Abstract
Myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS) is a syndrome of unknown etiology characterized by profound fatigue exacerbated by physical activity, also known as post-exertional malaise (PEM). Previously, we did not detect evidence of immune dysregulation or virus reactivation outside of PEM periods. Here we sought to determine whether cardiopulmonary exercise stress testing of ME/CFS patients could trigger such changes. ME/CFS patients (n = 14) and matched sedentary controls (n = 11) were subjected to cardiopulmonary exercise on 2 consecutive days and followed up to 7 days post-exercise, and longitudinal whole blood samples analyzed by RNA-seq. Although ME/CFS patients showed significant worsening of symptoms following exercise versus controls, with 8 of 14 ME/CFS patients showing reduced oxygen consumption () on day 2, transcriptome analysis yielded only 6 differentially expressed gene (DEG) candidates when comparing ME/CFS patients to controls across all time points. None of the DEGs were related to immune signaling, and no DEGs were found in ME/CFS patients before and after exercise. Virome composition (P = 0.746 by chi-square test) and number of viral reads (P = 0.098 by paired t-test) were not significantly associated with PEM. These observations do not support transcriptionally-mediated immune cell dysregulation or viral reactivation in ME/CFS patients during symptomatic PEM episodes.
Introduction
Myalgic encephalomyelitis/ chronic fatigue syndrome (ME/CFS) is characterized by long-term, debilitating fatigue that is characteristically exacerbated by physical and mental exertion [1,2]. Patients also typically experience impaired sleep, cognitive complaints, myalgia, arthralgia, headache, and other symptoms. Patients with ME/CFS have more unmet medical and home care needs and greater functional disability overall than those with other chronic disorders [3,4]. Post-exertional malaise (PEM) is a key symptom of ME/CFS and is described as a cluster of symptoms following mental or physical exertion, often involving a loss of physical or mental stamina, rapid muscle or cognitive fatigability, and sometimes lasting 24 hours or more [2]. These symptoms form the basis for a recent redefinition of the condition [1].
No specific cause for ME/CFS has been identified. Diagnosis of the syndrome based on symptoms and exclusion of other diseases in the absence of established biomarkers contributes to inconsistent clinical case definitions [5]. Working etiological hypotheses have included roles for viruses, bacteria, environmental triggers, immune dysregulation, mitochondrial dysfunction and disorders of oxidative metabolism [2,6,7]. Several lines of evidence point toward a role for disordered immunity or inflammation. These include disordered cytokine expression in serum [8] and cerebrospinal fluid [9], NK cell dysfunction [10] and promising response to early trials of B cell depletion [11]. Separately, these results suggest that irregularities in circulating immune cell subsets, and their gene expression, drive chonic autoimmune activation. Dysregulation of the immune response can also lead to increases in viral titers [12,13]. ME/CFS has been associated with reactivation of various viral infection [14]. Taken together these studies do not validate each other, but rather describe heterogeneous putative disease mechanisms [15].
RNA-seq can be leveraged to identify and count at once all transcripts and RNA genomes within a sample. This method has been used to discover host biomarkers and study molecular pathways involved in disease response [16], as well as for the identification of known and unsuspected infectious agents [17]. Using RNA-seq, we previously published data comparing gene expression profiles of patients with ME/CFS against a matched control group [18]. No differentially expressed genes and no differences in the blood virome were found to be associated with ME/CFS in the resting state. One 2014 review concluded that there may be altered immune responses to exercise in ME/CFS [19]. We launched the current study to provide an experimental approach to search for differential gene expression and changes in viral abundance induced by cardiopulmonary exercise testing (CPET) in association with the cardinal symptom of PEM. This approach also provides the benefit of allowing objective subtyping of patients according to exercise response phenotype [20].
Methods
Ethics, consent, and permissions
Our study protocol was approved by the Institutional Review Board at the University of British Columbia (Certificate # H14-01149). Potential subjects were recruited through postings to relevant newsletters and websites and information made available by participating physicians. Informed consent was obtained from all participants and/or their legal surrogates. Written informed consent included a full explanation of how the CPET regimen had been designed to provide an objectively measurable physiological stimulus to induce fatigue. Healthy people were matched with ME/CFS subjects by 5-year age stratum, ethnicity and gender. Patients were excluded from any group if they did not provide consent, were <18 years of age, were unable to understand English, or if they had another medical condition that accounted for their main symptoms. Any specific diagnosis that would exclude a person from a diagnosis of ME/CFS also excluded a healthy person from being recruited as a control. Because our sample size in this small pilot study was too small to address gender related differences, we recruited female cases and controls only.
Study cohort
We recruited female patients with ME/CFS (Canadian 2003 criteria) [21] and age- and gender-matched sedentary controls. Controls met the American College of Sport Medicine criteria for sedentary lifestyle, not participating in a regular exercise program nor accumulating 30 minutes or more of moderate physical activity on most days of the week [22]. After informed consent, subjects completed study questionnaires including demographics, history, SF 36 [23], Fatigue Severity Scale [24], a Functional Capacity Scale used widely by ME/CFS practitioners [25], Karnofsky [26], CESD [27], State Trait Anxiety Inventory (STAI) [28], Physical Activity Scale for the Elderly (PASE) [29] and the Pittsburgh Sleep Quality Index [30] and underwent a screening physical examination and screening laboratory tests. Important elements of the history included the acuity of onset of symptoms, duration of diagnosis of ME/CFS, history of a classical infectious illness at onset, and gender. Screening laboratories included tests for complete blood count (CBC), C-reactive protein (CRP); calcium, random glucose; lactate; magnesium; phosphate; sodium; potassium; chloride; total carbon dioxide level (CO2); urea; creatinine; total bilirubin; uric acid; alanine transaminase (ALT); aspartate transaminase (AST); creatine kinase (CK); gamma-glutamyl transferase (GGT); albumin; rheumatoid factor; thyroid stimulating hormone (TSH); ferritin; anti-nuclear antibody (ANA), total protein with protein electrophoresis; human immunodeficiency virus (HIV); hepatitis B virus (HBV); hepatitis C virus (HCV); syphilis; and two-tiered Lyme serology. A complete physical examination was conducted with a strong focus on musculoskeletal and neurological findings. All baseline data were reviewed to assure that case definitions were met.
Baseline accelerometry
Before enrollment, cases and controls wore a wGT3X-BT accelerometer (ActigraphCorp, Pensacola FL) on an elasticized belt around their waist for a period of five days, including one weekend. The device records human activity in three axes. Participants were asked to remove the device in order to shower or bathe but to wear it at all other times, including sleep periods. Parameters provided by the accelerometer report include: mean percent of time it was worn, total steps, percent of time spent in sedentary, light, moderate, vigorous and very vigorous activity, time in bed, time sleeping and number of awakenings.
Cardiopulmonary exercise testing
The protocol called for each subject to undergo two maximal cardiopulmonary exercise tests (CPET) approximately 24h apart. Subjects were fitted with electrocardiogram (ECG) electrodes for monitoring of heart rhythm, a mouthpiece and headgear for collection of expired air, and a pulse oximeter for monitoring arterial oxygen saturation. Subjects were allowed to pedal for a short period (less than one minute) prior to an incremental exercise test performed on an electronically braked bicycle ergometer (Lode Excalibur Sport, Lode BV, Groningen, the Netherlands). Workload was increased 15 watts per minute until volitional fatigue. ECG was monitored continuously for signs of cardiac arrhythmia or ischemia, and pulse oximetry was monitored to ensure safe levels of arterial oxygenation. Blood pressure was regularly monitored for patient safety. Expired respiratory gases were collected using a metabolic cart (Moxus System, AEI Technologies, Pittsburgh, PA) and minute ventilation (, L/min), oxygen consumption (, L/min or mL/min/kg), carbon dioxide production (, L/min), the respiratory exchange ratio (RER), and the ventilatory equivalents for oxygen (/() and carbon dioxide (/() were calculated. The ventilatory threshold was calculated using the V-slope method [31]. Subjects were encouraged to pedal as long as possible and testing was terminated when criteria for maximal effort were met (according to American College of Sports Medicine Guidelines or upon participant self-reported exhaustion). Subjects then remained seated on the ergometer through recovery for 10 minutes. Questionnaires on fatigue and other experienced symptoms were administered before each exercise test, within 15 minutes of completion of each test and at days 3 and 7 of follow-up.
Sample collection, preparation and sequencing
Study blood for total RNA was collected at day 1 and day 2 within 2 hours prior to each exercise test session, and during a home visit on day 3 and day 7. Each subject thus contributed 4 whole blood samples for RNA-seq analysis. Whole blood (2.5 mL) from cases and controls was drawn into a PAXgene Blood RNA Tube (Qiagen, Valencia, CA) to stabilize RNA prior to extraction and stored at -20°C. Total RNA was extracted at University of British Columbia using the PAXgene Blood RNA Kit (Qiagen, Valencia, CA) and all samples were lyophilized in RNAstable reagent (Biomatrica, San Diego, CA) for shipment at room temperature to University of California, San Francisco (UCSF) for further processing and long-term storage. The Ovation Human blood RNA-seq kit (Nugen, San Carlos, CA) was used to generate strand-specific RNA-seq libraries depleted for reads derived from rRNA (12S, 16S, 18S and 28S genes) and globin (HBA1, HBA2, HBB and HBD genes) according to the manufacturer’s protocol. The Ovation RNA-seq kit employs depletion of human RNA and globin transcripts, which can constitute up to 76% of mRNA in whole blood [32]; in our experience, up to a 4-fold increase in sensitivity for informative transcripts is observed using this kit. Briefly, 100ng of RNA extract, as measured by Qubit RNA high sensitivity kit (Thermo Fisher, South San Francisco), were treated with DNase according to the manufacturer’s instructions, and cDNA was prepared from extracted total RNA by reverse transcription using a mixture of random and poly(T) primers. Successive steps of end-repair, adaptor ligation, strand selection via nucleotide analog-targeted degradation, insert-dependent adaptor cleavage for targeted depletion of rRNA and globin reads, PCR amplification, and bead-based purification were then used to construct cDNA libraries for RNA-seq analysis. The 100 resulting libraries were assessed for quality using the Agilent Bioanalyzer DNA High Sensitivity Kit (Agilent, Santa Clara, CA) and sequenced as 100 base pair (bp) paired-end runs across 8 lanes on a HiSeq 2500 instrument (Illumina, San Diego, CA). No ERCC (External RNA Control Consortium) spike-ins were added to the libraries; however, no batch effect was apparent by principal component analysis (PCA).
Transcriptome analysis
Gene expression analysis was conducted using Partek Flow software (version 5.0). Paired-end reads were mapped to the human genome (hg38), annotated to exons, and normalized to FPKM (fragments per kilobase of exon per million fragments mapped) values for all 25,278 human RNA reference sequences in the National Center for Biotechnology Information (NCBI) RefSeq database (August 2016 build) using STAR v2.4.1 [33] and Cufflinks v2.2.1 [34]. Differential expression of genes was calculated using a multimodel approach (normal, lognormal, lognormal with shrinkage, negative binomial and Poisson distributions) in which the best model fit for each gene is chosen based on the Akaike information criterion corrected for small sample sizes [35]. Genes were considered to be differentially expressed when their fold change was > ± 1.5, p-value < 0.05, and adjusted p-value (or false discovery rate, FDR) < 0.1%.
Viral metagenomic analysis
Sequencing data from whole transcriptome libraries were analyzed for the presence of RNA sequences corresponding to known human viral pathogens using the sequence-based ultra-rapid pathogen identification (SURPI) computational pipeline [36]. After computationally subtracting human reads, remaining reads were aligned against all microbial sequences in the National Center for Biotechnology Information (NCBI) GenBank reference database. The SNAP aligner [37] was used at moderate stringency (edit distance = 12) to align reads to the NCBI nucleotide nt database, allowing for detection of reads with ≥90% nucleotide identity to known viruses, while RAPSearch [38] was used to detect divergent reads from potential novel viruses by translated nucleotide alignment to the NCBI protein nr database. A rapid taxonomic classification algorithm based on the lowest common ancestor was incorporated into SURPI, as previously described [39], and used to assign viral reads to the species, genus, or family level.
Clinical and epidemiological analysis
All clinical, laboratory and exercise data were anonymized to study number and stored securely in a common linked database at the University of British Columbia. Descriptive statistical tests were performed in R. To avoid the assumption that the data fit a fixed probability distribution, univariate analyses comparing groups were performed using non-parametric methods; a Fisher’s Exact Test was used for categorical variables and a Mann-Whitley rank sum test for continuous variables.
ME/CFS patients were classified according to whether or not they had a significant decline in performance on the second exercise test defined as ≥ 7% decrease in at either the peak or at the ventilatory threshold. CPET test results were provided to a group of investigators (SS, JS, MVN, CS) who were blinded as to case and control status in order to allow expert identification of a test-retest effect on repeat CPET.
Results
Study cohort
The CPET study screened 136 potential participants and enrolled a total of 25 subjects (14 cases, 11 controls). The potential participants who were not enrolled included those who were lost to follow-up (n = 2), withdrew from the study prior to exercise testing (n = 2), were unable to participate due to the lack of eligible age-matched controls or cases (n = 26), declined to participate (n = 40, many who wished to avoid triggering symptoms of exercise-induced PEM), or were ineligible according to Canadian Consensus Criteria because of the presence of an underlying illness precluding a diagnosis of ME/CFS (n = 41). Seven out of the fifteen ME/CFS subjects had also participated in a previous published study examining gene expression profiles in comparison to a matched control group [18]; however, the CPET study was a separate study with its own enrollment cohort.
Characteristics of our 14 cases and 11 matched controls are shown in Table 1. Patients were significantly matched to controls for age, gender and body mass index (p > 0.62). Cases had more defining symptoms and scored lower on disability scales than did controls (p < 0.01). Nine cases described a history of an infectious prodrome at disease onset, manifesting as an acute “flu-like illness” or gastroenteritis, while five described a sudden onset of ME/CFS. Baseline accelerometry revealed that sedentary controls trended toward logging more steps over a five-day period than did ME/CFS subject (Table 1), albeit not reaching statistical significance. However, the distribution of time spent on different levels of activity (sedentary, light, moderate and vigorous exercise) was similar between control and ME/CFS patients. While controls trended toward logging even more awakenings per night than cases, they slept more over a 24-hour cycle; these differences did not reach statistical significance.
Table 1. Characteristics of the study population.
| Variable | ME/CFS (n = 14) | Control (n = 11) | P Value |
|---|---|---|---|
| Age in years, median (IQR) | 49 (38, 58.3) | 50 (45.5, 58.5) | 0.6216 |
| BMI, median (IQR) | 26.63 (21.4, 34.9) | 26.45 (24.1, 35.2) | 0.7675 |
| Core Symptoms, n (%) | |||
| Fatigue | 14 (100) | 1 (9) | < .00001 |
| Pain | 14 (100) | 3 (27) | < .001 |
| Post Exertional Fatigue | 14 (100) | 1 (9) | < .00001 |
| Karnofsky Score Last 7 Days | 60 (56.25, 68.75) | 100 (90, 100) | < .0001 |
| Functional Capacity Last 7 Days | 4 (3, 5.75) | 8 (7.75, 8) | < .0001 |
| Illness Onset Pattern n (%) | |||
| Gradual | 9 (64) | NA | NA |
| Sudden | 5 (36) | NA | NA |
| History of Infection at Onset | 9 (64) | NA | NA |
| Illness duration yrs, median (IQR) | 5.75 (5, 7.5) | NA | NA |
| Baseline 5 Day Accelerometry, Median(IQR) | |||
| Wear Time (% of time) | 90.5 (89, 94) | 95 (93, 96) | 0.1958 |
| Steps in 5 Days | 28447(15722,33186) | 32995 (20940,50688) | 0.2671 |
| Activity Distribution (% of time) | |||
| Sedentary | 78.4 (71,81.5) | 74.5 (71.1,77.2) | 0.3111 |
| Light | 21.05 (18,26) | 22.8 (20.5,24.6) | 0.5719 |
| Moderate | 1.1 (0.3,2.1) | 1.3 (0.8,4.2) | 0.2612 |
| Vigorous | 0.0 (0, 0) | 0.0 (0, 0) | 0.8084 |
| Sleeping (Hours of Sleep Per 24 Hours) | 6.7 (5.9, 7.9) | 7.3 (6.2, 7.9) | 0.4593 |
| Awakenings (Per 24 Hours) | 5.8 (4.6,6.9) | 8.2 (5.3, 10) | 0.0708 |
Values are presented as median (IQR). P values were calculated with Wilcoxon rank-sum test. Statistically significant values (p < 0.05) were denoted in bold.
Cardiopulmonary exercise results
On day 2 of exercise testing, controls exercised for longer periods of time, achieved higher peak power output, and achieved higher peak than ME/CFS participants (Table 2). Heart rate and blood pressure responses were similar between the groups, while ME/CFS patients self-reported higher scores for perceived exertion. In comparing the second to the first day of exercise testing, those with ME/CFS were able to exercise for significantly less time while controls actually increased their exercise time on the second day (p = 0.0299).
Table 2. Cardiopulmonary exercise test parameters in CFS patients compared to controls on 2 consecutive days.
| Measure (unit) | Day 1 | Day 2† | Day 2 vs. Day 1 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Case (n = 14) |
Control (n = 11) |
P | Case (n = 12) |
Control (n = 10) |
P | Case (n = 12) |
Control (n = 10) |
P | |
| Exercise Time (s) | 467.0 (447.2, 579.8) | 556.0 (533.0, 618.5) | 0.1072 | 444.5 (418.2, 520.5) | 573.5 (535.8, 648.5) | 0.0161 | - 23.0 (-36.5, 2.0) | 13.0 (-4.5, 28.5) | 0.0479 |
| Peak Power Output (watts) | 120.0 (105.0, 146.2) | 135.0 (135.0, 165.0) | 0.0539 | 105.0 (105.0, 135.0) | 142.5 (135.0, 165.0) | 0.0188 | 0.0 (-15.0, 0.0) | 0.0 (0.0, 0.0) | 0.1151 |
| Metabolic Equivalent Units | 6.6 (5.9, 8.1) | 7.3 (5.5, 8.1) | 0.6443 | 6.1 (5.2, 7.3) | 7.1 (5.9, 7.7) | 0.2622 | -0.5 (-1.1, -0.1) | -0.1 (-0.4, 0.0) | 0.1964 |
| Peak Heart Rate (bpm) | 160.0 (143.5, 182.0) | 157.0 (153.5, 164.0) | 0.6606 | 153.5 (141.2, 170.0) | 160.0 (154.0, 162.0) | 0.4674 | -3.0 (-7.0, 1.5) | 1.0 (-2.8, 3.0) | 0.2595 |
| Peak Systolic Blood Pressure (mmHg) | 178.0 (160.0, 196.0) | 184.0 (171.0, 201.0) | 0.3379 | 177.0 (154.2, 193.0) | 185.0 (175.0, 191.5) | 0.3064 | -4.0 (-6.0, 12) | 6.0 (-4.0, 13.0) | 0.8321 |
| Peak Diastolic Blood Pressure (mmHg) | 88.0 (80.0, 94.0) | 86.0 (82.5, 91.5) | 0.8274 | 85.0 (79.0, 90.5) | 87.0 (84.0, 91.5) | 0.5491 | -2.0 (-2.0, 0.0) | 2.0 (-2.0, 4.0) | 0.3969 |
| Lowest Oxygen Saturation (%) | 96.0 (95.0, 98.0) | 96.0 (93.5, 96.5) | 0.3748 | 97.0 (95.5, 98.0) | 96 (94.3, 97.8) | 0.5212 | 0.0 (-1.5, 1.5) | 1.0 (-0.8, 2.5) | 0.6695 |
| Rate of Perceived Exertion* | 19.0 (19.0, 20.0) | 17.0 (14.5, 18.0) | 0.0145 | 19.0 (17.8, 20.0) | 17.0 (15.0, 19.0) | 0.0973 | 0.0 (-0.3, 0.3) | 0.5 (-1.5, 1.0) | 0.6829 |
| Minute Ventilation (L/min) | 64.1 (49.7, 78.9) | 79.2 (63.4, 83.5) | 0.1056 | 62.4 (54.9, 70.6) | 71.8 (64.1, 86.4) | 0.2030 | -0.9 (-6.1, 6.7) | -2.0 (-5.7, 2.6) | 0.4287 |
| Absolute Peak (mL/min) | 1557 (1474, 1795) | 1792 (1698, 1914) | 0.2066 | 1460 (1344, 1566) | 1679 (1646, 1846) | 0.0426 | -108.5 (-243.5, -18.5) | -30.5, (-73.0, 6.8) | 0.1562 |
| Relative Peak (mL/min/kg) | 23.2 (20.6, 28.3) | 25.6 (19.2, 28.2) | 0.8393 | 22.0 (18.1, 25.5) | 24.6 (20.7, 26.9) | 0.2543 | -1.6 (-3.8, -0.3) | -0.4 (-1.5, 0.1) | 0.1983 |
|
Relative at the Ventilatory Threshold (mL/min/kg) |
13.5 (7.3, 19.8) | 12.0 (9.5, 15.0) | 0.4761 | 14.5 (5.8, 20.3) | 11.5 (8.3, 14.8) | 0.6277 | 4.5 (-1.0, 6.0) | 1.5 (-1.0, 5.3) | 0.6425 |
| Absolute Peak (mL/min) | 1814 (1684, 2241) | 2171 (1880, 2270) | 0.2767 | 1688 (1566, 1832) | 2146 (1910, 2332) | 0.0249 | -164.5 (-292.8, -17.3) | 9.0 (-38.3, 46.3) | 0.1402 |
| Respiratory Exchange Ratio | 1.16 (1.04, 1.26) | 1.15 (1.12, 1.21) | 1 | 1.16 (1.11, 1.26) | 1.19 (1.14, 1.27) | 0.6918 | 0.02 (-0.01, 0.04) | 0.04 (-0.03, 0.08) | 0.7414 |
| Subjects with ≥7% decline in peak or at the ventilatory threshold day 2 vs day 1 | 8 | 4 | |||||||
| Test/Retest Effect** | 7 | 4 | |||||||
Values are presented as median (IQR). P values were calculated with Wilcoxon rank-sum test. Statistically significant values (p < 0.05) were denoted in bold.
†: Three subjects did not complete the second day of testing, two (1 case and 1 control) for safety reasons (high blood pressure response) and another (case) due to technical problems.
* Perceived effort measured by modified Borg scale
** Blinded expert reading of full spectrum of repeat CPET parameters indicated a test/retest effect.
Two subjects (one case and one control) successfully completed only one exercise test because systolic blood pressure was found to be high after testing. These subjects were retained for the gene expression analysis because follow-up confirmed the development of PEM for the patient with ME/CFS.
We identified eight ME/CFS subjects with a significant decline in performance from day 1 to day 2 based on a decrease in at either the peak or at the ventilatory threshold. Seven of these eight were also assigned a test-retest effect based on blinded expert review of full test data.
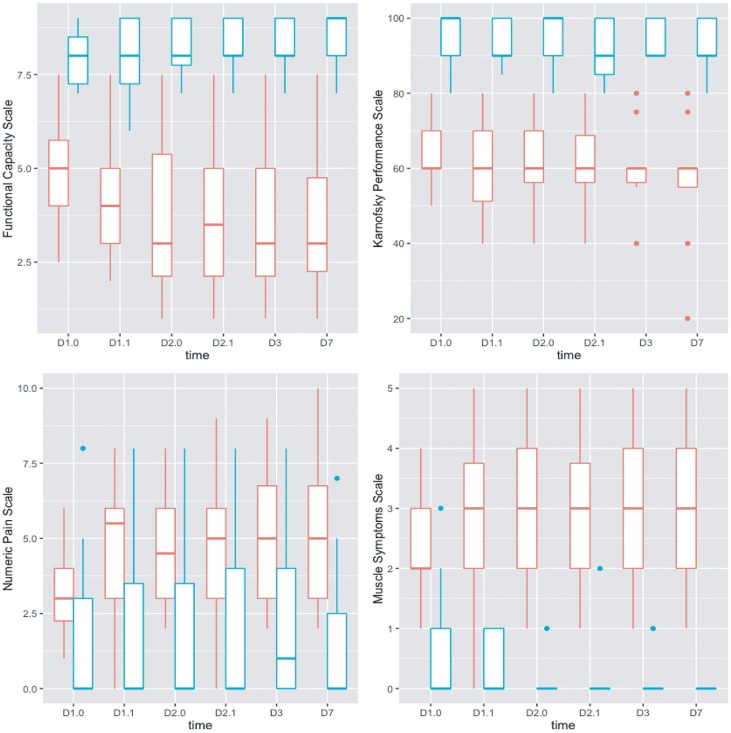
Participants with ME/CFS but not controls reported a worsening of symptoms following exercise that became maximal by day 3 or day 7 on most scales (Fig 1). This was most clear with a decrease in the Functional Capacity Scale and by increases in numeric pain and muscle symptom scores.
Fig 1. Change of numeric scales for functional scores, Karnofsky performance, pain and muscle symptoms over time.
CFS patients = red, matched controls = green. D1.0 and D2.0 indicate pre-exercise assessments on day 1 and day 2, and D1.1 and D2.1 indicate post-exercise assessments on day 1 and day 2. D3 and D7 are no-exercise follow-up results.
Differential gene expression by transcriptome analysis
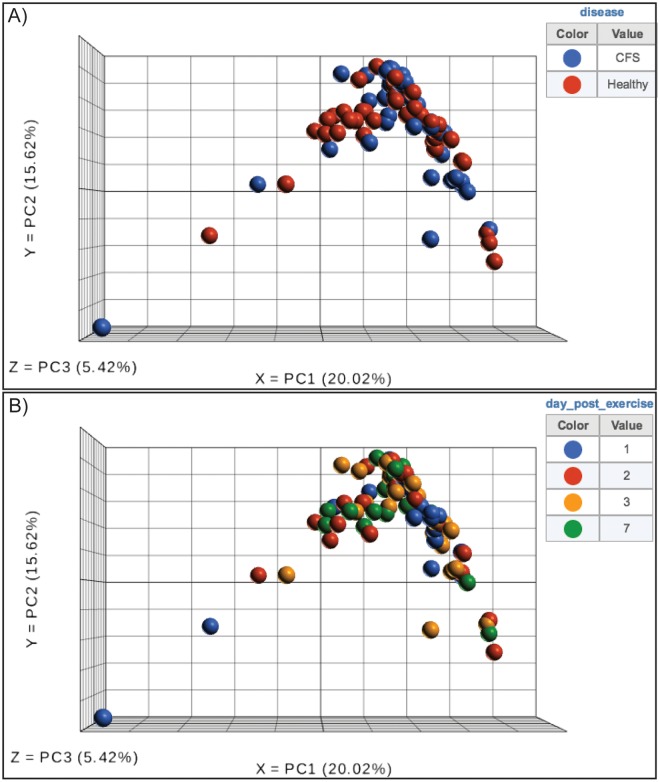
An average of 15.4 million reads per sample were generated (IQR: 13.4–19.4 million reads per sample), with an average of 78% uniquely mapping reads and average transcriptome coverage of 68%. Two samples from a single subject (day 3 and 7 samples) had unusually low number of expressed genes detected (< 40%) and thus were removed from the analysis (Fig A in S1 Appendix). Principal component analysis of the whole transcriptome showed no clustering of samples on the basis of disease status or study time point (Fig 2). No clear clustering based on library preparation batch was observed by PCA (Fig B in S1 Appendix). Additionally, samples had been blinded and randomized during processing of the sample.
Fig 2. Principal component analysis of the global gene expression shows no sampling bias between CFS patients and controls (A), nor between time points (B).
No DEGs were detected when comparing pre- to post-exercise samples in ME/CFS as compared to controls, both overall (days 1, 2 versus day 3, 7) or at any single time point (Table 3). Six DEGs were detected comparing ME/CFS to controls at all time points combined, and 1 DEG was detected at day 7 alone (Table 3). One to three DEGs were detected when comparing the low subset of ME/CFS patients against subjects with regular re-test at days 1, 3 and 7. In total, 19 unique DEGs were identified (Table 4, Figs C-F in S1 Appendix). Thirteen DEGs had average gene coverage lower than 1 normalized read/sample (CREB3L1, HFN4A-AS1, HOXA9, LINC01068, LINC01158, LOC100133050, LOC105372441, NRON, PMS2P2, PRR21, RNASE8, TMEM262, and USP50), and two DEGs were ribosomal genes targeted for depletion during RNA library preparation (RPL23A, RPS12). The other four DEGs correspond to small nucleolar RNAs SNORA27 and SNORA32, uncharacterized non-coding RNA LOC101928767, and MBIP (MAP3K12 binding inhibitory protein 1).
Table 3. Number of differentially expressed genes in ME/CFS patients compared to controls.
| Timepoint | Total | Up-Regulated | Down-Regulated | |
| ME/CFS vs Controls | Day 1 | 0 | 0 | 0 |
| Day 2 | 0 | 0 | 0 | |
| Day 3 | 0 | 0 | 0 | |
| Day 7 | 0 | 0 | 1 | |
| All days | 6 | 4 | 2 | |
| Low ME/CFS subset vs Regular repeat exercise | Day 1 | 1 | 1 | 0 |
| Day 2 | 0 | 0 | 0 | |
| Day 3 | 2 | 2 | 0 | |
| Day 7 | 3 | 3 | 0 | |
| All days | 0 | 0 | 0 | |
| Test-retest effect ME/CFS subset vs Regular repeat exercise | Day 1 | 0 | 0 | 0 |
| Day 2 | 2 | 1 | 1 | |
| Day 3 | 3 | 3 | 0 | |
| Day 7 | 4 | 4 | 0 | |
| All days | 0 | 0 | 0 | |
| Disease | Total | Up-Regulated | Down-Regulated | |
| Day 1 vs Day 2 | CFS | 0 | 0 | 0 |
| HC | 0 | 0 | 0 | |
| Day 1 vs Day 3 | CFS | 0 | 0 | 0 |
| HC | 0 | 0 | 0 | |
| Day 1 vs Day 7 | CFS | 0 | 0 | 0 |
| HC | 0 | 0 | 0 |
Table 4. List of differentially expressed genes in ME/CFS patients compared to controls.
| Comparison | Gene ID | Gene name | Fold change | FDR | Gene count (avg.) |
|---|---|---|---|---|---|
| ME/CFS vs controls; all days | HOXA9 | Homeobox A9 | 2.57 | 0.08 | 0.37 |
| LOC101928767 | Uncharacterized | 2.03 | 0.08 | 1.92 | |
| NRON | Noncoding Repressor Of NFAT | 1.53 | 0.08 | 0.36 | |
| RPL23A | Ribosomal Protein L23a | -1.77 | 0.06 | 39.63 | |
| RPS12 | Ribosomal Protein S12 | -1.56 | 0.02 | 646.28 | |
| SNORA27 | Small Nucleolar RNA, H/ACA Box 27 | 6.35 | 0.06 | 50.88 | |
| ME/CFS vs controls; Day 7 | LINC01158 | Long Intergenic Non-Protein Coding RNA 1158 | 1054 | 0.10 | 0.11 |
| Lower vs Normal ; Day 1 | LOC105372441 | Uncharacterized | 5745 | 3.72E-04 | 0.12 |
| Lower vs Normal ; Day 2 | LOC100133050 | Glucuronidase Beta Pseudogene | 6.42 | 1.19E-03 | 0.01 |
| PMS2P2 | PMS1 Homolog 2, Mismatch Repair System Component Pseudogene 2 | 813 | 0.05 | 0.01 | |
| Lower vs Normal ; Day 7 | PRR21 | Proline Rich Protein 21 | 2072 | 1.98E-03 | 0.04 |
| TMEM262 | Transmembrane Protein 262 | 11.07 | 1.98E-03 | 0.16 | |
| USP50 | Ubiquitin Specific Peptidase 50 | 1979 | 6.86E-03 | 0.04 | |
| Test-retest effect vs Regular exercise; Day 2 | MBIP | MAP3K12 Binding Inhibitory Protein 1 | -1.94 | 0.1 | 3.28 |
| SNORA32 | Small Nucleolar RNA, H/ACA Box 32 | 726520 | 0.04 | 5.24 | |
| Test-retest effect vs Regular exercise; Day 3 | LOC100133050 | Glucuronidase Beta Pseudogene | 4.7 | 0.04 | 0.01 |
| PMS2P2 | PMS1 Homolog 2, Mismatch Repair System Component Pseudogene 2 | 947.93 | 4.81E-03 | 0.01 | |
| RNASE8 | Ribonuclease A Family Member 8 | 7956 | 0.04 | 0.12 | |
| Test-retest effect vs Regular exercise; Day 7 | CREB3L1 | CAMP Responsive Element Binding Protein 3 Like 1 | 5.82 | 0.04 | 0.04 |
| HNF4A-AS1 | HNF4A Antisense RNA 1 | 2293 | 0.03 | 0.03 | |
| LINC01068 | Long Intergenic Non-Protein Coding RNA 1068 | 20.41 | 0.04 | 0.14 | |
| TMEM262 | Transmembrane Protein 262 | 14.06 | 1.19E-05 | 0.16 |
Viral metagenomics
We detected sequences from a small number of viruses in the RNA-seq data, including enterovirus A, influenza A virus, anelloviruses/torque teno viruses (TTVs), and human herpesviruses (HHVs) (Table 5). Only one subject, matched control #01, showed an increase in the number of viral reads from day 1 to day 7, corresponding to anelloviruses. The overall virome composition in ME/CFS did not differ significantly from controls (P = 0.746 by chi-square test) and the number of viral reads did not significantly change in ME/CFS compared to controls (P = 0.098 by Welch’s t-test).
Table 5. Number of reads matching human viruses in positive samples by metagenomic RNA-seq.
| Subject | Disease | Day | Enterovirus A | Human herpesvirus 1 | Human herpesvirus 4 | Human herpesvirus 6A | Human herpesvirus 6B | Human herpesvirus 7 | Influenza A virus | Torque teno virus |
|---|---|---|---|---|---|---|---|---|---|---|
| Control #01 | − | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Control #01 | − | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 6 |
| Control #01 | − | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 16 |
| Control #01 | − | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 18 |
| Control #02 | − | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 |
| Control #06 | − | 3 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 |
| Control #10 | − | 1 | 0 | 32 | 0 | 0 | 0 | 0 | 0 | 0 |
| Control #10 | − | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Control #13 | − | 7 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 |
| Control #14 | − | 7 | 17 | 0 | 0 | 0 | 0 | 6 | 0 | 0 |
| Patient #02 | ME/CFS | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Patient #04 | ME/CFS | 3 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Patient #05 | ME/CFS | 2 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 |
| Patient #06 | ME/CFS | 2 | 0 | 16 | 0 | 0 | 0 | 0 | 0 | 0 |
| Patient #08 | ME/CFS | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 |
| Patient #09 | ME/CFS | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Patient #09 | ME/CFS | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Patient #10 | ME/CFS | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 |
| Patient #10 | ME/CFS | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Patient #12 | ME/CFS | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
Discussion
This study builds on previous observations we have made in people with ME/CFS outside of PEM episodes [18]. While we documented profound clinical differences in health, disability and functional capacity in this population, we did not detect evidence of a transcriptionally-mediated immune mechanism driving the symptoms in ME/CFS. Here we sought to determine whether induced PEM in patients with ME/CFS following experimental CPET triggers differential immune responses and/or changes in the virome relative to controls and before and after exercise. Our rate of ME/CFS subjects enrolled among the screened population, 10.3% (14/136), is much higher than the self-reported prevalence of ME/CFS in Canada from national surveys of approximately 1.5% [4]. This is not unexpected as the screened population was enriched for subjects with symptoms of ME/CFS.
Overall, we did not find significant alterations in gene expression in patients with PEM relative to controls. Fifteen out of 19 DEGs identified in this study were likely false positives due to low gene coverage; the other four DEGs (MBIP, SNORA27, SNORA32 and LOC101928767) were of unclear function and/or showed borderline differences in gene expression. Patients with ME/CFS did also not show significant or relevant exercise-induced after exercise in ME/CFS using RT-PCR of targeted genes [40,41] and in discordant twins using microarrays [42], without identifying important DEGs. This study reinforces these observations by using a more comprehensive genome-wide RNA-seq approach [43].
Reasons for the absence of differential gene expression between ME/CFS patients and controls include (1) the lack of objective diagnostic testing for ME/CFS and reliance on subjective definitions, resulting in heterogeneity in the ME/CFS study cohort, (2) the lack of an immunological signature in ME/CFS that is detectable by transcriptomics, (3) localization of ME/CFS pathogenicity to a specific tissue (e.g. skeletal muscle or brain tissue) rather than blood, (4) heterogeneity of whole blood components with respect to the transcriptional signature, (5) multiple mechanisms underlying ME/CFS in different patients, complicating the identification of a unique signature. Dynamic shifts in viral abundance have been associated with immune cell dysregulation in setting of immunosuppression and obesity [12,13]; here, we observed no differences in viral abundance in ME/CFS patients following exercise.. In addition, detected viral transcripts were to DNA viruses commonly associated with chronic infection, including herpesviruses and anelloviruses. Detection of herpesviruses may suggest latent low-level infection of white blood cells, inflammatory reactivation, and/or active replication [44], while anelloviruses are considered non-pathogenic viral flora and have not yet been linked to any human disease [45]. Regardless, there were no differences in abundance of these viruses between ME/CFS and controls, and pre/post-exercise.
A limitation of the current study is the small size of the study cohort. However, a power analysis study reviewing 6 RNA-seq datasets measuring differential gene expression in human and mouse showed a study power >0.9 when comparing more than 10 samples per condition at a sequencing depth of 10–25 million reads per sample, 8–36% transcriptome mapping rate and comparing 5 differential expression calculation methods [46]. Our present longitudinal study design resulted in a higher transcriptome resolution thanks to increased transcriptome mapping (average, 78%), and increased differential expression accuracy by employing a multi-model approach correcting for small sample sizes. We anticipate our study to be adequately powered when comparing all CFS patients to all healthy controls, or all CFS samples pre- vs post-CPET. Nonetheless, given the lack of accurate and objective diagnostic markers for ME/CFS, if differences in gene expression are indeed present in one or more subsets of these patients, very large cohort studies may be required to identify these genes.
In conclusion, we observed no important differences in gene expression in ME/CFS patients over time and relative to controls in association with experimentally induced PEM. Previously reported differences in immunologic and metabolic function were derived from cross-sectional studies for which causation may not be inferred. Further progress in understanding ME/CFS may be dependent on nested analyses within prospective cohort studies and larger multi-center randomized clinical trials.
Supporting information
Contains Figures A-F. (Fig A) Next-generation sequencing total read counts (grey bar), percentage of reads uniquely mapping to the human transcriptome (black diamond), and transcriptome coverage as the percentage of genes detected (red diamond). Two outlier samples with transcriptome coverage <40% were removed from subsequent human transcriptome analysis. (Fig B) Principal component analysis of the global gene expression shows no batch effect among the different sets of whole blood samples processed by RNA-seq analysis. (Fig C). Expression level dot plot and box plot of 6 differentially expressed genes (RPS12, SNORA27, RPL23A, HOXA9, NRON, LOC101192767) found when comparing CFS patients to controls at all time points. (Fig D). Expression level dot plot of LINC01158 found when comparing CFS patients to controls at day 7 only. (Fig E). Expression level dot plots of 6 differentially expressed genes found at day 1 (LOC105372441), day 3 (LOC100133050, PMS2P2), and day 7 (TMEM262, PRRP21, USP50) when comparing a subset of CFS patients with reduced peak at day 2 to CFS and controls with regular peak . (Fig F). Expression level dot plots of 9 differentially expressed genes found at day 2 (MBIP, SNORA32), day 3 (LOC100133050, PMS2P2, RNASE8), and day 7 (TMEM262, LINC1068, CREB3L1, HNF4A-AS1) when comparing a subset of CFS patients with test-retest effect compared to CFS and controls without test-retest effect.
(DOCX)
Acknowledgments
This study was funded by NIH grant R21NS088166 (DMP and CYC) and by a non-overlapping grant from ME Research UK (Scottish Charity Number SC036942 to DMP) that funded extended sample collection.
Data Availability
Illumina HiSeq raw sequencing data, FPKM values from the transcriptome analysis, and an annotated spreadsheet have been submitted to the NCBI GEO (Gene Expression Omnibus) repository (BioProject: PRJNA526259; GEO: GSE128078).
Funding Statement
This study was funded by NIH grant R21NS088166 (DMP and CYC) and by a non-overlapping grant from ME Research UK (Scottish Charity Number SC036942 to DMP) that funded extended specimen collection. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Clayton EW. Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: An IOM Report on Redefining an Illness. Jama. 2015;180 10.1001/jama.2015.1346 [DOI] [PubMed] [Google Scholar]
- 2.Carruthers BM. Definitions and aetiology of myalgic encephalomyelitis: how the Canadian consensus clinical definition of myalgic encephalomyelitis works. J Clin Pathol. 2006/08/29. 2007;60: 117–119. 10.1136/jcp.2006.042754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reynolds KJ, Vernon SD, Bouchery E, Reeves WC. The economic impact of chronic fatigue syndrome. Cost Eff Resour Alloc. 2004;2: 4 10.1186/1478-7547-2-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rusu C, Gee ME, Lagacé C, Parlor M. Chronic fatigue syndrome and fibromyalgia in Canada: Prevalence and associations with six health status indicators. Chronic Dis Inj Can. 2015;35: 3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnston S, Brenu EW, Staines D, Marshall-Gradisnik S. The prevalence of chronic fatigue syndrome/ myalgic encephalomyelitis: a meta-analysis. Clin Epidemiol. 2013/04/12. 2013;5: 105–110. 10.2147/CLEP.S39876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reid S, Chalder T, Cleare A, Hotopf M, Wessely S. Chronic fatigue syndrome. BMJ. 2000;320: 292–296. 10.1136/bmj.320.7230.292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naviaux RK, Naviaux JC, Li K, Bright AT, Alaynick WA, Wang L, et al. Metabolic features of chronic fatigue syndrome. Proc Natl Acad Sci. 2016;113: E5472–E5480. 10.1073/pnas.1607571113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moneghetti KJ, Skhiri M, Contrepois K, Kobayashi Y, Maecker H, Davis M, et al. Value of Circulating Cytokine Profiling During Submaximal Exercise Testing in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Sci Rep. 2018;8: 2779 10.1038/s41598-018-20941-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hornig M, Gottschalk G, Peterson DL, Knox KK, Schultz AF, Eddy ML, et al. Cytokine network analysis of cerebrospinal fluid in myalgic encephalomyelitis/chronic fatigue syndrome. Mol Psychiatry. 2016;21: 261–269. 10.1038/mp.2015.29 [DOI] [PubMed] [Google Scholar]
- 10.Brenu EW, van Driel ML, Staines DR, Ashton KJ, Hardcastle SL, Keane J, et al. Longitudinal investigation of natural killer cells and cytokines in chronic fatigue syndrome/myalgic encephalomyelitis. J Transl Med. 2012/05/11. 2012;10: 88 10.1186/1479-5876-10-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fluge Ø, Bruland O, Risa K, Storstein A, Kristoffersen EK, Sapkota D, et al. Benefit from B-lymphocyte depletion using the anti-CD20 antibody rituximab in chronic fatigue syndrome. A double-blind and placebo-controlled study. PloS One. 2011;6: e26358 10.1371/journal.pone.0026358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karlsson EA, Sheridan PA, Beck MA. Diet-Induced Obesity in Mice Reduces the Maintenance of Influenza-Specific CD8+ Memory T Cells. J Nutr. 2010;140: 1691–1697. 10.3945/jn.110.123653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li L, Deng X, Linsuwanon P, Bangsberg D, Bwana MB, Hunt P, et al. AIDS alters the commensal plasma virome. J Virol. 2013;87: 10912–10915. 10.1128/JVI.01839-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Navaneetharaja N, Griffiths V, Wileman T, Carding SR. A Role for the Intestinal Microbiota and Virome in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)? J Clin Med. 2016;5 10.3390/jcm5060055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mensah FKF, Bansal AS, Ford B, Cambridge G. Chronic fatigue syndrome and the immune system: Where are we now? Neurophysiol Clin Clin Neurophysiol. 2017;47: 131–138. 10.1016/j.neucli.2017.02.002 [DOI] [PubMed] [Google Scholar]
- 16.Barabási A-L, Gulbahce N, Loscalzo J. Network medicine: a network-based approach to human disease. Nat Rev Genet. 2011;12: 56 10.1038/nrg2918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Byron SA, Keuren-Jensen KRV, Engelthaler DM, Carpten JD, Craig DW. Translating RNA sequencing into clinical diagnostics: opportunities and challenges. Nat Rev Genet. 2016;17: 257 10.1038/nrg.2016.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bouquet J, Gardy JL, Brown S, Pfeil J, Miller RR, Morshed M, et al. RNA-Seq Analysis of Gene Expression, Viral Pathogen, and B-Cell/T-Cell Receptor Signatures in Complex Chronic Disease. Clin Infect Dis. 2017;64: 476–481. 10.1093/cid/ciw767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nijs J, Nees A, Paul L, De Kooning M, Ickmans K, Meeus M, et al. Altered immune response to exercise in patients with chronic fatigue syndrome/myalgic encephalomyelitis: a systematic literature review. Exerc Immunol Rev. 2014;20: 94–116. [PubMed] [Google Scholar]
- 20.Snell CR, Stevens SR, Davenport TE, Van Ness JM. Discriminative validity of metabolic and workload measurements for identifying people with chronic fatigue syndrome. Phys Ther. 2013;93: 1484–1492. 10.2522/ptj.20110368 [DOI] [PubMed] [Google Scholar]
- 21.Carruthers BM, Jain AK, De Meirleir K, Peterson D, Klimas N, Lerner AM, et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols. J Chronic Fatigue Syndr. 2003;11: 7–36. [Google Scholar]
- 22.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee I-M, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43: 1334–1359. 10.1249/MSS.0b013e318213fefb [DOI] [PubMed] [Google Scholar]
- 23.Ware J.E. Kosinski M., Bjorner J.B., Turner-Bowker D.M., Gandek B. and Maruish M.E. J. User’s Manual for the SF-36v2TM Health Survey (2nd Ed). Lincoln, RI: QualityMetric Incorporated; 2007. [Google Scholar]
- 24.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989/10/01. 1989;46: 1121–1123. [DOI] [PubMed] [Google Scholar]
- 25.IACFSME—ME/CFS Primer for Clinical Practitioners (2014 revision) [Internet]. [cited 6 Mar 2018]. http://iacfsme.org/ME-CFS-Primer-Education/News/News-Related-Docs/2014/ME-CFS-Primer-for-Clinical-Practitioners-(2014-rev.aspx
- 26.Karnofsky DA BJH. The Clinical Evaluation of Chemotherapeutic Agents in Cancer CM M, editor. Evaluation of Chemotherapeutic Agents. Columbia University Press; 1949. [Google Scholar]
- 27.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1: 385–401. [Google Scholar]
- 28.Spielberger CD, Gorsuch RL, Lushene RE. Manual for the state-trait anxiety inventory. 1970;
- 29.Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The Physical Activity Scale for the Elderly (PASE): Evidence for validity. J Clin Epidemiol. 1999;52: 643–651. 10.1016/S0895-4356(99)00049-9 [DOI] [PubMed] [Google Scholar]
- 30.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989/05/01. 1989;28: 193–213. [DOI] [PubMed] [Google Scholar]
- 31.Schneider DA, Phillips SE, Stoffolano S. The simplified V-slope method of detecting the gas exchange threshold. Med Sci Sports Exerc. 1993;25: 1180–1184. [PubMed] [Google Scholar]
- 32.Hitchen J, Sooknanan R, Khanna A. Rapid and Efficient Methods for Preparing Globin- and rRNA-Depleted Directional RNA-Seq Libraries. J Biomol Tech JBT. 2013;24: S43–S44. [Google Scholar]
- 33.Dobin A, Davis CA, Schlesinger F, Drenkow J, Zaleski C, Jha S, et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics. 2013;29: 15–21. 10.1093/bioinformatics/bts635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trapnell C, Roberts A, Goff L, Pertea G, Kim D, Kelley DR, et al. Differential gene and transcript expression analysis of RNA-seq experiments with TopHat and Cufflinks. Nat Protoc. 2012;7: 562–578. 10.1038/nprot.2012.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burnham KP, Anderson DR. Model selection and multimodel inference: a practical information-theoretic approach. Springer Science & Business Media; 2003. [Google Scholar]
- 36.Naccache SN, Federman S, Veeeraraghavan N, Zaharia M, Lee D, Samayoa E, et al. A cloud-compatible bioinformatics pipeline for ultrarapid pathogen identification from next-generation sequencing of clinical samples. Genome Res. 2014; 10.1101/gr.171934.113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zaharia M, Bolosky WJ, Curtis K, Fox A, Patterson D, Shenker S, et al. Faster and More Accurate Sequence Alignment with SNAP. ArXiv11115572 Cs Q-Bio. 2011;
- 38.Zhao Y, Tang H, Ye Y. RAPSearch2: a fast and memory-efficient protein similarity search tool for next-generation sequencing data. Bioinformatics. 2011;28: 125–126. 10.1093/bioinformatics/btr595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Greninger AL, Naccache SN, Messacar K, Clayton A, Yu G, Somasekar S, et al. A novel outbreak enterovirus D68 strain associated with acute flaccid myelitis cases in the USA (2012–14): a retrospective cohort study. Lancet Infect Dis. 2015;15: 671–682. 10.1016/S1473-3099(15)70093-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Keech A, Vollmer-Conna U, Barry BK, Lloyd AR. Gene expression in response to exercise in patients with chronic fatigue syndrome: a pilot study. Front Physiol. 2016;7: 421 10.3389/fphys.2016.00421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Light AR, Bateman L, Jo D, Hughen RW, Vanhaitsma TA, White AT, et al. Gene expression alterations at baseline and following moderate exercise in patients with Chronic Fatigue Syndrome and Fibromyalgia Syndrome. J Intern Med. 2012;271: 64–81. 10.1111/j.1365-2796.2011.02405.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Byrnes A, Jacks A, Dahlman-Wright K, Evengard B, Wright FA, Pedersen NL, et al. Gene expression in peripheral blood leukocytes in monozygotic twins discordant for chronic fatigue: no evidence of a biomarker. PLoS One. 2009/06/09. 2009;4: e5805 10.1371/journal.pone.0005805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang W, Yu Y, Hertwig F, Thierry-Mieg J, Zhang W, Thierry-Mieg D, et al. Comparison of RNA-seq and microarray-based models for clinical endpoint prediction. Genome Biol. 2015;16: 133 10.1186/s13059-015-0694-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Whitley R, Kimberlin DW, and Prober, CG. Pathogenesis and disease. In: Human Herpesviruses:Biology, Therapy, and Immunoprophylaxis. 2007. [PubMed]
- 45.Simmonds P, Prescott LE, Logue C, Davidson F, Thomas AE, and Ludlam CA. TT virus--part of the normal human flora?. J Infect Dis. 1999;180(5):1748–50. 10.1086/315103 [DOI] [PubMed] [Google Scholar]
- 46.Ching T, Huang S, Garmire LX. Power analysis and sample size estimation for RNA-Seq differential expression. RNA. 2014;20: 1684–1696. 10.1261/rna.046011.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Contains Figures A-F. (Fig A) Next-generation sequencing total read counts (grey bar), percentage of reads uniquely mapping to the human transcriptome (black diamond), and transcriptome coverage as the percentage of genes detected (red diamond). Two outlier samples with transcriptome coverage <40% were removed from subsequent human transcriptome analysis. (Fig B) Principal component analysis of the global gene expression shows no batch effect among the different sets of whole blood samples processed by RNA-seq analysis. (Fig C). Expression level dot plot and box plot of 6 differentially expressed genes (RPS12, SNORA27, RPL23A, HOXA9, NRON, LOC101192767) found when comparing CFS patients to controls at all time points. (Fig D). Expression level dot plot of LINC01158 found when comparing CFS patients to controls at day 7 only. (Fig E). Expression level dot plots of 6 differentially expressed genes found at day 1 (LOC105372441), day 3 (LOC100133050, PMS2P2), and day 7 (TMEM262, PRRP21, USP50) when comparing a subset of CFS patients with reduced peak at day 2 to CFS and controls with regular peak . (Fig F). Expression level dot plots of 9 differentially expressed genes found at day 2 (MBIP, SNORA32), day 3 (LOC100133050, PMS2P2, RNASE8), and day 7 (TMEM262, LINC1068, CREB3L1, HNF4A-AS1) when comparing a subset of CFS patients with test-retest effect compared to CFS and controls without test-retest effect.
(DOCX)
Data Availability Statement
Illumina HiSeq raw sequencing data, FPKM values from the transcriptome analysis, and an annotated spreadsheet have been submitted to the NCBI GEO (Gene Expression Omnibus) repository (BioProject: PRJNA526259; GEO: GSE128078).