (r = .98) (Echeburúa, Báez, Fernández, & Páez, 1994). Consistency in the sample of this work was very good (α = .82).
Diagnostic questionnaire for Pathological Gambling according to DSM criteria (Stinchfield, 2003)
This 19-item questionnaire allows for the assessment of DSM-5 (APA, 2013) diagnostic criteria for GD. Convergent validity with SOGS scores in the original version was very good (r = .77 for representative samples and r = .75 for gambling treatment groups; Stinchfield, 2003). Internal consistency in the Spanish adaptation used in this study was α = .81 for the general population and α = .77 for gambling treatment samples (Jiménez-Murcia et al., 2009). In this study, the total number of DSM-5 criteria for GD was analyzed. Cronbach’s α in the sample was very good (α = .80).
Temperament and Character Inventory – Revised (TCI-R; Cloninger, 1999)
This reliable and valid 240-item questionnaire measures seven personality dimensions: four temperaments (novelty seeking, harm avoidance, reward dependence, and persistence) and three character dimensions (self-directedness, cooperativeness, and self-transcendence). All items are measured on a 5-point Likert-type scale. A validated Spanish version was used (Gutiérrez-Zotes et al., 2004). The scales in the Spanish revised version showed adequate internal consistency (Cronbach’s α mean value = .87). In the study, consistency indices ranged from good (α = .70 for novelty seeking) to very good (α = .84 for persistence and self-transcendence). Table 1 contains the α values for all the scales.
Table 1.
Comparison between clusters in sociodemographic and clinical measures
| Total (n = 280) | C1 (n = 82) | C2 (n = 142) | C3 (n = 56) | Cluster | Pairwise comparisons (p) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Categorical indicators | N | % | N | % | n | % | n | % | p | C1–C2 | C1–C3 | C2–C3 | ||
| *Education | Primary | 168 | 60.0 | 51 | 62.2 | 93 | 65.5 | 24 | 42.9 | .061 | .787 | .078 | .014 | |
| Secondary | 91 | 32.5 | 26 | 31.7 | 39 | 27.5 | 26 | 46.4 | ||||||
| University | 21 | 7.5 | 5 | 6.1 | 10 | 7.0 | 6 | 10.7 | ||||||
| *Civil status | Single | 109 | 38.9 | 26 | 31.7 | 71 | 50.0 | 12 | 21.4 | <.001 | .013 | .016 | <.001 | |
| Married | 113 | 40.4 | 31 | 37.8 | 47 | 33.1 | 35 | 62.5 | ||||||
| Divorced/widow | 58 | 20.7 | 25 | 30.5 | 24 | 16.9 | 9 | 16.1 | ||||||
| *Employed | Yes | 135 | 48.2 | 39 | 47.6 | 62 | 43.7 | 34 | 60.7 | .096 | .572 | .128 | .031 | |
| Origin | Spanish | 254 | 90.7 | 73 | 89.0 | 134 | 94.4 | 47 | 83.9 | .061 | .146 | .383 | .018 | |
| Tobacco use | Yes | 152 | 54.3 | 48 | 58.5 | 81 | 57.0 | 23 | 41.1 | .083 | .827 | .044 | .043 | |
| Quantitative indicators | Mean | SD | Mean | SD | Mean | SD | Mean | SD | p | C1–C2 | C1–C3 | C2–C3 | ||
| *Age (years) | 49.64 | 12.37 | 48.24 | 10.00 | 50.51 | 13.37 | 49.48 | 12.90 | .416 | .187 | .564 | .598 | ||
| *GD onset (years) | 44.72 | 12.44 | 42.61 | 10.16 | 45.67 | 13.68 | 45.37 | 11.99 | .189 | .077 | .201 | .879 | ||
| *Duration (years) | 12.60 | 9.59 | 12.86 | 9.50 | 12.37 | 9.30 | 12.81 | 10.58 | .919 | .712 | .974 | .773 | ||
| Mean bets-episode | 76.10 | 111.5 | 76.90 | 110.6 | 70.90 | 113.8 | 88.10 | 107.8 | .620 | .698 | .564 | .330 | ||
| Cumulated debts | 8,647.7 | 18,989.5 | 7,555.7 | 14,280.8 | 7,881.3 | 16,474.8 | 12,189.9 | 28,583.2 | .295 | .902 | .160 | .151 | ||
| *SOGS-total | α = .82 | 11.53 | 3.16 | 12.87 | 3.08 | 11.28 | 2.85 | 10.21 | 3.33 | <.001 | <.001 | <.001 | .026 | |
| DSM-5 total | α = .80 | 7.02 | 1.80 | 7.78 | 1.50 | 7.01 | 1.66 | 5.93 | 2.03 | <.001 | .001 | <.001 | <.001 | |
| *SCL-90-R: somatization | α = .91 | 1.61 | 0.89 | 2.57 | 0.74 | 1.45 | 0.48 | 0.62 | 0.48 | <.001 | <.001 | <.001 | <.001 | |
| *SCL-90-R: obsessive–compulsive | α = .88 | 1.52 | 0.83 | 2.35 | 0.72 | 1.43 | 0.48 | 0.54 | 0.41 | <.001 | <.001 | <.001 | <.001 | |
| *SCL-90-R: interpersonal sensitivity | α = .87 | 1.40 | 0.87 | 2.39 | 0.68 | 1.23 | 0.45 | 0.40 | 0.31 | <.001 | <.001 | <.001 | <.001 | |
| *SCL-90-R: depressive | α = .91 | 2.16 | 0.92 | 3.13 | 0.55 | 2.10 | 0.46 | 0.89 | 0.53 | <.001 | <.001 | <.001 | <.001 | |
| *SCL-90-R: anxiety | α = .90 | 1.52 | 0.91 | 2.58 | 0.73 | 1.33 | 0.40 | 0.46 | 0.33 | <.001 | <.001 | <.001 | <.001 | |
| *SCL-90-R: hostility | α = .83 | 1.04 | 0.85 | 1.97 | 0.85 | 0.79 | 0.41 | 0.28 | 0.39 | <.001 | <.001 | <.001 | <.001 | |
| *SCL-90-R: phobic anxiety | α = .86 | 0.84 | 0.90 | 1.75 | 1.01 | 0.59 | 0.49 | 0.13 | 0.24 | <.001 | <.001 | <.001 | <.001 | |
| *SCL-90-R: paranoia | α = .74 | 1.22 | 0.80 | 2.05 | 0.82 | 1.05 | 0.41 | 0.44 | 0.34 | <.001 | <.001 | <.001 | <.001 | |
| *SCL-90-R: psychotic | α = .86 | 1.15 | 0.78 | 2.08 | 0.61 | 0.96 | 0.37 | 0.27 | 0.25 | <.001 | <.001 | <.001 | <.001 | |
| *SCL-90-R: GSI index | α = .98 | 1.49 | 0.75 | 2.44 | 0.45 | 1.32 | 0.20 | 0.51 | 0.27 | <.001 | <.001 | <.001 | <.001 | |
| *SCL-90-R: PST index | α = .98 | 53.39 | 20.98 | 75.24 | 9.17 | 50.12 | 15.34 | 29.66 | 13.89 | <.001 | <.001 | <.001 | <.001 | |
| *SCL-90-R: PSDI index | α = .98 | 2.28 | 0.62 | 2.93 | 0.47 | 2.21 | 0.32 | 1.53 | 0.40 | <.001 | <.001 | <.001 | <.001 | |
| *TCI-R: novelty seeking | α = .70 | 110.33 | 12.70 | 112.38 | 13.83 | 110.24 | 11.29 | 107.55 | 13.99 | .090 | .223 | .028 | .179 | |
| *TCI-R: harm avoidance | α = .81 | 108.73 | 15.95 | 116.65 | 15.45 | 108.49 | 13.14 | 97.73 | 16.76 | <.001 | <.001 | <.001 | <.001 | |
| *TCI-R: reward dependence | α = .72 | 102.87 | 12.69 | 102.59 | 14.54 | 103.12 | 10.75 | 102.64 | 14.47 | .945 | .763 | .979 | .813 | |
| *TCI-R: persistence | α = .84 | 104.61 | 17.17 | 107.06 | 19.27 | 103.18 | 15.06 | 104.64 | 18.78 | .265 | .104 | .417 | .588 | |
| *TCI-R: self-directedness | α = .82 | 118.79 | 18.25 | 107.22 | 16.73 | 118.39 | 13.59 | 136.77 | 16.60 | <.001 | <.001 | <.001 | <.001 | |
| *TCI-R: cooperativeness | α = .78 | 134.63 | 13.96 | 132.06 | 16.99 | 134.65 | 11.32 | 138.36 | 14.51 | .033 | .179 | .009 | .090 | |
| *TCI-R: self-transcendence | α = .84 | 70.28 | 14.52 | 74.76 | 16.56 | 68.79 | 11.85 | 67.52 | 16.21 | .003 | .003 | .004 | .573 | |
Note. Bold values represent significant comparison (.05 level). SD: standard deviation; α: Cronbach’s α in the study sample; SCL-90-R: Symptom Checklist – Revised; SCL-90-R: GSI: global severity index; SCL-90-R: PST: positive symptom total; SCL-90-R: PSDI: Positive Symptom Distress Index; TCI-R: Temperament and Character Inventory – Revised; DSM-5: Diagnostic and Statistical Manual of Mental Disorders; SOGS: South Oaks Gambling Screen; GD: gambling disorder.
Variable used as indicator in the clustering process.
Symptom Checklist – Revised (SCL-90-R; Derogatis, 1990)
This checklist evaluates a broad range of psychological and psychopathological symptoms. This questionnaire contains 90 items and measures 9 primary symptom dimensions: somatization, obsession–compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. It also includes three global indices: (a) a global severity index (GSI), designed to measure overall psychological distress; (b) a Positive Symptom Distress Index, to measure symptom intensity; and (c) a positive symptom total, which reflects self-reported symptoms. A validated Spanish version was used (Derogatis, 2002). The Spanish validation scale obtained good psychometrical indices, with a mean internal consistency of .75 (Cronbach’s α). In the study sample, consistency indices were in the very good (α = .83 for hostility) to excellent range (α = .98 for the global indexes), with the only exception of paranoia (α = .74, good). Table 1 contains the α values for all the scales.
Other sociodemographic and clinical variables
Additional demographic, clinical, and social/family variables related to gambling were measured using a semi-structured face-to-face clinical interview described elsewhere (Jiménez-Murcia, Aymamí-Sanromà, Gómez-Peña, Álvarez-Moya, & Vallejo, 2006). Some of the GD behavior variables that are covered included the age of GD onset, the mean and maximum amount of money spent in a single gambling episode, and the total amount of gambling-related debts.
Statistical analysis
Statistical analysis was carried out using the software SPSS24 for Windows. Empirical clusters were explored through TwoStep Clustering Component analyses, entering the patients’ years of education, civil status, employment status, age, age of GD onset, GD duration, GD severity (SOGS-total), psychopathology (SCL-90-R scales), and personality traits (TCI-R scales) as indicators. The TwoStep Clustering system constitutes a scalable algorithm designed to handle large data sets including both continuous and categorical variables. In the first step, subjects are preclustered into many small subclusters according to a sequential clustering approach. During the second step, the resulting subclusters are considered as inputs and grouped into the specified number of clusters according to the agglomerative hierarchical clustering method. The TwoStep algorithm uses a combination of the Schwarz Bayesian Information Criterion (Schwarz, 1978) and log-likelihood distance by default in autodetermining the final number of clusters, choosing as the optimal solution with a reasonably large ratio of Schwarz Bayesian Information Criterion changes and a large ratio of distance measures (optionally, users can specify the maximum number of clusters that the procedure should consider). The log-likelihood measure is computed using normal density for continuous variables and multinomial probability mass function for categorical variables. In this study, we compared the automatic number of clusters selected by the TwoStep Clustering procedure as finalistic candidate solutions, and two additional models: the autodetermined number of clusters minus one, and the autodetermined plus one. The final selected model was based on (Nylund, Asparouhov, & Muthén, 2007): (a) the highest cohesion and separation index, (b) adequate number of individuals in each group (to allow for statistical comparisons), and (c) the best clinical interpretability. In addition, Silhouette’s index was used as a validity measure of consistency within clusters, which can be interpreted as the level of cohesion/separation for the empirical derived groups (Rousseeuw, 1987).
The comparison between the derived empirical clusters for the variables of the study (sociodemographic, clinical, and personality measures) was carried out using χ2 tests for categorical factors and analysis of variance for quantitative measures. Bonferroni–Finner’s correction controlled the inflation in type-I error due to multiple comparisons.
Ethics
The study procedures were carried out in accordance with the Declaration of Helsinki. The University Hospital of Bellvitge Ethics Committee of Clinical Research approved the study. All subjects were informed about the study and all provided informed consent.
Results
Cluster composition: Description of the cluster indicators
The three-cluster solution was selected as being most optimal in the study sample. This structure was autodetermined as the most appropriate by the TwoStep Clustering procedure. Silhouette’s index was equal to 0.3 (value into the fair range), suggesting reasonable evidence of validity within the clusters of data. The comparison between the largest cluster size (n = 142, 50.7%) and the smallest (n = 56, 20.0%) yielded a ratio of 2.54.
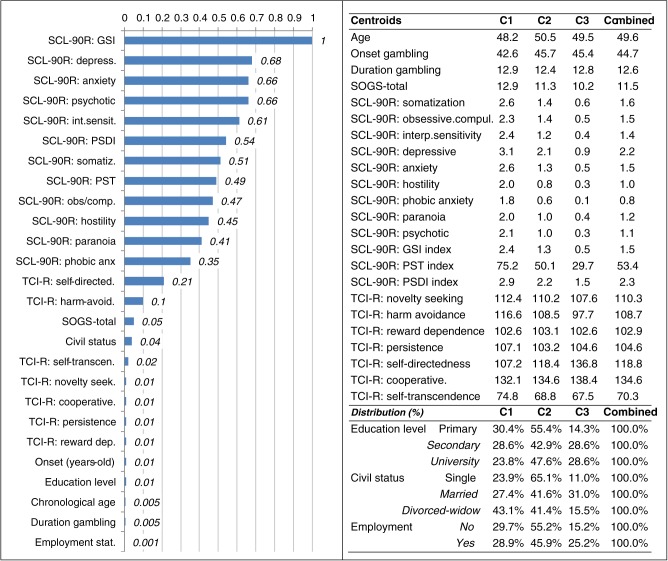
Figure 1 summarizes the final three-cluster model. The first figure contains a bar graph with the relative importance of each indicator in the clustering, which reports how well each variable can differentiate the different derived clusters (the higher the importance measure, the less likely it is that the variation for the variable between clusters is due to chance and the more likely it is due to an underlying difference). In this study, the SCL-90-R GSI scale achieved the highest relative importance for clustering, followed by the SCL-90-R depression, anxiety, psychotic, and interpersonal sensitivity scales. Age, duration of the gambling problem, and employment status obtained the poorest relevance for clustering. The table included in Figure 1 contains the centroids for the indicators in the clustering (means for the quantitative variables and the percentage distribution for categorical variables), which summarizes the cluster patterns for this set of variables.
Figure 1.
Clustering summary: relative importance of each indicator and centroids. SCL-90-R: GSI: global severity index; SCL-90-R: PST: positive symptom total; SCL-90-R: PSDI: Positive Symptom Distress Index
Comparison between the clusters in sociodemographic and clinical variables
Table 1 contains the distribution of the variables analyzed in this study and the statistical comparison between clusters. Figure 2 summarizes (through a radar-chart) the phenotypes of the three clusters in the main variables that obtained significant differences between the derived empirical groups (since these variables have different ranges, z-standardized scores in the sample were plotted for quantitative measures and proportions for categorical measures to simplify the interpretation of the figure). Table 2 compares the three clusters according to the patients’ main gambling activity during seeking treatment. According to these sets of results, the clusters were named as follows: Cluster 1 “highly dysfunctional,” Cluster 2 “dysfunctional,” and Cluster 3 “functional.”
Figure 2.
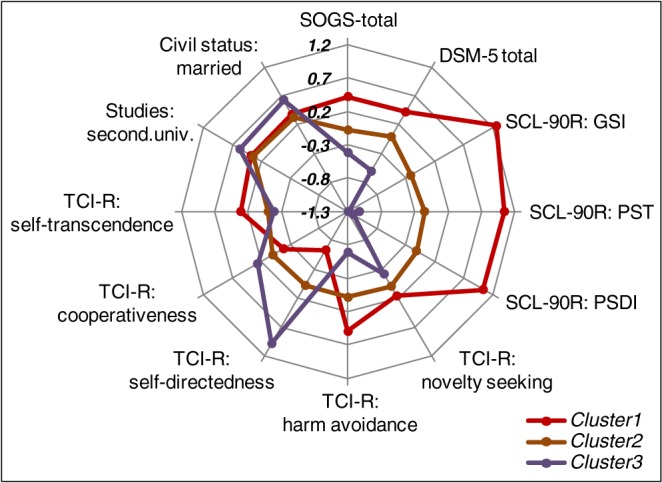
Radar chart displaying the main differences between clusters. SCL-90-R: GSI: global severity index; SCL-90-R: PST: positive symptom total; SCL-90-R: PSDI: Positive Symptom Distress Index
Table 2.
Comparison between clusters based on gambling activity preferences
| Main gambling activity | Total (n = 280) | C1 (n = 82) | C2 (n = 142) | C3 (n = 56) | Cluster | Pairwise comparison (p) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | n | % | n | % | n | % | (p) | C1–C2 | C1–C3 | C2–C3 | |
| Slots | 167 | 59.6 | 44 | 53.7 | 93 | 65.5 | 30 | 53.6 | .129 | .080 | .992 | .119 |
| Bingo | 105 | 37.5 | 38 | 46.3 | 49 | 34.5 | 18 | 32.1 | .138 | .080 | .095 | .752 |
| Lotteries | 33 | 11.8 | 11 | 13.4 | 16 | 11.3 | 6 | 10.7 | .857 | .634 | .636 | .911 |
| Casinos | 14 | 5.0 | 6 | 7.3 | 2 | 1.4 | 6 | 10.7 | .013 | .022 | .487 | .003 |
| Cards | 9 | 3.2 | 4 | 4.9 | 2 | 1.4 | 3 | 5.4 | .218 | .121 | .900 | .111 |
| Sports betting | 3 | 1.1 | 3 | 3.7 | 0 | 0.0 | 0 | 0.0 | .026 | .022 | .148 | – |
| Online gambling | 9 | 3.2 | 6 | 7.3 | 0 | 0.0 | 3 | 5.4 | .007 | .001 | .647 | .005 |
| Other | 7 | 2.5 | 3 | 3.7 | 3 | 2.1 | 1 | 1.8 | .720 | .490 | .520 | .883 |
Note. Bold values represent significant comparison (.05 level), which are not estimable due to a lack of cases.
Cluster 1 (highly dysfunctional; n = 82, 29.3%) was consists of women with the least number of years of education and the highest mean scores in gambling severity (SOGS) and in psychopathology (SCL-90-R). The personality traits of women in the highly dysfunctional group were characterized by high levels of novelty seeking, harm avoidance, and self-transcendence and low levels of self-directedness and cooperativeness.
Cluster 2 (dysfunctional; n = 142, 50.7%) was characterized by mostly single women, who reported medium mean scores in gambling severity and in psychopathology. Regarding gambling preferences, this cluster obtained the lowest prevalence of casinos games and online gambling.
Cluster 3 (functional; n = 56, 20.0%) consists of women with a higher level of education and they were more likely to be married and employed. This group obtained the lowest scores in gambling severity and in psychopathology. Their personality profile was characterized by the lowest levels in novelty seeking, harm avoidance, and self-transcendence, and the highest levels in self-directedness and cooperativeness.
Discussion
This study set out to analyze clinical subtypes in a sample of women seeking treatment for GD. Defining sociodemographic and clinical variables as indicators, three empirical clusters emerged: highly dysfunctional, dysfunctional, and functional.
The first cluster (highly dysfunctional) was characterized by high levels in gambling severity and psychopathology. Petry, Stinson, and Grant (2005) researched the comorbidity of GD with other psychiatric conditions, and their results showed high comorbidity between GD with substance use, mood, anxiety, and personality disorders. Relatedly, other studies have demonstrated that GD commonly presents comorbidity with other disorders (Lorains et al., 2011). In the case of women with GD, the most frequently identified associated disorders have been anxiety and affective disorders (Desai & Potenza, 2008). This tendency also seems to be present in women with subclinical pathological gambling habits, as other research has found that women are more likely to report being motivated to gamble in order to escape problems or improve their mood compared to men (Blanco et al., 2006). This suggests that that emotional distress may serve as a maintaining factor for a dysfunctional gambling behavior (Ciccarelli, Griffiths, Nigro, & Cosenza, 2017). In this sense, women might use gambling as a maladaptive mechanism of emotion regulation (Iancu, Lowengrub, Dembinsky, Kotler, & Dannon, 2008).
We must highlight that personality variables are important in separating GD subtypes. In this study, the highly dysfunctional cluster was characterized by high novelty-seeking levels. This personality trait is associated with exploratory activity in response to novel stimuli, sensitivity to reward cues, making decisions impulsively, and fleeing from frustration (Cloninger, Svrakic, & Przybeck, 1993). In addition, this personality trait is related to a preference for activities involving chance, turning the gambling into a constant source of novelty (Spinella, 2003). This result, therefore, supports previous research in this field showing that women with GD with higher levels of novelty seeking respond worse to treatment interventions (Mestre-Bach et al., 2016) and are more likely to commit gambling-related illegal acts (Mestre-Bach et al., 2018).
Harm avoidance is also a relevant personality trait found in the highly dysfunctional cluster. This dimension is characterized by a tendency to passively avoid punishment (Hu et al., 2016). Several studies have identified harm avoidance as a motivational factor during gambling episodes (Tavares, Zilberman, Hodgins, & El-Guebaly, 2005; Yau, Crowley, Mayes, & Potenza, 2012). Our research suggests that as impairment in female gamblers worsens, levels in harm avoidance increase.
Our findings indicate that high levels of self-transcendence contribute to gambling severity. Martinotti et al. (2006) found that self-transcendence was positively associated with GD severity and that this tendency increases with age. This personality trait is associated with having superstitious beliefs and some studies conclude that irrational attitudes related to this trait would play an instrumental role in the maintenance of the GD (Joukhador, Blaszczynski, & Maccallum, 2004). However, it should be considered that the self-transcendence scores obtained in this study are within the average range for the general population (Gutiérrez-Zotes et al., 2004).
Finally, the low levels in self-directedness observed in the highly dysfunctional cluster are also coherent with other studies relating this personality trait and GD severity. It has been argued that the feeling of not having control over one’s own life, not possessing coping skills to solve daily problems, and a lack of self-acceptance of one’s personality contribute to gambling severity (Montag, Jurkiewicz, & Reuter, 2010). Therefore, it is plausible that women who have lost stability or meaning in their lives and are unable to tackle everyday problems may use gambling as a means of escape.
The cluster characterized by low impairment included patients who also reported the lowest levels in novelty seeking and the highest levels in self-directedness and cooperativeness. This personality profile (compared with the profile found in the other two clusters) could partly explain why this group endorsed lower levels of psychopathology and GD severity. Recent research has supported the relevance of personality traits in impulsivity-related disorders (including substance use and behavioral addictions), with novelty seeking obtaining the most significance in distinguishing subjects with comorbid conditions (del Pino-Gutiérrez et al., 2017). These results are in concordance with previous studies using samples including males that have shown impulsivity and sensation seeking to be the key features separating GD patient clusters (Álvarez-Moya et al., 2010).
Implications for practice
One of the main issues that emerges from these findings is the need to consider these evident clinical differences between the three clusters of women with a diagnosis of GD. In order to guarantee an optimal and personalized therapeutic approach for GD treatment-seeking women, impairment level should be considered a clinical feature. In the specific case of those women who present greater impairment, high levels of psychopathology and the personality traits mentioned (mainly high novelty seeking and harm avoidance and low self-direction) should be considered. Both can interfere significantly in the treatment process and therefore it would be timely to directly address these clinical aspects. In less severe cases, therefore, it could be more beneficial to directly focus the therapy on features of GD, in order to minimize all types of gambling behavior and to eventually achieve full abstinence. The results from our cluster analysis also somewhat coincide with commonly utilized pathways models of gambling, from which we were able to distinguish between emotionally vulnerable gamblers and more impulsive gamblers (Blaszczynski & Nower, 2002). However, it should be noted that the measures used in this study did not entirely coincide with previous studies (Milosevic & Ledgerwood, 2010; Valleur et al., 2016).
Limitations
There are several limitations to this study. First, it was carried out in a clinical sample of women who sought professional treatment for GD, so the results cannot be generalized to other populations. Future studies would benefit from including non-treatment-seeking gamblers, to obtain a more exhaustive perspective of different existing clinical profiles. Second, including other clinical variables that are associated with GD in the cluster analysis, such as impulsivity or emotional regulation, would allow a more exhaustive description of patient phenotype. Third, this is a cross-sectional study and implications regarding causality cannot be performed. Finally, it must be considered that the sample was recruited between 2005 and 2015, and that there have been significant changes in the availability and accessibility to certain types of gambling activities, especially sports betting and online gambling. Therefore, the profile of female gamblers has changed over the recruitment period of the study to the present.
Acknowledgements
The authors would like to thank CERCA Programme/Generalitat de Catalunya for institutional support and Fondo Europeo de Desarrollo Regional (FEDER) “Una manera de hacer Europa”/“a way to built Europe.”
Funding Statement
Funding sources: Financial support was received through the Ministerio de Economía y Competitividad (grant PSI2011-28349 and PSI2015-68701-R). FIS PI14/00290, FIS PI17/01167, and 18MSP001 – 2017I067 received aid from the Ministerio de Sanidad, Servicios Sociales e Igualdad. CIBER Fisiología Obesidad y Nutrición (CIBERobn) and CIBER Salud Mental (CIBERSAM), both of which are initiatives of ISCIII. GM-B is supported by a predoctoral Grant of AGAUR (2018 FI_B2 00174), co-financed by the European Social Fund, with the support of the Secretaria d’Universitats I Recerca del Departament d’Economia i Coneixement de la Generalitat de Catalunya. TM-M is supported by a predoctoral Grant of the Ministerio de Educación, Cultura y Deporte (FPU16/02087).
Authors’ contribution
BG-C, GM-B, TS, FP, BG-F, RG, SJ-M, and FF-A contributed to the development of the study concept and design. RG, BG-F, and VM-R performed the statistical analysis. GM-B, TS, FF-A, AdP-G, LM, NA, MG-P, TM-M, FF-A, and SJ-M aided with our interpretation of data. FF-A, JM-M, and SJ-M obtained funding and supervised the study.
Conflict of interest
The authors declare no conflict of interest.
References
- Álvarez-Moya E. M., Jiménez-Murcia S., Aymamí M. N., Gómez-Peña M., Granero R., Santamaría J., Menchón J. M., Fernández-Aranda F. (2010). Subtyping study of a pathological gamblers sample. Canadian Journal of Psychiatry, 55(8), 498–506. doi: 10.1177/070674371005500804 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association [APA]. (2000). Diagnostic and statistical manual of mental disorders (DSM-IV-TR) (4th ed., text rev.). Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association [APA]. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Binde P. (2014). Gambling in Sweden: The cultural and socio-political context. Addiction, 109(2), 193–198. doi: 10.1111/add.12103 [DOI] [PubMed] [Google Scholar]
- Bischof A., Meyer C., Bischof G., John U., Wurst F. M., Thon N., Lucht M., Grabem H. J., Rumpf H. J. (2016). Type of gambling as an independent risk factor for suicidal events in pathological gamblers. Psychology of Addictive Behaviors, 30(2), 263–269. doi: 10.1037/adb0000152 [DOI] [PubMed] [Google Scholar]
- Blanco C., Hasin D. S., Petry N., Stinson F. S., Grant B. F. (2006). Sex differences in subclinical and DSM-IV pathological gambling: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine, 36(7), 943–953. doi: 10.1017/S0033291706007410 [DOI] [PubMed] [Google Scholar]
- Blaszczynski A., Nower L. (2002). A pathways model of problem and pathological gambling. Addiction, 97(5), 487–499. doi: 10.1046/j.1360-0443.2002.00015.x [DOI] [PubMed] [Google Scholar]
- Braun B., Ludwig M., Sleczka P., Bühringer G., Kraus L. (2014). Gamblers seeking treatment: Who does and who doesn’t? Journal of Behavioral Addictions, 3(3), 189–198. doi: 10.1556/JBA.3.2014.3.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castrén S., Basnet S., Salonen A. H., Pankakoski M., Ronkainen J. E., Alho H., Lahti T. (2013). Factors associated with disordered gambling in Finland. Substance Abuse: Treatment, Prevention, and Policy, 8(1), 24. doi: 10.1186/1747-597X-8-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Challet-Bouju G., Hardouin J.-B., Renard N., Legauffre C., Valleur M., Magalon D., Fatséas M., Chéreau-Boudet I., Gorsane M. A., Vénisse J.-L., Grall-Bronnec M. (2015). A gamblers clustering based on their favorite gambling activity. Journal of Gambling Studies, 31(4), 1767–1788. doi: 10.1007/s10899-014-9496-8 [DOI] [PubMed] [Google Scholar]
- Ciccarelli M., Griffiths M. D., Nigro G., Cosenza M. (2017). Decision making, cognitive distortions and emotional distress: A comparison between pathological gamblers and healthy controls. Journal of Behavior Therapy and Experimental Psychiatry, 54, 204–210. doi: 10.1016/j.jbtep.2016.08.012 [DOI] [PubMed] [Google Scholar]
- Cloninger C. R. (1999). The Temperament and Character Inventory – Revised. St. Louis, MO: Center for Psychobiology of Personality. [Google Scholar]
- Cloninger C. R., Svrakic D. M., Przybeck T. R. (1993). A psychobiological model of temperament and character. Archives of General Psychiatry, 50(12), 975–990. doi: 10.1001/archpsyc.1993.01820240059008 [DOI] [PubMed] [Google Scholar]
- Coriale G., Ceccanti M., De Filippis S., Caravasso C. F., De Persis S. (2015). Gambling disorder: Epidemiology, diagnosis, interpretative models and intervention. Rivista Di Psichiatria, 50(5), 216–227. doi: 10.1708/2040.22162 [DOI] [PubMed] [Google Scholar]
- Cowlishaw S., Merkouris S., Chapman A., Radermacher H. (2014). Pathological and problem gambling in substance use treatment: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 46(2), 98–105. doi: 10.1016/j.jsat.2013.08.019 [DOI] [PubMed] [Google Scholar]
- Crisp B. R., Thomas S. A., Jackson A. C., Smith S., Borrell J., Ho W. Y., Holt T. A., Thomason N. (2004). Not the same: A comparison of female and male clients seeking treatment from problem gambling counselling services. Journal of Gambling Studies, 20(3), 283–299. doi: 10.1023/B:JOGS.0000040280.64348.d1 [DOI] [PubMed] [Google Scholar]
- del Pino-Gutiérrez A., Jiménez-Murcia S., Fernández-Aranda F., Agüera Z., Granero R., Hakansson A., Fagundo A. B., Bolao F., Valdepérez A., Mestre-Bach G., Steward T., Penelo E., Moragas L., Aymamí N., Gómez-Peña M., Rigol-Cuadras A., Martín-Romera V., Menchón J. M. (2017). The relevance of personality traits in impulsivity-related disorders: From substance use disorders and gambling disorder to bulimia nervosa. Journal of Behavioral Addictions, 6(3), 396–405. doi: 10.1556/2006.6.2017.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L. (1990). SCL-90-R. Administration, scoring and procedures manual. Baltimore, MD: Clinical Psychometric Research. [Google Scholar]
- Derogatis L. (2002). SCL-90-R. Cuestionario de 90 síntomas-Manual [SCL-90-R: 90 Symptoms Questionnaire-Manual ]. Madrid, Spain: TEA Ediciones. [Google Scholar]
- Desai R. A., Potenza M. N. (2008). Gender differences in the associations between past-year gambling problems and psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology, 43(3), 173–183. doi: 10.1007/s00127-007-0283-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Nicola M., Tedeschi D., De Risio L., Pettorruso M., Martinotti G., Ruggeri F., Swierkosz-Lenartd K., Guglielmoa R., Calleae A., Ruggeria G., Pozzia G., Di Giannantonioc M., Janiriab L., Janiri L. (2015). Co-occurrence of alcohol use disorder and behavioral addictions: Relevance of impulsivity and craving. Drug and Alcohol Dependence, 148, 118–125. doi: 10.1016/j.drugalcdep.2014.12.028 [DOI] [PubMed] [Google Scholar]
- Dion J., Cantinotti M., Ross A., Collin-Vézina D. (2015). Sexual abuse, residential schooling and probable pathological gambling among indigenous Peoples. Child Abuse & Neglect, 44, 56–65. doi: 10.1016/j.chiabu.2015.03.004 [DOI] [PubMed] [Google Scholar]
- Dowling N. A., Cowlishaw S., Jackson A. C., Merkouris S. S., Francis K. L., Christensen D. R. (2015). Prevalence of psychiatric co-morbidity in treatment-seeking problem gamblers: A systematic review and meta-analysis. Australian & New Zealand Journal of Psychiatry, 49(6), 519–539. doi: 10.1177/0004867415575774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Echeburúa E., Báez C., Fernández J., Páez D. (1994). Cuestionario de juego patológico de South Oaks (SOGS): Validación española [South Oaks Gambling Screen (SOGS): Spanish validation]. Análisis de Modificación de Conducta, 20, 769–791. [Google Scholar]
- Echeburúa E., González-Ortega I., de Corral P., Polo-López R. (2011). Clinical gender differences among adult pathological gamblers seeking treatment. Journal of Gambling Studies, 27(2), 215–227. doi: 10.1007/s10899-010-9205-1 [DOI] [PubMed] [Google Scholar]
- Fattore L., Melis M., Fadda P., Fratta W. (2014). Sex differences in addictive disorders. Frontiers in Neuroendocrinology, 35(3), 272–284. doi: 10.1016/j.yfrne.2014.04.003 [DOI] [PubMed] [Google Scholar]
- García-Rodríguez O., Blanco C., Wall M. M., Wang S., Jin C. J., Kendler K. S. (2014). Toward a comprehensive developmental model of smoking initiation and nicotine dependence. Drug and Alcohol Dependence, 144, 160–169. doi: 10.1016/j.drugalcdep.2014.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Ortega I., Echeburúa E., Corral P., Polo-López R., Alberich S. (2013). Predictors of pathological gambling severity taking gender differences into account. European Addiction Research, 19(3), 146–154. doi: 10.1159/000342311 [DOI] [PubMed] [Google Scholar]
- Goudriaan A. E. (2014). Gambling and problem gambling in the Netherlands. Addiction, 109(7), 1066–1071. doi: 10.1111/add.12213 [DOI] [PubMed] [Google Scholar]
- Granero R., Fernández-Aranda F., Aymamí N., Gómez-Peña M., Fagundo A. B., Sauchelli S., Del Pino-Gutiérrez A., Moragas L., Savvidou L. G., Islam M. A., Tàrrega S., Menchón J. M., Jiménez-Murcia S. (2015). Subtypes of pathological gambling with concurrent illegal behaviors. Journal of Gambling Studies, 31(4), 1161–1178. doi: 10.1007/s10899-014-9499-5 [DOI] [PubMed] [Google Scholar]
- Granero R., Fernández-Aranda F., Steward T., Mestre-Bach G., Baño M., del Pino-Gutiérrez A., Moragas L., Aymamí N., Gómez-Peña M., Mallorquí-Bagué N., Tárrega S., Menchón J. M., Jiménez-Murcia S. (2016). Compulsive buying behavior: Characteristics of comorbidity with gambling disorder. Frontiers in Psychology, 7, 625. doi: 10.3389/fpsyg.2016.00625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granero R., Penelo E., Martínez-Giménez R., Álvarez-Moya E., Gómez-Peña M., Aymamí M. N., Bueno B., Fernández-Aranda F., Jiménez-Murcia S. (2009). Sex differences among treatment-seeking adult pathologic gamblers. Comprehensive Psychiatry, 50(2), 173–180. doi: 10.1016/j.comppsych.2008.07.005 [DOI] [PubMed] [Google Scholar]
- Granero R., Penelo E., Stinchfield R., Fernandez-Aranda F., Savvidou L. G., Fröberg F., Aymamí N., Gómez-Peña M., Pérez-Serrano M., del Pino-Gutiérrez A., Menchón J. M., Jiménez-Murcia S. (2014). Is pathological gambling moderated by age? Journal of Gambling Studies, 30(2), 475–492. doi: 10.1007/s10899-013-9369-6 [DOI] [PubMed] [Google Scholar]
- Grant J. E., Chamberlain S. R., Schreiber L. R. N., Odlaug B. L. (2012). Gender-related clinical and neurocognitive differences in individuals seeking treatment for pathological gambling. Journal of Psychiatric Research, 46(9), 1206–1211. doi: 10.1016/j.jpsychires.2012.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant J. E., Kim S. W. (2002). Gender differences in pathological gamblers seeking medication treatment. Comprehensive Psychiatry, 43(1), 56–62. doi: 10.1053/comp.2002.29857 [DOI] [PubMed] [Google Scholar]
- Grant J. E., Odlaug B. L., Mooney M. E. (2012). Telescoping phenomenon in pathological gambling: Association with gender and comorbidities. Journal of Nervous and Mental Disease, 200(11), 996–998. doi: 10.1097/NMD.0b013e3182718a4d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutiérrez-Zotes J. A., Bayón C., Montserrat J., Valero J., Labad A., Cloninger C. R., Fernández-Aranda F. (2004). Inventario del Temperamento y el Carácter-Revisado (TCI-R). Baremación y datos normativos en una muestra de población general. Actas Españolas de Psiquiatría, 32(1), 8–15. [PubMed] [Google Scholar]
- Heiskanen M., Toikka A. (2016). Clustering Finnish gambler profiles based on the money and time consumed in gambling activities. Journal of Gambling Studies, 32(2), 363–377. doi: 10.1007/s10899-015-9556-8 [DOI] [PubMed] [Google Scholar]
- Hing N., Russell A., Tolchard B., Nower L. (2016). Risk factors for gambling problems: An analysis by gender. Journal of Gambling Studies, 32(2), 511–534. doi: 10.1007/s10899-015-9548-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgins D. C., Holub A. (2015). Components of impulsivity in gambling disorder. International Journal of Mental Health and Addiction, 13(6), 699–711. doi: 10.1007/s11469-015-9572-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu J., Lee D., Hu S., Zhang S., Chao H., Li C.-S. R. (2016). Individual variation in the neural processes of motor decisions in the stop signal task: the influence of novelty seeking and harm avoidance personality traits. Brain Structure & Function, 221(5), 2607–2618. doi: 10.1007/s00429-015-1061-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iancu I., Lowengrub K., Dembinsky Y., Kotler M., Dannon P. N. (2008). Pathological gambling: An update on neuropathophysiology and pharmacotherapy. CNS Drugs, 22(5), 406–406. [DOI] [PubMed] [Google Scholar]
- Ibáñez A., Blanco C., Moreryra P., Saiz-Ruiz J. (2003). Gender differences in pathological gambling. The Journal of Clinical Psychiatry, 64(3), 295–301. [DOI] [PubMed] [Google Scholar]
- Jiménez-Murcia S., Aymamí-Sanromà M., Gómez-Peña M., Álvarez-Moya E., Vallejo J. (2006). Protocols de tractament cognitivoconductual pel joc patològic i d’altres addiccions no tòxiques [Treatment protocols for CBT treatment for pathological gambling and other non-substance addictions]. Barcelona: Hospital Universitari de Bellvitge, Departament de Salut, Generalitat de Catalunya. [Google Scholar]
- Jiménez-Murcia S., Fernández-Aranda F., Granero R., Menchón J. M. (2014). Gambling in Spain: Update on experience, research and policy. Addiction, 109(10), 1595–1601. doi: 10.1111/add.12232 [DOI] [PubMed] [Google Scholar]
- Jiménez-Murcia S., Granero R., Moragas L., Steiger H., Israel M., Aymamí N., Gómez-Peña M., Sauchelli S., Agüera Z., Sánchez I., Riesco N., Penelo E., Menchón J. M., Fernández-Aranda F. (2015). Differences and similarities between bulimia nervosa, compulsive buying and gambling disorder. European Eating Disorders Review, 23(2), 111–118. doi: 10.1002/erv.2340 [DOI] [PubMed] [Google Scholar]
- Jiménez-Murcia S., Steiger H., Isräel M., Granero R., Prat R., Santamaría J. J., Moragas L., Sánchez I., Custal N., Orekhova L., Fagundo A. B., Menchón J., Fernández-Aranda F. (2013). Pathological gambling in eating disorders: Prevalence and clinical implications. Comprehensive Psychiatry, 54(7), 1053–1060. doi: 10.1016/j.comppsych.2013.04.014 [DOI] [PubMed] [Google Scholar]
- Jiménez-Murcia S., Stinchfield R., Alvarez-Moya E., Jaurrieta N., Bueno B., Granero R., Aymamí M. N., Gómez-Peña M., Martínez-Giménez N., Fernández-Aranda F., Vallejo J. (2009). Reliability, validity, and classification accuracy of a Spanish translation of a measure of DSM-IV diagnostic criteria for pathological gambling. Journal of Gambling Studies, 25(1), 93–104. doi: 10.1007/s10899-008-9104-x [DOI] [PubMed] [Google Scholar]
- Joukhador J., Blaszczynski A., Maccallum F. (2004). Superstitious beliefs in gambling among problem and non-problem gamblers: Preliminary data. Journal of Gambling Studies, 20(2), 171–180. doi: 10.1023/B:JOGS.0000022308.27774.2b [DOI] [PubMed] [Google Scholar]
- Ladd G. T., Petry N. M. (2002). Gender differences among pathological gamblers seeking treatment. Experimental and Clinical Psychopharmacology, 10(3), 302–309. doi: 10.1037/1064-1297.10.3.302 [DOI] [PubMed] [Google Scholar]
- Lesieur H. R., Blume S. B. (1987). The South Oaks Gambling Screen (SOGS): A new instrument for the identification of pathological gamblers. The American Journal of Psychiatry, 144(9), 1184–1188. doi: 10.1176/ajp.144.9.1184 [DOI] [PubMed] [Google Scholar]
- Lorains F. K., Cowlishaw S., Thomas S. A. (2011). Prevalence of comorbid disorders in problem and pathological gambling: Systematic review and meta-analysis of population surveys. Addiction, 106(3), 490–498. doi: 10.1111/j.1360-0443.2010.03300.x [DOI] [PubMed] [Google Scholar]
- Martinotti G., Andreoli S., Giametta E., Poli V., Bria P., Janiri L. (2006). The dimensional assessment of personality in pathologic and social gamblers: The role of novelty seeking and self-transcendence. Comprehensive Psychiatry, 47(5), 350–356. doi: 10.1016/j.comppsych.2005.12.005 [DOI] [PubMed] [Google Scholar]
- Mestre-Bach G., Granero R., Steward T., Fernández-Aranda F., Baño M., Aymamí N., Gómez-Peña M., Agüera Z., Mallorquí-Bagué N., Moragas L., Del Pino-Gutiérrez A., Soriano-Mas C., Navas J. F., Perales J. C., Menchón J. M., Jiménez-Murcia S. (2016). Reward and punishment sensitivity in women with gambling disorder or compulsive buying: Implications in treatment outcome. Journal of Behavioral Addictions, 5(4), 658–665. doi: 10.1556/2006.5.2016.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mestre-Bach G., Steward T., Granero R., Fernández-Aranda F., Talón-Navarro M. T., Cuquerella À., Del Pino-Gutiérrez A., Aymamí N., Gómez-Peña M., Mallorquí-Bagué N., Mena-Moreno T., Vintró-Alcaraz C., Baño M., Moragas L., Magaña P., Menchón J. M., Jiménez-Murcia S. (2018). Sociodemographic and psychopathological predictors of criminal behavior in women with gambling disorder. Addictive Behaviors, 80, 124–129. doi: 10.1016/j.addbeh.2018.01.022 [DOI] [PubMed] [Google Scholar]
- Milosevic A., Ledgerwood D. M. (2010). The subtyping of pathological gambling: A comprehensive review. Clinical Psychology Review, 30(8), 988–998. doi: 10.1016/j.cpr.2010.06.013 [DOI] [PubMed] [Google Scholar]
- Montag C., Jurkiewicz M., Reuter M. (2010). Low self-directedness is a better predictor for problematic Internet use than high neuroticism. Computers in Human Behavior, 26(6), 1531–1535. doi: 10.1016/j.chb.2010.05.021 [DOI] [Google Scholar]
- Moragas L., Granero R., Stinchfield R., Fernández-Aranda F., Fröberg F., Aymamí N., Gómez-Peña M., Fagundo A. B., Islam M. A., Del Pino-Gutiérrez A., Agüera Z., Savvidou L. G., Arcelus J., Witcomb G. L., Sauchelli S., Menchón J. M., Jiménez-Murcia S. (2015). Comparative analysis of distinct phenotypes in gambling disorder based on gambling preferences. BMC Psychiatry, 15(1), 86. doi: 10.1186/s12888-015-0459-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nower L., Derevensky J. L., Gupta R. (2004). The relationship of impulsivity, sensation seeking, coping, and substance use in youth gamblers. Psychology of Addictive Behaviors, 18(1), 49–55. doi: 10.1037/0893-164X.18.1.49 [DOI] [PubMed] [Google Scholar]
- Nylund K. L., Asparouhov T., Muthén B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. doi: 10.1080/10705510701575396 [DOI] [Google Scholar]
- Oleski J., Cox B. J., Clara I., Hills A. (2011). Pathological gambling and the structure of common mental disorders. The Journal of Nervous and Mental Disease, 199(12), 956–960. doi: 10.1097/NMD.0b013e3182392931 [DOI] [PubMed] [Google Scholar]
- Petry N. M., Stinson F. S., Grant B. F. (2005). Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry, 66(5), 564–574. doi: 10.4088/JCP.v66n0504 [DOI] [PubMed] [Google Scholar]
- Pilver C. E., Libby D. J., Hoff R. A., Potenza M. N. (2013). Gender differences in the relationship between gambling problems and the incidence of substance-use disorders in a nationally representative population sample. Drug and Alcohol Dependence, 133(1), 204–211. doi: 10.1016/j.drugalcdep.2013.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quigley L., Yakovenko I., Hodgins D. C., Dobson K. S., El-Guebaly N., Casey D. M., Currie S. R., Smith G. J., Williams R. J., Schopflocher D. P. (2014). Comorbid problem gambling and major depression in a community sample. Journal of Gambling Studies, 31(4), 1135–1152. doi: 10.1007/s10899-014-9488-8 [DOI] [PubMed] [Google Scholar]
- Rash C. J., Weinstock J., Petry N. M. (2011). Drinking patterns of pathological gamblers before, during, and after gambling treatment. Psychology of Addictive Behaviors, 25(4), 664–674. doi: 10.1037/a0025565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronzitti S., Lutri V., Smith N., Clerici M., Bowden-Jones H. (2016). Gender differences in treatment-seeking British pathological gamblers. Journal of Behavioral Addictions, 5(2), 231–238. doi: 10.1556/2006.5.2016.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rousseeuw P. J. (1987). Silhouettes: A graphical aid to the interpretation and validation of cluster analysis. Journal of Computational and Applied Mathematics, 20, 53–65. doi: 10.1016/0377-0427(87)90125-7 [DOI] [Google Scholar]
- Schwarz G. (1978). Estimating the dimension of a model. The Annals of Statistics, 6, 461–464. [Google Scholar]
- Shin Y. C., Choi S. W., Ha J., Mok J. Y., Lim S. W., Choi J. S., Kim D. J. (2014). Age of pathological gambling onset: Clinical and treatment-related features. Journal of Addiction Medicine, 8(3), 205–210. doi: 10.1097/ADM.0000000000000031 [DOI] [PubMed] [Google Scholar]
- Slutske W. S., Blaszczynski A., Martin N. G. (2009). Sex differences in the rates of recovery, treatment-seeking, and natural recovery in pathological gambling: Results from an Australian community-based twin survey. Twin Research and Human Genetics, 12(5), 425–432. doi: 10.1375/twin.12.5.425 [DOI] [PubMed] [Google Scholar]
- Slutske W. S., Piasecki T. M., Deutsch A. R., Statham D. J., Martin N. G. (2015). Telescoping and gender differences in the time course of disordered gambling: Evidence from a general population sample. Addiction, 110(1), 144–151. doi: 10.1111/add.12717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith D., Battersby M., Harvey P. (2015). Does gender moderate the subjective measurement and structural paths in behavioural and cognitive aspects of gambling disorder in treatment-seeking adults? Addictive Behaviors, 48, 12–18. doi: 10.1016/j.addbeh.2015.04.001 [DOI] [PubMed] [Google Scholar]
- Spinella M. (2003). Evolutionary mismatch, neural reward circuits, and pathological gambling. International Journal of Neuroscience, 113(4), 503–512. doi: 10.1080/00207450390162254 [DOI] [PubMed] [Google Scholar]
- Stewart S. H., Zack M., Collins P., Klein R. M. (2008). Subtyping pathological gamblers on the basis of affective motivations for gambling: Relations to gambling problems, drinking problems, and affective motivations for drinking. Psychology of Addictive Behaviors, 22(2), 257–268. doi: 10.1037/0893-164X.22.2.257 [DOI] [PubMed] [Google Scholar]
- Stinchfield R. (2003). Reliability, validity, and classification accuracy of a measure of DSM-IV diagnostic criteria for pathological gambling. American Journal of Psychiatry, 160(1), 180–182. doi: 10.1176/appi.ajp.160.1.180 [DOI] [PubMed] [Google Scholar]
- Tackett J. L., Krieger H., Neighbors C., Rinker D., Rodriguez L., Edward G. (2017). Comorbidity of alcohol and gambling problems in emerging adults: A bifactor model conceptualization. Journal of Gambling Studies, 33(1), 131–147. doi: 10.1007/s10899-016-9618-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavares H., Zilberman M. L., Hodgins D. C., El-Guebaly N. (2005). Comparison of craving between pathological gamblers and alcoholics. Alcoholism: Clinical and Experimental Research, 29(8), 1427–1431. doi: 10.1097/01.alc.0000175071.22872.98 [DOI] [PubMed] [Google Scholar]
- Valleur M. (2015). Gambling and gambling-related problems in France. Addiction, 110(12), 1872–1876. doi: 10.1111/add.12967 [DOI] [PubMed] [Google Scholar]
- Valleur M., Codina I., Vénisse J. L., Romo L., Magalon D., Fatséas M., Chéreau-Boudet I., Gorsane M. A., Guilleux A., Groupe J. E. U., Grall-Bronnec M., Challet-Bouju G. (2016). Towards a validation of the three pathways model of pathological gambling. Journal of Gambling Studies, 32(2), 757–771. doi: 10.1007/s10899-015-9545-y [DOI] [PubMed] [Google Scholar]
- Yau Y. H. C., Crowley M. J., Mayes L. C., Potenza M. N. (2012). Are Internet use and video-game-playing addictive behaviors? Biological, clinical and public health implications for youths and adults. Minerva Psichiatrica, 53(3), 153. [PMC free article] [PubMed] [Google Scholar]