Abstract
Purpose:
Patients with estrogen receptor positive (ER+) breast cancer are often non-adherent to endocrine therapies, despite clear survival benefits. We utilized a nationally representative cancer cohort to examine the role of specific mental illnesses on endocrine therapy adherence.
Methods:
Using the SEER-Medicare database, we included 21,894 women aged 68+ at their first surgically treated stage I-IV ER+ breast cancer during 2007–2013. All had continuous fee-for-service Medicare Parts A and B for 36+ months before, 18+ months after diagnosis, and continuous Part D for 4+ months before, 18+ after diagnosis. Mental illness was defined as occurring in the 36 months prior to cancer onset. We analyzed endocrine therapy adherence, initiation, and discontinuation using longitudinal linear and Cox regression models.
Results:
Unipolar depression (11.0%), anxiety (9.5%), non-schizophrenia psychosis (4.6%), and dementias (4.6%) were the most prevalent diagnoses. Endocrine therapies were initiated by 80.0% of women. Among those with at least one year of use, 28.0% were non-adherent (<0.80 adherence, mean=0.84) and 25.7% discontinued. Patients with dementia or bipolar depression/psychotic/schizophrenia disorders had lower adjusted initiation probabilities by year one of follow-up, versus those without these diagnoses [0.74 95% CI (0.73–0.74) and 0.73 (0.72–0.73), respectively, reference 0.76 (0.76–0.77)]. Patients with substance use or anxiety disorders less frequently continued endocrine therapy for at least one year, after adjustment, [0.85 95% CI (0.85–0.86) and 0.88 (0.87–0.88), respectively, reference 0.90 (0.89–0.90)]. Patients with substance use disorders had 2.3% lower adherence rates (p<0.001).
Conclusions:
Nearly one-quarter of female Medicare beneficiaries have diagnosed mental illness preceding invasive breast cancer. Those with certain mental illnesses have modestly reduced rates of initiation, adherence, and discontinuation and this may help define patients at higher risk of treatment abandonment. Overall, endocrine therapy adherence remains suboptimal, unnecessarily worsening recurrence and mortality risk.
Introduction
Endocrine therapies improve survival in patients with estrogen receptor positive (ER+) breast cancer [1]. Guidelines suggest endocrine therapies should be taken daily for a minimum of five years [1]. Despite the gravity of a cancer diagnosis, most patients do not adhere to a five-year endocrine therapy regimen [2–4]. A study of over 8700 women in the Northern California Kaiser Permanente system found only 49% fully adhered to endocrine therapy [3]. Endocrine therapy adherence is critically related to patient outcomes; as adherence decreases, all-cause mortality can increase up to 49% [5].
Identified factors affecting endocrine therapy adherence include age, adverse reactions/pain, and “psychological problems” [6]. In the National Surgical Adjuvant Breast and Bowel Project P-1 Study, poor mental “well-being” was identified as a risk factor for non-adherence [7]. A meta-analysis of depression and endocrine therapy adherence reported that it increased the odds of non-adherence, OR 1.89 (95% CI 1.38–2.57) [8]. However, the studies were heterogenous in measurement and few focused on specific mental health diagnoses [8]. Although not examining endocrine therapy, studies of Medicare-enrolled breast cancer patients found bipolar disorder, schizophrenia and psychotic disorders were associated with primary treatment delays and increased mortality [9, 10]. The role of mental illness in endocrine therapy adherence remains unclear.
To examine the prevalence and influence of preexisting mental illness on endocrine therapy adherence, we used the NCI linkage of Medicare claims to Surveillance, Epidemiology, and End-Results (SEER) data to identify a large, nationally representative cohort of older women with breast cancer. Because breast cancer diagnoses occur at a median age of 62, SEER-Medicare data provide a near-ideal population and healthcare claims to assess this question [11].
Methods
Study Population
We selected a cohort of women from the SEER-Medicare database aged 68 or older at the time of a surgically treated first primary estrogen receptor positive (ER+) stage I-IV breast cancer, diagnosed in 2007–2013 [11]. SEER registries cover 28% of the US population, including approximately 25% of White Americans, 26% of Black Americans, 43% of American Indians, 50% of Asian Americans, and 38% of Hispanic Americans [12]. These data include patient demographics, tumor characteristics, cancer and other diagnoses (International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)), clinical procedures (Healthcare Common Procedure Coding System (HCPCS) and Current Procedural Terminology (CPT) codes), and prescription National Drug Codes (NDC))[13].
Included women had continuous fee-for-service Parts A and B Medicare coverage for 36 or more months before and 18 or more after cancer diagnosis, and Part D coverage for 4 or more months before and 18 or more after cancer diagnosis. Women with only non-invasive ductal carcinoma in situ or lobular carcinoma in situ were excluded. Because diagnosis can occur as a process over time, additional breast tumors detected within three months of the first were considered the same cancer treatment experience (applied to 4.7% of cohort), characterized by the first diagnosis date and the highest tumor stage reported. To ensure data reliability, we required cancer diagnosis prior to date of death and concordant death dates between SEER and Medicare files. We excluded 154 patients with unreliable endocrine therapy claims (exceeding a 10:1 ratio of prescription fill size to days supplied, or vice versa), which biases adherence measures. Using these criteria, we identified 21,894 eligible patients. We censored observations at death date, start of hospice care, diagnosis of a new breast cancer, and end of continuous feefor-service Medicare coverage or available claims information.
Measures
Demographic variables (age at diagnosis, race, ethnicity) and tumor characteristics (estrogen and progesterone receptor status, AJCC 6th edition stage, month and year of breast cancer diagnosis) were obtained from SEER data [13, 14]. General comorbidity and mental illness diagnoses were obtained from Medicare claims. We measured general comorbidity in the 36 months prior to diagnosis using an adjusted NCI comorbidity index, excluding dementia [15]. Using the Diagnostic and Statistical Manual of Mental Disorders-IV categories as a guide, we selected 11 mental illness classes [16] (Table 1). “Non-schizophrenia psychotic” disorders excluded schizophrenia/schizoaffective diseases, but included psychoses with delusional, depressive, and non-specific subtypes. “Drug use” disorders included tobacco and illicit substances. Dementia disorders were included as they impact cognition and behavior, and to control for potential confounding with comorbid mental illness and adherence. We required a single inpatient ICD-9 mental illness diagnosis in the 36 months prior to cancer diagnosis, or two outpatient claims for the same illness class separated by 30 or more days to confirm a diagnosis. Only one outpatient claim was required to characterize prior experience of delirium, as a measure of cognitive vulnerability.
Table 1:
Characteristics of Breast Cancer Patients Diagnosed 2007–2013, According to Endocrine Therapy Use
| Covariate | Level | Total Cohort | Endocrine Therapy Initiation | HR (95% CI) | p value* | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N=21,894 | Yes N=17,512 | No N=4,382 | ||||||||
| Age at Diagnosis | 68–74 | 9,308 (42.5%) | 8,133 | 46.4% | 1,175 | 26.8% | ref | |||
| 75–84 | 9,659 (44.1%) | 7,588 | 43.3% | 2,071 | 47.3% | 0.91 (0.88–0.94) | <.001 | |||
| 85–94 | 2,831 (12.9%) | 1,744 | 10.0% | 1,087 | 24.8% | 0.64 (0.60–0.67) | <.001 | |||
| 95+ | 96 (0.4%) | 47 | 0.3% | 49 | 1.1% | 0.44 (0.33–0.59) | <.001 | |||
| Race | Asian | 950 (4.3%) | 781 | 4.5% | 169 | 3.9% | 1.11 (1.04–1.20) | 0.004 | ||
| Black | 1,315 (6.0%) | 1,083 | 6.2% | 232 | 5.3% | 0.99 (0.93–1.05) | 0.77 | |||
| Other | 149 (0.7%) | 119 | 0.7% | 30 | 0.7% | 1.02 (0.85–1.22) | 0.83 | |||
| White | 19,480 (89.0%) | 15,529 | 88.7% | 3,951 | 90.2% | ref | ||||
| Ethnicity | Hispanic | 1,166 (5.3%) | 983 | 5.6% | 183 | 4.2% | 1.03 (0.97–1.10) | 0.33 | ||
| Non- Hispanic | 20,728 (94.7%) | 16,529 | 94.4% | 4,199 | 95.8% | ref | ||||
| Year of Diagnosis | 2007 | 1,961 (9.0%) | 1,528 | 8.7% | 433 | 9.9% | ref | |||
| 2008 | 2,968 (13.6%) | 2,312 | 13.2% | 656 | 15.0% | 0.99 (0.93–1.06) | 0.76 | |||
| 2009 | 3,144 (14.4%) | 2,473 | 14.1% | 671 | 15.3% | 1.01 (0.95–1.08) | 0.72 | |||
| 2010 | 3,131 (14.3%) | 2,525 | 14.4% | 606 | 13.8% | 1.13 (1.06–1.20) | <.001 | |||
| 2011 | 3,300 (15.1%) | 2,664 | 15.2% | 636 | 14.5% | 1.18 (1.10–1.25) | <.001 | |||
| 2012 | 3,492 (15.9%) | 2,832 | 16.2% | 660 | 15.1% | 1.17 (1.10–1.25) | <.001 | |||
| 2013 | 3,898 (17.8%) | 3,178 | 18.1% | 720 | 16.4% | 1.21 (1.14–1.29) | <.001 | |||
| Stage at Diagnosis | 1 | 13,194 (60.3%) | 10,046 | 57.4% | 3,148 | 71.8% | ref | |||
| 2 | 6,534 (29.8%) | 5,596 | 32.0% | 938 | 21.4% | 1.13 (1.10–1.17) | <.001 | |||
| 3 | 1,516 (6.9%) | 1,378 | 7.9% | 138 | 3.1% | 1.07 (1.01–1.13) | 0.02 | |||
| 4 | 201 (0.9%) | 181 | 1.0% | 20 | 0.5% | 1.50 (1.29–1.74) | <.001 | |||
| Unknown | 449 (2.1%) | 311 | 1.8% | 138 | 3.1% | 0.82 (0.73–0.92) | <.001 | |||
| Receptor Status | ER+PR+ | 18,789 (85.8%) | 15,095 | 86.2% | 3,694 | 84.3% | 1.16 (1.11–1.21) | <.001 | ||
| ER+PR− | 3,105 (14.2%) | 2,417 | 13.8% | 688 | 15.7% | ref | ||||
| Endocrine Therapy Class Used | AIs | 13,659 (62.4%) | 13,659 | 78.0% | 0 | 0.0% | n/a | |||
| Both | 1,903 (8.7%) | 1,903 | 10.9% | 0 | 0.0% | |||||
| None | 4,382 (20.0%) | 0 | 0.0% | 4,382 | 100.0% | |||||
| SERMs | 1,950 (8.9%) | 1,950 | 11.1% | 0 | 0.0% | |||||
| Adjusted NCI Comorbidity Score | Mean (Median) | 2.1 (2.0) | 2.0 | 2.0 | 2.2 | 2.0 | 0.99 (0.98–1.00) | 0.01 | ||
| Any Mental Illness | N (%) | 5,459 (24.9%) | 4,232 | 24.2% | 1,227 | 28.0% | 0.95 (0.92–0.98) | 0.003 | ||
| Emotional Disorders: | ||||||||||
| Unipolar Depression | N (%) | 2,418 (11.0%) | 1,876 | 10.7% | 542 | 12.4% | 0.95 (0.90–0.99) | 0.03 | ||
| Anxiety | N (%) | 2,089 (9.5%) | 1,651 | 9.4% | 438 | 10.0% | 1.00 (0.95–1.05) | 0.87 | ||
| Adjustment | N (%) | 81 (0.4%) | 62 | 0.4% | 19 | 0.4% | 0.93 (0.72–1.19) | 0.56 | ||
| Cognitive Disorders: | ||||||||||
| Delirium | N (%) | 515 (2.4%) | 365 | 2.1% | 150 | 3.4% | 0.85 (0.77–0.94) | 0.002 | ||
| Dementia | N (%) | 1,017 (4.6%) | 690 | 3.9% | 327 | 7.5% | 0.82 (0.76–0.88) | <.001 | ||
| Personality | N (%) | 59 (0.3%) | 38 | 0.2% | 21 | 0.5% | 0.77 (0.56–1.07) | 0.12 | ||
| Mania and Psychoses: | ||||||||||
| Bipolar Depression | N (%) | 265 (1.2%) | 198 | 1.1% | 67 | 1.5% | 0.85 (0.74–0.98) | 0.02 | ||
| Schizophrenia | N (%) | 185 (0.8%) | 144 | 0.8% | 41 | 0.9% | 0.99 (0.84–1.17) | 0.94 | ||
| Non-Schizophrenia Psychosis | N (%) | 1,004 (4.6%) | 755 | 4.3% | 249 | 5.7% | 0.89 (0.83–0.96) | 0.003 | ||
| Substance Use: | ||||||||||
| Drug Use | N (%) | 970 (4.4%) | 774 | 4.4% | 196 | 4.5% | 0.99 (0.92–1.06) | 0.69 | ||
| Alcohol Use | N (%) | 75 (0.3%) | 57 | 0.3% | 18 | 0.4% | 1.01 (0.78–1.31) | 0.96 | ||
| Follow-Up Days | Mean (Median) | 1,377.9 (1,280.0) | 1,382.8 | 1,280.0 | 1,358.2 | 1,242.0 | 0.98 (0.97–0.99) (per 1 year change) | <.001 | ||
| Number Who Initiated | 17,512 | n/a | ||||||||
| Days to Initiation | Mean (Median) | 156.6 | 120.0 | |||||||
| Number Who Discontinued | 4,503 | n/a | ||||||||
| aDays to Discontinuation | Mean (Median) | 701.5 | 521.0 | |||||||
| Number with 1+ years Endocrine Therapy Use | 14,517 | n/a | ||||||||
| bAverage Adherence (PDC) | Mean (Median) | 0.84 | 0.90 | |||||||
| Percent With 0.80 or Higher | 72.0 | |||||||||
Proportion of Days Covered (PDC).
Discontinuation analyzed for the first 5 years of endocrine therapy use.
Average adherence calculated for patients with 1+ years of endocrine therapy use observed, and less than half of follow-up spent hospitalized or in skilled nursing facilities.
p values calculated from bivariable Cox regression.
Endocrine therapy variables were derived from prescription drug claims. Endocrine therapies included selective estrogen receptor modulators (SERMs: tamoxifen and toremifene), and aromatase inhibitors (AIs: anastrozole, exemestane, letrozole). Initiation was defined as the first endocrine therapy claim date after cancer diagnosis. Discontinuation occurred the day after the last available pill, with no further use in the remaining 90 or greater days of follow-up [17]. Prior to 2014, ASCO guidelines suggested five years of endocrine therapy use, so we examined discontinuation within the first five years of treatment [18].
Adherence was calculated using the “Proportion of Days Covered” measure (PDC = days covered by endocrine therapy prescriptions/days in follow-up) [19]. We calculated PDC in one-year intervals, beginning at treatment initiation, concluding at discontinuation or a maximum fifth available year of follow-up. If patients switched SERM and AI classes, remaining medication from the prior class was assumed discarded when new treatment began. Medication extending beyond the available follow-up period was not included in calculations. Time hospitalized or in skilled nursing facilities was removed from observation because medication received in those care settings should not be billed to Medicare Part D [20]. If greater than half of an observation year was spent hospitalized/in skilled care, that year was excluded from analysis.
Initiation Model and Discontinuation Model Selection
Initiation and discontinuation were assessed using Cox regression, with censoring at end of continuous fee-for-service Medicare coverage or available claims, diagnosis of a new breast cancer, start of hospice care, or death. Endocrine therapy initiation follow-up began the day of cancer diagnosis, whereas discontinuation follow-up began the day of endocrine therapy initiation. Bivariable Hazard Ratios were produced using unadjusted Cox regression. Multivariable models included individual predictors for mental illness and baseline covariates (at cancer diagnosis) for stage, age, year of diagnosis, race, ethnicity, and adjusted three-year NCI comorbidity index [21].
In multivariable analysis, we used the Akaike Information Criterion (AIC) to compare models fit with individual mental illnesses against models fit with prespecified combinations of phenotypically similar illnesses [22]. Combinations included: emotional (unipolar depression, adjustment, anxiety), bipolar and psychoses (bipolar depression, non-schizophrenia psychosis, schizophrenia), substance use (alcohol use disorder, drug use disorder), and cognitive disorders (dementia, delirium). A combined variable was retained if it reduced initiation model AIC relative to individual mental illness variables.
To quantify effects of mental illness on initiation and discontinuation, we calculated direct adjusted Cox model curves, producing probabilities adjusted for baseline characteristics, in landmark analyses at year one of follow-up [23]. Instead of estimating probability for a theoretical patient with average covariate values, the direct adjustment method calculates probability for every patient and presents an overall average, improving estimations [23].
Adherence Model Selection
Adherence was assessed using linear regression models fit with the method of generalized estimating equations (normal distribution and identity link), to account for repeated longitudinal observations. An “unstructured” within-subject correlation structure was selected among autoregressive(1), Toeplitz, compound symmetry, and independent structures, based on Quasi-likelihood Information Criteria values computed with models including predictors for all mental illnesses and baseline covariates [21, 24].
Unadjusted bivariable models described individual effects of mental illness. Our final multivariable model employed the same combination mental illness categories selected for the Cox models, allowing for comparison between all outcomes. Statistical analysis was conducted with SAS v9.4 statistical software (SAS Institute Inc., Cary, NC).
Results
We identified 21,894 SEER-Medicare patients with ER+ breast cancer diagnosed between 2007–2013. At diagnosis, 42.5% of patients were aged 68–74, 44.1% were 75–84, 12.9% were 85–94, and less than 1% were 95+. Most patients were White (89.0%), most tumors were stage I at diagnosis (60.3%), followed by stage II (29.8%), all were ER+, and 85.8% were PR+. Mental illness was common; 24.9% of patients had some diagnosis prior to cancer. Unipolar depression (11.0%), anxiety (9.5%), dementias (4.6%), and non-schizophrenia psychotic (4.6%) disorders were most prevalent, followed by drug use disorders (4.4%), delirium (2.4%), bipolar depression (1.2%), schizophrenia (0.8%), adjustment (0.4%), alcohol use (0.3%), and personality disorders (0.3%) (Table 1).
After cancer diagnosis, 80.0% of patients initiated endocrine therapies. AIs were used by 78.0%, SERMs by 11.1%, and both AI and SERMs by 10.9%. Of initiators, 25.7% discontinued therapy within five years of follow-up. Among initiators with at least one year of continuous treatment, mean adherence was 0.84, and 72.0% had adherence rates of 0.80+ (Table 1).
Patients who initiated endocrine therapies were younger compared to never-users (46.4% aged 68–74 vs 26.8%, p<0.001) (Table 1). Initiators less frequently had stage I tumors (57.4% vs 71.8%, p<0.05), and less frequently had mental illness diagnoses (24.2% vs 28.0%, p=0.003). Never-users had higher rates of unipolar and bipolar depression, delirium, dementia, and non-schizophrenia psychoses (all p<0.05).
Compared to patients without, those with mental illness were more frequently age 85+ at cancer diagnosis, White, Black, Hispanic, diagnosed at stage II or higher, and had greater comorbidity. Patients with mental illness had shorter available follow-up (1,150 median days vs 1,326, p<0.001) and were more frequently censored due to death (8.9% vs 5.4%, p<0.001). Although fewer patients with mental illness initiated endocrine therapies, those who did started slightly earlier (median 115 vs 121 days, p=0.002) but discontinued earlier (median 445.0 vs 547.5 days, p<0.001). Among patients with 1+ year of observed endocrine therapy use, fewer patients with mental illness had 0.80+ adherence rates (70.1% vs 72.6%, p=0.005) (Table 2).
Table 2:
Characteristics of Breast Cancer Patients Diagnosed 2007–2013, According to History of Mental Illness
| Covariate | Level | History of Mental Illness | p value* | |||
|---|---|---|---|---|---|---|
| No n=16,435 | Yes n=5,459 | |||||
| Age at Diagnosis | 68–74 | 7,006 | 42.6% | 2,302 | 42.2% | 0.004 |
| 75–84 | 7,307 | 44.5% | 2,352 | 43.1% | ||
| 85–94 | 2,057 | 12.5% | 774 | 14.2% | ||
| 95+ | 65 | 0.4% | 31 | 0.6% | ||
| Race | Asian | 808 | 4.9% | 142 | 2.6% | <0.001 |
| Black | 950 | 5.8% | 365 | 6.7% | ||
| Other | 108 | 0.7% | 41 | 0.8% | ||
| White | 14,569 | 88.6% | 4,911 | 90.0% | ||
| Ethnicity | Hispanic | 848 | 5.2% | 318 | 5.8% | 0.06 |
| Non-Hispanic | 15,587 | 94.8% | 5,141 | 94.2% | ||
| Year of Diagnosis | 2007 | 1,526 | 9.3% | 435 | 8.0% | <0.001 |
| 2008 | 2,280 | 13.9% | 687 | 12.6% | ||
| 2009 | 2,394 | 14.6% | 750 | 13.7% | ||
| 2010 | 2,360 | 14.4% | 771 | 14.1% | ||
| 2011 | 2,469 | 15.0% | 831 | 15.2% | ||
| 2012 | 2,572 | 15.6% | 920 | 16.9% | ||
| 2013 | 2,833 | 17.2% | 1,065 | 19.5% | ||
| Stage at Diagnosis | 1 | 10,081 | 61.3% | 3,113 | 57.0% | <0.001 |
| 2 | 4,790 | 29.1% | 1,744 | 31.9% | ||
| 3 | 1,075 | 6.5% | 441 | 8.1% | ||
| 4 | 160 | 1.0% | 41 | 0.8% | ||
| Unknown | 329 | 2.0% | 120 | 2.2% | ||
| Receptor Status | ER+PR+ | 14,151 | 86.1% | 4,638 | 85.0% | 0.04 |
| ER+PR− | 2,284 | 13.9% | 821 | 15.0% | ||
| Endocrine Therapy Class Used | AIs | 10,366 | 63.1% | 3,293 | 60.3% | <0.001 |
| Both | 1,468 | 8.9% | 435 | 8.0% | ||
| None | 3,155 | 19.2% | 1,227 | 22.5% | ||
| SERMs | 1,446 | 8.8% | 504 | 9.2% | ||
| Adjusted NCI Comorbidity Score | Mean (Median) | 1.8 (1.0) | 2.8 (2.0) | <.001 | ||
| Follow–Up Days | Mean (Median) | 1,141.7 (1,326.0) | 1,267.0 (1,150.0) | <.001 | ||
| Number Censored at Death | 889 | 5.4% | 487 | 8.9% | <.001 | |
| Number Who Initiated | 13,280 | 4,232 | ||||
| Days to Initiation | Mean (Median) | 157.7 (121.0) | 153.5 (115.0) | 0.002 | ||
| Number Who Discontinued | 3,376 | 1,127 | ||||
| aDays to Discontinuation | Mean (Median) | 727.0 (547.5) | 625.1 (445.0) | <.001 | ||
| Number With 1+ Years Endocrine Therapy Use | 11,120 | 3,397 | ||||
| bAverage Adherence (PDC) | Mean (Median) | 0.84 (0.90) | 0.84 (0.90) | 0.27 | ||
| Percent With 0.80 or Higher | 72.6 | 70.1 | 0.005 | |||
Proportion of Days Covered (PDC).
Discontinuation analyzed for the first 5 years of endocrine therapy use.
Average adherence calculated for patients with 1+ years of endocrine therapy use observed, and less than half of their follow-up spent hospitalized or in skilled nursing facilities.
Categorical and continuous p values calculated from Chi-square and Wilcoxon tests, respectively.
Initiation was less common in patients with any mental illness (HR 0.95, 95% CI 0.92–0.98), unipolar depression (HR 0.95, 95% CI 0.90–0.99), bipolar depression (HR 0.85, 95% CI 0.74–0.98), dementia (HR 0.82, 95% CI 0.76–0.88), delirium (HR 0.85, 95% CI 0.77–0.94), and non-schizophrenia psychosis (HR 0.89, 95% CI 0.83–0.96) disorders (bivariable Cox regression, Table 3).
Table 3:
Unadjusted Associations of Mental Illness With Endocrine Therapy Initiation, Discontinuation, Adherence
| Models | |||||||
|---|---|---|---|---|---|---|---|
| Initiation | aDiscontinuation | bAdherence | |||||
| Illness | Number with Illness | HR | p value | HR | p value | Estimate | p value |
| Any Mental Illness | 5,459 (24.9%) | 0.95 (0.92–0.98) | 0.01 | 1.19 (1.11–1.27) | <.001 | −0.006 (−0.012, 0.000) | 0.06 |
| Emotional Disorders: | |||||||
| Unipolar Depression | 2,418 (11.0%) | 0.95 (0.90–0.99) | 0.03 | 1.09 (1.00–1.20) | 0.06 | −0.006 (−0.015, 0.002) | 0.14 |
| Anxiety | 2,089 (9.5%) | 1.00 (0.95–1.05) | 0.87 | 1.24 (1.13–1.37) | <.001 | −0.004 (−0.013, 0.005) | 0.35 |
| Adjustment | 81 (0.4%) | 0.93 (0.72–1.19) | 0.56 | 1.42 (0.92–2.20) | 0.12 | −0.006 (−0.046, 0.034) | 0.76 |
| Cognitive Disorders: | |||||||
| Delirium | 515 (2.4%) | 0.85 (0.77–0.94) | 0.01 | 1.14 (0.92–1.40) | 0.23 | 0.009 (−0.009, 0.027) | 0.32 |
| Dementia | 1,017 (4.6%) | 0.82 (0.76–0.88) | <.001 | 1.10 (0.94–1.28) | 0.25 | 0.008 (−0.005, 0.021) | 0.20 |
| Personality | 59 (0.3%) | 0.77 (0.56–1.07) | 0.12 | 1.12 (0.61–2.09) | 0.71 | 0.011 (−0.040, 0.061) | 0.68 |
| Mania and Psychoses: | |||||||
| Bipolar Depression | 265 (1.2%) | 0.85 (0.74–0.98) | 0.02 | 0.95 (0.71–1.28) | 0.75 | −0.009 (−0.037, 0.019) | 0.06 |
| Schizophrenia | 185 (0.8%) | 0.99 (0.84–1.17) | 0.94 | 0.81 (0.56–1.18) | 0.28 | 0.035 (0.007, 0.062) | 0.01 |
| Non-Schizophrenia Psychosis | 1,004 (4.6%) | 0.89 (0.83–0.96) | 0.01 | 1.20 (1.04–1.37) | 0.01 | −0.001 (−0.013, 0.012) | 0.91 |
| Substance Use: | |||||||
| Drug use | 970 (4.4%) | 0.99 (0.92–1.06) | 0.69 | 1.40 (1.22–1.59) | <.001 | −0.023(−0.038,−0.009) | 0.002 |
| Alcohol use | 75 (0.3%) | 1.01 (0.78–1.31) | 0.96 | 1.71 (1.11–2.63) | 0.01 | −0.105 (−0.175,–0.034) | 0.004 |
Discontinuation analyzed for the first 5 years of endocrine therapy use.
Proportion Days Covered (PDC) adherence was calculated in 1-year intervals, concluding after the 5th year of follow-up, if available. Individuals with less than 1 year of follow-up did not contribute to adherence values. Year adherence values not included if patient spent greater than half of that year hospitalized or in skilled nursing facilities. Adherence estimate of 0.01 corresponds to 1% change.
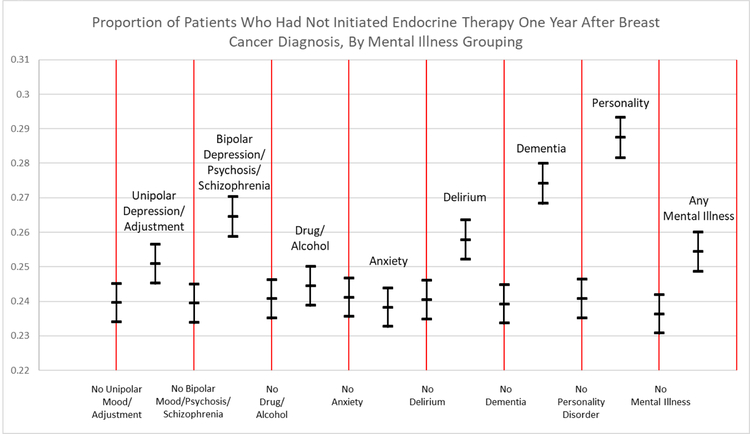
The best fit multivariable initiation model included the substance use disorder phenotype and subsets of the emotional (unipolar depression and adjustment disorder) and bipolar and psychoses (bipolar depression, non-schizophrenia psychotic, and schizophrenia disorder) phenotypes. Remaining disorders were included as individual variables. After multivariable adjustment, patients with dementia (HR 0.90, 95% CI 0.83–0.98) and bipolar and psychotic (HR 0.93, 95% CI 0.87–0.99) disorders were less likely to initiate treatment (Table 4). Higher initiation rates occurred with younger age, Asian race, more recent cancer diagnosis, and high cancer stage. In adjusted one-year landmark analyses, 3.5% more patients with dementia had not initiated therapy compared to those without dementia [0.274 (95% CI 0.268–0.280) vs 0.239 (95% CI 0.234–0.245)] (Figure 1). Patients with bipolar and psychoses were 2.5% more likely to have not initiated endocrine therapy [0.265 (95% CI 0.259–0.270) vs. 0.239 (95% CI 0.234–0.245)] (Figure 1).
Table 4:
Multivariable Analysis of Mental Illness Associated with Endocrine Therapy Initiation, Discontinuation, and Adherence
| Number with Illness | HR | HR | Estimate | ||
|---|---|---|---|---|---|
| cIntercept | - | - | - | 0.758 (0.748, 0.768) | |
| Emotional: | |||||
| Unipolar or Depression Adjustment Disorder | 2,473 (11.3%) | 0.97 (0.92–1.02) | 1.07 (0.92–1.13) | −0.007 (−0.016, 0.002) | |
| Anxiety | 2,089 (9.5%) | 1.01 (0.96–1.06) | **1.21 (1.09–1.34) | −0.003 (−0.012, 0.006) | |
| Cognitive: | |||||
| Delirium | 515 (2.4%) | 0.95 (0.85–1.06) | 1.04 (0.83–1.29) | 0.010 (−0.008, 0.029) | |
| Dementia | 1,017 (4.6%) | *0.90 (0.83–0.98) | 0.97 (0.83–1.15) | 0.011 (−0.002, 0.025) | |
| Personality | 59 (0.3%) | 0.87 (0.63–1.21) | 0.87 (0.46–1.63) | 0.017 (−0.031, 0.066) | |
| Substance Use (Alcohol, Drug) | 1,006 (4.6%) | 0.99 (0.92–1.06) | **1.43 (1.26–1.64) | **−0.023 (−0.037,–0.010) | |
| Bipolar and Psychoses (Bipolar Depression, Non-schizophrenia psychosis/Schizophrenia) | 1,259 (5.8%) | *0.93 (0.87–0.99) | 1.08 (0.94–1.24) | 0.004 (−0.008, 0.015) | |
| Stage at Diagnosis | |||||
| ref = 1 | 2 | **1.14 (1.10–1.18) | **0.80 (0.75–0.86) | 0.001 (−0.005, 0.006) | |
| 3 | 1.05 (0.99–1.11) | **0.72 (0.64–0.82) | *−0.012 (−0.023, –0.002) | ||
| 4 | **1.52 (1.31–1.76) | 1.19 (0.92–1.55) | *−0.049 (−0.080, –0.019) | ||
| Unknown | *0.86 (0.77–0.97) | 0.83 (0.66–1.04) | 0.001 (−0.018, 0.020) | ||
| Race | |||||
| ref = White | Asian | *1.09 (1.02–1.18) | *0.82 (0.71–0.96) | *0.012 (0.001, 0.023) | |
| Black | 0.96 (0.90–1.02) | **0.73 (0.63–0.84) | −0.009 (−0.020, 0.002) | ||
| Other | 0.98 (0.82–1.18) | 0.93 (0.63–1.38) | *–0.039 (−0.073, –0.005) | ||
| Ethnicity ref= Non-Hispanic | Hispanic | 1.00 (0.94–1.07) | *0.82 (0.71–0.94) | −0.003 (−0.014, 0.008) | |
| Age at Diagnosis | |||||
| ref= 68–74 | 75–84 | **0.92 (0.89–0.95) | **1.26 (1.18–1.34) | −0.002 (−0.008, 0.003) | |
| 85–94 | **0.65 (0.61–0.68) | **1.55 (1.41–1.71) | *0.012 (0.004, 0.021) | ||
| 95+ | **0.45 (0.34–0.60) | **2.61 (1.57–4.36) | −0.024 (−0.089, 0.041) | ||
| Adjusted NCI Comorbidity Score | 1.00 (0.99–1.01) | 1.00 (0.98–1.01) | 0.001 (−0.001, 0.002) | ||
| Year of Cancer Diagnosis | 2008 | 0.98 (0.92–1.05) | 0.95 (0.86–1.05) | 0.003 (−0.008, 0.014) | |
| ref= 2007 | 2009 | 1.01 (0.95–1.07) | *0.90 (0.81–1.00) | **0.024 (0.013, 0.034) | |
| 2010 | **1.11 (1.05–1.19) | *0.85 (0.76–0.95) | **0.059 (0.048, 0.070) | ||
| 2011 | **1.17 (1.09–1.24) | 0.90 (0.80–1.01) | **0.070 (0.060, 0.081) | ||
| 2012 | **1.15 (1.08–1.23) | 0.91 (0.80–1.03) | **0.086 (0.075, 0.096) | ||
| 2013 | **1.19 (1.12–1.27) | 0.92 (0.81–1.06) | **0.084 (0.072, 0.095) | ||
| cYear of Endocrine Therapy Use | 2 | - | - | **0.066 (0.062, 0.070) | |
| ref = 1 | 3 | - | - | **0.088 (0.084, 0.093) | |
| 4 | - | - | **0.118 (0.112, 0.124) | ||
| 5 | - | - | **0.130 (0.122, 0.138) | ||
<0.05,
<0.001, 95% confidence interval.
Discontinuation analyzed for the first 5 years of endocrine therapy use.
Proportion Days Covered (PDC) adherence was calculated in 1-year intervals, concluding after the 5th year of follow-up, if available. Individuals with less than 1 year of follow-up did not contribute to adherence values. Year adherence values not included if patient spent greater than half of that year hospitalized or in skilled nursing facilities. Adherence estimate of 0.01 corresponds to 1% change.
Intercept, year only apply to linear adherence model.
Fig. 1.
Direct adjusted rates (endocrine therapy non-initiation) at year 1 of follow-up were calculated from final multivariable initiation Cox model, with 95% confidence interval, including adjustments for stage, age, year of diagnosis, race, ethnicity, and 3-year NCI modified comorbidity index
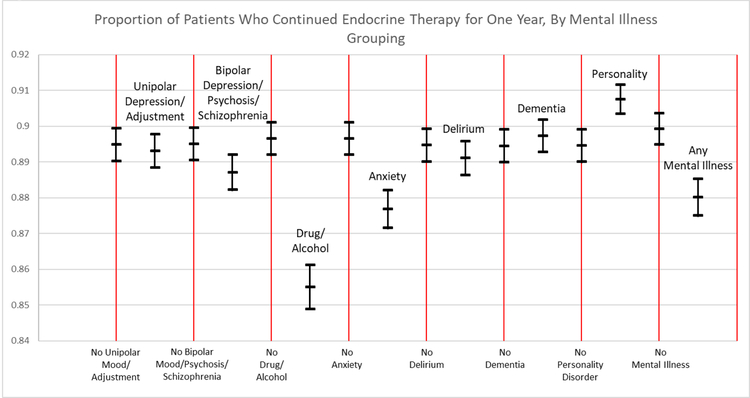
Discontinuation was more common in patients with “any mental illness” (HR 1.19, 95% CI 1.11–1.27), anxiety (HR 1.24, 95% CI 1.13–1.37), non-schizophrenia psychotic (HR 1.20, 95% CI 1.04–1.37), drug use (HR 1.40, 95% CI 1.22–1.59), and alcohol use disorders (HR 1.71, 95% CI 1.11–2.63) (bivariable Cox regression, Table 3). After multivariable adjustment, patients with anxiety (HR 1.21, 95% CI 1.09–1.34) and substance use (HR 1.43, 95% CI 1.26–1.64) disorders were more likely to discontinue (Table 4). Younger, Black, Asian, and Hispanic patients were less likely to discontinue, as were patients with stage II and III disease, compared to I (Table 4). In adjusted one-year landmark analyses, 4.1% fewer patients with substance use disorders [0.855 (95% CI 0.849–0.861) vs 0.896 (95% CI 0.892–0.901)] and 2.1% fewer patients with anxiety disorders [0.877 (95% CI 0.871–0.882) vs 0.896 (95% CI 0.892–0.901)] had continued endocrine therapy, compared to those without the condition (Figure 2).
Fig. 2.
Direct adjusted rates (continuous endocrine therapy use) at year 1 of follow-up were calculated from final multivariable discontinuation Cox model, with 95% confidence interval, including adjustments for stage, age, year of diagnosis, race, ethnicity, and 3-year NCI modified comorbidity index
Mean adherence was lower in patients with drug use (estimated mean difference −2.3%, 95% CI −3.8,−0.9), alcohol use (−10.5%, 95% CI −17.5,−3.4) disorders (bivariable linear regression, Table 3). Adherence rates were slightly elevated in patients with schizophrenia (+3.5%, 95% CI 0.7, 6.2). After multivariable adjustment, the only mental illnesses associated with adherence were substance use disorders, with 2.3% worse adherence (Table 4). Compared to younger patients, those aged 85–94 at diagnosis had 1.2% greater adherence. Asian patients had 1.2% greater adherence than White patients, and “other” races saw a 3.9% reduction. Adherence decreased with advancing stage (stage III −1.2%; stage IV −4.9%). Patients more recently diagnosed with cancer had higher adherence rates (+8.4% 2013 vs 2007). With each consecutive year of use, adherence improved (year 2 +6.6%; year 3 +8.8%; year 4 +11.8%; year 5 +13.0%).
Discussion
In this large, nationally representative cohort of older women with ER+ stage I-IV breast cancer, preexisting mental illness was common. Mental illness modestly reduced endocrine therapy initiation, adherence, and discontinuation rates, but no single disorder affected all three. One-fifth of women never initiated treatment, and patients with dementia and bipolar and psychotic disorders were at additional risk of non-initiation. Of initiators, 25.7% discontinued prior to five years of use, with anxiety and substance use significantly associated with increasing discontinuation risk. Overall adjusted adherence rates among active continuous users (mean 84%) exceeded a commonly referenced 80% minimum threshold, but a 2.1% reduction was seen in patients with substance use disorders. These at-risk subgroups may be explored further to identify actionable interventions.
Treatment Initiation
Endocrine therapy is recommended for all patients with ER+ breast cancer, but we observed that 20% of women did not receive any, worsening recurrence and mortality risk [1, 5]. Patients with dementia or bipolar and psychotic disorders less frequently initiated endocrine therapy. We expected dementia symptoms to complicate health behaviors, as reduced independence may negatively impact medication adherence [25]. Also, patients with dementia often have substantial comorbidity, potentially making endocrine therapy a lesser priority in the face of other burdens [26]. Bipolar and psychotic disorder symptoms can greatly disrupt daily life [27]. This population often struggles with general medication adherence [28].
While endocrine therapy initiation is likely affected by dependence or disability, significant comorbidity, and debilitating symptoms, provider decision-making affects whether a prescription is recommended and filled. Patients with mental illness are at known risk to receive worse quality of general medical care [29]. However, we saw comparable initiation rates among those with and without most mental illnesses, suggesting provider knowledge of patient mental illness may not strongly affect whether endocrine therapies are prescribed.
Non-adherence
Endocrine therapy adherence was reduced in patients with substance use disorders. The use of mind-altering substances can result in impairment and social isolation, and often co-occurs with additional psychiatric illness [30]. While tobacco use may not reflect the broader neuropsychiatric disturbances seen with opioids or alcohol, smoking is associated with mental illness and social disparities [31]. Patients with substance use disorders may have pervasive disruption in life and social stability, resulting in an inability to maintain long-term medication use.
We found no association of unipolar depression with adherence after multivariable adjustment. Previous research suggested depression decreases adherence. However, these studies included a heterogeneous set of cohorts and measures with only one using ICD-9 diagnosis codes [8]. In our cohort, continuous Medicare Part D coverage may have improved access to medication and enabled adherence. While mental illness contributes to diagnostic and primary treatment delays, it appears that most patients who initiate endocrine therapies adhere as well as the general population [9]. Timely diagnosis and receipt of primary breast cancer treatment may be key to improving morbidity and mortality rates in patients with mental illness.
Discontinuation
Discontinuation of endocrine therapy was more common in patients with anxiety or substance use disorders. As discussed above, the disruptions seen in substance use disorders are likely to destabilize health behaviors, increasing discontinuation. Anxiety disorders can include “persistent, excessive, and/or unrealistic worry”, phobias, and panic attacks [32]. While some physiologic anxiety may be motivating, chronic pathologic anxiety can impair decision making and promote avoidance behaviors [33]. Overwhelming anxiety could distract from breast cancer treatment, which may precipitate discontinuation. Long-term patient-provider relationships may help improve health behaviors, reduce anxiety, and thus increase continuous endocrine therapy use.
Other Patient Characteristics
Patients diagnosed with stage IV cancer were more likely to initiate but had lower adherence rates among continued users. Initiation and discontinuation may be more influenced by provider factors and benefit-to-risk perception than is daily medication taking, which may be susceptible to treatment and disease burdens that increase with advancing stage. Older age was associated with lower initiation rates, consistent with other reports [4]. Older women may prioritize immediate quality of life over future recurrence potential when treatment lasts five years and can cause physical side effects [4, 34, 35]. Finally, Asian race and recent year of cancer diagnosis were often associated with increased endocrine therapy use. However, these effects should not be assumed causal as these variables were introduced to control for potential unmeasured confounding and were not the focus of analysis.
Study Strengths and Potential Limitations
Strengths of the study include the nationally representative cohort with a large sample size sufficient to examine low prevalence illnesses and finer adherence metrics. While adherence can be examined as a dichotomous (≥0.80) outcome, continuous PDC captures lost detail. Changes in adherence below the 80% adherence threshold may be clinically significant; incremental decreases may affect mortality [5].
Potential limitations include generalizability and limits of claims data measurements. Although the median age at breast cancer diagnosis is 62 years, close to the age of Medicare enrollment, 65 years, results from Medicare patients may not generalize to younger, privately or uninsured women [11]. We did not have a reliable measure of cancer recurrence, which may contribute to treatment discontinuation. Mental illness diagnoses are not always captured accurately in claims data. For example, substance abuse is often underdiagnosed [36]. Cultural beliefs and behaviors may affect mental illness diagnosis, contributing to measurement bias [37]. Patients with undiagnosed mental illness may less frequently utilize healthcare, possibly due to severe symptoms, which may contribute to non-adherence. Medicare Part D claims also do not assure medication was taken as directed after acquisition. Adherence calculations may be improved with follow-up surveys, diaries, or electronic measurement tools. However, we used accepted claims-based adherence measures, and adjustments for medication overfill, class switching, and time hospitalized [19].
We found that patients with mental illness had less available follow-up and were more frequently censored at death, consistent with prior evidence that Medicare enrolled women with breast cancer and severe mental illness had higher rates of all-cause mortality [10]. While patients with mental illness in our study were on average diagnosed with later stages and greater comorbidity, we still saw statistically significant effects for certain mental illnesses after adjustment. Finally, mechanisms for mental illness effects are not identified in these data and could be due to behavioral symptoms, differential experience of side effects, physician judgement, or access to care.
Conclusions
Even though endocrine therapy adherence is important for breast cancer survival, 20.0% of female Medicare beneficiaries never initiated, and 25.7% of users discontinued treatment prior to five years of use. Nearly one-quarter of Medicare patients with breast cancer had diagnosed mental illness preceding breast cancer. While prior studies suggest mental illness contributes to diagnostic and primary treatment delays, we saw modest impacts on whether endocrine therapy was initiated, adhered to, or discontinued. This study identifies potential groups at-risk for non-adherence, and future work should explore risk factors which disproportionately affect vulnerable patients, as well as actionable interventions.
Acknowledgements
This work was supported by the University of Iowa Holden Comprehensive Cancer Center Population Research Core (P30 CA086862), and the University of Iowa Medical Scientist Training Program (T32 GM007337). This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the National Cancer Institute; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database. The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement # U58DP003862–01 awarded to the California Department of Public Health. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California Department of Public Health, the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred. The authors acknowledge the efforts of the National Cancer Institute; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database.
Footnotes
Conflict of Interest Disclosures
Mr. Haskins, and Drs. McDowell, Carnahan, Wallace, Smith, and Chrischilles have no disclosures or conflict of interest to report. Dr. Fiedorowicz reports a consultation role with Myriad Genetics, Inc. (consultation for mood disorder proteomics study), as well as research funding from Myriad Genetics, Inc. (not applied to this work).
Data Availability
The SEER-Medicare data supporting the findings of this study are available from the National Cancer Institute but restrictions apply to the availability for these data, which were under license for the study, and are not available without approval. Data are available from the authors upon reasonable request and with permission of the National Cancer Institute.
Ethical Standards
This study did not involve any direct human interventions. All research and analysis was performed in compliance with the current University of Iowa IRB regulations and laws of the United States.
References
- 1.Davies C, et al. , Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet, 2013. 381(9869): p. 805–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Partridge AH, et al. , Nonadherence to adjuvant tamoxifen therapy in women with primary breast cancer. J Clin Oncol, 2003. 21(4): p. 602–6. [DOI] [PubMed] [Google Scholar]
- 3.Hershman DL, et al. , Early discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of8,769 early-stage breast cancer patients. J Clin Oncol, 2010. 28(27): p. 4120–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doggrell SA et al. (2011) Adherence to oral endocrine treatments in women with breast cancer: can it be improved? Breast Cancer Res Treat 129(2):299–308 [DOI] [PubMed] [Google Scholar]
- 5.Hershman DL, et al. , Early discontinuation and non-adherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancer. Breast Cancer Res Treat, 2011. 126(2): p. 529–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hadji P et al. (2010) Improving compliance and persistence to adjuvant tamoxifen and aromatase inhibitor therapy. Crit Rev Oncol Hematol 73(2):156–166 [DOI] [PubMed] [Google Scholar]
- 7.Land SR, et al. , Symptoms and QOL as Predictors of Chemoprevention Adherence in NRG Oncology/NSABP Trial P-1. J Natl Cancer Inst, 2016. 108(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mausbach BT et al. (2015) Depression as a predictor of adherence to adjuvant endocrine therapy (AET) in women with breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat 152(2):239–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iglay K, et al. , Diagnosis and treatment delays among elderly breast cancer patients with pre-existing mental illness. Breast cancer research and treatment, 2017. 166(1): p. 267–275. [DOI] [PubMed] [Google Scholar]
- 10.Iglay K, et al. , Impact of preexisting mental illness on all-cause and breast cancer- specific mortality in elderly patients with breast cancer. Journal of Clinical Oncology, 2017. 35(36): p. 4012–4018. [DOI] [PubMed] [Google Scholar]
- 11.Howlader N at al (2017) SEER cancer statistics review, 1975–2014. National Cancer Institute, Rockville [Google Scholar]
- 12.NIH. SEER-Medicare: SEER Program & Data. NIH Healthcare Delivery Research Program 2018; Available from: https://healthcaredelivery.cancer.gov/seermedicare/aboutdata/program.html.. [Google Scholar]
- 13.NIH. SEER-Medicare: Medicare Claims Files. NIH Healthcare Delivery Research Program 2018; Available from: https://healthcaredelivery.cancer.gov/seermedicare/medicare/claims.html#partd. [Google Scholar]
- 14.NIH. Breast Schema for 1988+ based on AJCC 6th edition. NIH Surveillance, Epidemiology, and End Results Program 2018; Available from: https://seer.cancer.gov/seerstat/variables/seer/ajcc-stage/6th/breast.html. [Google Scholar]
- 15.NIH. NCI Comorbidity Index Overview. NIH Healthcare Delivery Research Program 2018; Available from: https://healthcaredelivery.cancer.gov/seermedicare/considerations/comorbidity.html. [Google Scholar]
- 16.American Psychiatric Association (1994) Diagnostic and statistical manual IV. ed. American Psychiatric Association, Washington DC [Google Scholar]
- 17.Tajeu GS, et al. , Trends in Antihypertensive Medication Discontinuation and Low Adherence Among Medicare Beneficiaries Initiating Treatment From 2007 to 2012. Hypertension, 2016. 68(3): p. 565–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burstein HJ, et al. , Adjuvant endocrine therapy for women with hormone receptor- positive breast cancer: american society of clinical oncology clinical practice guideline focused update. J Clin Oncol, 2014. 32(21): p. 2255–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hess LM, et al. , Measurement of adherence in pharmacy administrative databases: a proposal for standard definitions and preferred measures. Ann Pharmacother, 2006. 40(7–8): p. 1280–88. [DOI] [PubMed] [Google Scholar]
- 20.Chang A et al. (2015) A SAS Macro to Calculate the PDC Adjustment of Inpatient Stays. SAS Global Forum Proceedings 2015. Paper 3560
- 21.NIH. SEER-Medicare: Calculation of Comorbidity Weights. NIH Healthcare Delivery Research Program 2018; Available from: https://healthcaredelivery.cancer.gov/seermedicare/considerations/calculation.html. [Google Scholar]
- 22.Akaike H, Likelihood of a Model and Information Criteria. Journal of Econometrics, 1981. 16. [Google Scholar]
- 23.Zhang X, et al. , A SAS macro for estimation of direct adjusted survival curves based on a stratified Cox regression model (vol 88, pg 95, 2007) Computer Methods and Programs in Biomedicine, 2008. 89(3): p. 313–314. [DOI] [PubMed] [Google Scholar]
- 24.Pan W, Akaike’s information criterion in generalized estimating equations. Biometrics, 2001. 57(1): p. 120–5. [DOI] [PubMed] [Google Scholar]
- 25.Insel KC et al. (2006) The negative association of independent personality and medication adherence. J Aging Health 18(3):407–418 [DOI] [PubMed] [Google Scholar]
- 26.Arlt S, et al. , Adherence to medication in patients with dementia: predictors and strategies for improvement. Drugs Aging, 2008. 25(12): p. 1033–47. [DOI] [PubMed] [Google Scholar]
- 27.Reus VI, Mental Disorders, in Harrison’s Principles of Internal Medicine, 19e, Kasper D, et al. , Editors. 2015, McGraw-Hill Education: New York, NY. [Google Scholar]
- 28.Lingam R and Scott J, Treatment non-adherence in affective disorders. Acta Psychiatr Scand, 2002. 105(3): p. 164–72. [DOI] [PubMed] [Google Scholar]
- 29.De Hert M, et al. , Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry, 2011. 10(2): p. 138–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cruz ES et al. (2014), Medical rehabilitation—substance abuse, in current diagnosis and treatment: physical medicine and rehabilitation. McGraw-Hill, New York [Google Scholar]
- 31.Leonard S, et al. , Smoking and mental illness. Pharmacol Biochem Behav, 2001. 70(4): p. 561–70. [DOI] [PubMed] [Google Scholar]
- 32.Reus VI, Psychiatric Disorders, in Harrison’s Principles of Internal Medicine, 20e, Jameson JL, et al. , Editors. 2017, McGraw-Hill Education: New York, NY. [Google Scholar]
- 33.Marion D, Psychological factors affecting other medical conditions: Clinical features, assessment, and diagnosis, in UpToDate; 2017: Waltham, MA. [Google Scholar]
- 34.Hudani ZK and Rojas-Fernandez CH, A scoping review on medication adherence in older patients with cognitive impairment or dementia. Res Social Adm Pharm, 2016. 12(6): p. 815–829. [DOI] [PubMed] [Google Scholar]
- 35.Rizzuto D, et al. , Personality and Survival in Older Age: The Role ofLifestyle Behaviors and Health Status. Am J Geriatr Psychiatry, 2017. 25(12): p. 1363–1372. [DOI] [PubMed] [Google Scholar]
- 36.American College of Obstetricians and Gynecologists. (2015). Committee Opinion No. 633: Alcohol abuse and other substance use disorders: ethical issues in obstetric and gynecologic practice. Obstet Gynecol, 125(6), 1529–1537. [DOI] [PubMed] [Google Scholar]
- 37.Chapter 2: Culture counts: The influence of culture and society on mental health US Department of Health & Human Services; Mental Health: Culture, Race, Ethnicity—A Supplement to Mental health: A Report of the Surgeon General. 2001. [Google Scholar]