Abstract
Rationale:
Extranodal natural killer T-cell lymphoma nasal type (ENKL) is an extremely rare tumor with a very low survival rate. In recent decades, only a few ENKL cases have been published. Presenting a special ENKL case lead the authors to emphasize the primary features of ENKL in early diagnosis and therapy. Here we report an unusual ENKL case which was initially found in the eyes and presented as masqueraded uveitis
Patient concerns:
A 55 years old female, with vision loss in the right eye for approximately 6 months, and vision blurry, redness and pain in the left eye for 2 weeks, was referred to our hospital.
Diagnosis:
Clinical examinations and images demonstrated bilateral anterior uveitis, retinal and choroidal detachment, and secondary glaucoma. After 3 months, the patient began to present a sore throat, fever, and headaches. The computed tomography (CT) and magnetic resonance imaging (MRI) of her skull demonstrated nothing positive. One month later, a neoplasm was found in her nasopharynx and tonsil, which was confirmed, by histopathology, as ENKL
Interventions:
This patient was prescribed with steroid for 3 months because of the first diagnosis by the ophthalmologist. After the other symptoms like a sore throat, fever and headaches occurred, symptomatic treatment was given. Unfortunately, when the real cause was found, the patient could not tolerate the other treatment for ENKL.
Outcomes:
Since the patient was treated with steroid without improvement, she died due to the septic shock and multiple organ failure.
Lessons:
Clinicians should always be cautious to ENKL which can be easily be misdiagnosed in the early stage. Early diagnosis and appropriate treatment are keys to raise the survival rate of ENKL patients.
Keywords: diagnosis, extranodal NK/T-cell lymphoma nasal-type, masquerade syndrome, therapy
1. Introduction
Extranodal NK/T-cell lymphoma nasal type (ENKL) is a rare subtype of non-Hodgkin lymphoma (NHL), accounts for approximately 2% to 10% of total lymphoma. In general, ENKL occurred mostly in adult males and the median age is 45.[1] The incidence of lymphoma was highest among the Caucasians, but NK/T-cell lymphoma was more common in Asian and Latin American countries. Nasal cavity and upper aerodigestive tract are the most frequently affected organs, usually, accompany with Epstein-Barr virus (EBV) infection.[2] Primary clinic presentations of ENKL include nasal obstruction,[3] epistaxis, sore throat, destructive mass (in sinuses, nose, and palate), skin lesions,[4] gastrointestinal tract, orbital diseases,[5] and so on. Only a few cases with initial orbital manifestations were reported,[7,8] including dacryoadenitis,[6] orbital cellulitis, myositis, and uveitis.
The uveitis masquerade syndromes (UMS) are a group of ocular diseases that may mimic chronic intraocular inflammation. UMS is usually caused by the intraocular invasion of tumor cells and often lead to misdiagnosis. In this paper, we would like to report a rare case of ENKL with masquerade syndrome presenting as bilateral uveitis.
2. Case presentation
A 55-year-old woman was referred to an ophthalmologist for vision loss in the right eye for approximately 6 months, and blurred vision, redness, and pain in the left eye for 2 weeks. Her visual acuity was light perception (LP) in both eyes. The intraocular pressure (IOP) was 28mmHg in her right eye and 18mmHg in the left. Conjunctiva was mildly hyperemic in her left eye (Fig. 1). The cells and flare were present in the bilateral anterior chamber (AC). The vitreous was hazy; the retina was detached and hemorrhagic in both eyes (Fig. 2). According to these clinical manifestations, she was diagnosed as bilateral anterior uveitis, exudative retinal detachment, choroidal detachment, and secondary glaucoma. The patient was treated with systemic methylprednisolone and ganciclovir. Unfortunately, no improvement happened and the patient complained about the sore throat, fever, and headaches. The chest X-ray, skull MR, and B-type ultrasonic of abdomen showed no positive finding (Fig. 3).
Figure 1.
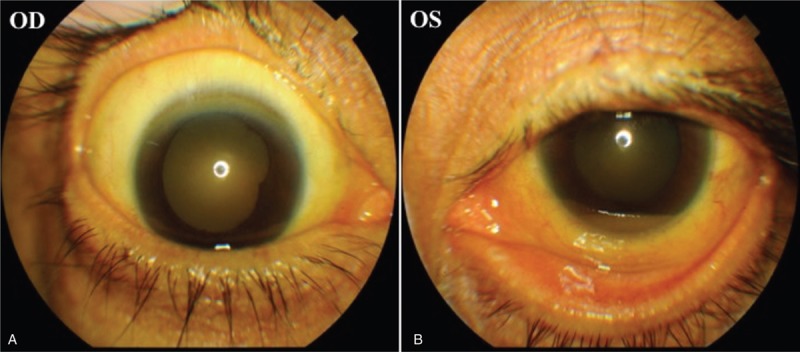
Clinical photographs of the patient's bilateral anterior segment in the beginning. Her left eye has mild conjunctival injection.
Figure 2.
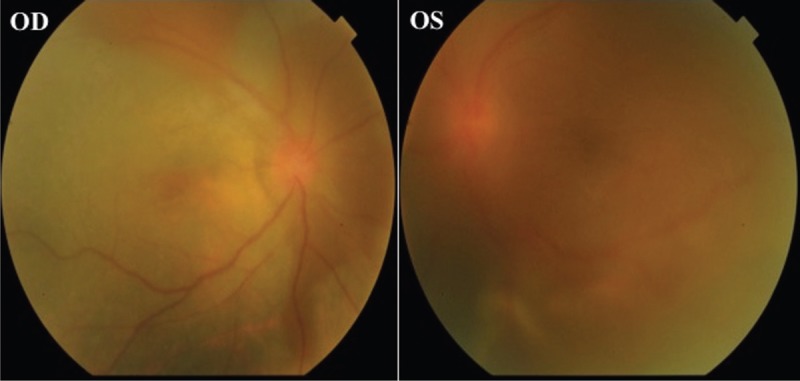
The fundus of this patient. She had retinal detachment and hemorrhage.
Figure 3.
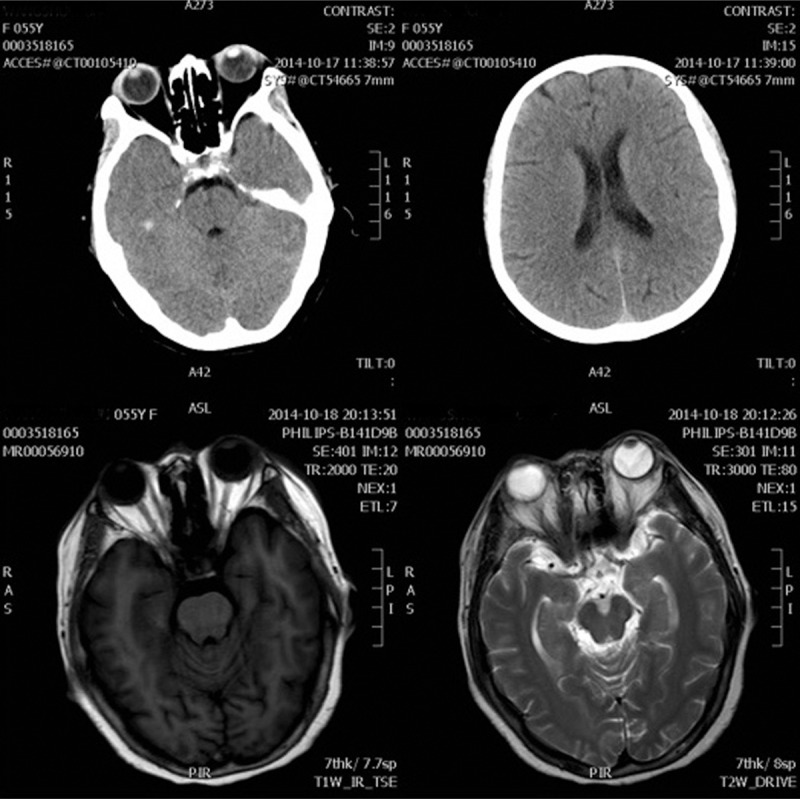
Skull CT and MRI show nothing. CT = computed tomography, MRI = magnetic resonance imaging.
After 1 week's treatment, the eye pain got even worse (Fig. 4). Periorbital ecchymosis occurred with conjunctival chemosis, more severe in the right. Despite symptomatic steroid was applied, symptoms still progressed.
Figure 4.

Clinical photographs of the patient on presentation after one week. Top panel, this is the appearance of the patient's orbital. The periorbital ecchymosis occurred in her eyes, especially in the right. Bottom left, her left eye had chemosis and injection. Bottom right, her right eye had severe conjunctival chemosis and congestion.
Later the patient received nasopharyngoscopic examination and a neoplasm was found in her nasopharynx and tonsil. The biopsy of the nasopharynx neoplasm was also performed and histopathologic findings indicated dense and diffuse infiltrated atypical lymphoid cells (Fig. 5A). The histoimmunostaining revealed that those atypical cells were CD56+ (Fig. 5B) and CD3++ (Fig. 5C). Therefore, the final diagnosis of NK/T-cell lymphoma nasal-type was made. Unfortunately, although the chemotherapy was given, the patient still died of multiple organs failure 1 month after her first visit.
Figure 5.
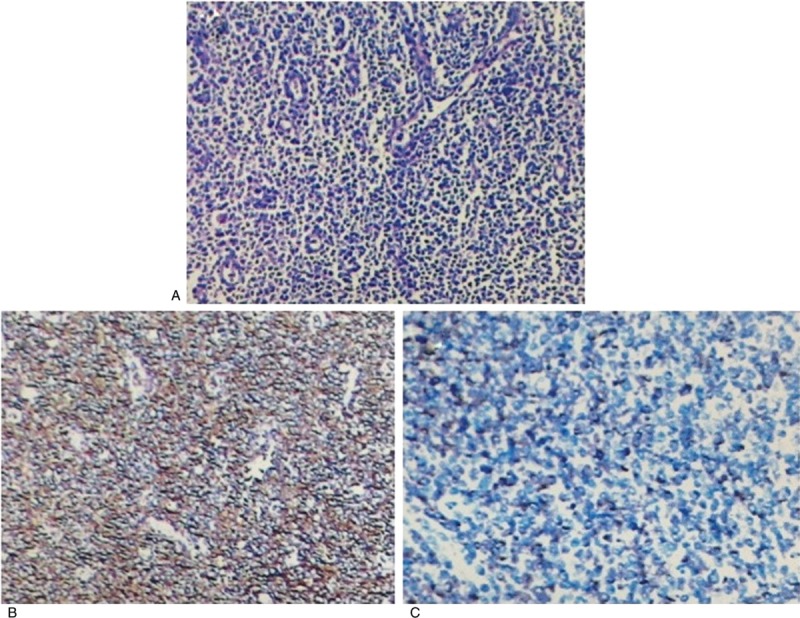
Small- to Medium atypical lymphoid cells show a diffuse proliferation (A). These cells are positve for CD56 (B) and CD3 (C). (A) Hematoxylin and eosin, (B, C) immunohistochemistry. All × 100.
3. Discussion
Extranodal NK/T-cell lymphoma nasal type is a highly aggressive malignant neoplasm, with only 25% to 50% of 5-year overall survival (OS) rate.[9] In general, the median age is 40 to 58, and about 65% of patients are male. Nasal cavities, paranasal, sinuses, and upper aerodigestive tract are the most frequently affected sites, accounting for about 87% of total ENKL patients.[10] Clinical features of ENKL are similar in many countries. According to previously reported ENKL cases with ocular involvement, the survival rate was grimmer, and the median survival period was only 4 months.[8] In fact, ocular presentations as initial manifestation are not usual in ENKL patients, only a few cases were published. Ocular involvement in ENKL patients was mainly caused by the direct invasion of the paranasal sinuses.[11,12] Those ocular presentations could masquerade as many other diseases, such as uveitis,[13] dacryoadenitis,[6] orbital cellulitis, and so on.
The term masquerade syndrome is defined as those malignant diseases but mainly manifested as intraocular inflammation. It is always caused by primary ocular tumors such as retinoblastoma (RB), choroidal melanoma and intraocular lymphoma. Cancer cells metastases from other sites can cause masquerade syndrome too. The morbidity of binoculus masquerade syndrome is 64% to 83%. Common initial presentations are blurred vision, slowly-decreased vision or multiple floaters in front of the eye.[14] Besides, there are some differences between the primary intraocular lymphoma (PIOL) and secondary intraocular lymphoma. PIOL is a subset of CNS lymphoma, and most of PIOL is diffuse large B-cell lymphoma. Posterior uveitis with posterior vitreous detachment, vitreous hemorrhage, and exudative retinal detachment are not rare in PIOL patients. Hormone treatment usually is useless. Most of the secondary intraocular lymphoma is T cell type and NK/T cell type and always cause anterior uveitis, vitreous inflammation or choroid detachment. Unlike the PIOL, the hormone therapy can slow down the progress in secondary intraocular lymphoma patients.
In our case, the patient's clinical manifestations presented at first mimicked chronic intraocular inflammation and led the clinicians to the misdiagnosis of anterior uveitis. The patient missed the best treatment time due to the wrong diagnosis. Incorrect or delayed diagnosis of uveitic masquerade syndromes (UMS) resulting from ENKL may cause severe consequences. Rothova et al[15] followed 828 uveitis patients and forty of them were diagnosed with UMS. Among these UMS patients, malignancy was found in 19 of them. Notwithstanding, ophthalmologists only recognized malignancy in 11 of 19 patients (58%). Those data indicated that misdiagnosis of UMS is not an individual incident. Many patients have severe consequences because of their late or incorrect diagnosis conducted by clinical doctors. Therefore, awareness of clinical manifestations of ENKL and application of appropriate diagnostic procedures would promote timely diagnosis and treatment, which are especially important for the prognosis. For clinicians, especially ophthalmologist, it is important for them to recognize clinical manifestations of ENKL and make the right diagnosis at the very early stage.
ENKL is an aggressive lymphoma and should be treated with the same strategies as other lymphomas. Conventional anthracycline-containing regimens, such as cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP), showed no benefit to ENKL patients[16] and thus are not optimal treatments for ENKL.[17,18] The 5-year OS rate of those patients with localized ENKL, treated by CHOP and followed with involved-field radiotherapy (RT) was less than 50%.[19] Current guidelines recommended that the optimal treatment for newly diagnosed nasal ENKL patients with stage I and contiguous stage II disease is local radiotherapy. Furthermore, chemotherapy of L-asparaginase (L-asp) and/or non-MDR-related agents for newly diagnosed advanced ENKL patients is promising.[20]
Finally, we have learned from this case that if a rapidly progressive disease, such as ENKL, is suspected, the invasive biopsy should be done as early as possible. In addition, if the pathological analysis showed a negative result, another biopsy from the same site should be redone.
Author contributions
FZ and KL conceived and wrote the paper. FZ, KL, XCD collected information and made figures. KL and XCD reviewed and edited the manuscript.
Conceptualization: Xuanchu Duan.
Funding acquisition: Xuanchu Duan.
Methodology: Feng Zhang.
Resources: Ke Liu.
Supervision: Xuanchu Duan.
Writing – original draft: Feng Zhang.
Writing – review & editing: Feng Zhang, Xuanchu Duan, Ke Liu.
Footnotes
Abbreviations: CHOP = cyclophosphamide, doxorubicin, vincristine, and prednisone, ENKL = extranodal natural killer T-cell lymphoma nasal type, OS = overall survival, PIOL = primary intraocular lymphoma, UMS = uveitic masquerade syndromes.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Second Xiangya Hospital Ethics Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from the patient's family. The patient's family consented to publish photos in the paper.
Informed written consent was obtained from the patient for publication of this case report and accompanying images.
All data are fully available without restriction.
This work was supported by National Natural Science Foundation of China (Grant No.81670859).
The authors declare no conflict of interest.
References
- [1].Aozasa K, Katsuyuki MA. Epidemiology and pathogenesis of nasal NK/T-cell lymphoma: a mini-review. Sci World J 2011;5:422–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Suzuki R, Yamaguchi M, Izutsu K, et al. Prospective measurement of epstein-barr virus-DNA in plasma and peripheral blood mononuclear cells of extranodal NK/T-cell lymphoma, nasal type. Blood 2011;118:6018–22. [DOI] [PubMed] [Google Scholar]
- [3].Zou H, Pan KH, Wu L, et al. Nasal NK/T cell lymphoma presents with long-term nasal blockage and fever: a rare case report and literature review. Oncotarget 2016;7:9613–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Chen T, Yu Y, Zhang Y. A case report of primary cutaneous natural killer/T-cell lymphoma. Mol Clin Oncol 2016;5:777–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Jiménez-Pérez JC, Yoon MK. Natural killer T-cell lymphoma of the orbit: an evidence-based approach. Semin Ophthalmol 2016;32:116–24. [DOI] [PubMed] [Google Scholar]
- [6].Jiménez-Pérez JC, Jakobiec FA, Zakka FR, et al. Dacryoadenitis as the initial presentation of a natural killer T-cell lymphoma. Ophthalmic Plast Reconstr Surg 2017;33:e147–50. [DOI] [PubMed] [Google Scholar]
- [7].Hon C, Kwok AK, Shek TW, et al. Vision-threatening complications of nasal T/NK lymphoma. Am J Ophthalmol 2002;134:406–10. [DOI] [PubMed] [Google Scholar]
- [8].Ely A, Evans J, Sundstrom JM, et al. Orbital involvement in extranodal natural killer T cell lymphoma: an atypical case presentation and review of the literature. Orbit 2012;31:267–9. [DOI] [PubMed] [Google Scholar]
- [9].Kwong Y-L. Natural killer-cell malignancies: diagnosis and treatment. Leukemia 2005;19:2186–94. [DOI] [PubMed] [Google Scholar]
- [10].Kim SJ, Yoon DH, Jaccard A, et al. A prognostic index for natural killer cell lymphoma after non-anthracycline-based treatment: a multicentre, retrospective analysis. Lancet Oncol 2016;17:389–400. [DOI] [PubMed] [Google Scholar]
- [11].Dai W, Zhong M, Shen W, et al. Natural killer T-Cell lymphoma originating from the orbit. Chin Med J 2012;125:1677–80. [PubMed] [Google Scholar]
- [12].Kwong YL, Kim WS, Lim ST, et al. SMILE for natural killer/T-cell lymphoma: analysis of safety and efficacy from the Asia lymphoma study group. Blood 2012;120:2973–80. [DOI] [PubMed] [Google Scholar]
- [13].Imai A, Takase H, Imadome KI, et al. Development of extranodal NK/T-cell lymphoma nasal type in cerebrum following Epstein-Barr virus-positive uveitis. Intern Med 2017;56:1409–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Rothova A, ten Berge J, Thiadens A, et al. Benign masquerade syndromes in uveitis. Acta Ophthalmologica 2018;96:39.28661562 [Google Scholar]
- [15].Rothova A, Ooijman F, Kerkhoff F, et al. Uveitis masquerade syndromes. Ophthalmology 2001;108:386–99. [DOI] [PubMed] [Google Scholar]
- [16].Suzuki, Ritsuro. NK/T cell lymphoma: updates in therapy. Current Hematologic Malignancy Reports 2018;13:7–12. [DOI] [PubMed] [Google Scholar]
- [17].Oshimi K. Progress in understanding and managing natural killer-cell malignancies. Br J Haematol 2007;139:532–44. [DOI] [PubMed] [Google Scholar]
- [18].Liang R, Raymond Advances in the management and monitoring of extranodal NK/T-cell lymphoma, nasal type. Br J Haematol 2009;147:13–21. [DOI] [PubMed] [Google Scholar]
- [19].Merli F, Luminari S, Rossi G, et al. Cyclophosphamide, doxorubicin, vincristine, prednisone and rituximab versus epirubicin, cyclophosphamide, vinblastine, prednisone and rituximab for the initial treatment of elderly ‘fit’ patients with diffuse large B-cell lymphoma: results from the ANZINTER3 trial of the Intergruppo Italiano Linfomi. Leuk Lymphoma 2012;53:581–8. [DOI] [PubMed] [Google Scholar]
- [20].Yamaguchi M, Miyazaki K. Current treatment approaches for NK/T-cell lymphoma. J Clin Exp Hematopathol 2017;57:98–108. [DOI] [PMC free article] [PubMed] [Google Scholar]


