Abstract
Introduction: Introduction: Pressure ulcer is one of the most common and painful complications in patients admitted to intensive care units (ICUs). This study aimed to compare the effects of tragacanth gel cushions and foam-filled ones on the prevention of pressure ulcers.
Methods: This triple-blind, randomized, clinical trial was performed on 94 patients admitted to the ICU of Taleqhani Hospital of Mashhad, Iran. The participants were divided into two groups of tragacanth gel pad and foam (n=47 for each group). Both groups received all the routine care. The participants were examined on a daily basis during a ten-day period. We considered sacral region as the most affected site, and the patients with erythema were excluded from the study. To analyze the data, Chi-squared test, Fisher’s exact test, and t-test were run, using Stata version 12.
Results: The data showed significant differences in terms of the incidence of skin redness in the tragacanth gel cushions group and foam cushion group, respectively, 6.84 (1.58) and 5.67 (1.26) days after admission. In addition, in the tragacanth gel cushions group 14 patients (29.7%) did not have skin redness compared with the foam cushion group (8.51%), which indicated a significant difference.
Conclusion: This study showed that the use of tragacanth gel cushion is effective in the prevention of pressure ulcers in ICU patients. Cushions filled with tragacanth gel also delayed the onset of erythema. Considering their cost-effectiveness and naturalness, the use of tragacanth gel cushions is recommended to improve the sacral skin health and prevent pressure ulcers.
Keywords: Pressure ulcers, Intensive care unit, Prevention and control
Introduction
Pressure ulcers are characterized by a damage to the skin and underlying tissues caused by the pressure. The risk factors for this complication include inactivity, high skin temperature, moisture, and the presence of frictional and shear forces.1 Thus, the risk of pressure ulcers would increase in cases of unconsciousness, paralysis, and neurological diseases or patients admitted to intensive care units (ICUs).2 Currently, pressure ulcers affect 5-10% of patients. The death rate caused by pressure ulcers is 2-6 times higher among these patients and sixty thousand deaths occur due to pressure ulcers annually. In Iran, Reyhani and Haghiri reported a mortality rate of 22.7% due to pressure ulcers in ICUs.3,4 Pressure ulcers occur in different parts of the body such as the sacrum, iliac, heel, elbow, ankle, trochanter, head, and shoulders; the most common site being the sacral region which mostly happens among patients who are in supine position due to illness, 24% of whom develop bedsores in ICUs. The treatment of this complication is costly and time-consuming; however, according to the National Pressure Ulcer Advisory Panel (NPUAP), pressure ulcers and bedsores are preventable. A wide range of studies have been carried out to prevent or reduce the risk of pressure ulcers.5-7 Some grading scales are available to prevent pressure ulcers, and the Braden Scale is one of them. This scale consists of six subscales of sensory perception, moisture, mobility, activity, nutrition, and friction and shear.1,4,8 Generally, pressure ulcers are quite irritating and can even be lethal if untreated. In addition to high costs of the treatment, the patients suffering from this problem require more care than other patients do.9 In case of the incidence of pressure ulcers, surgical methods can pose several problems including infection, rejection, and recurrence.10 The current methods applied to prevent bedsores comprise various creams, air mattresses, and medical sheepskin products. All the listed methods are applied as complementary methods to prevent bedsores and a few studies have been conducted on their effects separately.11 The use of mattresses and cushions is one approach to prevent the development of decubitus ulcers by modifying the pressure on the skin or reducing the friction and frictional forces.12
In Iranian traditional medicine, tragacanth (Astragalus gossypinusfisch) has been commonly used as an herbal medicine because its polysaccharides contents, bassorin and tragacantin. Bassorin, swell up in water forming a viscous solution, and tragacantin is known as an insoluble polysaccharide which is reportedly pretty effective in certain skin diseases.13,14 Currently, one of the tools employed to remove the pulling and shearing forces that produce pressure ulcers are foams whose utility is not conclusively established.13 Foam has a flexible nature and is able to form parts of the body at any point. However, as other static instruments, it does not have fluidity property and should be used in patients who have a displacement power. In some studies, cushions or bags containing synthetic gels or water have been used for this purpose, which is sometimes questioned due to the infiltration of moisture on the patient's skin and the possibility of incidence of ulcers.12
In addition to adjusting the pressure on the skin, the slippery feature of tragacanth gel is used to remove friction between the patient's body and the bed, as well. In the case of gel penetration, the tragacanth gel also has therapeutic effects on the skin, unlike other gels. This would have led to the use of these cushions as supportive of the patient's skin.15 Considering the viscosity and flexibility of tragacanth, and due to its low cost and ease of plantation in Iran, we aimed to study the effects of cushions filled by tragacanth gel on the prevention of bedsores compared to foam at the sacrum region in traumatic patients admitted to ICU.
Materials and methods
This study was a two-group, triple-blinded randomized clinical trial, with a parallel design. In this clinical trial, we simultaneously assessed the effect of tragacanth gel cushions and foam-filled ones on the prevention of pressure ulcers and compared them. The study population consisted of 100 trauma patients admitted to the ICU of Taleghani Hospital from December 2015 to September 2016. Taleghani Hospital is affiliated with Mashhad University of Medical Sciences in Mashhad, Iran. This is a governmental hospital, with specialized medical wards, a CCU, and two trauma intensive care units (ICU).The inclusion criteria included 15˂ age ˂65, no underlying diseases such as diabetes and skin disorders, and Braden scale score of less than 18.
However, ICU stay of less than five days, allergic reactions and erythema, and an unwillingness to participate in the study constituted the exclusion criteria. All the study participants were selected through convenience sampling according to the inclusion criteria by the researcher, and then by using permutation blocks, randomized allocation was performed for the foam and gel cushion groups. Each six blocks were labeled as A, B, C, D, E, and F. The A, B, and C blocks were assigned to the tragacanth gel group and the other three to the foam group. The blocks were selected randomly and re-used.
The sample size was determined with power to detect a difference of at least 20% of bedsores in the intervention group Based on the previous studies.15 Assuming 5% and 20% probability of type I and II errors, respectively, 44 patients were selected for each group. Considering the potential attrition (13%), 50 cases were allocated to each group (Figure 1). All the demographic data such as gender, age, educational level, occupation, income, and history of addiction were recorded in a form. Moreover, by reading the relevant articles and resources and based on Braden’s criteria, a checklist was prepared. To determine the content and face validity of the checklist, it was reviewed by eight professors of Nursing and Midwifery Department of Sabzevar University of Medical Sciences and their suggestions were incorporated. The regional sacral skin of each patient was examined based on incidence or progression of ulcers until the end of the 10th day; the skin of sacrum was studied in terms of color.5
Figure 1.
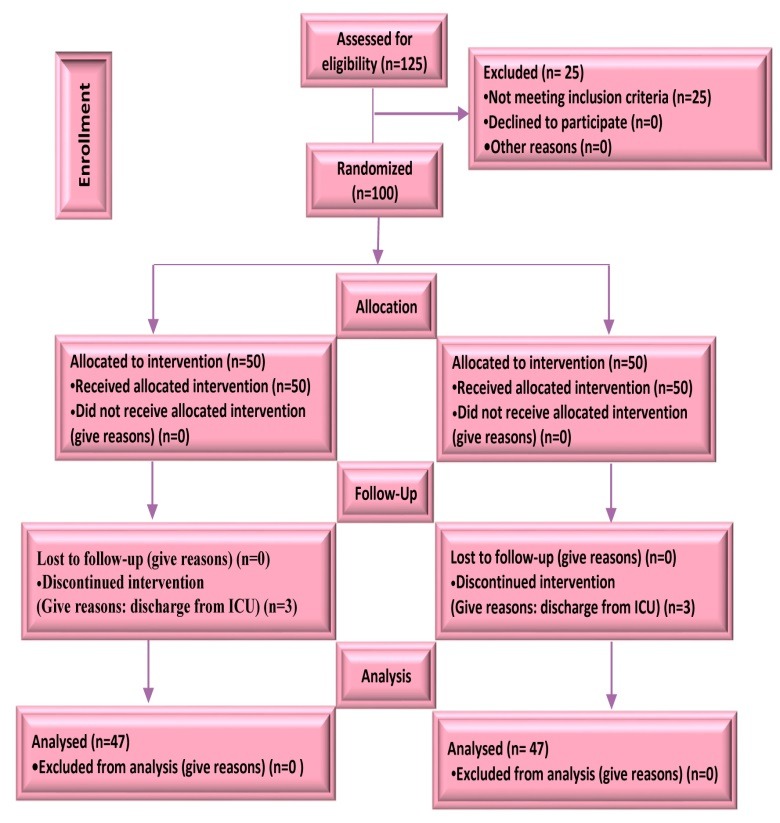
Flowchart of the design, groups, and participants in the study
Having obtained the approval of the Ethics Committee (No. IR.Medsab.Rec.95.14) of Sabzevar University of Medical Sciences, The study protocol was registered in the clinical trial registration website (IRCT201609 1129781N1). The researcher and research assistant presented to the hospital daily at 8 a.m. The research assistant was blinded to the intervention and the control groups while all the required trainings were being provided. The researcher recorded the demographic data and past medical history for each participant. The researcher explained the objectives, economic and health benefits, and the procedures of the study for the participants. Afterwards, the patients were allocated into two groups of foam and tragacanth gel cushions. The cases could also receive the routine health care such as wavy mattresses and having their positions changed. The researcher supervised all the study procedures to avoid any possible mistakes.The blinding method was used to avoid bias, and all the patients received the routine care.
All the cushions were built in accordance with the standards of NPUAP. The tragacanth gel cushions were made in a size 50x70 cm and in double layers. The raw material was made by Khorasani white tragacanth, which tragacanth was mixed with water in clean condition. Then the heat was administered so as to obtain the correct gel (gel viscosity=1%). Later, it was laid in the first layer of the plastic. The outer layer was made of soft velvet. The foam cushion was a Polyurethane product manufactured by Farafoam Company which was routinely used in Taleghani Hospital of Mashhad. The cushions were washable, convex in shape with two plastic and velvet layers. All the cushions used in the intervention group were equal in size (i.e., 70 cm long, 50 cm wide, and 5 cm in diameter). The only difference between the cushions was a code that was assigned to each group and only the researcher knew which code belongs to which group. The researcher supervised all the study procedures to avoid any possible problems or complications. Following ICU admission, foam and tragacanth gel cushions were constantly used in each group. Every morning, the research assistant monitored the patients and recorded the findings in a checklist; finally, the results were compared with each other. The data gathering tool in this research includes: demographic characteristics questionnaire and a researcher-made wound diagnostic checklist for the observation of the pressure ulcer incidence. With this tool, the studied area (sacrum) of the patients was examined for color changes. The skin color changing to red was considered as the beginning of the pressure ulcer through daily skin color assessment by the checklist. In case of reddening in the skin of the patient, they were excluded from the study to prevent the expansion of the pressure ulcer. In order to determine the validity of the demographic information questionnaire and the wound diagnostic checklist, the content and face validity were used. So, first these forms were prepared by reading the articles and resources. Then, it was considered by 8 Nursing and Midwifery Faculty. The reliability of the wound assessor (data collector) with researcher was performed by observing 10 wound-prone patients simultaneously, they completed the checklist form by observing the patients' skin, in all cases was completed by both of them results was alike, The consensus score within the assessors (Cohen Kappa coefficient) was 100%.
To describe quantitative variables, the mean (SD) and for qualitative variables, frequency (%) were used. A chi-squared test was used to compare the incidence rate of pressure ulcers between the two groups. To analyze the data, Stata version 12 was used. P-values less than 0.05 were considered statistically significant.
Results
The total age range was 15-65 years; the mean age of the patients in the tragacanth gel cushion group was 35.34 (13.61) and the mean age of the participants in the foam group was 38.64 (12.11) years, which was not significantly different between the two groups. The total mean weight was 71.57 (8.28) kg, 70.23 (7.31) and 72.91(9.04) kg in the Tragacanth Gel Cushion [TGC] and Foam Cushion [FC] groups, respectively). Furthermore, 57 (60.63%) cases were male and 37 (39.37%) were female.
Most patients (93.62%) had no previous history of hospitalization. Skin turgor was measured 1.40 (0.49) seconds. Moreover, 74.46% and 25.54 % of the cases were married and single, respectively. Most of the patients (65.96%) had light skin color. No underlying diseases were recorded among the majority of the cases (94.38%).
The mean consciousness levels were 8.87 (1.32) and 8.55 (1.74) in the TGC and FC groups, respectively. The education level was under Diploma among 34.04% of the patients. Most of the participants (27.66%) had a job, 88 (93.62%) had sufficient income, and 59 (62.77%) were living in urban areas. Most of the participants 81 (86.18%) had no history of addiction. The two groups were not significantly different in terms of demographic data (P˃0.05). The comparison of Braden score between the TGC and FC groups on the first day of admission did not show any significant differences 13.72 (3.38) and 12.72 (3.41), respectively; P=0.891). However, there was a significant difference between the two groups in terms of erythema (P= 0.008). Moreover, regarding the onset of erythema, a t-test showed a significant difference between the groups (P= 0.006).
Discussion
The present study compared the effects of tragacanth gel and foam cushions on the prevention of pressure ulcers among trauma patients admitted to ICU. Our findings demonstrated the positive effects of Tragacanth gel in the intervention group in comparison with the FC group; we found that the incidence of pressure ulcers was lower in the TGC compared to the FC, and the onset of erythema was delayed in the TGC group. Correspondingly, several published studies have reported the effectiveness of interventions such as lambskin, liquid mattress, foam, and air mattress.15-18 However, there are only a limited number of studies examining the effect of gel cushions, especially tragacanth gel due to its viscosity and fluidity features, on the prevention of pressure ulcer among hospitalized patients. Duetzmann et al., in a clinical trial examined the impact of pads containing liquid on sacral pressure ulcers in the patients with spinal cord injuries.13
They showed that the peak sacral pressure was reduced when liquid-based pad was used and they concluded that it could be economically advantageous in countries and hospitals with limited financial resources. Yanling et al., studied the effects of gelatin sponge combined with moist wound-healing nursing intervention in the treatment of phase III pressure ulcer.19
They showed that ulcer healing improved in intervention group compared to the control group, while comparatively less medication was used other studies have emphasized the natural compounds. Hawaibam et al., and Madadi et al., in two separate studies, examined the effectiveness of olive oil in the prevention of pressure ulcers in immobilized patients.20,21 They reported that the regular use of olive-oil-based formulas should be effective in preventing pressure ulcers, thus, leading to a more cost-effective product and an alternative treatment.
Our findings were in line with those of the study by Hawaibam due to the similarity of tragacanth with olive in terms of fluidity and slipperiness, which may lead to the elimination of frictional forces between patient’s skin and bed. Fluid preventive materials are efficacious in the
Table 1. Mean braden score on the 1st day after admission, lack of erythema, and time of erythema presentation.
| Variables | Tragacanth gel cushions group | Foam cushions group | Total | P | |||
| Mean (SD) | N (%) | Mean (SD) | N (%) | Mean (SD) | N (%) | ||
| Mean Braden score on the 1st day after admission | 13.72 (3.38) | 47 (50) | 12.72 (3.41) | 47 (50) | 13.28 (3.4) | 94 (100) | 0.89* |
| Lack of erythema | - | 14 (29.78) | - | 4 (8.51) | - | 18 (38.29) | 0.008* |
| The onset of erythema (Day) | 6.84 (1.58) | 33 (35) | 5.67 (1.26) | 43 (46) | 6.81 (1.25) | 76 (81) | 0.006* |
*t-test
prevention of pressure ulcers as they reduce pressure and shear forces. Mistiaen et al., assessed the effectiveness of the Australian Medical Sheepskin in the prevention of pressure ulcers at somatic nursing homes.22they revealed that the elasticity of sheepskin is an effective factor in the prevention of sacral pressure ulcers in nursing home patients. Although the materials in the present study are different from those applied by Mistiaen, the current reports demonstrate that natural compounds prevent the onset of the ulcersand improve the healing process of the ulcers caused by sacral pressure. The results of this study indicated that the tragacanth gel cushions could be effective in the prevention of pressure ulcers and delaying the onset of erythema, at least one day more than foam cushions. One day later, affected by pressure ulcers in ICUs is of a great importance because, in this distance, ICU patients may be become consciousness and as a result, achieve more mobility, and adequate nutrition. So, pressure ulcers may be completely prevented. Moreover, the use of tragacanth gel cushions is cost effective in comparison to foam cushions. Therefore, it is recommended to use tragacanth gel cushions in ICUs. The sample size in this study was 100, which can provide more accurate, and generalizable results if increased. Many individual differences, including genetics and some of the components that could not be detected in this study, can affect the development of ulcers on the skin of the patients.
Conclusion
This study revealed that the use of tragacanth gel cushions is effective in the prevention of pressure ulcers and delaying the onset of erythema in ICU patients. Given their cost-effectiveness and limited use of chemical compounds, tragacanth gel cushions are recommended to improve the sacral skin health system and prevent pressure ulcers. Nurses as caregivers, should always consider the prevention of pressure ulcers in critical settings. Nurses with the knowledge of the new method of pressure ulcer prevention, such as tragacanth gel cushions, can employ these methods in clinical settings. Future studies are recommended to replicate this study with a larger sample size and consideration of the effects of interfering factors such as genetics as it was not within the scope of this study. Moreover, it is suggested that the effect of tragacanth gel cushions
with other preventive pressure ulcer aids should be considered.
Acknowledgments
This study was sponsored by Sabzevar University of Medical Sciences. We wish to thank the deputy of research and all the patients (or their legal guardians) for their cooperation with us.
Ethical issues
None to be declared.
Conflict of interest
The authors declare no conflict of interest in this study.
Citation: Shakibamehr J, Rad M, Akrami R, Rad M. Effectiveness of tragacanth gel cushions in prevention of pressure ulcer in traumatic patients: a randomized controlled trial. J Caring Sci 2019; 8 (1): 45-9. doi: 10.15171/jcs.2019.007.
References
- 1.Chou R, Dana T, Bougatsos C, Blazina I, Starmer AJ, Reitel K. et al. Pressure ulcer risk assessment and preventiona systematic comparative effectiveness review. Annals of Internal Medicine. 2013;159(1):28–38. doi: 10.7326/0003-4819-159-1-201307020-00006. [DOI] [PubMed] [Google Scholar]
- 2.Brienza D, Kelsey S, Karg P, Allegretti A, Olson M, Schmeler M. et al. A randomized clinical trial on preventing pressure ulcers with wheelchair seat cushions. J Am Geriatr Soc. 2010;58(12):2308–14. doi: 10.1111/j.1532-5415.2010.03168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iranmanesh S, Rafiei H, Foroogh Ameri G. Critical care nurses' knowledge about pressure ulcer in southeast of iran. International Wound Journal. 2011;8(5):459–64. doi: 10.1111/j.1742-481X.2011.00817.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qaseem A, Mir TP, Starkey M, Denberg TD. Risk assessment and prevention of pressure ulcers: a clinical practice guideline from the american college of physicians. Annals of Internal Medicine. 2015;162(5):359–69. doi: 10.7326/M14-1567. [DOI] [PubMed] [Google Scholar]
- 5.Qaseem A, Humphrey LL, Forciea MA, Starkey M, Denberg TD. Treatment of pressure ulcers: a clinical practice guideline from the american college of physicians. Annals of Internal Medicine. 2015;162(5):370–9. doi: 10.7326/M14-1568. [DOI] [PubMed] [Google Scholar]
- 6.Fujii K, Sugama J, Okuwa M, Sanada H, Mizokami Y. Incidence and risk factors of pressure ulcers in seven neonatal intensive care units in Japan: a multisite prospective cohort study. International wound journal. 2010;7(5):323–8. doi: 10.1111/j.1742-481X.2010.00688.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wurster J. What role can nurse leaders play in reducing the incidence of pressure sores? Nurs Econ. 2007; 25(5):267–9. [PubMed] [Google Scholar]
- 8.Pancorbo-Hidalgo PL, Garcia-Fernandez FP, Lopez- Medina IM, Alvarez-Nieto C. Risk assessment scales for pressure ulcer prevention: a systematic review. Journal of Advanced Nursing. 2006;54(1):94–110. doi: 10.1111/j.1365-2648.2006.03794.x. [DOI] [PubMed] [Google Scholar]
- 9.Fonder MA, Lazarus GS, Cowan DA, Aronson-Cook B, Kohli AR, Mamelak AJ. Treating the chronic wound: a practical approach to the care of nonhealing wounds and wound care dressings. J Am Acad Dermatol. 2008;58(2):185–206. doi: 10.1016/j.jaad.2007.08.048. [DOI] [PubMed] [Google Scholar]
- 10.Kuo PJ, Chew KY, Kuo YR, Lin PY. Comparison of outcomes of pressure sore reconstructions among perforator flaps, perforator-based rotation fasciocutaneous flaps, and musculocutaneous flaps. Microsurgery. 2014;34(7):547–53. doi: 10.1002/micr.22257. [DOI] [PubMed] [Google Scholar]
- 11.Gao L, Yang L, Li X, Chen J, Du J, Bai X. et al. The use of a logistic regression model to develop a risk assessment of intraoperatively acquired pressure ulcer. Journal of Clinical Nursing. 2018;27(15-16):2984–92. doi: 10.1111/jocn.14491. [DOI] [PubMed] [Google Scholar]
- 12.McInnes E, Jammali-Blasi A, Bell-Syer SE, Dumville JC, Cullum N. Support surfaces for pressure ulcer prevention. 9th ed. United Kingdom: Cochrane Database of Systematic Reviews; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duetzmann S, Forsey LM, Senft C, Seifert V, Ratliff J, Park J. Sacral peak pressure in healthy volunteers and patients with spinal cord injury: with and without liquid-based pad. Nursing Research. 2015;64(4):300–5. doi: 10.1097/NNR.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 14.Moghbel A, Agheli H, Kalantari E, Naji M. Design and formulation of tragacanth dressing bandage for burn healing with no dermal toxicity. Toxicology Letters. 2008;180(Supll):S154. doi: 10.1016/j.toxlet.2008.06.341. [DOI] [Google Scholar]
- 15.Reihani H, Haghiri A. Determination of bed sore risk factors in craniospinal trauma patients in intensive care units. Arak Medical University Journal. 2007;10(39-46):2. (Persian) [Google Scholar]
- 16.Wong H, Kaufman J, Baylis B, Conly JM, Hogan DB, Stelfox HT. et al. Efficacy of a pressure-sensing mattress cover system for reducing interface pressure: study protocol for a randomized controlled trial. Trials. 2015;16(1):434. doi: 10.1186/s13063-015-0949-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beniamino P, Vadala M, Laurino C. Cross-linked hyaluronic acid in pressure ulcer prevention. Journal of Wound Care. 2016;25(7):400–5. doi: 10.12968/jowc.2016.25.7.400. [DOI] [PubMed] [Google Scholar]
- 18.Reger SI, Ranganathan VK, McNulty AK. Use of a powered coverlet for moisture removal, skin temperature reduction, odor, and bacteria control. J Wound Ostomy Continence Nurs. 2014;41(1):35–9. doi: 10.1097/WON.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 19.Li Y, Yao M, Wang X, Zhao Y. Effects of gelatin sponge combined with moist wound-healing nursing intervention in the treatment of phase III bedsore. Experimental and Therapeutic Medicine. 2016;11(6):2213–6. doi: 10.3892/etm.2016.3191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hawaibam B, Tryambake R, Memchoubi K. Effectiveness of olive oil massage on prevention of decubitus ulcer among bedridden patients. Int J Recent Sci Res. 2016;7(5):10933–7. [Google Scholar]
- 21.Abbas Ali Madadi Z, Zeighami R, Azimiyan J, Javadi A. The effect of topical olive oil on prevention of bedsore in intensive care units patients. International Journal of Research in Medical Sciences. 2015;3(9):2342–7. doi: 10.18203/2320-6012.ijrms20150628. [DOI] [Google Scholar]
- 22.Mistiaen P, Achterberg W, Ament A, Halfens R, Huizinga J, Montgomery K, Post H, Spreeuwenberg P, Francke AL. The effectiveness of the australian medical sheepskin for the prevention of pressure ulcers in somatic nursing home patients: a prospective multicenter randomized‐controlled trial (ISRCTN17553857) Wound Repair and Regeneration. 2010;18(6):572–9. doi: 10.1111/j.1524-475X.2010.00629.x. [DOI] [PubMed] [Google Scholar]


