Abstract
Background
In addition to screening by Pap smears, vaccination against human papillomavirus (HPV) can dramatically reduce cervical cancers caused by the virus. The acceptance of HPV vaccination is directly related to HPV knowledge. This research aimed to evaluate knowledge about HPV and vaccination among men and women aged 16–25 years who use the public health system in Brazil.
Methods
This was a cross-sectional, multicenter study of sexually active young adults recruited from 119 primary care units between 2016 and 2017. All participants answered a face-to-face standardized questionnaire.
Results
Of 8581 participants, the mean percentage of correct answers about HPV and vaccination was 51.79% (95% CI 50.90-52.67), but 75.91% (95% CI 74.13-77.69) had awareness of the HPV vaccination. Women answered a higher proportion of questions correctly than men did (p = 0.0003). Lower education level was the variable that most interfered with knowledge. The best information sources for knowledge were both health professionals and the media (1.33%, 95% CI 1.03-1.70).
Conclusions
The results emphasize the importance of educational programs about HPV and vaccination among young adults, especially in socially disadvantaged populations. These findings can help to increase the vaccination rate in the country and to stimulate public health policies.
Keywords: Vaccination, Sexual health, Sexually transmitted disease, Public health
Highlights
-
•
This is the first nationwide study of young adults who use the public health system.
-
•
Lower education level was the variable that most interfered with knowledge.
-
•
The best information source was the combination of health professionals and the media.
-
•
These results can complement surveillance data on increasing the vaccination rate.
1. Introduction
The strategy for vaccination against human papillomavirus (HPV) for women in Brazil through the National Immunization Program started in 2014 [1]. The age groups for this vaccination varied over the years, and men were included in the coverage of public vaccination (in 2017) [1]. Nonetheless, a decrease in vaccination coverage throughout the years of vaccination coverage was observed [1]. Decreasing coverage rates are observed in many countries around the world to be a challenge for public health disease prevention. HPV vaccination coverage is still lower than desirable in many countries [2], despite the growing evidence about its benefits [3].
This situation may be associated, according to some studies, not only with the absence of health promotion and prevention strategies [[4], [5], [6], [7]] but also with the difficulty in sensitizing adolescents, the age group with the lowest coverage for all vaccines [8]. The lack of interaction between vaccination strategies and educational actions by health professionals may lead to massive ignorance and consequential lack of prevention [4], since the acceptance of HPV vaccination is directly related to HPV knowledge [5].
HPV is a sexually transmitted infection (STI) that requires control, according to the Global Health Sector Strategy on STI 2016-2021 of the World Health Organization, due to high association with cervical cancer, which is responsible for 264,000 deaths in the world each year [9]. In addition, there is increasing evidence that HPV plays a relevant role in the development of anal, vulvar, vaginal, penile, head and neck cancers in both sexes [10].
In the fight against cervical cancer, it is established that in addition to screening by cytological examination, vaccination against HPV can dramatically reduce cancers caused by the virus [11]. For this reason, it is crucial that young people, who are the targets for HPV vaccination, have knowledge and awareness about the virus and the importance of the vaccine. The present study aimed to evaluate knowledge about HPV and vaccination among men and women aged 16–25 years who use the public health system in Brazil. This study also aimed to identify current sources of HPV information.
2. Methods
It was used data from the POP-Brazil Study, a nationwide, multicenter cross-sectional study that includes sexually active young adults from capitals of all 26 states and the Federal District across the five geographical regions. Besides Manaus, that also included a rural primary care unit, all other recruitment centers were in urban or peri-urban areas [12]. These young adults were recruited from 119 public primary care units between September 2016 and December 2017. Participants were invited via patient lists, during visits to health units, and during visits by community health agents or nurses in the school-based health promotion program. In all, 99.08% of eligible participants agreed to participate in the study. The manuscript follows reports of cross-sectional studies according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [13].
The study was approved by the local research and ethics committees (number 1,607,032) and by the committees of the 26 Brazilian capitals and the Federal District of Brasília. All participants provided written consent after they were informed about the content of the study.
2.1. HPV knowledge and vaccination
For data acquisition, primary care professionals were trained in person by the central study coordinator. All participants responded to a face-to-face standardized interview that included the following data [14]:
-
1)
It was collected information on age, sex, race/skin color, education level, socioeconomic class, relationship status, and number of visits to primary care units in the last year. The Brazilian Criteria of Economic Classification (ABEP) were used to analyze socioeconomic class based on ownership of assets. All possessions have a score, and each class is defined by the sum of these scores [15].
-
2)
HPV and vaccination knowledge assessment was based on Saulle et al. [16]. We categorized these items as dichotomic measures (correct = 1 or not correct = 0). The sum of correct questions was divided by the total number of questions (14 for men and 16 for women), ranging from 0 to 100% (Supplement 1). This sex difference in the number of questions arose because men did not answer questions related to Pap smears. The number of correct questions was presented as a continuous variable, with higher scores indicating more hits. The scores were divided into quartiles, and the lowest quartile (fewer correct answers) was compared to the higher quartile (more correct answers).
-
3)
To evaluate information sources, we asked, “How have you learned about HPV vaccination?” This question included multiple-choice responses (school, health professional, friends, media, or have not learned about it). To evaluate the best information source for HPV knowledge, we excluded the participants who had not learned about HPV vaccination.
-
4)
We also asked if the participant was already vaccinated against HPV.
A study sample size of 7935 individuals was calculated to detect differences of 5% in HPV prevalence between regions with a power of 80% and an alpha error of 5% for women, using an estimate of 30% [17] for the prevalence of HPV in Brazil. To maximize diversity across regions, we divided the sample size into equal numbers among regions. We also weighted the measures by the size of the population in each capital within the age range and by sex. Brazil is a multicultural country of 207 million inhabitants, and this study represents approximately 7 million young adults from all capitals of the country [18].
2.2. Statistical analysis
Descriptive analysis was used to characterize the study population and to detect differences between groups. Categorical variables were summarized using absolute frequencies and percentages, while continuous variables were analyzed using means and confidence intervals (CIs) or medians and interquartile ranges (IQRs). Chi-square test and Student's t-tests were used when indicated. The answer option “don't know” was considered to be a missing value.
Poisson regression with a robust variance model was conducted to examine factors associated with knowledge about HPV infection and vaccination by sex and with knowledge and vaccination based on the source of information about HPV vaccination. For the multivariable analyses, a theoretical framework was structured with the variables associated with the outcome: personal characteristics as age and skin color (Model 1), demographic factors as socioeconomic class and education level (Model 2), and behavior factors as relationship status and number of visits to primary care in the last year (Model 3).
Analyses were performed using SAS software (Statistical Analysis System, SAS Institute Inc., Cary, N.C.), version 9.4, and statistical significance was defined as p < 0.05.
3. Results
Of the 8581 participants included in the study, 6366 were women. The mean age was 21.40 (95% CI 21.30-21.51) years. The majority defined themselves as mixed race/brown (56.76%, 95% CI 54.82-58.70) from social class C (55.75%, 95% CI 53.84-57.67), with a secondary education level (55.07%, 95% CI 53.13-57.00). Approximately 60% of participants visited the primary care unit 2 or more times in the last year, and differences between sexes were observed [women: 3 (IQR 1-5) and men: 2 (IQR 1-3), p = < 0.001] (data not shown).
3.1. HPV knowledge and vaccination
Overall, the mean percentage of correct answers was 51.79% (95% CI 50.90-52.67). Only 25% of participants correctly answered more than 68.75% of the questions. When compared the extreme quartiles, women had a higher proportion of correct answers about HPV and vaccination than men did (p = 0.0003) (Table 1). Moreover, the frequency of visits to primary care in the last year also had a positive influence on knowledge (p = 0.0013), as well as being divorced/widowed (p < 0.0001), being older than 20 years (p = 0.0018), having a higher education level (p < 0.0001) and being part of socioeconomic class A-B (p < 0.0001).
Table 1.
Characteristics of participants according to knowledge about human papillomavirus (HPV) and vaccination. POP-Brazil Study 2016–2017.
| Variables | Overall | Lower quartile |
Higher quartile |
p-valuea |
|---|---|---|---|---|
| Weighted % (n) | ||||
| Sex | 0.0003 | |||
| Female | 2616 | 51.91 (1506) | 48.09 (1110) | |
| Male | 1232 | 62.11 (793) | 37.89 (439) | |
| Age | 0.0018 | |||
| ≤ 20 years old | 1782 | 62.64 (1665) | 37.36 (617) | |
| Over 20 years old | 2066 | 53.48 (1134) | 46.52 (932) | |
| Race/skin color | 0.0666 | |||
| White | 934 | 51.12 (534) | 48.89 (400) | |
| Black | 576 | 62.71 (369) | 37.29 (207) | |
| Pardo | 2224 | 59.14 (1325) | 40.86 (899) | |
| Others | 84 | 47.75 (46) | 52.25 (38) | |
| Education level | <.0001 | |||
| Primary (some or complete) | 889 | 77.77 (691) | 22.23 (198) | |
| Secondary (some or complete) | 2080 | 57.55 (1274) | 42.45 (806) | |
| University level or higher | 878 | 31.03 (333) | 68.97 (545) | |
| Socioeconomic class | <.0001 | |||
| A-B | 746 | 45.34 (364) | 54.66 (382) | |
| C | 1980 | 54.19 (1147) | 45.81 (833) | |
| D-E | 1122 | 72.07 (788) | 27.93 (334) | |
| Relationship status | <.0001 | |||
| Single or without partner | 969 | 50.77 (518) | 49.23 (451) | |
| Dating or flirting | 1486 | 53.92 (829) | 46.08 (657) | |
| Married or living together | 1354 | 66.89 (928) | 33.11 (426) | |
| Divorced or widowed | 38 | 43.39 (23) | 56.61 (15) | |
| Number of visits to primary care in the last year | 0.0013 | |||
| 0 | 843 | 60.97 (535) | 39.03 (308) | |
| 1 | 780 | 64.81 (495) | 35.19 (295) | |
| 2 or 3 | 1112 | 54.99 (649) | 45.01 (463) | |
| ≥ 4 | 1111 | 52.72 (618) | 47.28 (493) | |
Chi-square test.
Regarding the characteristics associated with knowledge by sex, the multivariate model showed that among women, being black, being part of socioeconomic classes C and D/E, having a primary and secondary-level education, and did not visit the primary care unit were associated with low knowledge levels, whereas older age and to be dating or flirting were associated with high knowledge levels. Among men, primary and secondary education levels, divorced/widowed status, and number of visits to primary care were associated with having fewer correct answers (Table 2). When we excluded the vaccinated participants or included them in the adjustment, the results remained the same.
Table 2.
Multivariate analysis of characteristics associated with HPV knowledge by sex. POP-Brazil Study, 2016–2017.
| Variable | Prevalence ratio (95% Confidence Interval) |
|||||
|---|---|---|---|---|---|---|
| Women |
Men |
|||||
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| Age | ||||||
| ≤ 20 years old | 1 | 1 | 1 | 1 | 1 | 1 |
| Over 20 years old | 0.79 (0.71–0.88) | 0.89 (0.80–0.99) | 0.87 (0.78–0.97) | 0.91 (0.79–1.05) | 0.97 (0.85–1.10) | 0.94 (0.82–1.07) |
| Skin color/race | ||||||
| White | 1 | 1 | 1 | 1 | 1 | 1 |
| Black | 1.37 (1.15–1.64) | 1.23 (1.04–1.45) | 1.24 (1.05–1.45) | 1.12 (0.87–1.44) | 0.98 (0.79–1.23) | 0.98 (0.78–1.22) |
| Pardo | 1.12 (0.96–1.31) | 1.00 (0.87–1.16) | 0.99 (0.86–1.14) | 1.17 (0.97–1.43) | 1.12 (0.94–1.34) | 1.11 (0.93–1.33) |
| Others | 0.89 (0.56–1.40) | 0.85 (0.54–1.33) | 0.87 (0.56–1.37) | 0.93 (0.49–1.78) | 0.80 (0.47–1.37) | 0.84 (0.51–1.38) |
| Socioeconomic class | ||||||
| A-B | 1 | 1 | 1 | 1 | ||
| C | 1.30 (1.03–1.65) | 1.27 (1.00–1.60) | 0.89 (0.73–1.09) | 0.88 (073–1.08) | ||
| D-E | 1.46 (1.15–1.86) | 1.41 (1.11–1.80) | 1.12 (0.92–1.36) | 1.06 (0.87–1.29) | ||
| Education level | ||||||
| Primary (some or complete) | 2.44 (1.92–3.10) | 2.37 (1.85–3.03) | 2.28 (1.71–3.03) | 2.23 (1.69–2.96) | ||
| Secondary (some or complete) | 1.88 (1.49–2.38) | 1.86 (1.47–2.35) | 1.71 (1.30–2.26) | 1.72 (1.31–2.25) | ||
| University level or higher | 1 | 1 | 1 | 1 | ||
| Relationship status | ||||||
| Single or without partner | 0.87 (0.75–1.02) | 0.84 (0.70–1.01) | ||||
| Dating or flirting | 0.84 (0.75–0.96) | 0.95 (0.82–1.09) | ||||
| Married or living together | 1 | 1 | ||||
| Divorced or widowed | 0.61 (0.32–1.17) | 1.54 (1.24–1.91) | ||||
| Number of visits to primary care in the last year | ||||||
| 0 | 1.23 (1.07–1.42) | 1.21 (0.99–1.48) | ||||
| 1 | 1.08 (0.93–1.26) | 1.27 (1.04–1.55) | ||||
| 2 or 3 | 1.05 (0.91–1.20) | 1.09 (0.88–1.36) | ||||
| ≥ 4 | 1 | 1 | ||||
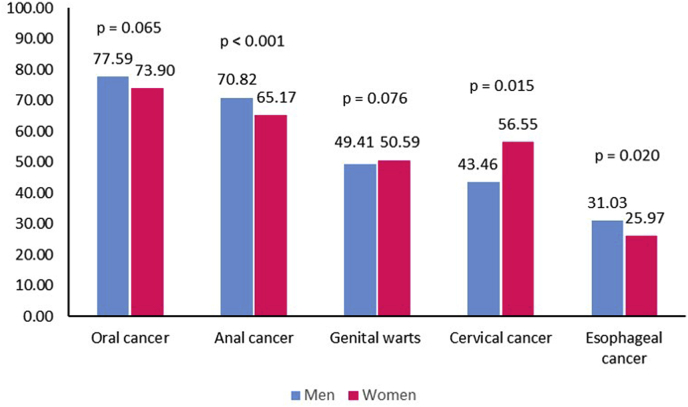
Approximately 46.30% (95% CI 44.14-48.46) of subjects believed that HPV has signs and symptoms; there were no significant differences between sexes (p = 0.164). Regarding HPV-related diseases, some differences between men and women's answers were noted (Fig. 1). Women were more aware of the association between HPV and cervical cancer, while men had more knowledge about the association between HPV and anal and esophageal cancer.
Fig. 1.
Knowledge on HPV-associated cancers according to sex. The answer option “don't know” was considered to be a missing value.
3.2. Attitudes toward and awareness about HPV vaccination
Of the 8577 participants, 7.48% (95% CI 6.69-8.27) were vaccinated against HPV. The scores for HPV knowledge among vaccinated subjects were significantly higher than those among nonvaccinated subjects [59.52% (95% CI 58.36-60.69) versus 51.17% (95% CI 50.0-51.65), respectively]. When differences between sexes were analyzed, 54.71% (n = 5618) of nonvaccinated women had correct answers, compared to 60.27% (n = 745) of vaccinated women (p < 0.001). A total of 47.90% (n = 2139) of nonvaccinated men had correct answers, compared to 55.26% (n = 75) of vaccinated men (p = 0.022) (data not shown).
The most common reasons for not receiving the vaccination were being outside of the age group covered by the public health system (41.01%, 95% CI 38.70-43.31), not knowing about the vaccine (22.53%, 95% CI 20.56-24.49), not having received medical advice about the vaccine (20.96%, 95% CI 19.17-22.74) and paying for the vaccine (6.11%, 95% CI 5.09-7.12). Only 2.79% (95% CI 1.97-3.61) were not vaccinated due to side effects. Among women, 97.70% (95% CI 97.07-98.32) reported that they would undergo a Pap smear even after receiving the vaccine.
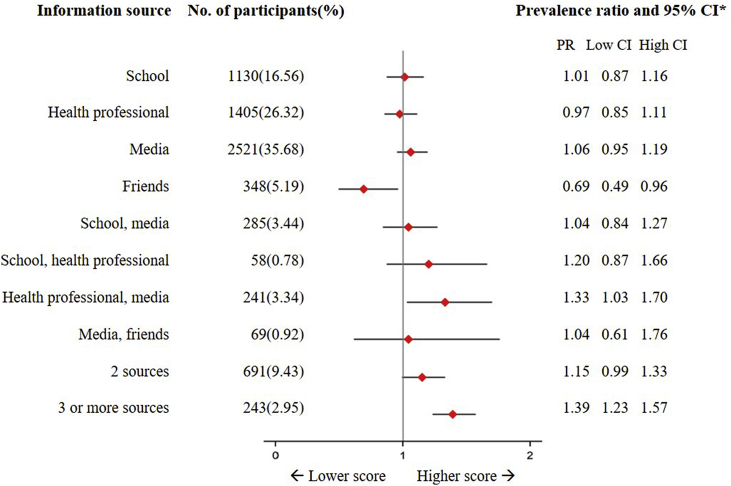
3.3. Information source
Of the participants, 75.91% (95% CI 74.13-77.69) reported that they had already been aware of HPV vaccination. Most participants were informed by the media (television, Internet and/or radio) [35.05% (95% CI 33.27-36.82)], followed by health professionals [25.03% (95% CI 23.32-26.74)], school [12.57% (95% CI 11.35-13.79) or friends [6.22% (95% CI 5.35-7.09)] (data not shown).
On the other hand, the information source associated with higher scores for HPV knowledge was the combination of both health professionals and the media. Participants informed by these two sources had a 33% increase in the number of correct answers in relation to those informed by other sources (1.33%, 95% CI 1.03-1.70). Being informed by friends was a risk factor for having less knowledge (0.69%, 95% CI 0.49-0.96). Those who were informed by two sources other than the media and health professionals did not show a significant difference in knowledge from participants informed by only one source (Fig. 2). The results remained similar when adjusted for the frequency of visits to primary care in the last year.
Fig. 2.
HPV knowledge and vaccination by information source. POP-Brazil Study, 2016–2017. *Weighted by sex and the size of the population in each capital.
In relation to HPV knowledge in women, being black, being of lower socioeconomic class and having a lower educational level were associated with having fewer correct answers. Among men, only primary and secondary education levels were risk factors for having fewer correct answers. The best information sources for HPV knowledge and vaccination were the combination of health professionals and the media (1.33%, 95% CI 1.03-1.70).
4. Discussion
This is the first nationwide study of young adults who use the public health system with the aim of evaluating knowledge about HPV and vaccination in Brazil. The factors associated with the percentage of correct answers about HPV differed by sex. Lower education level was the variable that most interfered with knowledge. Women scored higher than men, and the best information source was the combination of health professionals and the media.
More than 70% of young adults had awareness about HPV vaccination, which is similar to figures in other countries (87% in United Sates [19] and 75% in Italy [20]). Previous regionally restricted and specific population data have shown HPV vaccination knowledge varying from 49.7% [21] to 77.93% [22]. However, having awareness of HPV did not ensure knowledge. Although most of the participants were aware of the HPV vaccine, they had little knowledge about the infection, especially about the link between sexual behavior and HPV-related cancers.
Women reported having more knowledge about the HPV vaccine and the relationship between HPV and cervical cancer (56.56% in women vs. 43.43% in men) than men did, which is consistent with findings from other studies [21,[23], [24], [25]]. The number of correct answers is higher among women because the vaccination coverage that started in 2014 was only for female adolescents in Brazil. Vaccination coverage for males was not introduced into the public health system until 2017 [26]. Another possible factor is that women usually have more primary health care visits than men, as shown in the present study. However, this factor did not affect the number of correct answers.
Several factors may be important for HPV vaccination status, i.e., demographic and socioeconomic factors, individual beliefs and knowledge, and behavioral aspects [27]. However, for HPV knowledge, these results showed that lower social class and education level were important associated factors [21]. Skin color/race was also a risk factor for fewer correct answers [19], but only in women. Therefore, the most vulnerable population was the most affected.
Of the vaccination strategies adopted worldwide, vaccination was also made more available in primary care units and schools in Brazil [4]. Vaccination in schools is a proven strategy to increase vaccine coverage [8]. Brazil used this strategy in the first year of national vaccination and achieved very high coverage. In the subsequent year, the vaccinations were provided in primary care units, with a substantial decrease in coverage [1]. The school environment should be a place of discussion about sexual health and HPV, but such topics are considered taboo in Brazil [28]. The failure to include this theme in the curriculum may reflect the lack of influence of knowledge provided by schools in the study.
In 2017, the cumulative vaccine coverage of HPV in girls aged 9–14 years was 82.6% for the first dose but only 52.8% for the second dose. For boys aged 12 to 13, the level of vaccine coverage with the first dose was even lower (43.8%) [1]. In addition to information provided in school, coverage can also be increased through dissemination by the media and health professionals, as the combination of these two was found to be the best information source for more correct answers about HPV. Although the majority of participants were aware of HPV because of the media, as previously reported [21], knowledge from this single source was not significant, showing that information dissemination campaigns are important but not sufficient. Since knowledge about HPV is still low, it is recommended that teachers, parents, and health professionals educate young adolescents about the transmission of HPV as well as associated diseases and methods of preventing infection.
Despite being recognized as one of the most successful public health measures, vaccination is perceived as unsafe and unnecessary by a growing number of parents [29]. One of the arguments of the anti-vaccine movement that negatively impacted rates of coverage is the suspected side effects of the vaccine, but only 2.80% of participants reported being “afraid of its side effects” in this study. In addition, almost all women reported that they would undergo cytopathological exams even after receiving the vaccine. This observation may temper concerns that vaccination against HPV is likely to decrease cervical cancer screening behaviors [30].
The strength of this study is the nationwide sampling, with the inclusion of a large and diverse population. Furthermore, the data were collected face to face, in contrast to the data collection in most previous studies [31]. However, the study has some limitations. Several studies have already evaluated knowledge about HPV but used different forms of evaluation. There is no standardized method for the evaluation of knowledge. In this study, we used a scoring procedure because we believe that it is more appropriate than evaluating knowledge with only one question. Although the study participants were recruited from public health units, the study included participants of all social classes, with a distribution similar to that of the Brazilian population [18]. Finally, it is important to emphasize that a large portion of the studied participants were not the targets of the vaccination.
In conclusion, the results reinforce the importance of educational interventions in the population, especially among the socially disadvantaged, to provide adequate information about the virus and vaccination. These findings can complement public health surveillance data on increasing the vaccination rate in the country.
Conflicts of interest
None.
Contributors
NLK and EMW contributed substantially to the conception and design of the work; NLK wrote the first draft; MB conducted the data analyses; all authors contributed to the interpretation of the data and approved the final version published, with EMW, GFH, JDCH, CMD, AGKM, FLAS, ASB, and GFP primarily responsible for revising the drafts for publication.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pvr.2019.03.003.
Funding source
This study was supported by the Hospital Moinhos de Vento in a partnership with the Department of Surveillance, Prevention and Control of Sexually Transmitted Infections, HIV/AIDS and Viral Hepatitis, of the Secretariat for Health Surveillance of the Brazilian Ministry of Health through the Program for Institutional Development of the Brazilian Unified Health System (PROADI-SUS).
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.da Saúde Ministério. 2016. Boletim Informativo Do PNI-02/2016 Vacinação Contra HPV. [Google Scholar]
- 2.Bruni L., Diaz M., Barrionuevo-Rosas L., Herrero R., Bray F., Bosch F.X. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob. Health. 2016;4:e453–463. doi: 10.1016/S2214-109X(16)30099-7. [DOI] [PubMed] [Google Scholar]
- 3.Arbyn M., Xu L., Simoens C., Martin-Hirsch P.P. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst. Rev. 2018;5:CD009069. doi: 10.1002/14651858.CD009069.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hofstetter A.M., Rosenthal S.L. Factors impacting HPV vaccination: lessons for health care professionals. Expert Rev. Vaccines. 2014;13:1013–1026. doi: 10.1586/14760584.2014.933076. [DOI] [PubMed] [Google Scholar]
- 5.Pereira R.G.V., Machado J.L.M., Machado V.M., Mutran T.J., Dos santos L.S., Oliveira E. A influência do conhecimento na atitude frente à vacina contra o Papilomavírus Humano: ensaio clínico randomizado. ABCS Health Sci. 2016;41 [Google Scholar]
- 6.Zhang Y., Wang Y., Liu L., Fan Y., Liu Z., Wang Y. Awareness and knowledge about human papillomavirus vaccination and its acceptance in China: a meta-analysis of 58 observational studies. BMC Public Health. 2016;16:216. doi: 10.1186/s12889-016-2873-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neto C., Augusto Coelho Braga N., Delgado Campos J., Ramos Rodrigues R., Golçalves Guimarães K., Luiza Sobreira Sena A. Atitudes dos pais diante da vacinação de suas filhas contra o HPV na prevenção do câncer de colo do útero. Cad. Saúde Coletiva. 2016;24:248–251. [Google Scholar]
- 8.Stokley S. Interventions to improve adolescent vaccination coverage. J. Adolesc. Health. 2015;56:S3–S4. doi: 10.1016/j.jadohealth.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 9.WHO . 2016. Global Health Sector Strategy on Sexually Transmitted Infections, 2016-2021; p. 60. [Google Scholar]
- 10.Bruni L., Barrionuevo-Rosas L., Albero G., Serrano B., Mena M., Gómez D., Muñoz J., Bosch F.X., de Sanjosé S. 27 July 2017. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the World. Summary Report. (n.d) [Google Scholar]
- 11.World Health Organization (WHO) Human papillomavirus vaccines: WHO position paper, May 2017-Recommendations. Vaccine. 2017;35:5753–5755. doi: 10.1016/j.vaccine.2017.05.069. [DOI] [PubMed] [Google Scholar]
- 12.Wendland E.M., Caierão J., Domingues C., Maranhão A.G.K., De Souza F.M.A., Hammes L.S. POP-Brazil study protocol: a nationwide cross-sectional evaluation of the prevalence and genotype distribution of human papillomavirus (HPV) in Brazil. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-021170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Editors TPM Observational Studies: getting clear about transparency. PLoS Med. 2014;11 doi: 10.1371/journal.pmed.1001711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horvath J.D.C., Kops N.L., Caierão J., Bessel M., Hohenberger G., Wendland E.M. Human papillomavirus knowledge, beliefs, and behaviors: a questionnaire adaptation. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018;0 doi: 10.1016/j.ejogrb.2018.09.023. [DOI] [PubMed] [Google Scholar]
- 15.Critério Brasil - Associação Brasileira de Empresas de Pesquisa (ABEP) 2018. http://www.abep.org/criterio-brasil [Google Scholar]
- 16.Saulle R., Miccoli S., Unim B., Semyonov L., Giraldi G., Vito E.D. Validation of a questionnaire for young women to assess knowledge, attitudes and behaviors towards cervical screening and vaccination against HPV: survey among an Italian sample. Epidemiol. Biostat. Public Health. 2014;11 [Google Scholar]
- 17.Ayres A.R.G., e Silva G.A. Cervical HPV infection in Brazil: systematic review. Rev. Saude Publica. 2010;44:963–974. doi: 10.1590/s0034-89102010000500023. [DOI] [PubMed] [Google Scholar]
- 18.IBGE . 2016. Coordenação de Trabalho e Rendimento. Pesquisa nacional por amostra de domicílios: síntese de indicadores. [Google Scholar]
- 19.Ragin C.C., Edwards R.P., Jones J., Thurman N.E., Hagan K.L., Jones E.A. Knowledge about human papillomavirus and the HPV vaccine – a survey of the general population. Infect. Agents Cancer. 2009;4:S10. doi: 10.1186/1750-9378-4-S1-S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sopracordevole F., Cigolot F., Gardonio V., Di Giuseppe J., Boselli F., Ciavattini A. Teenagers' knowledge about HPV infection and HPV vaccination in the first year of the public vaccination programme. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2012;31:2319–2325. doi: 10.1007/s10096-012-1571-4. [DOI] [PubMed] [Google Scholar]
- 21.Abreu M.N.S., Soares A.D., Ramos D.A.O., Soares F.V., Nunes Filho G., Valadão A.F. Knowledge and perception of HPV in the population over 18 years of age in the city of Ipatinga – state of Minas Gerais, Brazil. Ciênc. Amp. Saúde Coletiva. 2018;23:849–860. doi: 10.1590/1413-81232018233.00102016. [DOI] [PubMed] [Google Scholar]
- 22.Freitas W.R., Fedrizzi E.N., Aguiar F.G. Knowledge among college students and employees of local health units about human papillomavirus and cervical cancer and its implications for public health strategies and vaccination. J. Bras. Doenças Sex Transm. 2015;27:40–47. [Google Scholar]
- 23.Rashid S., Labani S., Das B.C. Knowledge, awareness and attitude on HPV, HPV vaccine and cervical cancer among the college students in India. PLoS One. 2016;11 doi: 10.1371/journal.pone.0166713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen L., Song Y., Ruan G., Zhang Q., Lin F., Zhang J. Knowledge and attitudes regarding HPV and vaccination among Chinese women aged 20 to 35 Years in Fujian province: a cross-sectional study. Cancer Control J. Moffitt Cancer Cent. 2018;25 doi: 10.1177/1073274818775356. 1073274818775356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kontos E.Z., Emmons K.M., Puleo E., Viswanath K. Contribution of communication inequalities to disparities in human papillomavirus vaccine awareness and knowledge. Am. J. Public Health. 2012;102:1911–1920. doi: 10.2105/AJPH.2011.300435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.da Saúde Ministério. 2018. Secretaria de Vigilância em Saúde. Informe técnico da ampliação da oferta das vacinas papilomavírus humano 6, 11, 16 e 18 (recombinante) – vacina HPV quadrivalente e meningocócica C (conjugada) [Google Scholar]
- 27.Grandahl M., Larsson M., Dalianis T., Stenhammar C., Tydén T., Westerling R. Catch-up HPV vaccination status of adolescents in relation to socioeconomic factors, individual beliefs and sexual behaviour. PLoS One. 2017;12 doi: 10.1371/journal.pone.0187193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.da Silva A.K.L.S. Diversidade sexual e de gênero: a construção do sujeito social. Rev. NUFEN. 2013;5:12–25. [Google Scholar]
- 29.Dubé E., Vivion M., MacDonald N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Expert Rev. Vaccines. 2015;14:99–117. doi: 10.1586/14760584.2015.964212. [DOI] [PubMed] [Google Scholar]
- 30.Udesky L. Push to mandate HPV vaccine triggers backlash in USA. Lancet. 2007;369:979–980. doi: 10.1016/S0140-6736(07)60475-9. [DOI] [PubMed] [Google Scholar]
- 31.Caskey R., Lindau S.T., Alexander G.C. Knowledge and early adoption of the HPV vaccine among girls and young women: results of a national survey. J. Adolesc. Health. 2009;45:453–462. doi: 10.1016/j.jadohealth.2009.04.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.