Abstract
We investigated the level of amyloid beta (Aβ) in nasal secretions of patients with Alzheimer’s disease dementia (ADD) using interdigitated microelectrode (IME) biosensors and determined the predictive value of Aβ in nasal secretions for ADD diagnosis. Nasal secretions were obtained from 35 patients with ADD, 18 with cognitive decline associated with other neurological disorders (OND), and 26 cognitively unimpaired (CU) participants. Capacitance changes in IMEs were measured by capturing total Aβ (ΔCtAβ). After 4-(2-hydroxyethyl)-1-piperazinepropanesulfonic acid (EPPS) was injected, additional capacitance changes due to the smaller molecular weight Aβ oligomers disassembled from the higher molecular weight oligomeric Aβ were determined (ΔCoAβ). By dividing two values, the capacitance ratio (ΔCoAβ/ΔCtAβ) was determined and then normalized to the capacitance change index (CCI). The CCI was higher in the ADD group than in the OND (p = 0.040) and CU groups (p = 0.007). The accuracy of the CCI was fair in separating into the ADD and CU groups (area under the receiver operating characteristic curve = 0.718, 95% confidence interval = 0.591–0.845). These results demonstrate that the level of Aβ in nasal secretions increases in ADD and the detection of Aβ in nasal secretions using IME biosensors may be possible in predicting ADD.
Introduction
Alzheimer’s disease (AD) is the most common cause of dementia, as it accounts for 60 to 70% of the overall prevalence of dementia. AD is a neurodegenerative disorder characterized by an insidious onset and a progressive deterioration in cognition, functional ability, and behaviour1. Current therapies such as acetylcholinesterase inhibitors and the N-methyl-D-aspartate receptor antagonist memantine may provide relief with respect to symptoms, but they do not treat the underlying process of AD. Neuropathological hallmarks of AD include amyloid β (Aβ)-containing plaques and tau-containing neurofibrillary tangles, which are found throughout the brain2. These hallmarks have become the main target of current drug development. However, several drug candidates that target Aβ have not been successful in large, multicentre clinical trials3–5. It is now generally acknowledged that this is partly because a large proportion of clinically diagnosed patients show no evidence of amyloid pathology on positron emission tomography (PET) scans5. Recent advances in AD research also show that amyloid pathology begins 20–30 years before the clinical onset of AD6. These findings indicate the need for validated biomarkers in drug development and clinical practice.
In the last decade, remarkable progress has been achieved in the study of AD biomarkers. Biomarkers of Aβ plaques include cortical amyloid PET ligands7–9 and low cerebrospinal fluid (CSF) Aβ4210,11. Biomarkers of fibrillar tau include elevated CSF phosphorylated tau (p-tau) and cortical tau PET ligands12,13. Biomarkers of neurodegeneration or neuronal injury are CSF total tau (t-tau)13, 18fluorodeoxyglucose PET hypometabolism, and atrophy on magnetic resonance imaging (MRI)14,15. However, PET and MRI are expensive, and CSF biomarker analysis requires a lumbar puncture, which is an invasive procedure with potential adverse side effects such as headache and back pain. Interlaboratory variability of CSF biomarker analysis is also high. Recently, the results of studies of blood-based biomarkers of AD pathology such as plasma Aβ and tau have been reported16–19. Simple and inexpensive tests for blood-based biomarkers would be desirable due to their safety and minimal invasiveness. However, given the lack of consistency of most blood-based biomarkers across studies, validation in another cohort is needed, and other cost-effective and feasible methods for the early diagnosis of AD are needed.
In a recent study, older adults with olfactory dysfunction were more than twice as likely to develop dementia 5 years later, and more odour identification errors were associated with a greater probability of an interval dementia diagnosis20. It has been reported that in AβPP/PS1 transgenic mice, the deposition of Aβ began in the olfactory system and then spread to the hippocampus and cortex21. In experiments in rats, ventricle-injected isotope-labelled Aβ peptide (125I-Aβ40) was shown to be transported to the nasal cavity through a non-haematogenous pathway22. In another recent study, median levels of p-tau/t-tau ratios in the middle nasal meatus and in the olfactory cleft were significantly higher in AD cases than in controls, but the levels of Aβ42 and Aβ40 were near zero and were not different between AD cases and controls23. However, the methods used in the study may not have detected a very low level of Aβ in nasal secretions.
In this study, we investigated the level of Aβ in nasal secretions of patients with AD dementia (ADD) using interdigitated microelectrode (IME) methods and examined the predictive value of Aβ in nasal secretions for the diagnosis of ADD.
Results
Nasal secretions were obtained from 35 patients with ADD, 18 patients with cognitive decline associated with other neurological disorders (OND), and 26 cognitively unimpaired (CU) participants. Table 1 presents the baseline demographic and clinical characteristics of the participants according to the groups. The participants in the CU group were younger than those in the ADD and OND groups, respectively. There was no significant difference in gender and education among the groups. The prevalence of Apolipoprotein E (APOE) ε4 carriers and Aβ deposition on PET were higher in the ADD group than in the OND and CU group. There was a significant difference in the Clinical Dementia Rating (CDR) scale among the groups. The Mini-Mental State Examination (MMSE)24 and CDR-Sum of Boxes (SB) scores were significantly different among the groups after adjusted for age. The MMSE (p < 0.001), and CDR-SB (p < 0.001) scores were significantly lower in the ADD group than in the CU group. The MMSE (p = 0.003) and CDR-SB (p < 0.001) scores were also significantly lower in the ADD group than in the OND group. Finally, the MMSE (p < 0.001) and CDR-SB (p < 0.001) scores were significantly lower in the OND group than in the CU group.
Table 1.
Demographic and clinical characteristics of the participants. Notes: ADD = Alzheimer’s disease dementia; OND = other neurological disorders; CU = cognitively unimpaired; MMSE = Mini-Mental State Examination; CDR = Clinical Dementia Rating scale; CDR-SB = CDR-Sum of Boxes; APOE = apolipoprotein E; Aβ, amyloid beta. Values are mean (standard deviation) or numbers (%).
| Variables | ADD (n = 35) | OND (n = 18) | CU (n = 26) | P value | P < 0.05§ |
|---|---|---|---|---|---|
| Age, years | 75.8 (9.9) | 76.9 (7.5) | 68.9 (5.7) | 0.002* | b, c |
| Female | 26 (74.3%) | 12 (66.7%) | 22 (84.6%) | 0.373† | |
| Education, years | 7.4 (5.0) | 7.0 (4.6) | 6.7 (4.8) | 0.861* | |
| MMSE | 15.2 (3.7) | 18.9 (5.5) | 26.1 (2.8) | <0.001‡ | a, b, c |
| CDR 0: 0.5: 1: 2: 3 | 0: 12: 15: 7: 1 | 0: 12: 4: 2: 0 | 26: 0: 0: 0: 0 | <0.001† | |
| CDR-SB | 6.34 (4.05) | 3.94 (3.67) | 0.19 (0.29) | <0.001‡ | a, b, c |
| APOE ε4 carrier | 12/33 (36.4%) | 1/13 (7.7%) | 3/22 (13.6%) | 0.041† | |
| Aβ deposition on PET | 28/28 | 0/15 | 0/20 | <0.001† |
*P value from analysis of variance; †Results from chi-square tests; ‡P value from analysis of covariance with age as a covariate; §Pairwise comparisons on age between diagnosis groups were conducted with Tukey method, and pairwise comparisons on MMSE and CDR-SB between diagnosis groups were conducted with Bonferroni post hoc analysis; a, ADD vs. OND; b, ADD vs. CU; c, OND vs. CU.
The capacitance change index (CCI) in nasal secretions was significantly different among the groups after adjusted for age (Table 2). Bonferroni post hoc analysis showed that the CCI in nasal secretions was significantly higher in the ADD group than in the OND (p = 0.040) and CU groups (p = 0.007) (Fig. 1). The CCI in nasal secretions showed a negative correlation with the MMSE score and a positive correlation with CDR or CDR-SB scores (Table 3).
Table 2.
Capacitance change index in nasal secretions according to each group.
| Variables | ADD (n = 35) | OND (n = 18) | CU (n = 26) | P value* | Pairwise comparisons† |
|---|---|---|---|---|---|
| CCI | 49.4 (31.7) | 29.8 (21.8) | 26.9 (20.6) | 0.003 | Pa = 0.040 Pb = 0.007 Pc = 1.000 |
Notes: ADD = Alzheimer’s disease dementia; OND = other neurological disorders; CU = cognitively unimpaired; CCI = capacitance change index. Values are mean (standard deviation). *P value from analysis of covariance with age as a covariate; †Results from Bonferroni post hoc analysis; a, ADD vs. OND; b, ADD vs. CU; c, OND vs. CU.
Figure 1.
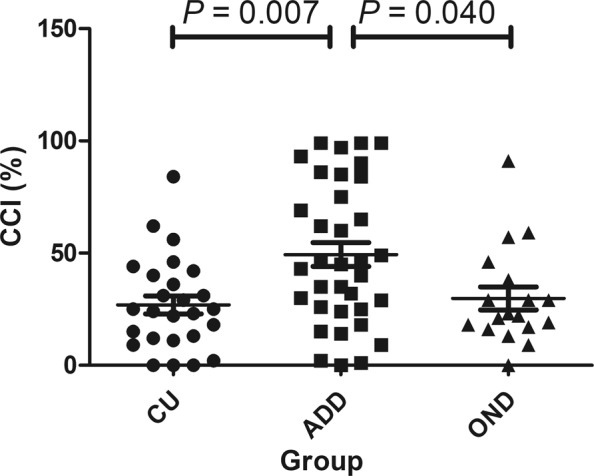
The distribution pattern of the capacitance change index (CCI) in nasal secretions in patients with Alzheimer’s disease dementia (ADD), those with cognitive decline related to other neurological diseases (OND), and cognitively unimpaired (CU) individuals. The CCI was significantly higher in the ADD group than in the OND (p = 0.040) and CU groups (p = 0.007) after application of Bonferroni post hoc analysis.
Table 3.
Correlations between the capacitance change index and global cognitive function. Notes: MMSE = Mini-Mental State Examination; CDR = Clinical Dementia Rating scale; CDR-SB = CDR-Sum of Boxes.
| Capacitance change index | ||
|---|---|---|
| Spearman’s rho | P value | |
| MMSE (range, 0–30)* | −0.252 | 0.027 |
| CDR (range, 0–3)† | 0.271 | 0.016 |
| CDR-SB (range, 0–18)† | 0.294 | 0.009 |
*Decreases in scores represent worsening. †Increases in scores represent worsening.
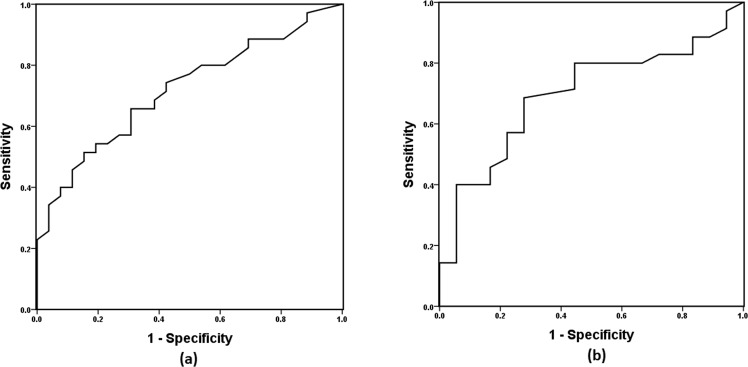
The receiver operating characteristic (ROC) curve was used to examine the predictive value of the CCI in nasal secretions for a diagnosis of ADD. The area under the ROC curve (AUC) was 0.718 (95% confidence interval [CI], 0.591–0.845, standard error [SE] = 0.065, p = 0.004) for the diagnosis of ADD among the participants of the ADD and CU groups (Fig. 2a). The sensitivity and specificity values of the CCI in nasal secretions in the diagnosis of ADD were 65.7% and 69.2%, respectively, at the cutoff point of 31.5. The ability of the CCI in nasal secretions to differentiate between ADD and OND patients was newly validated in a separate ROC analysis. The AUC was 0.696 (95% CI, 0.551–0.841, SE = 0.074, p = 0.020) for the diagnosis of ADD among the participants of the ADD and OND groups (Fig. 2b). The sensitivity and specificity values of the CCI in nasal secretions for a diagnosis of ADD among the participants of the ADD and OND groups were 68.6% and 72.2%, respectively, at the cutoff point of 29.5.
Figure 2.
The receiver operating characteristic (ROC) curve of the capacitance change index (CCI) used for the diagnosis of Alzheimer’s disease dementia (ADD). (a) The sensitivity and specificity of the CCI for the diagnosis of ADD among patients with ADD and cognitively unimpaired individuals was 65.7% and 69.2%, respectively, at the cutoff point of 31.5. The area under the ROC curve (AUC) was 0.718 (95% confidence interval [CI], 0.591–0.845, standard error [SE] = 0.065, p = 0.004). (b) The sensitivity and specificity of the CCI in nasal secretions for the diagnosis of ADD among participants with ADD or other neurological disorders was 68.6% and 72.2%, respectively, at the cutoff point of 29.5. The AUC was 0.696 (95% CI, 0.551–0.841, SE = 0.074, p = 0.020).
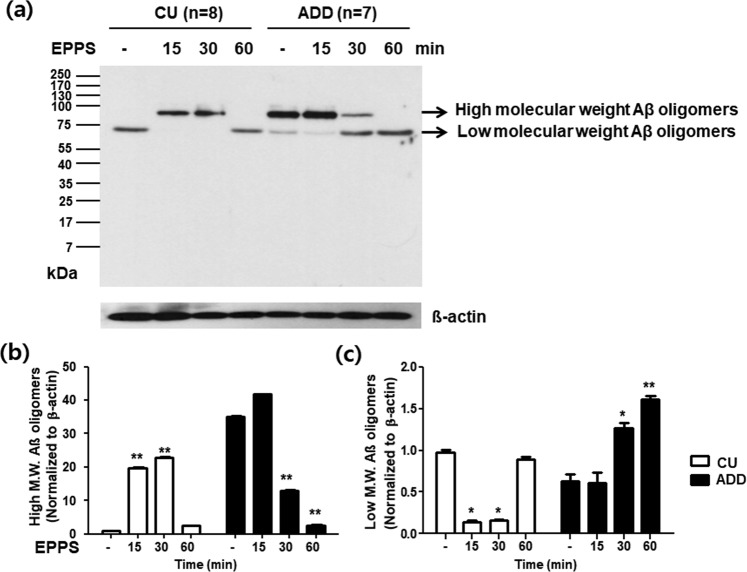
To confirm the disassembly of Aβ oligomers related to the principle of capacitance change of IME sensor, the nasal secretion samples of 7 ADD patients and 8 CU individuals at baseline and their 4-(2-hydroxyethyl)-1-piperazinepropanesulfonic acid (EPPS)-treated samples according to time (15, 30, and 60 min) were analyzed by western blots. Figure 3a presents that the baseline nasal secretions of ADD patients contain larger amounts of high molecular weight Aβ oligomers of ~90 kDa compared to the CU individuals and less other molecular weight Aβ oligomers (lane 5), and by treating EPPS for 60 min, high molecular weight Aβ oligomers were gradually disassembled to lower molecular weight Aβ oligomers with a distinct band at ~70 kDa and various sizes of Aβ oligomers under 70 kDa. After 60 min, a band at ~90 kDa completely disappeared and a band at ~70 kDa definitely emerged (lane 6–8). The amount of high molecular weight Aβ oligomers in the ADD group was significantly lower at 30 min and 60 min than at baseline (Fig. 3b). The amount of disassembled lower molecular weight Aβ oligomers gradually increased until 60 min in the nasal sample of ADD patiens, and the amount of disassembled lower molecular weight Aβ oligomers in the ADD group was significantly higher at 30 min and 60 min than at baseline (Fig. 3c).
Figure 3.
Western blot analysis of nasal secretions in 7 patients with Alzheimer’s disease dementia (ADD) and 8 cognitively unimpaired (CU) individuals. Western blots using 6E10 antibody were performed for nasal secretions of 7 ADD patients with amyloid deposition on PET and 8 CU individuals without amyloid deposition on PET. (a) Western blotting of nasal secretions of the ADD patients and CU individuals at baseline, and 15, 30 and 60 min after 4-(2-hydroxyethyl)-1-piperazinepropanesulfonic acid (EPPS) treatment. It presents that the baseline nasal secretion of ADD patients contains larger amount of high molecular weight amyloid β (Aβ) oligomers of ~90 kDa compared to the CU individuals and less other molecular weight Aβ oligomers (lane 1, 5), and by treating EPPS for 60 min, high molecular weight Aβ oligomers were gradually disassembled to lower molecular weight Aβ oligomers under 70 kDa. After 60 min, a band at ~90 kDa completely disappeared and a band at ~70 kDa definitely emerged (lane 6–8). (b) The amount of high molecular weight Aβ oligomers gradually decreases until 60 min in the nasal sample of ADD patients. The amount of high molecular weight Aβ oligomers in the ADD group was significantly lower at 30 min and 60 min than at baseline. (c) The amount of disassembled lower molecular weight Aβ oligomers gradually increases until 60 min in the nasal sample of ADD patients. The amount of disassembled lower molecular weight Aβ oligomers in the ADD group was significantly higher at 30 min and 60 min than at baseline. Data are mean (SEM). *p < 0.005 vs. baseline and **p < 0.001 vs. baseline by Bonferroni post hoc analysis.
Discussion
In this study, the CCI in nasal secretions was elevated in the patients with ADD compared to the CU individuals and those with OND. The CCI in nasal secretions is greater when the level of soluble Aβ in nasal secretions is higher. Therefore, the present results demonstrate that the soluble Aβ such as oligomeric Aβ in nasal secretions is elevated in ADD patients compared to CU individuals and those with OND. The present results demonstrate the possibility that the ultra-sensitive detection of soluble Aβ in nasal secretions using IME biosensors may be effective in predicting ADD. However, the accuracy of the CCI as measured by the AUC was fair in separating into the ADD and CU groups. The accuracy of CCI in nasal secretions for the prediction of ADD was lower than that of amyloid PET ligands and CSF AD biomarkers found in previous studies11,25. More studies are needed before Aβ in nasal section can be used as a biomarker for AD. The following studies may be needed to improve accuracy. First, the amount of nasal secretions collected varied among the participants, so the concentration of Aβ needs to be considered. Second, if there is a diurnal variation in the amount of Aβ in nasal secretions, it is necessary to collect them from participants at similar times. Third, we need to consider using a more powerful substance than EPPS to disaggregate high molecular weight Aβ. Fourth, more advanced measurement system may be needed.
The accuracy of the CCI in nasal secretions was also nearly fair to distinguish between ADD and OND patients. To be a diagnostic marker for ADD, it is important that a biomarker is able to distinguish ADD from patients with other diseases as well as from normal individuals. Although the results of this study are still lacking, the present results suggest that if accuracy improves, the CCI reflecting the amount of soluble Aβ in nasal secretions may be useful in distinguishing ADD from other causes of dementia. Although the presence or absence of amyloid deposition using PET or CSF studies was found in about 82% of the participants in this study, some participants of the OND group may also have had multiple brain pathologies including AD26. In the future, the CCI should be evaluated only in OND patients with amyloid-negative results on PET or CSF studies.
The CCI was significantly correlated with global cognitive function scales. Higher CCI was related to lower global cognitive function, and thus the CCI may reflect the natural course of AD. However, whether a change in the CCI is associated with cognitive decline should be evaluated in a longitudinal observational study. No correlation was observed between CSF and PET amyloid value changes in a longitudinal study27. This result suggests that Aβ in body fluids may measure different aspects of AD Aβ pathology from those of amyloid PET.
The ultra-sensitive detection of small amounts of Aβ in nasal secretions could be performed using IME methods28. Previously, we had failed to measure Aβ in nasal secretions by Luminex multiplex assay. Electrical impedimetric biosensors have attracted attention due to their label-free and real-time monitoring of the morphological and physiological changes in DNA, protein, and cells29. For the electrical impedance measurement of the specimens, micro- or nano-sized electrode-based sensors are used. The IME biosensor could therefore be a method by which ultra-low levels of proteins are measured in body fluids.
The previous clinical studies and a meta-analysis showed that patients with ADD had the evidence for olfactory deficits30,31. In a previous report, olfactory impairment in cognitively normal elderly was associated with incident amnestic mild cognitive impairment (aMCI) and progression from aMCI to ADD over a mean 3.5 years of follow-up32. This study suggests that olfactory deterioration may precede cognitive decline in AD. More research is needed on the olfactory function and measurement of Aβ in nasal secretions in AD.
The study of EPPS-derived disassembly of soluble Aβ by the western blots demonstrated that soluble Aβ proteins such as high molecular weight Aβ oligomer33 were disassembled to several numbers of lower molecular weight Aβ oligomers (~70 kDa and much smaller oligomers). Thus, it looks clear that the increase of target molecules is closely related to the increase of capacitance change (ΔCoAβ) and furthermore, clinical effectiveness of CCI for ADD diagnosis based on the nasal secretions. The reason why other bands of disassembled Aβ oligomers except a band at ~70 kDa were not clearly shown in the blot image might have been that their concentrations were too low to be detectable by western blots. The western blot analysis did not provide any information on the isoforms of Aβ oligomers (40 and 42 or their mixture) captured by 6E10 anti-Aβ antibody as well. Nevertheless, Aβ42 can be the most reasonable candidate among the amyloid proteins which are contained in discrete bands. In a previous study, authors have used a western blot analysis, to which 6E10 antibody applied, for the characterization of high molecular weight Aβ42 oligomers as well as its monomer isolated from human hippocampal samples34.
Our study had several limitations. First, the results should be interpreted with caution due to the small sample size. The results of this study should be reproduced in other studies with large sample sizes. Second, amyloid biomarkers such as amyloid PET ligands and CSF biomarkers were not studied for all participants, although approximately 82% of participants had historical results available for amyloid PET or CSF Aβ42 levels. Some patients without brain amyloid pathology may have been included in the ADD group, while other individuals with brain amyloid pathology may have been included in the CU and OND groups. Third, we did not examine the associations of the CCI in nasal secretions with other AD biomarkers such as amyloid PET, CSF Aβ42, t-tau and p-tau levels, and cortical thickness. Fourth, we did not directly measure the levels of Aβ in nasal secretions, but rather, we measured the Aβ levels in nasal secretions indirectly by assessing changes in capacitance. Fifth, we did not pinpoint the species of Aβ detected by 6E10 anti-Aβ antibody in the baseline nasal secretions as well as in the nasal secretions after disaggregation by EPPS. In the future, it is necessary to define the size and isoforms of Aβ using mass spectrometry. It is also necessary to analyze nasal secretion with other anti-Aβ antibodies, such as antibodies targeting oligomeric Aβ42. Sixth, we did not investigate the efficiency of examining the amount of EPPS that allows the CCI to reach its maximum value35.
To our knowledge, this is the first study to show that Aβ levels in nasal secretions are elevated in ADD patients compared to CU individuals and those with OND. The results of this study are still preliminary but suggest that CCI reflecting the amount of soluble Aβ in nasal secretions, such as oligomeric Aβ, may be useful in predicting ADD if accuracy improves. More studies are needed before Aβ in nasal secretions can be used as a biomarker for AD.
Methods
Participants
From October 2015 to August 2018, 38 patients with ADD, 18 patients with cognitive decline associated with OND, and 27 CU elderly controls participated in this study. Three patients with ADD and one CU individual withdrew their consent. Finally, nasal secretions were obtained from 79 participants, who ranged in age from 50 to 90 years. We recruited patients with ADD or OND from the memory clinic at Inha University Hospital, Incheon, South Korea. The participants with ADD met the criteria for probable ADD according to the National Institute on Aging-Alzheimer’s Association core clinical criteria36. The OND group consisted of nine patients with vascular cognitive impairment37, three patients with frontotemporal lobar degeneration38, one patient with Parkinson’s disease39, one patient with epilepsy, and four patients with other dementia.
The CU individuals were recruited from patients who visited the neurology clinic at the same hospital for other reasons (e.g., dizziness, hypertension, Bell’s palsy). They did not have any of the 28 diseases associated with decreases in cognitive function or a history suggestive of a decrease in cognitive function40: stroke or transient ischaemic attack, seizures, Parkinson’s disease, multiple sclerosis, cerebral palsy, Huntington’s disease, encephalitis, meningitis, brain surgery, surgery to clear arteries to the brain, diabetes that requires insulin to control, hypertension that is not well controlled, cancer other than skin cancer diagnosed within the past three years, shortness of breath while sitting still, use of oxygen at home, heart attack that resulted in changes in memory, walking or problem solving lasting at least 24 hours, kidney dialysis, liver disease, hospitalization for mental or emotional problems within the past five years, current use of medications for mental or emotional problems, alcohol consumption greater than three drinks per day, drug abuse in the past five years, treatment for alcohol abuse in the past five years, unconsciousness for more than one hour other than during surgery, overnight hospitalization because of a head injury, illness causing a permanent decrease in memory or other mental functions, trouble with vision that prevents reading ordinary print even with glasses, and difficulty understanding conversations because of hearing even if wearing a hearing aid. They also had MMSE scores more than 1.5 standard deviation below the age- and education adjusted normative means24.
We excluded participants who took medications that affect nasal function within 1 week of the study entry, those who underwent nasal surgery within 3 months, those who were diagnosed with rhinitis or sinusitis by simple X-ray or computed tomography scan, those with a history of exposure to chemical stimulants, current smokers, those with severe or uncontrolled medical disease, and those who were pregnant or lactating.
All participants underwent comprehensive physical and neurological examinations, including an extensive standardized neuropsychological battery, the Seoul Neuropsychological Screening Battery (SNSB)41. They were also administered a brain MRI and routine biochemical and serological tests that included a thyroid function test, tests for serum vitamin B12 and folate levels, and a Venereal Disease Research Laboratory test.
The presence or absence of cortical amyloid deposition was confirmed by amyloid PET imaging in 63 (79.7%) participants and by CSF Aβ measurements in two participants. Evidence of brain amyloid pathology in the ADD group was demonstrated in fifteen patients with positive 18F-flutemetamol PET imaging, nine with positive 18F-florbetaben PET imaging, three with positive ¹¹C-Pittsburgh compound-B (11C-PIB) PET imaging, and one with positive 18F-florbetapir PET imaging (Table 1). Amyloid pathology in the brain was demonstrated by low Aß42 levels in the CSF in two other patients in the ADD group. There were eight participants with amyloid-negative results on 18F-flutemetamol PET imaging and seven with amyloid-negative results on 18F-florbetaben PET imaging in the OND group. There were ten participants with amyloid-negative results on 18F-flutemetamol PET imaging, nine with amyloid-negative results on 18F-florbetaben PET imaging, and one with amyloid-negative results on 11C-PIB PET imaging in the CU group. The amyloid PET data were visually assessed by two doctors of nuclear medicine, who were masked to the clinical diagnosis and all other clinical findings.
The study was performed in accordance with the International Harmonization Conference guidelines on Good Clinical Practice and was approved by the institutional review board of Inha University Hospital prior to study initiation. Prior to participation in the study, all participants provided written informed consent for their participation in the study. The legal representatives of the participants with dementia also provided written informed consent.
Collection of nasal secretions
The collection of nasal secretions was performed according to the method previously reported by Cho et al.42 A Merocel® sponge was placed into both nasal cavities of the patient for 1 minute. At this stage, the sponge was placed towards the nasal roof so that it was as close to the olfactory bulb as possible. After the sponge was removed from the participant’s nose, we inserted it in a specially shaped tube with a funnel. When the sponge is placed on the funnel in this tube, the nasal secretion absorbed by the sponge flows down through the funnel which is designed to be tucked down. We performed centrifugation at 4 °C and 5000 rpm for 10 minutes to isolate all nasal secretions from the sponge. The nasal secretions were then stored at a temperature of −80 °C until further analysis.
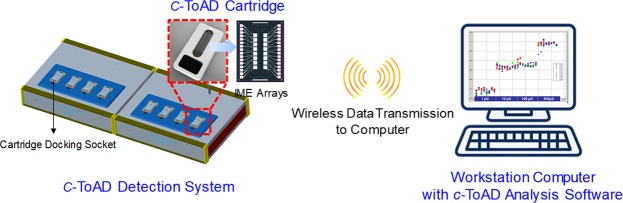
System Configuration of AD Diagnostic System
The electrical capacitance measurement-based AD diagnostic system (c-ToAD, Cantis Inc., South Korea) used to analyse human nasal secretions is briefly composed of (i) c-ToAD detection system, which is a customized impedance analyser with 8 device docking sockets and a syringe pump, (ii) the workstation computer for data acquisition from the c-ToAD detection system, the process of which is related to visualization and motion control of the syringe pump connected to the c-ToAD cartridge, and (iii) the disposable c-ToAD cartridge. All communications between the c-ToAD detection system including the micro-pump and the computer were achieved via Bluetooth wireless technology (Fig. 4). In detail, the cartridge is composed of a glass chip on which 16 interdigitated platinum microelectrode (Pt-IME) arrays were fabricated, polycarbonate (PC) packaging with 2 microfluidic channels containing 8 electrodes per channel and the electric interface that connects Pt-IMEs to the device docking sockets. To analyse the human samples, IgG monoclonal antibody 6E10 (BioLegend, USA) used to capture Aβ was immobilized between Pt-IMEs in the ToAD cartridges, which were prepared immediately before use.
Figure 4.
Overview of the c-ToAD diagnostic system developed by Cantis Inc. IME = interdigitated microelectrode.
Sample Analysis Protocol
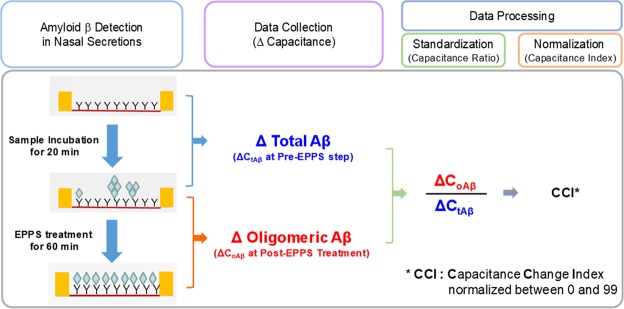
Before the analyse, the nasal secretions were collectively diluted to 25% of their original concentration in phosphate-buffered saline (PBS) (1×, pH 7.4) to adjust their viscosity, after which they were contained in a 200 μL syringe. By driving the microsyringe pump, a maximum of 16 samples was carefully delivered to the microfluidic channels of the c-ToAD cartridges. The samples were then incubated for 20 min at room temperature. To clean the IMEs and channels, the sample solutions were pumped out, and the microfluidic channels were washed with PBS with Tween 20 (×1) and PBS (×3) sequentially by repeating the flow of the wash buffers. Capacitance changes in the IMEs were measured by capturing the molecules of total Aβ at this step (pre-EPPS step, 1000 Hz, 20 min). After the measurement, EPPS was carefully injected into the microfluidic channels, and simultaneously, the second capacitance measurement was performed (1000 Hz, 1 h). The capacitance change over time at the post-EPPS step indicates that monomeric or lower molecular weight Aβ molecules that disassembled from oligomeric Aβ by EPPS were gradually associated with the unoccupied antigen binding fragment (Fab) binding sites of the Aβ antibody (Fig. 5)33. Using the capacitance change, the system was able to avoid the deviation of the capacitance values of the IME array that were determined by the different lengths and locations of the transmission lines between the sensing area and the terminal pads.
Figure 5.
Assay protocol for the measurement of oligomeric amyloid β in diluted nasal secretions. It shows the process by which electronic data are collected from the ToAD diagnostic system and data standardization/normalization through which the capacitance change index is calculated. EPPS = 4-(2-hydroxyethyl)-1-piperazinepropanesulfonic acid.
Data analysis
As mentioned above, all data measured by the c-ToAD detection system were spontaneously transmitted to the c-ToAD workstation via wireless transmission during measurement. In principle, the c-ToAD software averaged all of capacitances obtained from the 8-IME array in a single microfluidic channel according to an electric parameter setting and algorithm and calculated capacitance changes of the total Aβ (ΔCtAβ) at the pre-EPPS step and those of the oligomeric Aβ (ΔCoAβ) at the post-EPPS step to yield the capacitance ratio (ΔCoAβ/ΔCtAβ) of each sample. Finally, all of ΔCoAβ/ΔCtAβ values were normalized to specific indices between 0 and 99 according to a measurement standard (Capacitance Change Index, CCI (a.u.)).
Western blot analysis of nasal secretions
Nasal secretions collected from 7 ADD patients with amyloid deposition on PET and 8 CU individuals without amyloid deposition on PET were used in the western blot analysis. Nasal secretions were lysed in ice-cold RIPA buffer containing 1× proteinase inhibitor cocktail. Lysate was incubated in ice for 20 minutes and centrifuged at 14,000 r.p.m., 4 °C for 30 min. The supernatant was used in Aβ western blots for biochemical changes. Protein samples (40 μg) were loaded on each lane of SDS–PAGE gels to detect Aβ oligomer, disassembled lower molecular Aβ oligomer and β-actin (a loading control). Afterward, the blots were probed with anti-Aβ (6E10) or anti-β-actin antibodies (1:1000) at 4 °C overnight, followed by incubation with secondary goat anti-mouse horse radish peroxidase-conjugated immunoglobulin G (1:20,000) at room temperature for 1 h. The signals were visualized using enhanced chemiluminescence. The band intensity was quantified on ImageJ software (http://rsbweb.nih.gov/ij/index.html).
Statistical analyses
Characteristic data were presented as means and standard deviations (SD) for continuous variables and frequency and percentages for categorical variables. The analysis of variance (ANOVA) was used to compare age and education among the groups. When a statistical significant overall difference was detected in the ANOVA test, pairwise comparisons on means between diagnosis groups were conducted with Tukey method. For the categorical variables, namely, gender, CDR, APOE ε4 carrier status and Aβ deposition on PET, we calculated the frequencies and compared their differences across the groups using the χ² test. The analysis of covariance (ANCOVA) with age as a covariate was used to compare MMSE, CDR-SB, and CCI among the groups. When a statistical significant overall difference was detected in the ANCOVA test, pairwise comparisons on means between diagnosis groups were conducted with Bonferroni post hoc analysis. The ANOVA and Bonferroni post hoc analysis were used to compare the amounts of proteins according to the time in the western blot. Spearman’s rho was used to measure the correlations between CCI and global cognitive function. The sensitivity and specificity of the CCI for the diagnosis of ADD were evaluated by ROC curve analysis. The cutoff values were determined to yield the best Youden index (sensitivity + specificity − 1) for ADD diagnosis. Significance for all tests was set at α = 0.05, two-tailed. All statistical analyses were performed using SPSS 19.0 (SPSS, Chicago, IL, USA).
Supplementary information
Acknowledgements
This study was supported by grants from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI18C0479), the Original Technology Research Program for Brain Science through the National Research Foundation of Korea (NRF) funded by the Korean government (MSIP) (NRF-2014M3C7A1064752 and NRF-2018M3A9F1023697), and Eisai Korea Inc.
Author Contributions
Conception and design of study: Y.H.K., S.-M.L., S.H.C., J.-H.K. Acquisition of data (laboratory or clinical): Y.H.K., S.H.C., S.-M.L., J.-H.K., H.P. Data analysis and/or interpretation: Y.H.K., S.H.C., S-M.L., H.P. Drafting of manuscript and/or critical revision: Y.H.K., S.H.C., S.-M.L., S.C., Y.-K.M., H.P. All authors read and approved the final manuscript.
Data Availability
Data is available.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Young Hyo Kim and Sang-Myung Lee contributed equally.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-41429-1.
References
- 1.Reisberg B, et al. Diagnosis of Alzheimer’s disease. Report of an International Psychogeriatric Association Special Meeting Work Group under the cosponsorship of Alzheimer’s Disease International, the European Federation of Neurological Societies, the World Health Organization, and the World Psychiatric Association. Int. Psychogeriatr. 1997;9(Suppl 1):11–38. doi: 10.1017/S1041610297004675. [DOI] [PubMed] [Google Scholar]
- 2.Blennow K, de Leon MJ, Zetterberg H. Alzheimer’s disease. Lancet. 2006;368:387–403. doi: 10.1016/S0140-6736(06)69113-7. [DOI] [PubMed] [Google Scholar]
- 3.Cummings J, Lee G, Ritter A, Zhong K. Alzheimer’s disease drug development pipeline: 2018. Alzheimers Dement. (N Y) 2018;4:195–214. doi: 10.1016/j.trci.2018.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doody RS, et al. Phase 3 trials of solanezumab for mild-to-moderate Alzheimer’s diseas. e. N. Engl. J. Med. 2014;370:311–321. doi: 10.1056/NEJMoa1312889. [DOI] [PubMed] [Google Scholar]
- 5.Salloway S, et al. Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s disease. N. Engl. J. Med. 2014;370:322–333. doi: 10.1056/NEJMoa1304839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jansen WJ, et al. Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. J.A.M.A. 2015;313:1924–1938. doi: 10.1001/jama.2015.4668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klunk WE, et al. Imaging brain amyloid in Alzheimer’s disease with Pittsburgh Compound-B. Ann. Neurol. 2004;55:306–319. doi: 10.1002/ana.20009. [DOI] [PubMed] [Google Scholar]
- 8.Bullich S, et al. Optimized classification of 18F-Florbetaben PET scans as positive and negative using an SUVR quantitative approach and comparison to visual assessment. Neuroimage Clin. 2017;15:325–332. doi: 10.1016/j.nicl.2017.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morris E, et al. Diagnostic accuracy of (18)F amyloid PET tracers for the diagnosis of Alzheimer’s disease: a systematic review and meta-analysis. Eur. J. Nucl. Med. Mol. Imaging. 2016;43:374–385. doi: 10.1007/s00259-015-3228-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mattsson N, et al. CSF biomarkers and incipient Alzheimer disease in patients with mild cognitive impairment. J.A.M.A. 2009;302:385–393. doi: 10.1001/jama.2009.1064. [DOI] [PubMed] [Google Scholar]
- 11.Park SA, et al. Cerebrospinal Fluid Biomarkers for the Diagnosis of Alzheimer Disease in South Korea. Alzheimer Dis. Assoc. Disord. 2017;31:13–18. doi: 10.1097/WAD.0000000000000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chhatwal JP, et al. Temporal T807 binding correlates with CSF tau and phospho-tau in normal elderly. Neurology. 2016;87:920–926. doi: 10.1212/WNL.0000000000003050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jack CR, Jr., et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14:535–562. doi: 10.1016/j.jalz.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Landau SM, et al. Associations between cognitive, functional, and FDG-PET measures of decline in AD and MCI. Neurobiol. Aging. 2011;32:1207–1218. doi: 10.1016/j.neurobiolaging.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dickerson BC, et al. The cortical signature of Alzheimer’s disease: regionally specific cortical thinning relates to symptom severity in very mild to mild AD dementia and is detectable in asymptomatic amyloid-positive individuals. Cereb. Cortex. 2009;19:497–510. doi: 10.1093/cercor/bhn113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang MJ, et al. Oligomeric forms of amyloid-β protein in plasma as a potential blood-based biomarker for Alzheimer’s disease. Alzheimers Res. Ther. 2017;9:98. doi: 10.1186/s13195-017-0324-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mielke MM, et al. Plasma phospho-tau181 increases with Alzheimer’s disease clinical severity and is associated with tau- and amyloid-positron emission tomography. Alzheimers Dement. 2018;14:989–997. doi: 10.1016/j.jalz.2018.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olsson B, et al. CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: a systematic review and meta-analysis. Lancet Neurol. 2016;15:673–684. doi: 10.1016/S1474-4422(16)00070-3. [DOI] [PubMed] [Google Scholar]
- 19.Park JC, et al. Chemically treated plasma Aβ is a potential blood-based biomarker for screening cerebral amyloid deposition. Alzheimers Res. Ther. 2017;9:20. doi: 10.1186/s13195-017-0248-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adams DR, et al. Olfactory Dysfunction Predicts Subsequent Dementia in Older USAdults. J. Am. Geriatr. Soc. 2018;6:140–144. doi: 10.1111/jgs.15048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu N, Rao X, Gao Y, Wang J, Xu F. Amyloid-β deposition and olfactory dysfunction in an Alzheimer’s disease model. J. Alzheimers Dis. 2013;37:699–712. doi: 10.3233/JAD-122443. [DOI] [PubMed] [Google Scholar]
- 22.Kameshima N, Yanagisawa D, Tooyama I. β-Amyloid peptide (1-40) in the brain reaches the nasal cavity via a non-blood pathway. Neurosci. Res. 2013;76:169–172. doi: 10.1016/j.neures.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 23.Liu Z, et al. Development of a High-Sensitivity Method for the Measurement of Human Nasal Aβ42, Tau, and Phosphorylated Tau. J. Alzheimers Dis. 2018;62:737–744. doi: 10.3233/JAD-170962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Han C, et al. An adaptation of the Korean mini-mental state examination (K-MMSE) in elderly Koreans: Demographic influence and population-based norms (the AGE study) Arch. Gerontol. Geriatr. 2008;47:302–310. doi: 10.1016/j.archger.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 25.Ben Bouallègue, F., Mariano-Goulart, D., Payoux, P. & Alzheimer’s Disease Neuroimaging Initiative (ADNI). Comparison of CSF markers and semi-quantitative amyloid PET in Alzheimer’s disease diagnosis and in cognitive impairment prognosis using the ADNI-2 database. Alzheimers Res. Ther. 9, 32, 10.1186/s13195-017-0260-z (2017). [DOI] [PMC free article] [PubMed]
- 26.Schneider JA, Arvanitakis Z, Bang W, Bennett DA. Mixed brain pathologies account for most dementia cases in community-dwelling older persons. Neurology. 2007;69:2197–2204. doi: 10.1212/01.wnl.0000271090.28148.24. [DOI] [PubMed] [Google Scholar]
- 27.Toledo JB, et al. Nonlinear association between cerebrospinal fluid and Florbetapir F-18 β-amyloid measures across the spectrum of Alzheimer disease. J.A.M.A. Neurol. 2015;72:571–581. doi: 10.1001/jamaneurol.2014.4829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoo YK, et al. Ultra-sensitive detection of brain-derived neurotrophic factor (BDNF) in the brain of freely moving mice using an interdigitated microelectrode (IME) biosensor. Sci. Rep. 2016;6:33694. doi: 10.1038/srep33694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yagati AK, et al. Silver nanoflower-reduced graphene oxide composite based micro-disk electrode for insulin detection in serum. Biosens. Bioelectron. 2016;80:307–314. doi: 10.1016/j.bios.2016.01.086. [DOI] [PubMed] [Google Scholar]
- 30.Serby M, Corwin J, Conrad P, Rotrosen J. Olfactory dysfunction in Alzheimer’s disease and Parkinson’s disease. Am. J. Psychiatry. 1985;142:781–782. doi: 10.1176/ajp.142.6.781-a. [DOI] [PubMed] [Google Scholar]
- 31.Mesholam RI, Moberg PJ, Mahr RN, Doty RL. Olfaction in neurodegenerative disease: a meta-analysis of olfactory functioning in Alzheimer’s and Parkinson’s diseases. Arch. Neurol. 1998;55:84–90. doi: 10.1001/archneur.55.1.84. [DOI] [PubMed] [Google Scholar]
- 32.Roberts RO, et al. Association between olfactory dysfunction and amnestic mild cognitive impairment and Alzheimer disease dementia. J.A.M.A. Neurol. 2016;73:93–101. doi: 10.1001/jamaneurol.2015.2952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fukumoto H, et al. High-molecular-weight beta-amyloid oligomers are elevated in cerebrospinal fluid of Alzheimer patients. FASEB J. 2010;24:2716–2726. doi: 10.1096/fj.09-150359. [DOI] [PubMed] [Google Scholar]
- 34.Izzo NJ, et al. Alzheimer’s therapeutics targeting amyloid beta 1-42 oligomers II: Sigma-2/PGRMC1 receptors mediate Abeta 42 oligomer binding and synaptotoxicity. PLoS One. 2014;9:e111899. doi: 10.1371/journal.pone.0111899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim HY, et al. EPPS rescues hippocampus-dependent cognitive deficits in APP/PS1 mice by disaggregation of amyloid-β oligomers and plaques. Nat. Commun. 2015;6:8997. doi: 10.1038/ncomms9997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McKhann GM, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging–Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bordet R, et al. Towards the concept of disease-modifier in post-stroke or vascular cognitive impairment: a consensus report. BMC Med. 2017;15:107. doi: 10.1186/s12916-017-0869-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Knopman DS, et al. Development of methodology for conducting clinical trials in frontotemporal lobar degeneration. Brain. 2008;131:2957–2968. doi: 10.1093/brain/awn234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vasconcellos LF, Pereira JS. Parkinson’s disease dementia: Diagnostic criteria and risk factor review. J. Clin. Exp. Neuropsychol. 2015;37:988–993. doi: 10.1080/13803395.2015.1073227. [DOI] [PubMed] [Google Scholar]
- 40.Christensen KJ, Multhaup KS, Nordstrom S, Voss K. A cognitive battery for dementia: Development and measurement characteristics. Psychol. Asses. 1991;3:168–174. doi: 10.1037/1040-3590.3.2.168. [DOI] [Google Scholar]
- 41.Ahn HJ, et al. Seoul Neuropsychological Screening Battery-dementia version (SNSB-D): a useful tool for assessing and monitoring cognitive impairments in dementia patients. J. Korean Med. Sci. 2010;25:1071–1076. doi: 10.3346/jkms.2010.25.7.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cho DY, et al. Expression of dual oxidases and secreted cytokines in chronic rhinosinusitis. Int. Forum Allergy Rhinol. 2013;3:376–383. doi: 10.1002/alr.21133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is available.