Abstract
The Research Centers in Minority Institutions (RCMI) program was established by the US Congress to support the development of biomedical research infrastructure at minority-serving institutions granting doctoral degrees in the health professions or in a health-related science. RCMI institutions also conduct research on diseases that disproportionately affect racial and ethnic minorities (ie, African Americans/Blacks, American Indians and Alaska Natives, Hispanics, Native Hawaiians and Other Pacific Islanders), those of low socioeconomic status, and rural persons. Quantitative metrics, including the numbers of doctoral science degrees granted to underrepresented students, NIH peer-reviewed research funding, peer-reviewed publications, and numbers of racial and ethnic minorities participating in sponsored research, demonstrate that RCMI grantee institutions have made substantial progress toward the intent of the Congressional legislation, as well as the NIH/NIMHD-linked goals of addressing workforce diversity and health disparities. Despite this progress, nationally, many challenges remain, including persistent disparities in research and career development awards to minority investigators. The continuing underrepresentation of minority investigators in NIH-sponsored research across multiple disease areas is of concern, in the face of unrelenting national health inequities. With the collaborative network support by the RCMI Translational Research Network (RTRN), the RCMI community is uniquely positioned to address these challenges through its community engagement and strategic partnerships with non-RCMI institutions. Funding agencies can play an important role by incentivizing such collaborations, and incorporating metrics for research funding that address underrepresented populations, workforce diversity and health equity.
Keywords: Minority-serving Institutions, Underrepresented, Health Inequities, Workforce Diversity
In Memoriam
In loving memory of Mrs. Cassandra Denise Jackson, Program Manager, RCMI Translational Research Network at Morehouse School of Medicine (May 30, 1962 - August 8, 2018).
Introduction
The Department of Health and Human Services (DHHS) action plan to reduce racial and ethnic health disparities emphasizes the importance of a diverse workforce.1 A growing field of investigation has unveiled the potential of a diverse workforce to improve health care access, increase patient satisfaction, and ensure culturally competent care by adequately addressing social determinants that impact health during medical interactions with patients.2 The central role of the Research Centers in Minority Institutions (RCMI) consortium in addressing National Institutes of Health (NIH)-linked objectives of a diverse workforce and health equity was highlighted in three keynote presentations delivered at the RCMI Translational Science 2017 Conference in Washington, DC. During the opening plenary keynote, NIH Director Dr. Francis S. Collins, stated, “we look to the RCMI community as the brain trust to help develop novel solutions on health disparities”.3 During his plenary address, Dr. Eliseo Pérez-Stable, director of the National Institute on Minority Health and Health Disparities (NIMHD), underscored the importance of addressing the levels of influence from the individual to the societal level, across the various domains of influence from the biological to the sociocultural environment and indeed beyond, to the health care system.4 At the closing plenary, Dr. Lawrence A. Tabak, NIH principal deputy director, called attention to the importance of RCMI grantee institutions in the nation’s biomedical research and workforce diversity, stating, “everything about RCMI is embedded in the strategic plan of NIH”.5
This article presents data on the impact of the RCMI program and the RCMI Translational Research Network (RTRN). The historical context of the RCMI program and its impact on NIH priorities is relevant to the network’s value as a strategic partner in addressing current challenges in workforce diversity and health equity.
History of the RCMI Program
The RCMI program was established in 1985 in response to committee report language (House Report 98-911) attached to H.R. 6028, the Departments of Labor, Health and Human Services, and Education and Related Agencies Appropriation Act, 1985, to “establish research centers in those predominantly minority institutions which offer doctoral degrees in the health professions or the sciences related to health.”6 Subsequent legislation (H.R. 3010) upheld and further recognized the critical role played by the RCMI program and encouraged NIH to strengthen participation from minority institutions and resources available for this area.
Through the original legislation that established the RCMI program in 1985, NIH moved to strengthen the research environment in predominantly minority institutions by providing funds to: “1) develop and enhance the institutional research infrastructure necessary for the conduct of biomedical and/or behavioral research; 2) enable minority institutions to become more successful in obtaining competitive extramural support for the conduct of biomedical and/or behavioral research; and 3) enhance the biomedical research environment at these institutions.” To accomplish this, at least two-thirds of the requested funds were expected to be directed to build multi-user resources, rather than to support individual research projects. Thus, research infrastructure is central to the legislative intent of the RCMI program.
Design of the RCMI Program
RCMI Research Infrastructure and Research Development
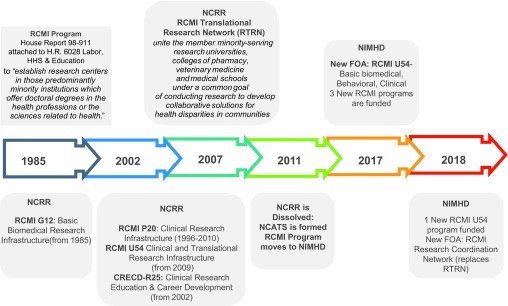
The National Center for Research Resources (NCRR) at NIH served as the administrative home of the RCMI program, which evolved from its initial focus on providing infrastructure solely for basic biomedical research. In the mid-1990s, the focus was expanded to include the development of infrastructure to increase research capacity for clinical research, and in 2002-2003 infrastructure for community-based research. The RCMI program at NCRR also administered a trans-NIH-funded Clinical Research Education and Career Development (CRECD) program supported through an R25 mechanism. (Figure 1 shows the timeline and mechanisms of RCMI funding. Regardless of the mechanism, all RCMI awards were competitively funded to support infrastructure and research development. Each RCMI-funded Center and the RCMI Network (RTRN) have independent external advisory board members, most of whom are from non-RCMI institutions.
Figure 1. The Research Centers in Minority Institutions (RCMI) programa.
a. Established by the US Congress to take a “critical role in addressing the health research and training needs of minority populations.”
NCRR, National Center for Research Resources; NIMHD, National Institute on Minority Health and Health Disparities; NCATS, National Center for Advancing Translational Science; RCMI, Research Centers in Minority Institutions.
The RCMI Translational Research Network (RTRN) was established in 2007 to enhance collaboration across RCMI grantee institutions. The network is designed to engage all RCMI stakeholders, increase the quality and efficiency of basic biomedical, behavioral, and clinical research, facilitate study participant recruitment and retention, and increase the efficiency of the implementation and dissemination of research advances to improve health outcomes among minority and health disparity populations.
In 2011, NCRR was abolished, as part of an NIH reorganization to create the National Center for Advancing Translational Sciences (NCATS). Several of the NCRR programs were reassigned to other NIH institutes. At that time, the overall RCMI Program was transferred to NIMHD, where it has since remained. Starting in 2017, NIMHD began a transition of the various RCMI funding mechanisms to a single U54 program (Figure 1).
RCMI Translational Research Network (RTRN): A Collaboration Framework for Multi-site Research and Investigator Development
Since its establishment in 2007, RTRN has served to unite the member minority-serving research universities, colleges of pharmacy and veterinary medicine and medical schools under a common goal of conducting research to develop collaborative solutions for health disparities in communities impacted by high disease burden and poor access to health care. RTRN leverages the scientific expertise, technologies and innovations of its RCMI minority-serving research institutions to accelerate the delivery of solutions to address critical health problems, particularly health disparities.7,8
The network is governed by a steering committee, which has representation from RCMI and non-RCMI grantee institutions, industry collaborators, and community partners. The steering committee develops and ratifies policies for network activities, such as data sharing and IRB harmonization. The Network has six steering subcommittees, which are responsible for optimizing resource utilization: Education and Dissemination; Ethics and Regulatory; Protocol Review; Publications and Presentations; Core Resources; and Community Engagement.
The Network’s Infrastructure Supports Investigator Development, Research Implementation and Data Coordinating Functions
The Network’s ability to support translational science – from laboratory research to clinical research and from clinical research to the community and public health practice – hinges around the implementation of the translational research cluster (TRC) system. This system comprises 10 clusters, based on disease and cross-cutting scientific focus areas that include: Cancer; Cardiovascular and Related Diseases; Community Engagement; Genes & Environmental Health/Toxicology; HIV/AIDS; Infectious & Immunologic Diseases; Informatics; Neurologic Disorders & Mental Health; Obesity & Metabolic Syndromes; Child Health; Women’s Health & Reproductive Biology. The clusters are embedded within cyber workspaces, where clinical, biomedical and behavioral researchers meet monthly to collaboratively develop concepts into research projects. RCMI investigators also compete for small research grant/pilot research awards to support inter-institutional collaborative research.8
The RTRN enables multi-site clinical and behavioral health research through: 1) training in good clinical practice (GCP), including regulatory compliance and single IRB implementation to support multi-site research studies; 2) clinical research study management, including best practices for the facilitation, coordination, financial/budgeting, project management and other administrative processes regarding clinical trials; 3) supporting participant recruitment with informatics tools, such as i2b2 (Informatics for Integrating Biology and the Bedside).9 Network-supported projects and investigators receive: support for biostatistics; clinical data management and data safety monitoring; project management and communication; research data management from the Data Coordinating Center at Jackson State University.
The Challenge of Achieving Diversity in the Biomedical Research Workforce
The NIH has long recognized that achieving diversity in the biomedical and behavioral research workforce is critical to ensuring that the best and brightest minds have the opportunity to contribute to the achievement of our national research goals. Despite long-standing efforts from the NIH and other entities across the biomedical and behavioral research landscape to increase the number of scientists from underrepresented groups, investigator diversity still falls far short of mirroring that of the US population.10,11
Additionally, a disturbing discrepancy in success rates for research grant (R01) applications between White and Black applicants, even after controlling for numerous observable variables, was reported in 2011 by Ginther and colleagues.11 Marked differences in funding success were also observed depending upon the institution from which an applicant submitted their application. Applications from the 30 most highly NIH-funded institutions had a higher probability of funding than those from institutions ranked 31 to 200. In turn, applications from the 31 to 200 institutions were more likely to be funded than those from institutions ranked 201 and beyond. In all groups, a disparity was observed for Black applicants relative to majority applicants in the same rank group. Subsequently, to address this unacceptable status quo on minority underrepresentation in biomedical and behavioral research and other challenges cited by the Working Group on Diversity in the Biomedical Research Workforce (WGDBRW), NIH funded the Diversity Program Consortium (DPC) in 2014. This consortium includes three programs: Building Infrastructure Leading to Diversity (BUILD);12 National Research Mentoring Network (NRMN);13 and Coordination and Evaluation Center (CEC).14
The RTRN Responds: Collecting Impact Data
Given that the RTRN addresses many of the areas of concern raised by the WGDBRW and has much to offer the BUILD, NRMN, and CEC endeavors, the RTRN and RCMI site lead investigators convened to review their collective experience as a network addressing the science of health disparities and research that provided evidence for the benefits of multi-site research,15-22 meaningful inclusion of diverse populations in research studies,23,24 training,25-27 and coaching models to advance the careers of underrepresented early stage investigators.28
During RTRN-convened meetings of RCMI, principal investigators and program directors agreed on the process and timeline for data collection to support research publications and dissemination. Meetings included regularly scheduled monthly meetings, as well as a full-day leadership research retreat. A standardized data survey was electronically administered to all 18 institutions with active RCMI awards in 2016 (Table 1); all 18 institutions participated in the survey. Total funding and funding periods for RCMI programs, including G12 RCMI, U54 RCTR and R25 CRECD, were obtained from the NIH RePORTER database.
Table 1. RCMI institutions that contributed workforce and research participant data.
| Charles R. Drew University, Los Angeles, CA | Ponce Health Sciences University, Ponce, PR |
| City College of New York, New York, NY | Texas Southern University, Houston, TX |
| Clark Atlanta University, Atlanta, GA | Tuskegee University, Tuskegee, AL |
| Florida Agricultural & Mechanical University, Tallahassee, FL | Universidad Central del Caribe, Bayamón, PR |
| Howard University, Washington, DC | University of Hawaii at Manoa, Honolulu, HI |
| Hunter College, CUNY, New York, NY | University of Puerto Rico Medical Sciences, San Juan, PR |
| Jackson State University, Jackson, MS | University of Texas at El Paso, TX |
| Meharry Medical College, Nashville, TN | University of Texas at San Antonio TX |
| Morehouse School of Medicine, Atlanta, GA | Xavier University of Louisiana, New Orleans, LA |
In addition, RCMI-funded programs provided reports on other funding (from government, foundation, industry, etc.) leveraged by RCMI-funded programs, clinical and translational research scholars trained, research participants enrolled in protocols, and patents awarded. We used progress reports submitted to NIH for funding renewal and publications citing RCMI funding from PubMed Central. Data were collected for 2000–2015.
Impact of the RCMI Centers and RTRN on Collaboration and Scientific Discovery
RCMI Collaborative Authorship was quantified using the Profiles Research Networking Software (Profiles RNS), which is an NIH-funded open-source tool to identify researchers with specific areas of expertise for collaboration and professional networking. Built-in network analysis and data visualization tools show connections and what factors influence collaborations. RTRN implemented Profiles RNS in collaboration with the Harvard Catalyst Clinical and Translational Science Award (CTSA). RTRN also implemented the eagle-i resource discovery tool. Profiles RNS and eagle-i resources support research collaboration.
Analysis of collaborative authorship revealed increased connections after RTRN, compared with before RTRN. Inter-institutional co-authorship data showed increased collaboration and co-authorship across the Network. From a baseline of 157 authors and 282 connections, during 2000 to 2007 (before RTRN), co-authorship increased to 421 authors and 1,294 connections from 2007 to 2018 (after RTRN). Thus, RTRN enabled less-siloed science, as demonstrated by more connections and co-authorships.
RCMI Impact on Discovery Science: Research Funding, Publications, Patents and Return on Investment
Based on data from 18 institutions funded between 2000 and 2015, RCMI investigators leveraged $805 million in RCMI program funds into $3.7 billion in additional awards, including 1,643 R01 (or equivalent) awards. The impact of RCMI discoveries is documented in 14,672 publications over the same time period; 2,562 publications have multiple citations. There were more than 500 patent disclosures over the same time period.
RCMI Impact on Doctoral Science and Doctoral Health Professions Workforce Diversity
A total of 22,227 science and health professions doctoral degrees were awarded by 18 RCMI institutions between 2000 and 2015, including 3,570 PhD, 9,417 MD, 6,242 PharmD, 812 DVM, and 2,186 DMD. (Table 2) Based on 2002 and 2012 data from the National Science Foundation,29 the 18 RCMI grantee institutions contributed almost 1 in 4 science doctoral degrees and 1 in 4 health professions doctoral degrees awarded to African Americans and Hispanics each year, in 2002 and 2012.
Table 2. Number of science doctoral degrees and health professions doctoral degrees awarded, by race/ethnicity from 18 RCMI grantee institutions (2000–2015)a.
| Race/ethnicity | Science doctoral degrees | Health professions doctoral degrees |
| African American/Black | 924 (25.9%) | 7,594 (40.7%) |
| Hispanic | 885 (24.8%) | 5,785 (31.0%) |
| American Indian/Alaska Native | - | - |
| Asianb | 548 (15.3%) | 2,566 (13.8%) |
| White | 915 (25.6%) | 1,230 (6.6%) |
| Other (multi-racial/bi-racial) | 298 (8.3%) | 1,482 (7.9%) |
| Total | 3,570 | 18,657 |
a. New RCMI Institutions (since 2017 and 2018), did not contribute data: Florida International University, Miami, FL; North Carolina Central University, Durham, NC; Northern Arizona University, Flagstaff, AZ; San Diego State University, CA.
b. Asian includes Native Hawaiian/Pacific Islanders.
RCMI Collaborative Impact: Supporting Biomedical Research
With funding from the NIH DPC, the RCMI RTRN supported the Research Resources and Outreach Core of the NRMN to recruit diverse early stage investigators across RCMI and non-RCMI institutions. Scholars participated in an innovative grant writing, coaching and mentoring program, called Strategic Empowerment Tailored for Health Equity Investigators (SETH). RCMI and CTSA principal investigators served as advisors and helped to recruit early-stage investigators (ESI). Between 2016 and 2017, SETH trained 113 ESIs in four different cohorts. Two cohorts participated in the Health Equity Collaboratory (EQ-Collaboratory) Virtual learning environment. ESI cohorts that had access to the Collaboratory (post-Collaboratory) were 4.8 times more likely to submit grant applications following grant writing/coaching training, compared with the ESI cohorts that did not have access to the Collaboratory (pre-Collaboratory). In all, regardless of cohort, the 113 ESI trainees submitted 78 total grants; 50% of trainees submitted at least 1 grant and 26% were awarded. Most (93%) of awards went to under-represented groups (URGs); 73% of awards went to RCMI investigators. 28
This model will support future RCMI-sponsored research development, in collaboration with NIH-funded programs, such as CTSAs.30
RCMI Impact: Clinical Research Centers
To report impact on clinical research centers, we obtained data from the following RCMI Clinical Research Centers at RCMI grantee institutions with medical schools/health systems and active U54 awards between 2008 and 2016: Charles R. Drew University; Howard University; Meharry Medical College; Morehouse School of Medicine; Puerto Rico Clinical and Translational Research Consortium (a partnership of three medical school/health science institutions in Puerto Rico); and University of Hawaii at Manoa.
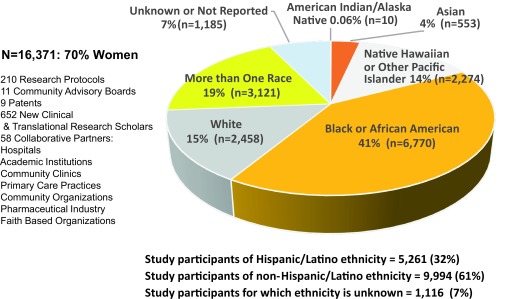
Competitive NIH National Center for Research Resources (NCRR) funding of the RCMI Clinical Research Infrastructure Initiative expanded the capacity of these RCMI institutions to conduct clinical research and training (Figure 1). Between 2008 and 2016, these centers collectively enrolled 16,371 diverse research participants. Participants included 70% women; 41% Black or African American; 32% Hispanic; 14% Native Hawaiian; 15% White; 3% Asian and 1% Native American/Alaska Native. The RCMI Clinical Research Centers (CRCs) supported the training and career development of 652 new clinical and translational research scholars over the same time period. Nine patents, 58 collaborative partners, and 11 community advisory boards illustrate the effectiveness of the unique approach to partnerships and community engagement across RCMI institutions (Figure 2), while also demonstrating the significance and impact of RCMI institutions in addressing the interconnected goals of workforce diversity and health equity research. Of additional importance, the funding base of $157,994,808 over nine years across all RCMI clinical research centers resulted in an additional $248,623,524, in extramural funding, for a return on investment (ROI) of 57.4% based on invested research dollars.
Figure 2. RCMI Clinical Research Centers: Study participants enrolled by race/ethnicity (2008-2016).
Discussion
The RCMI program continues to substantially impact the diversity of the nation’s biomedical research workforce while improving the health of minority communities and advancing knowledge in the science of health disparities. RCMI researchers are using advanced technologies to support collaborations that address cancer, cardiovascular diseases, HIV/AIDS, neurologic disorders, child health, environmental health, and many other health problems plaguing underserved and underrepresented populations at disproportionately high rates.
RCMI funding support has helped awardee institutions make progress toward the Congressional-legislated goals and has been critical to developing and enhancing the research environment and competitiveness at these institutions. The RCMI program enables these institutions to become competitive in obtaining support to conduct biomedical, clinical, and/or behavioral research that is relevant to health disparities and the health of the nation. RCMI serves as a national resource for workforce diversity by playing a crucial role in the recently launched BUILD and NRMN, NIH’s initiative on Diversity and Inclusion. RTRN is uniquely fostering team science across translational research among scientists in the network.
RTRN and RCMI are a substantial resource to NIH’s strategic framework on health disparities, diversity and inclusion in the biomedical workforce. Continuing investment in the RCMI program, including its basic biomedical, clinical and behavioral health research infrastructure, is crucial to sustaining productivity.
Funding agencies, such as NIH, can play an important role in sustaining the network by incentivizing collaborations between RCMI and non-RCMI NIH funded programs. For example, when NCRR launched CTSAs, research intensive institutions that submitted collaborative applications with RCMI partners, were more competitively reviewed for funding. Similarly, NIH and other sponsors can incentivize and promote diversity by incorporating metrics for new and competing renewal of research awards, including meaningful inclusion of underrepresented populations in research, as well as recruitment and training of diverse scientists on research teams.
Conclusion and Future Directions
The RCMI program has demonstrated a track record in addressing health disparities research, along with diversity and inclusion in the biomedical research workforce. RCMI investigators and institutions are uniquely positioned to address the national challenges of underrepresentation and persistent health inequities through community engagement and strategic partnerships with non-RCMI institutions. Funding agencies, like the National Heart Lung and Blood Institute (NHLBI), The National Institute of General Medical Sciences (NIGMS), National Cancer Institute (NCI), National Institute of Allergy and Infectious Diseases (NIAID), National Center for Advancing Translational Sciences (NCATS), National Institute of Neurological Disorders and Stroke (NINDS), can play an important role by supporting such collaborations. In order to advance health equity, metrics for research funding should include underrepresented populations and workforce diversity.
The RCMI consortium partners include health systems implementing innovative payment models, such as Accountable Care Organizations (ACO),31 and population health resources such as illness registries or specimen banks.32 RTRN is coordinating efforts to leverage these population health resources by deploying informatics tools such as i2b2,9 that will support data science initiatives, and accelerate research on the science of health disparities.33
Acknowledgments
Grant Funding: This research was funded by the National Institute on Minority Health and Health Disparities: U54MD008149, 8U54MD007588, and U54MD008173; National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002378; Grant funding to RCMI Centers: 2U54MD007602, U54MD007587, 5G12MD007579, 5U54MD007600, G12 MD007582, 2U54 MD007586, 5U54MD007593, U54MD012393, U54MD012388, 3G12MD007603, 3G12MD007599, G12MD007581, 5G12MD007592, U54MD007584, 5G12MD007597, 5G12MD007597, G12MD007590, 5U54MD007585, 3G12MD007591, 5U54MD012392, 1U54MD012397,5G12MD007605, CDU54AXIS5U54MD007598, 5U54MD007601, 5U54MD007585-25.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health
We would like to thank the principal investigators and staff of the RCMI Research Centers, RCMI Institutions, RCMI Translational Research Network, and the RTRN Data Coordinating Center at Jackson State University for supporting the data collection process. We acknowledge the tremendous support from each RCMI Center’s External Advisory Board. We are especially grateful to the External Advisory Board members of the RCMI Translational Research Network: Lee M. Nadler, MD, Co-Chair, PI, Harvard Catalyst (CTSA), Harvard Medical School; Linda Barry, MD, MPH Co-Chair, Director of Multicultural and Community Affairs, University of Connecticut School of Medicine; Henry Kautz, PhD, Robin & Tim Wentworth Director of the Goergen Institute for Data Science; Melva Thompson-Robinson, DrPH, Department of Health Promotion, University of Nevada, Las Vegas; Dan M. Cooper, MD, PI University of California, Irvine CTSA; Bert Boyer, PhD, Oregon Health Sciences University, Alaska Native Health & Developmental Research; Luis Abreu-Garcia, PharmD, Director Medical Affairs, Pfizer Inc. Pharmaceutical Research; Chul Ahn, PhD, Director of Biostatistics, Epidemiology and Research Design, CTSA-University of Texas Southwestern Medical Center; Uma Sundaram, MD, Director, Edwards Comprehensive Cancer Center, Joan C. Edwards School of Medicine, Marshall University.
RCMI Investigators and RTRN Team Members
Charles R. Drew University: Jaydutt Vadgama, PhD
City College of New York: Mark Pezzano, PhD
Clark Atlanta University: Shafiq Kahn, PhD
Florida Agriculture and Mechanical University: Karam Soliman, PhD; Carl Goodman, PhD
Florida International University: Eric F. Wagner, PhD
Howard University: William Southerland, PhD
Hunter College: Jesus Angulo, PhD
Jackson State University and the RTRN Data Coordinating Center: Paul Tchounwou, PhD; Solomon Garner, PhD; Traci Hayes, MBA, DrPH; Jae Lee, DrPH; Mohamad Malouhi, BE; M. Edwina Barnett, MD, PhD, MBA; Alnida Ngare, MHSA; Andrew Dent, II, MS; Mohamad Malouhi, BE; Muna Abdelrahim, MMIS
Meharry Medical College: Maria F. Lima, PhD, Samuel Adunyah, PhD; Josiah Ochieng, PhD; James E. Hildreth, MD, PhD
Morehouse School of Medicine: Elizabeth Ofili, MD, MPH; Almelida Baker, MPH; Nicole Crowell, MS, Latrice Rollins, PhD; Vincent Bond, PhD; Tabia Akintobi, PhD; Marilyn Forman, MD; Sandra Harris-Hooker, PhD, Valerie Montgomery Rice, MD
North Carolina Central University: Deepak Kumar, PhD
Northern Arizona University: Julie A. Baldwin, PhD; Diane Stearns, PhD
Nova Southeastern University: Daniel E. Dawes, JD
Ponce School of Medicine: Richard J. Noel, Jr., Jose A. Torres-Ruiz, PhD
San Diego State University: Kristen J. Wells, PhD, Guadalupe X. Ayala, PhD
Universidad Centrale Del Caribe: Misty Eaton, PhD, Eddie Rios-Olivares, PhD
University of Hawaii at Manoa: Richard Yanagihara, MD, MPH; Jerris R Hedges, MD; Noreen Mokuau, DSW; Bruce Shiramizu, MD; Marla J Berry, PhD; Sandra P. Chang, PhD; Debra Taira, Sc.D.; Angela Sy, DrPH; Brenda Y. Hernandez, PhD; Pamela L. Bullard, BA
University of Puerto Rico Medical Sciences Campus: Emma Fernández-Repollet; Marcia Cruz-Correa, MD, PhD; Carlos A. Luciano, MD
University of Texas El Paso: Robert A. Kirken, PhD
University of Texas San Antonio: George Perry, PhD; Floyd Wormley, Jr., PhD
Texas Southern University: Adebayo Oyekan, PhD
Tuskegee University: Clayton Yates, PhD; Stephen Sodeke, PhD; Temesgen Samuel, DVM, PhD
University of California Los Angeles: Keith C. Norris, MD
Xavier University of Louisiana: Gene D’Amour, PhD; Daniel Sarpong, PhD; Guangdi Wang, PhD
References
- 1. US Dept. of Health and Human Services, Office of the Secretary, Office of the Assistant Secretary for Planning and Evaluation and Office of Minority Health. HHS Action Plan to Reduce Racial and Ethnic Health Disparities Implementation Progress Report. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation; 2015. [Google Scholar]
- 2. Jackson CS, Gracia JN. Addressing health and health-care disparities: the role of a diverse workforce and the social determinants of health. Public Health Rep. 2014;129(1_suppl2)(suppl 2):57-61. 10.1177/00333549141291S211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Collins F. NIH Research Agenda: How the RCMI Program Contributes. Opening Plenary Keynote Presentation. Delivered at the RCMI Translational Science 2017: Innovate, Translate, Collaborate, Engage, Community; October 30, 2017.
- 4. Perez-Stable E. NIMHD Research Agenda: How the RCMI Program Contributes. Keynote Presentation. Delivered at the RCMI Translational Science 2017: Innovate, Translate, Collaborate, Engage, Community; October 30, 2017
- 5. Tabak L. NIH Research and Workforce Agenda: How the RCMI Program Contributes. Closing Plenary Keynote Presentation. Delivered at the RCMI Translational Science 2017: Innovate, Translate, Collaborate, Engage, Community October 30, 2017.
- 6.HR 6028, July 26, 1984. The Research Centers in Minority Institutions (RCMI) program was established in 1985 in response to committee report language (House Report 98-911) attached to H.R. 6028, the Departments of Labor, Health and Human Services, and Education and Related Agencies Appropriation Act, 1985.
- 7. Fleming E, Perkins J, Easa D, Conde J, Baker R, Southerland W, Dottin R, Benabe J, Ofili E, Bond V, McClure S, Sayre M, Beanan M, Norris K. The role of translational research in addressing health disparities: a conceptual rramework. Ethn Dis. 2008;18(2 Suppl 2):S2-155-160. PMCID: PMC2705204 [PMC free article] [PubMed]
- 8. Fleming ES, Perkins J, Easa D, Conde J, Baker R, Southerland W, Dottin R, Benabe J, Ofili E, Bond V, McClure S, Sayre M, Beanan M, Norris K. addressing health disparities through multi-institutional, multidisciplinary collaboratories. Ethn Dis. 2008;18(2 Suppl 2):S2-161-167. [PMC free article] [PubMed]
- 9. Mandl KD, Kohane IS, McFadden D, et al. Scalable Collaborative Infrastructure for a Learning Healthcare System (SCILHS): architecture. J Am Med Inform Assoc. 2014;21(4):615-620. 10.1136/amiajnl-2014-002727 10.1136/amiajnl-2014-002727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Working Group on Diversity in the Biomedical Research Workforce Draft Report of the Advisory Committee to the Director Working Group on Diversity in the Biomedical Research Workforce. June 13, 2012. Last accessed January 16, 2019 from https://acd.od.nih.gov/documents/reports/DrsityBiomedicalResearchWorkforceReport.pdf
- 11. Ginther DK, Schaffer WT, Schnell J, et al. Race, ethnicity, and NIH research awards. Science. 2011;333(6045):1015-1019. 10.1126/science.1196783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Urizar GG Jr, Henriques L, Chun CA, et al. Advancing research opportunities and promoting pathways in graduate education: a systemic approach to BUILD training at California State University, Long Beach (CSULB). BMC Proc. 2017;11(S12)(suppl 12):26. 10.1186/s12919-017-0088-3 10.1186/s12919-017-0088-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sorkness CA, Pfund C, Ofili EO, et al. ; Duplicate Of Weber-Main; NRMN team . A new approach to mentoring for research careers: the National Research Mentoring Network. BMC Proc. 2017;11(S12)(suppl 12):22. 10.1186/s12919-017-0083-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McCreath HE, Norris KC, Calderόn NE, Purnell DL, Maccalla NMG, Seeman TE. Evaluating efforts to diversify the biomedical workforce: the role and function of the Coordination and Evaluation Center of the Diversity Program Consortium. BMC Proc. 2017;11(S12)(suppl 12):27. 10.1186/s12919-017-0087-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ferchmin PA, Andino M, Reyes Salaman R, et al. 4R-cembranoid protects against diisopropylfluorophosphate-mediated neurodegeneration. Neurotoxicology. 2014;44(44C):80-90. 10.1016/j.neuro.2014.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Martins D, Meng YX, Tareen N, et al. The effect of short term Vitamin D supplementation on the inflammatory and oxidative mediators of arterial stiffness. Health (Irvine Calif). 2014;6(12):1503-1511. 10.4236/health.2014.612185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rice VM, Maimbolwa MC, Nkandu EM, Hampton JF, Lee JE, Hildreth JEK. Cultural differences in acceptability of a vaginal microbicide: a comparison between potential users from Nashville, Tennessee, USA, and Kafue and Mumbwa, Zambia. HIV AIDS (Auckl). 2012;4:73-80. 10.2147/HIV.S25848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Thota C, Menon R, Fortunato SJ, Brou L, Lee JE, Al-Hendy A. 1,25-Dihydroxyvitamin D deficiency is associated with preterm birth in African American and Caucasian women. Reprod Sci. 2014;21(2):244-250. 10.1177/1933719113493513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Amaro-Rivera K, López-Cepero A, Diaz B, Lee JE, Palacios C. Micronutrient intake and the contribution of dietary supplements in Hispanic infants. J Diet Suppl. 2018;15(2):129-139. 10.1080/19390211.2017.1330300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Norris KC, Edwina Barnett M, Meng Y-X, et al. Rationale and design of a placebo controlled randomized trial to assess short term, high-dose oral cholecalciferol on select laboratory and genomic responses in African Americans with hypovitaminosis D. Contemp Clin Trials. 2018;72:20-25. 10.1016/j.cct.2018.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Banna J, Campos M, Gibby C, et al. Multi-site trial using short mobile messages (SMS) to improve infant weight in low-income minorities: Development, implementation, lessons learned and future applications. Contemp Clin Trials. 2017;62:56-60. 10.1016/j.cct.2017.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Palacios C, Campos M, Gibby C, Meléndez M, Lee JE, Banna J. Effect of a Multi-Site Trial using Short Message Service (SMS) on Infant Feeding Practices and Weight Gain in Low-Income Minorities. J Am Coll Nutr. 2018;37(7):605-613. 10.1080/07315724.2018.1454353 10.1080/07315724.2018.1454353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rollins L, Sy A, Crowell N, et al. Learning and Action in Community Health: Using the Health Belief Model to Assess and Educate African American Community Residents about Participation in Clinical Research. Int J Environ Res Public Health. 2018;15(9):E1862. 10.3390/ijerph15091862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ofili EO, Pemu PE, Quarshie A, et al. DEMOCRATIZING DISCOVERY HEALTH WITH N=Me. Trans Am Clin Climatol Assoc. 2018;129:215-234. [PMC free article] [PubMed] [Google Scholar]
- 25. Estape ES, Quarshie A, Segarra B, et al. Promoting diversity in the clinical and translational research workforce. J Natl Med Assoc. 2018;110(6):598-605. 10.1016/j.jnma.2018.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rubio DM, Mayowski CA, Norman MK. A Multi-Pronged Approach to Diversifying the Workforce. Int J Environ Res Public Health. 2018;15(10):2219. 10.3390/ijerph15102219 10.3390/ijerph15102219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Stephens DS, West AC, Ofili EO, Boyan BD, Blumberg HM. The Atlanta Clinical and Translational Science Institute: clinical and translational science education and training partnership. Clin Transl Sci. 2011;4(3):143-145. 10.1111/j.1752-8062.2011.00293.x 10.1111/j.1752-8062.2011.00293.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hall M, Engler J, Hemming J, et al. Using a Virtual Community (the Health Equity Learning Collaboratory) to Support Early-Stage Investigators Pursuing Grant Funding. Int J Environ Res Public Health. 2018;15(11):E2408. 10.3390/ijerph15112408 10.3390/ijerph15112408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Science Foundation Report on Science and Engineering Degrees, by Race/Ethnicity of Recipients: 2002–2012. Last accessed January 16, 2019 from http://www.nsf.gov/statistics/2015/nsf15321/#chp2
- 30. Ofili EO, Fair A, Norris K, et al. Models of interinstitutional partnerships between research intensive universities and minority serving institutions (MSI) across the Clinical Translational Science Award (CTSA) consortium. Clin Transl Sci. 2013;6(6):435-443. 10.1111/cts.12118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brown M, Ofili EO, Pemu PE, et al. Morehouse Choice Accountable Care Organization and Education System (MACO-ES): integrated model delivering equitable and quality care. Presented at RCMI Translational Science 2017: Innovate, Translate, Collaborate, Engage – Community October 30, 2017. Int J Environ Res Public Health. 2018. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ofili EO, Hutchinson B, Sogade F, et al. The Association of Black Cardiologists (ABC) Cardiovascular Disease Implementation Study (CVD-IS) to support care for underserved. Presented at the RCMI Translational Science 2017: Innovate, Translate, Collaborate, Engage, Community October 30, 2017. Int J Environ Res Public Health. 2018. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zhang X, Pérez-Stable EJ, Bourne PE, et al. Big data science: opportunities and challenges to address minority health and health disparities in the 21st century. Ethn Dis. 2017;27(2):95-106. 10.18865/ed.27.2.95 10.18865/ed.27.2.95 [DOI] [PMC free article] [PubMed] [Google Scholar]