Highlights
-
•
The majority of women do not have access to physical therapy for urinary incontinence in primary health centers.
-
•
Physical therapy intervention can be succssesfully implemented in primary health care centers.
-
•
The PFMT and bladder training was effective, with positive results as early as 6 weeks.
-
•
The protocols tested should be used in primary health centers.
Keywords: Urinary incontinence, Pelvic floor, Physical therapy modalities, Primary health care.
Abstract
Background
Although the efficacy of pelvic floor muscle training (PFMT) and bladder training are well established, there is a paucity of patient centered models using these interventions to treat women with UI at primary level of health assistance in Brazil.
Objective
To investigate the effectiveness of a physical therapy intervention to treat women with UI in primary health centers.
Methods
Pragmatic non-randomized controlled trial in which women with UI from the community participated in a supervised physical therapy program consisting of bladder training plus 12 weeks of PFMT, performed either at home or in the health center. Outcome measures were amount and frequency of urine loss measured by the 24-h pad-test and the 24-h voiding diary; secondary outcome was the impact of UI on quality of life measured by the ICIQ-SF. Outcomes were measured at baseline, at the 6th and 12th weeks of the intervention and 1 month after discharge.
Results
Interventions reduced the amount (pad-test, p = 0.004; d = 0.13, 95% CI = −0.23 to 0.49) and frequency of urine loss (voiding diary, p = 0.003; d = 0.51, 95%CI = 0.14 to 0.87), and the impact of UI on quality of life (ICIQ-SF, p < 0.001; d = 1.26, 95%CI = 0.87 to 1.66) over time, with positive effects from the 6th week up to 1 month for both intervention setting (home and health center), and no differences between them.
Conclusion
Interventions were effective, can be implemented in primary health centers favoring the treatment of a greater number of women who do not have access to specialized physical therapy.
Trial registration: RBR-8tww4y.
Introduction
Urinary incontinence (UI), defined as the involuntary loss of urine,1 is a chronic health condition that affects up to 69.0% of the female population,2, 3, 4 demands high treatment costs,5, 6, 7 high rates of sick leave,5, 8 and negatively impacts woman's quality of life.9 Therefore, UI is considered an important public health problem.10
The pelvic floor muscle training (PFMT) is the first-line treatment for women with UI due to its efficacy, low cost, lack of side effects and the absence of impact on subsequent treatments.11, 12, 13 Additionally, bladder training can potentiate the results obtained with the PFMT due to urgency and frequency symptoms, in women with mixed and urge incontinence.12 In countries like Brazil, the public health system offers limited access to this physical therapy treatment. Also, the number of physical therapists working in primary health centers still low and not well distributed across the country. Therefore, the majority of women with UI do not have access to this cost-effective treatment.14, 15
If the treatment of women with UI could also be effectively offered in primary health centers where the majority of the population has access, it would minimize the treatment costs for both, to the women with UI and to the health care system. Also, it would provide assistance to the majority of women with UI who do not have access to specialized physical therapy services.
The efficacy of the PFMT was proven by studies developed under well-controlled conditions,16 aimed to maximize the probability of observing the treatment effect when it exists. However, the results of such studies might have limited generalizability, once it does not account for specific factors related to the patient, the therapist, and the health care service.17 For example, patient's preferences regarding the setting to perform the PFMT, either at home or in the health center, might be a barrier or a facilitator to PFMT compliance.18, 19 Also, general physical therapists might find embarrassing to perform vaginal palpation since in Brazil not all of them are trained to do so. Therefore effectiveness, instead of only efficacy of the PFMT delivered at primary health centers should be addressed.
Effectiveness studies focus on the investigation of treatment effect under circumstances that more closely approximate the real world. It involves less standardized and controlled, more patient oriented treatment protocols, more heterogeneous patient samples, and delivery of the interventions in situations and settings where the compliance to the treatment can be facilitated.17, 20 Effectiveness studies are necessary because analysis of product evaluations for Health Technology Assessments found that efficacy data is often assumed to be effectiveness data, when in fact are not.17 Also, the clinical applicability of studies using an effectiveness approach is beginning to be considered more favorably by those who construct evidence-based guidelines.20
Therefore, the aim of this study was to investigate the implementation and effectiveness of a physical therapy intervention including PFMT and bladder training to treat women with UI in primary health centers in Brazil.
Method
Design, participants and settings
This was a pragmatic non-randomized controlled trial that investigated the effectiveness of service and patient oriented’ physical therapy intervention for community women with UI symptoms delivered at health centers. Intervention program was service and patient oriented regarding to: (a) participant's preference about the setting to perform the intervention, either at health center or at home; (b) pelvic floor muscle (PFM) contraction capacity evaluated by inspection over the underwear; (c) PFMT dose prescribed according to the participant's PFM endurance; (d) bladder training according to the participant's 24-h micturition diary.
All women who attended two primary care centers, from July 2010 to Oct 2011 were invited by community health agents or by nurses to answer the International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF) and signed the informed consent.21 In a second moment, women identified in the ICQ-SF as having UI, aged ≥ 18 years, and had never received physical therapy intervention for pelvic floor dysfunction were invited to participate in the study. Women who could not contract their PFM, were pregnant, presented symptoms of urinary infection, neurological disorders and/or difficulty understanding the treatment protocols were excluded and referred to the primary care physician for further consultation.
The intervention program was conducted in two community health centers in Belo Horizonte, Brazil, by a physical therapist with one-year experience in womens’ health physical therapy. This researcher was trained to perform participants’ assessment and intervention by the study project manager, a 20 year experienced women's health physical therapist, until the interrater reliability for the PFM contraction capacity and endurance were over 80.0%.
Participants’ physical therapeutic evaluation
Participants’ were interviewed about socio-demographic and clinical factors associated to UI symptoms, which were classified according to the answers to ICIQ-SF questionnaire. Then, they were educated about the structure and function of the pelvic floor and their relation to UI symptoms, and informed about the procedures for the 24-h pad test and the 24-h micturition diary.
After being verbally oriented about how to perform a correct PFM contraction,22 participants’ PFM contraction capacity and endurance were evaluated by pelvic floor inspection over the underwear. This procedure, specifically designed for this study, was as follows: participants lied in bed in supine position with bent knees, with women wearing their underwear. The physical therapist asked for a PFM contraction “as if holding urine” and observed any perineum displacement. PFM contraction capacity was rated as yes (able to contract) when any cranial displacement of the perineum was observed; or no (unable to contract) when no displacement of the perineum was observed, when caudal displacement of the perineum was observed (Bø et al.),22 or in cases in which the physical therapist was unsure about the perineum displacement. Women who could contract their PFM were further examined about the PFM endurance, i.e., the ability to sustain the PFM contraction, in seconds. They were then informed about their muscle endurance and that this was the time they should hold the contraction during the PFMT. Any doubts regarding the participants’ ability to correctly contract, and sustain the contraction of the PFM were solved at this time.
The concurrent validity of the pelvic floor inspection over the underwear was pilot tested against vaginal palpation by two independent examiners with 20 and 12 years experience in womens’ health physical therapy, who evaluated 17 women with UI, not included in the actual sample. Sensitivity was 0.88 with a positive predictive value of 1.00. Specificity was 1.00, with a negative predictive value of 0.33. Area under the receiver operating curve (ROC) was 0.93 (0.79–1.00).
Intervention
Participants who agreed to participate and signed the consent form were invited to choose one of the two settings to perform the PFMT: at the health center (HC) or at home (HM). For both settings, treatment comprised of the PFMT plus written instructions regarding how to perform the PFMT at home; bladder training consisting of information about adequate micturition habits and liquid intake based on their micturition diary; and a diary chart to track the compliance to the physical therapy intervention. The PFMT consisted of: (a) up to 10 PFM contractions sustained for each participants’ endurance (sec); (b) up to 10 fast PFM contractions (contract/relax) according to each participants endurance (repetition). The sustained PFM contractions were to be performed as strongly as possible, holding for the time of their muscle endurance (sec), three times per day, (in the morning, afternoon and at night, or according to participants preferences); 7 days per week, during 12 weeks. Participants were instructed to adequate contract their PFM, focusing the contraction on the PFM and avoiding visible contraction of synergistic muscles. When they could no longer hold the adequate contraction of the PFM, the PFMT was interrupted for that set and should be resumed later on as planned. The time (in sec) holding the contraction (PFM endurance) should gradually increase according to the participants’ perception of ability to hold the adequate contraction. Participants who chose training at home were followed up by weekly phone calls to improve compliance and to answer possible questions about their PFMT. The participants who chose training at the health center, performed the PFMT supervised by the physical therapist once a week, and exercised at home on the other days, as described for home setting. Questions regarding PFMT and bladder training (urinary symptoms) were solved by demand. Any adverse effect was to be reported by the participants.
Outcomes
Outcomes were measured at baseline, at the 6th and 12th weeks of the intervention and at 1 month after the end of treatment for all participants, by the same physical therapist. The primary outcome was the severity of UI symptoms, defined as the amount and frequency of urine loss during 24 h, measured by the 24-h pad test in grams (g)1, 23 and by the 24-h micturition diary, measured as the frequency of urine loss in 24 h (24 h frequency urine loss).1, 23 The pad test was performed in the same day as the micturition diary. Participants should use and replace pads according to their needs over the 24-h of the tests. Used pads should be folded and kept in a closed plastic bag in the refrigerator. On the next day, which was the second day of participants’ assessment, they should bring all the used pads as well a non-used one. Non-used pad were weighted using a precision scale; the used pads were counted and then weighted in the same scale; the 24 h pad-test result was the net weight from the sum of the used pads to the sum of the non-used ones. The micturition diary comprised of the following questions displayed in a table: micturition time (from the first to the last micturition of that day – over 24 h), urine volume measured in mL, time of liquid intake, volume of liquid intake measured in mL, time of urine loss (if any), time of urgency (if any). Secondary outcome was the impact of the UI symptoms on daily activities, measured by the total ICIQ-SF score (sum of the scores of the questions one, two and three). This is a valid questionnaire that was culturally adapted and translated into Brazilian Portuguese.21 The range of scores varies from 0 to 21, were higher scores indicate greater severity. Compliance to physical therapy intervention was checked every week either in person or by phone calls. Also, participants were asked to fill up a form containing the number of times per day they performed the PFMT.
Data analysis
Descriptive statistics characterized sample according to demographics, symptoms and severity of UI. Similarities between the participants’ characteristics were tested by the Chi-squared test, Fisher's exact test or Student's t-test. Repeated measures ANOVA tested within and between setting differences over time (baseline, 6 and 12 weeks of treatment, and 1 month after end of treatment). Multiple comparison tests were used as post hoc analyses; Bonferroni correction was applied when appropriate. A posteriori differential loss analysis was performed by the Chi-squared test, Fisher's exact test or Student's t-test, to test differences in participants who did and did not comply to the physical therapeutic intervention. The significance level was set at 0.05; data were processed by SPSS – 17.0.
The Ethics Research Committee of the Universidade Federal of Minas Gerais (UFMG), Belo Horizonte, MG, Brazil approved the study protocol (protocol number ETIC 0026.0.410.203-10). All women provided written informed consent before participating.
Results
Flow of participants
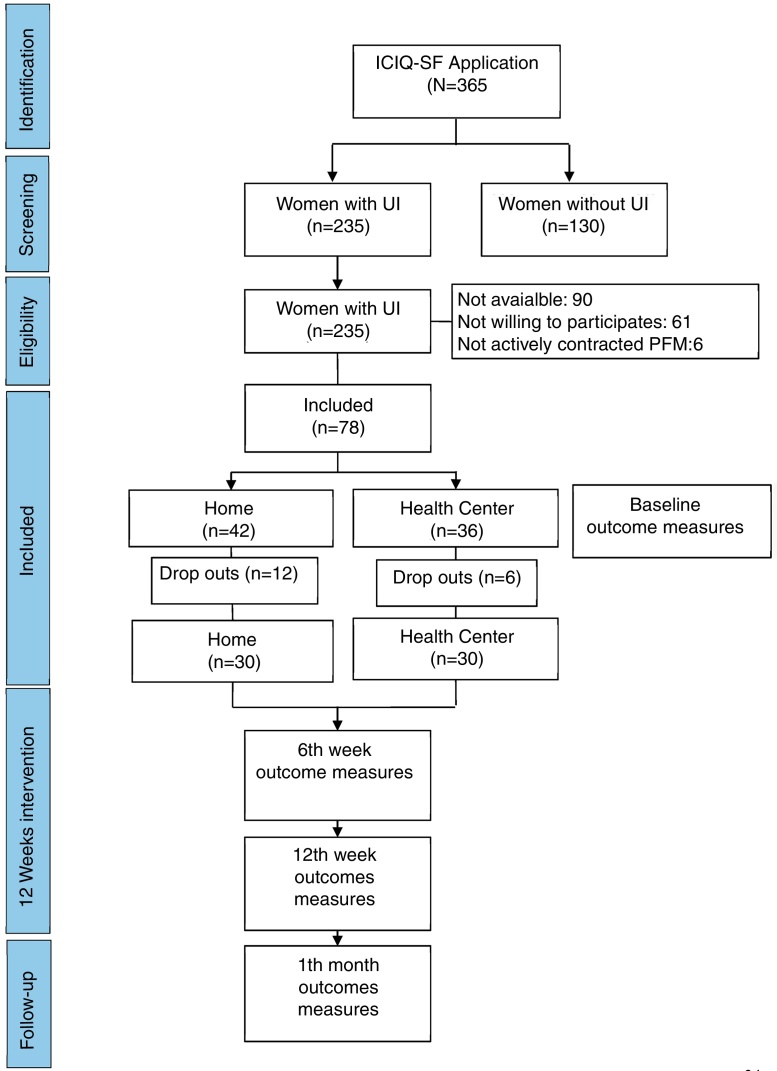
The flowchart of participants’ recruitment and dropouts is depicted in Fig. 1. During the study period, 365 women answered the ICIQ-SF and 235 (64.4%) reported symptoms of UI. Among the women who reported symptoms of UI, 90 (38.3%) could not be contacted, 61 (26%) refused to participate mostly due to work schedule, and 6 (2.6%) were not included because they could not actively contract their PFM.
Figure 1.
Design and flow of participants. PFM: pelvic floor muscles; HC: Health Center; HM: Home.
Compliance with physical therapy intervention and participants’ characteristics
A total of 78 (33.1%) women initiated treatment: 36 in the HC and 42 at HM. Up to two weeks of intervention, 6 (33.3%) participants in the HC and 12 (66.7%) in the HM dropped out the study. These women were similar regarding all characteristics, except occupation, in which those who dropped out presented significantly higher frequency of employed compared to the compliers (p = 0.028). Sixty participants, 30 in each treatment protocol, complied with 100% of the intervention. At baseline, participants were statistically similar regarding the socio-demographic and clinical variables (Table 1). The most prevalent symptoms of UI were related to mixed UI reported by 42 (70.0%) participants, followed by exclusive symptoms of stress incontinence in 13 (21.7%) participants and the exclusive symptom of urge UI in 5 (8.3%) participants.
Table 1.
Socio-demographic and clinical characteristics of the participants by settings (N = 60).
| HM (n = 30) | HC (n = 30) | p-Value | |
|---|---|---|---|
| Age (years) – mean (SD) | 55.2 (9.6) | 55.6 (12.2) | 0.888*** |
| Marital status – n (%) | 0.930* | ||
| Single | 2 (6.7) | 1 (3.3) | |
| Married | 17 (56.6) | 15 (43.3) | |
| Divorced | 6 (20.0) | 7 (23.3) | |
| Widowed | 5 (16.7) | 7 (23.3) | |
| Educational level – n (%) | |||
| Under 8 years | 16 (53.3) | 17 (56.7) | 0.795** |
| 8 or more years | 14 (46.7) | 13 (43.3) | |
| Occupation – n (%) | |||
| Retired | 10 (33.3) | 8 (26.7) | 0.105* |
| Housewife | 15 (50.0) | 9 (30.0) | |
| Employed | 5 (16.7) | 11 (36.7) | |
| Unemployed | 0 (0) | 2 (6.7) | |
| Hormone status – n (%) | |||
| Premenopausal | 9 (30.0) | 8 (26.6) | 0.288* |
| Postmenopausal | 21 (70.0) | 22 (73.4) | |
| Hormone replacement – n (%) | |||
| Yes | 1 (4.8) | 0 (0) | 0.488* |
| No | 20 (95.2) | 22 (100.0) | |
| Obstetric history – mean (SD) | |||
| Pregnancies | 3.8 (2.6) | 3.9 (2.6) | 0.845*** |
| Vaginal deliveries | 2.9 (1.9) | 3.1 (2.8) | 0.749*** |
| Cesarean deliveries | 0.4 (0.8) | 0.6 (0.9) | 0.432*** |
| Abortions | 0.5 (1.8) | 0.3 (0.5) | 0.510*** |
| PFM endurance (sec) mean (SD) | 4.70 (1.37) | 4.77(1.33) | 0.580*** |
| 24 h pad test (g) mean (SD) | 13.7 (23.7) | 16.3 (35.1) | 0.726*** |
| 24 h frequency urine loss mean (SD) | 2 (2.3) | 2 (2.6) | 0.741*** |
| ICIQ-SF mean (SD) | 12.2 (4.9) | 12.2 (4.1) | 0.849*** |
F-test.
Chi-square test.
Student's t-test. HM, Home; HC, Health Center; sec, seconds. PFM: pelvic floor muscles.
Effectiveness of intervention
Primary outcomes
There was a significant reduction in the severity of urine loss with reduction in the 24-h pad test (p = 0.004; d = 0.13, 95% CI = −0.23 to 0.49) and in the 24-h frequency of urine loss (p = 0.003; d = 0.51, 95%CI = 0.14 to 0.87) over time. These results were identified from the 6th week intervention for both treatment settings (Table 2, Table 3). Additionally, the positive changes in these outcomes remained at 1 month after the end of intervention (Table 3). There were no significant differences between settings (HC and HM) for the 24-h pad test (p = 0.73) and for the 24-h micturition diary (p = 0.74) over time (Table 4). The estimated treatment effect sizes (D’Cohen) and its precision (95% confidence interval) for each treatment setting are also displayed in Table 4.
Table 2.
Changes in the outcomes over time for the total sample (within groups comparison) (N = 60).
| Outcome | N | Baseline | 6 weeks | 12 weeks | 1 month | p-Value* |
|---|---|---|---|---|---|---|
| 24 h pad test (g) mean (SD) | 58 | 10.8 (17.3) | 7.0 (14.5) | 4.6 (11.1) | 5.3 (12.0) | 0.004 |
| 24 h frequency urine loss mean (SD) | 60 | 2.0 (2.4) | 1.4 (2.5) | 0.9 (2.3) | 0.8 (2.2) | 0.003 |
| ICIQ-SF mean (SD) | 60 | 12.2 (4.5) | 8.3 (5.5) | 6.0 (6.1) | 5.6 (6.9) | <0.001 |
F-test; g, grams; N, sample size; SD, standard deviation.
Table 3.
Multiple comparisons over time for each outcome for the total sample, collapsed by setting (N = 60).
| Mean difference | SE | p-Value | 95% CI | |
|---|---|---|---|---|
| 24-h pad test (g) | ||||
| Baseline | ||||
| 6 weeks | 3.7 | 1.4 | 0.010 | 0.9 to 6.5 |
| 12 weeks | 6.2 | 1.8 | 0.001 | 2.5 to 9.9 |
| 1 month | 5.5 | 2.0 | 0.007 | 1.5 to 9.5 |
| 6 weeks | ||||
| 12 weeks | 2.5 | 1.5 | 0.100 | −0.5 to 5.4 |
| 1 month | 1.8 | 1.7 | 0.293 | −1.6 to 5.1 |
| 12 weeks | ||||
| 1 month | −0.7 | 0.6 | 0.220 | −1.8 to 0.4 |
| 24-h frequency of urine loss | ||||
| Baseline | ||||
| 6 weeks | 0.6 | 0.3 | 0.053 | 0.0 to 1.1 |
| 12 weeks | 1.0 | 0.4 | 0.007 | 0.3 to 1.8 |
| 1 month | 1.2 | 0.4 | 0.003 | 0.4 to 1.9 |
| 6 weeks | ||||
| 12 weeks | 0.5 | 0.3 | 0.065 | 0.0 to 1.0 |
| 1 month | 0.6 | 0.3 | 0.015 | 0.1 to 1.1 |
| 12 weeks | ||||
| 1 month | 0.1 | 0.1 | 0.167 | −0.1 to 0.3 |
| ICIQ-SF total score | ||||
| Baseline | ||||
| 6 weeks | 3.9 | 0.6 | <0.001 | 2.7 to 5.1 |
| 12 weeks | 6.2 | 0.7 | <0.001 | 4.8 to 7.6 |
| 1 month | 6.6 | 0.7 | <0.001 | 5.2 to 8.1 |
| 6 weeks | ||||
| 12 weeks | 2.3 | 0.6 | 0.001 | 1.0 to 3.6 |
| 1 month | 2.7 | 0.7 | <0.001 | 1.4 to 4.1 |
| 12 weeks | ||||
| 1 month | 0.4 | 0.4 | 0.245 | −0.3 to 1.2 |
SE, Standard Error; CI, Confidence Interval; UI, Urinary Incontinence; ICIQ-SF: International Consultation on Incontinence Questionnaire-Short.
Table 4.
Changes in the outcomes over time according to settings (within and between settings comparisons) (N = 60).
| Outcome | Baseline | 6 weeks | 12 weeks | 1 month | p-Value* | Effect size# (95% CI) |
|---|---|---|---|---|---|---|
| 24-h pad-test(g) mean (SD) | ||||||
| HC (n = 28) | 16.3 (35.1) | 8.1 (16.4) | 14.1 (46.5) | 15.3 (46.5) | 0.73 | 0.02 (−0.34 to 0.38) |
| HM (n = 30) | 13.7 (23.7) | 13.8 (34.7) | 8.8 (30.3) | 6.2 (16.3) | 0.37 (0.01 to 0.74) | |
| 24-h frequency urine loss mean (SD) | ||||||
| HC (n = 30) | 2.0 (2.6) | 1.3 (2.2) | 0.7 (1.2) | 0.8 (1.3) | 0.74 | 0.57 (0.21 to 0.95) |
| HM (n = 30) | 2.0 (2.3) | 1.5 (2.9) | 1.2 (3.1) | 0.8 (3.0) | 0.46 (0.09 to 0.82) | |
| ICIQ-SF mean (SD) | ||||||
| HC (n = 30) | 12.2 (4.1) | 8.1 (4.8) | 6.6 (6.1) | 5.6 (5.8) | 0.85 | 1.33 (0.93 to 1.73) |
| HM (n = 30) | 12.2 (4.9) | 8.5 (6.2) | 5.4 (6.2) | 5.6 (6.2) | 1.21 (0.82 to 1.60) | |
F-test, p-values correspond to between setting comparison; HM, Home; HC, Health Center; g, grams; N, sample size; SD, standard deviation.
Treatment effect sizes (D′ Cohen) and its precision (95% confidence interval) correspond to within setting comparison.
Secondary outcome
There was a significant reduction in the ICIQ-SF total score (p < 0.001; d = 1.26, 95%CI = 0.87 to 1.66) over time, identified from the 6th week of intervention for both treatment settings (Table 2, Table 3). These positive changes remained at 1 month after the end of intervention (Table 3). There were no significant differences between HC and HM settings for the ICIQ-SF total score (p = 0.85) (Table 4).
Discussion
Main findings
The physical therapy intervention investigated in this study was effective for women with symptoms of either mixed, stress or urge UI. Positive results were observed from the 6th week intervention and remained up to one month after treatment, despite of the setting to perform the PFMT. Physical therapy intervention was well received with no reports of adverse effects.
Strengths and limitations
As far as we know, this is the first study reporting effectiveness data about a physical therapy intervention for women with UI at primary health centers in Brazil. Effectiveness studies, also called pragmatic studies, assesses intervention under real-life conditions, in terms that matter to the patient.17, 20 The investigated protocols were designed to attend both the primary health care service and participants’ needs regarding the ability of general physical therapists to evaluate the pelvic floor as well as regarding setting preferences and dose specificity, respectively. The results presented are promising since women who had complied the treatment start to benefit from it as early as 6 weeks of intervention up to one month after discharge, despite treatment setting. However results must be interpreted with caution in light of methodological limitations. Being a study with small sample size the results have limited generalizability, mostly to post menopausal women who do not use hormone therapy, with mild UI symptoms, who can actively contract their PFM, and motivated to manage the treatment in their routine. The assessment methods of the primary outcomes, especially in regard to measuring and filling error, might also be a study limitation. The majority of participants has low level of education and might have difficulties in filling up the micturition diary. The sample was not randomized. This might have posed a selection bias, driving women with a self-care positive attitude to the HM, while women who need external support to comply to treatment might have been driven to the HC group. Yet, this bias may have favored the effectiveness of the patient oriented physical therapy intervention, as it accounts for personal factors that could not be considered in randomized trials. Also, the long-term effects of this physical therapy intervention delivered in primary health care centers should be investigated in future studies.
Interpretation
As hypothesized, the physical therapy intervention was effectively implemented in primary health care centers. Improvements in the UI symptoms and impact of these symptoms on QoL were observed at the 6th week of intervention for all outcomes, for both treatment settings. This is important since most studies report results of the PFMT applied for more than 6 weeks.24 A systematic review of twenty-four studies analyzing optimal PFMT regimens for women with stress UI reported that only 3 described positive results from a short term (1, 4 and 6 weeks) PFMT program. Positive effects ranged from 8 weeks up to 3–6 months of PFMT.24 Another systematic review suggested that the effects of supervised PFMT programs for women with stress UI might require treatment of at least 3 months.25 The present results suggest that patient oriented dose specific PFMT might achieve positive results more quickly. Dose specificity is an important issue in PFMT that needs further investigation because variations in the programs make comparative analyses of their potential effectiveness difficult.25 We believe that the evaluation of the PFM function, either via digital palpation or inspection, is the key to prescribing dose specific PFMT and to subsequently guarantee its effectiveness. In addition, from a public health perspective, it is worthwhile offering educational programs associated with PFMT and bladder training to women with IU in primary health centers. A recent study showed that an educational program delivered in a primary health center in Brazil increased women's knowledge about the location, (dys)functions of the PFM, and treatment options. Nevertheless, urinary incontinence complaints were not reduced.26 Therefore, the association of both interventions, education and PFMT as reported in the present study may improve results toward urinary continence.
The effects of the techniques that comprised the present physical therapy intervention, PFMT and bladder training, were previously tested under well-controlled conditions. They are recommended by the International Continence Society12 as the first line conservative treatment of women with UI. In the present study to test its effectiveness, protocols were adapted regarding the pelvic floor inspection over the underwear that was designed specifically for this study. It is a simplified method that was tested valid to identify PFM contraction capacity. Also, adequate interrater reliability can be achieved. This was important since physical therapists who work at primary health centers in Brazil are generalists. Many of them are not trained to perform vaginal palpation of the pelvic floor. This pelvic floor inspection method might be a fundamental aspect of the PFMT to women with UI delivered in primary care centers. It allows the dose specificity of the PFMT, and can be performed by general physical therapists who might feel embarrassed performing vaginal palpation. The dose specificity seems to be fundamental for the success of the physical therapy treatment.24, 27
The PFMT was offered in settings according to participants’ preference either in the HC under direct physical therapeutic supervision or at home with supervision provided by weekly phone calls. It was well received by participants with no reports of adverse effects. Previous studies estimate that 64.0% of women comply to PFMT in the short term but only 23.0% in the long term.28, 29 In the present study, the differential loss of follow-up analysis indicated that women did dropped out the study or did not comply to the physical therapy intervention mostly due to work schedule restrictions. This suggests that the ease of access to the PFMT is critical when offering this treatment to women with UI in primary health centers. The dose of the PFMT was also patient oriented. It was established according to the participants’ PFM contraction capacity and endurance, allowing dose-specific PFMT and therefore to the effectiveness of the intervention.
In this pragmatic study, sample was not randomized. This might have posed a bias selection, driving women with a self-care positive attitude to the home setting, while women who need an external support to comply to treatment might have driven to the health center. Yet, this bias may had favored the effectiveness of patient oriented intervention.
We did not observe differences between participants’ outcomes who performed the PFMT at home or in the health centers. It is important to note that both intervention protocols were designed to provide the best intervention to the participants’ needs/preferences according to (a) setting; (b) PFM contraction capacity; (c) PFMT dose specific; (d) bladder training according to participant's micturition diary. Also, it was granted that all participants received individual instructions to correctly perform the PFM contractions and to ensure that they understood what they should perform at home.28, 29 Furthermore, in order to improve compliance we did provide weekly physical therapy supervision to all participants, either in person at the health centers or by phone calls at home. This is in accordance to Hay-Smith et al.30 that have indicated better results of PFMT when health professional contact is more frequent. Therefore, the lack of differences between treatment settings was not a surprising result. What should be highlighted is that the physical therapy intervention delivered at the primary level showed positive effects as early as 6 week of intervention and endure up to 1 month after intervention. These positive effects were observed for the primary and secondary outcomes, demonstrating the effectiveness of the physical therapy intervention to women with UI delivered in primary care centers.
Conclusion
The physical therapy intervention comprised of PFMT plus bladder training was successfully implemented in primary health centers and was effective to treat women with UI, showing positive results as early as 6 weeks intervention up to one month after discharge. Therefore, due to its potential to reduce costs to both women and the health care system, its implementation should be considered by physical therapists and health care managers at the primary health centers.
Contributions to authorship
EMF and RFS conceived the idea and designed the study; EMF, RFS and CTV wrote the protocol; CTV supervised participants, follow-up and collected the data; EMF and RFS performed the data analysis; CTV and FS participated in the inter-reliability testing of PFM evaluation and wrote the manuscript with the input of other co-authors. All authors read and approved the final version.
Funding
No funding.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgements
We acknowledge the community health agents and nurses of the primary care centers were the data was collected. Raquel Gontijo, Maria Cristina Cruz and Rafaela Newmayr for their support to the first author during the absence of the coordinator due to health issues.
Footnotes
This paper is part of a Special Issue on Women's Health Physical Therapy.
References
- 1.Haylen B.T., Ridder D., Freeman R.M. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20. doi: 10.1002/nau.20798. [DOI] [PubMed] [Google Scholar]
- 2.Cerruto M.A., D’Elia C., Aloisi A., Fabrello M., Artibani W. Prevalence, incidence and obstetric factors’ impact on female urinary incontinence in Europe: a systematic review. Urol Int. 2013;90:1–9. doi: 10.1159/000339929. [DOI] [PubMed] [Google Scholar]
- 3.Bedretdinova D., Fritel X., Panjo H., Ringa V. Prevalence of female urinary incontinence in the general population according to different definitions and study designs. Eur Urol. 2016;69:256–264. doi: 10.1016/j.eururo.2015.07.043. [DOI] [PubMed] [Google Scholar]
- 4.Reigota R.B., Pedro A.O., Machado V.S.S., Costa-Paiva L., Pinto-Neto A.M. Prevalence of urinary incontinence and its association with multimorbidity in women aged 50 years or older: a population-based study. Neurourol Urodyn. 2016;35:62–68. doi: 10.1002/nau.22679. [DOI] [PubMed] [Google Scholar]
- 5.Milsom I., Coyne K.S., Nicholson S., Kvasz M., Chen C., Wein A.J. Global prevalence and economic burden of urgency urinary incontinence: a systematic review. Eur Urol. 2014;65:79–95. doi: 10.1016/j.eururo.2013.08.031. [DOI] [PubMed] [Google Scholar]
- 6.Moore K.H., Wagner T.H., Subak L.L., Wachter S., Dudding T., Hu T.-W. Economics of urinary & faecal incontinence, and prolapse. In: Abrams P., Cardozo L., Khoury S., Wein A., editors. Incontinence: 5th International Consultation on Incontinence. 5a ed. Health Publication; Paris: 2013. pp. 1829–1861. [Google Scholar]
- 7.DATASUS. SUS hospital procedures – by place of hospitalization – Brazil – Cumulative from January 2016 to December 2016. Available from: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/qiuf.def Accessed 28.03.17.
- 8.Brazil. Ministry of Social Security. Safety and Occupational health. Available from: http://www.previdencia.gov.br/wp-content/uploads/2013/05/Auxilio-Doença-Previdenciario_2016_completo_CID.pdf Accessed 28.03.17.
- 9.Nyström E., Sjöström M., Stenlund H., Samuelsson E. ICIQ symptom and quality of life instruments measure clinically relevant improvements in women with stress urinary incontinence. Neuroulol Urodyn. 2015 Nov;34(8):747–751. doi: 10.1002/nau.22657. [DOI] [PubMed] [Google Scholar]
- 10.Milsom I., Altman D., Cartwright R. Epidemiology of urinary incontinence (UI) and other lower urinary tract symptoms (LUTS), pelvic organ prolapse (POP) and anal (AI) incontinence. In: Abrams P., Cardozo L., Khoury S., Wein A., editors. Incontinence: 5th International Consultation on Incontinence. 5a ed. Health Publication; Paris: 2013. pp. 15–107. [Google Scholar]
- 11.Bø K., Hagen R.H., Kvarstein B., Jørgensen J., Larsen S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: III. Effects of two different degrees of pelvic floor muscle exercises. Neurourol Urodyn. 1990;9:489–502. [Google Scholar]
- 12.Moore K., Dumoulin C., Bradley C. Adult conservative management. In: Abrams P., Cardozo L., Khoury S., Wein A., editors. Incontinence: 5th International Consultation on Incontinence. 5a ed. Health Publication; Paris: 2013. pp. 1101–1227. [Google Scholar]
- 13.Dumoulin C., Hay-Smith J., Mac Habbée Séguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2014;14(May (5)) doi: 10.1002/14651858.CD005654.pub3. CD005654. [DOI] [PubMed] [Google Scholar]
- 14.Spedo S.M., Pinto N.R.S., Tanaka O.Y. O difícil acesso a serviços de média complexidade do SUS: o caso da cidade de São Paulo, Brasil. Physis [Internet] 2010;20(3):953–972. [cited 29.03.17] [Google Scholar]
- 15.Garcia-Subirats I., Vargas I., Mogollón-Pérez A.S. Barriers in access to healthcare in countries with different health systems. A cross-sectional study in municipalities of central Colombia and north-eastern Brazil. Soc Sci Med. 2014;106:204–213. doi: 10.1016/j.socscimed.2014.01.054. [DOI] [PubMed] [Google Scholar]
- 16.Dumoulin C., Hay-Smith J., Mac Habbée Séguin G., Mercier J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: a short version Cochrane systematic review with meta-analysis. Neurourol Urodyn. 2015;34(April (4)):300–308. doi: 10.1002/nau.22700. [DOI] [PubMed] [Google Scholar]
- 17.Singal A.G., Higgins P.D.R., Waljee A.K. A primer on effectiveness and efficacy trials. Clin Transl Gastroenterol. 2014;5(January (1)):e45. doi: 10.1038/ctg.2013.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hay-Smith J., Dean S., Burgio K., McClurg D., Frawley H., Dumoulin C. Pelvic-floor-muscle-training adherence “modifiers”: a review of primary qualitative studies – 2011 ICS State-of-the-Science Seminar Research Paper III of IV. Neurourol Urodyn. 2015;34(7):622–631. doi: 10.1002/nau.22771. [DOI] [PubMed] [Google Scholar]
- 19.Frawley H.C., McClurg D., Mahfooza A., Hay-Smith J., Dumoulin C. Health professionals’ and patients’ perspectives on pelvic floor muscle training adherence – 2011 ICS State-of-the-Science Seminar Research Paper IV of IV. Neurourol Urodyn. 2015;34(7):632–639. doi: 10.1002/nau.22774. [DOI] [PubMed] [Google Scholar]
- 20.Fritz J.M., Cleland J. Effectiveness versus efficacy: more than a debate over language. J Orthop Sports Phys Ther. 2003;33(April (4)):163–165. doi: 10.2519/jospt.2003.33.4.163. [DOI] [PubMed] [Google Scholar]
- 21.Tamanini J.T.N., Dambros M., D’Ancona C.A.L., Palma P.C.R., Netto N.R. Validation of the “International Consultation on Incontinence Questionnaire – Short Form” (ICIQ-SF) for Portuguese. Rev SaúdePública. 2004;38(3):438–444. doi: 10.1590/s0034-89102004000300015. [DOI] [PubMed] [Google Scholar]
- 22.Bø K., Sherburn M., Vodušek D.B. Measurement of pelvic floor muscle function and strength and pelvic organ prolapse. In: Bø K., editor. Evidence-Based Physical Therapy for the Pelvic Floor: Bridging Science and Clinical Practice. 2a ed. Elsevier; 2015. pp. 47–53. [Google Scholar]
- 23.Staskin D., kelleher C., Bosch R. Initial assessment of Urinary Incontinence in Adult Male and Female Patients. In: Abrams P., Cardozo L., Khoury S., Wein A., editors. Incontinence: 5th International Consultation on Incontinence. 5a ed. Health Publication; Paris: 2013. pp. 361–388. [Google Scholar]
- 24.Dumoulin C., Glazener C., Jenkinson D. Determining the optimal pelvic floor muscle training regimen for women with stress urinary incontinence. Neurourol Urodyn. 2011;30(5):746–753. doi: 10.1002/nau.21104. [DOI] [PubMed] [Google Scholar]
- 25.Dumoulin C., Hay Smith J., Habeé-Seguin G.M., Mercier J. Pelvic floor muscle training versus no treatment, or in active control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2014;(1) doi: 10.1002/14651858.CD005654.pub3. CD005654. [DOI] [PubMed] [Google Scholar]
- 26.de Andrade R.L., Bø K., Antonio F.I. An education program about pelvic floor muscles improved women's knowledge but not pelvic floor muscle function, urinary incontinence or sexual function: a randomised trial. J Physiother. 2018 doi: 10.1016/j.jphys.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 27.Jette A.M. The importance of dose of a rehabilitation intervention. Phys Ther. 2017;97(11):1043. doi: 10.1093/ptj/pzx085. [DOI] [PubMed] [Google Scholar]
- 28.Felicíssimo M.F., Carneiro M.M., Saleme C.S., Pinto R.Z., Fonseca A.M.R.M., Silva-Filho A.L. Intensive supervised versus unsupervised pelvic floor muscle training for the treatment of stress urinary incontinence: a randomized comparative trial. Int Urogynecol J. 2010;21(7):835–840. doi: 10.1007/s00192-010-1125-1. [DOI] [PubMed] [Google Scholar]
- 29.Parkkinen A., Karjalainen E., Vartiainen M., Penttinen J. Physiotherapy for female stress urinary incontinence: individual therapy at the outpatient clinic versus home-based pelvic floor training: a 5-year follow-up study. Neurourol Urodyn. 2004;23(7):643–648. doi: 10.1002/nau.20065. [DOI] [PubMed] [Google Scholar]
- 30.Hay-Smith J., Herderschee R., Dumoulin C., Herbison P. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women: an abridged Cochrane systematic review. Eur J Phys Rehabil Med. 2012;48(4):689–705. [PubMed] [Google Scholar]