Supplemental Digital Content is available in the text
Keywords: electromagnetic navigation bronchoscopy, localization, pulmonary nodule, thoracoscopy
Abstract
Thoracoscopic resection of small subsolid nodules is challenging and requires preoperative localization. We investigated the efficacy, safety, and factors affecting accuracy in localizing pulmonary nodules with electromagnetic navigation bronchoscopy (ENB)-guided dye marking.
Patients with small subsolid nodule(s) who underwent thoracoscopic resection after ENB-guided dye marking were retrospectively reviewed. Dye marking was performed at the nearest pleura and the localized nodule(s) was resected thoracoscopically. Efficacy was evaluated by success rates of dye marking and resection of nodules. Navigation accuracy was represented by target distance, which was the closest distance between target and the tip of locatable guide. Factors affecting target distance were evaluated by linear regression analyses.
Twenty-nine ENB-guided dye markings were done for 24 nodules in 20 patients. The success rate of the dye marking and nodule localization were 93.1% (27/29) and 95.8% (23/24), respectively. Twenty-three nodules were completely resected thoracoscopically without conversion. There were no ENB-related complications: pneumothorax or bronchopulmonary hemorrhage. Nine targets were in the upper, 14 in the middle, and 6 in the lower zone. Even though navigation time was longer in the upper zone, target distance showed no significant inter-zone difference. Approach angle was the only significant predictor for target distance (0–45°, estimate = −1.24, P = .01; 45–90°, estimate = −1.26, P = .006; reference = ≥90°).
Localization with ENB-guided dye marking is effective and safe for thoracoscopic resection of small subsolid nodules. For better performance, a pathway with smaller approach angle (<90°) should be selected to increase the navigation accuracy.
1. Introduction
Subsolid pulmonary nodules are being detected with increasing frequency as low-dose computed tomography (CT) screening becomes more popular. Also the use of diagnostic and therapeutic thoracoscopic surgery for CT-detected nodules is also increasing.[1–3] However, resection of subsolid nodules by thoracoscopic surgery is challenging because intraoperative identification via video images or manual palpation is not always possible. Hence, the procedure for preoperative localization is crucial for intraoperative detection of subsolid pulmonary nodule which is small or deeply located within lung parenchyma during thoracoscopic surgery.[4]
Electromagnetic navigation bronchoscopy (ENB) allows physicians to access peripheral lung lesions that are beyond the reach of conventional bronchoscopy with high accuracy.[5] ENB also provides more obvious landmarks for the surgeons to facilitate thoracoscopic resection of small pulmonary nodules when it is combined with dye-marking.[6] The safety and effectiveness of ENB-guided localization for peripheral pulmonary nodules has been recognized by several studies. The success rate of ENB-guided localization for thoracoscopic resection of small pulmonary nodules has been reported to range from 97.2% to 100%.[6–8]
An effective ENB procedure incorporates choosing the best route among various bronchial courses. Hence, target planning that is optimal and reproducible in planning appropriate navigation routes is very desirable. However, there is little information regarding the influence of anatomic features and navigation-associated variables on the accuracy of navigation procedure. The rarity of ENB data on the effect of navigation accuracy makes our findings valuable.
We analyzed the clinical outcomes of ENB-guided dye localization for thoracoscopic resection of small subsolid pulmonary nodules and the factors affecting the accuracy of ENB navigation.
2. Methods
2.1. Patients and data collection
We retrospectively reviewed patients who underwent ENB-guided dye localization followed by thoracoscopic resection for subsolid pulmonary nodules from July 2016 to August 2017. Collected data comprised: demographic information; radiologic diagnosis; radiologic size of nodules; nodule location; numbers of dye markings; type of resection; ENB planning information; ENB navigation information with duration; pathologic diagnosis; perioperative outcomes; adverse events. Nine patients with insufficient planning information were excluded from our analyses. The present study was conducted in accordance with ethical principles of the Helsinki Declaration. The study protocol was approved by the Institutional Review Board of Seoul National University (# 1703-016-836).
The locations of nodules were categorized into 3 zones according to their bronchial anatomic structure; upper zone (right upper lobe and left upper division); middle zone (right middle lobe, lingular segment, and both superior segments); lower zone (both basal segments). The target distance from the navigation tip to target, approach angle at the bronchiole exit point between the tunneled path and bronchial navigation route, and tunneling distance from the bronchiole exit point to the target were recorded during ENB planning. The time spent for ENB targeting and engagement success to the planned route was also obtained during the ENB procedure.
Approach angle was the maximal angle at axial, coronal or sagittal planes (Fig. 1A). The degree of the angle was created with the vertex on the bronchiole exit point and formed by the vector of the tunneled path and the horizontal axis along the navigation route. The measurement was calculated using Adobe Photoshop CC (Adobe systems incorporated, San Jose, CA) by one of the authors (KYH) to reduce potential inter-observer bias. This approach angle was recorded in degrees but analyzed in terms of the categories of 0–45°, 45–90°, and over 90° to minimize measurement bias. Navigation time was defined as the time taken between loading of the navigational bronchoscope at the trachea and locking of the angled guide-sheath immediately after the tip of locatable guide-wire had reached the final location near the target.
Figure 1.
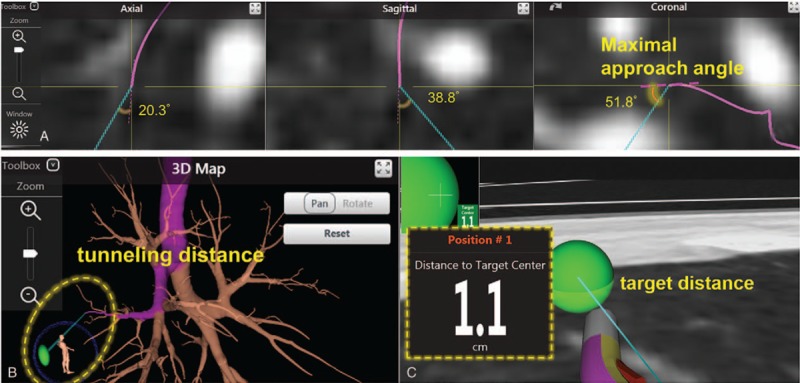
Illustrations for navigation parameters. (A) Approach angle and (B) tunneling distance from the bronchiole exit point, and (C) target distance from navigation tip to the target.
2.2. ENB planning, dye-marking, and surgical procedures
Indications for ENB-guided dye-marking were subsolid nodules smaller than 10 mm near the pleura or nodules smaller than 20 mm located >10 mm deep from the pleural surface. Lesions were localized with one or more dye-markings. Marking targets were set at the nearest pleura from the nodule or at the pleura of the expected intersegmental plane (Fig. 2). Planning was carried out using a superDimension system (Medtronic, Minneapolis, MN). The axial, coronal, and sagittal views of the CT image were used for optimal planning. If a bronchiole did not lead directly to the target, the best available exit point from the bronchial tree was used.
Figure 2.
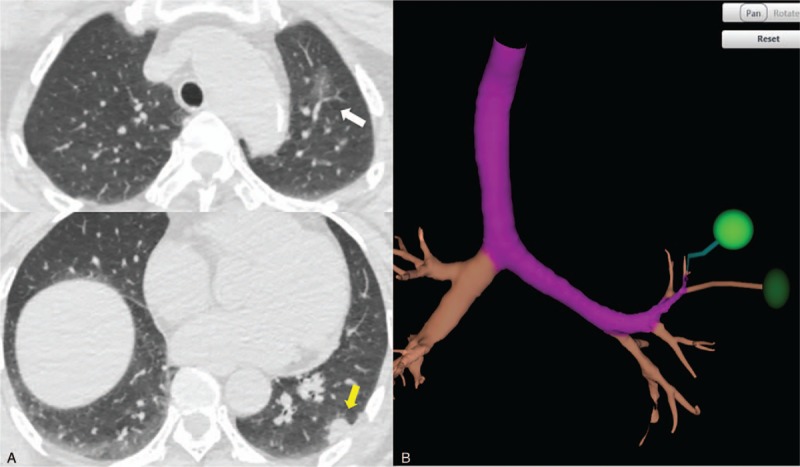
(A) Computed tomography images of nondominant subsolid nodule in the left upper lobe (white arrow) and dominant nodule in the left lower lobe (yellow arrow). (B) Planning map showing 2 marking targets for the nodule in the left upper lobe (green balls).
General anesthesia was induced using a single-lumen endotracheal tube. The ENB procedure was undertaken in supine position. A fiberoptic bronchoscope with a working channel of diameter 2.8 mm (BF-1T260; Olympus, Tokyo, Japan) and a guide-sheath with an external diameter of 2.7 mm were used for locatable guide. The tip of the guide-sheath had an angle of 45°, 90°, or 180° and the surgeon chose the appropriate angle. After completing the navigation to the target, the locatable guide was removed from the sheath and a catheter for dye injection were inserted through the sheath. After injection of indigo carmine (0.5–1 mL) to the target, endotracheal tube was changed to a double-lumen tube and thoracoscopic resection was performed in lateral decubitus position. Dye marks were identified thoracoscopically and the lesion was resected by wedge resection or segmentectomy. Depending on the frozen examination findings and the radiologic features, additional segmentectomy or lobectomy with lymph node dissection was undertaken.
2.3. Statistical analyses
Statistical analyses were undertaken using R 2008 (R Foundation for Statistical Computing, Vienna, Austria). Success of localization was defined as visible dye-mark on the lung surface. Accuracy of navigation was represented by the target distance. Continuous variables are described using the mean ± standard deviation. Categorical variables are expressed using counts and percentages. Three groups divided according to nodule location were compared with respect to demographic and clinical features using frequency tests for categorical variables and one-way analysis of variance for continuous variables. Linear regression was utilized to determine the relationships between the patients’ variables and endpoints (target distance). Among the significant variables on the regression model, approach angle was selected for further categorization. We divided the patients into 3 groups, according to their approach angle on the planning map (<45°; 45–90°; ≥90°) and post-hoc analysis was performed. After univariate analysis, variables with a P = .20 were selected for multivariate analysis. Navigation time was also chosen for multivariate analysis because this variable is clinically important and could have an effect on primary outcome (navigation accuracy). Multiple linear regression analyses were carried out to identify the impact of navigation-associated variables on the accuracy (target distance) of ENB with age, navigation time and engagement failure used as adjustment variables. P values <.05 was considered significant.
3. Results
Twenty patients underwent ENB-guided dye-localization for 24 sub-solid nodules. There were 6 men and 14 women and the median age was 62.5 years. According to the recommendation of Naidich et al[9] at multiple subsolid nodules, 6 nodules were dominant lesion and 18 nodules were nondominant lesion. Eighteen (75%) nodules were pure ground-glass nodules (GGNs) and 6 nodules were part-solid GGNs. The median nodule size was 6.9 (range, 3.5–25.7) mm. The median distance from the pleural surface was 6.9 (range, 0.8–26.6) mm.
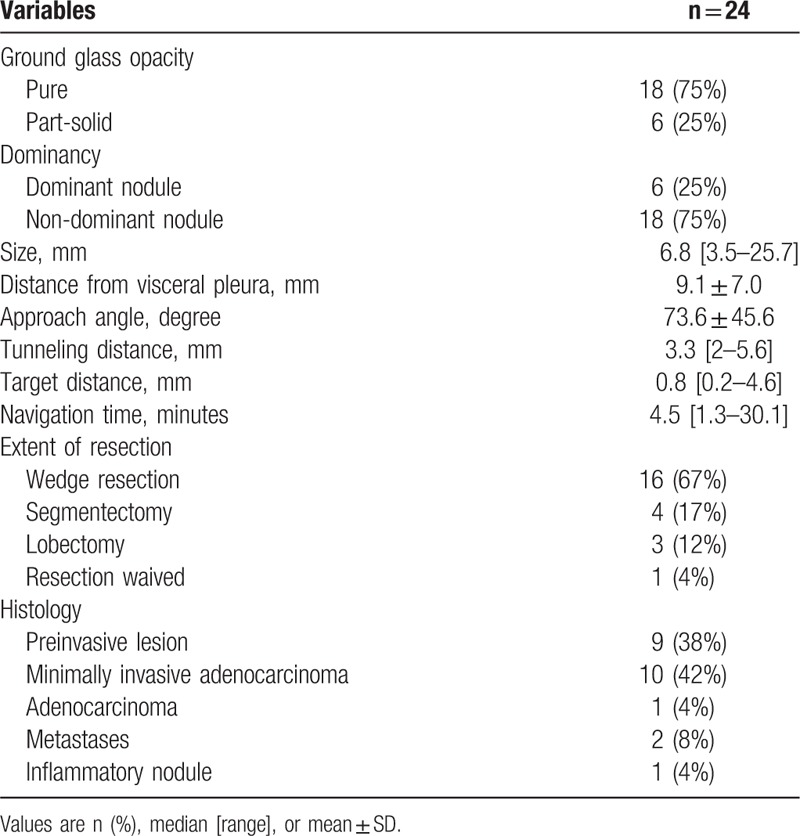
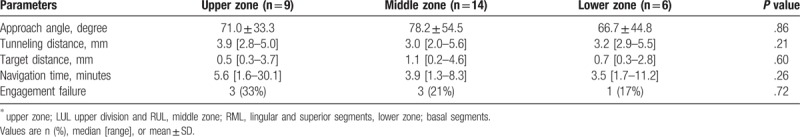
The median navigation time was 4.5 minutes (range, 1.3–30.1) (Table 1). Twenty-nine markings were performed for 24 nodules. Five nodules were localized with 2 dye-markings for better identification and one of which was set on the expected segmental plane.
Table 1.
Characteristics of nodules and navigation outcomes.
Success rate of dye-marking (visible dye-marker in thoracoscopy) was 93.1% (27/29). Two dye markers were not visible since the dye was injected far away from visceral pleura. Overall, localization by dye marking was successful in 95.8% nodules (23/24). The nodule that was not localized by dye marking was identified by manual palpation. Twenty-three nodules were resected successfully by thoracoscopic surgery. A 6 mm sized right middle lobe pure GGN in a patient who simultaneously underwent right lower lobectomy and wedge resection of right upper lobe for synchronous invasive adenocarcinomas was not resected to save pulmonary function.
For frozen-section diagnosis, 20 wedge resections and 3 segmentectomies were performed. Twenty nodules were primary lung tumors. The remaining 2 nodules were pulmonary metastases from other organs and one nodule was inflammatory nodule. Primary lung tumors comprised 9 preinvasive lesions and 11 invasive lesions for lung adenocarcinomas. Additional anatomic resection was performed in 6 primary lung tumors (Fig. 3). Complete resection was achieved in all lesions. There were no ENB-related complications such as pneumothorax and endobronchial bleeding. An operation-related complication (chylothorax) occurred in one patient. There were neither conversions to thoracotomy nor operative mortality.
Figure 3.
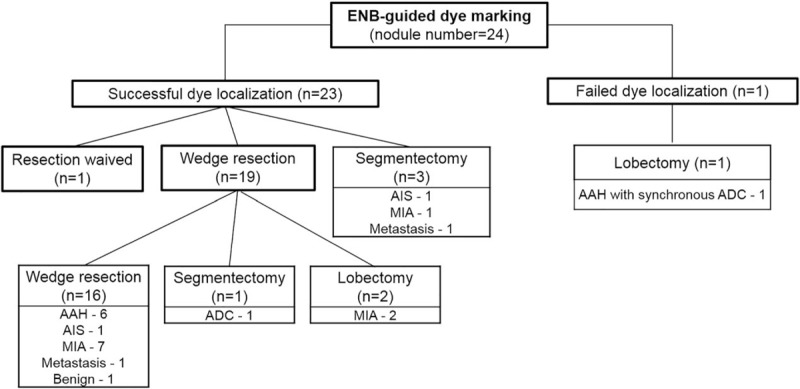
Flow diagram of surgery for 24 subsolid nodules. ADC = adenocarcinoma, MIA = minimally invasive adenocarcinoma, AIS = adenocarcinoma in situ, AAH = atypical adenomatous hyperplasia.
According to the zone categorization, the locations of marking targets were 9 in the upper zone, 14 in the middle zone, and 6 in the lower zone. Three groups were not different with respect to demographic or planning variables (including approach angle and tunneling distance) (Table 1). The median target distance was 0.8 (range, 0.2–4.6) mm and did not show a significant inter-zone difference (P = .60) (Table 2).
Table 2.
Navigation outcomes according to the target location∗ (n = 29, markings).
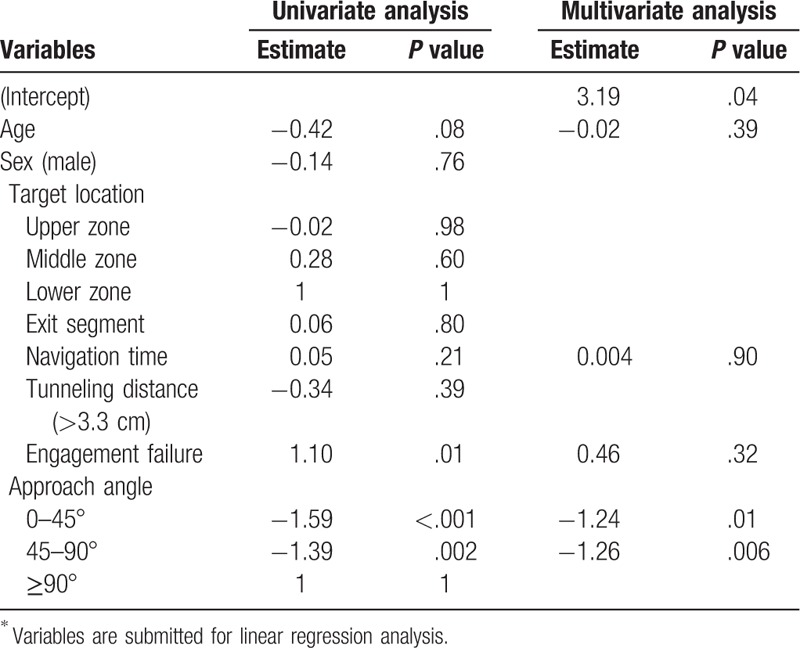
3.1. Factors affecting navigation accuracy
There were positive correlations between the approach angle and target distance (r = 0.64; P = .001) and between engagement failure and target distance (r = 0.46; P = .013). According to the analysis of the 3 subgroups based on approach angle (<45°; 45–90°; ≥90°), a cut-off value of 90° was determined to be the most significant cut-off angle for navigation accuracy. These positive correlations were also significant in a multivariate model using the navigation time and engagement failure as independent variables (Table 3).
Table 3.
Factors∗ for navigation accuracy (target distance).
4. Discussion
The present study showed that ENB-guided dye marking for thoracoscopic resection of small subsolid nodules was an effective and safe method and the approach angle was an important factor for the accuracy of ENB navigation.
Thoracoscopic surgery for solitary or multiple subsolid nodules is increasing due to increasing use of low-dose CT screening.[1–3] In cases with multiple subsolid nodules in which a dominant lesion can be identified, the dominant lesion determines further management.[9] However, most patients with lung cancer who present with multiple nodules, particularly multiple GGNs or part-solid lesions, actually have synchronous primary carcinomas. Accumulating surgical data favors aggressive treatment of these patients because their survival is comparable to that of patients with solitary lung cancers of comparable stage.[10,11] Judging from this, in patients with multiple lesions in whom surgery is indicated, VATS sublobar resections for nondominant lesions in the same side should be considered given recent documentation of long-term survival following multiple sublobar resections.[12,13]
However, thoracoscopic identification of small subsolid nodules is challenging, which makes preoperative localization crucial.[8] Several methods have been described to localize pulmonary nodules.[4,14,15] Notwithstanding several disadvantages, CT-guided placement of hook wires is the most popular method. Chen et al[16] reported that pneumothorax rate was 23% and wire dislodgement rate was 4.9%. Apart from the concerns of radiation exposure during localization procedure, patients are susceptible to having discomfort while undergoing procedure, being transported to surgical unit, and waiting for induction of anesthesia. Thus, a safer and more convenient method is required.
ENB is an image-based virtual endobronchial technology that facilitates approaching peripheral lung lesions, which are difficult to access with conventional bronchoscopy.[5] Efficiency of ENB navigation have been verified by several studies. In the NAVIGATE study with 1000 patients, success rate of ENB-guided biopsy was 91.8% (1038/1129 nodules).[17] ENB-guided dye marking also have been increasingly applied for the localization of pulmonary nodules.[6–8] Success rates of ENB-guided dye marking are higher than those of ENB-guided biopsy because on-target marking is not always necessary for localization. When doing a biopsy, the distance of nodule to pleura is important to reach the nodule by navigation, but this is not the case with dye marking. Likewise, an airway going right into the nodule on the CT scan (positive bronchus sign) makes the nodule accessible to ENB and improves diagnostic yield in transbronchial biopsy technique,[18] the bronchus sign does not gain any significance in dye localization. By setting marking targets at the nearest pleura from the nodule, the success of localization is higher and not in relation with the distance of nodule to pleura nor the bronchus sign. Average navigation accuracy of ENB was 5.7 mm in a study[5] and such degree of misaiming would not erode the success rate of localization. Awais et al[7] reported 100% (33/33) of success rate of ENB-guided dye marking for thoracoscopic resection of small pulmonary nodules. Marino et al[6] reported 97.2% (70/72) of accuracy and 2 nodules that were not localized by dye marking were identified by palpation. In the present study, 93.1% of dye markings were successful. Two out of 29 markings were unsuccessful owing to the deeply injected dye from the pleural surface. However, we were able to increase the success rate of localization to 95.8% by multiple dye markings.
There are several advantages of ENB-guided dye marking compared with CT-guided techniques. The first advantage is its superior safety. The reported pneumothorax rates were about tenfold lower than that of CT-guided transthoracic approaches.[19,20] Pooled pneumothorax rate in studies using ENB-guided dye marking was 0% and none of the studies reported bronchopulmonary hemorrhage.[6–8,21,22] We also did not experience bronchial hemorrhage nor pneumothorax in 29 dye injections, and ENB procedure did not compromise subsequent thoracoscopic surgery. If any, localization followed immediately by surgery could mitigates adverse effects of potential complications. Second benefit is the comfort of patient. As ENB-guided localization is performed under general anesthesia in the operation room, patients do not feel discomfort or anxiety during localization procedure and waiting period up until the induction of general anesthesia. The other advantage lies in efficiency of the procedure and entire work flow. The process and personnel for the transportation of the patient from localization unit to the operation room are not necessary in intraoperative ENB-guided dye marking. Bolton et al[21] reported that ENB-guided localization significantly reduced the waiting time compared with CT-guided localization (27 vs 189 minutes, P = .001).
4.1. Factors influencing the navigation accuracy
The planning of ENB navigation procedure involves three-dimensional location of the nodule using CT images. A bronchiole exit point is determined by operating personnel and a navigation software-generated tunneled pathway is created from that exit point. Hence, performance of ENB procedure depends on the planning strategy for the navigation pathway.
In our study, the approach angle was a significant predictor of the navigation accuracy. Thus, choosing a navigation pathway approaching the target at a smaller angle would make the target more accessible and improve the accuracy of ENB. However, anatomical limitation in some cases would make large approach angle inevitable and our study showed wide range of approach angle. Bronchoscopic transparenchymal nodule access (BTPNA) was developed to overcome this limitation.[23] A hole is made by a coring needle and balloon dilator, and navigation is performed through this hole. Since the transparenchymal pathway is created with smaller target angle from the artificial bronchiole exit, BTPNA could provide more accurate target localization.
Bolton and colleagues[24] reported a wide range of procedure duration of the ENB-localization (17 to 40 minutes). The present study also showed a wide range of navigation time (1.3–30.1 minutes). This finding suggests difficulties in approaching certain bronchial branches of interest. The navigation time was longer for targets in the upper zone compared with those in middle or lower zones while the target distance remained relatively constant. This result suggests that targets in the upper zone is less accessible due to the acute angle of the corresponding bronchus.[25]
Another factor that influences navigation accuracy of ENB is respiratory movement. Average motion of pulmonary lesions from full inspiration to end-exhalation during tidal volume breathing was 17.6 mm and lower lobe lesions moved significantly more than upper lobe lesions in a study.[25] This observation implies that control of respiratory movements would enhance the accuracy of ENB navigation. Therefore, general anesthesia is preferred during ENB. In Navigate study, 80% of ENB were performed under general anesthesia.[17] A meta-analysis showed that the diagnostic yield at bronchoscopic biopsy was better with the use of general anesthesia than with sedation.[20] In this regard, intraoperative ENB-guided localization performed under paralytic general anesthesia and controlled ventilation would be more effective than other localization methods.
Fluoroscopic guidance might increase the navigation accuracy of ENB by helping guide the deployment of the needle near the pleura. However, fluoroscopy is a time-consuming and inconvenient modality and results in radiation exposure of surgical team and patients.[26] Thus, we carried out ENB-guided dye marking without fluoroscopic assistance. To compensate the absence of fluoroscopic guidance, we set multiple targets for a single nodule and did multiple marking to increase the success rate of localization.
4.2. Limitations
The present study was limited by its retrospective nature of data collection and selection bias in that the navigating method was dependent on the operating personnel. Since ENB has a considerable learning curve, producing an increasing diagnostic yield with increasing experience,[27,28] interpersonnel differences in navigating skills may exist. We limited the number of operating personnel to 2 surgeons to offset this potential selection bias. Our study was also limited by the small size of the comparison groups. Statistical significance of navigation time among zones was probably absent. In addition, the present study was our initial experience; large numbers of target planning should be expanded in the future and with more patients on ENB localization, we should be able to evaluate the accuracy and efficacy of ENB fully.
5. Conclusions
ENB-guided dye marking is a safe and efficient modality for the localization of small subsolid pulmonary nodules in thoracoscopic sublobar resection. To increase the accuracy of navigation, smallest approach angle should be selected when planning the navigation route. More experience at setting the target and selecting the catheter angle is necessary to enhance the accuracy of ENB-guided dye-localization and to standardize the procedure.
Author contributions
Conceptualization: In Kyu Park, Kwanyong Hyun
Data curation: In Kyu Park, Chang Hyun Kang, Young Tae Kim
Formal analysis: Kwanyong Hyun, Jae Won Song, In Kyu Park.
Investigation: Kwanyong Hyun, Jae Won Song
Methodology: In Kyu Park, Samina Park, Jae Won Song.
Project administration: Jae Won Song, Samina Park
Resources: In Kyu Park, Chang Hyun Kang, Young Tae Kim, Samina Park
Software: Kwanyong Hyun
Supervision: In Kyu Park, Chang Hyun Kang, Young Tae Kim
Validation: Samina Park, Young Tae Kim
Visualization: Kwanyong Hyun
Writing – original draft: Kwanyong Hyun, Jae Won Song, In Kyu Park
Writing – review & editing: Kwanyong Hyun, In Kyu Park
Kwanyong Hyun orcid: 0000-0002-2103-3122.
Supplementary Material
Footnotes
Abbreviations: AAH = atypical adenomatous hyperplasia, ADC = adenocarcinoma, AIS = adenocarcinoma in situ, CT = computed tomography, ENB = electromagnetic navigation bronchoscopy, GGN = ground-glass nodule, MIA = minimally invasive adenocarcinoma.
The authors have no funding and no conflicts of interest to disclose.
Supplementary Figures:.
Supplemental Digital Content is available for this article.
References
- [1].Henschke CI, Yankelevitz DF, Mirtcheva R, et al. CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol 2002;178:1053–7. [DOI] [PubMed] [Google Scholar]
- [2].Aberle DR, Adams AM, et al. National Lung Screening Trial Research T. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].MacMahon H, Naidich DP, Goo JM, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology 2017;284:228–43. [DOI] [PubMed] [Google Scholar]
- [4].Zaman M, Bilal H, Woo CY, et al. In patients undergoing video-assisted thoracoscopic surgery excision, what is the best way to locate a subcentimetre solitary pulmonary nodule in order to achieve successful excision? Interact Cardiovasc Thorac Surg 2012;15:266–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Schwarz Y, Greif J, Becker HD, et al. Real-time electromagnetic navigation bronchoscopy to peripheral lung lesions using overlaid CT images: the first human study. Chest 2006;129:988–94. [DOI] [PubMed] [Google Scholar]
- [6].Marino KA, Sullivan JL, Weksler B. Electromagnetic navigation bronchoscopy for identifying lung nodules for thoracoscopic resection. Ann Thorac Surg 2016;102:454–7. [DOI] [PubMed] [Google Scholar]
- [7].Awais O, Reidy MR, Mehta K, et al. Electromagnetic navigation bronchoscopy-guided dye marking for thoracoscopic resection of pulmonary nodules. Ann Thorac Surg 2016;102:223–9. [DOI] [PubMed] [Google Scholar]
- [8].Luo K, Lin Y, Lin X, et al. Localization of peripheral pulmonary lesions to aid surgical resection: a novel approach for electromagnetic navigation bronchoscopic dye marking. Eur J Cardiothorac Surg 2017;52:516–21. [DOI] [PubMed] [Google Scholar]
- [9].Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 2013;266:304–17. [DOI] [PubMed] [Google Scholar]
- [10].Finley DJ, Yoshizawa A, Travis W, et al. Predictors of outcomes after surgical treatment of synchronous primary lung cancers. J Thorac Oncol 2010;5:197–205. [DOI] [PubMed] [Google Scholar]
- [11].Vazquez M, Carter D, Brambilla E, et al. Solitary and multiple resected adenocarcinomas after CT screening for lung cancer: histopathologic features and their prognostic implications. Lung Cancer 2009;64:148–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kohno T, Fujimori S, Kishi K, et al. Safe and effective minimally invasive approaches for small ground glass opacity. Ann Thorac Surg 2010;89:S2114–7. [DOI] [PubMed] [Google Scholar]
- [13].Mun M, Kohno T. Efficacy of thoracoscopic resection for multifocal bronchioloalveolar carcinoma showing pure ground-glass opacities of 20 mm or less in diameter. J Thorac Cardiovasc Surg 2007;134:877–82. [DOI] [PubMed] [Google Scholar]
- [14].Sortini D, Feo C, Maravegias K, et al. Intrathoracoscopic localization techniques. Review of literature. Surg Endosc 2006;20:1341–7. [DOI] [PubMed] [Google Scholar]
- [15].Khereba M, Ferraro P, Duranceau A, et al. Thoracoscopic localization of intraparenchymal pulmonary nodules using direct intracavitary thoracoscopic ultrasonography prevents conversion of VATS procedures to thoracotomy in selected patients. J Thorac Cardiovasc Surg 2012;144:1160–5. [DOI] [PubMed] [Google Scholar]
- [16].Chen S, Zhou J, Zhang J, et al. Video-assisted thoracoscopic solitary pulmonary nodule resection after CT-guided hookwire localization: 43 cases report and literature review. Surg Endosc 2011;25:1723–9. [DOI] [PubMed] [Google Scholar]
- [17].Khandhar SJ, Bowling MR, Flandes J, et al. Electromagnetic navigation bronchoscopy to access lung lesions in 1,000 subjects: first results of the prospective, multicenter NAVIGATE study. BMC Pulm Med 2017;17:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Seijo LM, de Torres JP, Lozano MD, et al. Diagnostic yield of electromagnetic navigation bronchoscopy is highly dependent on the presence of a Bronchus sign on CT imaging: results from a prospective study. Chest 2010;138:1316–21. [DOI] [PubMed] [Google Scholar]
- [19].Eberhardt R, Morgan RK, Ernst A, et al. Comparison of suction catheter versus forceps biopsy for sampling of solitary pulmonary nodules guided by electromagnetic navigational bronchoscopy. Respiration 2010;79:54–60. [DOI] [PubMed] [Google Scholar]
- [20].Gex G, Pralong JA, Combescure C, et al. Diagnostic yield and safety of electromagnetic navigation bronchoscopy for lung nodules: a systematic review and meta-analysis. Respiration 2014;87:165–76. [DOI] [PubMed] [Google Scholar]
- [21].Bolton WD, Cochran T, Ben-Or S, et al. Electromagnetic navigational bronchoscopy reduces the time required for localization and resection of lung nodules. Innovations (Phila) 2017;12:333–7. [DOI] [PubMed] [Google Scholar]
- [22].Brown J, Lee TJ, Joiner T, et al. Using electromagnetic navigation bronchoscopy and dye injection to aid in video-assisted lung resection. Am Surg 2016;82:1052–4. [PubMed] [Google Scholar]
- [23].Herth FJ, Eberhardt R, Sterman D, et al. Bronchoscopic transparenchymal nodule access (BTPNA): first in human trial of a novel procedure for sampling solitary pulmonary nodules. Thorax 2015;70:326–32. [DOI] [PubMed] [Google Scholar]
- [24].Bolton WD, Howe H, 3rd, Stephenson JE. The utility of electromagnetic navigational bronchoscopy as a localization tool for robotic resection of small pulmonary nodules. Ann Thorac Surg 2014;98:471–5. discussion 475-476. [DOI] [PubMed] [Google Scholar]
- [25].Chen A, Pastis N, Furukawa B, et al. The effect of respiratory motion on pulmonary nodule location during electromagnetic navigation bronchoscopy. Chest 2015;147:1275–81. [DOI] [PubMed] [Google Scholar]
- [26].Jain P, Fleming P, Mehta AC. Radiation safety for health care workers in the bronchoscopy suite. Clin Chest Med 1999;20:33–8. ix-x. [DOI] [PubMed] [Google Scholar]
- [27].Bansal S, Hale K, Sethi S, et al. Electromagnetic navigational bronchoscopy: a learning curve analysis. Chest 2007;132:514B. [Google Scholar]
- [28].Port J, Harrison S. Electromagnetic navigational bronchoscopy. Semin Intervent Radiol 2013;30:128–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


