Abstract
Neuropathic pain is a chronic debilitating symptom characterized by spontaneous pain and mechanical allodynia. It occurs in distinct forms, including brush-evoked dynamic and filament-evoked punctate mechanical allodynia. Potassium channel 2.1 (Kir2.1), which exhibits strong inward rectification, is and regulates the activity of lamina I projection neurons. However, the relationship between Kir2.1 channels and mechanical allodynia is still unclear. In this study, we first found that pretreatment with ML133, a selective Kir2.1 inhibitor, by intrathecal administration, preferentially inhibited dynamic, but not punctate, allodynia in mice with spared nerve injury (SNI). Intrathecal injection of low doses of strychnine, a glycine receptor inhibitor, selectively induced dynamic, but not punctate allodynia, not only in naïve but also in ML133-pretreated mice. In contrast, bicuculline, a GABAA receptor antagonist, induced only punctate, but not dynamic, allodynia. These results indicated the involvement of glycinergic transmission in the development of dynamic allodynia. We further found that SNI significantly suppressed the frequency, but not the amplitude, of the glycinergic spontaneous inhibitory postsynaptic currents (gly-sIPSCs) in neurons on the lamina II-III border of the spinal dorsal horn, and pretreatment with ML133 prevented the SNI-induced gly-sIPSC reduction. Furthermore, 5 days after SNI, ML133, either by intrathecal administration or acute bath perfusion, and strychnine sensitively reversed the SNI-induced dynamic, but not punctate, allodynia and the gly-sIPSC reduction in lamina IIi neurons, respectively. In conclusion, our results suggest that blockade of Kir2.1 channels in the spinal dorsal horn selectively inhibits dynamic, but not punctate, mechanical allodynia by enhancing glycinergic inhibitory transmission.
Keywords: Dynamic allodynia, ML133, Kir2.1 channel, Glycinergic transmission, Spared nerve injury
Introduction
Neuropathic pain is a chronic debilitating symptom that follows nerve injury, persists long after the initial injury has subsided, affects 7%–10% of the general population, and decreases the quality of life of patients [1]. There are two hallmarks of neuropathic pain – spontaneous pain and mechanical allodynia, which is a painful response to an innocuous stimulus [2]. Mechanical allodynia occurs in multiple forms in humans including dynamic, punctate, and static. Several studies have suggested that the distinct pain types arise through different pathophysiological mechanisms [3]. Dynamic allodynia is caused by moving, non-painful light pressure stimuli and is mediated by low-threshold mechanoreceptors. Punctate allodynia, measured by the von Frey assay, is evoked by non-painful punctate pressure and signaled by both thin unmyelinated C fibers and myelinated Aβ fibers. Static allodynia, different from punctate alloodynia, is considered to be evoked by pressure generated by a large probe and mediated by unmyelinated C fibers [4–6]. In the past decades, most efforts have focused on the mechanism underlying punctate allodynia, and little is known about dynamic allodynia. However, in the clinic, most patients with post-herpetic neuralgia suffer from dynamic allodynia and lack an effective therapy [7, 8]. In a previous study, we demonstrated that spinal circuits with neurons expressing vesicular glutamate transporter 3 are preferentially involved in dynamic mechanical pain, but not punctate allodynia [6]. However, the underlying mechanisms involved in the distinct forms of mechanical allodynia, including dynamic allodynia, remain unclear. Thus, it is imperative to investigate the mechanism underlying dynamic mechanical allodynia and provide new strategies for its treatment.
The gate control theory of pain was first proposed by Melzack and Wall, who suggested that touch normally inhibits acute pain through the direct activation of inhibitory interneurons [9]. Both GABAergic and glycinergic inhibitory interneurons are widely distributed in the superficial dorsal horn and are essential as the gate to prevent touch from turning into pain. Nerve injury can result in a decrease of inhibitory control, which instead allows touch to directly activate pain circuits [10]. The majority of lamina I projection neurons that express the receptor for neurokinin 1 respond to noxious stimuli, and these neurons are predominantly regulated by GABA. In pathophysiological pain states, GABA inhibition is suppressed in dorsal horn nociceptive neurons, and this leads to neuronal hyperexcitability [11]. It has been proposed that excitatory interneurons expressing protein kinase C gamma (PKCγ) in inner lamina II (lamina IIi) are involved in spinal transmission to lamina I projection neurons [12]. They receive both Aβ primary afferent and inhibitory input, especially glycinergic inhibitory input [13]. Glycinergic inhibition is decreased in PKCγ neurons after nerve injury and intrathecal (i.t.) administration of the glycine receptor antagonist strychnine in naïve mice induces mechanical allodynia [14]. Facial dynamic mechanical allodynia, measured by the air-puff method, can be evoked by intracisternal injection of strychnine, and this type of allodynia is morphine-resistant. This is caused by dysfunction of glycine inhibition of PKCγ interneurons and turns touch into dynamic pain [15]. Dynamic mechanical allodynia is mediated by Aβ fibers which mainly innervate into laminae III-VI with some extension to lamina IIi [16]; this is in accord with the distribution of glycinergic neurons [17]. Foster and colleagues demonstrated strong innervation of dorsal horn glycinergic neurons by non-nociceptive sensory neurons [18]. However, the relationship between the inhibitory regulation in the dorsal horn and the development of dynamic mechanical allodynia remains unclear.
Potassium channel-2.1 (Kir2.1) is constitutively active and exhibits strong inward rectification. It is involved in the establishment of a hyperpolarized resting membrane potential and long-lasting action potential plateau in various cells such as cardiac cells [19]. The inward rectification is caused by intracellular ions such as Mg2+ and polyamines which block the pore structure of Kir2.1 channels [20]. In hippocampal neurons and neonatal rat spinal motor neurons, Kir currents are detectable and thought to contribute to maintenance of the resting potential and regulation of the excitability of the neurons. Furthermore, blockade of Kir channels in isolated neurons from brain slices results in depolarization and initiates action potential firing [21]. In the spinal cord, Kir2.1 channels are scattered in the gray matter of the dorsal and ventral horns [22], which raises the possibility that glycinergic neurons express Kir2.1 channels. In addition, reduced conductance through Kir2.1 channels near physiological potential is an essential determinant of intrinsic burst-firing in lamina I neurons during early life, which are involved in pain networks [23]. Accordingly, Kir2.1 channels contribute to shaping the output of lamina I projection neurons to the parabrachial nucleus and the periaqueductal gray and regulating nociceptive information in the immature spinal cord [24]. However, the role of Kir2.1 channels in regulating mechanical pain is still uncertain. Whether Kir2.1 regulates spinal glycinergic neuron activity remains to be studied.
Thus, the aim of this study was to investigate the mechanism underlying dynamic mechanical allodynia, which might further contribute to the treatment of clinical dynamic pain. Our results showed that blockade of spinal Kir2.1 channels by ML133, a selective Kir2.1 blocker, enhanced glycinergic transmission to compensate for spared nerve injury (SNI)-induced reduction of glycinergic transmission, which, in turn, resulted in inhibition of the dynamic, but not punctate, allodynia in the SNI mouse model.
Materials and Methods
Animals
All experiments were performed on adult male C57BL/6J mice (6–8 weeks old) from Shanghai SLAC Laboratory Animal Co., Ltd. The mice were maintained at room temperature (RT, 25°C) in a pathogen-free environment with a 12 h/12 h light/dark cycle and ad libitum access to food and water. All animal experiments, including behavioral tests, were approved by the Committee of Animal Use for Research and Education of Fudan University (Shanghai, China).
Surgery and Drug Administration
Surgery to establish the SNI mouse model was performed as described previously [25, 26]. Briefly, mice were anaesthetized with isoflurane (3% induction, 2% maintenance). A 1-cm skin and muscle incision was made in the left thigh to expose the left sciatic nerve. Then, the tibial and common peroneal nerves were ligated and transected distal to the ligature. The third branch, the sural nerve, was left intact and stretch or contact carefully avoided. In the sham controls, the sciatic nerve and its branches were identically exposed without ligation and transection. After surgery, the mice were observed in the home cage until they were able to take food and water. All drugs were administered i.t. in a volume of 10 μL. ML133 (S2825; Selleckchem, Houston, TX) was dissolved in dimethylsulfoxide (200 mmol/L) and diluted in normal saline to the final concentrations of 0.3 mmol/L, 1 mmol/L, and 3 mmol/L before i.t. administration. For pretreatment with ML133, mice received ML133 30 min prior to surgery. For post-SNI treatment, mice received ML133 once a day from days 5 to 7 after surgery.
Behavioral Testing
Behavioral pain testing was as described in our previous study [6]. Mice were placed on an elevated wire grid apparatus for 30 min/day for 3 consecutive days to acclimate to the testing environment before baseline measurement. Experimenters were blind to the drug treatment during testing. After baseline testing, mice underwent surgery and were tested for punctate and dynamic allodynia in the lateral plantar region of the hindpaw, which was mediated by the sural nerve remaining after SNI surgery. Von Frey assays were used to evaluate the punctate mechanical allodynia. The lateral plantar surface of the hindpaw was stimulated with a series of calibrated von Frey filaments (0.02 g–1 g). Three positive responses in 5 trials at 3-min intervals for each stimulus intensity were considered a nociceptive response. The paw-withdrawal threshold (PWT) was determined according to Dixon’s up-down method [27]. To measure dynamic allodynia, mice were lightly stroked on the lateral plantar region with a paintbrush, in the heel-to-toe direction. The paintbrush was prepared by smoothing the tip and removing the outer layer of hairs. We repeated the test three times at 10-s intervals to obtain the average score for each mouse. The scoring system was as follows: 0: walking away or occasional, very brief paw-lifting within 1 s (as for normal touch behavior); 1: sustained lifting (> 2 s) of the stimulated paw toward the body; 2: strong lateral paw lift above the level of the body; 3: multiple flinching or licking of the stimulated paw.
Preparation of Spinal Cord Slices
As previously described [28], mice (6–8 weeks at the time of slice preparation) were deeply anesthetized with pentobarbital sodium (0.1 g/kg, i.p.) and then perfused transcardially with oxygenated ice-cold sucrose-based artificial cerebrospinal fluid (ACSF) that contained (mmol/L): 75 sucrose, 80 NaCl, 2.5 KCl, 25 NaHCO3, 0.5 CaCl2, 3.5 MgCl2, 1.25 NaH2PO4, 1.3 sodium ascorbate, and 3 pyruvate, pH 7.4 and osmolarity 310 mOsm/L–320 mOsm/L. The lumbar region of the spinal cord was quickly exposed and removed. Transverse 350-μm slices were cut on a vibratome (VT1200s; Leica, Wetzlar, Germany) and transferred to a submerged chamber containing oxygenated N-methyl-D-glucamine-based recovery ACSF (for 15 min at 34°C) composed of (mmol/L): 92 N-desmethylclozapine, 2.5 KCl, 1.2 NaH2PO4, 20 HEPES, 30 NaHCO3, 25 D-glucose, 5 sodium ascorbate, 5 pyruvate, 2 thiourea, 10 MgSO4, 0.5 CaCl2 adjusted to pH 7.4 with HCl. The slices were then incubated in normal oxygenated ACSF for 45 min at 34°C and then maintained at RT for at least 30 min to recover. Normal ACSF contained (mmol/L): 125 NaCl, 2.5 KCl, 2 CaCl2, 1 MgCl2, 1.25 NaH2PO4, 26 NaHCO3, 25 D-glucose, 1.3 ascorbate, and 3 pyruvate, equilibrated with 95% O2 and 5% CO2.
Electrophysiological Recordings
Slices were transferred to a recording chamber and continuously perfused with normal ACSF at 5 mL/min at RT. A transparent band in the dorsal horn was considered to be lamina II using infrared differential interference contrast video microscopy under an upright microscope equipped with a CCD camera. Neurons in the inner part of lamina II were identified as lamina IIi neurons. To record the glycinergic spontaneous inhibitory postsynaptic currents (gly-sIPSCs), patch pipettes (3 MΩ–5 MΩ) pulled from borosilicate glass (Sutter Instruments, Novato, CA) were filled with a Cs+-based internal solution, which contained (mmol/L): 140 CsCl, 10 EGTA, 5 HEPES, 2 CaCl2, 2 MgATP, 0.3 NaGTP, 5 QX-314.Cl adjusted to pH 7.2–7.3 with CsOH and osmolarity 300 mOsm/L–310 mOsm/L. Under perfusion with normal ACSF, neurons were recorded at a holding potential of −70 mV. Gly-sIPSCs were recorded in the presence of DNQX, AP5, and bicuculline. After recording for 5 min, ML133 (100 μmol/L) was added to the bath perfusion solution. To record Kir currents, patch pipettes were filled with (mmol/L) 130 K+-gluconate, 5 KCl, 0.5 EGTA, 20 HEPES, 4 NaATP, and 0.5 NaGTP adjusted to pH 7.2–7.3 with KOH and osmolarity 300 mOsm/L–310 mOsm/L. The neurons were held at −70 mV in the presence of DNQX (20 μmol/L), AP5 (25 μmol/L), bicuculline (10 μmol/L), strychnine (2 μmol/L), and tetrodotoxin (1 μmol/L). The Kir currents were recorded through a series of step command potentials from −60 mV to −160 mV at 10-mV steps and a pulse-width of 200 ms. Data were acquired using a MultiClamp 700B patch-clamp amplifier (Axon Instruments, Sunnyvale, CA). The drug effect on the frequency and amplitude of gly-sIPSCs was measured using Clampfit 10.0 and Mini 60 software (Molecular Devices, Sunnyvale, CA).
Immunostaining
For immunohistochemistry, deeply anesthetized mice were sacrificed and perfused transcardially with normal saline followed by 4% paraformaldehyde (PFA, Sigma, Darmstadt, Germany). The spinal cord was removed and post-fixed in 4% PFA for 2 h and submerged in 15% then 30% sucrose for dehydration. Coronal lumbar sections were cut at 40 μm on a freezing microtome (Leica). The sections were permeabilized and blocked for 2 h in 0.3% Triton X-100 (Sigma) and 10% normal donkey serum (Millipore, Darmstadt, Germany) in phosphate-buffered saline. Then the sections were incubated with mouse anti-Kir2.1 antibody (1:200, ab85492; Abcam, London, UK) and rabbit anti-NeuN antibody (1:1000, R-3770-100; Novus Biologicals, Littleton, CO) overnight at 4°C. After rinsing, sections were incubated with secondary antibodies (1:500, Alexa Fluor 488 for neuN and Alexa Fluor 594 for Kir2.1, Invitrogen, Waltham, MA) for 2 h at RT. Then the sections were rinsed, mounted on slides, and coverslipped with antifade agent. Fluorescence images were captured through the 25× objective of a confocal microscope (Nikon, Tokyo, Japan).
Western Blot
Mice were deeply anesthetized and the lumbar cord was quickly removed and placed in ice-cold ACSF. Then the left dorsal horn was isolated and homogenized in pre-cooled lysis buffer (#K268-50; Biovision, Milpitas, CA). The membrane proteins were extracted using a Membrane Protein Extraction Kit (#K268-50; Biovision). The protein concentration was measured using a bicinchoninic acid protein assay kit (Beyotime, Haimen, China). Membrane protein was separated on 10% SDS-PAGE gels and electrophoretically transferred to polyvinylidene fluoride membranes (Millipore, Darmstadt, Germany). Then the membrane was blocked in 5% skimmed milk for 2 h and incubated with the primary antibodies rabbit anti-Kir2.1 (1:1000, ab65796; Abcam), rabbit anti-GAPDH (1:1000, #2118; Cell Signaling Technology, Danvers, MA) in 5% skimmed milk overnight at 4°C, followed by incubation with secondary goat anti-rabbit (1:20000; Jackson ImmunoResearch, West Grove, PA). Bands were visualized by an ECL detection system (Pierce, Rockford, IL). The intensity of individual bands was measured by AlphaView (Protein Simple, San Jose, CA) and normalized to GAPDH.
Data Analysis
Results are presented as mean ± SEM. Statistical analysis was performed using GraphPad Prism (La Jolla, CA). For mechanical allodynia assessment, data were analyzed by two-way ANOVA with Bonferroni post-tests. For electrophysiological assays, comparisons of acute perfusion in the same group were made using the paired t test, and comparisons of different groups were made using the two-tailed unpaired t test. Significance was set at P <0.05.
Results
Intrathecal ML133 Pretreatment Selectively Inhibited SNI-Induced Dynamic, but not Punctate, Mechanical Allodynia
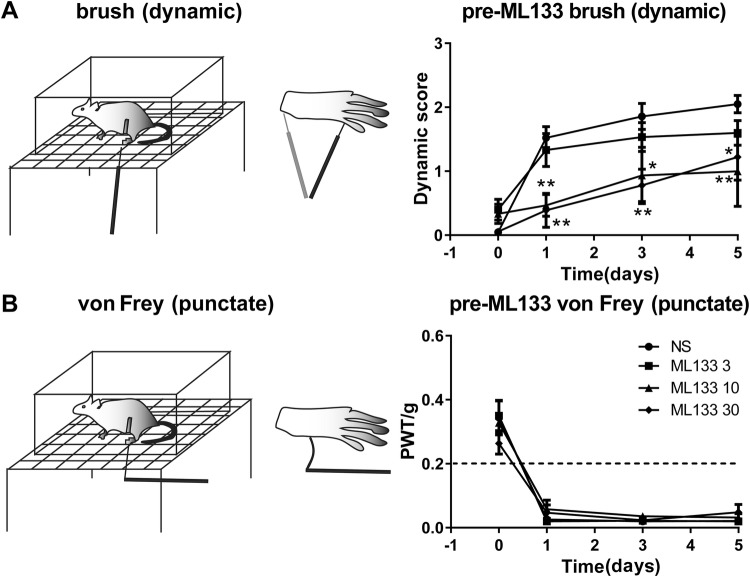
The SNI model is one of the classic neuropathic pain models, which induces long-lasting ipsilateral mechanical allodynia. As we reported previously [6], SNI surgery induced two forms of allodynia: brush-evoked dynamic and filament-evoked punctate allodynia. Pre-treatment with i.t. injection of ML133, a Kir2.1 channel inhibitor, at 3 nmol, 10 nmol, and 30 nmol before SNI, dose-dependently attenuated the brush-evoked dynamic score (Fig. 1A), but, surprisingly, had no effect on the von Frey filament-evoked PWT, and this lasted for up to 5 days after SNI (Fig. 1B). The lowest dose of ML133 (3 nmol) had no effect on dynamic and punctate allodynia; however, 10 nmol and 30 nmol preferentially attenuated the dynamic score, but not the von Frey-evoked PWT. These results indicated that blockade of spinal kir2.1 channels with ML133 prevents the development of dynamic, but not punctate, allodynia after SNI.
Fig. 1.
Effects of ML133 pretreatment on the development of dynamic and punctate allodynia. A Schematics of brush-evoked dynamic allodynia. Pretreatment with ML133 (3 nmol, 10 nmol, 30 nmol, i.t.) prevented the development of dynamic allodynia in SNI mice (normal saline (NS), n = 7; ML133 3, n = 5; ML133 10, n = 5; ML133 30, n = 6; NS versus ML133 3 nmol, P > 0.05; NS vs ML133 10 nmol, P < 0.05; NS vs ML133 30 nmol, P < 0.05, two-way ANOVA with Bonferroni post-hoc). B Schematics of von Frey filament-evoked punctate allodynia. Pretreatment with ML133 (3 nmol, 10 nmol, 30 nmol, i.t.) had no effect on punctate allodynia (NS vs ML133 3 nmol, P > 0.05; NS vs ML133 10 nmol, P > 0.05; NS vs ML133 30 nmol, P > 0.05, two-way ANOVA with Bonferroni post-hoc). Graphs show mean ± SEM. *P < 0.05, **P < 0.01.
Blockade of Spinal Glycinergic Transmission Selectively Induced Transient Dynamic but not Punctate Allodynia
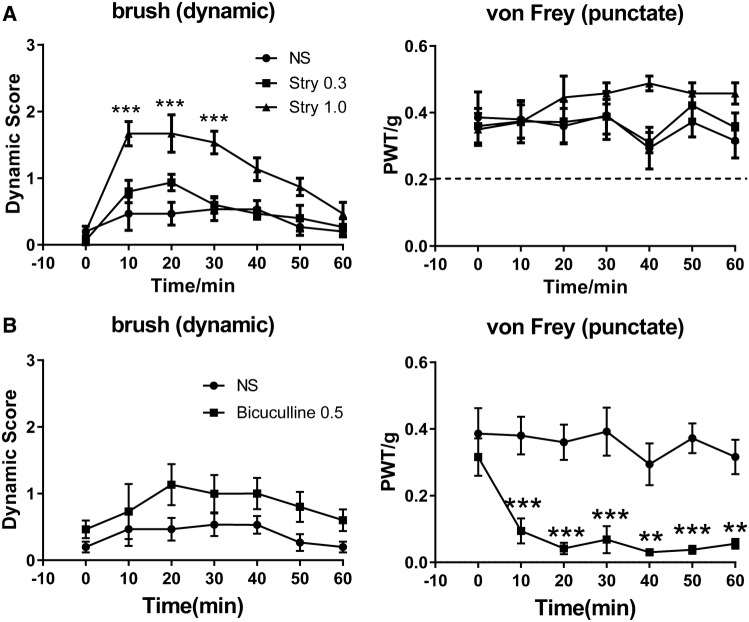
Both spinal glycinergic and GABAergic transmission play key roles in modulating pain processing [17, 29]. Previous studies have reported that intracisternal injection of strychnine, a specific glycine receptor antagonist, selectively induces dynamic, but not punctate, allodynia in both the face [15] and the trigeminal distribution [30]. To further clarify the relationship between glycinergic transmission in the spinal cord and the different forms of mechanical allodynia, we studied the pain behavior of mice after i.t. administration of strychnine. The result showed that the effect of strychnine was dose-dependent and selective for dynamic allodynia at a low dose. Strychnine at the low dose of 0.3 nmol was insufficient to evoke either punctate or dynamic allodynia. Surprisingly, when strychnine was injected at 1 nmol (~3 μg), it only evoked brush-evoked dynamic allodynia; the pain score increased at 20 min and recovered after 50 min. However, the von Frey-evoked punctate threshold remained normal (Fig. 2A).
Fig. 2.
Effects of intrathecal strychnine on naïve mice. A Strychnine at 1.0 nmol induced transient dynamic allodynia in naïve mice, but did not change the dynamic score at 0.3 nmol (n = 5/group, normal saline (NS) vs strychnine (Stry) 0.3 nmol, P = 0.3836; NS vs Stry 1 nmol, P < 0.01). Strychnine at 0.3 nmol and 1.0 nmol had no effect on paw withdrawal threshold (NS vs Stry 0.3 nmol, P > 0.05; NS vs Stry 1 nmol, P > 0.05). B Intrathecal bicuculline at 0.5 nmol induced a decrease of paw withdrawal threshold (n = 5/group, NS vs bicuculline 0.5 nmol, P > 0.05), but did not change the dynamic score (NS vs bicuculline 0.5 nmol, P > 0.05). Graphs show the mean ± SEM. **P < 0.01, ***P < 0.001, two-way ANOVA with Bonferroni post-hoc test.
Bicuculline at 0.5 nmol i.t., in contrast, only induced punctate, but not dynamic allodynia (Fig. 2B). Therefore, these results suggested that dynamic allodynia is likely more sensitive to glycinergic transmission dysfunction and blockade of spinal glycinergic transmission selectively induces dynamic allodynia. In contrast, punctuate mechanical allodynia might be more sensitive to modulation by GABAergic transmission.
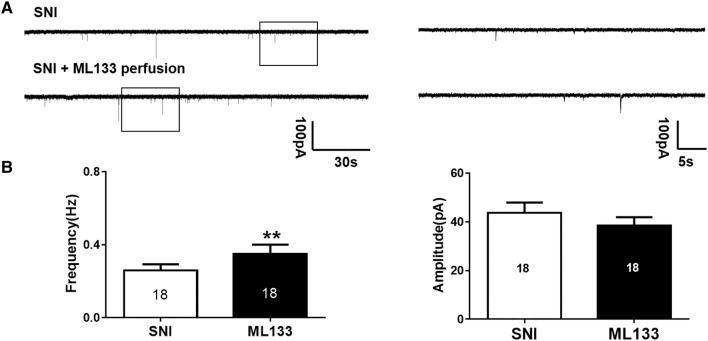
Acute ML133 Perfusion Increased Glycinergic Neurotransmission in Spinal Cord Lamina IIi Neurons in vitro
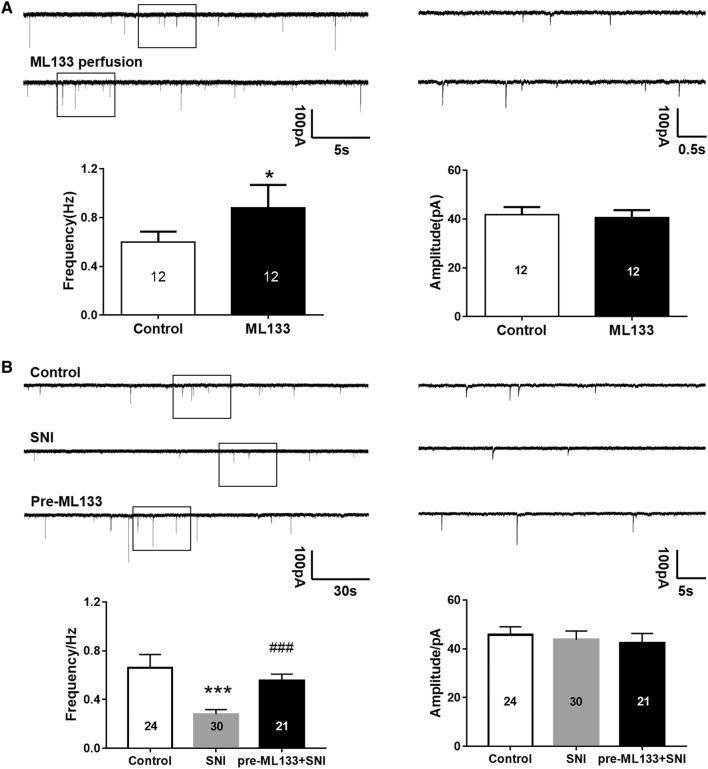
Since the above results showed that SNI surgery and the application of strychnine alone had a similar effect of evoking dynamic allodynia, and blocking the Kir2.1 channel with ML133 reversed the SNI-induced dynamic allodynia, we hypothesize that SNI reduces, and ML133 enhances, glycinergic transmission in the dorsal horn to modulate the development of dynamic allodynia after SNI. Thus, to understand the relationship between Kir2.1 and glycinergic transmission, we used patch-clamp in spinal cord slices to record gly-sIPSCs from lamina IIi neurons. First, we measured the effect of acute perfusion with ML133 (100 μmol/L) on gly-sIPSCs in naive mice. Our results showed that acute perfusion with ML133 significantly increased the frequency of gly-sIPSCs, but did not affect their amplitude (Fig. 3A). This result demonstrated that acute blockade of the Kir2.1 channel enhances glycinergic transmission in lamina IIi neurons in the dorsal horn.
Fig. 3.
Effect of pretreatment with ML133 in vivo on glycinergic sIPSCs (gly-sIPSCs) in SNI mice. A Effect of acute perfusion with ML133 (100 μmol/L) on lamina IIi gly-sIPSCs (n = 12). Upper panels: left, raw traces of whole-cell patch clamp recording of glycinergic sIPSCs in a lamina IIi neuron before and after ML133 perfusion in control mice; right, amplification of raw traces from boxes at left. Lower panels: SNI reduced the frequency (P < 0.05#), but not the amplitude (P = 0.6399#), of the glycinergic sIPSCs. B Effect of SNI surgery and pretreatment with ML133 (30 nmol, i.t.) on gly-sIPSCs recorded from two lamina IIi neurons 5 days after SNI (Control, n = 24; SNI, n = 30; pre-ML133: n = 21). Upper panels: left, sample traces of gly-sIPSCs from different groups; right, amplified traces from boxes at left. Lower panels: SNI profoundly reduced the frequency (P < 0.001#), but not the amplitude, of gly-sIPSCs (P > 0.05#) in dorsal horn lamina IIi neuron. Treatment with ML133 before SNI remarkably increased the gly-sIPSC frequency (P < 0.001#), but had no effect on amplitude (unpaired t tests, P > 0.05). Graphs represent the mean ± SEM. *P < 0.05, ***P < 0.001, ###P < 0.001. #paired t tests, # unpaired t tests.
SNI Reduced and Pretreatment with ML133 Retained the Glycinergic Transmission in Spinal Lamina IIi Neurons
Next, we recorded gly-sIPSCs from both control and SNI mice at day 5 after surgery. Compared to the control group, the frequency of gly-sIPSCs remarkably decreased in the SNI group, while the amplitude did not change (Fig. 3B). This indicated that inhibitory transmission is damped in the SNI condition. Then, to verify the mechanism underlying the effect of pretreatment with ML133 on dynamic allodynia, we measured the gly-sIPSCs at day 5 after surgery and pretreatment with ML133 (30 nmol, i.t.). No significant difference was found in gly-sIPSC amplitude, but their frequency was significantly reversed in comparison with SNI alone group (Fig. 3B). These results indicated that blockade of Kir2.1 activity in the spinal cord before SNI prevents the reduction of glycinergic transmission induced by SNI, and thus regulates the development of dynamic allodynia.
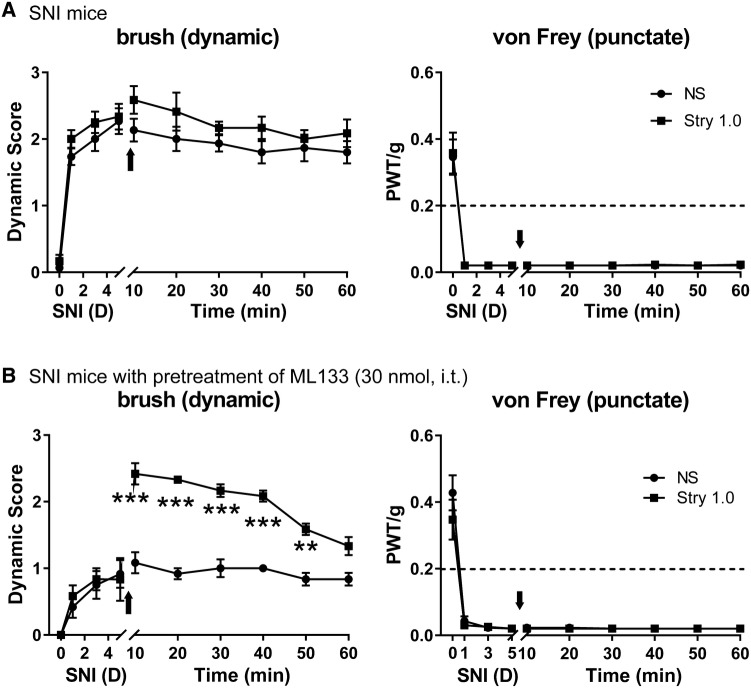
Strychnine Restored SNI-Induced Dynamic Allodynia in ML133-Pretreated Mice
Since SNI reduced and ML133 prevented the reduction in glycinergic transmission in the dorsal horn, we then evaluated whether strychnine could block the analgesic effect of ML133 on dynamic allodynia in SNI mice. We investigated the effect of strychnine on both SNI alone and SNI with ML133 pretreatment on day 5 after SNI, when both the dynamic and punctuate allodynia were fully established. Our results showed that strychnine alone (1 nmol, i.t.) had no synergistic effect on SNI-induced dynamic and punctate allodynia (Fig. 4A). However, we found that strychnine fully reversed the blocking effect of ML133 (30 nmol) pretreatment on SNI-induced dynamic allodynia, but still had no effect on SNI-induced punctate allodynia (Fig. 4B). Since the protective effect of ML133 on dynamic allodynia was abolished by strychnine, our results further indicated that the selective analgesic effect of ML133 on dynamic allodynia is likely via enhancing glycinergic transmission in the spinal cord in SNI mice.
Fig. 4.
Strychnine abolished the dynamic analgesic effect of pre-treatment with ML133 on SNI mice. A At day 5 after SNI, brush-evoked dynamic pain score (NS, n = 5; Stry 1.0, n = 4; NS vs Stry 1.0, P > 0.05) and Von Frey evoked PWT (NS vs Stry 1, P > 0.05) did not change after administration of strychnine (1.0 nmol, i.t.). B Five days after mice were pre-treated with ML133 (30 nmol) 30 min before SNI, strychnine (1.0 nmol, i.t.) increased the pain score (n = 4/group, NS vs Stry, P < 0.001), but PWT did not change (NS vs Stry, P > 0.05). Graphs represent the mean ± SEM. **P < 0.01, ***P < 0.001, two-way ANOVA with Bonferroni post-hoc test.
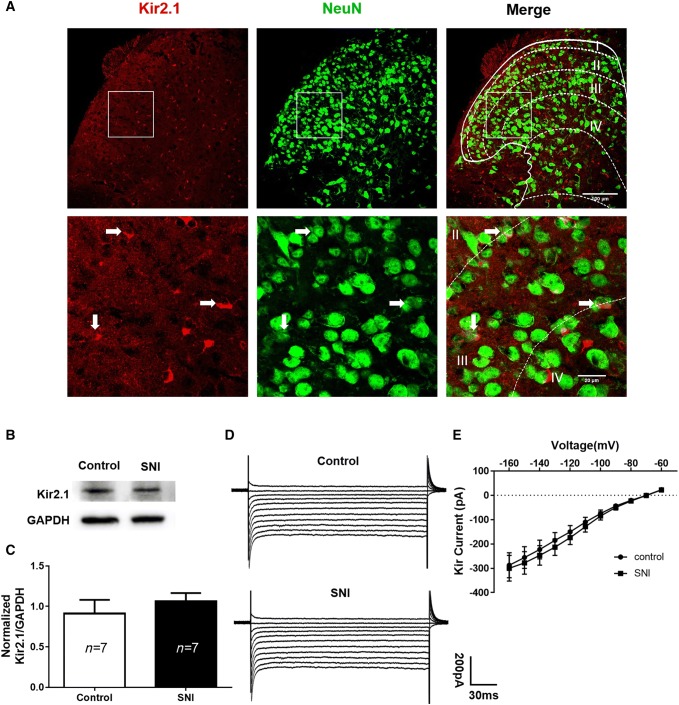
Neither Expression nor Function of Kir2.1 Channels in the Spinal Dorsal Horn Changed after SNI Surgery
Glycinergic neurons marked by glycine transporter 2 (GlyT2) have been reported to be located in the deeper dorsal horn (laminae III–V) and in lamina I [17]. Neurons at the lamina II/III border receive tonic glycinergic inhibition as well as mostly glycinergic synaptic inputs [31]. Our results showing that blockade of Kir2.1 channels in the spinal cord reversed the SNI-induced mechanic allodynia raised the question of whether Kir2.1 expression and function had changed in the dorsal horn after SNI. To determine whether Kir2.1 was expressed on neurons in the superficial dorsal horn, we used immunohistochemical assays to label Kir2.1 and NeuN. We found that Kir2.1 was widely distributed in the spinal cord (Fig. 5A). In the lamina III region, most of the Kir2.1 fluorescent signals were indeed co-localized with those of NeuN, while some Kir2.1 signals were separated from the NeuN signals. We next investigated whether Kir2.1 channels were altered after SNI. To test this, we examined membrane Kir2.1 expression in the dorsal horn by western blot assays. The intensity of the immunobands for Kir2.1 from both control and SNI mice were quantified and normalized to the GAPDH loading control. The results showed no difference in the Kir2.1 protein level between the SNI and control groups (Fig. 5B, C), suggesting that Kir2.1 regulates glycinergic transmission without affecting Kir2.1 expression during SNI. We further tested whether SNI affected Kir2.1 function by recording the Kir currents in randomly-selected lamina II–III neurons using patch clamp. Again, the result showed that Kir currents did not differ between neurons from the SNI and control groups (Fig. 5D, E). Taken together, our data suggested that SNI surgery does not affect Kir2.1 channels in the dorsal horn despite the development of mechanical allodynia.
Fig. 5.
Distribution, expression, and function of Kir2.1 in the spinal dorsal horn. A Confocal scanning images of Kir2.1 (red) and neuN (green) showing that Kir2.1 was distributed widely (lower panels are magnified images of the squares in the upper panel; arrows indicate co-localization of Kir2.1 and NeuN in lamina III neurons. B Representative immunobands of Kir2.1 and GAPDH from control and SNI (5 days) mice. C Quantitative analysis of Kir2.1 in the SNI versus the control group (n = 7 for both). The Kir2.1 level in the dorsal horn did not change after SNI (P = 0.4562, unpaired t tests). D Representative traces showing no change in Kir currents after SNI. EI–V curves of Kir currents also showed no change compared to the control group (Control, n = 14; SNI, n = 16; P = 0.9999, two-way ANOVA). Graph represents the mean ± SEM.
Acute ML133 Perfusion Increased the Frequency, but not the Amplitude, of Glycinergic sIPSCs in Lamina IIi Neurons in SNI Mice
Since pretreatment with ML133 protected against the SNI-induced dysfunction in spinal glycinergic transmission and prevented the SNI-induced dynamic allodynia, the next question was whether the enhancement of glycinergic transmission by ML133 could reverse the dynamic allodynia established after SNI. Thus, we first recorded the gly-sIPSCs in lamina IIi neurons from SNI mice. As expected, the gly-sIPSC frequency, but not amplitude, showed a remarkable decrease 5 days after SNI; however, acute perfusion with ML133 (100 μmol/L) significantly enhanced the gly-sIPSCs (Fig. 6). These results demonstrated that acute blockade of Kir2.1 channels regulates glycinergic transmission in a pathological state of pain in the dorsal horn.
Fig. 6.
ML133 perfusion enhanced glycinergic transmission in lamina IIi neurons in SNI mice on day 5. A Upper traces: representative traces of gly-sIPSCs from lamina IIi neurons superfused with 20 μmol/L DNQX, 25 μmol/L AP5, and 10 μmol/L bicuculline. Lower traces: gly-sIPSCs recorded during perfusion with 100 μmol/L ML133. Right traces are amplified from the boxes at left. B In lamina IIi neurons, bath application of ML133 (100 μmol/L) significantly enhanced the frequency of gly-sIPSCs (P = 0.0056, paired t tests). The amplitude of gly-sIPSCs did not change after ML133 perfusion (P = 0.6399, paired t tests). Graphs represent the mean ± SEM. **P < 0.01.
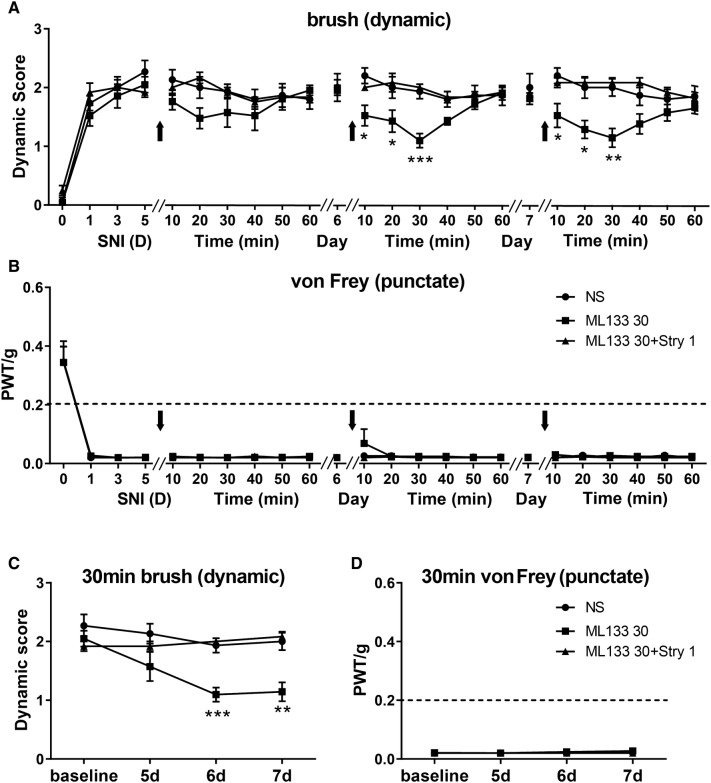
ML133 Selectively Inhibited Established Dynamic but not Punctate Allodynia Induced by SNI in Mice
Since acute perfusion with ML133 enhanced glycinergic transmission, we then investigated its therapeutic effect on established mechanical allodynia after SNI. Mice were given ML133 (30 nmol, i.t.) once a day from days 5 to 7 after SNI. We found that ML133 treatment at day 5 had little effect on punctate allodynia, but a mild but not statistically significant inhibitory effect on dynamic allodynia. However, consecutive administration of ML133 on days 6 and 7 significantly inhibited dynamic, but not punctate, allodynia. In addition, when ML133 (30 nmol) was co-injected with strychnine (1 nmol), ML133 failed to affect the dynamic allodynia (Fig. 7A, B). Therefore, these results showed that the inhibition of dynamic allodynia by ML133 was abolished by strychnine, indicating that ML133 acts on glycinergic transmission to exert an analgesic effect on dynamic allodynia. However, the inhibition of dynamic allodynia by ML133 increased at 30 min after i.t. injection, and lasted for ~50 min (Fig. 7C, D). These results further suggested that enhancing the glycinergic transmission by inhibition of Kir2.1 channels in the dorsal horn selectively suppresses the dynamic, but not punctate, allodynia induced by SNI in mice.
Fig. 7.
Effects of intrathecal administration of ML133 after SNI. A, B Drugs were administered i.t. once a day from postoperative day (POD) 5 to POD 7 (NS, n = 5; ML133 30, n = 7; ML133 30+Stry 1, n = 4). On POD 5, ML133 did not change the dynamic score (P > 0.05) or PWT (P > 0.05). The time course of the ML133 effect showed effective inhibition of dynamic allodynia on POD 6 (P < 0.05) to POD 7 (P > 0.05), but had no effect on punctate allodynia. Arrows indicate drug administration. However, ML133 (30 nmol, i.t.) and strychnine (1.0 nmol, i.t.) simultaneously did not change either the dynamic score (POD 5, P > 0.05; POD 6, P > 0.05; POD 7, P > 0.05) or the PWT (POD 5, P > 0.05; POD 6, P > 0.05; POD 7, P > 0.05). C, D Graphs of effects on dynamic and punctate allodynia 30 min after i.t. ML133 from POD 5 to POD 7. ML133 had a remarkable effect on dynamic allodynia but no effect on punctate allodynia, whereas ML133 and strychnine did not affect the SNI-induced dynamic and punctate allodynia. Graphs represent the mean ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001, two-way ANOVA with Bonferroni post-hoc test.
Discussion
Our studies have, for the first time, revealed that Kir2.1 channels are involved in regulating spinal glycinergic transmission, which further selectively contributes to dynamic, but not punctate mechanical allodynia. The present study provides evidence showing that pretreatment with ML133, a Kir2.1 channel inhibitor, preferentially prevented the development of dynamic, but not punctate, allodynia in a mouse SNI model. Spinal glycinergic dysfunction by i.t. strychnine, at a relatively low dose, selectively induced dynamic, but not punctate allodynia in naïve mice. In contrast, spinal administration of a low dose of bicuculline, a GABA receptor antagonist, only induced punctate, but not dynamic allodynia. Under SNI conditions, glycinergic inhibitory transmission was dampened, but ML133 enhanced this transmission in dorsal horn neurons. Furthermore, either in vivo pretreatment or acute application of ML133 reversed the reduction in the frequency of glycine transmission to the dorsal horn neurons after SNI surgery, and further selectively suppressed the dynamic, but not the punctate allodynia induced by SNI in mice.
SNI, a well-developed model of peripheral neuropathic pain, was chosen to induce mechanical allodynia in the lateral area of the paw [32]. Most previous studies measured mechanical allodynia using von Frey filaments [2, 26], however, this method cannot distinguish the different forms of mechanical allodynia, which may be mediated through distinct spinal circuits [6]. In the current study, we used a paintbrush to induce dynamic allodynia and von Frey filament to induce punctate allodynia, as in our previous report [6]. We found that i.t. administration ML133 before SNI dose-dependently prevented the development of dynamic allodynia, but not punctate allodynia. ML133 is a selective Kir2.1 inhibitor and has little affinity for other Kir2.x family channels [33]. Kir2.1 is expressed widely and differentially in the brain [22], spinal cord, and dorsal root ganglia (DRG)[34]. Here, we used immunohistochemistry to visualize the location of Kir2.1 channels and found that they were scattered in the spinal cord and most of their signals co-localized with neuN staining. Our results are consistent with the previous report that Kir2.1 channels are present in neuronal somata in the spinal cord [34]. Kir2.1 channels, which are constitutively active and exhibit strong inward rectification, possess transmembrane and cytoplasmic regions and a pore structure [20]. They play an essential role in modulating neuronal excitability and membrane potential and are involved in pain processing. For example, blockade of Kir2.1 in spinal lamina I projection neurons causes an increase of intrinsic membrane excitability [23, 24], and overexpression of Kir2.1 channels inhibits neurons by resisting depolarization to action potential threshold [35]. A mutation of Kir2.1 is associated with Andersen-Tawil syndrome, and one patient has reported occasional muscle pain after exercise [36]. In addition, in vivo viral gene transfer of Kir2.1 channels into the DRG results in a hyperpolarized resting membrane potential, and partially prevents the development of mechanical hyperalgesia in chronic compressed DRG (CCD) injury but has no effect on formed CCD injury pain behavior [37]. All these studies provide strong evidence that Kir2.1 channels are involved in the modulation of mechanical allodynia in the spinal cord. However, one limitation of those studies is that they only used the von Frey assay, measuring punctate pain behavior, but did not test the dynamic form of pain. In the current study, we used a pharmacological method to block Kir2.1 channels and found strong and selective preventive and suppressive effects on dynamic allodynia in the SNI model in mice. Different substrates of spinal circuits may be involved in either punctate or dynamic allodynia [2, 6, 38, 39]. Kir2.1 may be preferentially involved in the modulation, by regulating glycinergic transmission, of microcircuits in processing dynamic allodynia in the spinal cord. Moreover, as Kir2.1 is also expressed in the DRG and modulates mechanical allodynia [37], we cannot rule out the influence of ML133 on DRG neurons involved in regulating the dynamic allodynia seen in our current study. Here, we also found that ML133 inhibited the formed dynamic, but not punctate, allodynia in SNI mice, which further demonstrated that Kir2.1 channels are involved in dynamic allodynia and pharmacological blockade of Kir2.1 channels can target this form of neuropathic pain.
We further investigated why spinal blockade of Kir2.1 channels had a distinct effect on dynamic but not punctate allodynia. Previous studies have shown that intracisternal administration of strychnine induces trigeminal [30, 40] as well as facial dynamic allodynia [15]. Intrathecal strychnine induces morphine-insensitive allodynia, which is similar to the sensory dysesthesia of clinical neural injury pain [41]. Thus, we wondered whether glycinergic inhibitory transmission is involved in the action of Kir2.1 on dynamic allodynia. To test this, we first injected either strychnine or bicuculline i.t. to measure both dynamic and punctate allodynia, and our behavioral study showed that spinal glycinergic dysfunction with a relatively low dose of strychnine selectively induced dynamic, but not punctate, allodynia. In contrast, GABAergic dysfunction with a relatively low dose of bicuculline selectively induced only punctate, but not dynamic, allodynia. As previously reported, rats responded to brush-evoked stimuli under GABAA receptor inhibition [15]. Therefore, spinal glycinergic and GABAergic inhibitory transmission may participate to different degrees in distinct forms of allodynia. Lu and colleagues reported that i.t. strychnine induces von Frey-evoked mechanical allodynia in rats at doses ranging from 0.1 μg to 10 μg, with profound effects starting at 1 μg and maximal at 3 and 10 μg [14], which is consistent with our current results showing that a high dose of 3 nmol strychnine (proximally equivalent to 1 μg), evoked both dynamic and punctate allodynia in mice (data not shown). Thus, our results suggest that dynamic allodynia may be more sensitive to glycinergic transmission than punctate allodynia. Furthermore, dynamic allodynia is mediated by myelinated Aβ fibers which mainly innervate in laminae III-VI with some extension into lamina IIi [16]. Most Aβ afferents are enriched in glycine, providing evidence that glycinergic transmission plays an essential role in dynamic allodynia transmission [42]. Glycinergic inhibitory transmission serves as a “gate” in spinal pain processing [18]. Nerve injury induces glycinergic dysfunction in dorsal horn radial interneurons in a partial sciatic nerve ligation model [43] and in PKCγ-expressing neurons in lamina IIi in a spinal nerve ligation model [14]. The glycine receptor α3 subunit is distinctly expressed in lamina IIi, overlaps with PKCγ neurons, and may be involved in pathological pain states [44]. Indeed, we found that SNI injury dampened the gly-sIPSC frequency, but not amplitude, in lamina IIi neurons. And this glycinergic transmission dysfunction in a pathological pain state is consistent with previous studies. Interestingly, a Kir2.1 channel blocker rescued the reduction of gly-sIPSC frequency in mice pre-treated with ML133. Moreover, acute perfusion with ML133 increased the gly-sIPSCs in lamina IIi neurons in both control and SNI mice. Our previous study reported that Vglut3 neurons mediate spinal microcircuits in processing brush-evoked dynamic allodynia. These Vglut3 neurons are located in dorsal laminae IIi-III and are highly co-expressed with PKCγ neurons [6]. The substrate Vglut3 may be subject to glycinergic transmission change after SNI, which needs further investigation. Involvement of the change of gly-sIPSCs frequency, but not amplitude, indicated the regulation of glycinergic neuronal activity by ML133. Moreover, strychnine reversed the protective effect of ML133 pretreatment on SNI-induced dynamic allodynia. And the therapeutic effect of ML133 failed when administered simultaneously with strychnine at day 5 after SNI. Thus, ML133 enhanced glycinergic inhibitory transmission to exert the analgesic effect. In the dorsal horn, numerous glycinergic neurons marked by GlyT2-EGFP are densely located in the deeper dorsal horn (laminae III–V) and a few in lamina I [17]. In our immunohistochemistry study, we found Kir2.1 co-localized with neuN in lamina III, suggesting that spinal glycinergic neurons express Kir2.1 channels. However, it is a limitation that we did not use immunohistochemistry to assess the co-localization of Kir2.1 channels and glycinergic neurons, since we did not find an appropriate way to label glycinergic neuronal somata. Further studies are needed to investigate the direct interaction of Kir2.1 channels and glycinergic neurons. Even Kir2.1 was expressed throughout the superficial dorsal horn, Kir2.1 channel on glycinergic neuronal population may exert higher sensitivity to ML133 when compared with that on dorsal horn neuron.
To determine whether the modulatory effect of ML133 is related to the expression change of Kir2.1, we evaluated the level of Kir2.1 in the dorsal horn by Western blot. There was no change in the Kir2.1 expression level after SNI. To be specific, we need to measure the level of Kir2.1 in glycinergic neurons which are rich in lamina III. However, since it is difficult to distinguish lamina III from L4 to L6, we finally measured the Kir2.1 levels in the ipsilateral dorsal horn. Kir current recordings also revealed no change in the dorsal horn after SNI. However, we could not distinguish neurons from the dorsal horn as glycinergic. Limited by the resolution of our method, we cannot conclude whether the glycinergic dysfunction after SNI is associated with variation in the expression or function of Kir2.1 channels in specific neurons in the spinal cord, such as glycinergic neurons. It is still possible that the expression of Kir2.1 in lamina III increased while decreasing in other regions. Moreover, a cumulative loss of neurons in the dorsal horn occurs after SNI [45], so the remaining glycinergic neurons may express more Kir2.1 channels after SNI. It is worth noting that further studies are needed to solve this problem.
In conclusion, we first provided evidence that blockade of Kir2.1 channels in the spinal cord selectively inhibits dynamic allodynia and this effect is exhibited via enhanced glycinergic transmission. Thus, our findings provide a potential drug candidate, ML133, for treating dynamic allodynia (but not influencing punctate allodynia) in the clinic and suggest that the Kir2.1 channel is a valid target for treating this form of pain.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (31771188 and 31471027) and the Science and Technology Commission of Shanghai Municipality, China (13DJ1400302).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflicts of interest.
References
- 1.Colloca L, Ludman T, Bouhassira D, Baron R, Dickenson AH, Yarnitsky D, et al. Neuropathic pain. Nat Rev Dis Primers. 2017;3:17002. doi: 10.1038/nrdp.2017.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petitjean H, Pawlowski SA, Fraine SL, Sharif B, Hamad D, Fatima T, et al. Dorsal horn parvalbumin neurons are gate-keepers of touch-evoked pain after nerve injury. Cell Rep. 2015;13:1246–1257. doi: 10.1016/j.celrep.2015.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Truini A, Garcia-Larrea L, Cruccu G. Reappraising neuropathic pain in humans—how symptoms help disclose mechanisms. Nat Rev Neurol. 2013;9:572–582. doi: 10.1038/nrneurol.2013.180. [DOI] [PubMed] [Google Scholar]
- 4.Koltzenburg M, Lundberg LE, Torebjork HE. Dynamic and static components of mechanical hyperalgesia in human hairy skin. Pain. 1992;51:207–219. doi: 10.1016/0304-3959(92)90262-A. [DOI] [PubMed] [Google Scholar]
- 5.Xu ZZ, Kim YH, Bang S, Zhang Y, Berta T, Wang F, et al. Inhibition of mechanical allodynia in neuropathic pain by TLR5-mediated A-fiber blockade. Nat Med. 2015;21:1326–1331. doi: 10.1038/nm.3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng L, Duan B, Huang T, Zhang Y, Chen Y, Britz O, et al. Identification of spinal circuits involved in touch-evoked dynamic mechanical pain. Nat Neurosci. 2017;20:804–814. doi: 10.1038/nn.4549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nurmikko T, Bowsher D. Somatosensory findings in postherpetic neuralgia. J Neurol Neurosurg Psychiatry. 1990;53:135–141. doi: 10.1136/jnnp.53.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watson PN. Postherpetic neuralgia. BMJ Clin Evid 2010, 2010. [PMC free article] [PubMed]
- 9.Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- 10.Basbaum AI, Bautista DM, Scherrer G, Julius D. Cellular and molecular mechanisms of pain. Cell. 2009;139:267–284. doi: 10.1016/j.cell.2009.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lau BK, Vaughan CW. Descending modulation of pain: the GABA disinhibition hypothesis of analgesia. Curr Opin Neurobiol. 2014;29:159–164. doi: 10.1016/j.conb.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 12.Gutierrez-Mecinas M, Furuta T, Watanabe M, Todd AJ. A quantitative study of neurochemically defined excitatory interneuron populations in laminae I-III of the mouse spinal cord. Mol Pain 2016, 12. [DOI] [PMC free article] [PubMed]
- 13.Takazawa T, Choudhury P, Tong CK, Conway CM, Scherrer G, Flood PD, et al. Inhibition mediated by glycinergic and GABAergic receptors on excitatory neurons in mouse superficial dorsal horn is location-specific but modified by inflammation. J Neurosci. 2017;37:2336–2348. doi: 10.1523/JNEUROSCI.2354-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu Y, Dong H, Gao Y, Gong Y, Ren Y, Gu N, et al. A feed-forward spinal cord glycinergic neural circuit gates mechanical allodynia. J Clin Invest. 2013;123:4050–4062. doi: 10.1172/JCI70026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miraucourt LS, Moisset X, Dallel R, Voisin DL. Glycine inhibitory dysfunction induces a selectively dynamic, morphine-resistant, and neurokinin 1 receptor- independent mechanical allodynia. J Neurosci. 2009;29:2519–2527. doi: 10.1523/JNEUROSCI.3923-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Todd AJ. Neuronal circuitry for pain processing in the dorsal horn. Nat Rev Neurosci. 2010;11:823–836. doi: 10.1038/nrn2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeilhofer HU. The glycinergic control of spinal pain processing. Cell Mol Life Sci. 2005;62:2027–2035. doi: 10.1007/s00018-005-5107-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foster E, Wildner H, Tudeau L, Haueter S, Ralvenius WT, Jegen M, et al. Targeted ablation, silencing, and activation establish glycinergic dorsal horn neurons as key components of a spinal gate for pain and itch. Neuron. 2015;85:1289–1304. doi: 10.1016/j.neuron.2015.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Masia R, Krause DS, Yellen G. The inward rectifier potassium channel Kir2.1 is expressed in mouse neutrophils from bone marrow and liver. Am J Physiol Cell Physiol. 2015;308:C264–276. doi: 10.1152/ajpcell.00176.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hibino H, Inanobe A, Furutani K, Murakami S, Findlay I, Kurachi Y. Inwardly rectifying potassium channels: their structure, function, and physiological roles. Physiol Rev. 2010;90:291–366. doi: 10.1152/physrev.00021.2009. [DOI] [PubMed] [Google Scholar]
- 21.Day M, Carr DB, Ulrich S, Ilijic E, Tkatch T, Surmeier DJ. Dendritic excitability of mouse frontal cortex pyramidal neurons is shaped by the interaction among HCN, Kir2, and Kleak channels. J Neurosci. 2005;25:8776–8787. doi: 10.1523/JNEUROSCI.2650-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pruss H, Derst C, Lommel R, Veh RW. Differential distribution of individual subunits of strongly inwardly rectifying potassium channels (Kir2 family) in rat brain. Brain Res Mol Brain Res. 2005;139:63–79. doi: 10.1016/j.molbrainres.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 23.Li J, Blankenship ML, Baccei ML. Inward-rectifying potassium (Kir) channels regulate pacemaker activity in spinal nociceptive circuits during early life. J Neurosci. 2013;33:3352–3362. doi: 10.1523/JNEUROSCI.4365-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ford NC, Baccei ML. Inward-rectifying K(+) (Kir2) leak conductance dampens the excitability of lamina I projection neurons in the neonatal rat. Neuroscience. 2016;339:502–510. doi: 10.1016/j.neuroscience.2016.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Decosterd I, Woolf CJ. Spared nerve injury: an animal model of persistent peripheral neuropathic pain. Pain. 2000;87:149–158. doi: 10.1016/S0304-3959(00)00276-1. [DOI] [PubMed] [Google Scholar]
- 26.Duan B, Cheng L, Bourane S, Britz O, Padilla C, Garcia-Campmany L, et al. Identification of spinal circuits transmitting and gating mechanical pain. Cell. 2014;159:1417–1432. doi: 10.1016/j.cell.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods. 1994;53:55–63. doi: 10.1016/0165-0270(94)90144-9. [DOI] [PubMed] [Google Scholar]
- 28.Cheng LZ, Han L, Fan J, Huang LT, Peng LC, Wang Y. Enhanced inhibitory synaptic transmission in the spinal dorsal horn mediates antinociceptive effects of TC-2559. Mol Pain. 2011;7:56. doi: 10.1186/1744-8069-7-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duan B, Cheng L, Ma Q. Spinal circuits transmitting mechanical pain and itch. Neurosci Bull. 2018;34:186–193. doi: 10.1007/s12264-017-0136-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee IO, Whitehead RA, Ries CR, Schwarz SK, Puil E, MacLeod BA. Evaluation of a novel mouse model of intracisternal strychnine-induced trigeminal allodynia. Can J Anaesth. 2013;60:780–786. doi: 10.1007/s12630-013-9975-x. [DOI] [PubMed] [Google Scholar]
- 31.Takazawa T, MacDermott AB. Glycinergic and GABAergic tonic inhibition fine tune inhibitory control in regionally distinct subpopulations of dorsal horn neurons. J Physiol. 2010;588:2571–2587. doi: 10.1113/jphysiol.2010.188292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richner M, Bjerrum OJ, Nykjaer A, Vaegter CB. The spared nerve injury (SNI) model of induced mechanical allodynia in mice. J Vis Exp. 2011 doi: 10.3791/3092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang HR, Wu M, Yu H, Long S, Stevens A, Engers DW, et al. Selective inhibition of the K(ir)2 family of inward rectifier potassium channels by a small molecule probe: the discovery, SAR, and pharmacological characterization of ML133. ACS Chem Biol. 2011;6:845–856. doi: 10.1021/cb200146a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murata Y, Yasaka T, Takano M, Ishihara K. Neuronal and glial expression of inward rectifier potassium channel subunits Kir2.x in rat dorsal root ganglion and spinal cord. Neurosci Lett. 2016;617:59–65. doi: 10.1016/j.neulet.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 35.Boulis NM, Handy CR, Krudy CA, Donnelly EM, Federici T, Franz CK, et al. Regulated neuronal neuromodulation via spinal cord expression of the gene for the inwardly rectifying potassium channel 2.1 (Kir2.1). Neurosurgery 2013, 72: 653–661; discussion 661. [DOI] [PubMed]
- 36.Ardissone A, Sansone V, Colleoni L, Bernasconi P, Moroni I. Intrafamilial phenotypic variability in Andersen-Tawil syndrome: A diagnostic challenge in a potentially treatable condition. Neuromuscul Disord. 2017;27:294–297. doi: 10.1016/j.nmd.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 37.Ma C, Rosenzweig J, Zhang P, Johns DC, LaMotte RH. Expression of inwardly rectifying potassium channels by an inducible adenoviral vector reduced the neuronal hyperexcitability and hyperalgesia produced by chronic compression of the spinal ganglion. Mol Pain. 2010;6:65. doi: 10.1186/1744-8069-6-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peirs C, Williams SP, Zhao X, Walsh CE, Gedeon JY, Cagle NE, et al. Dorsal horn circuits for persistent mechanical pain. Neuron. 2015;87:797–812. doi: 10.1016/j.neuron.2015.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bourane S, Grossmann KS, Britz O, Dalet A, Del Barrio MG, Stam FJ, et al. Identification of a spinal circuit for light touch and fine motor control. Cell. 2015;160:503–515. doi: 10.1016/j.cell.2015.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ressot C, Collado V, Molat JL, Dallel R. Strychnine alters response properties of trigeminal nociceptive neurons in the rat. J Neurophysiol. 2001;86:3069–3072. doi: 10.1152/jn.2001.86.6.3069. [DOI] [PubMed] [Google Scholar]
- 41.Sherman SE, Loomis CW. Morphine insensitive allodynia is produced by intrathecal strychnine in the lightly anesthetized rat. Pain. 1994;56:17–29. doi: 10.1016/0304-3959(94)90146-5. [DOI] [PubMed] [Google Scholar]
- 42.Todd AJ. GABA and glycine in synaptic glomeruli of the rat spinal dorsal horn. Eur J Neurosci. 1996;8:2492–2498. doi: 10.1111/j.1460-9568.1996.tb01543.x. [DOI] [PubMed] [Google Scholar]
- 43.Imlach WL, Bhola RF, Mohammadi SA, Christie MJ. Glycinergic dysfunction in a subpopulation of dorsal horn interneurons in a rat model of neuropathic pain. Sci Rep. 2016;6:37104. doi: 10.1038/srep37104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harvey RJ, Depner UB, Wassle H, Ahmadi S, Heindl C, Reinold H, et al. GlyR alpha3: an essential target for spinal PGE2-mediated inflammatory pain sensitization. Science. 2004;304:884–887. doi: 10.1126/science.1094925. [DOI] [PubMed] [Google Scholar]
- 45.Scholz J, Broom DC, Youn DH, Mills CD, Kohno T, Suter MR, et al. Blocking caspase activity prevents transsynaptic neuronal apoptosis and the loss of inhibition in lamina II of the dorsal horn after peripheral nerve injury. J Neurosci. 2005;25:7317–7323. doi: 10.1523/JNEUROSCI.1526-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]