Abstract
Background and Purpose
Cognitive training is known to be an effective tool in enhancing cognitive functioning. Research has also shown that playing video game improves certain aspects of visual attention and cognitive processing speed. The effect of computer-based cognitive training has not been demonstrated so far. This study therefore evaluated whether computer-based cognitive training improved the cognitive abilities in patients with early stage of Alzheimer's dementia.
Methods
Totally, 20 participants (early stage of Alzheimer's dementia) participated in this study. To test the effectiveness of computer-based cognitive training programs to cognition, all patients were randomly allocated to either an intervention group (n=10) or a control group (n=10). The intervention group regularly received 24 sessions of computer-based cognitive training, over a 12 week period. Neuropsychological examinations were conducted before and after this training period.
Results
After 12 weeks, the intervention group showed a significant change in language of Korean version of the Mini-Mental State Examination (K-MMSE), compared with the baseline cognitive examinations. Also, there was greater improvement in language, attention, calculation, verbal memory, and frontal function for the experimental group, as compared with controls.
Conclusions
Computer-based cognitive training might have beneficial effects on the general cognitive functions in early stage of Alzheimer's dementia.
Keywords: Alzheimer's dementia, computer-based cognitive training, cognition
INTRODUCTION
Since Korea is the world's fastest growing country in entering a super-aged society. It is therefore necessary to systematically prepare for geriatric disease management. Dementia is a disease that significantly occurs in the elderly, having a substantial expenditure towards the treatment and management of the patient, causing immense burden on individual medical expenses and national medical finances. In addition, it is typically a disease where delayed detection and treatment results in a gradual increase in the proportion of the national health finance.1 The degeneration of the cholinergic nerve, which migrates from the basal nucleus of Meynert to the hippocampus or temporal lobe, and consequent decrease of brain acetylcholine, is associated with cognitive impairment, behavioral impairment, and hypofunction in Alzheimer's disease. Based on these results, acetylcholinesterase inhibitors (AChEIs) have been developed and used as the foremost treatments in Alzheimer's disease. However, the main effect of AChEIs is symptomatic relief, but no prevention of disease progression.2 Since cognitive impairment interferes with behavioral and neuropsychiatric problems as well as the patient's ability to function independently in daily life,3 the cognitive programs are being introduced to ensure the self-sufficiency of the patient.4 Cognitive treatment as a non-pharmacologic treatment is divided into various processes: cognitive stimulation, which is a preventive measure for normal people; cognitive training, that integrates each area of concentration, language ability, executive function, and memory; and cognitive rehabilitation, which aims to improve daily life by intensively training one cognitive domain.5 The cognitive training program mainly aims at the recovery of impaired cognitive functions. However, with the concept of brain plasticity being recently introduced, where it is possible to reorganize the brain tissue for the utmost utilization of brain function,6 the cognitive training program has been actively studied for patients in early stages of Alzheimer's dementia.7 In particular, computer-based cognitive training programs which are relatively easy to access during cognitive training, are being developed and applied.8 Computer-based cognitive treatment was first used in 1988 by Glisky and Schacter.9 in a computer-based memory training for memory-impaired patients. In 2000, Palmese and Raskin10 applied the attention process training-II program for 10 weeks, to three patients with mild traumatic brain injury, which resulted in an improvement in the speed of concentration and achievement, and remained stable for up to 6 weeks after treatment. It has recently been reported that a 6-months computer-based program for patients with dementia improved the spatio-temporal ability in patients with mild cerebral atrophy, compared to the control group.8 The purpose of this study is to investigate the effects of computer-based cognitive programs on cognitive function in patients who are in the early stage of Alzheimer's dementia, and are taking medication.
METHODS
Study subjects
Memory deterioration patients who visited the Veteran Health Service Medical Center, Namyangju VHS Geriatric Hospital, and the Suwon VHS Geriatric Hospital, from January 2015 to October 2016, were selected for this study. Patients were diagnosed with Alzheimer dementia, based on the criteria of the National Institute of Neurologic and Communicative Disorders and Stroke-Alzheimer Disease and Related Disorders Association11 standard; patients with mild symptoms [Clinical Dementia Rating Scale (CDR)=0.5, CDR=1] were enrolled for the study. The dosage of medication for all patients remained unchanged for 3 months. Exclusion criteria were: 1) Brain tumor or encephalitis; 2) Mental illnesses, based on the Diagnostic and Statistical Manual of Mental Disorders criteria, within 2 years before the start of the study; 3) Severe depression (Hamilton Depression Rating Scale score >18); 4) Parkinson's disease, Huntington's disease, or any other neurological disorders of normal pressure hydrocephalus; 5) Cases of medical diseases (liver disease, kidney disease, thyroid disease) that cause other cognitive function decline; 6) Patients with alcohol or drug addiction within 2 years before the start of the study; 7) A physical disability, that hinders the completion of a computer program. All patients underwent basic demographic investigation and screening tests, using the Korean version of the Mini-Mental State Examination (K-MMSE)12 developed by Morris.13 The severity of Alzheimer's disease of patient was assessed according to the CDR.
Study design
All subjects underwent physical and neurological examinations by a neurologist. The same neuropsychologist conducted the basic neuropsychiatric test for all patients, before starting the program; all patients also underwent MRI examination. A total of 20 patients with mild Alzheimer's disease (CDR=0.5, CDR=1) were enrolled at the Veteran Health Service Medical Center, Namyangju VHS Geriatric Hospital, and the Suwon VHS Geriatric Hospital. Random number tickets were assigned to the test group; patients with odd number were assigned to the experimental group, whereas those with even number were assigned to the control group. Over the next 12 weeks, 24 sets of cognitive programs were conducted, and the same neuropsychological test was repeated within two weeks of completion. This study was approved by the Medical Research Ethics Committee of the Veteran Health Service Medical Center.
Computer-based cognitive program
Brain-Care is a step-by-step customized computer-based cognitive program, which distinguishes the ability to significantly lower each cognitive area, focusing on the functions of the seven cognitive domains, thereby improving the brain cognitive ability of the domain and enhancing the brain's higher level functions. Brain-Care is therefore a cognitive enhancement software that improves the brain function as per the following classifications: 1) Attention and concentration ability, 2) Spatio-temporal ability, 3) Memory, 4) Execution ability, 5) Language ability, 6) Calculation ability, and 7) Sound perception ability. In particular, the training program is designed to allow the device to self-assess and intensively train problem areas with low learning effects. Brain-Care was performed twice a week (60 minutes per session), for a total of 12 weeks. Each question was provided according to the guidance of voice and subtitles, and the subject provided a solution within a predetermined time by touching the screen with his finger, or moving the finger while touching. In addition, after each step, the results were automatically stored and designed to make the patient feel fulfilled. All courses were accompanied by a skilled occupational therapist to manage the progress of the program.
Neuropsychological test
The Seoul Neuropsychological Screening Battery was used for the neuropsychological assessment of each cognitive function area of the patient.14 For each sub-cognitive domain, concentration ability was investigated with the ‘forward and backward’ of the digit span, language ability was investigated with the Korean version of the Boston Naming Test (K-BNT),15 and spatio-temporal ability was investigated with the tracing drawings score of the Rey Complex Figure test (RCFT).16 Verbal memory and visual memory were assessed using immediate recall scores (total score of 3 trials), delayed recall scores, and recognition test scores of each Seoul Verbal Learning Test and RCFT. In order to examine functioning of the frontal lobe, each score of the two (animal and market) semantic word fluency of the Controlled Oral Word Association Test,17 the sum of the three (ㄱ, ㅇ, ㅅ) phonemic word fluency score, and the color reading score of the Korean-Color Word Stroop Test18 were used. Totally, the test was carried out twice. A 12-week computer-based cognitive program was performed after basic examination, and the neuropsychiatric re-examination was performed 13 to 14 weeks after the basic examination to confirm immediate effects.
Statistical analysis method
All statistical analyses used the SPSS 18.0 (IBM Corp., Armonk, NY, USA) with the 2-tailed test, with the level of significance 0.05. For analysis of means for continuous variables, the Mann-Whitney U test was used. The percentage comparison of categorical data was performed using the chi-square test. Efficacy assessment was based on a pre/post comparison of the evaluations carried out at the baseline, and at 12 weeks. For this test, repeated measure of general linear model was used.
RESULTS
Demographic analysis
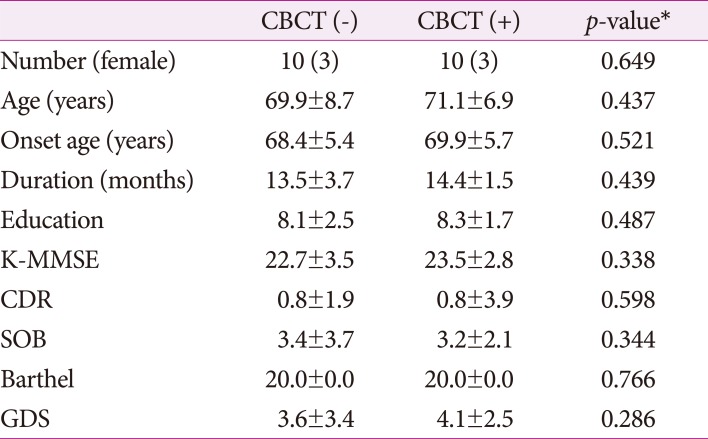
There was no difference in age, sex, education and training, and clinical dementia stage between the experimental and control groups. Also, no difference was observed between the groups in terms of K-MMSE, CDR, and Geriatric Depression Scale (Table 1).
Table 1. Demographic data between CBCT (−) patients and CBCT (+) patients (mean±standard deviation).
*Mann-Whitney U test was used for continuous variable, and chi-square test was used for categorical variable.
CBCT: computer-based cognitive training, CDR: Clinical Dementia Rating Scale, GDS: Geriatric Depression Scale, K-MMSE: Korean version of the Mini-Mental State Examination, SOB: sum of box.
Overall cognitive assessment
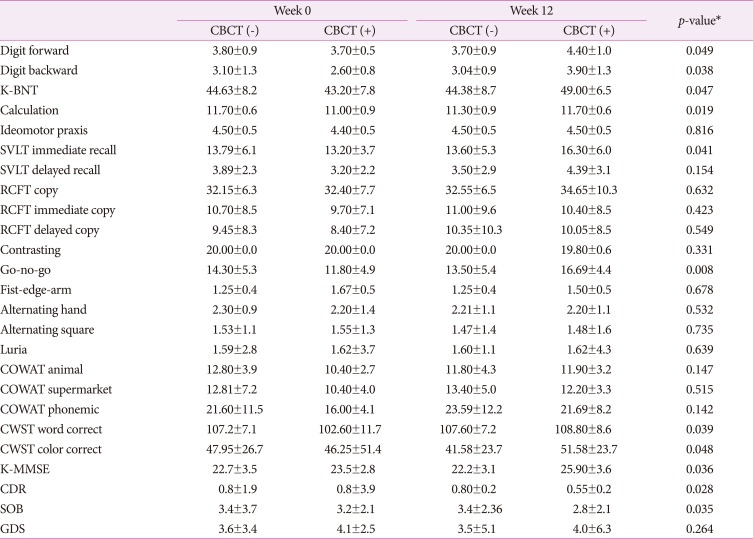
The K-MMSE score showed a significant improvement in the computer-based cognitive program group (25.90±3.6) when compared to the basic test group (23.5±2.8) (p=0.036). The CDR scores of the computer-based cognitive program group were significantly lowered to 0.55±0.2, compared with 0.8±3.9 of the basic test (p=0.028). Neuropsychological tests also showed significant improvements in various areas, when compared to control groups. The ‘digit forward span’ was 3.70±0.5 and 4.40±1.0, respectively, for before and after performance. In addition, the ‘digit backward span’ was 2.60±0.8 and 3.90±1.3, respectively, for before and after performance. In the ‘go-no-go’ test, the experiment group showed good results of 11.80±4.9 and 16.69±4.4, respectively, for before and after performance. The K-BNT was 43.20±7.8 and 49.00±6.5, respectively, for before and after performance, and showed significant improvement compared to the control group. The results of the experimental group for the stroop test showed improved results in both word and color. These changes were also observed in the computational area, with an overall score increase of 11.00±0.9 to 11.70±0.6. The memory tended to be improved for overall score in immediate recall of the language domain. However, visual memory was not different from the control group (Table 2). Comprehensively, there was significant improvement in language ability, verbal memory, attention and concentration, and in the frontal lobe function test of the experimental group compared to the control group.
Table 2. Comparison of neuropsychological tests between CBCT (−) patients and CBCT (+) patients, at baseline and 12 weeks follow up.
*Repeated measures of general linear model were used.
CBCT: computer-based cognitive training, CDR: Clinical Dementia Rating Scale, COWAT: Controlled Oral Word Association Test, CWST: Korean-Color Word Stroop Test, GDS: Geriatric Depression Scale, K-BNT: Korean version of the Boston Naming Test, K-MMSE: Korean version of the Mini-Mental State Examination, RCFT: Rey Complex Figure Test, SOB: sum of box, SVLT: Seoul Verbal Learning Test.
DISCUSSION
This study showed that the cognitive training program using the systematic computer resulted in an improvement of cognitive functions in various areas. It is expected that computer-based cognitive treatment will be more actively used in the area of cognitive rehabilitation since it has several advantages over conventional treatment. Compared to traditional cognitive training which is performed in groups, the advantage of computer-based cognitive treatment is that the self-training and self-learning of a patient can shorten the intervention time of the therapist, and feedback of results to the patient is immediate, thus motivating the patient to continue treatment as well as obtain objective and accurate results. Through this study, we found that computer-based cognitive programs help in improving the overall cognition, especially in language skills, verbal memory, attention, and frontal lobe function tests. Compared to the control group, computer-based cognitive program significantly affected multiple cognitive functions. It can be considered that this program is effective for the general brain function via active visual stimu-lation. In particular, memory and calculation ability are least used due to the development of digital machines, which are easy to use for daily purposes. These results will prove useful and have a good effect on the patients in the future. To date, memory training programs have been studied as rehabilitation methods that delay the deterioration of cognitive impairment. However, the effect of these methods is still unclear. In addition, it is expected that the use of computer-based attention training in patients will increase the range of cognitive treatment using computer-based treatment in areas other than brain injury. The reduced memory in the elderly is the main reason of decreased working memory due to attention disorder. Therefore, it is expected that the comprehensive cognitive program designed in this study will be effective in improving cognition. The limitation of this study is that the number of patients was not enough to generalize for all early stage of Alzheimer's patients. To confirm the timing of the good effects of the computer-based cognitive program, it is necessary to review the program shortly after its implementation, at 6 months, and after 1 year or more. However, it is necessary to carry out a follow-up study, since our study only evaluated the short-term effect. In this study, we used and systematically evaluated the effects of a computer-based cognitive training program. The results suggest the possibility of expecting good outcomes on the effectiveness of the cognitive training program other each type of dementia and various clinical dementia stages, using various methods in the future. The results of this study also indicate that in the basic test, there was no statistically significant difference in cognitive function before treatment, between the control group and the experimental group for each test item. However, the language ability, verbal memory, concentration, and the frontal lobe related functions were improved, thus confirming that the cognitive training program was effective in patients with impaired cognitive function. In current study, cognitive training program has significant effects in case of mid Alzheimer's dementia. It will therefore be necessary, in future, to develop the various cognitive training programs to cover the various other type and stage of dementia.
Footnotes
Conflicts of Interest: The authors have no financial conflicts of interest.
References
- 1.Wimo A, Jönsson L, Bond J, Prince M, Winblad B Alzheimer Disease International. The worldwide economic impact of dementia 2010. Alzheimers Dement. 2013;9:1–11.e3. doi: 10.1016/j.jalz.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Muayqil T, Camicioli R. Systematic review and meta-analysis of combination therapy with cholinesterase inhibitors and memantine in Alzheimer's disease and other dementias. Dement Geriatr Cogn Dis Extra. 2012;2:546–572. doi: 10.1159/000343479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Royall DR, Lauterbach EC, Kaufer D, Malloy P, Coburn KL, Black KJ Committee on Research of the American Neuropsychiatric Association. The cognitive correlates of functional status: a review from the Committee on Research of the American Neuropsychiatric Association. J Neuropsychiatry Clin Neurosci. 2007;19:249–265. doi: 10.1176/jnp.2007.19.3.249. [DOI] [PubMed] [Google Scholar]
- 4.Yamaguchi H, Maki Y, Yamagami T. Overview of non-pharmacological intervention for dementia and principles of brain-activating rehabilitation. Psychogeriatrics. 2010;10:206–213. doi: 10.1111/j.1479-8301.2010.00323.x. [DOI] [PubMed] [Google Scholar]
- 5.Clare L, Wilson BA, Carter G, Roth I, Hodges JR. Awareness in early-stage Alzheimer's disease: relationship to outcome of cognitive rehabilitation. J Clin Exp Neuropsychol. 2004;26:215–226. doi: 10.1076/jcen.26.2.215.28088. [DOI] [PubMed] [Google Scholar]
- 6.Woolf CJ, Salter MW. Neuronal plasticity: increasing the gain in pain. Science. 2000;288:1765–1769. doi: 10.1126/science.288.5472.1765. [DOI] [PubMed] [Google Scholar]
- 7.Yu F, Rose KM, Burgener SC, Cunningham C, Buettner LL, Beattie E, et al. Cognitive training for early-stage Alzheimer's disease and dementia. J Gerontol Nurs. 2009;35:23–29. doi: 10.3928/00989134-20090301-10. [DOI] [PubMed] [Google Scholar]
- 8.Zhuang JP, Fang R, Feng X, Xu XH, Liu LH, Bai QK, et al. The impact of human-computer interaction-based comprehensive training on the cognitive functions of cognitive impairment elderly individuals in a nursing home. J Alzheimers Dis. 2013;36:245–251. doi: 10.3233/JAD-130158. [DOI] [PubMed] [Google Scholar]
- 9.Glisky EL, Schacter DL. Long-term retention of computer learning by patients with memory disorders. Neuropsychologia. 1988;26:173–178. doi: 10.1016/0028-3932(88)90041-3. [DOI] [PubMed] [Google Scholar]
- 10.Palmese CA, Raskin SA. The rehabilitation of attention in individuals with mild traumatic brain injury, using the APT-II programme. Brain Inj. 2000;14:535–548. doi: 10.1080/026990500120448. [DOI] [PubMed] [Google Scholar]
- 11.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 12.Kang YW. A normative study of the Korean-Mini Mental State Examination (K-MMSE) in the elderly. Korean J Psychol. 2006;25:1–12. [Google Scholar]
- 13.Morris JC. Clinical dementia rating: a reliable and valid diagnostic and staging measure for dementia of the Alzheimer type. Int Psychogeriatr. 1997;9(Suppl 1):173–176. doi: 10.1017/s1041610297004870. discussion 177-178. [DOI] [PubMed] [Google Scholar]
- 14.Kang YW, Na DL. Seoul neuropsychological screening battery (SNSB) Incheon: Human Brain Research & Consulting Co.; 2003. [Google Scholar]
- 15.Kim H, Na DL. Normative data on the Korean version of the Boston Naming Test. J Clin Exp Neuropsychol. 1999;21:127–133. doi: 10.1076/jcen.21.1.127.942. [DOI] [PubMed] [Google Scholar]
- 16.Meyers JE, Meyers KR. Rey complex figure test and recognition trial: professional manual. Odessa: Psychological Assessment Resources Inc.; 1995. [Google Scholar]
- 17.Kang YW, Chin JH, Na DL, Lee JH, Park JS. A normative study of the Korean version of Controlled Oral Word Association Test (COWAT) in the elderly. Korean J Clin Psychol. 2000;19:385–392. [Google Scholar]
- 18.Lee JH, Kang YW, Na DL. Efficiencies of stroop interference indexes in healthy older adults and dementia patients. Korean J Clin Psychol. 2000;19:807–818. [Google Scholar]