Abstract
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is associated with a broad range of neuropsychological impairments that are attenuated with methylphenidate (MPH) treatment. The aim of this study was to determine how MPH effects attentional functioning in terms of reaction time (RT) in ADHD.
Methods
Eighteen pre-medicated ADHD children (7 to 12 years old) and eighteen gender matched normal controls (7 to 12 years old) were included in the study. Participants performed an auditory attention task and the RT of participants to each target response was calculated automatically. The same test was repeated 3 months after OROS-MPH administration for ADHD group. RT, RT standard deviation (RTSD), and response errors (omission and commission errors) were compared between control and pre-MPH ADHD groups, and between Pre-MPH and post-MPH ADHD groups.
Results
Relative to control subjects, significantly longer RTs, higher RTSD and more errors of omission were observed in unmedicated ADHD children during auditory attention task. Analyses revealed significant effects of medication across all measures except commission errors. After treatment RTs were faster, RTSD values were lower, and errors of omission were attenuated compared to pre-medication condition in ADHD group. There were no significant differences in terms of commission errors between groups.
Conclusion
In this study it was observed that MPH reduced RTs to stimuli, attenuated omission errors during the task in ADHD group and after 3 months of treatment ADHD children showed similar patterns in RT as compared to controls. Results suggest that when treating ADHD, it might help clinicians to evaluate objective and non-invasive cognitive outcomes such as RT, RTSD and response errors to evaluate the effects of treatment.
Keywords: Attention deficit hyperactivity disorder, reaction time, auditory attention task, methylphenidate
INTRODUCTION
Attention deficit/hyperactivity disorder (ADHD) is a highly prevalent neuropsychiatric disorder of childhood that is characterized by the symptoms of inattentiveness, impulsivity, and hyperactivity (1). Moreover, ADHD is associated with various neurocognitive impairments in executive and non-executive functioning including response inhibition (2), working memory (3), planning and set-shifting (4), timing (5), reaction time and reaction time variability (6). Reaction time (RT) that is the length of time between the presentation of the target stimulus and the initiation of the subject’s motor response is an important and informative tool in the study of cognitive ability in psychology and other disciplines. One of the more consistent findings in the ADHD neuropsychology literature is that these children demonstrate, slower and more variable RTs compared to typically-developing children on a number of different tasks. (7). Intra-individual RT variability (RTV) has been identified as a potential endophenotype for psychopathological disorders. Increased RTV has been observed in individuals with bipolar dementia (8) autism (9), schizophrenia (10), and ADHD (11). Studies have demonstrated that increased RT variability in ADHD is mostly related to extremely slow responses (12) that are caused by periodic lapses of attention in goal-directed processing (13–14).
The stimulant medication was found to reduce RT and RTV among children with ADHD. In a meta-analytic review of 319 studies Kofler et al. demonstrated RTV was attenuated by stimulants, but unaffected by non-stimulant medical and psychosocial treatments (6). Methylphenidate (MPH) is currently the most effective treatment for the symptoms of ADHD. MPH improves neurocognitive functioning on inhibitory control (15), visual-spatial working memory (16), sustained attention (17) and selective attention (18) in children with ADHD. Many studies have reported that the ADHD children showed better performance in attentional tasks after treatment with MPH, manifested in faster RTs to a target stimuli, reduced omission and commission errors and reduced RTV (7, 19, 20).
Tasks range from simple choice discrimination tasks (20) to more complex response inhibition tasks such as Go/No-Go task (21) and Stop Signal task (SST) (22) which are introduced to evaluate effects of MPH medication on RT in patients with ADHD. However, surprisingly very few studies have investigated auditory RT in this context. The existing, limitted literature is inconsistent with respect to effects of MPH on treatment in terms of auditory RT and RTV, where some of these studies did not detect significant effects of MPH on RT during auditory attention task and some showed enhancement in task accuracy and RT after treatment by MPH during both the visual and auditory modality in children with ADHD. Thus more work is needed to evaluate MPH effects on auditory RT, RTV and task accuracy. Since MPH has commonly been reported to reduce RTs to targets in ADHD, in this study we hypothesized that there will be significantly reduced RT and RTV after administration of stimulant medication. In addition to the medication effects we compared pre-MPH ADHD group with normal controls and hypothesized that controls would show faster RTs, lower RTV and higher task accuracy compared to ADHD group according to the afore-mentioned literature.
The aim of this study was to obtain more insight into the effects of MPH on auditory attention task which is less investigated compared to other tasks in ADHD children and to assess the differences in RT, RTV and task accuracy between ADHD children and normal children.
METHODS
The study was conducted on 18 pre-medicated, ADHD children with a mean age of 9.50 (SD 1.94, range 7–12 years) and 18 healthy children with a mean age of 9.78 (SD 1.86, range 7–12 years). Controls underwent a standard clinical assessment comprising neurological, endocrine and psychiatric evaluations. The ADHD patients were referred from Children Psychiatry Department of Erciyes University, Medical Faculty Hospital. All patients met criteria for ADHD according to DSM-IV. ADHD participants did not have any comorbidity with other psychiatric disorders such as obsessive-compulsive disorder, major depressive disorder, epilepsy, schizophrenia, and autism spectrum disorder. After the first assessment of children with ADHD, OROS-MPH at a dose of 0.5 mg/kg/day was prescribed to patients (min 27 mg/d, max 54 mg/d). Doses of OROS-MPH was titrated up to 1.2 mg/kg/day with increments at 2-week intervals. The time to reach optimal dose was generally 4–6 weeks; thus, effects of therapy was assessed 3 months after starting therapy. The Wechsler Intelligence Scale for Children-Revised (WISC-R) (23) full IQ scores of subjects were all over 80. All subjects were right handed, native Turkish speakers and had normal hearing functions. The hearing functions were tested with Rinne and Weber test. The research protocol was approved by the ethics committees of Erciyes University and was in accordance with the latest version of the Declaration of Helsinki. Written consent was obtained from the parents of all participants.
Task
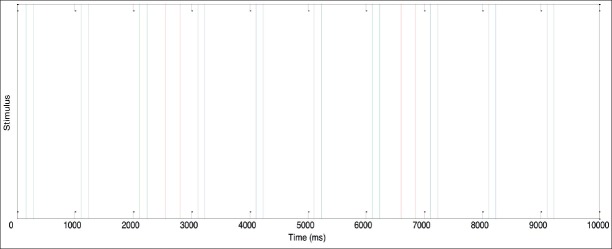
In this study 160 auditory stimuli that consist 128 standard (2000 Hz) and 32 target (1500 Hz) stimuli were presented in a random order. The interstimulus intervals (ISI) were randomized between 1250 and 2500 msec. Prior to the first run of the experiment, the participants were instructed to press the button when they hear target stimulus presented through headphones. The data acquisition was conducted in the Electrophysiology Laboratory of the Department of Physiology at Erciyes University, Medical Faculty. Patients and controls were tested under similar laboratory conditions after becoming familiarized with them. RT of 32 target stimulus were obtained using Matlab R2015a automatically by calculating length of time between the presentation of the target stimulus and the initiation of the subject’s motor response. In Fig. 1, the first ten stimuli of 128 stimuli sequence and a child’s response is presented.
Figure 1.
The first 10 stimuli sequence and responses of a child to the stimuli in control group. Blue and green blocks represent standard and target stimulus, respectively. Red blocks represent pressed button as the response of the child.
Statistical Analyses
We compared the variables between the ADHD (pre-treatment) and the control group using a student’s t-test and the variables before and after treatment using a two-tailed paired t-test with a statistical threshold of 0.05. Shapiro-Wilk normality test was used to confirm the normal distribution of variables. Mean RT for each participant was computed by averaging RTs. RT standard deviation (RTSD) was derived by computing the SD of each individual’s RTs which provides a measure of RT variability. Error of omission occurs when the participant fails to respond to a target stimulus (1500Hz) while error of commission occurs when the participant responds to a standard stimulus (2000Hz). All the statistical analyses were performed using the Statistical Package for the Social Sciences for Windows (SPSS Inc.; Chicago IL, ABD) Version 16.0.
RESULTS
We analyzed clinical characteristic of the participants and compared selected features between control and pre-MPH ADHD group as well as between pre-MPH and post-MPH ADHD group. ADHD children and controls did not differ statistically in terms of age, years of education, IQ and gender (Table 1). Measures including errors of commission, error of omission, mean RT and RT standard deviation (RTSD) are presented with statistical analyses between groups in Table 2.
Table 1.
Clinical characteristics of the participants
| ADHD | Control | t; df; p | |
|---|---|---|---|
| Participants | 18 | 18 | |
| Gender (Male: Female) | 14:4 | 14:4 | |
| Age in years | 9.5±1.94 | 9.78±1.86 | 0.437; 33.9; 0.66ns |
| Education in years | 3.5±1.94 | 3.78±1.86 | 0.437; 33.9; 0.66ns |
| WISC-R | 108.6±10.04 | 109.11±9.27 | 0.328; 33.78; 0.74ns |
Note: Mean ± standard deviation. Groups were compared with two-tailed unpaired Student’s t-tests. Abbreviations are as follows; t, t-value; df, degree of freedom; p, p value; ns, non-significance.
Table 2.
Statistical tests of medication effects with several potential confounding variables
| Control n=18 | Pre-MPH n=18 | Post-MPH n=18 | Control vs. Pre-MPH | Pre-MPh vs. Post MPH** | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| mean | SD | mean | SD | Mean | SD | t | p | t | p | |
| RT (ms) | 506.5 | 66.9 | 816.1 | 279.1 | 653.4 | 121.8 | 4.57 | <0.01 | 2.41 | 0.027 |
| RTSD (ms) | 53.46 | 43.6 | 232.9 | 143.1 | 84.46 | 85.43 | 5.086 | <0.01 | 4.25 | 0.001 |
| OE | 2.56 | 2.99 | 7.33 | 5.841 | 4 | 4.55 | 3.088 | <0.01 | 2.78 | 0.013 |
| CE | 1.39 | 2.16 | 0.89 | 2.56 | 0.28 | 0.826 | 0.634 | 0.53 | 1.66 | 0.213 |
Abbreviations: RT, Reaction Time; RTSD, Reaction Time Standard Deviation; OE: Omission Errors; CE, Commission Errors
Paired t-tests for their variables.
Pre-MPH comparison of variables between controls and ADHD patients
Children with ADHD showed longer RT (p<0.01) than controls. RT variability, as measured by RTSD was higher than controls (p<0.01). Compared to healthy children, children with ADHD made significantly more errors of omission (p<0.05) and there were no significant differences in terms of commission errors between groups (p>0.05).
Pre-MPH vs. post-MPH comparison of variables
RT was shorter and RTSD was lower in post-MPH compared to pre-MPH in children with ADHD. Compared to post-MPH, children with ADHD made significantly more errors of omission before treatment (p=0.013), there was no significant group differences in commission errors. Fig. 2 demonstrates mean RTMRT of groups. Errors bars are the standard deviation (SD) of the calculated values from different subjects of each group.
Figure 2.
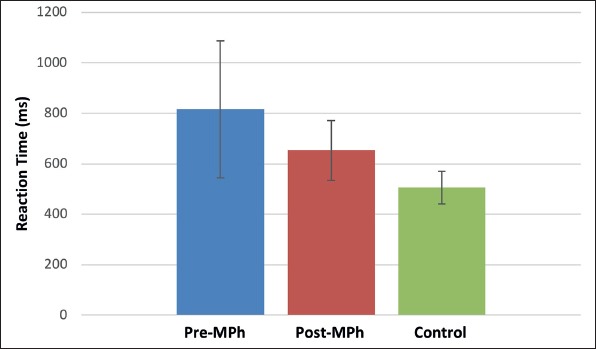
A comparison of groups between the values of mean RT. Errors bars are the standard deviation of the calculated values from different subjects of each group.
DISCUSSION
The present study investigated deficits in RT, RTV and task accuracy in children with ADHD. Consistent with our hypothesis, children with ADHD demonstrated significantly slower RT, higher RT variability and more response errors than controls. These results are in accordance with many previous studies in which individuals with ADHD across a wide range of tasks, including tasks measuring RT on choice decision, working memory, sustained attention has long been observed as slower and more variable compared to controls (13, 16, 22). Our results also supported the vigilance studies that assume slow RT, high RTV and increased errors of omission are associated with inattentive response (19).
The effects of stimulant medication on neuropsychological outcomes were also examined in this study by comparing ADHD participants before and after MPH treatment. We observed, MPH treatment reduced RTV, RT and task errors. The results were in agreement with the literature. In general, the effect of MPH medication on reducing these variables are consistent across studies despite different task characteristics. (24). A range of cognitive tasks evaluated in ADHD to examine effects of MPH medication on RT in patients with ADHD. Monden et al. claims selective tasks are more appropriate than one using a task and a rest period for ADHD children, because it is difficult for ADHD patients to stay still without performing any task, it may lead to unexpected movements or hyperactive behaviors that can cause loss of attention (25). Similarly, we used standard auditory stimuli as baseline and did not adopt rest period. We selected an easy, short task containing standard and target paradigm with random sequence that can be appropriate for ADHD children who have difficulty performing effortful cognitive tasks.
This current study was one of few studies using the selective auditory attention task to investigate the effects of stimulant medication on RT in ADHD children. The limited literature is inconsistent with respect to effects of MPH on treatment in terms of auditory RT and RTV. Although MPH commonly been reported to reduce RTs to target stimuli in ADHD subjects during attention tasks, Jonkman did not detected significant effects of MPH on RT during auditory attention task (26). They implemented 4 tasks composed of 2 auditory and 2 visual tasks. Their auditory task consisted of series of 300 stimuli which contains 60 target stimuli. The duration of each task took 10 minutes that is relatively long for ADHD children. Instead we choose shorter auditory task that contains only 160 stimuli that would be more appropriate for ADHD children. In this study we observed that omission errors increased especially in ADHD group towards the end of the record, suggesting a graduated loss of attention although the task took only five minutes. Our observation indicate that long attentional tasks may not be not appropriate for ADHD children which may cause more error of omissions that is associated with long RT (14). In accordance with our study, Klorman et al. reported reduced RTs to the targets and enhancement in task accuracy by MPH in children with ADHD during both the visual and auditory modality (18). Epstein et al suggest that treatment with MPH created an optimal energetic state so that children with ADHD had normalized RT patterns (27). In this study we observed improvement on RT patterns but not normalized as controls. This is maybe because of the duration of the treatment before assessing post-MPH results that took 24 months in their study which was three months in our study.
The important role of attention in auditory processing and listening has been reported in several studies. Auditory attention that is defined as the ability to focus on a specific source of sound (28) has been also declined in people with ADHD via impairment of P3 activation (29). Recently, Kemner et al. indicated that auditory cortical activity is modulated less in children with ADHD than in control children during performance of selective auditory task (30) and Baghdadi et al showed that the sensitivity of ADHD subjects to the sound intensity was lower than the normal group by means of RT (31). Furthermore, RT during an auditory attention task was utilized to investigate various other psychiatric disorders such as stress recognition (32), anxiety (33), autism (34), bipolar disorders (35). Inconsistent and limited auditory RT ADHD literature, positive effects of MPH in Auditory evoked potentials parameters in ADHD (36, 37) and positive findings in other psychiatric disorders have motivated us for evaluating MPH effects on auditory RT. The present study provided more insight into the effects of MPH on auditory attention task.
There are several limitations of this present study. Small sample size of our study is one of those limitations. Although we tested hearing functions with Rinne and Weber test, there would be difference in hearing threshold between subjects. Another limitation is we introduced only one task and RTV could change in multiple tasks.
In conclusion, RTV, which is one of the robust indicators of cognitive deficit, in patients with ADHD RTV was significantly attenuated by MPH treatment. It was found that MPH treatment enhanced task accuracy and reduced RTs of ADHD children in the auditory modality that is poorly introduced in literature, suggesting that the auditory attention task can be another possible test to be used in the evaluation of these patients. Results suggest that when treating ADHD, it might help clinicians to evaluate objective and non-invasive cognitive outcomes such as RT, RTSD and response errors to evaluate the effects of treatment. In future work, intra-individual RTV can be investigated via-exgauss parameters with other cognitive tasks in addition to auditory stimuli such as visual tasks and go/no-go paradigms.
Footnotes
Ethics Committee Approval: The research protocol was approved by the ethics committees of the Erciyes University (2014/195).
Informed Consent: Written consent was obtained from the parents of all participants.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - AG, ND, ED; Design - AG, MA, Mİ; Supervision - Mİ, AG, ND; Resource - ND, FP; Materials - ND, ED, SÖ; Data Collection and/ or Processing - FP, SÖ, MA; Analysis and/or Interpretation - AG, MA, ED; Literature Search - MA, FP; Writing - AG, MA; Critical Reviews - Mİ, ED, SÖ.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: This study was supported by the TUBITAK under project number 114S470.
REFERENCES
- 1.Barkley RA. Attention-deficit/hyperactivity disorder and self-regulation:taking an evolutionary perspective on executive functioning. In: Baumeister RF, Vohs KD, editors. Handbook of Self-Regulation:Research, theory, and applications. New York: Guilford Press; 2004. pp. 301–323. [Google Scholar]
- 2.Alderson RM, Rapport MD, Kofler MJ. Attention-deficit/hyper-activity disorder and behavioral inhibition:a meta-analytic review of the stop-signal paradigm. J Abnorm Child Psychol. 2007;35:745–758. doi: 10.1007/s10802-007-9131-6. [DOI] [PubMed] [Google Scholar]
- 3.Martinussen R, Hayden J, Hogg-Johnson S, Tannock R. A meta-analysis of working memory impairments in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2005;44:377–384. doi: 10.1097/01.chi.0000153228.72591.73. [DOI] [PubMed] [Google Scholar]
- 4.Toplak ME, Bucciarelli SM, Jain U, Tannock R. Executive functions:performance-based measures and the behavior rating inventory of executive function (BRIEF) in adolescents with attention deficit/hyperactivity disorder (ADHD) Child Neuropsychol. 2009;15:53–72. doi: 10.1080/09297040802070929. [DOI] [PubMed] [Google Scholar]
- 5.Noreika V, Falter CM, Rubia K. Timing deficits in attention-deficit/hyperactivity disorder (ADHD):Evidence from neurocognitive and neuroimaging studies. Neuropsychologia. 2013;51:235–266. doi: 10.1016/j.neuropsychologia.2012.09.036. [DOI] [PubMed] [Google Scholar]
- 6.Kofler MJ, Rapport MD, Sarver DE, Raiker JS, Orban SA, Friedman LM, Kolomeyer EG. Reaction time variability in ADHD:a meta-analytic review of 319 studies. Clin Psychol Rev. 2013;33:795–811. doi: 10.1016/j.cpr.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Coghill DR, Seth S, Pedroso S, Usala T, Currie J, Gagliano A. Effects of methylphenidate on cognitive functions in children and adolescents with attention-deficit/ hyperactivity disorder:evidence from a systematic review and a meta-Analysis. Biol Psychiatry. 2014;76:603–615. doi: 10.1016/j.biopsych.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Krukow P, Szaniawska O, Harciarek M, Plechawska-Wójcik M, Jonak K. Cognitive inconsistency in bipolar patients is determined by increased intra-individual variability in initial phase of task performance. J Affect Disord. 2017;210:222–225. doi: 10.1016/j.jad.2016.12.050. [DOI] [PubMed] [Google Scholar]
- 9.Karalunas SL, Geurts HM, Konrad K, Bender S, Nigg JT. Annual research review:Reaction time variability in ADHD and autism spectrum disorders:measurement and mechanisms of a proposed trans-diagnostic phenotype. J Child Psychol Psychiatry. 2014;55:685–710. doi: 10.1111/jcpp.12217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karantinos T, Tsoukas E, Mantas A, Kattoulas E, Stefanis NC, Evdokimidis I, Smyrnis N. Increased intra-subject reaction time variability in the volitional control of movement in schizophrenia. Psychiatry Res. 2014;215:26–32. doi: 10.1016/j.psychres.2013.10.031. [DOI] [PubMed] [Google Scholar]
- 11.Castellanos FX, Tannock R. Neuroscience of attention deficit/hyperactivity disorder:the search for endophenotypes. Nat Rev Neurosci. 2002;3:617–628. doi: 10.1038/nrn896. [DOI] [PubMed] [Google Scholar]
- 12.Vaurio RG, Simmonds DJ, Mostofsky SH. Increased intra-individual reaction time variability in attention-deficit/hyperactivity disorder across response inhibition tasks with different cognitive demands. Neuropsychologia. 2009;47:2389–2396. doi: 10.1016/j.neuropsychologia.2009.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tamm L, Narad ME, Antonini TN, O'Brien KM, Hawk LW, Jr, Epstein JN. Reaction time variability in ADHD. A review. Neurotherapeutics. 2012;9:500–508. doi: 10.1007/s13311-012-0138-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Epstein JN, Hwang ME, Antonini T, Langberg JM, Altaye M, Arnold LE. Examining predictors of reaction times in children with ADHD and normal controls. J Int Neuropsychol Soc. 2010;16:138–147. doi: 10.1017/S1355617709991111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aron AR, Dowson JH, Sahakian BJ, Robbins TW. Methylphenidate improves response inhibition in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2003;54:1465–1468. doi: 10.1016/s0006-3223(03)00609-7. [DOI] [PubMed] [Google Scholar]
- 16.Bedard AC, Martinussen R, Icokwicz A, Tannock R. Methylphenidate improves visual-spatial memory in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2004;43:260–268. doi: 10.1097/00004583-200403000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Hood J, Baird G, Rankin PM, Isaacs E. Immediate effects of methylphenidate on cognitive attention skills of children with attention-deficit-hyperactivity disorder. Dev Med Child Neurol. 2005;47:408–414. doi: 10.1017/s0012162205000794. [DOI] [PubMed] [Google Scholar]
- 18.Klorman R, Brumaghim JT, Salzman LF, Strauss J, Borgstedt AD, McBride MC, Loeb S. Effects of methylphenidate on processing negativities in patients with attention-deficit hyperactivity disorder. Psychophysiology. 1990;27:328–337. doi: 10.1111/j.1469-8986.1990.tb00391.x. [DOI] [PubMed] [Google Scholar]
- 19.Epstein JN, Conners CK, Hervey AS, Tonev ST, Arnold LE, Abikoff HB, Elliott G, Greenhill LL, Hechtman L, Hoagwood K, Hinshaw SP, Hoza B, Jensen PS, March JS, Newcorn JH, Pelham WE, Severe JB, Swanson JM, Wells K, Vitiello B, Wigal T MTA Cooperative Study Group. Assessing medication effects in the MTA study using neuropsychological outcomes. J Child Psychol Psychiatry. 2006;47:446–456. doi: 10.1111/j.1469-7610.2005.01469.x. [DOI] [PubMed] [Google Scholar]
- 20.Spencer SV, Hawk LW, Jr, Richards JB, Shiels K, Pelham W, Waxmonsky J. Stimulant treatment reduces lapses in attention among children with ADHD:the effects of methylphenidate on intra-individual response time distributions. J Abnorm Child Psychol. 2009;37:805–816. doi: 10.1007/s10802-009-9316-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Groom MJ, Scerif G, Liddle PF, Batty MJ, Liddle EB, Roberts KL, Cahill JD, Liotti M, Hollis C. Effects of motivation and medication on electrophysiological markers of response inhibition in children with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2010;67:624–631. doi: 10.1016/j.biopsych.2009.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boonstra AM, Kooij JJ, Oosterlaan J, Sergeant JA, Buitelaar JK. Does methylphenidate improve inhibition and other cognitive abilities in adults with childhood-onset ADHD? J Clin Exp Neuropsychol. 2005;27:278–298. doi: 10.1080/13803390490515757. [DOI] [PubMed] [Google Scholar]
- 23.Wechsler D. Wechsler Intelligence Scale for Children. 4th ed (WISC-IV) San Antonio, TX: Psychological Corporation; 2003. [Google Scholar]
- 24.Epstein JN, Brinkman WB, Froehlich T, Langberg JM, Narad ME, Antonini TN, Shiels K, Simon JO, Altaye M. Effects of stimulant medication, incentives, and event rate on reaction time variability in children with ADHD. Neuropsychopharmacology. 2011;36:1060–1072. doi: 10.1038/npp.2010.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Monden Y, Dan I, Nagashima M, Dan H, Uga M, Ikeda T, Tsuzuki D, Kyutoku Y, Gunji Y, Hirano D, Taniguchi T, Shimoizumi H, Watanabe E, Yamagata T. Individual classification of ADHD children by right prefrontal hemodynamic responses during a go/no-go task as assessed by fNIRS. Neuroimage Clin. 2015;9:1–12. doi: 10.1016/j.nicl.2015.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jonkman LM, Kemner C, Verbaten MN, Koelega HS, Camfferman G, vd Gaag RJ, Buitelaar JK, van Engel, and H. Effects of methylphenidate on event-related potentials and performance of attention-deficit hyperactivity disorder children in auditory and visual selective attention tasks. Biol Psychiatry. 1997;41:690–702. doi: 10.1016/s0006-3223(96)00115-1. [DOI] [PubMed] [Google Scholar]
- 27.Epstein JN, Erkanli A, Conners CK, Klaric J, Costello JE, Angold A. Relation between Continuous Performance Test performance measures and ADHD behaviors. J Abnorm Child Psychol. 2003;31:543–554. doi: 10.1023/a:1025405216339. [DOI] [PubMed] [Google Scholar]
- 28.Alho K, Salmi J, Koistinen S, Salonen O, Rinne T. Top-down controlled and bottom-up triggered orienting of auditory attention to pitch activate overlapping brain networks. Brain Res. 2015;1626:136–145. doi: 10.1016/j.brainres.2014.12.050. [DOI] [PubMed] [Google Scholar]
- 29.Romero AC, Capellini SA, Frizzo AC. Cognitive potential of children with attention deficit and hyperactivity disorder. Braz J Otorhinolaryngol. 2013;79:609–615. doi: 10.5935/1808-8694.20130109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kemner C, Jonkman LM, Kenemans JL, Böcker KB, Verbaten MN, Van Engeland H. Sources of auditory selective attention and the effects of methylphenidate in children with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2004;55:776–778. doi: 10.1016/j.biopsych.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 31.Baghdadi G, Towhidkhah F, Rostami R. Left and right reaction time differences to the sound intensity in normal and AD/HD children. Int J Pediatr Otorhinolaryngol. 2017;97:240–244. doi: 10.1016/j.ijporl.2017.04.025. [DOI] [PubMed] [Google Scholar]
- 32.Zhang B, Morère Y, Sieler L, Langlet C, Bolmont B, Bourhi G. Reaction time and physiological signals for stress recognition. Biomed Signal Process Control. 2017;38:100–107. [Google Scholar]
- 33.Langlet C, Hainaut JP, Bolmont B. Moderate anxiety modifies the electromyographic activity of a forearm muscle during a time-reaction task in women. Neurosci Lett. 2017;643:1–7. doi: 10.1016/j.neulet.2017.02.024. [DOI] [PubMed] [Google Scholar]
- 34.Williams DL, Goldstein G, Minshew NJ. The modality shift experiment in adults and children with high functioning autism. J Autism Dev Disord. 2013;43:794–806. doi: 10.1007/s10803-012-1618-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O'Donnell BF, Hetrick WP, Vohs JL, Krishnan GP, Carroll CA, Shekhar A. Neural synchronization deficits to auditory stimulation in bipolar disorder. Neuroreport. 2004;15:1369–1372. doi: 10.1097/01.wnr.0000127348.64681.b2. [DOI] [PubMed] [Google Scholar]
- 36.Young ES, Perros P, Price GW, Sadler T. Acute challenge ERP as a prognostic of stimulant therapy outcome in attention-deficit hyperactivity disorder. Biol Psychiatry. 1995;37:25–33. doi: 10.1016/0006-3223(94)00075-E. [DOI] [PubMed] [Google Scholar]
- 37.Ozdag MF, Yorbik O, Ulas UH, Hamamcioglu K, Vural O. Effect of methylphenidate on auditory event related potential in boys with attention deficit hyperactivity disorder. Int J Pediatr Otorhinolaryngol. 2004;68:1267–1272. doi: 10.1016/j.ijporl.2004.04.023. [DOI] [PubMed] [Google Scholar]