Abstract
Background
The global prevalence of obesity in women keeps increasing. The preconception period may be a window of opportunity to improve lifestyle, reduce obesity and improve cardiometabolic health. This study assessed the effect of a preconception lifestyle intervention on long-term cardiometabolic health in two randomized controlled trials (RCTs).
Methods
Participants of the LIFEstyle and RADIEL preconception lifestyle intervention studies with a baseline body mass index (BMI) ≥29 kg/m2 were eligible for this follow-up study. Both studies randomized between a lifestyle intervention targeting physical activity, diet and behaviour modification or usual care. We assessed cardiometabolic health 6 years after randomization.
Results
In the LIFEstyle study (n = 111) and RADIEL study (n = 39), no statistically significant differences between the intervention and control groups were found for body composition, blood pressure, arterial stiffness, fasting glucose, homeostasis model assessment of insulin resistance, HbA1c, lipids and high sensitive C-reactive protein levels 6 years after randomization. Participants of the LIFEstyle study who successfully lost ≥5% bodyweight or reached a BMI <29 kg/m2 during the intervention (n = 22, [44%]) had lower weight (−8.1 kg; 99% CI [−16.6 to −0.9]), BMI (−3.3 kg/m2; [−6.5 to −0.8]), waist circumference (−8.2 cm; [−15.3 to −1.3]), fasting glucose (−0.5 mmol/L; [−1.1 to −0.0]), HbA1c (−4.1 mmol/mol; [−9.1 to −0.8]), and higher HDL-C (0.3 mmol/L; [0.1–0.5]) compared with controls.
Conclusion
We found no evidence of improved cardiometabolic health 6 years after a preconception lifestyle intervention among overweight and obese women in two RCTs. Women who successfully lost weight during the intervention had better cardiometabolic health 6 years later, emphasizing the potential of successful preconception lifestyle improvement.
Introduction
The prevalence of obesity continues to increase globally.1 Obesity is a major modifiable risk factor for cardiometabolic disease.2 Among women, obesity increases the risk of pregnancy complications which also increases the risk of cardiovascular disease.3
Lifestyle interventions targeting diet, physical activity and behaviour are recommended as treatment for obesity.4 These interventions have the potential to decrease weight, lower the risks of cardiometabolic diseases, but also reduce the risks of pregnancy-associated complications.5,6 Because women who are planning a pregnancy are more susceptible to lifestyle advice, the preconception period might be an optimal window of opportunity for a lifestyle intervention.7–9 Preconception lifestyle interventions can improve lifestyle, induce weight loss and improve spontaneous pregnancy rates and outcomes.10–12 We previously showed that a 6-month preconception lifestyle intervention in obese infertile women improved cardiometabolic health, halved the odds for metabolic syndrome (MetS), and increased quality of life, during and directly after the intervention period.13
Although these short-term effects are promising, previous studies have shown that permanent lifestyle changes are difficult to achieve and many people regain weight over time.14 Therefore, we aimed to assess the long-term effects of a preconception lifestyle intervention on cardiometabolic health, based on the follow-up of the Dutch ‘LIFEstyle’ and Finnish ‘RADIEL’ preconception lifestyle intervention trials.15,16
Methods
The randomized controlled trials
The protocols of the LIFEstyle (NTR 1530) and RADIEL (IDr: NCT01698385) studies have been published previously and had ethical approval.15,16 Both studies were preconception lifestyle interventions among overweight or obese women (table 1). All participants provided written informed consent.
Table 1.
Comparison of lifestyle interventions applied in the LIFEstyle and RADIEL study
| LIFEstyle study | RADIEL study | |
|---|---|---|
| Inclusion criteria |
|
|
| Goal |
|
|
| Amount of consultations | Max. 10 consultations in the 6 months before fertility treatment:
|
Max. 14 consultations:
|
| Diet |
|
|
| Physical activity |
|
|
| Motivational counselling |
|
|
The initial LIFEstyle study
The LIFEstyle study, a multi-centre randomized controlled trial (RCT), was conducted in 23 medical centres in the Netherlands between 2009 and 2014. Infertile women between 18 and 39 years of age with a body mass index (BMI) ≥29 kg/m2 were eligible for inclusion. Infertility was defined as chronic anovulation or unsuccessful conception for over 12 months.
Women were successfully randomized (1: 1) to a 6-month lifestyle intervention preceding infertility treatment (intervention group) or prompt infertility treatment according the Dutch guidelines (control group) irrespective of BMI, stratified for trial centre and ovulatory status.17,18
The LIFEstyle intervention led by trained intervention coaches consisted of six 30-min face-to-face sessions at the outpatient clinics and four by telephone or e-mail, aiming at 5–10% weight reduction or a BMI <29 kg/m2 within 6 months. Women reaching this goal did not have to finish the 6-month intervention, but could proceed with conventional infertility treatment. The intervention consisted of a dietary, physical activity and behavioural modification component.19 The dietary component was supported with an online diary and aimed at caloric reduction of 600 kcal with a minimum intake of 1200 kcal/day. The physical activity component aimed at moderate-intensity physical activity for at least two or three times a week and 10 000 steps/day, stimulated with the use of a pedometer. The behavioural modification part of the intervention was focussed on creating awareness of lifestyle predisposing to obesity, and the goals were determined on individual basis. The intervention stopped in case of pregnancy, but was resumed after a miscarriage within 6 months after randomization.
Women in the control group were given written information about the negative effects of overweight/obesity on fertility, as part of the usual care.
The initial RADIEL study
The RADIEL study was a multi-centre RCT, conducted in four maternity hospitals in Finland, between 2008 and 2013. Women ≥18 years of age who were planning to become pregnant, with a BMI ≥30 kg/m2 and/or a history of gestational diabetes (GDM) were eligible for inclusion. Women who met these criteria were recruited through advertisements in newspapers, social media and antenatal clinics, as well as by personal invitation letters based on the hospital record information on their history of GDM.
Women were successfully randomized to a lifestyle intervention (intervention group) or usual care (control group), stratified for trial centre and risk factors (history of GDM or preconception BMI ≥30 kg/m2).20 The intervention group received a structured lifestyle intervention consisting of a maximum of 11 face-to-face sessions and 3 group sessions, provided by trained study nurses. The individual sessions were scheduled every 3 months before pregnancy, once in each trimester of pregnancy, and 6 weeks, 6 and 12 months postpartum. The aim of the intervention was 5% weight reduction and no gestational weight gain in the first and second trimesters. Dietary advice was based on Nordic dietary recommendations encouraging use of vegetables, berries and fish and avoiding sugar-rich foods and saturated fat.21,22 The recommendation for caloric intake was 1600–1800 kcal/day with 40–50% of total energy (E%) coming from carbohydrates, 30–40 E% from fats and 20–25 E% from proteins. Participants also attended group sessions led by a dietitian at the enrolment, during the first trimester, and 6 and 12 months after delivery. Physical activity goal was 150 min of moderately strenuous exercise per week. The participants received pedometers and were encouraged to reach 10 000 steps/day. Lifestyle advice was personalized according to individual preferences and pregnancy status. Women in the control group received general information leaflets about diet and physical activity.
The follow-up studies
The LIFEstyle follow-up study
Women who participated in the original LIFEstyle study and who were not lost to follow-up were eligible for the follow-up study. The follow-up was performed from April 2016 until August 2017. A physical assessment after a 2-h fast was performed minimally 6 months after pregnancy, under standardized conditions, inside of a mobile research vehicle close to the participants’ homes. Blood samples were taken at home, during a separate visit by a research nurse, after an overnight fast. Biochemical analyses were performed by the AMC Clinical Chemistry Laboratory for the biochemical analyses.23
The RADIEL follow-up study
Women who gave birth after participation in the original study and who had at least one study visit during pregnancy were approached for the follow-up study. The follow-up was performed from May 2014 until April 2017. The physical assessment took place at the Folkhälsan Research Center in Helsinki and Lappeenranta at the South Karelian Central Hospital. Anthropometric measurements and blood samples were taken during the study visit after a 10–12 h overnight fast. Biochemical analyses were performed by the HUSLAB central laboratory in Helsinki and Central Hospital laboratory in Lappeenranta. The current study includes women who entered the RADIEL study prior to pregnancy with a BMI ≥29 kg/m2.
Outcomes
Assessments included weight (LIFEstyle study: SECA 877; RADIEL: InBody720), height (SECA 206), and waist and hip circumferences (LIFEstyle: SECA 201; RADIEL: Prym). BMI was calculated as (weight [kg]/length [m2]). Systolic and diastolic blood pressure was measured in sitting position using oscillometry (LIFEstyle: OMRON HBP-1300; RADIEL: OMRON M6W Intellisense). We assessed fasting concentrations of triglycerides, total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C) and high sensitive C-reactive protein (hs-CRP), fasting glucose and insulin. The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated ([fasting insulin (mU/l)] × [fasting glucose (mmol/l)]/22.5).24
Pulse wave velocity (PWV), a marker for aortic elasticity, was measured between the carotid and femoral artery with mechanotransducer sensors using the Complior (ALAM Medical, France) at rest and in supine position. To calculate PWV the following equation was used: PWV = 0.8 × (direct distance between a. carotis and a. fermoralis measuring site/Δ time between upstroke of pressure waves). A scaling factor of 0.8 was used because direct distance leads to overestimation of real PWV.25 Body fat percentage (BFP) was measured in the RADIEL study with multi-frequency bio-impedance measurement method using the InBody 3.0 (Biospace Co, Ltd, Seoul, Korea), and in the LIFEstyle study BFP was measured with arm-to-leg bioelectrical impedance analysis using the Bodystat 1500 (Bodystat Ltd, Isle of Man, UK) and the fat-free mass prediction equation by Kyle et al.26 All outcomes were measured two times. In the LIFEstyle study outcomes were measured a third time in case of substantial differences (>1 cm or >10%) between the first two measurements. The mean of the measurements is used in the statistical analyses.
Participants were identified with MetS based on the 2001 revised criteria of the National Cholesterol Education Programme ATP III.27 Participants had to meet at least three of the following criteria: (i) plasma glucose ≥5.6 mmol/L or known drug treatment for elevated blood glucose; (ii) HDL-C < 1.3 mmol/L or known drug treatment for low HDL cholesterol; (iii) triglycerides ≥1.7 mmol/L or known drug treatment for elevated triglycerides; (iv) waist circumference ≥88 cm or (v) blood pressure ≥130/85 mmHg or known drug treatment for elevated blood pressure.
Statistical analyses
Participants were analysed on intention-to-treat basis, in the treatment group in which they were originally randomized. For comparison of the baseline variables independent student t-tests or Mann–Whitney-U tests were performed for continuous variables and Chi-Square tests for binary or categorical variables. The continuous outcomes were analysed with linear regression, including 1500 bootstrap samples to calculate 99% bias-corrected and accelerated confidence intervals (99% BCa CI), because the normality assumption of linear regression appeared to be violated for some of the outcome variables (IBM SPSS version 24.0, Armonk, NY, USA). The regression models included the outcomes of interest as the dependent and the treatment group as independent factor. If available, baseline values of the outcomes of interests and potential confounders that differed between the treatment groups were incorporated as covariates. The difference between the groups was considered statistically significant if the CI of the mean difference did not include zero. Mixed effect logistic regression analyses including baseline and follow-up data were performed for binary outcomes (STATA version 15.0, College Station, TX, USA). The intervention effect was assessed by the interaction between time and treatment group. Subgroup analyses were performed to compare successful women with the control group. Women were identified as ‘successful’ if they had reduced their body weight ≥5% or lowered their BMI under 29 kg/m2. Baseline differences in characteristics between the successful women and the control group were added as covariates to the adjusted model. Further explorative analyses were performed to assess (i) the interaction between treatment group and pregnancy status after randomization as well as (ii) between treatment group and polycystic ovary syndrome (PCOS) status on the outcomes of interest.28 These explorative analyses were only performed in the LIFEstyle study population, because of data availability.
Results
Participation
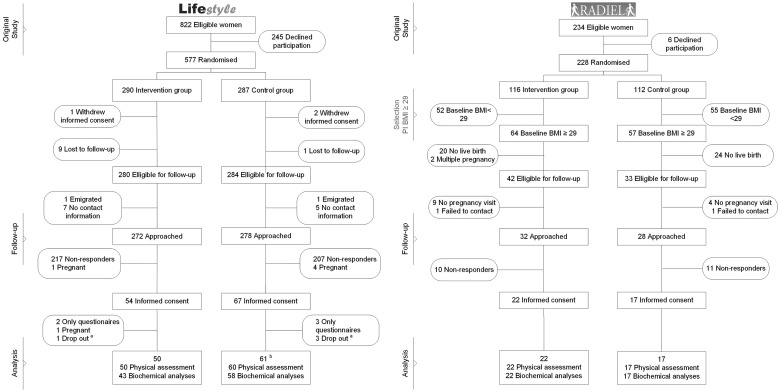
The flow charts of both studies are presented in Figure 1. Of the 577 women who participated in the LIFEstyle study, 111 (19.3%) with a median follow-up duration of 73.1 months (interquartile range [IQR] 63.9–80.4) were included in the current study, of whom 50 women were included in the intervention and 61 in the control group. Of the 234 women who were recruited before pregnancy in the RADIEL study, 121 women had a BMI of 29.0 or above. Of these eligible women 39 (32.2%) with a median follow-up duration of 74.2 months (IQR 70.7–81.8) were included in this study, of whom 22 women were included in the intervention and 17 in the control group.
Figure 1.
Flow-chart of study participants. a: One woman in the intervention and three women in the control group had given informed consent but cancelled the physical measurement visit. b: One woman only attended the blood sample collection, but cancelled the physical measurement.
Characteristics of participants
Baseline and follow-up characteristics of the participating women in both studies are presented in table 2. A total of 82 (74%) women of the LIFEstyle study, in comparison to all women of the RADIEL study had a pregnancy of more than 24 weeks between randomization and follow-up.
Table 2.
Baseline and follow-up characteristics of the study participants
| Baseline characteristics | LIFEstyle Study | RADIEL study | ||||
|---|---|---|---|---|---|---|
| Variables | Intervention (n = 50) | Control (n = 61) | P-valuea | Intervention (n = 22) | Control (n = 17) | P-valuea |
| Age, years—mean (SD) | 30.4 (4.0) | 30.4 (4.2) | 0.94 | 34.2 (3.3) | 31.6 (5.3) | 0.09 |
| Ethnicity—no. Caucasian (%) | 48 (96) | 57 (93.4) | 0.69 | 22 (100) | 17 (100) | n.a. |
| Education—no. (%) | 0.95 | 0.41 | ||||
| Basic education | 0 (0) | 1 (1.7) | 0 (0) | 0 (0) | ||
| Vocational education | 11 (23.4) | 12 (20.3) | 4 (19.0) | 2 (11.8) | ||
| Secondary education | 1 (2.1) | 1 (1.7) | 1 (4.8) | 4 (23.5) | ||
| Vocational & Secondary education | 24 (51.1) | 28 (47.5) | 9 (42.9) | 7 (41.2) | ||
| Higher education | 11 (23.4) | 17 (28.8) | 7 (33.3) | 4 (23.5) | ||
| Alcohol use—no. (%) | 19 (44.2) | 19 (32.8) | 0.24 | 11 (52.4) | 12 (70.6) | 0.25 |
| Current smoker—no. (%) | 14 (28.6) | 11 (18.0) | 0.19 | 1 (4.5) | 1 (5.9) | 1.00 |
| Nulliparous—no. (%) | 41 (82.0) | 45 (73.8) | 0.30 | 2 (9.1) | 5 (29.4) | 0.21 |
| Weight, kg—mean (SD) | 103.6 (13.0) | 102.8 (11.4) | 0.75 | 97.5 (15.0) | 94.7 (16.4) | 0.59 |
| BMI, kg/m2—mean (SD) | 35.5 (2.9) | 35.8 (3.2) | 0.64 | 35.2 (4.0) | 34.0 (5.2) | 0.44 |
| Systolic blood pressure, mmHg—mean (SD) | 123.1 (11.8) | 127.2 (12.5) | 0.08 | 127.3 (9.6) | 120.3 (9.6) | 0.03 |
| Diastolic blood pressure, mmHg—mean (SD) | 79.0 (8.3) | 81.6 (7.2) | 0.08 | 85.1 (8.5) | 80.8 (8.0) | 0.12 |
| Fasting glucose, mmol/L—mean (SD) | 5.1 (0.3) | 5.5 (0.9) | 0.02 | 5.6 (0.5) | 5.6 (0.4) | 0.82 |
| HOMA-IR—median (IQR) | 2.9 (1.8–3.9) | 3.1 (2.4–4.2) | 0.26 | 2.3 (1.8–3.5) | 2.3 (1.5–4.4) | 0.78 |
| Total Cholesterol, mmol/L—mean (SD) | 4.8 (1.0) | 4.7 (0.8) | 0.56 | 4.8 (0.6) | 4.7 (1.0) | 0.57 |
| LDL Cholesterol, mmol/L—mean (SD) | 3.1 (0.9) | 3.0 (0.7) | 0.54 | 3.0 (0.7) | 2.8 (0.7) | 0.28 |
| HDL Cholesterol, mmol/L—mean (SD) | 1.2 (0.3) | 1.1 (0.3) | 0.08 | 1.3 (0.3) | 1.4 (0.5) | 0.59 |
| Triglycerides, mmol/L—median (IQR) | 1.0 (0.7–1.3) | 1.2 (0.9–1.7) | 0.06 | 1.0 (0.7–1.3) | 0.9 (0.6–1.4) | 0.32 |
| HS-CRP, mg/l—median (IQR) | 3.6 (2.5–6.9) | 3.1 (1.4–7.6) | 0.25 | 2.7 (1.5–6.5) | 1.2 (0.9–2.0) | < 0.01 |
| Follow-up characteristics | ||||||
| Age at follow-up, years—mean (SD) | 36.3 (4.4) | 36.5 (4.3) | 0.83 | 40.6 (3.3) | 38.0 (5.3) | 0.08 |
| Follow-up duration, months—median (IQR) | 73.5 (61.3–80.4) | 72.9 (65.4–80.4) | 0.65 | 74.8 (71.0–82.2) | 72.2 (69.8–82.2) | 0.75 |
| Pregnancy after randomization, no. (%)b | 35 (70) | 47 (77) | 0.40 | 22 (100) | 17 (100) | n.a. |
P-values of continuous outcomes based on student t-test or Mann–Whitney-U test. P-values of dichotomous and categorical outcomes are based on the Pearson Chi-Square test, the Fisher’s exact test or Fisher-Freeman-Halton exact test.
Number of women that had a pregnancy of ≥24 weeks of gestation.
A comparison of baseline characteristics of participants and non-participants are presented in Supplementary table S1. Women who participated in the follow-up of the LIFEstyle study were more often Caucasian (94.6% vs. 85.7%; P = 0.01) and older at baseline (30.4 [4.1] vs. 29.6 [4.6] years; P = 0.07) than women who did not participate in the follow-up study.
Outcomes
Primary analyses
In both studies, weight, BMI, waist and hip circumferences, blood pressure, fasting glucose, HOMA-IR, HbA1c, triglycerides, total cholesterol, LDL-C, HDL-C, hs-CRP, BFP and PWV were not statistically different between the intervention and control group (table 3).
Table 3.
Cardiometabolic outcomes (change from baseline to 6-year follow-up and mean difference) in the intervention and control group of the LIFEstyle and RADIEL study
| Cardiometabolic outcomes | LIFEstyle study | RADIEL study | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Intervention | n | Control | MDb | BCa 99% | n | Intervention | n | Control | MDb,c | BCa 99% | |
| Δa | Δa | C.I. | Δa | Δa | C.I. | |||||||
| Weight, kg—mean (SD) | 50 | −3.4 (14.2) | 60 | −1.5 (13.5) | −1.8 | −8.8 to 4.7 | 22 | 2.9 (15.4) | 17 | −1.8 (9.3) | 2.0 | −10 to 11.8 |
| BMI, kg/m2—mean (SD) | 50 | –0.5 (5.1) | 60 | 0.0 (4.7) | –0.6 | –2.7 to 1.6 | 22 | 1.1 (5.6) | 17 | –0.6 (3.2) | 0.7 | −3.5 to 4.2 |
| Waist Circumference, cm—mean (SD) | 48 | –0.5 (12.5) | 60 | –0.3 (13.5) | –0.8 | –6.1 to 4.6 | 21 | 7.1 (12.9) | 17 | 8.1 (10.0) | –3.2 | –14.3 to 8.0 |
| Hip Circumference, cm—mean (SD) | 49 | –2.6 (9.9) | 60 | –2.5 (9.4) | –0.5 | –5.0 to 3.6 | 21 | 2.9 (13.1) | 17 | –3.2 (6.6) | 4.8 | –4.6 to 13.8 |
| Systolic Blood pressure, mmHg—mean (SD) | 48 | –3.9 (14.6) | 60 | –6.0 (15.3) | –0.2 | –7.3 to 6.9 | 22 | 2.7 (11.1) | 17 | 3.7 (15.0) | 1.6 | –11.2 to 17.5 |
| Diastolic Blood pressure, mmHg—mean (SD) | 48 | 1.6 (10.2) | 60 | 0.5 (9.4) | –0.5 | –5.1 to 4.4 | 22 | –0.8 (8.4) | 17 | –2.8 (11.0) | 4.1 | –4.1 to 12.4 |
| Fasting glucose, mmol/L—mean (SD) | 36 | 0.0 (0.6) | 52 | 0.0 (1.1) | –0.3 | –0.7 to 0.2 | 22 | –0.1 (0.7) | 17 | 0.0 (0.5) | –0.2 | –0.7 to 0.4 |
| HOMA-IR—mean (SD) | 35 | –0.1 (2.3) | 50 | 0 (2.6) | –0.4 | –1.6 to 0.9 | 18 | 1.4 (2.8) | 16 | 0.8 (2.2) | 0.3 | –2.3 to 2.6 |
| Total Cholesterol, mmol/L—mean (SD) | 36 | –0.1 (1.0) | 52 | 0.0 (0.8) | 0.0 | –0.5 to 0.5 | 22 | –0.1 (0.7) | 16 | –0.1 (0.6) | –0.1 | –0.6 to 0.5 |
| LDL Cholesterol, mmol/L—mean (SD) | 36 | –0.2 (1.0) | 52 | –0.2 (0.7) | 0.0 | –0.4 to 0.4 | 22 | 0.0 (0.7) | 16 | 0.2 (0.5) | –0.2 | –0.8 to 0.4 |
| HDL Cholesterol, mmol/L—mean (SD) | 36 | 0.2 (0.3) | 52 | 0.1 (0.3) | 0.1 | –0.0 to 0.3 | 22 | 0.1 (0.4) | 16 | 0.0 (0.4) | 0.1 | –0.2 to 0.5 |
| Triglycerides, mmol/L—mean (SD) | 36 | –0.3 (1.6) | 52 | –0.1 (0.6) | –0.3 | –0.7 to 0.3 | 22 | –0.1 (0.7) | 16 | 0.1 (0.6) | –0.1 | –0.6 to 0.4 |
| HS-CRP, mg/l—mean (SD) | 36 | 0.1 (4.5) | 52 | 1.8 (5.6) | –1.6 | –4.4 to 1.2 | 22 | –0.5 (6.3) | 17 | –0.1 (2.5) | 0.6 | –3.5 to 5.9 |
| HbA1c, mmol/mol—mean (SD)d | 42 | n.a. | 52 | n.a. | –1.7 | –5.2 to 1.2 | 18 | 1.6 (4.7) | 11 | –0.3 (5.7) | 1.2 | –3.3 to 7.1 |
| Fat percentage, %e | 50 | n.a. | 60 | n.a. | –0.5 | –2.7 to 1.3 | 17 | n.a. | 16 | n.a. | –1.1 | –8.5 to 5.8 |
| PWV, m/sf | 37 | n.a. | 49 | n.a. | 0.1 | –1.2 to 1.1 | 19 | n.a. | 16 | n.a. | 0.4 | –0.8 to 1.7 |
Change between baseline and follow-up.
Mean differences between intervention and control group at follow-up based on linear regression models adjusted for baseline values, unless stated otherwise.
Adjusted for age at baseline.
No baseline value in LIFEstyle study, mean difference is unadjusted.
No baseline value, mean difference is adjusted for BMI at baseline.
No baseline value, mean difference is adjusted for pulse pressure at baseline.
Although the prevalence of MetS at follow-up was lower in the LIFEstyle intervention group compared with the control group (25.7 vs. 52.7%), adjustments for baseline prevalence showed no statistically significant difference between the intervention and control group (aOR: 1.11 95% CI 0.19–6.64). Also, no statistical significant difference in MetS prevalence at follow-up was found in the RADIEL study (aOR: 0.20 95% CI 0.01–2.8).
Subgroup analyses
Of the 50 women in the LIFEstyle intervention group, 22 women lost ≥5% body weight or reached a BMI <29 kg/m2 during the 6-month intervention period. These women had a lower BMI at baseline (34.2 ± 2.6 vs. 35.8 ± 3.2; P = 0.02), more often smoked (9 [40.9%] vs. 11 (18.0%); P = 0.03) and had been trying to conceive for a longer period of time (27 [IQR 19.5–40.25] vs. 16 [12.0–26.0] months; P = 0.04) compared with the control group. No other statistically significant differences were detected.
At follow-up, these successful women had lower weight (–8.1 kg; 99% BCa CI = −16.6 to −0.9), BMI (−3.3 kg/m2; 99% BCa CI = –6.5 to −0.8), smaller waist circumference (−8.2 cm; 99% BCa CI = −15.3 to −1.3), lower fasting glucose (−0.5 mmol/L; 99% BCa CI = −1.1 to −0.0), lower HbA1c (−4.1 mmol/mol; 99% BCa CI = −6.4 to −0.3), and higher HDL-C (0.3 mmol/L; 99% BCa CI =0.1–0.5) compared with controls (Supplementary table S2).
No subgroup analyses of successful intervention were performed for the RADIEL study, because only four of the RADIEL intervention women successfully reached the short-term weight goals.
Exploratory analyses
No statistically significant interaction effects were found for treatment group with pregnancy status after randomization or for treatment group with PCOS status on any of the continuous outcomes (all interaction P ≥0.05).
Discussion
This is the first study reporting on the effects of preconception lifestyle interventions on long-term cardiometabolic health of overweight and obese women from two RCTs. Despite the positive short-term effects of the LIFEstyle preconception intervention, the six year follow-up of both the LIFEstyle and the RADIEL interventions did not show any effects on individual parameters of cardiometabolic health, nor on the prevalence of metabolic syndrome.13 However, in comparison to controls, women who successfully lost weight during the LIFEstyle intervention period had better long-term cardiometabolic outcomes in terms of smaller waist circumferences, lower weight, BMI, glucose and HbA1c, as well as higher HDL cholesterol concentrations.
The absence of an overall effect of the interventions on long-term cardiometabolic health is in line with the only other study with a similar follow-up duration after a lifestyle intervention in pregnancy.29 Other post-conception lifestyle interventions in overweight and obese women reported inconsistent effects on adverse maternal outcomes during and directly after pregnancy, and did not yet report on the long-term health of these women.30–32 Lifestyle is attained over time and is not easily changed without intrinsic motivation.33 The wish to have a child could be a strong motivator to improve lifestyle, but at the same time, the temporary nature of this motivator may explain the lack of long-term effects on cardiometabolic outcomes. After giving birth, mothers are exposed to the emotional post-partum period in which they adjust to their new role and often prioritize parenthood over their own wellbeing.34 However, we found no evidence that women who had an ongoing pregnancy (≥24 weeks) during the follow-up period had different long-term effects on cardiometabolic health compared with women who did not. The latter could be explained by the discouraging effect of persistent infertility on lifestyle improvement in this last group.35 In both scenario’s, an individualized relapse prevention phase following the actual intervention could help women to adhere to their improved lifestyle.36
The absence of long-term effects of the preconception lifestyle interventions on cardiometabolic health could also be explained by the high-risk profile of the study populations, who might need more intensive and prolonged lifestyle interventions for sustainable effects on cardiometabolic health. In the RADIEL study, 67% of the women in the current follow-up study were diagnosed with GDM in their index pregnancy, leading to additional lifestyle advice and intensive follow-up from the healthcare system in both treatment groups. This regular care might have overshadowed the effect of the preconception lifestyle intervention, diminishing the potential differences between the intervention and control group. In the LIFEstyle study, 39% of the women were diagnosed with PCOS. Intrinsic insulin resistance, alteration in appetite regulation and abdominal fat distribution can challenge weight management in women with PCOS.37,38 However, the relatively high prevalence of women with PCOS in the LIFEstyle study could not explain the absence of long-term effects since no interaction effect was observed between treatment group and PCOS status on cardiometabolic outcomes.
Timing and duration of lifestyle interventions are possible determinants of successful lifestyle change, but in this study we found no such evidence.39 Scheduling the intervention solely before (LIFEstyle) compared with before, during, and after pregnancy (RADIEL) both failed to provide beneficial cardiometabolic effects in the long run.
Both studies had considerable attrition (LIFEstyle study: 80.7%; RADIEL study: 67.8%), leading to limited statistical power to detect relevant differences and introduction of potential selection bias. To diminish potential confounding effects of selection on the outcome assessments, the regression analyses were adjusted for baseline values. Women of the LIFEstyle study follow-up were more likely to participate if they were Caucasian and slightly (0.8 year) older at randomization. Although cardiometabolic plasticity decreases with age, it is unlikely that this small difference in age explains our null-findings.40 Similar selection was not found for the RADIEL study (Supplementary table S1). Because of the high percentage of Caucasian women in both studies, it should be noted that our findings should not be generalized to women of other ethnicities.
Short-term success is usually a good indicator for long-term effects.14,35 Although we did not find overall effects, women who successfully lost weight during the LIFEstyle intervention, did have better cardiometabolic health 6 years after the intervention compared with control women. Future studies should therefore investigate determinants of a successful lifestyle intervention, in order to identify women who would benefit the most and to make tailored approaches more effective.
Supplementary Material
Acknowledgements
We thank all the women who participated in this study. We thank all participating hospitals and their staff for their contribution to this study, and the lifestyle coaches, research nurses, research midwives for their hard work and dedication. Furthermore, we thank all members of the WOMB-project and RADIEL study who contributed to the follow-up study; with special thanks to our colleague PhD students, post-docs, research assistants and students.
Funding
The LIFEstyle study has been conducted with the support of a grant [50-50110-96-518] from the Netherlands Organization for Health Research and Development and the Dutch Heart Foundation grant [2013T085]. Ben Willem J Mol is supported by a NHMRC Practitioner Fellowship [GNT1082548]. The RADIEL study was funded by Ahokas Foundation, the Finnish Foundation for Cardiovascular Disease, Academy of Finland, Special state subsidy for health science research of Helsinki University Hospital (HUH), Samfundet Folkhälsan, Finska Läkaresällskapet, Juho Vainio Foundation, Viipuri Tuberculosis Foundation, The Finnish Diabetes Research Foundation, State Provincial Office of Southern Finland, Health Promotion Grant (Ministry of Social Affairs and Health) EU H2020-PHC-2014-DynaHealth [633595] and The Social Insurance Institution of Finland.
Conflicts of interest: The department of Reproductive Medicine of the UMCG received an unrestricted educational grant from Ferring pharmaceuticals BV, The Netherlands. Ben Willem J. Mol reports consultancy for ObsEva, Merck and Guerbet.
Key points
The preconception period is a potential window of opportunity to improve long-term cardiometabolic health of overweight and obese women planning a pregnancy.
Despite promising short-term effects, a preconception lifestyle intervention does not lead to long-term improvements of cardiometabolic health based on two RCT’s.
Women who successfully reached their target weight during the intervention period, showed improved cardiometabolic health 6 years later.
References
- 1. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016;387:1377–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kivimäki M, Kuosma E, Ferrie JE, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health 2017;2:e277–e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cirillo PM, Cohn BA. Pregnancy complications and cardiovascular disease death. 50-year follow-up of the child health and development studies pregnancy cohort. Circulation 2015;132:1234–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Apovian CM, Aronne LJ, Bessesen DH, et al. Pharmacological management of obesity: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2015;100:342–62. [DOI] [PubMed] [Google Scholar]
- 5. Thangaratinam S, Rogozińska E, Jolly K, et al. Effects of interventions in pregnancy on maternal weight and obstetric outcomes: meta-analysis of randomised evidence. BMJ 2012;344:e2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tuomilehto J, Lindström J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344:1343–50. [DOI] [PubMed] [Google Scholar]
- 7. Herzig K, Danley D, Jackson R, et al. Seizing the 9-month moment: addressing behavioral risks in prenatal patients. Patient Educ Counsel 2006;61:228–35. [DOI] [PubMed] [Google Scholar]
- 8. McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res 2003;18:156–70. [DOI] [PubMed] [Google Scholar]
- 9. Pryor J, Patrick SW, Sundermann AC, et al. Pregnancy intention and maternal alcohol consumption. Obstetr Gynecol 2017;129:727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Legro RS, Dodson WC, Kris-Etherton PM, et al. Randomized controlled trial of preconception interventions in infertile women with polycystic ovary syndrome. J Clin Endocrinol Metab 2015;100:4048–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hillemeier MM, Downs DS, Feinberg ME, et al. Improving women’s preconceptional health: findings from a randomized trial of the Strong Healthy Women Intervention in the Central Pennsylvania Women’s Health Study. Women's Health Issues 2009;13:18– S96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The International Weight Management in Pregnancy (i-WIP) Collaborative Group. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: meta-analysis of individual participant data from randomised trials. BMJ 2017;358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. van Dammen L, Wekker V, van Oers AM, et al. Effect of a lifestyle intervention in obese infertile women on cardiometabolic health and quality of life: a randomized controlled trial. PLoS One 2018;13:e0190662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stelmach-Mardas M, Mardas M, Walkowiak J, Boeing H. Long-term weight status in regainers after weight loss by lifestyle intervention: status and challenges. Proc Nutr Soc 2014;73:509–18. [DOI] [PubMed] [Google Scholar]
- 15. Rönö K, Stach-Lempinen B, Klemetti MM, et al. Prevention of gestational diabetes through lifestyle intervention: study design and methods of a Finnish randomized controlled multicenter trial (RADIEL). BMC Pregnancy Childbirth 2014;14:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mutsaerts MAQ, Groen H, ter Bogt NCW, et al. The LIFESTYLE study: costs and effects of a structured lifestyle program in overweight and obese subfertile women to reduce the need for fertility treatment and improve reproductive outcome. A randomised controlled trial. BMC Women's Health 2010;10:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.NVOG. Data sheet Dutch Society of Obstetrics and Gynaecology. Available at: http://nvog-documenten.nl/index.php? pagina=/richtlijn/pagina.php&fSelectNTG_112=113&fSelectedSub=112 (25 January 2010, date last accessed).
- 18. Mutsaerts MAQ, van Oers AM, Groen H, et al. Randomized trial of a lifestyle program in obese infertile women. N Engl J Med 2016;374:1942–53. [DOI] [PubMed] [Google Scholar]
- 19. Yumuk V, Tsigos C, Fried M, et al. European guidelines for obesity management in adults. Obesity Facts 2015;8:402–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rönö K, Stach-Lempinen B, Eriksson J, et al. Prevention of gestational diabetes with a prepregnancy lifestyle intervention – findings from a randomized controlled trial. Int J Women's Health 2018;10:493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hasunen KKM, Keinonen H, Lagström H, et al.The Child, Family and Food. Nutrition Recommendations for Infants and Young Children as Well as Pregnant and Breastfeeding Mothers. Helsinki: Publications of the Ministry of Social Affairs and Health, 2004. [Google Scholar]
- 22.Valtion ravitsemusneuvottelukunta. Finnish Nutrition Recommendations – Diet and Physical Activity in Balance 2005. Committee Report. Helsinki, 2005.
- 23. van de Beek C, Hoek A, Painter RC, et al. Women, their Offspring and iMproving lifestyle for Better cardiovascular health of both (WOMB project): a protocol of the follow-up of a multicentre randomised controlled trial. BMJ Open 2018;8:e016579. Doi:10.1136/bmjopen-2017-016579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–9. [DOI] [PubMed] [Google Scholar]
- 25.Reference Values for Arterial Stiffness Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur Heart J 2010;31:2338–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kyle UG, Genton L, Karsegard L, et al. Single prediction equation for bioelectrical impedance analysis in adults aged 20–94 years. Nutrition 2001;17:248–53. [DOI] [PubMed] [Google Scholar]
- 27. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome. Circulation 2005;112:2735. [DOI] [PubMed] [Google Scholar]
- 28.The Rotterdam EA-SPCWG. Revised consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril 2003;81:19–25. [DOI] [PubMed] [Google Scholar]
- 29. Puhkala J, Raitanen J, Kolu P, et al. Metabolic syndrome in Finnish women 7 years after a gestational diabetes prevention trial. BMJ Open 2017;7:e014565. Doi:10.1136/bmjopen-2016-014565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vinter CA, Jensen DM, Ovesen P, et al. Postpartum weight retention and breastfeeding among obese women from the randomized controlled Lifestyle in Pregnancy (LiP) trial. Acta Obstetr Gynecol Scand 2014;93:794–801. [DOI] [PubMed] [Google Scholar]
- 31. Poston L, Bell R, Croker H, et al. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol 2015;3:767–77. [DOI] [PubMed] [Google Scholar]
- 32. Walsh JM, McGowan CA, Mahony R, et al. Low glycaemic index diet in pregnancy to prevent macrosomia (ROLO study): randomised control trial. Br Med J 2012; 345: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kozica S, Lombard C, Teede H, et al. Initiating and continuing behaviour change within a weight gain prevention trial: a qualitative investigation. PLoS One 2015;10:e0119773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bennett WL, Ennen CS, Carrese JA, et al. Barriers to and facilitators of postpartum follow-up care in women with recent gestational diabetes mellitus: a qualitative study. J Women's Health 2011;20:239–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Burgess E, Hassmén P, Pumpa KL. Determinants of adherence to lifestyle intervention in adults with obesity: a systematic review. Clin Obes 2017;7:123–35. [DOI] [PubMed] [Google Scholar]
- 36. Brennan L, Teede H, Skouteris H, et al. Lifestyle and behavioral management of polycystic ovary syndrome. J Women's Health 2017;26:836–48. [DOI] [PubMed] [Google Scholar]
- 37. Lisa JM, Catherine BL, Siew L, et al. Polycystic ovary syndrome and weight management. Women's Health 2010;6:271–83. [DOI] [PubMed] [Google Scholar]
- 38. Moran LJ, Noakes M, Clifton PM, et al. Ghrelin and measures of satiety are altered in polycystic ovary syndrome but not differentially affected by diet composition. J Clin Endocrinol Metab 2004;89:3337–44. [DOI] [PubMed] [Google Scholar]
- 39. Messina J, Campbell S, Morris R, et al. A narrative systematic review of factors affecting diabetes prevention in primary care settings. PLoS One 2017;12:e0177699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Flaatten H, Skaar E, Joynt GM. Understanding cardiovascular physiology of ageing. Intensive Care Med 2018;44:932–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.