Abstract
Objectives
Everyone deserves a long and healthy life, but in reality, health outcomes differ across populations. We use results from the Global Burden of Disease Study 2017 (GBD 2017) to report patterns in the burden of diseases, injuries, and risks at the global, regional, national, and subnational level, and by sociodemographic index (SDI), from 1990 to 2017.
Design
GBD 2017 undertook a systematic analysis of published studies and available data providing information on prevalence, incidence, remission, and excess mortality. We computed prevalence, incidence, mortality, life expectancy, healthy life expectancy, years of life lost due to premature mortality, years lived with disability, and disability-adjusted life years with 95% uncertainty intervals for 23 age groups, both sexes, and 918 locations, including 195 countries and territories and subnational locations for 16 countries from 1990 to 2017. We also computed SDI, a summary indicator combining measures of income, education, and fertility.
Results
There were wide disparities in the burden of disease by SDI, with smaller burdens in affluent countries and in specific regions within countries. Select diseases and risks, such as drug use disorders, high blood pressure, high body mass index, diet, high fasting plasma glucose, smoking, and alcohol use disorders warrant increased global attention and indicate a need for greater investment in prevention and treatment across the life course.
Conclusions
Policymakers need a comprehensive picture of what risks and causes result in disability and death. The GBD provides the means to quantify health loss: these findings can be used to examine root causes of disparities and develop programs to improve health and health equity.
Keywords: Global Burden of Disease, Health Equity, Disparities, Mortality, Injuries, Risk Factors
Introduction
The World Bank commissioned the original Global Burden of Disease (GBD) study and featured it in the landmark World Development Report 1993: Investing in Health.1 This early GBD study served as the most comprehensive effort up to that point to systematically measure the world’s health problems, generating estimates for 107 diseases and 483 sequelae (nonfatal health consequences related to a disease). It covered eight regions and five age groups with estimates for 1990.
The GBD has evolved over time; it is now produced annually by the Institute for Health Metrics and Evaluation at the University of Washington in Seattle, WA, with more than 3,600 collaborators in 140 countries.2–15 GBD 2017 used a comprehensive approach to report causes of death with garbage redistribution; systemically and simultaneously estimated disease incidence, prevalence, and exposure to risks and injuries; and used statistical models to pool data, adjust for bias, and incorporate covariates.2–15 It used several metrics to report results on health loss related to specific diseases, injuries, and risk factors: deaths and death rates, years of life lost due to premature mortality (YLLs), prevalence and prevalence rates for sequelae, years lived with disability (YLDs), Health Adjusted Life Expectancy (HALE), and disability-adjusted life years (DALYs). The study provided a comprehensive assessment of all-cause mortality and estimates for 282 causes of death, 354 causes of YLDs, and 359 causes of DALYs in 195 countries and territories from 1990 to 2017.
In this article, we used the publicly available GBD 2017 data to highlight how GBD data can identify health disparities and provide information for setting public health priorities to address health equity. We also outline proposed future directions for the GBD and explore how these additions could empower health officials to develop policies and interventions informed by local priorities.
Methods
To estimate the burden of disease, estimation for each sequela began with a systematic analysis of published studies and available data sources providing information on prevalence, incidence, remission, and excess mortality.
All-cause Mortality and Cause of Death
Six modeling approaches were used to assess cause-specific mortality, with the Cause of Death Ensemble Model (CODEm) generating estimates for the vast majority of causes.2 Deaths were tabulated by location, age group (<1, 1-4, 5-9, …, 90-94, and 95+), sex, year, and by cause. The cause list developed by GBD and used for this analysis has been widely used for cause of death analyses,2 and is arranged hierarchically in four levels.
Incidence and Prevalence
The study estimated incidence and prevalence by age, sex, cause, year, and location using a wide range of updated and standardized analytical procedures.4 GBD used DisMod-MR, a Bayesian meta-regression tool, to determine prevalence and incidence by cause and sequelae.4
Additional Metrics: YLLs, YLDs, DALYs, and HALE
Based on standard GBD methods, YLLs were computed by multiplying the number of deaths from each cause in each age group by the reference life expectancy at the average age of death among those who died in the age group.3 YLL computations used the same life table standard for calculating YLLs in all locations and years. This decision is essential in order to compare estimates of YLLs across locations and years. The life table standard is meant to represent the mortality experience of a population with minimal excess mortality, using the lowest observed age-specific mortality rates in 2017 among all countries with a population greater than five million. Prevalence of each sequela was multiplied by the disability weight for the corresponding health state to calculate YLDs for the sequela.4 The sum of all YLDs for relevant sequelae equated to overall YLDs for each disease. Details on disability weights for GBD 2017, including data collection and disability weight construction, are described elsewhere.16
DALYs were computed by summing YLLs and YLDs for each cause, age, and sex.5 DALYs were computed for 359 diseases with 95% uncertainty intervals (UIs) capturing the uncertainty for both YLL and YLD rates. Healthy life expectancy (HALE) was calculated using the Sullivan method,17 and generated 95% UIs that represented uncertainty for age-specific death rates and YLDs per capita for each location, age, sex, and year. HALE was calculated for each geographic location using multiple-decrement life tables and estimated YLDs per capita.
Risk Factors
GBD 2017 used the comparative risk assessment (CRA) framework developed for previous iterations of the GBD study to estimate attributable deaths, DALYs, and trends in exposure by age, sex, year, and location for 84 behavioral, environmental and occupational, and metabolic risks or clusters of risks over the period 1990 to 2017.6 Risk-outcome pairs were included in GBD 2017 if they met World Cancer Research Fund criteria for convincing or probable evidence.18 Relative risk estimates were extracted from published and unpublished randomized controlled trials, cohorts, and pooled cohorts. GBD uses the counterfactual scenario of theoretical minimum risk level (TMREL) to attribute burden. TMREL is the level for a given risk exposure that could minimize risk at the population level. A summary exposure value (SEV) was developed for GBD 2015 as the relative risk-weighted prevalence of exposure. SEV ranges from zero, when no excess risk exists in a population, to one, when the population is at the highest risk.
To calculate risk-attributable fractions of disease burden by cause, we modeled the effects of risk exposure levels, documented relative risks (RRs) associated with risk exposure and specific health outcomes, and computed counterfactual levels of risk exposure on estimates of deaths, YLLs, YLDs, and DALYs.
Sociodemographic Index and Decomposition of Variance
GBD 2017 created the socio-demographic index (SDI) based on lag-dependent income per capita, average educational attainment for those aged >15 years, and the total fertility rate under 25.7,10,19 Estimates of observed disease burden were compared with expected burden, or a country’s anticipated burden based on its development status.2–15
GBD 2017 documented each step of the estimation processes, as well as all data sources, in accordance with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) statement, and all data and codes are publicly available.20
Results
Age and Equity
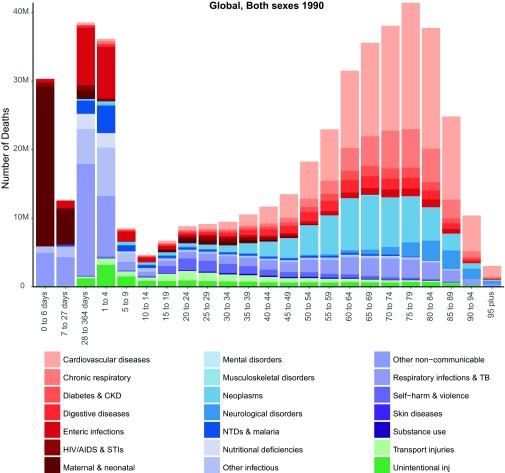
Figure 1 shows the number and causes of death by five-year age groups at the global level in 1990. There were clear patterns, with more infectious diseases causing deaths in younger age groups compared with a greater burden of non-communicable diseases at later ages. Diarrheal and lower respiratory infections were more common in younger ages. Injuries and self-harm were highest in young adults, while cardiovascular diseases and cancer were the main causes of death in older age groups.
Figure 1. Number and cause of deaths by five-year age group at the global level in 1990.
Time and Equity
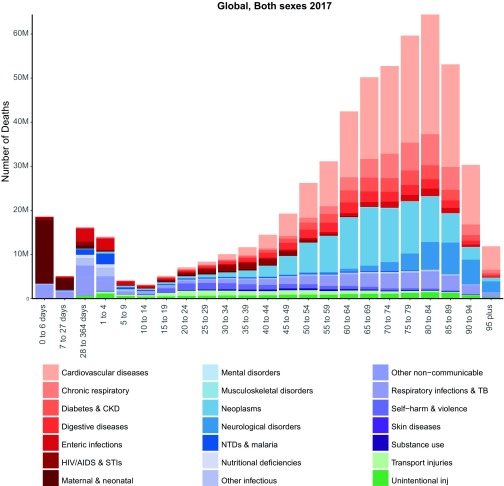
Figure 2 shows the number and causes of death by five-year age groups at the global level in 2017. The comparison with Figure 1 shows that from 1990 to 2017 there was a tremendous decrease in the number of global deaths, most notably in children under five. However, declines varied across countries, and in many, improvements have slowed over time (see GBD visualization tools at https://vizhub.healthdata.org/gbd-compare/).
Figure 2. Number and cause of deaths by five-year age group at the global level in 2017.
Ischemic heart disease and stroke remained the first and second causes of death. A noticeable general trend of declining infectious diseases occurred alongside a rise in non-communicable diseases, a trend which has been termed the epidemiologic transition. High systolic blood pressure, smoking, high fasting plasma glucose, high body-mass index, and particulate matter pollution were the leading causes in 2017, while child growth failure dropped from the 4th rank to the 19th at the global level.
Disabilities and Equity
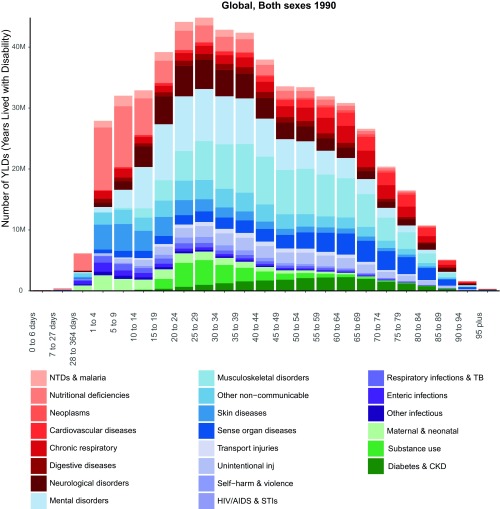
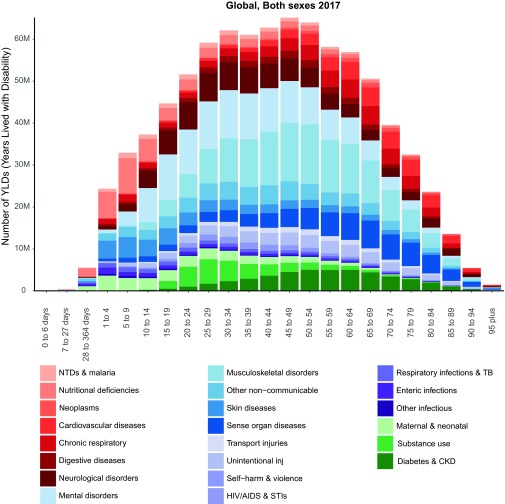
Figure 3 and Figure 4 show the number of YLDs by five-year age groups at the global level in 1990 and 2017 by cause. There was little improvement in the number of disabilities from 1990 to 2017, particularly compared with the improvements observed for deaths. There were huge variations by age in the cause of disabilities. For example, mental disorders were highest in those aged 25 to 29 years.
Figure 3. Number of YLDs by five-year age group at the global level in 1990 by cause.
Figure 4. Number of YLDs by five-year age group at the global level in 2017 by cause.
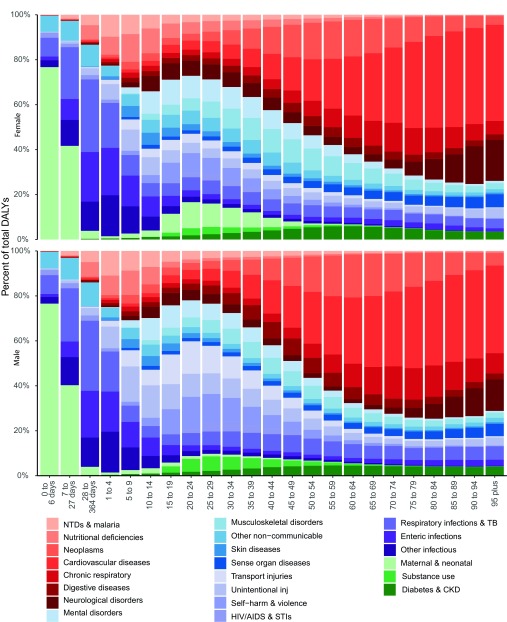
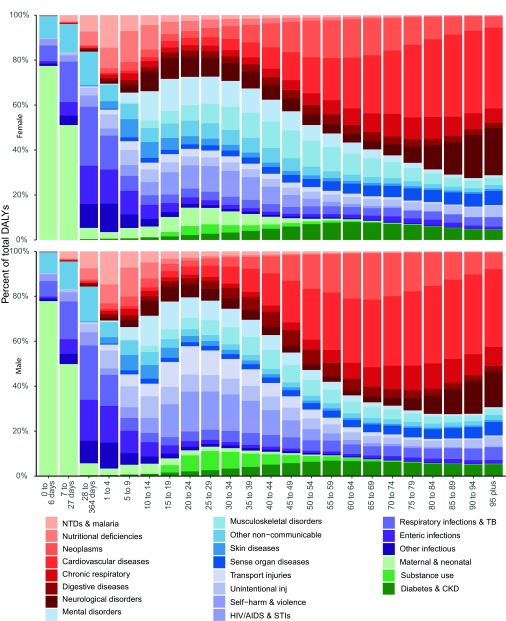
Sex and Equity
Figure 5 and Figure 6 show the percentage of DALYs by five-year age groups at the global level in 1990 and 2017 by cause for males and females. The results show clear patterns of burden by sex. Females had more DALYs from mental health and diabetes compared with males, while males had more DALYs from injuries and HIV/AIDs.
Figure 5. Percentage of DALYs by five-year age group at the global level in 1990 by cause for males and females.
Figure 6. Percentage of DALYs by five-year age group at the global level in 2017 by cause for males and females.
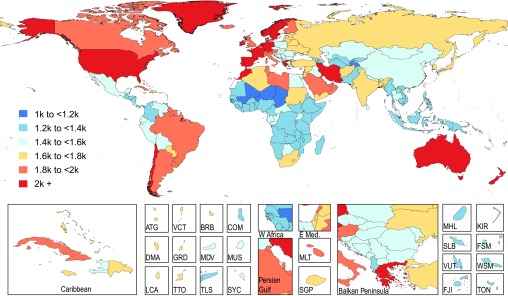
Geography and Equity
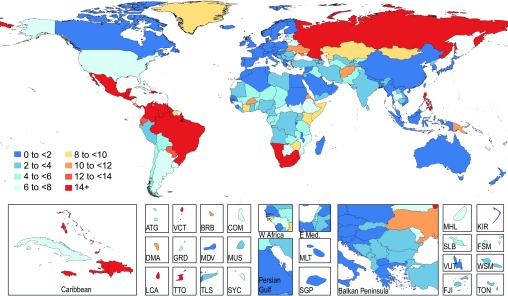
Figure 7 shows the global distribution of DALY rates per 100,000 from mental disorders in 2017. Greenland, Iran, Australia, New Zealand, the United States and other developed nations stood out as having larger burdens compared with the rest of the world. Another finding of note is the sharp difference in DALYs due to mental disorders between the United States and its neighbors.
Figure 7. Global distribution of DALY rates from mental disorders in 2017, both sexes, all ages, per 100,000.
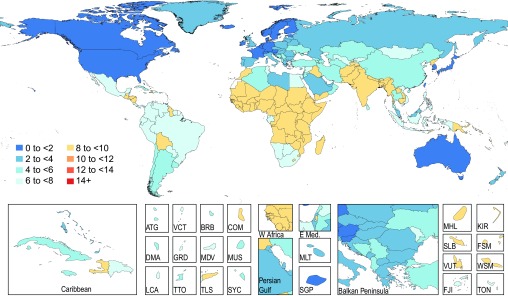
Equity Measured by Observed vs Expected SDI
Figure 8 and Figure 9 show the observed and expected rates of death (per 100,000) from interpersonal violence globally. There are very noticeable trends: countries in South America, South Africa, Philippines, and Russia had more deaths from interpersonal violence than would be expected given their SDI. Conversely, countries in Africa with some notable exceptions (ie, South Africa, Namibia, and Lesotho) and parts of Asia had much lower deaths from violence than would be expected.
Figure 8. Observed death rates from interpersonal violence globally, 2017, both sexes, all ages, per 100,000.
Figure 9. Expected death rates from interpersonal violence globally, 2017, both sexes, per 100,000.
Discussion
This article showcases several features of the GBD that enable the examination of health equity by sex, age, year, location, and SDI. The GBD provides a unique research opportunity, allowing for the detailed exploration of drivers and trends of the burden of disease. Moreover, as a global public good, it allows for comparisons between and within countries to examine disparities and empower health officials to address health equity.21–26 GBD data could also be used to assess progress from 1990 and as a baseline for future health trends.
The GBD is a global effort. Indeed, the level of complex analyses and resources required to produce the GBD cannot be achieved without the wide range of expertise at the Institute for Health Metrics and Evaluation (IHME) and available through the large number of international collaborators.
IHME undertakes several other projects alongside the GBD to improve the understanding of the issues impacting the burden of disease. For example, the Health Access and Quality of Care Index (HAQ) is based on 32 causes from which deaths should not occur in the presence of effective health care.27 The HAQ Index in 2016 varied from a high of 97.1 in Iceland to a low of 18.6 in the Central African Republic. The rank of the US in 2016, at 27th, represents a significant decrease from 1990, when it ranked 6th. Though the US made progress between 1990 and 2000, it witnessed a stagnation between 2001 and 2016.
IHME also produces a human capital index, measured as the number of years a person can be expected to work in the years of peak productivity, taking into account life expectancy, functional health, years of schooling, and learning.28 Countries that made greater improvements in the human capital index had faster economic growth in per capita GDP. The findings of this index highlight the need for countries to invest in health and education — improving economies by improving the productivity of labor forces.
The IHME Disease Expenditure project builds on the GBD to determine health care spending by health condition, age and sex, type of care, and time.29 This information can help health systems researchers and policymakers identify the drivers of spending increases and better plan for the future. Only by understanding the current health spending landscape can decision makers better allocate resources, technology, and innovation to improve health outcomes and systems performance.30–33
Another IHME project is the Local Burden of Disease, designed to produce estimates of health outcomes and related measures at a very fine resolution, at 5 by 5 kilometers.34–39 Such estimates allow decision-makers to target resources and health interventions precisely and tailor health policy for local areas rather than entire countries. Several publications from the local burden of disease showed huge variation in Africa in educational levels, anemia, diarrhea, and child growth.34–36 This project provides valuable information to governments, donors, and health agencies.
IHME’s Future Health Scenarios project examines future potential health outcomes such as life expectancy and causes of death.8 This project aims to help inform policies and programs to improve health. Understanding the drivers of health and their trajectories is crucial to setting investment priorities to maximize benefits, particularly given limited resources. The project’s projections show the burden that would occur if a country performed at a different level, using projections from all countries and applying the 15th or 85th percentiles of performance.40 In addition, IHME will expand the GBD to report on the burden that is amenable to health care, and on the percentage of the burden that could be averted by reducing specific risk factors or by improving specific determinants of health.41
The GBD and other IHME projects have documented the burden and have shown the magnitude of health disparities: the first step toward improving health. There is often a gap between the identification of a problem, the location of a solution, and the translation of that solution to an entire population. We currently lack a systematic, scalable process for determining which interventions are most likely to succeed in a given situation. There is an urgent need to fill this critical gap in the tools available to policy makers, health leaders, and others. By drawing on the interdisciplinary strengths of several players, such as universities, federal governments, United Nations agencies, donors, bilateral groups, non-government organizations, public-private partnerships, and others, one could create a groundbreaking knowledge base and process for the translation of successful population health interventions to sustainable implementation in wider practice and policy.
Two substantial steps would need to be taken in order to achieve this goal. First, identify, compile, and make publicly available the full spectrum of peer-reviewed and grey literature regarding interventions for a targeted disease, risk factor, social determinant, or other population health issue, with selected literature covering both successful and unsuccessful outcomes. Second, synthesize the available quantitative and qualitative evidence gathered in the previous step to develop a publicly accessible diagnosis of why specific population-level interventions and innovations for a targeted area succeed or fail, including an analysis of the quality of the available evidence for each area. Partnerships with communities, governments, foundations, and other collaborators will be essential.
Conclusion
In conclusion, GBD is a global public good that allows everyone to access health data to improve health. The GBD provides the health metrics needed to improve health equity by revealing existing health disparities at the local, national, and global level. This wealth of information is the first step toward reducing disparities: we cannot change what we are not able to measure.
Acknowledgments
Funding: Bill & Melinda Gates Foundation. Role of the Funder: The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
References
- 1.World Development Report 1993: Investing in Health. New York: World Bank; 1993. https://openknowledge.worldbank.org/handle/10986/5976.
- 2. Dicker D, Nguyen G, Abate D, et al. ; GBD 2017 Mortality Collaborators . Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1684-1735. 10.1016/S0140-6736(18)31891-9 10.1016/S0140-6736(18)31891-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Roth GA, Abate D, Abate KH, et al. ; GBD 2017 Causes of Death Collaborators . Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736-1788. 10.1016/S0140-6736(18)32203-7 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. James SL, Abate D, Abate KH, et al. ; GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789-1858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kyu HH, Abate D, Abate KH, et al. ; GBD 2017 DALYs and HALE Collaborators . Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859-1922. 10.1016/S0140-6736(18)32335-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stanaway JD, Afshin A, Gakidou E, et al. ; GBD 2017 Risk Factor Collaborators . Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1923-1994. 10.1016/S0140-6736(18)32225-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Murray CJL, Callender CSKH, Kulikoff XR, et al. ; GBD 2017 Population and Fertility Collaborators . Population and fertility by age and sex for 195 countries and territories, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1995-2051. 10.1016/S0140-6736(18)32278-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Foreman KJ, Marquez N, Dolgert A, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet. 2018;392(10159):2052-2090. 10.1016/S0140-6736(18)31694-5 10.1016/S0140-6736(18)31694-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lozano R, Fullman N, Abate D, et al. ; GBD 2017 SDG Collaborators . Measuring progress from 1990 to 2017 and projecting attainment to 2030 of the health-related Sustainable Development Goals for 195 countries and territories: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):2091-2138. 10.1016/S0140-6736(18)32281-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wang H, Abajobir AA, Abate KH, et al. ; GBD 2016 Mortality Collaborators . Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1084-1150. 10.1016/S0140-6736(17)31833-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Naghavi M, Abajobir AA, Abbafati C, et al. ; GBD 2016 Causes of Death Collaborators . Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151-1210. 10.1016/S0140-6736(17)32152-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vos T, Abajobir AA, Abate KH, et al. ; GBD 2016 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211-1259. 10.1016/S0140-6736(17)32154-2 10.1016/S0140-6736(17)32154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hay SI, Abajobir AA, Abate KH, et al. ; GBD 2016 DALYs and HALE Collaborators . Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1260-1344. 10.1016/S0140-6736(17)32130-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gakidou E, Afshin A, Abajobir AA, et al. ; GBD 2016 Risk Factors Collaborators . Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1345-1422. 10.1016/S0140-6736(17)32366-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fullman N, Barber RM, Abajobir AA, et al. ; GBD 2016 SDG Collaborators . Measuring progress and projecting attainment on the basis of past trends of the health-related Sustainable Development Goals in 188 countries: an analysis from the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1423-1459. 10.1016/S0140-6736(17)32336-X 10.1016/S0140-6736(17)32336-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Salomon JA, Haagsma JA, Davis A, et al. Disability weights for the Global Burden of Disease 2013 study. Lancet Glob Health. 2015;3(11):e712-e723. 10.1016/S2214-109X(15)00069-8 [DOI] [PubMed] [Google Scholar]
- 17. Sullivan DF. A single index of mortality and morbidity. HSMHA Health Rep. 1971;86(4):347-354. 10.2307/4594169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. American Institute for Cancer Research , World Cancer Research Fund, eds. Food, Nutrition, Physical Activity and the Prevention of Cancer: A Global Perspective: A Project of World Cancer Research Fund International. Washington, DC: American Institute for Cancer Research; 2007.
- 19. Wang H, Naghavi M, Allen C, et al. ; GBD 2015 Mortality and Causes of Death Collaborators . Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459-1544. 10.1016/S0140-6736(16)31012-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stevens GA, Alkema L, Black RE, et al. ; The GATHER Working Group . Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388(10062):e19-e23. 10.1016/S0140-6736(16)30388-9 [DOI] [PubMed] [Google Scholar]
- 21. Nomura S, Sakamoto H, Glenn S, et al. Population health and regional variations of disease burden in Japan, 1990-2015: a systematic subnational analysis for the Global Burden of Disease Study 2015. Lancet. 2017;390(10101):1521-1538. 10.1016/S0140-6736(17)31544-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gómez-Dantés H, Fullman N, Lamadrid-Figueroa H, et al. Dissonant health transition in the states of Mexico, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2016;388(10058):2386-2402. 10.1016/S0140-6736(16)31773-1 [DOI] [PubMed] [Google Scholar]
- 23. Dandona L, Dandona R, Kumar GA, et al. ; India State-Level Disease Burden Initiative Collaborators . Nations within a nation: variations in epidemiological transition across the states of India, 1990-2016 in the Global Burden of Disease Study. Lancet. 2017;390(10111):2437-2460. 10.1016/S0140-6736(17)32804-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mokdad AH, Ballestros K, Echko M, et al. ; US Burden of Disease Collaborators . The State of US Health, 1990-2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444-1472. 10.1001/jama.2018.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Marinho F, de Azeredo Passos VM, Carvalho Malta D, et al. ; GBD 2016 Brazil Collaborators . Burden of disease in Brazil, 1990-2016: a systematic subnational analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10149):760-775. 10.1016/S0140-6736(18)31221-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Newton JN, Briggs ADM, Murray CJL, et al. Changes in health in England, with analysis by English regions and areas of deprivation, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(10010):2257-2274. 10.1016/S0140-6736(15)00195-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fullman N, Yearwood J, Abay SM, et al. ; GBD 2016 Healthcare Access and Quality Collaborators . Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. 2018;391(10136):2236-2271. 10.1016/S0140-6736(18)30994-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lim SS, Updike RL, Kaldjian AS, et al. Measuring human capital: a systematic analysis of 195 countries and territories, 1990-2016. Lancet. 2018;392(10154):1217-1234. 10.1016/S0140-6736(18)31941-X 10.1016/S0140-6736(18)31941-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Institute for Health Metrics and Evaluation Disease Expenditure (DEX). Last accessed December 19, 2018 from http://www.healthdata.org/dex.
- 30. Bui AL, Dieleman JL, Hamavid H, et al. Spending on Children’s Personal Health Care in the United States, 1996-2013. JAMA Pediatr. 2017;171(2):181-189. 10.1001/jamapediatrics.2016.4086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Squires E, Duber H, Campbell M, et al. Health Care Spending on Diabetes in the U.S., 1996-2013. Diabetes Care. 2018;41(7):1423-1431. 10.2337/dc17-1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dieleman JL, Squires E, Bui AL, et al. Factors associated with increases in US health care spending, 1996-2013. JAMA. 2017;318(17):1668-1678. 10.1001/jama.2017.15927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hamavid H, Birger M, Bulchis AG, et al. Assessing the complex and evolving relationship between charges and payments in US hospitals: 1996 -2012. PLoS One. 2016;11(7):e0157912. 10.1371/journal.pone.0157912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Osgood-Zimmerman A, Millear AI, Stubbs RW, et al. Mapping child growth failure in Africa between 2000 and 2015. Nature. 2018;555(7694):41-47. 10.1038/nature25760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Graetz N, Friedman J, Osgood-Zimmerman A, et al. Mapping local variation in educational attainment across Africa. Nature. 2018;555(7694):48-53. 10.1038/nature25761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Reiner RC Jr, Graetz N, Casey DC, et al. Variation in childhood diarrheal morbidity and mortality in Africa, 2000-2015. N Engl J Med. 2018;379(12):1128-1138. 10.1056/NEJMoa1716766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Golding N, Burstein R, Longbottom J, et al. Mapping under-5 and neonatal mortality in Africa, 2000-15: a baseline analysis for the Sustainable Development Goals. Lancet. 2017;390(10108):2171-2182. 10.1016/S0140-6736(17)31758-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pigott DM, Deshpande A, Letourneau I, et al. Local, national, and regional viral haemorrhagic fever pandemic potential in Africa: a multistage analysis. Lancet. 2017;390(10113):2662-2672. 10.1016/S0140-6736(17)32092-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bhatt S, Weiss DJ, Cameron E, et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2015;526(7572):207-211. 10.1038/nature15535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dieleman JL, Sadat N, Chang AY, et al. ; Global Burden of Disease Health Financing Collaborator Network . Trends in future health financing and coverage: future health spending and universal health coverage in 188 countries, 2016-40. Lancet. 2018;391(10132):1783-1798. 10.1016/S0140-6736(18)30697-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. Inequalities in life expectancy among US counties, 1980 to 2014: temporal trends and key drivers. JAMA Intern Med. 2017;177(7):1003-1011. 10.1001/jamainternmed.2017.0918 [DOI] [PMC free article] [PubMed] [Google Scholar]