Abstract
The aim of the study was to observe the curative effect of long intestinal tube (LT) in the treatment of phytobezoar intestinal obstruction.
We performed a retrospective study of patients with phytobezoar intestinal obstruction who underwent decompression with different tube insertion method. A total of 80 patients were collected and divided into nasogastric tube (NGT) group (n = 36) and LT group (n = 44) between August 2015 and August 2018 at our hospital. Univariate analysis was used to assess the clinical efficacy of 2 groups of patients.
There were no significant differences in the mean age, sex ratio, and previous surgical history between the 2 groups. There were statistically significant differences between the 2 groups in terms of improvement time of clinical indications (4.2 ± 1.4 vs 2.5 ± 0.6 days; P = .008), liquid decompression amount on the first day of catheterization (870.4 ± 400.8 vs 1738.4 ± 460.2 mL; P = .000), transit operation rate (4/36 vs 0/44; P = .023), clinical cure rate (25/36 vs 40/44; P = .014), total treatment efficiency (32/36 vs 44/44; P = .023), and total hospitalization cost (3.25 ± 0.39 vs 2.07 ± 0.41 ¥ ten thousand; P = .000).
The curative effect of LT in the treatment of phytobezoar intestinal obstruction is accurate and reliable, which can effectively improve the clinical symptoms of patients, comprehensively improve the non-surgical rate of intestinal obstruction treatment, reduce the total cost of hospitalization, and is worthy of promotion in clinical application.
Keywords: intestinal obstruction, long intestinal tube, nasogastric tube, phytobezoar, rhubarb
1. Introduction
Bezoars grow due to the ingestion and accumulation of undigested material. Bezoars can be classified into 4 types based on their components[1–4]: a phytobezoar is one type of bezoar, a concretion of undigested particles that usually forms in the stomach, and descends through the digestive tract where small bowel obstruction can result. A trichobezoar is composed of hair, and is associated with psychiatric disorders such as trichotillomania. A pharmacobezoar usually comprises undigested pills from supplements and/or medications. Lactobezoars are more commonly seen in neonates, resulting from the formation of milk curds in the stomach due to the immaturity of the digestive system. Phytobezoar is currently the most common type of bezoars, mostly formed after eating food with a more tannic acid such as hawthorn and persimmon.
Phytobezoar is an unusual cause of small bowel obstruction. It accounts for about 0.4% to 4% of all mechanical bowel obstruction.[5] However, the symptoms are not very different from those caused by usual etiologies of small bowel obstruction. Gastrointestinal decompression is the most effective therapy for the patients with acute small bowel obstruction without any indications of strangulation. There are 2 ways of bowel decompression, with insertion of a nasogastric tube (NGT) or of a long intestinal tube (LT). The NGT is not long enough for suctioning the distal intestine and its decompression efficacy is relatively low. Since the 1930s, the concept of nasointestinal decompression and use of nasointestinal tubes have been developed and applied in clinical practice.[6] There have been reports describing the usefulness of LT decompression for the treatment of intestinal obstruction.[7] In addition, traditional Chinese medicine rhubarb was injected into intestinal tract through LT to improve intestinal function and make phytobezoar disintegrate as soon as possible.
On the basis of traditional treatment measures for intestinal obstruction, LT was used in our hospital to treat the patients with phytobezoar intestinal obstruction. This randomized controlled study attempted to investigate and compare the clinical efficacy between LT and NGT for patients with phytobezoar intestinal obstruction.
2. Materials and methods
2.1. Patients
The clinical data of 80 patients with phytobezoar intestinal obstruction admitted by our hospital between August 2015 and August 2018 were included in this retrospective study. The data were collected from patient charts and electronic medical records of the patients with Intestinal obstruction (ICD-10 code K56.4) in Zibo central hospital. All the patients were assigned to either of the following groups based on the method of tube insertion: conventional group (NGT group) or intervention group (LT group).
2.2. Inclusion and exclusion criteria
The selection criteria were case–control studies that compared the effect of LTs and NGTs decompression in the management of phytobezoar intestinal obstruction. All the patients had the incentive to eat hawthorn, persimmon and other foods, and the presence of fecal shadow (Fig. 1A) was confirmed by abdominal computed tomography (CT) examination, which was in line with the clinical manifestation (such as abdominal pain, distension, nausea and vomiting, stop exhaust defecation) of intestinal obstruction. The baseline characteristics of the patients were similar in the 2 groups.
Figure 1.

A, Abdominal CT scan shows an intestinal mass considered to be a phytobezoar (white arrow), and shows proximal intestinal dilatation and intestinal effusion. B, The red arrow indicates the long intestinal tube placed in the intestinal cavity, showing bezoar disintegrating, decreased expansion of the bowel after decompression and significantly reduced intestinal effusion.
The exclusion criteria were as follows: the treatment of gastric bezoar and large bowel obstruction; patients with strangulated intestinal obstruction; patients were also excluded if they had a severe chronic disease such as cardiovascular disease or renal failure that would interfere with the treatment.
2.3. Methods
2.3.1. Treatment methods
All the patients were given conventional treatment measures for intestinal obstruction, including guiding the patients to fasting, correcting the balance of water, electrolytes and acid–base, applying antibiotics and nutritional support, and suppressing the secretion of digestive juice by somatostatin. All patients were treated with colon hydrotherapy enema. Both groups of patients received somatostatin treatment with 6 mg of somatostatin added to 60 mL of 0.9% sodium chloride injection, intravenous infusion for 24 hours. After the patient resumed normal autonomic exhaust and the main symptoms of intestinal obstruction were significantly relieved, somatostatin was discontinued. The patient recovered normal exhaust, the main symptoms of intestinal obstruction were significantly relieved, and the catheter was closed, and the patients were extubated without obvious abdominal discomfort after feeding (Fig. 1B). If the patient has no obvious improvement in symptoms after 48 hours of conservative treatment and presents signs of peritonitis, enterotomy, and lithotomy should be performed.
2.3.2. NGT group
The NGT is made of domestic disposable nasogastric tubes, 16Fr, 5.3 mm in diameter, with a total length of 125 cm, connected with negative pressure suction bag. Before the treatment, the NGT was fully lubricated with paraffin oil, and the nasal cavity was thoroughly cleaned with a wet cotton swab. The NGT was gently inserted through the nasal cavity and inserted into the stomach through the throat with a depth of 55 to 65 cm. The NGT was properly fixed according to the specific conditions of the patient during the intubation.
2.3.3. LT group
The LT uses the CLINY type intestinal obstruction catheter kit produced by Japan Create Medic company, in which the LT is a pure silicone transparent tube with 3 lumens and 2 capsules (balloon before and after), the total length is 300 cm, 16Fr, side holes at the front end, the guide wire length is 350 cm, and the guide wire diameter is 1.24 mm. The front end of the catheter is a beaded front terminal with a stainless steel ball, which is impervious to x-ray and easily advances through the pylorus and forward in the small intestine. The front airbag is generally filled with 15 to 30 mL distilled water, and the rear airbag is filled with 30 to 60 mL air. A duct with a side hole between the front and rear airbags for decompression or imaging. The rear end is provided with a pressure reducing interface, a front and rear airbag interface, and a gas supply port (to prevent the negative pressure from causing the side hole to adhere to the wall and improve the drainage effect). The outer tube attracts the contents of the gastrointestinal tract, and the inner tube is filled with water into the top of the water sac. Under the guidance of x-ray, the LT was placed by conventional catheterization, the contrast agent was injected to observe the intestinal obstruction, while the contrast agent and the retained intestinal fluid were aspirated. The guidewire was pulled out under the x-ray, 15 mL sterile injection water was injected into the balloon front the catheter, and the catheter was fixed at the outer end of the nose and indicated the depth of insertion. The catheter was adjusted every 24 hours and the drug (rhubarb) was injected through the catheter. Rhubarb, which can be used as a prescribed drug “Powdered Rhubarb” (Yalan Pharmaceutical, Gansu, China) in the Chinese pharmacopoeia, can be administered for constipation.
2.4. Observation index and evaluation criteria
Observed the clinical indications of the 2 groups of patients, including the decompression volume on the first day of catheterization, abdominal circumference before and after decompression, remission time of abdominal distension and abdominal pain, exhaust recovery time, hospitalization days and total hospitalization expenses, statistical transit operation rate and patient satisfaction rate, to evaluated the clinical efficacy of the patients.
Cure means that the clinical symptoms of phytobezoar intestinal obstruction were completely disappeared, feces were unobstructed, and eating fluids were no obvious discomfort. Effectiveness means that the clinical symptoms of the patients were obviously improved and feces were basically unobstructed. Ineffectiveness means that the clinical symptoms were not improved or aggravated, and transit the surgical treatment. The total effect is the sum of cure and effectiveness.
2.5. Statistical analyses
SPSS version 24.0 (SPSS IBM, Chicago, IL) was used for statistical analyses. Data are expressed as the mean ± standard deviation (SD) for normally distributed continuous variables and as the absolute number for categorical variables. To compare groups, Student t test (for normal distribution) and nonparametric test (for non-normal distribution) were used for continuous variables. The chi-square test was used to compare categorical variables. All statistical analyses were 2-sided, and a P < .05 was considered statistically significant.
2.6. Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Biomedicine Research of the Zibo central hospital (registration No. 201508001). Informed consent was not required because of the retrospective and anonymous nature of this study.
3. Results
3.1. Baseline characteristics of patients
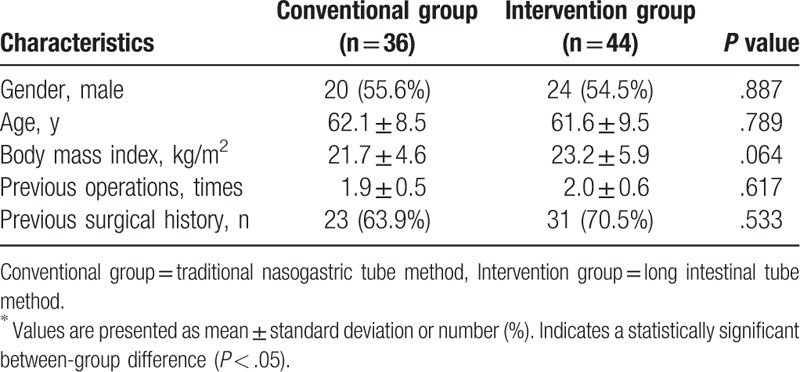
In all, 80 patients met the inclusion criteria: 36 underwent NGT and 44 underwent LT method. The study flow chart is presented in Fig. 2. In the conventional group including 20 men and 16 women, aged from 53 to 72 years, with an average age of 62.1 ± 8.5 years, and 23 patients with previous abdominal surgery. In the intervention group, there were 24 men and 20 women, aged from 51 to 78, with an average age of 61.6 ± 9.5 years. There was no statistically significant difference between the 2 groups in mean age, sex ratio, abdominal pain on admission, abdominal distension, nausea and vomiting, anorectal stopping of exhaust and defecation, and previous surgical history (P > .05) (Table 1).
Figure 2.
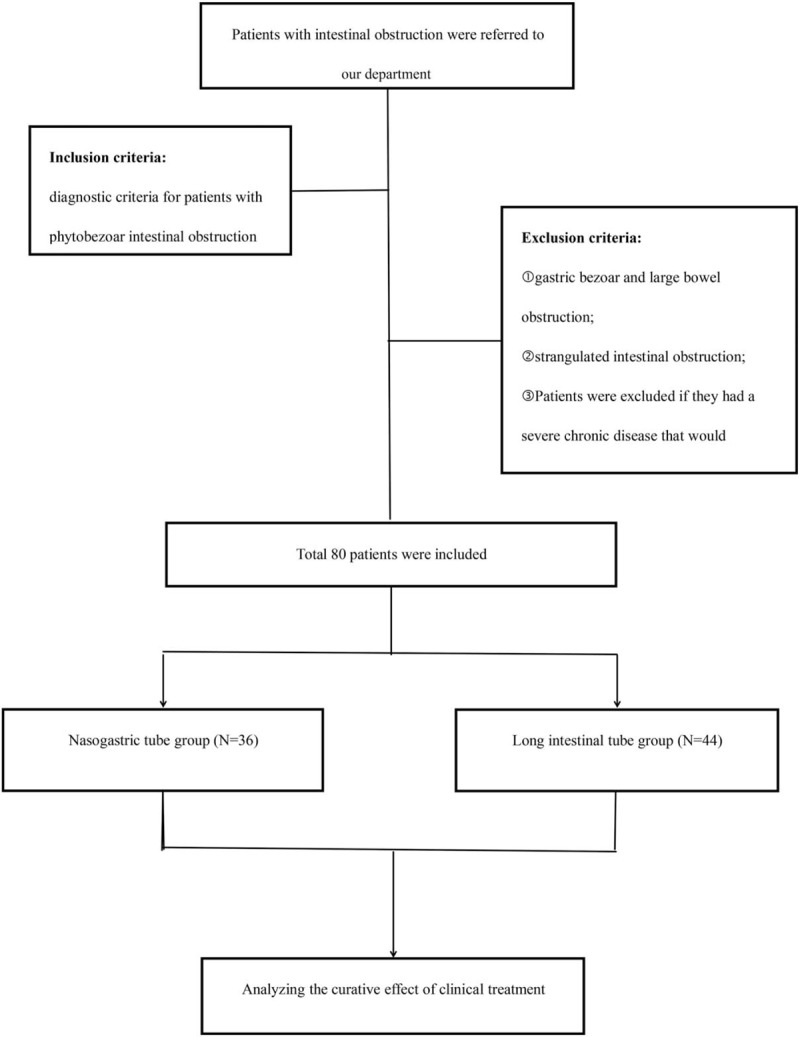
Flow chart of inclusion and exclusion criteria of the study.
Table 1.
Baseline characteristics of the study population∗.
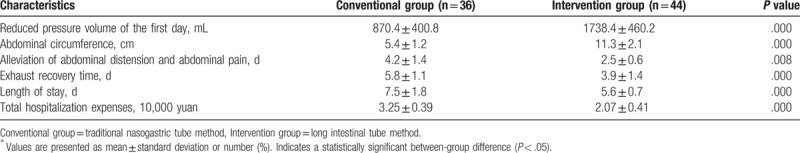
3.2. Clinical indication improvement results
The improvement time of clinical indications in intervention group was significantly shorter than that in conventional group, with statistically significant differences (P < .01) (Table 2).
Table 2.
Comparison of clinical indications between the 2 groups∗.
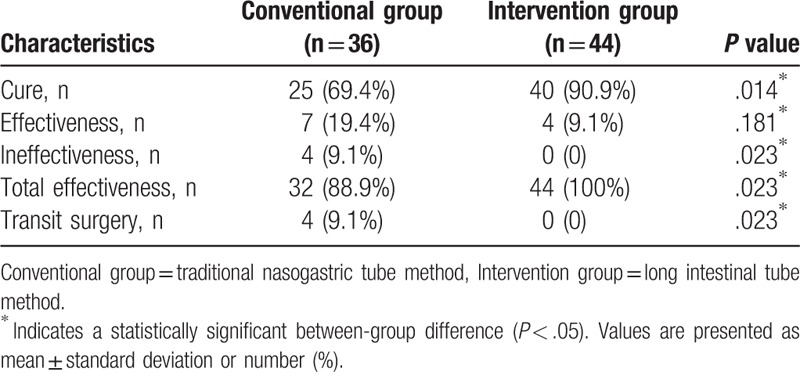
3.3. Clinical efficacy evaluation and transit surgery
The clinical cure rate of the intervention group was significantly higher than that of the conventional group, and the transit operation rate was significantly lower than that of the conventional group, with statistically significant differences (P < .05). The total effective rate of the intervention group was significantly higher than that of the conventional group, with statistically significant differences (P < .05) (Table 3).
Table 3.
Comparison of the efficacy evaluation and transit surgery between the 2 groups.
4. Discussion
Phytobezoar intestinal obstruction is a common type of mechanical intestinal obstruction, which is mostly caused by eating foods such as hawthorn and persimmon with more tannic acid. Improper eating methods, large amounts of food intake, and eating on an empty stomach is especially obvious. After eating, tannic acid and gastric acid coagulate and precipitate, forming a gelatinous polymer, namely stomach stone. In addition, tannic acid can combine with proteins in gastrointestinal fluid to form water-insoluble gelatinous tannin protein, which encases plant residues and fibers and forms phytobezoar in the gastrointestinal tract. It has astringency effect, which can reduce intestinal mucus secretion and inhibit intestinal peristalsis.[2] Patients with a history of abdominal surgery and gastrointestinal motility function dysplasia can increase the possibility of bezoar formation.[8] There is also reported that the formation of bezoar may be related to subtotal gastrectomy, gastrojejunostomy, or gastric vagotomy.[9,10] With the increasing number of bariatric surgery in recent years, the number of cases of postoperative bezoar formation has also increased.[11] Gastric vagotomy and partial gastrectomy can reduce gastric acid secretion, resulting in a weakly acidic environment, while reducing gastric motility, so removal of undigested solid food from the stomach may be delayed, resulting in the formation of large quantities of sticky substances in the stomach. Thereby it is easy to form a bezoar. Gastroenteroanastomosis or pyloroplasty can expand the gastric outlet, so undigested vegetable or fruit fibrous mass in the stomach can easily enter the small intestine and form an obstructive mass, resulting in incarceration and obstruction.[10,12]
The diagnosis of phytobezoar intestinal obstruction mainly depends on abdominal computed tomography (CT) examination. Abdominal CT mainly show the circular or oval soft tissue mass shadow with a clear boundary, and its internal density is not uniform or with a small air bubble. The wall around the phytobezoar is usually relatively complete with high-density or soft tissue density, and there is a low-density band between the phytobezoar and the intestinal wall, which may be caused by a small amount of intestinal fluid between the phytobezoar and the intestinal wall or local small intestinal mucosa compression oedema.[13,14] Abdominal ultrasonography also provides some help in the diagnosis.[15]
Gastrointestinal decompression is one of the effective methods for conservative treatment of intestinal obstruction, but the NGT is routinely used in clinic can only decompress gastric juice in the stomach, but retention of liquid or gas in small intestine, especially in low intestine retention content cannot directly to attract, therefore, the lower intestinal obstruction, the simple gastric tube decompression cannot reach the site of obstruction, cannot attract the contents or gas well, cannot carry out effective intestinal decompression, resulting in obstruction of the proximal intestinal mucosa congestion Edema. At the same time, the highly expanded intestinal tube has the destruction of the intestinal mucosal barrier, the intestinal wall presents a serious ischemia state, and it is easy to cause bacterial displacement, resulting in intestinal endotoxemia, which aggravates the damage to the body. Coca-Cola has been reported as an effective treatment for phytobezoar,[16,17] but for the phytobezoar in the small intestine, Coca-Cola cannot directly contact the fecal stone, so its effect is not significant. Most gastric bezoar can be treated by endoscopic combined with or without cola dissolution, and once bezoar enter the small intestine to form small intestinal obstruction, previous treatment believed that laparotomy or laparoscopic surgery is usually unavoidable for intestinal fecal stones in the case of poor conservative treatment effect. In recent years, the LT that can be placed into the small intestine has been used for the treatment of intestinal obstruction.[18,19] Transnasal the LT is a new method to relieve intestinal pressure. The gravity of the fluid in the front of the balloon and the hydrophilic coating hose driven by digestive tract peristalsis can reach the proximal end of the obstruction and even enter the colon through the blind part. As the LT moves forward continuously, the fluid or gas can be continuously attracted to the proximal end of the obstruction section in the obstruction area, significantly improving the symptoms of abdominal pain and abdominal distension in the patient. The decompression effect of the LT is more accurate than the simple NGT. The LT can quickly relieve the pressure in the intestinal cavity caused by obstruction, improve the blood supply of the intestinal wall, reduce the intestinal mucosa hyperemia oedema, and reduce the intestinal flora and endotoxin translocation greatly reduced the occurrence of intestinal strangulation. With the decrease of pressure in the bowel and the improvement of blood circulation, the intestinal peristalsis gradually recovered. At the same time, the LT can support the intestinal tract to play the role of intestinal arrangement, which reduces intestinal adhesion to some extent.
Rhubarb, a Chinese herb, was injected into the intestinal tract through the LT to improve the intestinal function and cause the phytobezoar to disintegrate as soon as possible. The intestinal tract is the largest reservoir and endotoxin reservoir in the human body. Once the intestinal mucosal barrier integrity and protection function damage, gut bacteria or bacterial endotoxin to parenteral shift can cause intestinal local or systemic inflammatory response of the uncontrolled, so that the gastrointestinal tract as a trigger of systemic inflammatory response syndrome (SIRS) and the central organs of multiple organ dysfunction syndrome (MODS), participate in pathophysiological process of organ damage of multiple serious diseases and organ injuries. The raw rhubarb powder belongs to traditional Chinese medicine, according to the Chinese traditional medicine record, the raw rhubarb bitter cold subsidence, it has the function of removing retained waste, clearing away the intestines and stomach, and draining the fire and cooling blood, comply with the principle of “the six hollow viscera must keep its unobstructed.” Modern pharmacology and animal experimental study confirmed that rhubarb is the main chemical composition of anthraquinone derivatives such as rhubarb phenol and rhein,[20] which can promote colon peristaltic function, promote the metabolism of the gastrointestinal tract and the recovery of intestinal function, improve the intestinal mucosal blood flow perfusion, relieve the ischemia and hypoxia, conducive to discharge dung, reduce and avoid the endotoxemia, especially in inhibiting inflammatory cytokines (such as tumor necrosis factor, interleukin, etc.), improve blood supply to intestinal mucosa and suppress the “second strike” of toxic substances in serum,[21,22] which reduces the severity of the SIRS, effectively prevent the progression of SIRS to MODS. Secondly, the heat-clearing and detoxifying function of rhubarb powder can inhibit enterococcus and Escherichia coli, alleviate enterogenous bacterial infection, avoid or alleviate bacterial translocation, maintain the ecological balance of intestinal flora and regulate immunity.[23]
The main limitation of our study was its retrospective design, which may have contributed some selection bias. In addition, we recognize that our study has small sample size limitations and it is a single center study. Given that rhubarb powder is responsible for laxative and cathartic activities and rhubarb (emodin) has potent anti-inflammatory activity, our studies did not distinguish which component contributed to the therapeutic effects we observed in this study. Due to the difference in drug absorption, individual patients might have variable doses of drug absorbed, leading to a variation in the therapeutic effects. Because the patients had variable disease severities and potential different sensitivities to rhubarb.
5. Conclusions
The retrospective study showed that the total effective rate and the relief of intestinal obstruction symptoms in the intervention group were significantly better than those in the conventional group. As the LT can effectively and rapidly reduce intestinal pressure and relieve mechanical obstruction, the rate of open surgery was greatly reduced. The way of relying on the surgery to cure such patients is becoming less and less, thereby reducing the trauma of the surgery. Although the LT is considerably more expensive than the gastric tube, the total cost of hospitalization shows that the LT significantly alleviates gastrointestinal symptoms within a short period of time, reducing the length of hospitalization and thereby reducing the total cost.
Acknowledgments
They are particularly grateful to all the people who have given us help on our article.
Author contributions
Conceptualization: Liang Li, Bing Xue.
Data curation: Liang Li, Hong-Qiang Xie.
Formal analysis: Qiang Zhao.
Investigation: Liang Li, Hong-Qiang Xie, Xue-Rong Luan.
Methodology: Liang Li, Qing Cui.
Writing – original draft: Liang Li, Bing Xue.
Writing – review & editing: Liang Li.
Liang Li orcid: 0000-0002-5707-0865.
Footnotes
Abbreviations: CT = computed tomography, LT = long intestinal tube, MODS = multiple organ dysfunction syndrome, NGT = nasogastric tube, SD = standard deviation, SIRS = systemic inflammatory response syndrome.
The authors have no conflicts of interest to disclose.
References
- [1].Gurzu S, Jung I. Gastric tricho-wool bezoar in an 18-year-old girl. S Afr J Surg 2013;51:33–4. [DOI] [PubMed] [Google Scholar]
- [2].Iwamuro M, Okada H, Matsueda K, et al. Review of the diagnosis and management of gastrointestinal bezoars. World J Gastrointest Endosc 2015;7:336–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Yamamoto M, Yamamoto K, Bian X, et al. Small bowel obstruction caused by dried persimmon. Case Rep Gastroenterol 2018;12:147–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Jain SA, Agarwal L, Khyalia A, et al. Pharmacobezoar-a rare case presented as gastric outlet obstruction. J Surg Case Rep 2018;2018:rjy116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Hall BM, Shapiro MJ, Vosswinkel JA, et al. Phytobezoar as a cause of intestinal obstruction. J Gastrointest Surg 2011;15:2293–5. [DOI] [PubMed] [Google Scholar]
- [6].Tanaka S, Yamamoto T, Kubota D, et al. Predictive factors for surgical indication in adhesive small bowel obstruction. Am J Surg 2008;196:23–7. [DOI] [PubMed] [Google Scholar]
- [7].Chen XL, Ji F, Lin Q, et al. A prospective randomized trial of transnasal ileum tube vs nasogastric tube for adhesive small bowel obstruction. World J Gastroenterol 2012;18:1968–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Erzurumlu K, Malazgirt Z, Bektas A, et al. Gastrointestinal bezoars: a retrospective analysis of 34 cases. World J Gastroenterol 2005;11:1813–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Bitton A, Keagle JN, Varma MG. Small bowel bezoar in a patient with Noonan syndrome: report of a case. Med Gen Med 2007;9:34. [PMC free article] [PubMed] [Google Scholar]
- [10].Sarhan M, Shyamali B, Fakulujo A, et al. Jejunal bezoar causing obstruction after laparoscopic Roux-en-Y gastric bypass. JSLS 2010;14:592–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ben-Porat T, Sherf Dagan S, Goldenshluger A, et al. Gastrointestinal phytobezoar following bariatric surgery: systematic review. Surg Obes Relat Dis 2016;12:1747–54. [DOI] [PubMed] [Google Scholar]
- [12].Bedioui H, Daghfous A, Ayadi M, et al. A report of 15 cases of small-bowel obstruction secondary to phytobezoars: predisposing factors and diagnostic difficulties. Gastroenterol Clin Biol 2008;32:596–600. [DOI] [PubMed] [Google Scholar]
- [13].Wang PY, Wang X, Zhang L, et al. Bezoar-induced small bowel obstruction: clinical characteristics and diagnostic value of multi-slice spiral computed tomography. World J Gastroenterol 2015;21:9774–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chen YC, Liu CH, Hsu HH, et al. Imaging differentiation of phytobezoar and small-bowel faeces: CT characteristics with quantitative analysis in patients with small- bowel obstruction. Eur Radiol 2015;25:922–31. [DOI] [PubMed] [Google Scholar]
- [15].Lee KH, Han HY, Kim HJ, et al. Ultrasonographic differentiation of bezoar from feces in small bowel obstruction. Ultrasonography 2015;34:211–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Ladas SD, Kamberoglou D, Karamanolis G, et al. Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatment. Aliment Pharmacol Ther 2013;37:169–73. [DOI] [PubMed] [Google Scholar]
- [17].Iwamuro M, Kawai Y, Shiraha H, et al. In vitro analysis of gastric phytobezoar dissolubility by Coca-Cola, Coca-Cola Zero, cellulase, and papain. J Clin Gastroenterol 2014;48:190–1. [DOI] [PubMed] [Google Scholar]
- [18].Gowen GF. Rapid resolution of small-bowel obstruction with the long tube, endoscopically advanced into the jejunum. Am J Surg 2007;193:184–9. [DOI] [PubMed] [Google Scholar]
- [19].Li M, Ren J, Zhu W. Long intestinal tube splinting really prevents recurrence of postoperative adhesive small bowel obstruction: a study of 1071 cases. Am J Surg 2015;209:289–96. [DOI] [PubMed] [Google Scholar]
- [20].Aichner D, Ganzera M. Analysis of anthraquinones in rhubarb (Rheum palmatum and Rheum officinale) by supercritical fluid chromatography. Talanta 2015;144:1239–44. [DOI] [PubMed] [Google Scholar]
- [21].Zhang X, Wang L, Chen DC. Effect of rhubarb on gastrointestinal dysfunction in critically ill patients: a retrospective study based on propensity score matching. Chin Med J (Engl) 2018;131:1142–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bajic JE, Eden GL, Lampton LS, et al. Rhubarb extract partially improves mucosal integrity in chemotherapy-induced intestinal mucositis. World J Gastroenterol 2016;22:8322–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Xiong Y, Chen L, Fan L, et al. Free total rhubarb anthraquinones protect intestinal injury via regulation of the intestinal immune response in a rat model of severe acute pancreatitis. Front Pharmacol 2018;9:75. [DOI] [PMC free article] [PubMed] [Google Scholar]


