Abstract
Background and Purpose
Acetyl-L-carnitine (ALC) is a widely used drug for various neurodegenerative diseases including dementia. The aim of the present study was to elucidate the efficacy of ALC in dementia patients with cerebrovascular disease (vascular cognitive impairment; VCI).
Methods
Fifty-six patients were randomized to treatment with 500 mg ter in die ALC, or placebo in this 28-week, double-blind, placebo-controlled trial. The primary outcome measure was the Korean version of Montreal Cognitive Assessment (MoCA-K).
Results
Following treatment with ALC, the cognitive function measured by the MoCA-K was significantly improved in the ALC-treated groups. However, other secondary outcomes were not statistically significant between ALC- and placebo-treated groups. In MoCA-K analysis, attention and language sub-items significantly favored the ALC-treated group.
Conclusions
Compared with placebo, treatment with ALC 1,500 mg/day produced significant changes in MoCA-K in dementia patients with VCI. ALC was well tolerated in this population. Despite the study limitations, the findings suggested the potential benefits associated with the use of ALC in dementia patients with VCI.
Keywords: Acetyl-L-carnitine, Dementia, Efficacy, Vascular Cognitive Impairment, MoCA-K
INTRODUCTION
Vascular cognitive impairment (VCI) includes the entire spectrum of vascular brain pathologies that contribute to cognitive dysfunction, ranging from subjective cognitive decline to dementia.1,2 Patients with VCI manifest mental slowness and problems with executive function such as planning, organizing, monitoring and feedback behavior. Memory problems, behavioral and psychological symptoms, including apathy, anxiety and depression, are also commonly observed. Neurological signs and symptoms such as reflex asymmetry, dysarthria (difficulty with speech), Parkinsonism, rigidity or urinary incontinence, often occur. However, individual signs or symptoms of the disease depend on the type, extent and location of the underlying cerebrovascular pathology.
Both in autopsy and clinical studies, pure vascular dementia (that is, dementia due solely to cerebrovascular disease) is not common.3 Indeed, vascular pathology alone without other causes probably accounts for only ≤10% of dementia cases.4 Further, up to 75% of patients with dementia show evidence of vascular pathology at autopsy,5 and accordingly, mixed dementia (also known as dementia due to mixed pathology) is common, particularly in the elderly population. In addition to simple co-existence, Alzheimer's disease and VCI are closely associated. First, they share several vascular risk factors (e.g., cerebrovascular disease, and arterial hypertension) and vascular pathology in the brain (e.g., lacunae, and white-matter lesions), which relate to the clinical manifestations of dementia.6 Furthermore, they share common pathogenic mechanisms such as neurotransmitter abnormalities.7
The major pathologies in VCI are focal, multifocal or diffuse white matter ischemic lesions involving various brain regions, with deafferentation of frontal and limbic cortical structures and interruption of basal ganglia, thalamus, white matter and other sub-frontal areas.4,8 Cholinergic dysfunction, which is similar to that observed in patients with AD occurs due to a dense network of cholinergic fibers in the injured area. Interestingly, cholinergic agents, such as acetylcholinesterase (AChE) inhibitors, have shown considerable benefits in patients with vascular dementia.9 Accumulating evidence derived from experimental cerebral ischemia models shows that in addition to cholinergic deficiency, post-ischemic inflammation in response to ischemic injury contributes to delayed brain damage.10
Acetyl-L-carnitine (ALC) is an endogenous substance derived from carnitine, which is involved in the synthesis of natural products of the cell by facilitating trans-acetylation. It also shuttles long chain fatty acids between the cytoplasm and mitochondria. In cells and tissues, carnitine occurs as free carnitine and as acyl-derivatives. Carnitine acyl-transferases are the enzymes responsible for synthesis of ALC.11 ALC is a known agonist of mitochondrial function, a neuronal growth factor with an antioxidant effect on the central nervous neurons. Although the effect of ALC on cholinergic neurotransmission has not been clearly documented, both postsynaptic12 and presynaptic13 mechanism is proposed. In addition, it may facilitate membrane stabilization, by increasing the adenosine levels. Furthermore, a recent review suggested that ALC and its derivatives improve tolerance to ischemia and reperfusion injury in various tissues.14
In human studies, ALC has multiple neurobiological effects, with possible benefits in degenerative brain disease. Although ALC it is not routinely used, it has been found to be safe in dementia patients with few adverse effects.15 Clinical studies have been performed in conjunction with the dementia treatment since the 1980s. These studies investigated the ALC role in cognitive and behavioral effects of elderly subjects. Early series of several small, uncontrolled and often unpublished studies suggested possible clinical efficacy of ALC in ameliorating the cognitive decline in subjects with cognitive impairment. However, reviews of these studies are less conclusive.16 Furthermore, no reliable data are available for ALC efficacy in VCI. ALC affects neuronal cells via diverse mechanisms including cholinergic system augmentation, and therefore, we elucidated the ALC efficacy in VCI using a double-blind randomized control study in patients with VCI.
METHODS
Study design
This trial was a 28-week, multicenter, randomized, double-blind, placebo-controlled, parallel-group study involving dementia patients with cerebrovascular disease. It included 4 hospitals. An initial screening visit was performed within 14 days of the baseline visit. At baseline, eligible patients were randomly allocated in a 50/50 split using a computerized randomization schedule to 28 weeks of ter in die (t.i.d) doses of either placebo or ALC (Carnitil®; Hanmi Pharmaceutical Co., Ltd., Seoul, Korea). Blinding was achieved by the use of identical-appearing ALC (Carnitil®) and placebo tablets. The 500 mg t.i.d ALC (Carnitil®) or placebo was constant during study period. Clinical visits occurred at screening, at baseline, and at weeks 4, 8, 12, 16, 20, 24, and 28. During these visits, physical and neurological examinations, laboratory analyses, vital sign measurements, medication compliance checks, and adverse event (AE) monitoring was performed. In the absence of computed tomography (CT) or magnetic resonance imaging (MRI) scans within the last 12 months, they were carried out at screening.
Before screening, written informed consent was obtained from both patients and their responsible caregivers. If the patient was not capable of providing informed consent, written consent was obtained from the patient's representative and assent was received from the patient. Caregivers participated as collateral informants. They were required to accompany the patient on each visit and assist the assessments during clinic visits. This study was approved by the Institutional Review Board (IRB) of Veteran Health Service Medical Center (IRB No. 2016-05-022) and met standards established by the Declaration of Helsinki.17
Patients
Patients were eligible for this trial only after they had met the following conditions: 1) age of 55 to 80 years; 2) ischemic brain lesion confirmed by CT or MRI within 12 months; 3) dementia confirmed by criteria of Diagnostic and Statistical Manual of Mental Disorders, 4th Edition; 4) a score of 12 to 26 on the Korean Mini-Mental State Examination (K-MMSE); and 5) current donepezil medication. Patients were excluded if 1) they had a diagnosis of Parkinson's disease, Huntington's disease, subdural hematoma, normal pressure hydrocephalus, cerebral encephalitis due to infectious disease, or toxic-metabolic encephalitis; 2) patients with no education and illiteracy; 3) treatment with other dementia medications except donepezil within 3 months; 4) exposure to nootropics and thyroid hormones within 3 months; 5) treatment with stimulants, antipsychotics, and anticholinergics within 3 months; 6) hematological abnormalities in baseline screening; 7) depressive illness, schizophrenia, alcohol and drug addiction during baseline screening; 8) unstable angina, myocardial infarction, and transient ischemic attack within 3 months; 9) history of cerebral trauma within 3 months; and 10) treatment with other clinical trial drugs within 3 months.
Efficacy assessment
The primary efficacy measures included changes from baseline to endpoint (week 28) in scores of the Korean version of Montreal Cognitive Assessment (MoCA-K). The MoCA-K consists of 12 individual cognitive tasks grouped into 7 subtests: visuo-executive, naming, attention, language, abstraction, delayed recall, and orientation, with a maximum total score of 30.18 Examiners scored the MoCA-K at baseline, visit 5 (12 week), and visit 8 (28 weeks or endpoint). Secondary outcomes were: the K-MMSE, Korean-Color Word Stroop Test (K-CWST), Controlled Oral Word Association Test (COWAT), Korean-Trail Making Test-Elderly's Version (K-TMT-E), Korean Instrumental Activity of Daily Living (K-IADL), Geriatric Depression Scale (GDS), Clinical Dementia Rating Scale (CDR), Clinical Dementia Rating Scale Sum of Boxes (CDR-SB), and measured at baseline, 12 weeks, and 28 weeks (or endpoint).
Safety assessment
The tolerability and safety of the study medication were continuously monitored from baseline to endpoint in terms of study discontinuations and by comparing the treatment groups with respect to rates of AE, changes in laboratory test values, changes in vital signs, electrocardiogram abnormalities, and treatment-emergent physical findings. Any AE that was life-threatening or resulted in death, hospitalization, prolonged hospitalization, or significant disability was coded as serious AE.
Statistical analysis
Based on treatment effect size reported in a previous carnitine study in Alzheimer's disease,19 a sample size of 59 patients in each treatment arm (118 in total) yielded an estimated effect size of 0.05 with 80% power to detect a 3.74 mean difference in MMSE. In the absence of a previous MoCA-K report in ALC, MMSE was adopted for sample size estimation. However, due to inclusion difficulty, a total of 56 patients were recruited in this study (ALC 30 vs. placebo 26). The primary efficacy was analyzed based on the change from baseline score on the MoCA-K at week 28 in the intent-to-treat population. If there were missing values, last-observation-carried-forward analysis was adopted. The intent-to-treat population included all patients who were treated with at least one dose of study medication and provided both a baseline assessment and at least one post-baseline efficacy result. Secondary analyses were carried out using an observed case analysis at each visit. Efficacy variables at baseline were summarized using analysis-of-variance models (2-way repeated measure) with effects for treatment and baseline, and were used to assess treatment differences at each post-baseline visit. All continuous variables with baseline assessment were analyzed at each time point and at week 28 last observation carried forward. All statistical tests were 2-sided, and p values of 0.05 were considered significant. The χ2 test was used for categorical variables.
RESULTS
Demographic characteristics
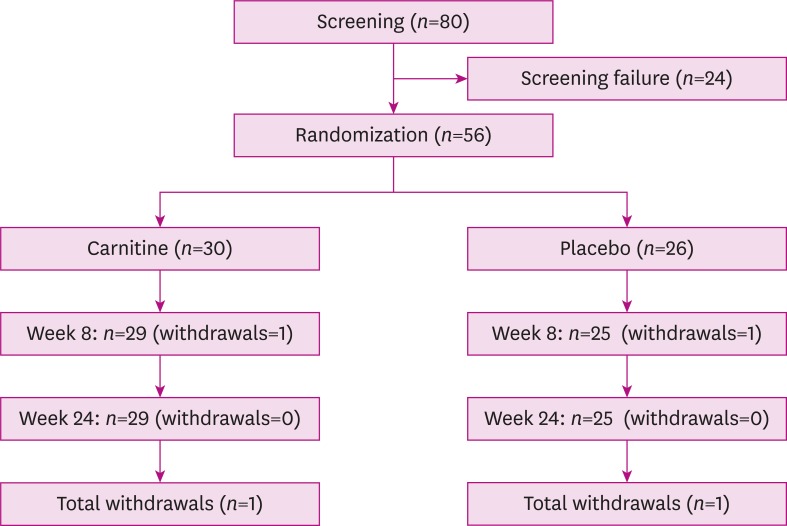
Among the 80 patients screened, 56 were included in the study and randomized to receive ALC 1,500 mg/day (n=30) and placebo (n=26). Reasons for screening failure included inability to meet entry criteria (K-MMSE score below 12 or above 26, n=13), withdrawal of consent (n=5), and unstable medical conditions (n=6) (Fig. 1). All patients showed evidence of cerebrovascular disease. The significant portion of the patients were diagnosed with hypertension (carnitine 46.7%, placebo 38.5%), and many carried a history of diabetes mellitus and hypercholesterolemia (Table 1). The prevalence of these conditions was similar between the two groups. The study groups were similar at baseline with respect to demographics and psychometric test scores (Table 1). The overall study completion rate was 96.4% (2 subjects dropped out from each study group), and the study groups showed only small differences in completion rate (carnitine 96.7%, placebo 96.1%). Reasons for discontinuation were protocol violation (1 patient) and changed medical condition (1 patient).
Fig. 1.
Flow diagram outlining the study design: patient screening, randomization, and timing of assessment.
Table 1. Patient demographics and baseline characteristics.
| Characteristics | ALC | Placebo | p-value* | |
|---|---|---|---|---|
| Numbers | 30 | 26 | ||
| Sex | NS | |||
| Male | 25 | 22 | ||
| Female | 5 | 4 | ||
| Age (yr) | 73.0±3.8 | 73.2±4.0 | NS | |
| Onset age (yr) | 2.4±1.1 | 2.5±1.3 | NS | |
| Education | 7.8±2.4 | 6.9±2.7 | NS | |
| Medical history | ||||
| Hypertension | 14 (46.7%) | 10 (38.5%) | NS | |
| Diabetes mellitus | 10 (33.3%) | 5 (19.2%) | NS | |
| Hyperlipidemia | 7 (23.3%) | 4 (15.4%) | NS | |
| MoCA-K | 17.2±4.1 | 16.8±3.8 | NS | |
| K-MMSE | 21.5±2.6 | 21.1±2.4 | NS | |
| CDR | 0.98±0.25 | 0.96±0.14 | NS | |
| CDR-SB | 4.85±1.5 | 4.68±1.1 | NS | |
| GDS | 12.9±5.4 | 13.7±5.1 | NS | |
| K-IADL | 11.4±6.3 | 13.2±6.9 | NS | |
ALC: Acetyl-L-carnitine, NS: not significant, MoCA-K: Korean version of Montreal Cognitive Assessment, K-MMSE: Korean Mini-Mental State Examination, CDR: Clinical Dementia Rating Scale, CDR-SB: Clinical Dementia Rating Scale Sum of Boxes, GDS: Geriatric Depression Scale, K-IADL: Korean Instrumental Activity of Daily Living.
*Independent t-test, χ2 test was done.
Primary outcome measure
Treatment effects on MoCA-K showed significant differences in favor of ALC-treated group, compared with placebo at endpoint (Table 2). Among MoCA-K sub-items, attention, language sub-items showed significant treatment differences in the ALC-treated group compared with placebo-treated group (Table 3).
Table 2. Changes in outcome measures after ALC treatment.
| Measure | Baseline | 12 weeks | 28 weeks | p-value | |
|---|---|---|---|---|---|
| MoCA-K | 0.010* | ||||
| ALC | 17.3±4.1 | 17.2±4.0 | 17.6±4.2 | ||
| Placebo | 16.7±3.8 | 16.3±3.1 | 15.9±3.8 | ||
| K-MMSE | 0.819 | ||||
| ALC | 21.5±2.7 | 21.6±3.5 | 21.6±3.6 | ||
| Placebo | 21.1±2.4 | 21.1±2.7 | 21.1±2.9 | ||
| CWST word correct | 0.732 | ||||
| ALC | 107.9±15.5 | 108.1±14.0 | 109.6±12.4 | ||
| Placebo | 100.7±15.5 | 100.9±27.6 | 100.7±28.0 | ||
| CWST color correct | 0.850 | ||||
| ALC | 97.5±33.6 | 97.9±32.0 | 97.9±32.3 | ||
| Placebo | 94.1±35.4 | 93.2±34.7 | 94.1±32.3 | ||
| CWST word incorrect | 0.753 | ||||
| ALC | 3.3±10.0 | 3.9±9.9 | 3.4±11.4 | ||
| Placebo | 12.7±16.8 | 12.3±20.4 | 11.7±28.0 | ||
| CWST color incorrect | 0.302 | ||||
| ALC | 13.1±25.5 | 12.3±20.9 | 14.1±21.4 | ||
| Placebo | 20.4±26.8 | 20.6±25.4 | 19.6±28.0 | ||
| COWAT | 0.403 | ||||
| ALC | 34.5±13.0 | 35.5±15.1 | 37.6±15.3 | ||
| Placebo | 31.4±10.0 | 34.6±14.0 | 33.8±15.3 | ||
| CDR-SB | 0.029† | ||||
| ALC | 4.7±1.2 | 4.6±1.1 | 4.2±1.3 | ||
| Placebo | 4.7±1.2 | 4.5±0.9 | 4.4±1.2 | ||
| GDS | 0.973 | ||||
| ALC | 12.8±5.4 | 13.9±5.1 | 13.6±5.1 | ||
| Placebo | 13.8±5.1 | 14.7±5.7 | 14.5±5.2 | ||
| K-IADL | 0.003† | ||||
| ALC | 10.7±5.1 | 10.6±10.2 | 9.7±9.6 | ||
| Placebo | 13.5±6.9 | 9.6±7.0 | 9.3±10.1 | ||
Two-way repeated measure of analysis of variance test was done.
ALC: Acetyl-L-carnitine, MoCA-K: Korean version of Montreal Cognitive Assessment, K-MMSE: Korean Mini-Mental State Examination, K-CWST: Korean-Color Word Stroop Test, COWAT: Controlled Oral Word Association Test, CDR: Clinical Dementia Rating Scale, CDR-SB: Clinical Dementia Rating Scale Sum of Boxes, GDS: Geriatric Depression Scale, K-IADL: Korean Instrumental Activity of Daily Living.
*Statistical difference was found between ALC- and placebo-treated groups according clinical trial follow -up; †Statistical difference was found according to clinical trial follow-up, but statistically significant group difference was not found.
Table 3. Changes in MoCA-K sub-items after treatment in study subjects.
| Measure | 0 week | 12 weeks | 28 weeks | p-value | |
|---|---|---|---|---|---|
| Visuospatial | 0.565 | ||||
| ALC | 2.8±1.4 | 2.9±1.4 | 3.0±1.3 | ||
| Placebo | 2.3±1.4 | 2.4±1.3 | 2.4±1.3 | ||
| Naming | 0.310 | ||||
| ALC | 2.5±0.7 | 2.5±0.8 | 2.5±0.8 | ||
| Placebo | 2.4±1.0 | 2.2±1.1 | 2.3±1.1 | ||
| Attention* | 0.025 | ||||
| ALC | 3.7±1.4 | 3.7±1.1 | 3.5±1.5 | ||
| Placebo | 4.1±1.7 | 3.5±1.3 | 3.3±1.3 | ||
| Language* | 0.012 | ||||
| ALC | 1.4±0.9 | 1.5±1.0 | 1.9±0.8 | ||
| Placebo | 1.3±0.8 | 1.8±1.0 | 1.5±0.7 | ||
| Abstract | 0.443 | ||||
| ALC | 0.8±0.6 | 0.9±0.8 | 0.9±0.6 | ||
| Placebo | 0.8±0.7 | 0.8±0.7 | 1.1±0.6 | ||
| Delayed recall | 0.100 | ||||
| ALC | 0.9±0.9 | 1.1±0.7 | 1.3±0.8 | ||
| Placebo | 1.2±1.0 | 1.2±0.9 | 1.2±0.9 | ||
| Orientation† | 0.000 | ||||
| ALC | 4.7±1.4 | 4.2±1.5 | 4.1±1.3 | ||
| Placebo | 4.3±1.3 | 4.0±1.4 | 3.8±1.3 | ||
MoCA-K: Korean version of Montreal Cognitive Assessment, ALC: Acetyl-L-carnitine.
*Statistically significant difference was found between ALC- and placebo-treated groups according to clinical trial follow-up; †Statistically significant difference was found according to clinical trial follow-up, but statistically significant group difference was not found.
Secondary outcome measure
Cognitive assessment tools such as K-MMSE, K-CWST, COWAT, K-TMT-E, and GDS, K-IADL showed no significant differences between ALC- and placebo-treated groups (Tables 2 and 4). Global cognitive impression scales such as CDR, and CDR-SB also showed non-significant changes between ALC- and placebo-treated groups (Table 2). CDR-SB and K-IADL showed significant changes according to clinical trial courses regardless of treatment groups (Table 2).
Table 4. K-TMT-E status according to follow-up.
| Measure | Baseline | Week 12 | Week 28 | p-value* | |
|---|---|---|---|---|---|
| ALC | 0.117 | ||||
| Success | 30 | 29 | 29 | ||
| Fail | 0 | 0 | 0 | ||
| Placebo | |||||
| Success | 24 | 23 | 23 | ||
| Fail | 2 | 2 | 2 | ||
K-TMT-E: Korean-Trail Making Test-Elderly's Version, ALC: Acetyl-L-carnitine.
*χ2 test was done.
AEs
The proportion of patients with AE was 13.3% in ALC-treated group, and 7.7% in placebo-treated group respectively (Table 5). One patient in the ALC-treated group died during the study and this death was considered to be unrelated to the study medication. Other symptoms also were considered not related to ALC, and these symptoms disappeared without dosage controls.
Table 5. AEs during follow-up.
| AEs | ALC (n=30) | Placebo (n=26) | |
|---|---|---|---|
| Any AE | 4 (13.3%) | 2 (7.7%) | |
| Dizziness | 0 | 1 | |
| Cardiac arrest | 1 | 0 | |
| Pyelonephritis | 1 | 0 | |
| Fatty liver | 1 | 0 | |
| Aggravation headache | 1 | 0 | |
| Dyspesia | 0 | 1 | |
AE: adverse event, ALC: Acetyl-L-carnitine.
*Pearson correlation; 0.967 (p<0.001) between 1st and 2nd test.
DISCUSSION
Several studies have reported that ALC treatment enhanced cognitive function or reduced the rate of cognitive deterioration in patients with Alzheimer's disease/mild cognitive impairment,20 Parkinson's disease,21 and hepatic encephalopathy.22 However, other good-quality trials or meta-analyses showed conflicting results regarding the efficacy of ALC in Alzheimer's disease and mild cognitive impairment. Furthermore, a reliable clinical trial investigating VCI has yet to be reported. ALC affected the pathophysiology of cholinergic dysfunction in VCI, suggesting that it may be a possible candidate for treatment of VCI. To elucidate this hypothesis, we evaluated carnitine levels in patients diagnosed with dementia and VCI, and already treated with donepezil.
In our study, dementia patients treated with ALC 1,500 mg demonstrated significant benefits compared with placebo-treated patients in terms of MoCA-K. The population studied here included dementia subjects with evidence of cerebrovascular disease, and a high prevalence of hypertension. CDR-SB and K-IADL significantly declined during the course of study trials, although group differences (ALC vs. placebo) were not significant. Other secondary measures (K-CWST, COWAT, K-TMT-E, GDS) showed no significant differences. In contrast to their relative stability in ALC-treated group, patients with placebo treated group may show functional decline in MoCA-K. The progression of placebo-treated group and the lack of deterioration in the ALC-treated group on MoCA-K may demonstrate carnitine-placebo differences. These findings suggested that significant treatment-related differences are driven by reduced rate of decline, and may not simply reflect actual improvement in the ALC-treated group. Interestingly, compared with MoCA-K, the K-MMSE has been widely used as a global cognitive function scale, and showed no significant differences between ALC- and placebo-treated groups (Table 1). The discrepancy may be attributed to differences in scale. MoCA usually cover frontal lobe function than MMSE.23 Patients with VCI usually manifest more frontal lobe dysfunction than temporo-parietal lobe dysfunction, and therefore, subtle clinical changes undetected in MMSE are reflected in MoCA-K. These findings suggested that an appropriate choice of primary outcome measures is important in clinical trials.
To elucidate the ALC response-specific cognitive function, the treatment-related changes in MoCA-K sub-items were analyzed. Among sub-items of MoCA-K, attention and language sub-items showed significant differences between ALC- and placebo-treated group. These findings suggested a significant effect of clinical trial time course and ALC treatment. Orientation showed significant difference according to time factor, but not group factors suggesting that orientation significantly deteriorated according to the course of clinical trials regardless of ALC treatment.
Compared with the relentlessly progressive natural clinical course of Alzheimer's disease, pure vascular dementia generally showed slight or no progression during the short-term follow up period.24 Although we recruited dementia patients with cerebrovascular evidence, who were already treated with donepezil, we cannot definitively conclude that study subjects included pure vascular dementia. Considering deterioration in CDR-SB and K-IADL data during the clinical trial, a considerable proportion of study subjects might include patients with Alzheimer's pathology.
The safety population consisted of all patients who received at least one dose of study medication. Regardless of suspected causal relationship with the study drug, all observed AE were reported (Table 5) including 13.3% of patients exposed to ALC (n=4) and 7.7% of those receiving placebo (n=2) who experienced at least one AE during the course of the trial. One of the ALC-treated patients died of cardiac arrest. Another ALC-treated patient experienced pyelonephritis, however, the patient completed clinical trials without ALC dosage adjustment. One patient treated with placebo dropped out due to changing mind. Detailed safety analysis concluded that all the AE were unrelated to ALC. These AEs were illnesses during the study or exacerbations of pre-existing illnesses, and resulted in no ALC dosage change during study periods.
Although benefits of MoCA-K occurred with ALC in this trial, significant benefits were not detected in terms of other outcome measures. Consequently, the primary objective of the study demonstrating a significant treatment effect on endpoints was not fully met. Several probable factors explain these conflicting results. First, as already reported, a few patients with Alzheimer's pathology may be included. All patients were treated with donepezil before study, and this continued during the study periods. Although the effects of ALC on dementia patients may be disputed, cholinergic augmentation may be the major mechanism underlying amelioration of dementia symptoms. However, our study patients were already treated with donepezil, suggesting that additional cholinergic support might have limited effects. In this environment, additional cholinergic effects of carnitine may be limited. Second, due to the recruiting center characteristics, male patients outnumbered female patients. These sex differences from previous studies may result in different clinical outcomes. For example, female patients with AD showed an improved response to treatment with AChE inhibitors.25 Finally, the sample size was less than aimed for due to recruitment difficulties, so our data must be interpreted with caution.
In summary, this randomized, double-blind, placebo-controlled trial demonstrated that, compared with placebo, treatment with ALC 1,500 mg/day produced significant changes in MoCA-K in dementia patients with VCI. ALC was also well tolerated in this population. Despite the limitations of study design, and sample size, this study suggested the potential benefits associated with the use of ALC in dementia patients with VCI. To further confirm these results, a large-sized study design with cholinergic drug-naïve patients is recommended.
Footnotes
Funding: This study was supported by research grants from Hanmi Pharmaceutical Co., Ltd.
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Yang Y.
- Data curation: Yang Y.
- Formal analysis: Kwak YT.
- Funding acquisition: Yang Y.
- Investigation: Yang Y, Choi H, Lee CN, Kim YB.
- Methodology: Yang Y, Choi H, Lee CN, Kim YB.
- Project administration: Yang Y, Choi H, Lee CN, Kim YB.
- Resources: Yang Y.
- Software: Kwak YT.
- Supervision: Yang Y, Kwak YT.
- Validation: Kwak YT.
- Visualization: Yang Y, Kwak YT.
- Writing - original draft: Yang Y, Kwak YT.
- Writing - review & editing: Yang Y, Kwak YT.
References
- 1.O'Brien JT, Erkinjuntti T, Reisberg B, Roman G, Sawada T, Pantoni L, et al. Vascular cognitive impairment. Lancet Neurol. 2003;2:89–98. doi: 10.1016/s1474-4422(03)00305-3. [DOI] [PubMed] [Google Scholar]
- 2.Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2672–2713. doi: 10.1161/STR.0b013e3182299496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barker WW, Luis CA, Kashuba A, Luis M, Harwood DG, Loewenstein D, et al. Relative frequencies of Alzheimer disease, Lewy body, vascular and frontotemporal dementia, and hippocampal sclerosis in the State of Florida Brain Bank. Alzheimer Dis Assoc Disord. 2002;16:203–212. doi: 10.1097/00002093-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Schneider JA, Arvanitakis Z, Bang W, Bennett DA. Mixed brain pathologies account for most dementia cases in community-dwelling older persons. Neurology. 2007;69:2197–2204. doi: 10.1212/01.wnl.0000271090.28148.24. [DOI] [PubMed] [Google Scholar]
- 5.Neuropathology Group of the Medical Research Council Cognitive Function and Ageing Study(MRC CFAS) Pathological correlates of late-onset dementia in a multicentre, community-based population in England and Wales. Lancet. 2001;357:169–175. doi: 10.1016/s0140-6736(00)03589-3. [DOI] [PubMed] [Google Scholar]
- 6.Skoog I, Kalaria RN, Breteler MM. Vascular factors and Alzheimer disease. Alzheimer Dis Assoc Disord. 1999;13(Suppl 3):S106–S114. doi: 10.1097/00002093-199912003-00016. [DOI] [PubMed] [Google Scholar]
- 7.Kalaria RN, Ballard C. Overlap between pathology of Alzheimer disease and vascular dementia. Alzheimer Dis Assoc Disord. 1999;13(Suppl 3):S115–S123. doi: 10.1097/00002093-199912003-00017. [DOI] [PubMed] [Google Scholar]
- 8.Jellinger KA. The pathology of “vascular dementia”: a critical update. J Alzheimers Dis. 2008;14:107–123. doi: 10.3233/jad-2008-14110. [DOI] [PubMed] [Google Scholar]
- 9.Kavirajan H, Schneider LS. Efficacy and adverse effects of cholinesterase inhibitors and memantine in vascular dementia: a meta-analysis of randomised controlled trials. Lancet Neurol. 2007;6:782–792. doi: 10.1016/S1474-4422(07)70195-3. [DOI] [PubMed] [Google Scholar]
- 10.Kumaran D, Udayabanu M, Kumar M, Aneja R, Katyal A. Involvement of angiotensin converting enzyme in cerebral hypoperfusion induced anterograde memory impairment and cholinergic dysfunction in rats. Neuroscience. 2008;155:626–639. doi: 10.1016/j.neuroscience.2008.06.023. [DOI] [PubMed] [Google Scholar]
- 11.Pettegrew JW, Levine J, McClure RJ. Acetyl-L-carnitine physical-chemical, metabolic, and therapeutic properties: relevance for its mode of action in Alzheimer's disease and geriatric depression. Mol Psychiatry. 2000;5:616–632. doi: 10.1038/sj.mp.4000805. [DOI] [PubMed] [Google Scholar]
- 12.Ghelardini C, Galeotti N, Bartolini A. Amitriptyline and clomipramine activate Gi-protein signaling pathway in the induction of analgesia. Naunyn Schmiedebergs Arch Pharmacol. 2002;365:1–7. doi: 10.1007/s00210-001-0496-8. [DOI] [PubMed] [Google Scholar]
- 13.Imperato A, Ramacci MT, Angelucci L. Acetyl-L-carnitine enhances acetylcholine release in the striatum and hippocampus of awake freely moving rats. Neurosci Lett. 1989;107:251–255. doi: 10.1016/0304-3940(89)90826-4. [DOI] [PubMed] [Google Scholar]
- 14.Moghaddas A, Dashti-Khavidaki S. L-carnitine and potential protective effects against ischemia-reperfusion injury in noncardiac organs: from experimental data to potential clinical applications. J Diet Suppl. 2017:1–17. doi: 10.1080/19390211.2017.1359221. [DOI] [PubMed] [Google Scholar]
- 15.Sano M, Bell K, Cote L, Dooneief G, Lawton A, Legler L, et al. Double-blind parallel design pilot study of acetyl levocarnitine in patients with Alzheimer's disease. Arch Neurol. 1992;49:1137–1141. doi: 10.1001/archneur.1992.00530350051019. [DOI] [PubMed] [Google Scholar]
- 16.Hudson S, Tabet N. Acetyl-L-carnitine for dementia. Cochrane Database Syst Rev. 2003:CD003158. doi: 10.1002/14651858.CD003158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Medical Association declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. JAMA. 1997;277:925–926. [PubMed] [Google Scholar]
- 18.Lee JY, Lee DW, Cho SJ, Na DL, Jeon HJ, Kim SK, et al. Brief screening for mild cognitive impairment in elderly outpatient clinic: validation of the Korean version of the Montreal Cognitive Assessment. J Geriatr Psychiatry Neurol. 2008;21:104–110. doi: 10.1177/0891988708316855. [DOI] [PubMed] [Google Scholar]
- 19.Onofrj M. Evaluation of efficacy of chronic administration (6 months) of acetyl-l-carnitine in patients suffering from Senile Dementia Alzheimer Type (SDAT) and Alzheimer Disease (AD) statistical report, study protocol no.: ST20032189 (DRN4-021), on file Sigma-Tau (unpublished data) Pomezia: Sigma-Tau; 1992. [Google Scholar]
- 20.Montgomery SA, Thal LJ, Amrein R. Meta-analysis of double blind randomised controlled clinical trials acetyl-lcarnitine versus placebo in the treatment of mild cognitive impairment and mild Alzheimer's disease. Int Clin Psychopharmacol. 2003;18:61–71. doi: 10.1097/00004850-200303000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Puca FM, Genco S, Specchio LM, Brancasi B, D'Ursi R, Prudenzano A, et al. Clinical pharmacodynamics of acetyl-L-carnitine in patients with Parkinson's disease. Int J Clin Pharmacol Res. 1990;10:139–143. [PubMed] [Google Scholar]
- 22.Malaguarnera M. Acetyl-L-carnitine in hepatic encephalopathy. Metab Brain Dis. 2013;28:193–199. doi: 10.1007/s11011-013-9376-4. [DOI] [PubMed] [Google Scholar]
- 23.Koski L. Validity and applications of the Montreal cognitive assessment for the assessment of vascular cognitive impairment. Cerebrovasc Dis. 2013;36:6–18. doi: 10.1159/000352051. [DOI] [PubMed] [Google Scholar]
- 24.Gill DP, Hubbard RA, Koepsell TD, Borrie MJ, Petrella RJ, Knopman DS, et al. Differences in rate of functional decline across three dementia types. Alzheimers Dement. 2013;9:S63–S71. doi: 10.1016/j.jalz.2012.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scacchi R, Gambina G, Broggio E, Corbo RM. Sex and ESR1 genotype may influence the response to treatment with donepezil and rivastigmine in patients with Alzheimer's disease. Int J Geriatr Psychiatry. 2014;29:610–615. doi: 10.1002/gps.4043. [DOI] [PubMed] [Google Scholar]