ABSTRACT
Although traditionally chikungunya virus is considered non-fatal, recent studies suggest that there may be in fact underreporting of deaths in some situations. A major chikungunya epidemic hit Jamaica in 2014 but no chikungunya-associated deaths were reported. We assessed the excess of all-cause deaths during this epidemic. Excess deaths were estimated by difference between observed and expected mortality based on the average age-specific mortality rate of 2012–2013, using the 99% confidence interval. There was an excess of 2,499 deaths during the epidemic (91.9/100,000 population), and a strong positive correlation between the monthly incidence of chikungunya and the excess of deaths (Rho = 0.939, p < 0.005). No significant concomitant epidemiological or climatic phenomenon occurred. Chikungunya is a major contributor to morbidity during epidemics and may be an unrecognized cause of death. Thus, it is urgent to review clinical protocols and improve the investigations of specific-cause deaths during chikungunya epidemics. Excess deaths could be a strategic tool for epidemiological surveillance.
KEYWORDS: Chikungunya, arbovirus, mortality, epidemiological surveillance, excess deaths, intelligence tools, Infectious diseases, Jamaica
1. Introduction
Chikungunya virus (CHIKV) is an emerging arbovirus (ARthropod-BOrne VIRUS) in the Americas where it was first identified in late 2013. On December 9th, 2013, the Pan American Health Organization (PAHO) issued an alert on the transmission of CHIKV in the Caribbean and on the risk of geographic expansion [1]. By the epidemiological week 30 of 2015, the transmission of CHIKV was already confirmed in most of the countries bathed by the Caribbean Sea with more than 1.6 million suspected or confirmed cases of chikungunya but only 253 deaths [1], a lower than expected mortality compared with the mortality observed in other locations such as Reunion Island [2].
In Jamaica the first imported cases of chikungunya were reported as soon as May 2014, and confirmation of autochthonous transmission was established on August 5th, 2014 [3]. In October of the same year, the epidemiological situation worsened, prompting the Jamaican government to declare a public health emergency, although no case of death by chikungunya was notified by Jamaica to PAHO [1].
Since the re-emergence of CHIKV in the first decade of the 21st century, numerous studies have reported on severe cases and related deaths to chikungunya [4–7], including in America [8–10]. Reports from Indian Ocean islands, continental India and Brazil suggest that in some situations, the passive surveillance system may not recognize a substantial proportion of the deaths associated with chikungunya, but an excess of deaths during the epidemic period can be identified [11,12]. The objective of this study was to evaluate the excess deaths associated with the 2014 chikungunya epidemic in Jamaica.
2. Materials and methods
It is an ecological study based on secondary data obtained from official and open access databases. Jamaica is a tropical island (Aw, Köppen climate classification) of the Caribbean Sea (Kingston, its capital, is located at latitude 17° 59’ N and longitude 76° 48’ W) populated with 2,720,554 inhabitants. We obtained chikungunya incidence data from the Jamaica Open Site Portal [3], which provide access of cases notified to the National Epidemiology Unit of the Ministry of Health. Population data were acquired from the Statistical Institute website that estimated based on census of 2001 and 2011 [13]. The mortality data are maintained by the Registrar General’s Department (RGD) [14] that records the Local District Registrars (LDRs), these latter register the vital events of births and deaths. As specified on its website, the objectives of the RGD are to ‘Provide timely statistics and analysis, categorized according to international standards, with the aim to support democratic planning by Government’ [14].
Monthly mortality rates were calculated for the years 2012 to 2014 (last year with data available). The number of deaths expected for each month of 2014 was estimated using the monthly average observed in the years 2012 and 2013, projected for the expected population of Jamaica in 2014. These years (2012 and 2013) were chosen to avoid changes in the population profile susceptible to altering the results. The maximum threshold of deaths expected in 2014 was the upper limit of the 99% confidence interval (CI). The mortality rate by age group between the years of 2012 and 2014 was also calculated, excluding deaths from external causes (death due to accidents and violence). The number of deaths expected by age group for the year 2014 was calculated using the average mortality by age group for the years 2012 and 2013 and the population estimated by age group. We defined excess deaths as the difference between observed and expected mortality. We calculated the Spearman correlation (rho) between excess deaths and the monthly incidence of chikungunya during the second half of 2014, considered the epidemic period. All these analyses were conducted while excluding external causes of deaths. External causes of deaths were next added to our modeling as a sensitivity analysis to test the robustness of the findings.
3. Results
There was an excess of 2,499 deaths for the year 2014, above the average of the two years prior to the epidemic leading to an overall mortality increase by 91.9 per 100,000 inhabitants. This excess mortality was greater among the elderly, but there was also an increase of deaths above the 99% CI in children under five, among young adults 20 to 29 years and in all age groups over 40 years (Table 1). The excess mortality rate in the 50–59 age group was 104.6 per 100,000 inhabitants (1‰), and among those over 70 years, 998.6 per 100,000 inhabitants (~1%). The increase in overall mortality during the year 2014 was most significant during the chikungunya epidemic event, as shown by mortality trends above the upper limit of the 99%CI coinciding with the epidemic peak (Figure 1).
Table 1.
Population by age group, expected, observed, excess deaths and excess mortality rate (deaths/100,000 inhabitants), Jamaica, 2014.
| Population | Expected Deaths for 2014 | UPPER 99% Confidence Interval | Observed Deaths 2014 | Excess Deaths | Excess Mortality Rate (deaths/100,000) | |
|---|---|---|---|---|---|---|
| 0 to 4 years | 199,170 | 694 | 742 | 758 | 64 | 32.3 |
| 5 to 9 years | 217,065 | 42 | 53 | 33 | −9 | −4.0 |
| 10 to 19 years | 523,010 | 117 | 136 | 132 | 15 | 2.9 |
| 20 to 29 years | 483,103 | 220 | 247 | 274 | 54 | 11.1 |
| 30 to 39 years | 376,788 | 491 | 531 | 531 | 40 | 10.7 |
| 40 to 49 years | 343,682 | 939 | 994 | 1,101 | 162 | 47.3 |
| 50 to 59 years | 257,205 | 1,500 | 1,570 | 1,769 | 269 | 104.6 |
| 60 to 69 years | 161,514 | 2,229 | 2,315 | 2,544 | 315 | 194.9 |
| 70 and more years | 159,017 | 8,916 | 9,087 | 10,504 | 1,588 | 998.6 |
| Total1 | 2,720,554 | 15,147 | 15,676 | 17,646 | 2,499 | 91.9 |
Observed mortality rate above the 99% confidence interval was bold and underlined.
Figure 1.
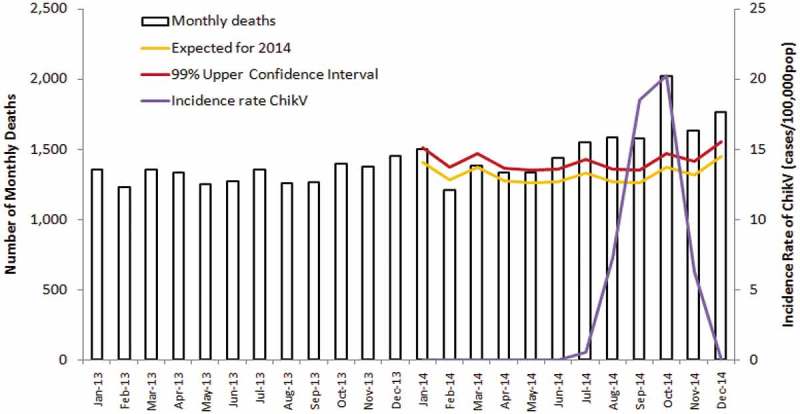
All-cause monthly deaths (white bars), expected deaths (yellow line) and upper 99% confidence interval (2014) and chikungunya incidence rate (cases/100,000 inhabitants), Jamaica, 2013–2014.
In addition, we identified a strong positive correlation between the monthly incidence of chikungunya and the excess of deaths during the epidemic period (Spearman Rho = 0.939; p < 0.005).
Further consideration of external causes of deaths in a sensitivity analysis did not change the overall sense of our findings (data not shown).
4. Discussion
The present study found a strong temporal correlation between general mortality and the chikungunya epidemic that occurred in Jamaica. Importantly, the age groups with the greatest increase in mortality during the epidemic event were the same previously identified as chikungunya in deaths certificate in La Réunion Island [2] and Brazil through excess mortality estimates [12]. As other possible sources of explanation, there was no coincident ambiental nor extreme weather phenomenon in Jamaica in 2014 [15]. The number of confirmed cases of dengue in 2014 (2.65 cases per 100,000 inhabitants) was lower than in the years of 2012 and 2013 (respectively 19.32 and 5.64 per 100,000 inhabitants) [16]. Absence of dengue-related deaths was confirmed in 2014 and in the years 2012 and 2013 respectively, 10 and 4 dengue-related deaths were confirmed [16]. The number of influenza cases in 2014 was also lower than in previous years [17]. These findings rule out the possibility that excess deaths may be caused by these other viruses.
Several studies conducted over the past decade India and Indian Ocean have shown an increase in overall mortality during chikungunya epidemics [11,18,19]. In La Réunion Island, a French overseas department, most of the deaths were laboratory confirmed [5–7], and in some cases deaths by chikungunya were attested as an underlying cause of death or as contributing cause [2]. During the 2005–2006 La Réunion Island epidemic, a robust diagnostic support resulted in similar numbers of deaths by chikungunya found in death certificates and excess deaths estimates. In Ahmedabad (India, 2006), there was a significant increase in overall mortality equivalent to 2,944 deaths during the epidemic. Despite scientific publications with laboratory confirmations of dozens of severe cases and deaths by chikungunya [5], there was however no report of deaths by Indian public health authorities [11]. Most recently studies in Brazil found an excess of 7,230 deaths higher than expected during the chikungunya epidemic of 2016 in three of the nine states of the Northeast, far above the 78 deaths identified by conventional passive epidemiological surveillance [12].
Since chikungunya spread in the Americas, several authors have demonstrated the occurrence of laboratory confirmed cases of chikungunya specific deaths [8–10]. These deaths occurred among people of various ages, including infants, children, young, middle-age or old adults, patients with comorbidities but also among previously healthy people. The main complications leading to death were myocarditis, septic shock, encephalitis, and respiratory causes [4,5,10], and it is worthwile to emphazize that the excess of deaths observed in Puerto Rico focused on the same causes [20], in that study the researchers used a methodology similar to the present work, reinforcing the reliability of excess deaths tool.
The excess mortality found in Jamaica was 2,499 deaths, more than 10 times the total deaths notified by all the countries of the Americas in the year 2014 to the PAHO. Noteworthy, it corresponds to a mortality rate of 91.9 per 100,000 inhabitants, almost twice the mortality found in Pernambuco (47.9 per 100,000 inhabitants), the most affected state in Brazil by the chikungunya epidemic in 2016 [12], and almost three times that found in La Réunion Island in 2005–2006 (33.8/100,000 inhabitants) [19]. Although this is an ecological study of time series limited in possibilities of causal inference, we believe that our results corroborate the hypothesis that CHIKV may be a significant contributor to the increase in the number of deaths in Jamaica. High mortality associated with chikungunya has been observed in the Indian Ocean [21], India [11], Brazil [12], French Antlles [22], Dominican Republic [23] and Puerto Rico [20] respectively, affected by the different circulating genotypes of the CHIKV, namely Indian Ocean Lineage (IOL); East, Central, and South African (ECSA) and Asian. Given Asian and ECSA lineages of CHIKV have been associated with higher rates of subclinical presentations [24,25] and trend towards lower prevalence of chronic chikungunya manifestations than the IOL [26–28], together with Brazilian, Puertorican and Dominican mortality data, these novel findings from Jamaica reinforce the hypothesis that mortality associated with chikungunya is not restricted to a single lineage and may be more dependent of host, population, or health-system related factors than driven by CHIKV virulence alone.
We believe that mortality associated with chikungunya has been underestimated and even neglected. This may be due to the poor access to diagnostic methods, but also given the difficulties in recognizing the severe forms of the disease. The finding that most of the deaths occurred in the elderly [2], together with the fact that the clinical picture in this age group may be different from the one presented by younger patients [29], may hamper the attending physicians for establishing links between the deaths and CHIKV infections. Indeed, a recently published study found that 42.7% of the old outpatients in Martinique with laboratory-confirmed chikungunya did not present a typical clinical picture owed to the absence of fever, absence of joint pain or both [29]. More studies detailing the clinical outcomes and prognostic features of CHIKV infection should be developed to disentangle the causal pathways of chikungunya-associated deaths. These studies may lead to substantive changes in clinical management strategies and refine public health policies during epidemics.
Our study may have limitations. Thus, we did not have access to 2015 years and could not be able to consolidate our findings, so that we cannot rule out a possible survivorship bias based on a mortality particularly low in 2012–2013 and not representative of the baseline.
In conclusion, adequate assessment of the impact of chikungunya as the cause of death is an important step forward in the scaling up of disease burden estimates and could help to revise the List of Blueprint priority diseases [30]. We propose that the evaluation of excess of deaths could be used as an indicator of the severity of chikungunya epidemics and be considered as a strategic tool for epidemiological surveillance to monitor the mortality trends associated with chikungunya as it is already used for influenza, respiratory syncytial virus and extreme climatic phenomena surveillance [31,32].
Funding Statement
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Pan American Health Organization 54th directing council report on chikungunya virus transmission and its impact in the region of the americas [Internet]. Washington, D.C.; 2015. Available from: http://www.paho.org/hq/index.php?option=com_docman&task=doc_download&gid=31210&Itemid=270&lang=en [Google Scholar]
- [2].Renault P, Solet J, Sissoko D, et al. A major epidemic of Chikungunya virus infection on Réunion Island, France, 2005-2006. Am J Trop Med Hyg. 2007;77:727–731. [PubMed] [Google Scholar]
- [3].Jamaica Open Data Portal G of J Chikungunya cases 2014 | Jamaica open data portal [Internet]. Gov. Jamaica. 2017. [cited 2017 November4]. Available from: http://data.gov.jm/dataset/chikungunya-cases-2014.
- [4].Economopoulou A, Dominguez M, Helynck B, et al. Atypical Chikungunya virus infections: clinical manifestations, mortality and risk factors for severe disease during the 2005-2006 outbreak on Réunion. Epidemiol Infect [Internet] 2009. [cited 2014 July14];137:534–541. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18694529 [DOI] [PubMed] [Google Scholar]
- [5].Tandale BV, Sathe PS, Arankalle VA, et al. Systemic involvements and fatalities during Chikungunya epidemic in India, 2006. J Clin Virol [Internet] 2009. [cited 2014 October27];46:145–149. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19640780 [DOI] [PubMed] [Google Scholar]
- [6].Gérardin P, Couderc T, Bintner M, et al. Chikungunya virus-associated encephalitis: A cohort study on La Réunion Island, 2005-2009. Neurology [Internet] 2016. [cited 2015 December5];86:94–102. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26609145 [DOI] [PubMed] [Google Scholar]
- [7].Lemant J, Boisson V, Winer A, et al. Serious acute chikungunya virus infection requiring intensive care during the reunion island outbreak in 2005–2006*. Crit Care Med [Internet] 2008. [cited 2014 October27];36:2536–2541. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00003246-200809000-00008. [DOI] [PubMed] [Google Scholar]
- [8].Hoz JMDL, Bayona B, Viloria S, et al. Fatal cases of Chikungunya virus infection in Colombia: diagnostic and treatment challenges. J Clin Virol [Internet] 2015. [cited 2015 June15];69:27–29. Available from: http://www.sciencedirect.com/science/article/pii/S1386653215001663 [DOI] [PubMed] [Google Scholar]
- [9].Sá PK de O, Nunes M de M, Leite IR, et al. Chikungunya virus infection with severe neurologic manifestations: report of four fatal cases. Rev Soc Bras Med Trop [Internet] 2017. [cited 2017 October8];50:265–268. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0037-86822017000200265&lng=en&tlng=en [DOI] [PubMed] [Google Scholar]
- [10].Rollé A, Schepers K, Cassadou S, et al. Severe sepsis and septic shock associated with Chikungunya virus infection, Guadeloupe, 2014. Emerg Infect Dis [Internet] 2016. [cited 2017 September17];22:891–894. Available from: https://wwwnc.cdc.gov/eid/article/22/5/pdfs/15-1449.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Mavalankar D, Shastri P, Bandyopadhyay T, et al. Increased mortality rate associated with Chikungunya epidemic, Ahmedabad, India. Emerg Infect Dis. 2008;14:412–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Freitas ARR, Cavalcanti L, Von Zuben AP, et al. Excess mortality related to Chikungunya epidemics in the context of co-circulation of other arboviruses in Brazil. PLOS Curr Outbreaks [Internet] 2017. [cited 2017 November19];140491 Available from: http://currents.plos.org/outbreaks/article/excess-mortality-related-to-chikungunya-epidemics-in-the-context-of-co-circulation-of-other-arboviruses-in-brazil/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Statistical Institute of Jamaica G of J Population statistics [Internet]. Goverment of Jamaica. 2017. [cited 2017 November4]. Available from: http://statinja.gov.jm/Demo_SocialStats/PopulationStats.aspx
- [14].Registrar General’s Department G of J Vital statistics | Registrar general’s department [Internet]. Gov. Jamaica. 2017. [cited 2017 November4]. Available from: https://www.rgd.gov.jm/index.php/vital-statistic
- [15].Weather Underground Weather history & data archive | Weather underground [Internet]. Weather Undergr. 2014. [cited 2017 November7]. Available from: https://www.wunderground.com/history/
- [16].Pan American Health Organization PAHO WHO | Dengue | Data, maps and statistics [Internet]. 2017. [cited 2017 January9]. Available from: https://www.paho.org/hq/index.php?option=com_topics&view=rdmore&cid=3273&lang=en
- [17].Pan American Health Organization Regional update EW 52, 2014: influenza and other respiratory virus [Internet]. Reg. Updat. Influ. Other Respir. Virus. Washington, D. C.; 2015. Available from: http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&Itemid=270&gid=28807&lang=en. [Google Scholar]
- [18].Beesoon S, Funkhouser E, Kotea N, et al. Chikungunya Fever, Mauritius, 2006. Emerg Infect Dis. 2008;14:337–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Manimunda SP, Mavalankar D, Bandyopadhyay T, et al. Chikungunya epidemic-related mortality. Epidemiol Infect [Internet] 2011. [cited 2014 August8];139:1410–1412. Available from: http://www.journals.cambridge.org/abstract_S0950268810002542 [DOI] [PubMed] [Google Scholar]
- [20].Freitas ARR, Donalisio MR, Alarcón-Elbal PM.. Excess mortality and causes associated with Chikungunya, Puerto Rico, 2014–2015. Emerg Infect Dis [Internet] 2018;24:2352–2355. Available from: http://wwwnc.cdc.gov/eid/article/24/12/17-0639_article.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Josseran L, Paquet C, Zehgnoun A, et al. Chikungunya disease outbreak, Reunion Island. Emerg Infect Dis. 2006;12:1994–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Freitas ARR, Alarcón-Elbal PM, Donalisio MR. Excess mortality in Guadeloupe and Martinique, islands of the French West Indies, during the chikungunya epidemic of 2014. Epidemiol Infect [Internet] 2018. 146(16):2059-2065. Available from: https://www.cambridge.org/core/product/identifier/S0950268818002315/type/journal_article [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Freitas ARR, Alarcón-Elbal PM, Paulino-Ramírez R, et al. Excess mortality profile during the Asian genotype chikungunya epidemic in the Dominican Republic, 2014. Trans R Soc Trop Med Hyg. 2018;112:443–449. Available from: https://academic.oup.com/trstmh/article-abstract/112/10/443/5066488 [DOI] [PubMed] [Google Scholar]
- [24].Yoon I-K, Alera MT, Lago CB, et al. High rate of subclinical Chikungunya virus infection and association of neutralizing antibody with protection in a prospective cohort in The Philippines. Powers AM, editor. PLoS Negl Trop Dis [Internet] 2015. [cited 2019 January9];9:E0003764 Available from: https://dx.plos.org/10.1371/journal.pntd.0003764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Dias JP, Costa M, Da CN CGS, et al. Seroprevalence of Chikungunya virus in 2 urban areas of Brazil 1 year after emergence. Emerg Infect Dis. 2018;24:617–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Paixão ES, Rodrigues LC, Costa M Da CN, et al. Chikungunya chronic disease: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg [Internet] 2018. [cited 2019 January9];112(7):301–316. Available from: https://academic.oup.com/trstmh/article/112/7/301/5051873 [DOI] [PubMed] [Google Scholar]
- [27].Gérardin P, Freitas ARR, Sissoko D, et al. Transmission dynamics and disease severity in children infected with East Central South African or ECSA-derived clades of chikungunya virus. Clin Infect Dis. 2019 Jan 1;68(1):171-172. doi: 10.1093/cid/ciy534. [DOI] [PubMed] [Google Scholar]
- [28].Gérardin P, Freitas ARR, Sissoko D. Seroprevalence of Chikungunya virus after its emergence in Brazil. Emerg Infect Dis [Internet] 2018. [cited 2019 January15];24:1773 Available from: http://wwwnc.cdc.gov/eid/article/24/9/18-0724_article.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Godaert L, Najioullah F, Bartholet S, et al. Atypical clinical presentations of acute phase Chikungunya virus infection in older adults. J Am Geriatr Soc. 2017;65:2510–2515. [DOI] [PubMed] [Google Scholar]
- [30].World Health Organization WHO | List of blueprint priority diseases [Internet]. WHO. World Health Organization; 2018. [cited 2018 February14]. Available from: http://www.who.int/blueprint/priority-diseases/en/.
- [31].Hoshiko S, English P, Smith D, et al. A simple method for estimating excess mortality due to heat waves, as applied to the 2006 California heat wave. Int J Public Health [Internet] 2010. [cited 2017 September8];55:133–137. Available from: http://link.springer.com/10.1007/s00038-009-0060-8 [DOI] [PubMed] [Google Scholar]
- [32].Freitas ARR, Donalisio MR. Excess of mortality in adults and elderly and circulation of subtypes of influenza virus in Southern Brazil. Front Immunol [Internet] 2018;8 Available from: http://journal.frontiersin.org/article/10.3389/fimmu.2017.01903/full [DOI] [PMC free article] [PubMed] [Google Scholar]


