Abstract
Pneumocystis pneumonia (PCP) is a common opportunistic infection in immunocompromised patients. In general, clinical response to therapy with cotrimoxazole is excellent. However, therapy may be limited by side effects or treatment failure. We present a case of PCP in a 35-year-old male patient with history of heart transplantation and renal failure who was admitted with a 10-day history of fever, nonproductive cough and elevated level of creatinine with a diagnosis of PCP confirmed by chest radiography and in bronchoalveolar lavage specimens. He was treated with trimethoprim-sulphamethoxazole (SMZ/TMP) and primaquine but treatment was completed with reduced dosage of cotrimoxazole, primaquine and with the addition of caspofungin. This therapy was effective and without any adverse effects in a patient with elevated level of creatinine.
Keywords: Pneumocystis Pneumonia, Chronic renal failure, Caspofungin
INTRODUCTION
Pneumocystis pneumonia (PCP) is one of the most current opportunistic, critical and life-threatening infection in immune compromised patient (1,2), Such as patients with connective tissue diseases, AIDS, history of transplantation and hematological malignancies (3).
The typical radiographic finding among patients who are infected with PCP is bilateral perihilar interstitial infiltration (4). The less common radiologic findings contain multiple or solitary nodules, upper-lobe infiltration, pneumatoceles and pneumothorax. Also pleural effusion and thoracic lymphadenopathy are seen rarely (5).
The first-line treatment for PCP infection is cotrimoxazole with various adverse effects, including leukopenia, rash, interstitial nephritis and thrombocytopenia (6). So we cannot prescribe it for patients with renal failure and creatinine level rising.
Caspofungin is a beta-1, 3-glucan synthesis inhibitor (antifungal) which in experimental animals has shown activity against PCP (7), but the clinical trials about this matter are rare (8–12). We here report our clinical experience with caspofungin in salvage treatment of PCP in a young man with a history of heart trantplantation and CRF; who referred owing to 10-day history of fever and nonproductive cough. We present our experience of the caspofungin consumption in the context of PCP in immune compromised individual with creatinine level rising and dramatic response.
CASE SUMMARIES
A 35-year-old man, who had received heart transplant 3.5 years previously, was admitted to our hospital with 10-day history of fever and nonproductive cough. He had no history of myalgia, upper respiratory, gastrointestinal symptoms, headache and dyspnea. He had received empiric ciprofloxacin as an outpatient without improvement. His past medical history included heart transplantation 3.5 years ago due to dilated cardiomyopathy. He had chronic renal failure (CRF) following transplantation but his serum creatinine had risen from a baseline of 2.0 mg/dl to 5–6 over the past 8 months. His immunosuppression included tacrolimus 0.5mg at morning and 1 mg at night with a level of 5–6ng/ml, mycophenolate mofetil 500 mg twice daily and prednisolone 7.5 mg once daily, He had received valgancyclovir and itraconasole for CMV and fungal prophylaxis for 3months after transplantation and cortrimoxazole(trimethoprim-sulfametoxazole) until 6 months before presentation; cotrimoxazole was discontinued due to renal failure.
On examination his respiratory rate was 20 breaths per minute and his oxygen saturations were 82% without oxygen therapy. His temperature was 39 °C and blood pressure was 120/80 mmHg. Respiratory auscultation was normal and other physical examinations were unremarkable.
Arterial blood gas showed hypoxemia and blood count was normal without leukocytosis, Cr and BUN was 7.7 and 85 mg/dL respectively, LDH was 704 IU/L, other biochemistry and electrolytes were unremarkable, Respiratory secretions were tested negative for Influenza and other respiratory viruses. He had negative CMV serum PCR. Echocardiography was normal.
The results of chest radiography on admission and a subsequent computed tomography scan revealed bilateral diffuse infiltrates. (Figure 1)
Figure 1.

Chest radiography of patient
Ceftriaxone, Azithromycin and oseltamivir had been initiated at admission and clindamycin with primaquine and intravascular hydrocortisone was added when Pneumocystis pneumonia (PCP) infection was suggested by the chest CT scan. Bronchoalveolar lavage (BAL) was performed. BAL was positive for Klebsiella pneumonia, PCR for CMV was positive but negative for HSV and EBV PCP monoclonal antibody, mycology smear and culture and galactomannan assays were negative. Meropenem 500 mg TDS and valcyte 450 mg every other day was initiated. After 4 days the patient didn't improve and O2 saturation declined to 87% despite facemask O2. Therefore Cotrmoxazole at dosage of 800/160 mg TDS was added.
Another broncoscopy with transbronchial lung biopsy (TBLB) was performed. Smear and culture of BAL was negative for acid fast bacilli and fungal organisms. At this time, bronchoalveolar lavage was negative for CMV PCR but positive for HSV1 PCR and histology showed many Pneumocyctis cysts in the lung biopsy (Figure 2) ten days after initiation of PCP-specific therapy. There was no evidence of CMV or other infections. The patient continued to deteriorate with O2 saturation on facemask decreased to 65%.
Figure 2.
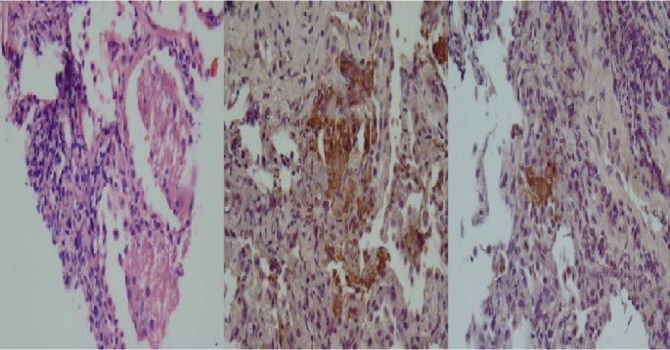
Histology of transbronchial biopsy of patient
Caspofungin 70 mg in first day, then 50 mg daily was added and cotrimoxazole at dosage of 800/160 mg twice daily was continued, clindamycin, primaquine and meropenem were discontinued .
In second day after caspofungin administration patient's general condition became better and after 4 days o2 saturation increased. The patient completed 14-days of therapy with caspofungin and oral cotrimxazole. During treatment his Creatinine level decreased gradually to about 2.2 mg/dL. After 14 days of therapy the O2 saturation increased to 92% without any oxygen therapy.
Three weeks after completion of treatment, the patient was without any symptoms or signs. We continued cotrimoxazole at a dosage of 800/160 mg as a secondary prophylaxis.
DISCUSSION
Pneumocystis pneumonia (PCP) is a leading cause of morbidity in immunocompromised individuals.
The diagnosis of PCP may be difficult without invasive diagnostic approaches including BAL or biopsy, notably in the non-AIDS immunocompromised host (13). In patients intolerant of cotrimoxazole, clindamycin plus primaquine, and atovaquone are second-line drugs and pentamidine intravenously is used in more severe form of disease (14).
Recent studies revealed that PCP is a fungal species with glucan-rich cyst wall (15). The effect of caspofungin against PCP has been shown in animal models (7), but there is limited clinical experience with this agent. This case may suggest that caspofungin in addition to reduced dose cotrimoxazole may provide advantages in patients intolerant of cotrimoxazole due to renal dysfunction (10,11)
Lobo and colleagues16 in their study reported that the administration of low doses of cotrimoxazole in combination with caspofungin provide an improved treatment protocol for PCP infection, in mice. Other studies also derived benefit from cotrimoxazole in combination with caspofungin in their patient (9,17)
Thus, caspofungin is recommended as a salvage treatment in patients with PCP (18).
Tu et al. (19) reported that the use of cotrimoxazole is associated with various side effects that may not be tolerated by critically ill patients so administration of caspofungin is recommended for PJP after solid organ transplantation. They showed that a combination of caspofungin and low-dose cotrimoxazole was useful in three cases of severe PCP in renal transplant recipients. In the current patient, combination therapy appears to be useful in the face of renal intolerance of full-dose cotrimoxazole.
Acknowledgement
The authors are highly indebted to Dr. Jay Fishman for his careful review and precious comments on this manuscript.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC) HIV/AIDS Surveillance Supplemental Report, vol 9, no. 3. Atlanta, GA: Centers for Disease Control and Prevention; 2003: 1–20. [Google Scholar]
- 2.Sepkowitz KA. Opportunistic infections in patients with and patients without Acquired Immunodeficiency Syndrome. Clin Infect Dis 2002;15;34(8):1098–1107. [DOI] [PubMed] [Google Scholar]
- 3.D'Avignon LC, Schofield CM, Hospenthal DR. Pneumocystis pneumonia. Semin Respir Crit Care Med 2008;29(2):132–140. [DOI] [PubMed] [Google Scholar]
- 4.DeLorenzo LJ, Huang CT, Maguire GP, Stone DJ. Roentgenographic patterns of Pneumocystis carinii pneumonia in 104 patients with AIDS. Chest 1987; 91(3):323–327. [DOI] [PubMed] [Google Scholar]
- 5.Gruden JF, Huang L, Turner J, Webb WR, Merrifield C, Stansell JD, et al. High-resolution CT in the evaluation of clinically suspected Pneumocystis carinii pneumonia in AIDS patients with normal, equivocal, or nonspecific radiographic findings. AJR Am J Roentgenol 1997; 169(4):967–975. [DOI] [PubMed] [Google Scholar]
- 6.Floris-Moore MA, Amodio-Groton MI, Catalano MT. Adverse reactions to trimethoprim/sulfamethoxazole in AIDS. Ann Pharmacother 2003; 37(12):1810–1813. [DOI] [PubMed] [Google Scholar]
- 7.Powles MA, Liberator P, Anderson J, Karkhanis Y, Dropinski JF, Bouffard FA, et al. Efficacy of MK-991 (L-743,872), a semisynthetic pneumocandin, in murine models of Pneumocystis carinii. Antimicrob Agents Chemother 1998; 42(8):1985–1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Annaloro C, Della Volpe A, Usardi P, Lambertenghi Deliliers G. Caspofungin treatment of Pneumocystis pneumonia during conditioning for bone marrow transplantation. Eur J Clin Microbiol Infect Dis 2006; 25(1):52–54. [DOI] [PubMed] [Google Scholar]
- 9.Zhang JC, Dai JY, Fan J, Wu XP. [The treatment of pneumocystis Carinii pneumonia with caspofungin in elderly patients: a case report and literature review]. Zhonghua Jie He He Hu Xi Za Zhi. 2006; 29(7):463–465. [PubMed] [Google Scholar]
- 10.Beltz K, Kramm CM, Laws HJ, Schroten H, Wessalowski R, Göbel U. Combined trimethoprim and caspofungin treatment for severe Pneumocystis jiroveci pneumonia in a five year old boy with acute lymphoblastic leukemia. Klin Padiatr 2006; 218(3):177–179. [DOI] [PubMed] [Google Scholar]
- 11.Utili R, Durante-Mangoni E, Basilico C, Mattei A, Ragone E, Grossi P. Efficacy of caspofungin addition to trimethoprim-sulfamethoxazole treatment for severe pneumocystis pneumonia in solid organ transplant recipients. Transplantation 2007;84(6):685–688. [DOI] [PubMed] [Google Scholar]
- 12.Hof H, Schnülle P. Pneumocystis jiroveci pneumonia in a patient with Wegener's granulomatosis treated efficiently with caspofungin. Mycoses. 2008;51 Suppl 1:65–7. [DOI] [PubMed] [Google Scholar]
- 13.Raab SS, Cheville JC, Bottles K, Cohen MB. Utility of Gomori methenamine silver stains in bronchoalveolar lavage specimens. Mod Pathol 1994;7(5):599–604. [PubMed] [Google Scholar]
- 14.Thomas CF, Jr, Limper AH. Pneumocystis pneumonia. N Engl J Med. 2004;350(24):2487–98. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto Y, Matsuda S, Tegoshi T. Yeast glucan in the cyst wall of Pneumocystis carinii. J Protozool 1989;36(1):21S–22S. [DOI] [PubMed] [Google Scholar]
- 16.Lobo ML, Esteves F, de Sousa B, Cardoso F, Cushion MT, Antunes F, et al. Therapeutic potential of caspofungin combined with trimethoprim-sulfamethoxazole for pneumocystis pneumonia: a pilot study in mice. PLoS One 2013;8(8):e70619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jiang XQ, Fang L, Mei XD, Wang XJ, Bao MH. Pneumocystis jiroveci pneumonia in patients with non-Hodgkin's lymphoma after Rituximab-containing regimen: two cases of report and literature review. J Thorac Dis. 2013;5(4):E162–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Armstrong-James D, Stebbing J, John L, Murungi A, Bower M, Gazzard B, et al. A trial of caspofungin salvage treatment in PCP pneumonia. Thorax 2011;66(6):537–538. [DOI] [PubMed] [Google Scholar]
- 19.Tu GW, Ju MJ, Xu M, Rong RM, He YZ, Xue ZG, et al. Combination of caspofungin and low-dose trimethoprim/sulfamethoxazole for the treatment of severe Pneumocystis jirovecii pneumonia in renal transplant recipients. Nephrology (Carlton) 2013;18(11):736–742. [DOI] [PubMed] [Google Scholar]


