Abstract
This retrospective study analyzed the effectiveness of neuromuscular electrical stimulation (NMES) for pain relief caused by necrosis of femoral head (NFH).
Totally, 80 cases of patients with NFH were analyzed and then were assigned to a treatment group or a control group in this study. Of these, 40 cases in the treatment group received ibuprofen and NMES therapy. The other 40 cases in the control group received ibuprofen alone. Cases in both groups were treated for a total of 6 weeks. The primary outcome of pain intensity was measured by a visual analog scale (VAS). The secondary outcome was assessed by Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). In addition, adverse events (AEs) were also recorded in each case. All outcomes were evaluated before and after the treatment.
After treatment, patients in the treatment group showed more effectiveness in pain relief, as measured by VAS (P < .01) and WOMAC sub-pain scale (P < .01), except stiffness, as evaluated by WOMAC sub-stiffness scale (P = .07), and function, as assessed by WOMAC sub-function scale (P = .09), than patients in the control group. Additionally, no significant differences in AEs were detected between 2 groups.
This study found that NMES may be helpful for pain relief in patients with NFH.
Keywords: effectiveness, femoral head, neuromuscular electrical stimulation, pain, retrospective study
1. Introduction
Necrosis of femoral head (NFH) is one of the most common progressive orthopedic disorders.[1–4] It has been reported that about 20,000 people can affect this disorder every year in USA.[5–7] It occurs at any age, especially in patients of 30 to 50 years old.[8] It can cause subchondral collapse initially, and then secondary osteoarthritis as the disease progresses.[9] This condition can result in complete destruction of the hip if left untreated.[10]
A variety of management options are available for the treatment of this condition.[11–18] These options include medications, surgical treatments, and other alternative interventions, such as Chinese herbal medicine, acupuncture, rest, extracorporeal shock wave therapy, and electrical stimulation.[11–18] However, these options still suffer from limited efficacy, and even very server adverse events (AEs) and complications. Thus, alternative candidates with few AEs are urgently needed to treat this condition.
Neuromuscular electrical stimulation (NMES) is a very powerful candidate for lots of pain conditions treatment, such as patellofemoral pain syndrome, shoulder pain, neck pain, endometriosis-associated pain, and neuropathic pain caused by spinal cord injury.[19–24] All of these studies reported to achieve promising outcome results. However, no study specifically investigated the effectiveness of NMES for the treatment of pain condition from NFH. Thus, in this retrospective study, we first explored the potential effectiveness of NMES therapy for pain relief in patients with NFH.
2. Methods and design
2.1. Ethical consideration
This study has been approved by the Ethical Committee of the First Affiliated Hospital of Jiamusi University. The informed written consent was waived from this study because all the data were selected from the completed medical records of eligible cases.
2.2. Design
The cases were collected from March 2016 to January 2018 at the First Affiliated Hospital of Jiamusi University. A total of 80 eligible cases with NFH were included in this study. Of them, 40 cases received ibuprofen plus NMES therapy and were assigned to a treatment group, while the other 40 cases received ibuprofen alone, and were assigned to a control group. The cases in both groups were treated for a total of 6 weeks. All outcomes were assessed before and after 6-week treatment in this study.
2.3. Cases selection
This study analyzed 80 eligible patient cases with NFH. All included cases had confirmed the diagnosis of NFH by plain radiography, computed tomography, or magnetic resonance imaging, and other examinations. All cases were reported to have disease duration of more than 2 years.
The cases were excluded if NFH caused by tuberculosis, infection, or a tumor; or cases also had other comorbidities, such as diabetes, hyperthyroidism, pregnancy, breastfeeding, severe organs diseases, coagulation disorders, cardiac pacemakers, and insufficient patient information; or received other therapies, such as electroacupuncture during the treatment period.
2.4. Treatment
All cases in both groups received ibuprofen 400 mg, every 6 hours, 4 times daily for a total of 6 weeks. In addition, subjects in the treatment group also received NMES therapy. It was applied by NMES stimulator (Globus ACTIVA 600 Pro, Globus, Italy). The 2 electrode pads were placed around the worst pain point of the femoral head for 30 minutes each session, with 50 Hz frequency, 250 μs pulse duration, and 10 seconds on and 30 seconds off. It was treated 3 times weekly for a total of 6 weeks.
2.5. Outcome measurement
The primary outcome was pain intensity. It was assessed by a 10-point visual analog scale (VAS).[25] The secondary outcome was measured by the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC).[26] In addition, any AEs were also documented. All outcomes were evaluated before and after the treatment.
2.6. Statistical analysis
All outcome and characteristic data were analyzed by the SPSS Statistics 17.0 (IBM Corp, Armonk, NY). All the continuous data were analyzed by t test or Mann–Whitney U test. All the categorical data were analyzed by Pearson chi-square or Fisher exact test. The value of P < .05 was set as having statistical significance.
3. Results
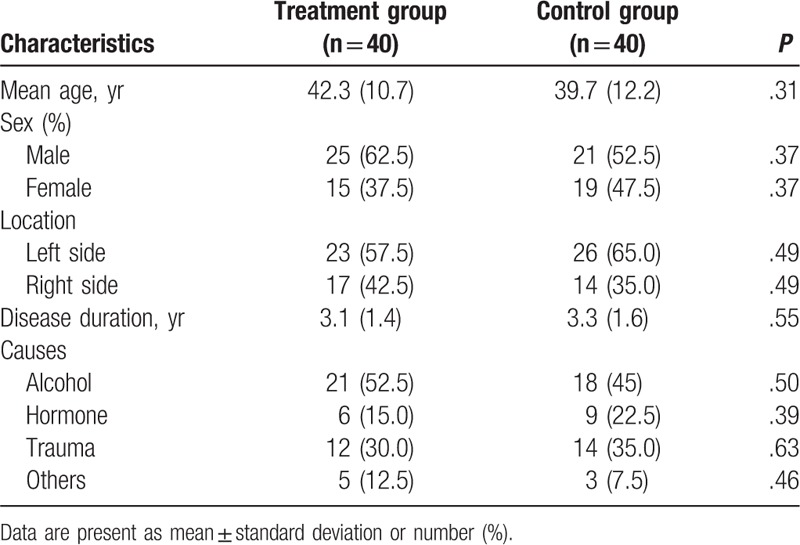
The characteristics of all included cases are summarized in Table 1. There were no significant differences in all these characteristics between 2 groups in this study (Table 1).
Table 1.
Characteristics of included patient cases.
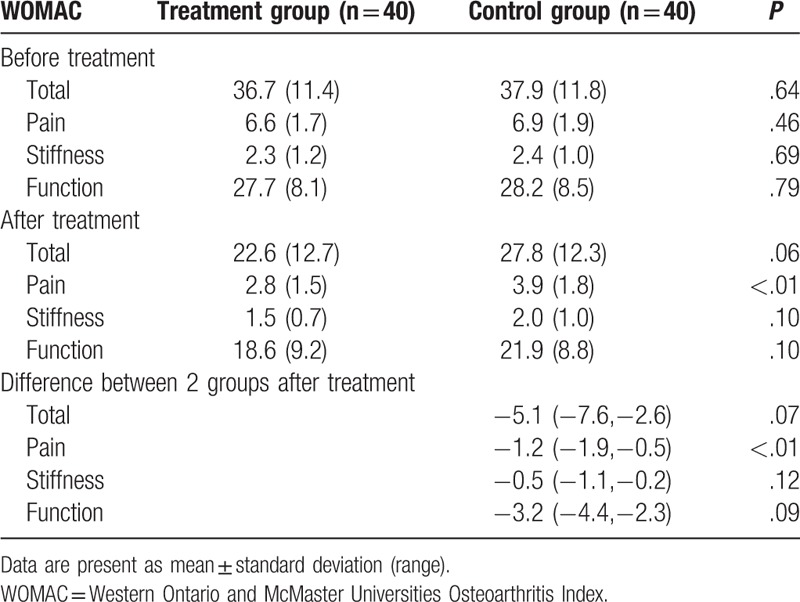
After treatment, patients who received ibuprofen and NMES therapy showed more significant effectiveness in pain relief, as measured by VAS (P < .01, Table 2), and WOMAC sub-pain scale (P < .01, Table 3), than patients who received ibuprofen alone. However, patients in the treatment group did not show better outcome in stiffness, as evaluated by WOMAC sub-stiffness scale (P = .07, Table 3), and function, as assessed by WOMAC sub-function scale (P = .09, Table 3).
Table 2.
Comparison of primary outcome between 2 groups.
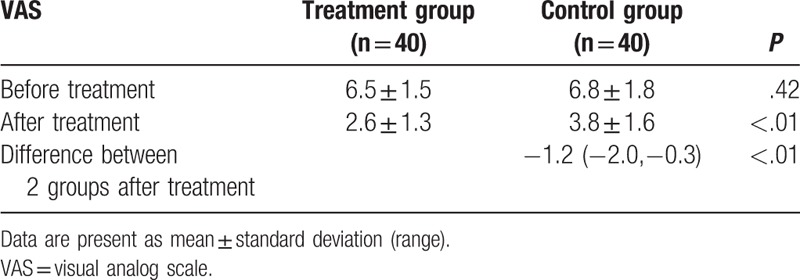
Table 3.
Comparison of secondary outcome between 2 groups.
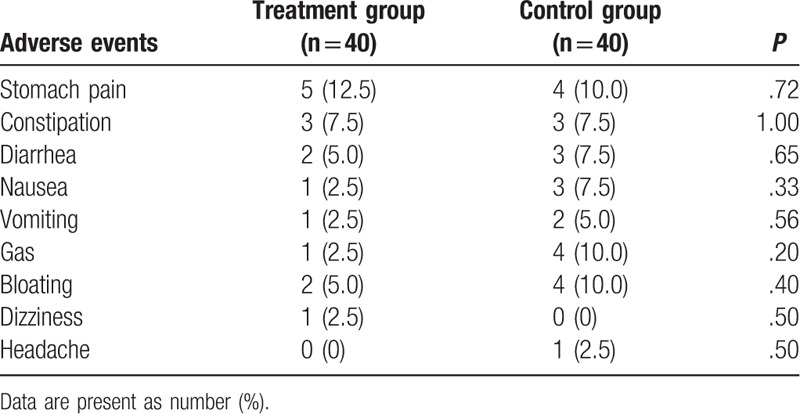
After treatment, mild AEs were recorded in either group (Table 4). No significant differences in all AEs were found between 2 groups (Table 4). Although several AEs were documented, all of them may result from ibuprofen, but not from the NMES.
Table 4.
Comparison of adverse events between 2 groups.
4. Discussion
Previous study has reported that electrical stimulation can be used to treat a variety of pain conditions, especially for NMES.[18–24] However, few studies focused on using electrical stimulation to treat patients with NFH. As far as we know, no study has explored the effectiveness of NMES for the treatment of NFH.
The present study is the first study to investigate the effectiveness of NMES for the treatment of patients with NFH. Moreover, it has achieved satisfied results. Although it first explored this issue, its results may provide very helpful evidence for pain relief in patients with NFH, as well as further studies.
The results of the present study exerted better outcome in pain relief, as assessed by both the VAS scale, and the WOMAC sub-pain scale. However, no significant differences in stiffness, as measured by WOMAC sub-stiffness scale, and function, as evaluated by WOMAC sub-function scale differed between 2 groups. The present results indicated that NMES may benefit for pain relief in patients with NFH, but may not for the stiffness and function.
The present study has the following limitations:
-
(1)
the treatment duration is quite short with only 6 weeks, which may affect effectiveness of NMES for patients with NFH;
-
(2)
the outcomes were not comprehensive, because it only assessed pain condition, as well as function and stiffness of the attacked joints. More outcomes were short of this study, such as quality of life assessment, because all data collected from completed medical cases in this retrospective study;
-
(3)
no randomization procedure was applied in this study, which may result in high risk of case selection in the present study.
5. Conclusion
The findings of this study showed that NMES may benefit for pain relief in patients with NFH after 6 weeks treatment.
Author contributions
Conceptualization: Qing-Hui Ji, Xiao-Feng Qiao, Shou-Feng Wang, Peng Zhao, Shi-Chen Liu, Yu Xue, Jian-Min Qiao, Yan-Bao Li.
Data curation: Qing-Hui Ji, Xiao-Feng Qiao, Shou-Feng Wang, Peng Zhao, Shi-Chen Liu, Yu Xue, Jian-Min Qiao.
Funding acquisition: Qing-Hui Ji, Yan-Bao Li.
Investigation: Shou-Feng Wang.
Methodology: Qing-Hui Ji, Jian-Min Qiao.
Project administration: Xiao-Feng Qiao, Peng Zhao, Yan-Bao Li.
Resources: Qing-Hui Ji, Xiao-Feng Qiao, Peng Zhao, Yu Xue, Jian-Min Qiao, Yan-Bao Li.
Software: Shou-Feng Wang, Jian-Min Qiao.
Supervision: Qing-Hui Ji, Shi-Chen Liu, Yan-Bao Li.
Validation: Qing-Hui Ji, Xiao-Feng Qiao, Shou-Feng Wang, Shi-Chen Liu, Yu Xue, Yan-Bao Li.
Visualization: Qing-Hui Ji, Xiao-Feng Qiao, Shou-Feng Wang, Shi-Chen Liu, Yu Xue, Yan-Bao Li.
Writing – original draft: Qing-Hui Ji, Xiao-Feng Qiao, Shou-Feng Wang, Peng Zhao, Shi-Chen Liu, Yu Xue, Jian-Min Qiao, Yan-Bao Li.
Writing – review and editing: Qing-Hui Ji, Xiao-Feng Qiao, Shou-Feng Wang, Peng Zhao, Shi-Chen Liu, Yu Xue, Jian-Min Qiao, Yan-Bao Li.
Footnotes
Abbreviations: AEs = adverse events; NFH = necrosis of the femoral head; NMES = neuromuscular electrical stimulation; VAS = visual analog scale; WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
X-FQ and Q-HJ contributed equally to this study.
This study was partly supported by the Heilongjiang Province's basic scientific research business fund research project (2017-KYYWF-0574); and Jiamusi University Science and Technology Key Project (12Z1201508, 12Z1201507).
The authors have no conflicts of interest to disclose.
References
- [1].Andriolo L, Merli G, Tobar C, et al. Regenerative therapies increase survivorship of avascular necrosis of the femoral head: a systematic review and meta-analysis. Int Orthop 2018;42:1689–704. [DOI] [PubMed] [Google Scholar]
- [2].Venkatadass K, Avinash M, Rajasekaran S. Bilateral avascular necrosis of the femoral head following asynchronous postictal femoral neck fractures: a case report and review of the literature. J Pediatr Orthop B 2018;27:274–8. [DOI] [PubMed] [Google Scholar]
- [3].Guerado E, Caso E. The physiopathology of avascular necrosis of the femoral head: an update. Injury 2016;47suppl 6:S16–26. [DOI] [PubMed] [Google Scholar]
- [4].Barquet A, Mayora G, Guimaraes JM, et al. Avascular necrosis of the femoral head following trochanteric fractures in adults: a systematic review. Injury 2014;45:1848–58. [DOI] [PubMed] [Google Scholar]
- [5].Aaron RK. Treatment of osteonecrosis of the femoral head with electrical stimulation. Instr Course Lect 1994;43:495–8. [PubMed] [Google Scholar]
- [6].Massari L, Fini M, Cadossi R, et al. Biophysical stimulation with pulsed electromagnetic fields in osteonecrosis of the femoral head. J Bone Joint Surg Am 2006;88suppl 3:56–60. [DOI] [PubMed] [Google Scholar]
- [7].Cebrian JL, Milano GL, Francis A, et al. Role of electromagnetic stimulation in the treatment of osteonecrosis of the femoral head in early stages. J Biomed Sci Eng 2014;7:252–7. [Google Scholar]
- [8].MacNeil JA, Francis A, El-Hawary R. A systematic review of rigid, locked, intramedullary nail insertion sites and avascular necrosis of the femoral head in the skeletally immature. J Pediatr Orthop 2011;31:377–80. [DOI] [PubMed] [Google Scholar]
- [9].Gómez-García F. Review of non-surgical treatment of avascular necrosis of the femoral head. Acta Ortop Mex 2013;27:265–72. [PubMed] [Google Scholar]
- [10].Gregory K, Carl A, Jonathan P. Osteonecrosis of the femoral head. Orthopedic surgery board review manual. Orthop Surg 2013;8:1–21. [Google Scholar]
- [11].Abbas-Zadeh MR, Azizi A, Abbas-Zadeh L, et al. Effect of surgical treatment on the quality of life in patients with non-traumatic avascular ecrosis of the femoral head. Rev Bras Ortop 2018;53:773–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Agarwala S, Banavali SD, Vijayvargiya M. Bisphosphonate combination therapy in the management of postchemotherapy avascular necrosis of the femoral head in adolescents and young adults: a retrospective study from India. J Glob Oncol 2018;1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Landgraeber S, Warwas S, Claßen T, et al. Modifications to advanced core decompression for treatment of avascular necrosis of the femoral head. BMC Musculoskelet Disord 2017;18:479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chen Y, Huang K, Lang F, et al. Experimental study on cheng zai wan for treatment of necrosis of the femoral head. J Tradit Chin Med 2003;23:292–8. [PubMed] [Google Scholar]
- [15].Jafarian AA, Farhoodi A, Momeni M, et al. Clinical and radiographic alterations in bilateral avascular necrosis of the femoral head following laser acupuncture: a case report. J Lasers Med Sci 2018;9:149–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Calori GM, Mazza E, Colombo A, et al. Core decompression and biotechnologies in the treatment of avascular necrosis of the femoral head. EFORT Open Rev 2017;2:41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Han Y, Lee JK, Lee BY, et al. Effectiveness of lower energy density extracorporeal shock wave therapy in the early stage of avascular necrosis of the femoral head. Ann Rehabil Med 2016;40:871–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Al-Jabri T, Tan JYQ, Tong GY, et al. The role of electrical stimulation in the management of avascular necrosis of the femoral head in adults: a systematic review. BMC Musculoskelet Disord 2017;18:319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Martimbianco ALC, Torloni MR, Andriolo BN, et al. Neuromuscular electrical stimulation (NMES) for patellofemoral pain syndrome. Cochrane Database Syst Rev 2017;12: CD011289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Zhou M, Li F, Lu W, et al. Efficiency of neuromuscular electrical stimulation and transcutaneous nerve stimulation on hemiplegic shoulder pain: a randomized controlled trial. Arch Phys Med Rehabil 2018;99:1730–9. [DOI] [PubMed] [Google Scholar]
- [21].Miao Q, Qiang JH, Jin YL. Effectiveness of percutaneous neuromuscular electrical stimulation for neck pain relief in patients with cervical spondylosis. Medicine (Baltimore) 2018;97:e11080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bi XL, Xie CX. Effect of neuromuscular electrical stimulation for endometriosis-associated pain: a retrospective study. Medicine (Baltimore) 2018;97:e11266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Li YP, Cui X, Liu SC, et al. Neuromuscular electrical stimulation for treating postpartum low back pain. Medicine (Baltimore) 2018;97:e11426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Chen FC, Shao HL, Han FL. A pilot study of neuromuscular electrical stimulation for neuropathic pain caused by spinal cord injury. Medicine (Baltimore) 2018;97:e11658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Bird SB, Dickson EW. Clinically significant changes in pain along the visual analog scale. Ann Emerg Med 2001;38:639–43. [DOI] [PubMed] [Google Scholar]
- [26].Jinks C, Jordan K, Croft P. Measuring the population impact of knee pain and disability with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Pain 2002;100:55–64. [DOI] [PubMed] [Google Scholar]


