Abstract
Rationale:
Spinal metastases are always associated with specific pain of back and limbs caused by nerve root compression. Although percutaneous endoscopic lumbar discectomy (PELD) has been widely performed on patients with back and radicular pain originating from lumbar disc herniation, this minimally invasive surgery is rarely used for the treatment of spinal metastases.
Patient concerns:
A 71-year-old woman with colon cancer and a known L3 vertebral body metastasis presented with significant progressive pain of low back and limbs.
Diagnoses:
Magnetic resonance imaging (MRI) showed the L3 vertebral body had been involved by osteolytic vertebral metastasis, which extended into spinal canal and compressed the dural sac and nerve root.
Interventions:
The patient was treated with percutaneous transforaminal endoscopic decompression and palliative resection of metastases was performed twice on both sides, respectively. After the minimally invasive procedure, the decompression of the dural sac and nerve root was ideal.
Outcomes:
No complications during the procedure were reported. The minimally invasive surgery resulted in prompt and permanent pain relief until the patient died 6 months later.
Lessons:
Percutaneous transforaminal endoscopic decompression could be an appropriate treatment option for the patients who suffer neurologic deficits that result from the spinal metastases.
Keywords: minimally invasive surgery, nerve root, percutaneous, spinal metastases, transforaminal endoscopic decompression
1. Introduction
Vertebral metastases are always associated with specific pain of back and limbs caused by spinal cord or nerve root compression in the late stage of the disease. Due to the short life expectancy of these afflicted patients, treatment protocols for this disease are often palliative rather than curative.[1–3] Although the benefit of aggressive surgeries in managing the pain and neurologic deficits from metastatic spine disease, these treatments are of high risk with low returns, especially the postoperative recovery consumes much of the remainder of life.[2–5] Thus a minimally invasive technique is desired. percutaneous endoscopic lumbar discectomy (PELD) via transforaminal approach is very effective as a minimally invasive surgery not only for herniated discs, but also for some degenerative diseases, such as spinal stenosis and spondylolisthesis.[6,7] In this report, we introduced and described the surgical technique using transforaminal endoscopic resection with foraminoplasty for decompression to overcome this barrier in spinal metastases.
2. Case report
A 71-year-old female was diagnosed with colon cancer, and had the operation of sigmoid colon cancer resection in the year 2011. After 1 year of the surgery, the patient underwent percutaneous vertebroplasty of L3 because of the pain of the low back which was caused by L3 vertebral metastasis. Then, 1 year later, the patient presented with complaints of severe pain in her lower back and left leg that had become progressively more severe and was made even worse by ambulating and sitting up. Magnetic resonance imaging (MRI) showed the L3 vertebral body had been completely involved by osteolytic vertebral metastasis and the compression of the dural sac and nerve root from pathologic fracture fragments and tumor tissue were common findings on presentation (Fig. 1A and B). The sharp pain could not be relieved even though the patient had taken dihydroetorphine hydrochloride tablets. These patients with limited life expectancy and poor general physical condition are ineligible for an invasive surgery. Therefore, the minimally invasive technique was defined at a multidisciplinary medical staff meeting, and approved by the Medical Ethics Committee of our hospital simultaneously.
Figure 1.
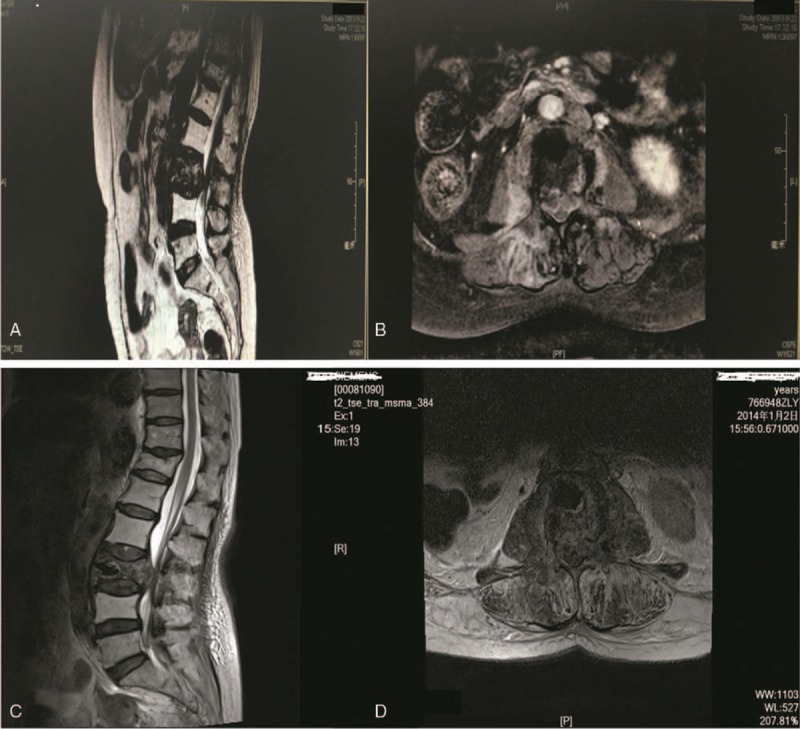
A and B: Preoperative MRI in sagittal (A) and axial (B) plane (2013-09-22) showed a huge metastatic mass destroying L3 body and pedicle and compressing the posterior dural sac and nerve root. C and D: MRI before the second surgery in sagittal (C) and axial (D) plane (2014-01-02) showed that the metastatic mass remained in L3 body and extruded to spinal canal compressing the dural sac and nerve root.
After obtained the informed consent from each participant, we performed the first percutaneous transforaminal endoscopic spinal decompression and palliative resection of metastases in the left side. After the first surgery, symptoms of pain radiating to the left leg were satisfactorily relieved, the visual analog scale (VAS) score decreased from 8/10 preoperatively to 1–2/10. Approximately 4 months after this therapy, the patient complained that radicular pain of the right leg was persistent existing. MRI showed the dural sac and right nerve root was compressed by spinal metastases (Fig. 1C and D). So, the second operation of percutaneous transforaminal endoscopic spinal decompression and palliative resection of metastases was performed in the right side. The patient accepted an operation of selective lumbar arteries chemoembolization before the minimally invasive surgery a week ahead of schedule.
2.1. Operation
Choose the right side of the operation as an example. This procedure was performed with the patient under local anesthesia in the prone position on a radiolucent table and under the guidance of C-arm fluoroscopy. The skin entry point was located 8 cm from the midline and the procedures of puncture and localization were according to the PELD technique.[7] A trephine was used for foraminoplasty to facilitate cannula insertion by removing ventral part of the articular process. Then an endoscope was inserted through the working cannula. Continuous feedback was obtained from the patient during the entire procedure so as not to cause damage to any neural structures. The TESSYS endoscopic system was used for the procedure. In the rear of the intervertebral space, the residual annulus fibrosus and elevated posterior longitudinal ligament, part of pathologic fracture fragments and tumor tissue could be observed under endoscopic visualization. The tumor had invaded the posterior border of L3 and L3-4 intervertebral space as well as compressed the dural sac and nerve root (Fig. 2A). All the tissues that caused the dural sac and nerve root compression were grasped and removed carefully with endoscopic forceps by adjusting the observation angle of the working cannula (Fig. 2B), and then a radiofrequency electrode was used to coagulate bleeding. These 2 procedures were operated to remove the compression tissue alternately, just like the mulberry leaf was swallowed up gradually by a silkworm. The criterion of complete decompression was the dural sac and the nerve root should be observed freely movable with the changes of irrigation pressure (Fig. 2C). At the end of the procedure, the spinal canal, intervertebral space, and foramen were visually inspected while the working cannula and endoscope were removed gradually. The tumor tissue which was taken down should be sent for pathological examination after the operation (Fig. 3).
Figure 2.
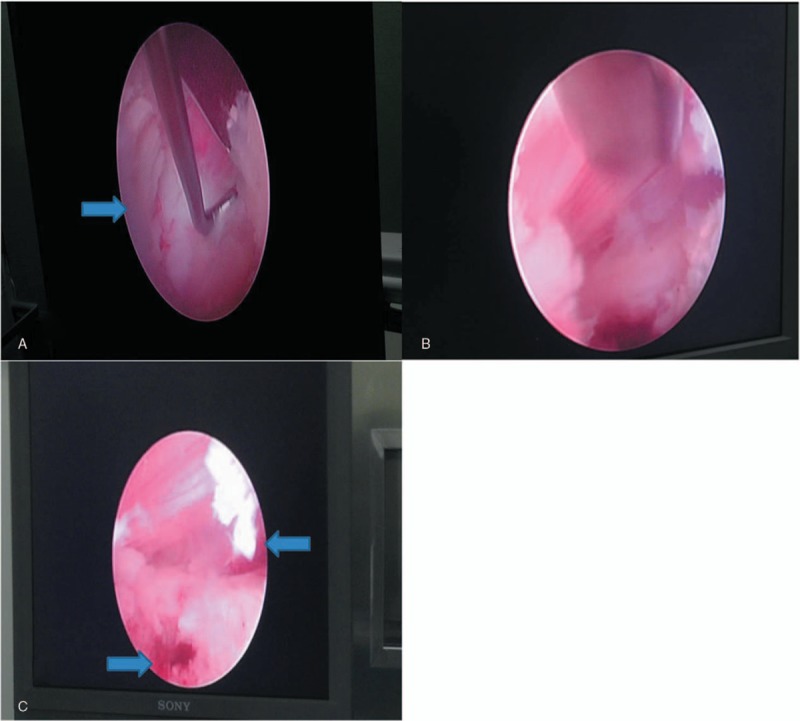
A: The tumor compressed the dural sac and nerve root (Arrow). B: When part of the tumor tissue was exposed, we grasped and removed it with endoscopic forceps. C: After complete decompression, the dural sac and the L4 nerve root were lax in the endoscopic vision (Arrow).
Figure 3.
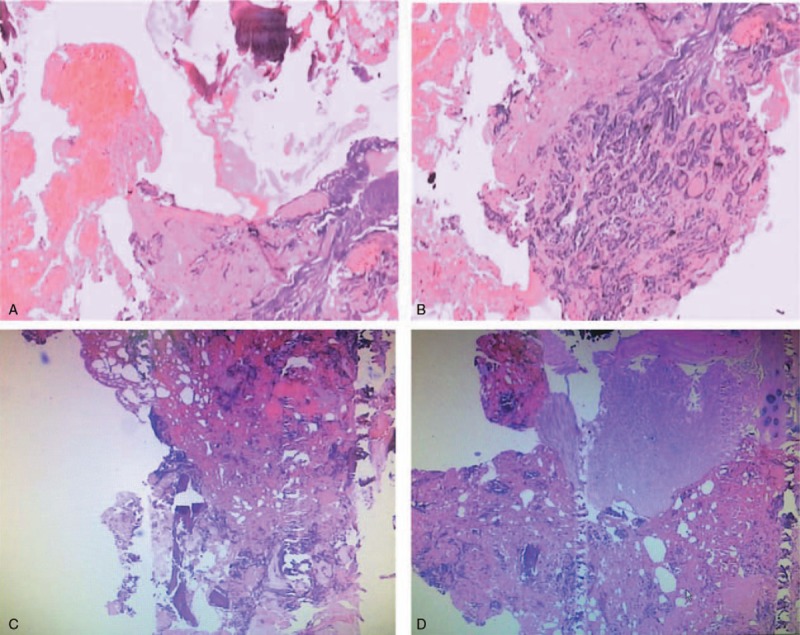
A and B: Pathology report of the tumor tissue after the first operation (2013-10-17) showed metastatic differentiated adenocarcinoma, Immunohistochemistry: CK7 (−); CK20 (+); Villin (+); CDX2 (±); muc2 (−); muc5AC (−); ki67 (70%+). C and D: Pathology report of the tumor tissue after the second operation (2014-01-09) showed metastatic colonic adenocarcinoma, Immunohistochemistry: CK7 (−); CK20 (+); Villin (+); CDX2 (+); CKPan (+); ki67 (50%+).
2.2. Postoperative course
The minimally invasive surgery was performed successfully without clinical complications. The patient's postoperative course was notable for immediate pain relief within 1 hour, and she was able to walk 500 M without a brace or ambulatory assistance device 1 day later. Pain severity in her back and lower limbs greatly decreased from VAS10/10 to 2/10 during the 6-month follow-up, and the use of analgesic opiate was suspended. Because of the aggressive growth of the malignant tumor had metastasized to the whole body, the patient died of respiratory failure 6 months after the second minimally invasive surgery.
3. Discussion
Osseous metastases have a high morbidity in oncology patients, and the spinal column is the most common location among osseous sites for metastatic deposits, especially the anterior spinal column.[8] A variety of surgical methods are available to treat spinal metastases, ranging from limited decompression to radical tumor excision.[4,5,9,10] The benefit of surgical treatment of symptomatic spine metastases often requires both posterior decompression and fixation, which is associated with significant surgery related morbidities including more blood loss, longer operative time, prolonged immobilization, and longer hospital stay. Due to progressive tumor growth and immunosuppression from disease or treatments, these patients may have poor nutritional status, medical comorbidities or contraindications such as ongoing chemotherapy, any of these morbidities will increase perioperative complications significantly (such as infection), even death.[4,5,10,11] Given the limited life expectancy in these patients, open surgery decompression may not be appropriate not only because of the high incidence of serious complications, but the postoperative recovery will take away much of the remainder of life. Therefore, an effective minimally invasive surgery may be an appropriate treatment option in managing the pain and neurologic deficits from spinal metastases.
PELD has been widely performed on patients with back and radicular pain originating from lumbar intervertebral disc herniation.[7] Multiple studies have confirmed that PELD has almost the same operative effects to conventional surgery and has some significant advantages in that it can allow for less tissue trauma, shorter operative time, fewer postoperative complications and faster recovery.[2–5,10] The operation has little impact on the spinal stabilization in virtue of PELD via transforaminal approach. Interestingly, this minimally invasive surgery is rarely used for the treatment of spinal metastases. For those afflicted patients with limited life expectancy, alleviating symptoms and improving the quality of the rest life are our primary concerns in the treatment regimens, and these are also one of the contents of hospice care. Therefore, after comprehensive consideration of the actual situation and demands of the patient, treatment regimen of minimally invasive decompression under percutaneous transforaminal microscopy was defined at a multidisciplinary medical staff meeting after obtained the patient's informed consent.
A detailed technical case report was presented here to illustrate how the vertebral metastatic tumor which compressing the spinal nerve roots was removed via percutaneous transforaminal endoscopic approach. Due to the pathologic fracture fragments and tumor tissue had almost submerged the whole spinal canal of L3, separation, and resection of tissue which adhered to the exiting nerve root and the spinal cord was careful during the operation. Research has shown that around 60% of all spinal metastasis, 40% of benign spinal neoplasms, and 85% of malignant spinal lesions are reportedly hypervascular.[12] One of the biggest risks of this operation was the hemorrhage of tumor tissue, for we could not prevent violent bleeding under the endoscopic vision. Endovascular embolization prior to surgical excision of these hypervascular lesions may help to identify the regional vascular supply of the spinal cord, decrease intraoperative blood loss, decrease local recurrence, and even provide palliative pain relief.[13] Therefore, we recommend that artery embolization of spinal metastases is needed in order to control hemorrhage before you decide to palliative resect tumor and decompress the nerve root. This patient had an operation of selective lumbar arteries chemoembolization about a week before the minimally invasive decompression operation. Adrenaline was added in physiological saline solution (physiological saline 3000 ml; adrenaline 1 mg) which flushing in the intervertebral space in order to constrict vessels throughout the entire process. When there was diffuse hemorrhage, we could improve the irrigation pressure of the flush fluid. Bleeding of small vessels of the metastatic tumor could be blocked by a radiofrequency electrode, and the growth of the tumor could be delayed by the cauterization simultaneously.
It is necessary to note that this technique has some limitations. First, this palliative treatment regimen applies only to patients with short life expectancy who would be less likely to be suitable for aggressive surgeries due to the commonly poor general condition. For patients with long-term life expectancy, minimally invasive decompression alone may not provide sufficient stability. Hence, open surgery for decompression and stabilization should be considered. The biggest risk of this operation is the hemorrhage of tumor tissue, for we could not control violent bleeding effectively under the limited endoscopic exposure. Endovascular embolization prior to surgical excision of these hypervascular lesions may help to identify the regional vascular supply of the spinal cord, decrease intraoperative blood loss. To reduce this risk, we recommend that artery embolization of spinal metastases is needed in order to control hemorrhage before you decide to palliative resect tumor and decompress the nerve root.
This treatment was shown to be an effective and safe modality of minimally invasive pain management for a single-level spinal tumor metastasis causing intractable radicular pain. In fact, the patient felt pain relief immediately during the palliative decompression procedure. In the six months of follow-up, this woman presented sustained pain relief and had no complications of nerve injury. We believe that this is an encouraging case of partly removing a vertebral metastatic tumor compressing the nerve roots by the percutaneous transforaminal endoscopic technique.
4. Conclusions
Percutaneous transforaminal endoscopic decompression is a valuable treatment option in patients presenting with pain and neurologic deficits from spinal metastases. This technique may reduce the incidence of serious complications, improve the overall quality of life for these patients with a limited life expectancy. Prospective studies are needed to validate the safety and efficacy of this surgery for spinal metastases.
Author contributions
Gao, Wu and Lin conceived and wrote the manuscript and participated in the literature review; Gao, Lin, and Zhang participated in the minimally-invasive surgery and helped to draft the manuscript. All authors read and approved the final manuscript.
Software: Pei Zhang.
Supervision: Zengxin Gao.
Writing – original draft: Zengxin Gao, Yucheng Lin, Pei Zhang, Zhanpo Wu.
Writing – review & editing: Zengxin Gao, Yucheng Lin, Zhanpo Wu.
Footnotes
Abbreviations: MRI = Magnetic resonance imaging, PELD = percutaneous endoscopic lumbar discectomy, TESSYS = transforaminal endoscopic spine system, VAS = visual analog scale.
ZG and ZW contributed equally to this work.
We also want to identify the Zengxin Gao as the only first author and affirm Zhanpo Wu as just corresponding author.
The relative of the patient has provided informed consent for publication of the case.
The authors have no conflicts of interest to disclose.
References
- [1].Bartel RH, Feuth T, van der Maazen R, et al. Development of a model with which to predict the life expectancy of patients with spinal epidural metastasis. Cancer 2007;110:2042–9. [DOI] [PubMed] [Google Scholar]
- [2].Stephenson MB, Glaenzer B, Malamis A. Percutaneous minimally invasive techniques in the treatment of spinal metastases. Curr Treat Oncol 2016;17:56. [DOI] [PubMed] [Google Scholar]
- [3].Hariri O, Takayanagi A, Miulli DE, et al. Minimally invasive surgical techniques for management of painful metastatic and primary spinal tumors. Cureus 2017;9:e1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Pennington Z, Ahmed AK, Molina CA, et al. Minimally invasive versus conventional spine surgery for vertebral matastases: a systematic review of the evidence. Ann Transl Med 2018;6:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Uei H, Tokuhashi Y, Maseda M, et al. Comparison between minimally invasive spine stabilization with and without posterior decompression for the management of spinal metastases: a retrospective cohort study. J Orthop Surg Res 2018;13:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ahn Y. Percutaneous endoscopic decompression for lumbar spinal stenosis. Expert Rev Med Devices 2014;11:1–2. [DOI] [PubMed] [Google Scholar]
- [7].Kim HS, Paudel B, Jang JS, et al. Percutaneous endoscopic lumbar disc herniations (LDH) including severely difficult and extremely difficult LDH cases. Pain Physician 2018;21:E401–8. [PubMed] [Google Scholar]
- [8].Bohm P, Huber J. The surgical treatment of bony metastases of the spine and limbs. J Bone Joint Sur Br 2002;84:521–9. [DOI] [PubMed] [Google Scholar]
- [9].Bernard F, Lemee JM, Lucas O, et al. Postoperative quality-of-life assessment in patients with spine metastases treated with long-segment pedicle-screw fixation. J Neurosurg Spine 2017;26:725–35. [DOI] [PubMed] [Google Scholar]
- [10].Miscusi M, Polli FM, Forcato S, et al. Comparison of minimally invasive surgery with standard open surgery for vertebral thoracic metastases causing acute myelopathy in patients with short- or mid-term life expectancy:surgical technique and early clinical results. J Neurosurg Spine 2015;22:518–25. [DOI] [PubMed] [Google Scholar]
- [11].Dustin DJ, Abd-EI-Barr MM, Yi Lu. Minimally invasive muscle spareing posterior-only approach for lumber circumferential decompression and stabilization to treat spine metastasis- technical report. World Neurosurg 2015;84:1484–90. [DOI] [PubMed] [Google Scholar]
- [12].Olerud C, Jonsson H, Jr, Lofberg AM, et al. Embolization of spinal metastases reduces peroperative blood loss. 21 patients operated on for renal cell carcinoma. Acta Orthop Scand 1993;64:9–12. [DOI] [PubMed] [Google Scholar]
- [13].Ghobrial GM, Chalouhi N, Harrop J, et al. Preoperative spinal tumor embolization: an institutional experience with Onyx. Clin Neurol Neurosurg 2013;115:2457–63. [DOI] [PubMed] [Google Scholar]


