Abstract
Background and Purpose
Previously developed Korean versions of the Trail Making Test (TMT) that replaced the English in part B, has been unsuccessful in Korea. The current study identifies the type of TMT tasks from the among multiple TMT versions, which practically and accurately detects the stage of cognitive decline.
Methods
We applied five TMT versions, which include the original TMT, TMT-Korean letter (TMT-KL), TMT-Korean consonant (TMT-KC), TMT-black and white (TMT-B&W), and TMT-square and circle (TMT-S&C). A total of 168 participants were enrolled: 42 cognitively normal controls (NC), 72 patients with mild cognitive impairment (MCI), and 54 patients with Alzheimer's disease (AD). Two sets of TMT (set "A" including TMT, TMT-KL and TMT-B&W, and set "B" including TMT, TMT-KC, and TMT-S&C) were randomly administered to subjects within the contact of a fixed neuropsychological battery.
Results
The completion times of TMT-B and TMT-B&W successfully distinguished NC from MCI and AD. TMT-B&W also showed a high correlation with other neuropsychological tests, and correlated well with the original TMT. The other TMT were frequently not successfully completed, nor could they differentiate the clinical groups.
Conclusions
Among the five TMT tasks, the original TMT and the TMT-B&W appeared to be most sensitive to the degree of cognitive impairment. TMT-B&W showed a pattern consistent with the original TMT; thus, this measure may be optimal in Korean older adults, where familiarity with the English alphabet is questionable.
Keywords: Trail Making Test, frontal lobe function test, mild cognitive impairment
INTRODUCTION
Trail Making Test (TMT) is a simple method1,2 used to distinguish and identify cognitive impairment.3,4 The TMT is composed of 2 parts: part A calls for the test-taker to connect randomly distributed numbers (1–25) on a test paper in ascending order (1->2->3...), whereas part B requires the test-taker to alternate numbers and letters (1->A->2->B...). Part B requires more complex cognitive functions,5 and has proven to be sensitive to prefrontal cortical dysfunction.6,7
Previous effort to develop a Korean version of TMT (TMT-K) has not been satisfactory. In the earlier version of TMT-K, part A consisted of the same test sheet as the original TMT, while part B used numbers and Korean alphabet (가, 나, 다...), instead of English. However, even adults with normal cognition had difficulty recalling the series of Korean alphabets, resulting in poorer than expected performance.8 To improve testing in the elderly, who have lower educational level and a shorter attention span, researchers designed the Korean-Trail Making Test for the elderly (K-TMT-e).9 However, K-TMT-e was so simple that it was unable to discriminate those with mild cognitive impairment (MCI) from cognitively normal subjects.9 As a result, past efforts to develop a TMT-K by replacing the English alphabet in TMT-B with other characters was unsuccessful,10 thus leading to a decreased clinical use of the TMT. The objectives of the current study were: 1) to determine if the original TMT may be successfully used in healthy and adult patients, 2) to validate the new versions of TMT in an effort to improve test-taker performance, and 3) to administer the original and the new versions of TMT in Korean healthy elderly and patient samples, to determine which TMT best distinguishes the groups.
METHODS
Subjects
This study enrolled 168 participants, comprising of 42 cognitively normal controls (NC), 72 patients diagnosed with MCI, and 54 patients diagnosed with probably Alzheimer's disease (AD). Participants were outpatients from a health care centre of Seoul National University Bundang Hospital; they included patients who complained of memory loss and their healthy caregivers. Inclusion and exclusion criteria appear below. Age range was from 50 to 80 years. Informed consent was obtained from each patient.
Criteria for the NC group were as follows: 1) no cognitive complaints verified by any measurable information; 2) Mini-Mental State Examination (MMSE) no more than one standard below the mean for education and age;11 3) absence of significant impairment in any cognitive functions; 4) preserved activities of daily living (ADL);12,13,14 5) absence of medical history that could undermine cognitive functions;15 6) Geriatric Depression Scale of less than 17 on the 30-item scale in the past week, suggesting absence of clinically significant depression.
Criteria for MCI patients16 were as follows: 1) cognitive complaints verified by a collateral source of information; 2) objectively abnormal cognitive impairment in one or more cognitive functions; 3) preserved ADL function; 4) normal visual and auditory functions; 5) no previously diagnosed neurological or psychiatric diseases; 6) failure to meet the diagnostic criteria of dementia based on the National Institute of Neurological and Communicative Disorders and Stroke and Alzheimer's Disease and Related Disorders Association (NINCDS-ADRDA).17
In the patients category, 54 were considered to have probable AD with mild dementia severity. All AD patients met the following criteria: 1) being diagnosed as probable AD according to the NINCDS-ADRDA; 2) having mild dementia severity according to the Clinical Dementia Rating scale-Sum of Boxes (CDR-SOB) scores between 2.5 and 4.0.18,19
Material
Trail Making Test
Given the high educational standards amongst Korean seniors, it is assumed that the elderly aged over 60 have knowledge of the English alphabet. Thus, use of the original TMT with no modifications other than extended time limit,20 was deemed feasible for this study. The current study used five different forms of TMT. The paper size [216×276 mm (letter size)], directions, and the trace of stimuli, were the same as the original TMT.21 The TMT versions included:
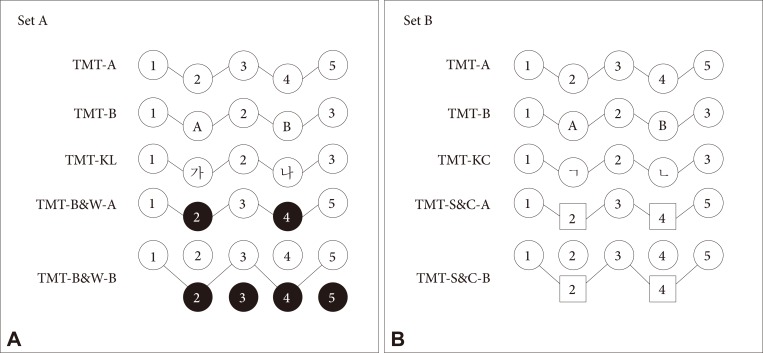
a) the original English version of the TMT;
b) the TMT-Korean letter (TMT-KL) in which English letters are replaced with "가, 나, 다";
c) the TMT-Korean consonant (TMT-KC) which utilizes "ㄱ, ㄴ, ㄷ..." in lieu of the English alphabet;
d) the TMT-black and white (TMT-B&W), which has white numbers in black circles and black numbers in white circles distributed on a test sheet, composed of part A and B. TMT-B&W part A (TMT-B&W-A) requires participants to draw a line to connect the 25 encircled numbers in ascending order, without lifting their pen or pencil from the test sheet. For the TMT-B&W part B (TMT-B&W-B), numbers from 1 to 25 are presented in white and black backgrounds. The participant is instructed to connect consecutive numbers, alternating between white and black circles [i.e., 1 (W)–2 (B)–3 (W)–4 (B)...].
e) the TMT-square and circle (TMT-S&C), which uses circles and squares. Like the original TMT-A, TMT-S&C part A (TMT-S&C-A) requires subjects to connect numbers from 1 to 25, with each even number separately embedded in a square. TMT-S&C part B (TMT-S&C-B) presents each number twice on the test sheet, one in a circle and the other in a square, except the number 1. The participant is instructed to connect consecutive numbers, alternating between circles and squares [i.e., 1 (C)–2 (S)–3 (C)–4 (S)...].
Prior to each TMT, an exercise trial was conducted to ensure the participant fully understood the task. As a validation check prior to the part B tasks involving letters, the researcher instructed the participant to write the English letters A through N in alphabetical order (original TMT), Korean letters from "가" to "하" (TMT-KL), and Korean consonants from "ㄱ" to "ㅎ" (TMT-KC).
Other instructions were same as the original TMT. A researcher started recording time as soon as the participant put the pen or pencil on the first circle, and stopped measuring time when the pencil touched the last number. Number of errors was also counted. In order to control for learning effects, the researcher did not administer every task for a subject. Instead, subjects were randomly assigned two sets of tests: set "A" included TMT, TMT-KL, TMT-B&W; set "B" was composed of TMT, TMT-KC, TMT-S&C (Fig. 1).
Fig. 1. Two Trail Making Sets. TMT: Trail Making Test, TMT-A: A form of TMT, TMT-B: B form of TMT, TMT-B&W-A: A form of black and white TMT, TMT-B&W-B: B form of black and white TMT, TMT-KC: Korean consonant version of TMT, TMT-KL: Korean letter version of TMT, TMT-S&C-A: A form of square and circle TMT, TMT-S&C-B: B form of square and circle TMT.
Other neuropsychological tests
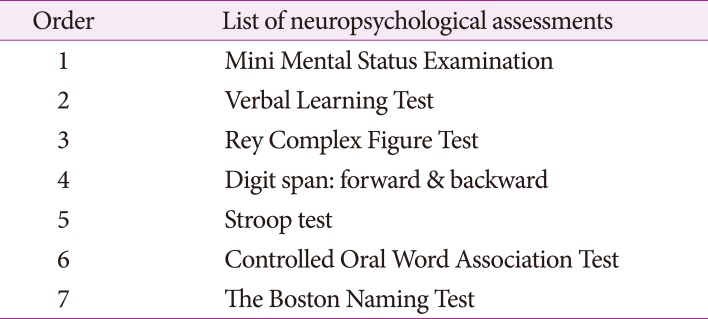
Given that the intention of the current study was to determine the feasibility of different versions of the TMT within the context of a full neuropsychological evaluation, several other standard neuropsychological assessment tools were used. These included a wide variety of cognitive functions: attention, verbal and visual memory, visuospatial ability, frontal lobe functions, and language functions (Table 1).
Table 1. Neuropsychological assessments.
Method
Prior to the test, the personal information and level of subjective cognitive impairment of all the patients was gathered through an interview, and Clinical Dementia Rating (CDR) ratings completed. Each participant was administered TMT set A or B, and subsequently given the neuropsychological battery in order to minimize any possible influence of other neuropsychological tests on TMT performance. All tests were individually administered.
Analysis
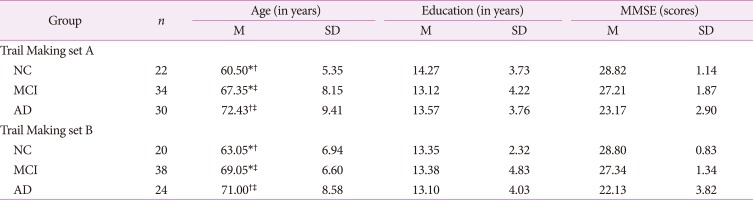
Among the 168 patients, 86 subjects completed set A, and the remaining 82 completed set B. The demographic characteristics of the participants of each set are described in Table 2.
Table 2. Demographic data for participant groups according to Trail Making sets.
Analysis of variance (ANOVA) was used to assess difference among clinical groups.
*p<0.05 for NC versus MCI, †p<0.05 for NC versus AD, ‡p<0.05 for MCI versus AD.
AD: Alzheimer's disease, M: mean, MCI: mild cognitive impairment, MMSE: Mini Mental Status Examination, n: number of participants, NC: normal controls, SD: standard deviation.
Analysis of variance was used to assess differences in age, education level, and the results on MMSE among the subject groups. Analysis of covariance test was used to determine the presence of any group differences in TMT time-to-completion, with age as a covariate. To ensure construct validity of each TMT, we conducted a correlation study among the five types of TMT and other neuropsychological tests. All analyses were done with the PASW statistics version 18.0 (SPSS Inc., Chicago, IL, USA), with the statistical significance level set to p<0.05. In this study, the researchers did not consider the number of errors made by subjects, excluding them from the analysis.
RESULTS
There were no significant differences in educational background between those completing set A versus set B. In contrast, there was a significant difference in age between NC and MCI, MCI and AD, NC and AD in each set [F(2,83)=13.98, F(2,79)=6.97, p<0.05]. The results also show no significant differences in age, education level and MMSE score between the two sets.
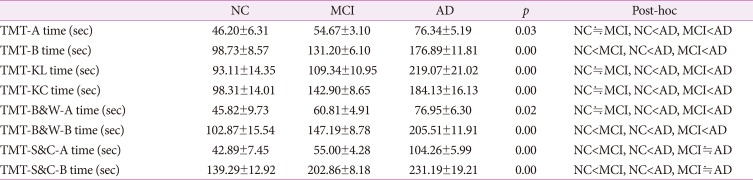
The original Trail Making Test
For both sets A and B, there were significant group differences in time-to-completion of TMT-A [F(2,80)=3.31, F(2,75)=23.44, p<0.05]. Significant differences in performance were seen between NC and AD, MCI and AD. There was no time-to completion difference between NC and MCI (Table 3).
Table 3. Results of time to completion among three patient groups in each TMT, according to two Trail Making sets.
Value is M±SD. Analysis of covariance (ANCOVA) test was used to determine group difference in TMT time-to-completion with age as a covariate.
AD: Alzheimer's disease, MCI: mild cognitive impairment, NC: normal controls, TMT: Trail Making Test, TMT-A: A form of TMT, TMT-B: B form of TMT, TMT-B&W-A: A form of black and white TMT, TMT-B&W-B: B form of black and white TMT, TMT-KC: Korean consonant version of TMT, TMT-KL: Korean letter version of TMT, TMT-S&C-A: A form of square and circle TMT, TMT-S&C-B: B form of square and circle TMT.
For set A, 51 subjects out of 86 completed the TMT-B, while 45 out of 82 completed the TMT-B in set B. The time-to-completion among the three groups were significantly different [F(2,45)=6.14, F(2,39)=11.57, p<0.05]. Significant differences were observed in each group comparison: NC and MCI, MCI and AD, as well as NC and AD (Table 3).
Korean version of Trail Making Test
Of the 168 subjects, 86 completed the TMT-KL. In the validation task that involved writing the Korean letters and English alphabet as directed, 51 subjects had an accurate performance. Fifteen wrote only English letters. Of the 35 participants unable to write the English alphabet, 27 also failed the Korean letter task. A significant difference in the completion time for the TMT-KL was noted between NC and AD, as well as MCI and AD [F(2,42)=13.33, p<0.05]; no differences were observed between NC and MCI (Table 3).
Remaining 82 participants were administered the TMT-KC in set B. Of these, 43 accurately completed the English alphabet validation task. Among them, 3 failed to accurately complete the Korean consonant task. Out of 39 subjects failing the English alphabet task, 22 also failed the Korean task. There was a significant difference in time-to-completion for the TMT-KC [F(2,44)=8.21, p<0.05] between NC and AD, as well as MCI and AD; no differences were observed between NC and MCI (Table 3).
Black and white Trail Making Test
TMT-B&W-A time-to-completion were disparate between NC and AD, MCI and AD [F(2,76)=4.06, p<0.05]. Time-to-completion in the TMT-B&W-B demonstrated significant differences among all groups [F(2,69)=14.96, p<0.05) (Table 3).
Square and circle Trail Making Test
Significant differences were observed in time-to-completion of the TMT-S&C-A between NC and MCI, as well as NC and AD [F(2,75)=28.45, p<0.05]. Similarly, a difference in time-to-completion of TMT-S&C-B [F(2,54)=11.23, p<0.05] was observed between NC and MCI, as well as NC and AD. No difference was observed between MCI and AD (Table 3).
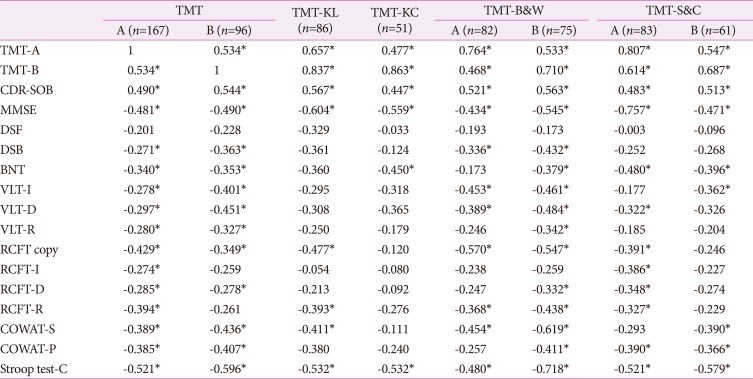
Correlations between Trail Making and other neuropsychological tests
Significant correlations among the TMTs, and between TMTs and other neuropsychological tests, were observed (Table 4).
Table 4. Correlation among the five TMTs and cognitive measures.
*p<0.01.
BNT: Boston Naming Test, COWAT-P: Controlled Oral Word Association Test-Phonemic word fluency, COWAT-S: Controlled Oral Word Association Test-Semantic word fluency, DSB: digit span backward, DSF: digit span forward, MMSE: Mini Mental Examination, RCFT copy: Rey Complex Figure Test copy, RCFT-D: Rey Complex Figure Test-20-minute delayed recall test, RCFT-I: Rey Complex Figure Test-Immediate recall test, RCFT-R: Rey Complex Figure Test-Recognition test, CDR-SOB: Clinical Dementia Rating scale-Sum of Boxes, Stroop test-C: Stroop test-color reading, TMT: Trail Making Test, TMT-A: A form of TMT, TMT-B: B form of TMT, TMT-B&W: TMT-black and white, TMT-KC: Korean consonants version of TMT, TMT-KL: Korean letter version of TMT, TMT-S&C: TMT-square and circle, VLT-D: Verbal Learning Test-20-minute delayed recall test, VLT-I: Verbal Learning Test-immediate recall test, VLT-R: Verbal Learning Test-recognition test.
DISCUSSION
The current study revealed that subjects performed poorly in all five types of TMT part B than TMT part A. The newly developed TMT-KL, TMT-KC, TMT-B&W-B, and TMT-S&C-B were designed as relevant and complicated as TMT-B, serving its role as modified part B of TMT.22,23,24,25
One purpose of this study was to determine if the original TMT would suffice for use in the Korean older adult population, or the development of TMT-K was necessary. Results of the two TMT-K tasks (TMT-KL and TMT-KC) discriminated only between NC and AD, MCI and AD, but did not differentiate NC from MCI. This suggests that the Korean language TMT differentiates only in the presence of substantial cognitive gaps. In contrast, completion time for the original TMT-B discriminated based on the degree of cognitive impairment, such that groups with different levels of cognitive impairment were consistently distinguishable from each other. In particular, the original TMT-B identified a difference in performance between NC and MCI that was not revealed by two TMT-Ks. This suggests that the original TMT is more sensitive in detecting earlier stages of cognitive decline.
Prior to conducting the TMT, participants completed the validation check of writing the Korean and English alphabets. Although better performance in writing the Korean alphabet was expected, most of the subjects who could not accurately complete the English alphabet were also unable to complete the task in Korean; rather, some subjects were better able to complete the English alphabet. Previous research25,26 and this study incorporated highly-educated subjects who showed greater difficulty in recalling the order of Korean alphabet rather than English ones. The current study suggests that education level is not related to the TMT-K performance, which contradicts previous research9 which suggest that performance rate of the TMT-K is influenced by education level. Therefore, it may be concluded that replacing the English alphabet with Korean letters does not provide greater benefit in distinguishing the level of cognitive impairment in older Korean adults, as the original TMT proved to be an effective tool in making that determination. However, given the high level of education attained in our study sample, it is possible that the development of an alternative is still required for those who are unable to complete the original English version of the TMT.
The TMT-B&W and TMT-S&C were created to address the need for evaluation of subjects with lower educational levels, and minimize effects of language. The TMT-B&W results suggest that time-to-completion of the TMT-B&W differed according to level of cognitive impairment, but the TMT-S&C did not significantly differentiate between MCI and AD. Thus, the results of the TMT-B&W were better aligned with results of the original TMT, effectively distinguishing these cognitive groups.
Results of the current study also demonstrate that, among the five TMT tasks utilized in this sample of older adult Koreans with varied levels of cognitive impairment, the original TMT and the TMT-B&W proved to be more sensitive to the degree of cognitive impairment. Similar to the original TMT, the TMT-B&W showed a high correlation with other neuropsychological tests, as well as between the original TMT and the TMT-B&W. Using the TMT-B&W, a participant did not require knowledge of the English alphabet, and test results show a pattern consistent with the original TMT. Thus, if a researcher is inclined to control language effects, then TMT-B&W is recommended. However, our study had some limitations. Although the participants were divided into two groups to avoid subjects fatigue and increase compliance, this study design is somewhat difficult to understand. In addition, the different number of subjects for each TMT task might influence the result of correlation analysis. Due to the low completion rate of TMT-B of each task, a lot of missing data might distort the analysis result, making the interpretation difficult, since the subset of all analysis results are different. Further studies with undereducated Korean subjects is needed to better determine the potential for a more general utilization of the TMT-B&W, considering the low completion rate.
Footnotes
Conflicts of Interest: The authors have no financial conflicts of interest.
References
- 1.Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. 4th ed. New York: Oxford University Press; 2004. pp. 317–374. [Google Scholar]
- 2.Spreen O, Strauss E. A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary. 2nd ed. New York: Oxford University Press; 1998. [Google Scholar]
- 3.Kraybill ML, Larson EB, Tsuang DW, Teri L, McCormick WC, Bowen JD, et al. Cognitive differences in dementia patients with autopsy-verified AD, Lewy body pathology, or both. Neurology. 2005;64:2069–2073. doi: 10.1212/01.WNL.0000165987.89198.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walker AJ, Meares S, Sachdev PS, Brodaty H. The differentiation of mild frontotemporal dementia from Alzheimer’s disease and healthy aging by neuropsychological tests. Int Psychogeriatr. 2005;17:57–68. doi: 10.1017/s1041610204000778. [DOI] [PubMed] [Google Scholar]
- 5.Crowe SF. The differential contribution of mental tracking, cognitive flexibility, visual search, and motor speed to performance on parts A and B of the Trail Making Test. J Clin Psychol. 1998;54:585–591. doi: 10.1002/(sici)1097-4679(199808)54:5<585::aid-jclp4>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 6.Anderson CV, Bigler ED, Blatter DD. Frontal lobe lesions, diffuse damage, and neuropsychological functioning in traumatic brain-injured patients. J Clin Exp Neuropsychol. 1995;17:900–908. doi: 10.1080/01688639508402438. [DOI] [PubMed] [Google Scholar]
- 7.Stuss DT, Bisschop SM, Alexander MP, Levine B, Katz D, Izukawa D. The Trail Making Test: a study in focal lesion patients. Psychol Assess. 2001;13:230–239. [PubMed] [Google Scholar]
- 8.Seo EH, Lee DY, Kim KW, Lee JH, Jhoo JH, Youn JC, et al. A normative study of the Trail Making Test in Korean elders. Int J Geriatr Psychiatry. 2006;21:844–852. doi: 10.1002/gps.1570. [DOI] [PubMed] [Google Scholar]
- 9.Yi HS, Chin JH, Lee BH, Kang YW, Na DL. Development and validation of Korean version of Trail Making Test for elderly persons. Dement Neurocognitive Disord. 2007;6:54–66. [Google Scholar]
- 10.Park JS, Kang YW, Yi HS, Kim YJ, Ma HI, Lee BC. Usefulness of the Korean Trail Making Test for the elderly (K-TMT-e) in detecting the frontal lobe dysfunction. Dement Neurocognitive Disord. 2007;6:12–17. [Google Scholar]
- 11.Kang Y, Na DL, Hahn SH. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997;15:300–308. [Google Scholar]
- 12.Kang SJ, Choi SH, Lee BH, Lee MA, Kwon JC, Na DL, et al. The reliability and validity of the Korean Instrumental Activities of Daily Living (K-IADL) J Korean Neurol Assoc. 2002;20:8–14. [Google Scholar]
- 13.Christensen KJ, Multhaup KS, Nordstrom SK, Voss KA. A cognitive battery for dementia: development and measurement characteristics. J Consult Clin Psychol. 1991;3:168–174. [Google Scholar]
- 14.Chin JH, Oh KJ, Seo SW, Shin HY, Na DL. The characteristics and subtypes of subjective memory impairment in older adults. Dement Neurocognitive Disord. 2010;9:115–121. [Google Scholar]
- 15.Marshall GA, Fairbanks LA, Tekin S, Vinters HV, Cummings JL. Neuropathologic correlates of activities of daily living in Alzheimer disease. Alzheimer Dis Assoc Disord. 2006;20:56–59. doi: 10.1097/01.wad.0000201852.60330.16. [DOI] [PubMed] [Google Scholar]
- 16.Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256:183–194. doi: 10.1111/j.1365-2796.2004.01388.x. [DOI] [PubMed] [Google Scholar]
- 17.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 18.O’Bryant SE, Waring SC, Cullum CM, Hall J, Lacritz L, Massman PJ, et al. Staging dementia using Clinical Dementia Rating Scale Sum of Boxes scores: a Texas Alzheimer’s research consortium study. Arch Neurol. 2008;65:1091–1095. doi: 10.1001/archneur.65.8.1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Bryant SE, Lacritz LH, Hall J, Waring SC, Chan W, Khodr ZG, et al. Validation of the new interpretive guidelines for the Clinical Dementia Rating scale Sum of Boxes score in the national Alzheimer’s coordinating center database. Arch Neurol. 2010;67:746–749. doi: 10.1001/archneurol.2010.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ashendorf L, Jefferson AL, O’Connor MK, Chaisson C, Green RC, Stern RA. Trail Making Test errors in normal aging, mild cognitive impairment, and dementia. Arch Clin Neuropsychol. 2008;23:129–137. doi: 10.1016/j.acn.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reitan RM. The relation of the Trail Making Test to organic brain damage. J Consult Psychol. 1955;19:393–394. doi: 10.1037/h0044509. [DOI] [PubMed] [Google Scholar]
- 22.Fossum B, Holmberg H, Reinvang I. Spatial and symbolic factors in performance on the Trail Making Test. Neuropsychology. 1992;6:71–75. [Google Scholar]
- 23.Rossini ED, Karl MA. The Trail Making Test A and B: a technical note on structural nonequivalence. Percept Mot Skills. 1994;78:625–626. doi: 10.2466/pms.1994.78.2.625. [DOI] [PubMed] [Google Scholar]
- 24.Arnett JA, Labovitz SS. Effect of physical layout in performance of the Trail Making Test. Psychol Assess. 1995;7:220–221. [Google Scholar]
- 25.Gaudino EA, Geisler MW, Squires NK. Construct validity in the Trail Making Test: what makes Part B harder? J Clin Exp Neuropsychol. 1995;17:529–535. doi: 10.1080/01688639508405143. [DOI] [PubMed] [Google Scholar]
- 26.Ivnik RJ, Malec JF, Smith GE, Tangalos EG, Petersen RC. Neuropsychological Tests’ norms above age 55: COWAT, BNT, MAE token, WRAT-R reading, AMNART, STROOP, TMT, and JLO. Clin Neuropsychol. 1996;10:262–278. [Google Scholar]