Abstract
Rationale:
A gouty tophus, arising from the deposition of monosodium urate crystals (MSU), rarely occurs in the nasal bridge. There have been only 7 documented cases of a gouty tophus in the nasal bridge from 1978 to 2018 in English-language literature.
Patient concerns:
A 65-year-old male had a chief complaint of a lump in the nasal bridge that was slowly growing for over 1 year.
Diagnosis:
MSU crystals were confirmed through ultrasonography (US) and pathological examinations.
Interventions:
A cosmetically less destructive method, ultrasound-guided fine needle aspiration cytology (FNAC) was used to approach the mass lesion of nasal bridge.
Outcomes:
The diagnosis was confirmed as a gouty tophus without performing a nasal subdermal exploration.
Lessons:
This case report is the first use of US with FNAC to approach and diagnosed a gouty tophus in the nasal bridge.
Keywords: fine needle aspiration cytology, gouty tophus, nasal bridge, ultrasonography
1. Introduction
The prevalence of gout is rising in the modern world. In Taiwanese society, the incidence of gouty arthritis is approximately 4.92%.[1] Gout attacks primarily involves a single joint of the lower extremities, especially the first metatarsophalangeal joint.[2] Other frequent sites include the knees, ankles, and elbows. It is uncommon that a gouty tophus occurs in the region of the head and neck. There have been only 7 documented cases of a gouty tophus in the nasal bridge from 1978 to 2018 in English-language literature.
In this study, we report a patient who presented with a nonpainful, slowly progressive, enlarged mass in the nasal bridge. We successfully used a cosmetically less destructive method, ultrasound-guided fine needle aspiration cytology (FNAC), to approach the mass lesion, and the diagnosis was confirmed as a gouty tophus without performing a nasal subdermal exploration. This was a rare case, as a tophus in the nasal bridge is a rare occurrence, and here, we report the first use of ultrasonography (US) with FNAC to approach the nasal bridge mass.
2. Case report
A 65-year-old male came to our department with a chief complaint of a lump in the nasal bridge that was slowly growing for over 1 year. The patient reported no epistaxis, rhinorrhea, nasal obstruction, traumatic episode, surgical history, or painful sensation. This patient had been treated for the underlying diseases of gouty arthritis, which were under regular Colchicine and Febuxostat control for 5 years. The physical examination demonstrated a fixed and hard mass in the central middle third nasal bridge (Fig. 1). The fiberoptic nasopharyngoscopy demonstrated nasal septal deviation to the right, but no mass or mucosal lesion was detected in the bilateral nasal cavities. The laboratory data revealed a normal C-reactive protein level (1.63 mg/L; normal: < 5 mg/L) without leukocytosis (6,600/μL; normal: 3,900–10,600/μL) but with hyperuricemia (9.1 mg/dL; normal: < 6.8 mg/dL). A head and neck computed tomography (CT) scan without contrast displayed one radiopaque mass protruding and crossing over the nasal bridge (Fig. 2). On the bone windows CT, the mass lesion invaded into the nasal bone and the septal cartilage. To differentiate this mass lesion, we arranged ultrasound-guided FNAC. The target US revealed an isoechoic soft tissue-like mass surrounding the nose bridge, sized of 19.9 mm in diameter and 6.6 mm in thickness (Fig. 3). There were a few internal hyperechoic foci, but no definite intrinsic flows appeared on the Doppler scan of the mass. FNAC was performed from the site using a 21-gauge needle. White particulate substance was obtained. Papanicolaou (PAP)-stained smears demonstrated a background of necrotic debris with clusters of amorphous materials, macrophages, and occasional multinucleated giant cells. Thin needle-shaped crystals in stacks (Fig. 4A) were distributed in the smears. Under direct polarized light, they presented high brightness against the black background with negative birefringence (Fig. 4B). Monosodium urate (MSU) crystals were confirmed.
Figure 1.
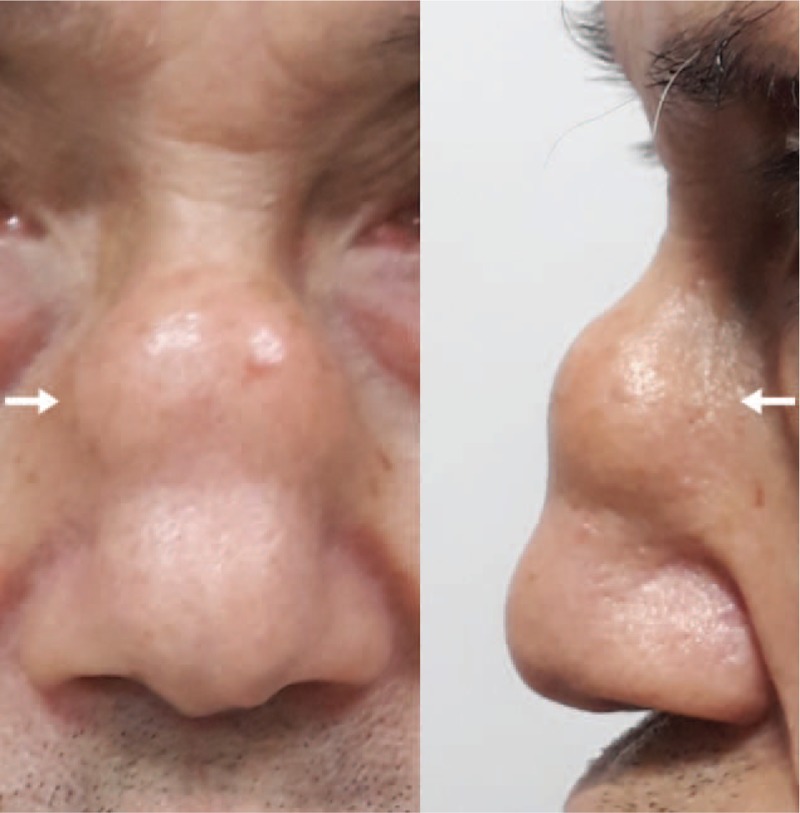
The fixed hard non-painful lump (arrow) in the central middle third nasal bridge.
Figure 2.
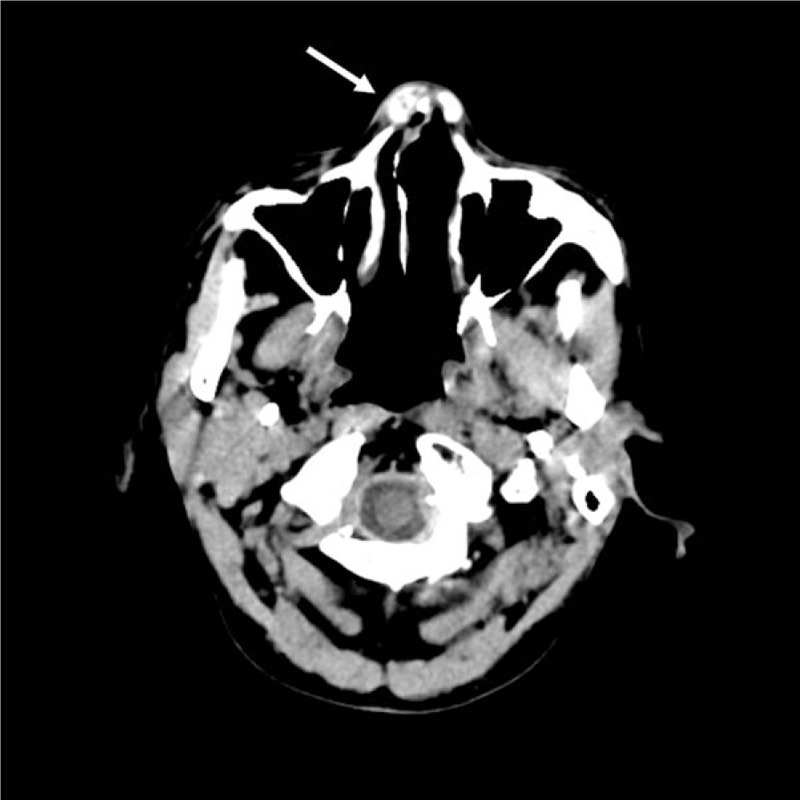
The head and neck CT scan displayed a mottled radiopaque mass lesion (arrow) that protruded and crossed over the nasal ridge.
Figure 3.
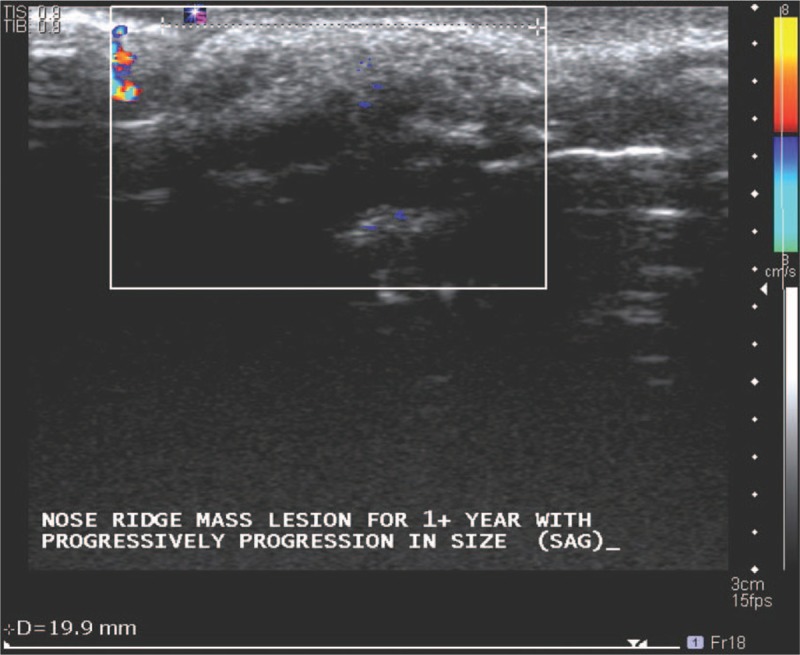
The target ultrasonography of the nasal sagittal view revealed an inhomogeneous appearance with certain internal hyperechoic foci in the upper nose ridge. A diameter of 19.9 mm was measured (dotted line). The hyperechoic contour of the nasal mass was outlined.
Figure 4.
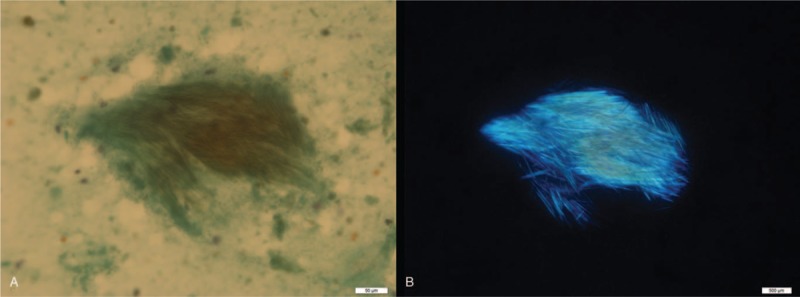
(A) Papanicolaou smears show needle-shaped crystals arranged in bundles (original magnification ×400). (B) These crystals show strong negative birefringence under polarized light (original magnification ×400).
The patient refused the advanced surgical excision of the nasal tophus, requesting medical treatment alone. The rheumatologist adjusted the doses of Colchicine and Febuxostat. The serum urate level has remained below 4.5 mg/dL over the entire 6 months of follow-up. No gout attack has been noted, and the lump has not progressed in size.
3. Ethical approval
Written informed consent was obtained from the patient for publication and any associated images. Approval of this case study was obtained from the Institutional Review Board of Chang Gung medical foundation (IRB No.201800958B0).
4. Discussion
A gouty tophus is composed of MSU crystals.[3] A tophus can deposit in various sites within the human body, which can be divided into typical or atypical locations. A tophus in the head and neck region is classified as atypical and is rare in the nasal bridge.[2]
A tophus can cause lytic changes in the peripheral structures and painful sensation.[2] The region of the nasal bridge is innervated by the anterior ethmoidal nerve and the infraorbital nerve. During surgery of the nasal bone fracture, these nerves can be blocked for anesthesia and pain relief.[4] Pain along with redness, warmness, swelling development in deposition of MSU is mediated by inflammatory substances that are produced after cell injury. The most important of pain-inducing molecules contains prostaglandins, bradykinin, cytokines, and substance P.[5,6]
It is unknown why the tophus in the nasal bridge was painless in the presented case despite the underlying nasal bone being eroded. We reviewed all case reports regarding a tophus of the nasal bridge in English-language literature, and the painless characteristic was often described (Table 1).[3,7–12] Nevertheless, other types of pathology within the nasal bridge could contribute to a painful sensation.[13]
Table 1.
Reported cases of a nasal tophus in the nasal bridge.
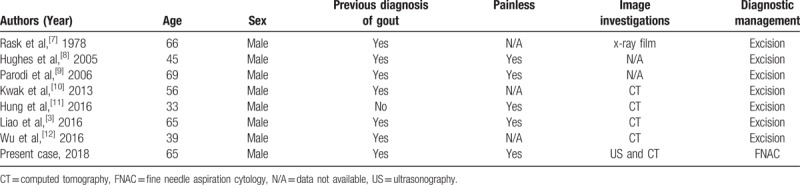
A nasal tophus is strongly associated with gouty arthritis. In the previous 7 case reports regarding the tophi of the nasal bridge, only one article mentioned that their patient had no history of gouty arthritis, and the nasal tophus was even the initial presentation of gout.[11] Others revealed the history of gouty arthritis persisting for years, even under medical control (Table 1).[3,7–10,12]
Probenecid was prescribed in one report.[7] In addition, 2 reports employed Allopurinol to control gout.[3,8] Our patient differed from earlier patients. He received Cochicine and Febuxostat to control his gout.
MSU crystal formation reflects excessive levels of blood urate. Hyperuricemia is defined as a serum urate level above the MSU saturation point (> 6.8 mg/dL), at which point the risk of crystallization increases.[14] Lin et al[15] stated that the incidence of gout increased as the serum urate level rose. Although hyperuricemia is essential for MSU crystal formation, only 2 to 36% of hyperuricemic patients in fact develop gout.[15,16] The mechanism of MSU formation is complex, being affected by environmental factors such as cold temperature, acidity, and physical perturbation.[14] However, whether biomedical factors such as albumin, antibodies, and immunoglobulins promote MSU formation remains controversial.[14] Further, a tophus is a feature of advanced gout; a tophus contains a nest of MSU crystals surrounded by soft tissue and inflammatory cells that are microscopically evident.[17] Extracellular trapping of crystals by neutrophils contribute to tophus formation. A tophus contains 3 primary zones: a central core of MSU crystals; a surrounding, high-density, cellular coronal zone; and an outer fibrovascular zone. Both of the coronal and fibrovascular zones contain many macrophages and plasma cells, fewer mast cells, and scattered T and B lymphocytes.[17]
We performed US and FNAC to approach the mass lesion in the nasal bridge. US is noninvasive and useful to detect MSU crystals over articular cartilages.[18] Some distinctive characteristics of gout under US include being hypoechoic to hyperechoic, with an inhomogeneous appearance, frequently surrounded by a small anechoic rim.[19] Our sonographic images showed an inhomogeneous appearance with certain internal hyperechoic foci but no internal flow, which is compatible with the characteristics of tophi under US (Fig. 3).
FNAC is an alternative option for a minimally invasive procedure and diagnostic test to verify the tophus in the nasal bridge. The PAP stain and the polarized light of microscopy can confirm the diagnosis of gouty tophus.[20] PAP-stained smears of gout display a granular amorphous substance and slim needle-shaped crystals in groups. Under the polarized light of microscopy, the MSU crystals would be negative birefringence.[21] Our cytological findings were consistent with these findings and verified the diagnosis of gouty tophus (Fig. 4). Currently, dual energy CT-scan can be used as another diagnostic option for detection of MSU deposits.[22]
Wu et al. stated the patients with nasal tophi in the literature are more likely to be male and middle aged.[12] Our finding was in accordance with theirs (Table 1). They concluded that surgery was indicated for cosmetic purposes or recalcitrant symptoms, such as nasal obstruction or difficulty breathing.[12] However, the aesthetic appearance appeared not to concern our patient, and there was no reported discomfort except for the convex lump on the nasal bridge. Consequently, after cytological diagnosis demonstrated a benign lesion, the patient did not request further surgical excision and elected to take adjusted doses of Cochicine and Febuxostat. The lump remained stable, and the serum urate was kept below 4.5 mg/dL over the following 6 months. Two prior reports mentioned that, after surgery, the local tophus did not recur over follow-up periods of 6 months and 2 years, respectively.[8,12]
In the previous case reports, surgical excision was conducted after the head and neck CT scan was performed. Three case reports described the surgical procedures in detail. Hughes et al[8] used intranasal transfixion and inter-cartilaginous incision with the endoscopic approach to remove the tophus. Kwak et al[10] created an external, inverted-V-shaped incision along the columella and dissected the subperichondrial plane to remove the tophus. The harvested septal cartilage was placed alone with remnant nasal septum to correct saddling. Wu et al[12] made a diagonal incision along the line of the nasal fold to remove the entire tophus. The nasal bony defect was repaired with titanium mesh and a microscrew to prevent the depression of the nasal bridge. The definite diagnosis was made by the pathological examination of the surgical specimen. The operation would likely lead to scar formation and possibly the alteration of facial cosmetic outlooks. However, through the FNAC approach, the facial contour was not destructed. The diagnosis can be achieved before the decision of definite treatment is made. Therefore, we consider US with FNAC to be a promising tool to approach and diagnose a facial mass without substantial surgical destruction.
5. Conclusion
We demonstrated a gouty tophus in the nasal bridge, presenting as a hard and fixed mass, leading to the erosion of the nasal bone and the septal cartilage. The painless presentation and strong correlation with the gouty arthritis are the distinguishing features. The use of US and FNAC to approach the tophus in the nasal bridge is promising for the diagnosis and is not as destructive as surgery. We suggest that US with FNAC should be considered as a tool for evaluating a facial mass before a definite treatment modality is chosen. Although very rare, a gouty tophus should be considered in the differential diagnosis of a nasal bridge lump and can be successfully diagnosed by US with FNAC.
Acknowledgment
The authors thank all of the members of Department of Otolaryngology-Head and Neck Surgery, Chang Gung Memorial Hospital, Keelung, for their invaluable help.
Author contributions
Resources: Shih-Lung Chen, Jim-Ray Chen, Shih-Wei Yang.
Supervision: Shih-Wei Yang.
Writing – original draft: Shih-Lung Chen.
Writing – review & editing: Shih-Wei Yang
Shih-Lung Chen orcid: 0000-0003-4051-4009.
Footnotes
Abbreviation: CT = computed tomography, FNAC = fine needle aspiration cytology, MSU = Monosodium urate, PAP = Papanicolaou, US = ultrasonography.
The authors have no funding and no conflicts of interest to disclose.
References
- [1].Kuo CF, Grainge MJ, Zhang W, et al. Global epidemiology of gout: prevalence, incidence and risk factors. Nat Rev Rheumatol 2015;11:649–62. [DOI] [PubMed] [Google Scholar]
- [2].Forbess LJ, Fields TR. The broad spectrum of urate crystal deposition: unusual presentations of gouty tophi. Semin Arthritis Rheum 2012;42:146–54. [DOI] [PubMed] [Google Scholar]
- [3].Liao PH, Chang KP. Nasal gouty tophus. Ear Nose Throat J 2016;95:478–80. [PubMed] [Google Scholar]
- [4].Cok OY, Erkan AN, Eker HE, et al. Practical regional blocks for nasal fracture in a child: blockade of infraorbital nerve and external nasal branch of anterior ethmoidal nerve. J Clin Anesth 2015;27:436–8. [DOI] [PubMed] [Google Scholar]
- [5].Ramonda R, Oliviero F, Galozzi P, et al. Molecular mechanisms of pain in crystal-induced arthritis. Best Pract Res Clin Rheumatol 2015;29:98–110. [DOI] [PubMed] [Google Scholar]
- [6].Ramonda R, Frallonardo P, Oliviero F, et al. Pain and microcrystalline arthritis. Reumatismo 2014;66:48–56. [DOI] [PubMed] [Google Scholar]
- [7].Rask MR, Kopf EH. Nasal gouty tophus. JAMA 1978;240:636. [PubMed] [Google Scholar]
- [8].Hughes JP, Di Palma S, Rowe-Jones J. Tophaceous gout presenting as a dorsal nasal lump. J Laryngol Otol 2005;119:492–4. [DOI] [PubMed] [Google Scholar]
- [9].Parodi PC, De Biasio F, Nadalig B, et al. Tophaceous lesion of the middle third of the nose. Dermatol Surg 2006;32:556–7. [DOI] [PubMed] [Google Scholar]
- [10].Kwak PE, Gorman BK, Olson KL. Nasal gout presenting as nasal obstruction. JAMA Otolaryngol Head Neck Surg 2013;139:411–3. [DOI] [PubMed] [Google Scholar]
- [11].Hung SF, Wu CC, Chang FC, et al. Tophaceous gout in the nasal root: an unusual initial presentation. Am J Med Sci 2016;351:321–2. [DOI] [PubMed] [Google Scholar]
- [12].Wu JC, Chou PY, Chen CH. Nasal gouty tophus: report a rare case presenting as a nasal hump with nasal obstruction. Biomed J 2016;39:295–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Wong G, Randhawa P, Stephens J, et al. Fibrous dysplasia of the nasal bone: case reports and literature review. J Laryngol Otol 2013;127:1152–4. [DOI] [PubMed] [Google Scholar]
- [14].Martillo MA, Nazzal L, Crittenden DB. The crystallization of monosodium urate. Curr Rheumatol Rep 2014;16:400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lin KC, Lin HY, Chou P. The interaction between uric acid level and other risk factors on the development of gout among asymptomatic hyperuricemic men in a prospective study. J Rheumatol 2000;27:1501–5. [PubMed] [Google Scholar]
- [16].Hall AP, Barry PE, Dawber TR, et al. Epidemiology of gout and hyperuricemia. A long-term population study. Am J Med 1967;42:27–37. [DOI] [PubMed] [Google Scholar]
- [17].Chhana A, Dalbeth N. The gouty tophus: a review. Curr Rheumatol Rep 2015;17:19. [DOI] [PubMed] [Google Scholar]
- [18].Thiele RG, Schlesinger N. Diagnosis of gout by ultrasound. Rheumatology (Oxford) 2007;46:1116–21. [DOI] [PubMed] [Google Scholar]
- [19].Thiele RG. Role of ultrasound and other advanced imaging in the diagnosis and management of gout. Curr Rheumatol Rep 2011;13:146–53. [DOI] [PubMed] [Google Scholar]
- [20].Bhadani PP, Sah SP, Sen R, et al. Diagnostic value of fine needle aspiration cytology in gouty tophi: a report of 7 cases. Acta Cytol 2006;50:101–4. [DOI] [PubMed] [Google Scholar]
- [21].Berendsen D, Neogi T, Taylor WJ, et al. Crystal identification of synovial fluid aspiration by polarized light microscopy. An online test suggesting that our traditional rheumatologic competence needs renewed attention and training. Clin Rheumatol 2017;36:641–7. [DOI] [PubMed] [Google Scholar]
- [22].Bongartz T, Glazebrook KN, Kavros SJ, et al. Dual-energy CT for the diagnosis of gout: an accuracy and diagnostic yield study. Ann Rheum Dis 2015;74:1072–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


