Abstract
To assess the clinical effect of miniaturized percutaneous nephrolithotomy (MPCNL) and flexible ureteroscopy lithotripsy (FURL) for the treatment of renal and proximal ureteral calculi of ≤2 cm.
A retrospective analysis was carried out on clinical data of 106 patients with kidney or upper urethral calculi. Among these patients, 58 underwent the MPCNL, and 48 received FURL. Stone-free rates, operating time, blood loss, hemoglobin drop, length of hospital stay, complications, and renal damage indexes were compared.
The stone removal rates of the FURL and MPCNL groups were 81.25% versus 87.93% (p > .05). Although operating time was significantly shorter in the MPCNL group, hospital stays were significantly shorter in the FURL group. In addition, pooled analysis showed that mean estimated blood loss was significantly higher in the PCNL group but the hemoglobin decline of the FURL group and PCNL group had no significant difference. The PCNL group had no significant difference in complications compared to the FURL group. Differences on the creatinine levels and urea nitrogen levels before the operation and after the operation were not statistically significant.
FURL is an effective method for treating renal stone. FURL not only had a similar stone-free rate as compared to MPCNL but also was associated with less blood loss and more favorable recovery time. However, FURL had a longer operative time.
Keywords: efficacy, flexible ureteroscopy lithotripsy, kidney stone, percutaneous nephrolithotomy
1. Introduction
Urinary calculus is a common medical problem, with a prevalence of about 2% to 3% in the general population. Kidney stone accounted for 80% to 90% of all urinary calculi with high recurrence risk.[1,2] It was associated with many factors such as malnutrition, metabolic abnormalities, and environmental and dietary factors. More patients are presenting with small renal calculi.[3] The kidney stone can cause pain, blood in the urine, infection, impaired renal function, and kidney failure.[4] When these symptoms occurred, treatment is usually required. With the goal of making the patient stone free with minimal complications, treatment options for ≤2 cm renal stones have shifted from open surgery to minimally invasive surgery, including extracorporeal shock wave lithotripsy (ESWL), percutaneous nephrolithotomy (PCNL) and flexible ureteroscopy lithotripsy (FURL) alone or in combination.[5] Due to the limitations of the success rate and the complications of ESWL, other minimally invasive modalities for kidney stones such as PCNL and FURL are widely used. The 2013 European Association of Urology guidelines recommend PCNL and FURL as the first-line treatment for lower pole stones when anatomic factors make ESWL unfavorable.[6] However, for the PCNL, its higher stone-free rates are counterbalanced by the risk of complications. With improvements in technology, this situation is further promoted by the introduction of Mini-PCNL (MPCNL), which adopted the smaller tract access (≤22F)[7] and ensured less postoperative morbidity when compared with conventional PCNL due to the miniaturized tract access. And another an alternative to the conventional percutaneous approaches is provided by FURL. It is extremely effective for stones that are ≤2 cm in diameter and complex kidney stones.[8] FURL could also be considered for elderly patients, patients with hemorrhagic disorders, which were not suitable for ESWL or PCNL.[9,10] The purpose of this study was to evaluate and compare the efficacy and safety of FURL and MPCNL for the treatment of renal and proximal ureteral calculi of ≤20 mm
2. Patients and methods
A retrospective study of 106 patients was included with renal or upper urethral calculi who underwent MPCNL or FURL in China-Japan Friendship Hospital from July 2013 to January 2018. For the present study, in lieu of formal approval from the ethical committee, the principles of the Declaration of Helsinki were followed. Written informed consent was obtained from all patients for their data to be used for research purposes. Inclusion criteria included: age ≥18 years and a renal or proximal ureter stone (single or multiple) of no ≤2 cm in diameter on preoperative abdominal computed tomography (CT). Follow-up data should be complete with adequate postoperative checkups. The exclusion criteria included: the patients combined with abnormal renal anatomy, uncorrected coagulopathy, previous renal surgery history, solitary kidney, severe urinary infection or tuberculosis, and severe cardiac and pulmonary dysfunction, and concomitant stones at other sites (eg, bladder, mid, or distal ureter). The selection of procedural technique was primarily based on the patients’ choice. Among these patients, 58 had an MPCNL and 48 received a FURL. The procedures were performed by the well-experienced urologists (ZG, TYW) according to the standard steps as described below.
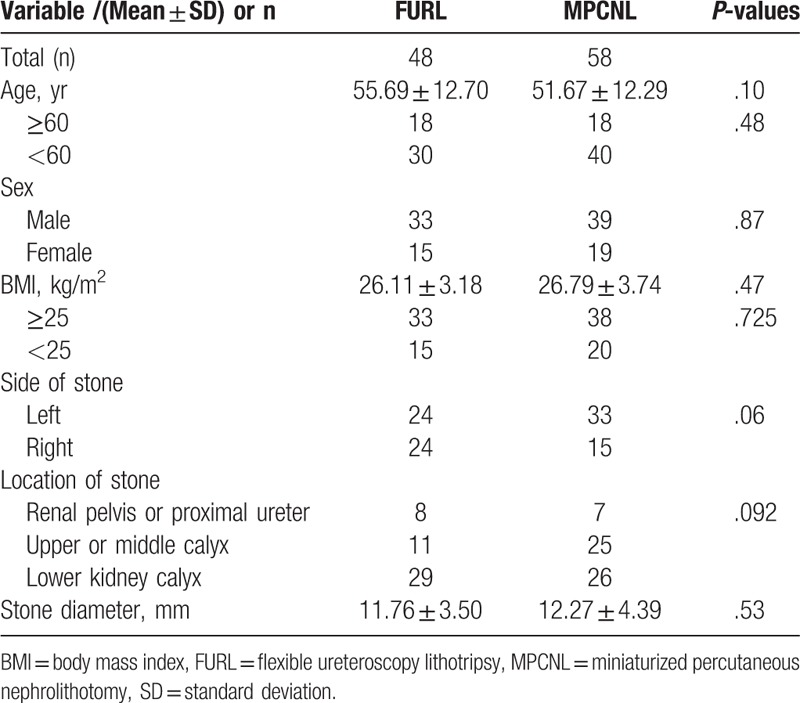
In order to compare the feasibility and outcomes of the 2 methods, we retrospectively reviewed the medical records and all relevant data. Detailed demographic characteristics and clinical data are described in Table 1. The follow-up period was defined as the time from the date of surgery to the latest follow-up.
Table 1.
Clinical data and perioperative data comparison between FURL and MPCNL group.
3. Surgical procedures
In the FURL group, all patients were successfully managed by FURL. Under general anesthesia, patients were placed in the lithotomy position. An 8/9.8F Wolf rigid ureteroscope was inserted through the urine tract under direct vision. It was followed by removing the D-J tube if it was placed preoperatively. Next, the ureterostoma of the affected side was located to insert the super smooth guide wire. The ureteroscope was inserted along with the super smooth guidewire to observe and dilate the ureter and then the ureteroscope was removed. Subsequently, the flexible ureteroscope sheath (12/14F) was placed into the affected side ureter along the guide wire. The flexible ureteroscope (Olympus, Japan) with a 200 um laser fiber was advanced through the sheath. The holmium laser was applied as an energy source set at 1/1.2 J and at a rate of 10 Hz. The stones were fragmented with a holmium laser until they were deemed small enough to pass spontaneously. After laser lithotripsy, the renal pelvis and renal calyx were examined for any abnormality, and then the D-J tube (4.8 or 5F) was inserted. After the operation, the patients were treated with conventional antibiotics and took plain film of kidney-–ureter–bladder (KUB), ultrasound or CT within three days and one month to observe stone breakage and location of the D-J tube. The D-J tube was removed after 2 to 4 weeks.
In the MPCNL group, under general anesthesia, in the lithotomy position, a ureteric catheter (5F) was inserted into to the target renal pelvis under cystoscopy vision. Then the patients were placed in the prone position. The abdomen at the renal region was raised and a puncture site was made. A percutaneous access was achieved by a urologist under the guidance of Doppler ultrasonography using a puncture needle and guidewire. Subsequently, the dilatation of the percutaneous tract was formed using serial fascial dilators (6–16F) until a peel-away sheath (16 or 20F) was retained in the percutaneous access. Thereafter, a rigid ureteroscope was inserted into the guidewire under direct vision. The stones were fragmented by a pneumatic or holmium laser. After the operation, a D-J (5 or 6F) ureteric stent was left and the silicone nephrostomy tube was placed in the PCNL channel for drainage.
The coprimary endpoints of the present study were stone removal rate. The differences in operation time, blood loss, hemoglobin drop, hospital stay, complication incidence, creatinine level, urea nitrogen level of the 2 groups were compared. The stone removal rate referred to no retained stones found or the fragments of retained stone of a size of ≤4 mm and free from any clinical symptoms under KUB, ultrasound or CT examination 1 month after the operation.
The data were computerized using SPSS 23.0 for Windows (IBM, Chicago). Categorical data were examined using the Chi-square test and the continuous variable was assessed using the independent sample t test. p < .05 was considered to indicate a statistically significant difference.
4. Results
One hundred six patients met the criterion were included in this study. No significant difference had been found regarding age, sex, body mass index, side of stone (left or right), location of stone (renal pelvis or proximal ureter, upper or middle calyx, lower calyx) and stone diameter between FURL and MPCNL groups. The operation was successfully completed in all cases with no conversion to open surgery.
Comparison of the stone free rate. Within 3 days and 1 month after the operation, the stone free rate of the FURL and MPCNL group was 72.92% versus 84.48% and 81.25% versus 87.93%, respectively, and had no significant difference in 2 groups (p > .05). According to the subgroup analysis, the difference in the different location of kidney calyx also had no significant difference, as shown in Table 2.
Table 2.
Analysis of the results for the 106 patients who were followed up.
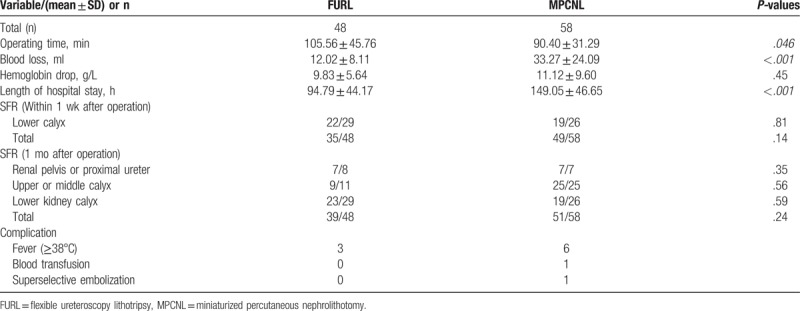
Comparison of operation time, blood loss, hemoglobin drop, hospital stay. Mean operation times were shorter in the MPCNL group than those in the FURL group, (90.40 ± 31.29 minutes vs 105.56 ± 45.76 minutes; p < .05). Mean estimated blood loss was significantly higher in the MPCNL group than that in the FURL group (33.27 ± 24.09 ml vs 12.02 ± 8.11 ml; p < .001). However, there was no significant difference in mean hemoglobin drop in both group for FURL and MPCNL groups, (9.83 ± 5.64 g/L vs 11.12 ± 9.60 g/L; p > .05). The mean total length of hospitalization was significantly shorter in the FURL group (94.79 ± 44.17 hours vs 149.05 ± 46.65 hours; p < .001), as shown in Table 2
Comparison of complications. The minor complication rate for the FURL group was 6.25% and 13.7% for the PCNL group according to the modified Clavien-Dindo classification system. Complication in PCNL group included six cases of fever, one case blood transfusion, and one superselective embolization. In the FURS group, complications included three cases of fever. No other seemingly intraoperative or postoperative complications were observed.
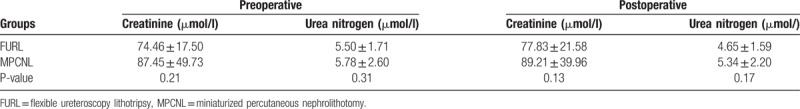
Comparison of renal damage indexes. Differences on the creatinine levels and urea nitrogen levels before the operation, after the operation between the two groups were not statistically significant (p > .05), as shown in Table 3.
Table 3.
Analysis of renal damage index for the patients who were followed up.
5. Discussion
Renal stone is one of the three common diseases in urology, and accounts for 80% to 90% of all urinary calculi and more patients are presenting with small renal calculi.[11,12] For small renal calculi, the currently available management options include ESWL, standard PCNL, and FURL.[6] The drawbacks of ESWL is that the stone clearance rate is relatively low and requires repeated treatment, especially for the harder stones or the stone in lower pole.[4] PCNL and FURL are superior to ESWL in terms of stone clearance rates.[13] Although PCNL has good stone clearance rates it is associated with a significant risk of morbidity, such as bleeding (7.8%), renal pelvis perforation (3.4%), hydrothorax (1.8%), and blood transfusion (5.7%).[14] Minimally invasive PCNL (MPCNL), which is modified PCNL using a miniature endoscope by way of a small access tract, could reduce the risk of conventional PCNL. For the FURL, it can minimize the risks associated with percutaneous renal surgery, and stone-free rates were comparable with those obtained by PCNL.[15] Different studies have been carried out to explore the clinical effects of FURL and MPNCL for the treatment of kidney stones, but the results were contradictory and relatively few studies were performed to assess the efficiency for the stone of ≤2 cm. This study observed and analyzed the clinical effect of MPCNL and FURL in the treatment of kidney or upper urethral calculi of ≤2 cm in diameter.
When considering the stone-free rate, it is often regarded as the key index to evaluate the efficacy of a stone surgical procedure for the treatment of patients with urinary stones. There was no statistically significant difference between the FURL group and the MPCNL group. However, the conclusions were not consistent some published studies that MPCNL has a better stone-free rate. But why did the conclusion vary to each investigator? After consulting relative literatures, the reason may be associated with the following factors. First, the size and location and the number of the stone made a difference on the stone-free rates. The stone clearance rate is relatively low for the larger stones or the stone in lower polar compared with other location. Second, Karakoyunlu et al[16] suggested that the reasons for this different stone clearance rate could be that the power of holmium laser has great influence on the stone removal rate. Besides, the definition of success rate some studies use was complete absence of fragments or residues <5 mm while it was complete absence of fragments or residues ≤4 cm. Bryniarski et al[17] suggested that urologists try to disintegrate larger fragments in lower calix with a flexible ureteroscope, but rarely with such equipment are urologists able to leave the kidneys without any stone debris, which is the main reason for failure of FURL when assessed one day after the procedure. However, MPNCL provides direct access to reach the lower calyx of the kidney. Netsch et al[18] found that preoperative ureteral stent placement is associated with a higher stone removal rate compared with non-stented patients for urinary calculi.
Total operative time was longer in patients who were treated with FURL compared with those in the MPCNL group in the present study. Akman et al[19] think that the application of semirigid ureteroscopy for visual assessment of the ureter in all patients contributes to the increase of FURL operative time. On the other hand, operative times critical due to the increased demand for blood transfusions in MPCNL. Moreover, operative times are strictly related to nuances of in the surgical technique and surgical experience. Chu et al[20] found that preoperative stent placement was associated with a decreased operative time and in patients with larger stone burdens of >1 cm. Sugihara et al[21] considered that there was a positive correlation between operative time and severe complications, and the relative risk of serious complications was 1.58 when the operation time exceeded 90 minutes.
Blood loss was higher in the MPCNL group compared with those in the FURL group. Renal hemorrhage is one of the most common and worrisome complications for the patients after percutaneous renal surgery,[22,23] and 1 patient in our study required blood transfusion. MPCNL required initial ultrasound or fluoroscopic access, guidewire placement, removal of the initial puncture needle, serial or single-step dilation of the tract, which might increase the risk of the possibility of tract bleeding.[24] In the FURL group, it retrogrades into ureter, renal pelvis, and calyx through the natural canal of human body, so the major complications, such as severe bleeding, ureteral avulsion, and perforation were at lower risk.
Our pooled data indicated that FURL had shorter hospital stay than MPCNL with a statistically significant difference. We hypothesized that one of the most important points affect the length of hospitalization was the existence of nephrostomy tube to drainage. Most patients in MPCNL group were hospitalized until nephrostomy tube was removed. Urinary leakage from the nephrostomy tract after the removal of the tube usually prolong the hospital stay. Akman et al[19] also take the factors such as the presence of diabetes, large stone burden, intercostal access, multiple accesses, impaired kidney function, and the use of the tubeless procedure into account. Shorter hospital stays, lower major complications and faster recovery and less invasiveness in FURL compared with MPCNL. Those differences are likely to benefit the patient in reducing costs.
Although no significant difference was found in complication rate, we noticed a relatively higher occurrence in the MPCNL group. Bozkurt et al[25] suggested that complications such as bleeding, renal pelvis perforation, hydrothorax, and blood transfusion are often the result of obtaining percutaneous access and the technique of stone removal. The tract size was attributed to many of the complications associated in MPCNL, and the loss of blood increases with the increasing of tract size.[22] The relatively lower occurrence of postoperative fever may be associated with the preoperative ureter dilation and successful ureteral access sheath placement with a resultant lower intrarenal pressure.[26] Preplaced stent, semirigid ureteroscopy to test the ureteral tightness and simultaneous placement with fluoroscope might prevent the ureteral injury. In the study of Karakoyunlu et al,[16] the most widespread complaint was pain, he thinks that it was not only related with D-J tube or residual stones in FURL, but also the bleeding and nephrostomy in MPCNL.
Differences on the creatinine and urea nitrogen levels before the operation, and after the operation between the 2 groups were not statistically significant, which indicated that patients tolerated MPCNL well. Moskovitz et al[27] used the single-photon emission CT which can measure dimercaptosuccinic acid uptake by the kidneys to evaluate the effect of PCNL on global and regional renal function in adult patients. It showed that the total functional volume of the treated kidney was slightly decreased while no significant alteration of global uptake was noted. However, a statistically significant decrease was revealed in the functional volume at the PCNL site of entry for the regional assessment. Li et al[8] mentioned that the cystatin C level of the FURL group was significantly higher than that of the PCNL group at three and seven days after the operation. KIM-1 was expressed in the early stage of renal function damage, which was positively correlated with the severity of renal tissue pathology and Cystatin C was a recognized index for the early evaluation of renal function injury.[28–30] It meant that the FURL caused less damage to the renal compared with the PCNL.
There were several limitations in our study. First, the study was retrospective in nature, so the potential selection bias cannot be ignored. Second, some patients underwent KUB or ultrasonography to assess the stone-free status, which are less accurate as compared to non-contrast CT. Moreover, it is difficult to represent the characteristics of patients in general for this single-center analysis. Finally, there were limits for the overall sample size and follow-up. Thus, further multicenter, randomized controlled trial with the long-term follow-up and a larger patient series in future would be needed to verify this outcome.
6. Conclusion
This study indicated that FURL is an effective method for treating renal stone. When compared with MPNCL, it not only has a similar stone-free rate, but also is associated with less blood loss, more favorable recovery time. But it has longer operative time. However, the findings of this study should be further confirmed by well-designed prospective RCTs with a larger patient series.
Author contributions
Conceptualization: Guan Zhang.
Data curation: Binbin Jiao, Meng Zhang, Xin Xu.
Formal analysis: Shicong Lai, Xin Xu, Guan Zhang.
Methodology: Binbin Jiao, Shicong Lai, Guan Zhang.
Software: Binbin Jiao, Meng Zhang, Tongxiang Diao.
Supervision: Guan Zhang.
Writing – original draft: Binbin Jiao.
Writing – review and editing: Binbin Jiao, Guan Zhang.
Footnotes
Abbreviations: CT = computed tomography, ESWL = extracorporeal shock wave lithotripsy, FURL = flexible ureteroscopy lithotripsy, KUB = plain film of kidney-–ureter–bladder, MPCNL = miniaturized percutaneous nephrolithotomy, PCNL = percutaneous nephrolithotomy, RCT = randomized controlled trial.
The authors declared that this study has received no financial support and there was no conflict of interest.
References
- [1].Moe OW. Kidney stones: pathophysiology and medical management. Lancet 2006;367:333–44. [DOI] [PubMed] [Google Scholar]
- [2].Portis AJ, Sundaram CP. Diagnosis and initial management of kidney stones. Am Fam Physician 2001;63:1329–38. [PubMed] [Google Scholar]
- [3].Taylor EN, Stampfer MJ, Curhan GC. Dietary factors and the risk of incident kidney stones in men: new insights after 14 years of follow-up. J Am Soc Nephrol 2004;15:3225–32. [DOI] [PubMed] [Google Scholar]
- [4].Srisubat A, Potisat S, Lojanapiwat B, et al. Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst Rev 2014;11:CD007044. [DOI] [PubMed] [Google Scholar]
- [5].Geavlete P, Multescu R, Geavlete B. Influence of pyelocaliceal anatomy on the success of flexible ureteroscopic approach. J Endourol 2008;22:2235–9. [DOI] [PubMed] [Google Scholar]
- [6].Türk C, Knoll T, Petrik A, et al. Guidelines on Urolithiasis. European Urological Association Web site. Available at: http://www.uroweb.org/gls/pdf/22%20Urolithiasis_LR.pdf Updated 2014. Accessed March 18, 2017. [Google Scholar]
- [7].Zeng G, Zhu W, Lam W. Miniaturised percutaneous nephrolithotomy: its role in the treatment of urolithiasis and our experience. Asian J Urol 2018;5:295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Li ZG, Zhao Y, Fan T, et al. Clinical effects of FURL and PCNL with holmium laser for the treatment of kidney stones. Exp Ther Med 2016;12:3653–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hassan M, El-Nahas AR, Sheir KZ, et al. Percutaneous nephrolithotomy vs. extracorporeal shockwave lithotripsy for treating a 20-30 mm single renal pelvic stone. Arab J Urol 2015;13:212–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bagcioglu M, Demir A, Sulhan H, et al. Comparison of flexible ureteroscopy and micropercutaneous nephrolithotomy in terms of cost-effectiveness: analysis of 111 procedures. Urolithiasis 2016;44:339–44. [DOI] [PubMed] [Google Scholar]
- [11].Dwyer ME, Krambeck AE, Bergstralh EJ, et al. Temporal trends in incidence of kidney stones among children: a 25-year population based study. J Urol 2012;188:247–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Marickar YM, Vijay A. Female stone disease: the changing trend. Urol Res 2009;37:337–40. [DOI] [PubMed] [Google Scholar]
- [13].El-Nahas AR, Ibrahim HM, Youssef RF, et al. Flexible ureterorenoscopy versus extracorporeal shock wave lithotripsy for treatment of lower pole stones of 10-20 mm. BJU Int 2012;110:898–902. [DOI] [PubMed] [Google Scholar]
- [14].De la Rosette J, Assimos D, Desai M, et al. The clinical research office of the endourological society percutaneous nephrolithotomy global study: indications, complications, and outcomes in 5803 patients. J Endourol 2011;25:11–7. [DOI] [PubMed] [Google Scholar]
- [15].Chung BI, Aron M, Hegarty NJ, et al. Ureteroscopic versus percutaneous treatment for medium-size (1-2-cm) renal calculi. J Endourol 2008;22:343–6. [DOI] [PubMed] [Google Scholar]
- [16].Karakoyunlu N, Goktug G, Şener NC, et al. A comparison of standard PCNL and staged retrograde FURS in pelvis stones over 2 cm in diameter: a prospective randomized study. Urolithiasis 2015;43:283–7. [DOI] [PubMed] [Google Scholar]
- [17].Bryniarski P, Paradysz A, Zyczkowski M, et al. A randomized controlled study to analyze the safety and efficacy of percutaneous nephrolithotripsy and retrograde intrarenal surgery in the management of renal stones more than 2 cm in diameter. J Endourol 2012;26:52–7. [DOI] [PubMed] [Google Scholar]
- [18].Netsch C, Knipper S, Bach T, et al. Impact of preoperative ureteral stenting on stone-free rates of ureteroscopy for nephroureterolithiasis: a matched-paired analysis of 286 patients. Urology 2012;80:1214–9. [DOI] [PubMed] [Google Scholar]
- [19].Akman T, Binbay M, Ugurlu M, et al. Outcomes of retrograde intrarenal surgery compared with percutaneous nephrolithotomy in elderly patients with moderate-size kidney stones: a matched-pair analysis. J Endourol 2012;26:625–9. [DOI] [PubMed] [Google Scholar]
- [20].Chu L, Farris CA, Corcoran AT, et al. Preoperative stent placement decreases cost of ureteroscopy. Urology 2011;78:309–13. [DOI] [PubMed] [Google Scholar]
- [21].Sugihara T, Yasunaga H, Horiguchi H, et al. A nomogram predicting severe adverse events after ureteroscopic lithotripsy: 12 372 patients in a Japanese national series. BJU Int 2013;111:459–66. [DOI] [PubMed] [Google Scholar]
- [22].Sabnis RB, Ganesamoni R, Doshi A, et al. Micropercutaneous nephrolithotomy (microperc) vs retrograde intrarenal surgery for the management of small renal calculi: a randomized controlled trial. BJU Int 2013;112:355–61. [DOI] [PubMed] [Google Scholar]
- [23].Srivastava A, Singh KJ, Suri A, et al. Vascular complications after percutaneous nephrolithotomy: are there any predictive factors? Urology 2005;66:38–40. [DOI] [PubMed] [Google Scholar]
- [24].Williams SK, Leveillee RJ. Management of staghorn calculus: single puncture with judicious use of the flexible nephroscope. Curr Opin Urol 2008;18:224–8. [DOI] [PubMed] [Google Scholar]
- [25].Bozkurt OF, Resorlu B, Yildiz Y, et al. Retrograde intrarenal surgery versus percutaneous nephrolithotomy in the management of lower-pole renal stones with a diameter of 15 to 20 mm. J Endourol 2011;25:1131–5. [DOI] [PubMed] [Google Scholar]
- [26].Stern JM, Yiee J, Park S. Safety and efficacy of ureteral access sheaths. J Endourol 2007;21:119–23. [DOI] [PubMed] [Google Scholar]
- [27].Moskovitz B, Halachmi S, Sopov V, et al. Effect of percutaneous nephrolithotripsy on renal function: assessment with quantitative SPECT of (99m)Tc-DMSA renal scintigraphy. J Endourol 2006;20:102–6. [DOI] [PubMed] [Google Scholar]
- [28].Hyams ES, Munver R, Bird VG, et al. Flexible ureterorenoscopy and holmium laser lithotripsy for the management of renal stone burdens that measure 2 to 3 cm: a multi-institutional experience. J Endourol 2010;24:1583–8. [DOI] [PubMed] [Google Scholar]
- [29].Akdeniz D, Celik HT, Kazanci F, et al. Is kidney injury molecule 1 a valuable tool for the early diagnosis of contrast-induced nephropathy? J Investig Med 2015;63:930–4. [DOI] [PubMed] [Google Scholar]
- [30].Deyà-Martínez À, Fortuny C, Soler-Palacín P, et al. Cystatin C: a marker for inflammation and renal function among HIV-infected children and adolescents. Pediatr Infect Dis J 2016;35:196–200. [DOI] [PubMed] [Google Scholar]


