Abstract
The morbidity of invasive aspergillosis in burn patients is low but the diagnosis is difficult and the mortality rate is high. A severe burned patient at the Vietnam National Institute of Burn was suspected of fungal wound infection (FWI) with fungal growth on the wound. The diagnosis of FWI caused by Aspergillus fumigatus was made by isolation and histological examination. This may be the first reported case of FWI caused by Aspergillus fumigatus in Vietnam.
Keywords: Burns, Burn wound infections, Aspergillosis, Aspergillus fumigatus, Vietnam
1. Introduction
Due to thermal damage to the skin barrier, burn patients are at high risk of getting wound infections which comprise the three-quarters of deaths among them [1]. The most common responsible agent of wound infection is bacteria followed by fungi, virus [2]. Fungal wound infection (FWI) is uncommon but has a high rate of mortality, especially aspergillosis (may be as high as 87.1%) [3]. Diagnosis of FWI is difficult due to atypical clinical symptoms and the need for biopsy to take viable tissue [4] so the prevalence of FWI may be underestimated, yet may be as high as 13% [3]. For most patients with FWI the responsible fungi cannot be seen by the naked eye but in some cases, the fungal burden is so significant that they can be seen macroscopically [5], however, the precise identification of responsible agents is difficult with conventional methods [6]. Vietnam is a developing country and people are at higher risk of burn injuries compared to those living in developed countries [7]. There are thousands of burn injuries annually and most severe burn patients who live in northern Vietnam are transferred to Vietnam National Institute of Burn (NIB). Nevertheless, there have been no reports of FWI in Vietnam, especially those caused by Aspergillus. This may reflect the lack of awareness or reluctance to look for FWI. Here we report a case of FWI in a severe burn patient at NIB caused by Aspergillus fumigatus which spread on the surface and infiltrated the wound.
2. Case
A 61-year-old male admitted to Vietnam NIB with burns estimated to 50% of total body surface area (41% full thickness) including face, trunk, limbs and inhalation injury (day 0). After recovering from shock during the first two days he sustained an infection from the day +3 with fever (temperature higher than 39 °C) and wet necrosis of the lesions even though he was under treatment of broad-spectrum antibiotics (Ciprofloxacin, Meropenem, Piperacillin, Tazobactam). On the day+ 4 some samples (oropharyngeal secretion, feces, urine, wound swabs and blood) were taken to screen for fungi. Candida tropicalis was isolated from the gastrointestinal tract, urine and wound swabs and the patient received intravenous fluconazole from day +8 with loading dose of 800 mg for the first day and 400 mg per day for the following day. On the day +8 many blue patches appeared on the surface of burn lesions (Fig. 1) so a skin biopsy was taken for fungal culture and histopathological examination. Some hyphae and conidia of Aspergillus were discovered on the slide stained with Periodic acid Schiff (Fig. 2) and a strain of Aspergillus was isolated from the biopsy specimen. The isolated strain was subjected to molecular analysis by sequencing internal transcribed spacer (ITS) region and then identified as Aspergillus fumigatus (the sequence generated from ITS was submitted to GenBank under the code MH932411). With the aggressive progression of the infection, the patient was unable to recover and died on the day+ 10 before appropriate treatment was initiated due to the incubation time (two days) of the culture.
Fig. 1.
Blue patches suspected of fungal infection on the surface of burn lesions (day+ 8).
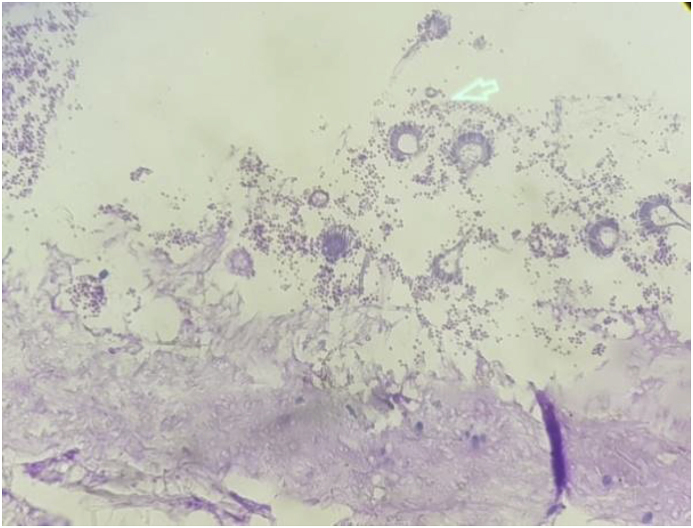
Fig. 2.
Hyphae and conidia (arrow) of Aspergillus on slide stained with Periodic acid Schiff (day+ 8). A high-resolution version of this slide for use with the Virtual Microscope is available as eSlide: VM05638.
3. Discussion
Fungal infection in burn patients compose of fungal wound colonization (FWC) (fungus is isolated on the surface of burn or non-sterile samples such as sputum, urine, stool …); FWI (identification of microorganisms in viable tissue) and fungemia (fungus is isolated in the blood). FWI and fungemia are considered invasive infection [4]. This patient had both FWC (with Candida in the urine, feces and wound swabs) and FWI (caused by A. fumigatus). Although invasive candidiasis was suspected (severe infections with high fever, the worsening progression of the wounds despite a course of broad-spectrum antibiotics and negative bacterial culture) [8] but Candida was only found on non-sterile samples. With the detection of A. fumigatus in biopsy specimens by culture and histopathology the diagnosis of invasive aspergillosis had been made [9]. The discrimination between FWI and FWC is difficult and biopsy samples are needed, but this sampling requires an invasive technique that has not been routinely performed in clinical practices [10]. For the current patient, the biopsy samples were only taken after the occurrence of fungi on the surface of lesions that had raised the suspicion of FWI. Although galactomannan (GM) can help in diagnosing FWI due to Aspergillus [11] this assay was not available in Vietnam. Besides, GM assay may not be cost-effective and has little impact on clinical decision making [12] and for most burn patients this assay may not be associated with FWI or FWC [13]. It was notable that the patient had fungal colonies on the surface of lesions and conidia of Aspergillus was found on histologic examination, a very rare phenomenon. In 2014 Resch, T. R et al. reported a case of fungal burn infection with fungal colonies easily seen at the bedside [5].
The source of infection maybe conidia of Aspergillus from the surrounding air that fell and invaded the wound [14], which differed from an infection caused by Candida where the responsible agents were mainly endogenous in origin and need time to translocation from colonized sites (gastrointestinal or respiratory tracts) to the wound [15]. There have been some reports showing the genotypic matches between Aspergillus strains isolated from patients and from the environment [16] and measures to protect the wound from Aspergillus colonization were considered the only reliable method to prevent invasive aspergillosis for burn patients [17].
For identification of responsible agents, even in most recent reports of FWI the speciation of Aspergillus, has been performed using phenotypic examination [11,18]. Identification of Aspergillus based on phenotypic characteristics is simple and low cost but may lead to confusion due to the variability in the phenotypic characteristics of fungi. At present, the best approach to species differentiation is a polyphasic approach incorporating the phenotypic characters and molecular data [6]. The identification of the isolated strain in the present study was done by both phenotypic and molecular tool with analyzing the ITS gene, one of the most useful genes for species identification of fungi [19].
The treatment of FWI caused by Aspergillus or primary cutaneous aspergillosis is difficult and may require the combination of general (voriconazole) and local antifungal (amphotericin B) drugs [18]. Though the patient was treated with fluconazole, a drug used for preemptive therapy when C. tropicalis was isolated; a FWI still occurred and progressed severely. Triazoles are considered the drug of choice for most patients with invasive aspergillosis however fluconazole has no effect on Aspergillus [9].
In conclusion, we report a case of fungal wound infection caused by Aspergillus fumigatus in a severe burn patient with gross appearance of fungal colonies on the surface of lesions. The responsible agent was confirmed with histologic examination and identified by the molecular tool. This may be the first reported case of fungal wound infection caused by Aspergillus fumigatus in Vietnam. With the higher risk of burn injuries and the lack of supporting tests for definite diagnosis, there would be more undiagnosed patients with FWI in Vietnam. This case report emphasizes the need for performing surveillance tests and effective measures to prevent invasive aspergillosis for burn patients.
Conflict of interest
This work was partially supported by the Vietnam Ministry of National Defence, (grant no. 2017.75.054, to TAL).
Ethical form
Written informed consent was obtained from the legal guardian(s) for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Acknowledgements
The authors are grateful to Mr. Robert Mayrhofer for revising the English text.
References
- 1.Revathi G., Puri J., Jain B. Bacteriology of burns. Burns. 1998;24(347–9) doi: 10.1016/s0305-4179(98)00009-6. [DOI] [PubMed] [Google Scholar]
- 2.Capoor M.R., Sarabahi S., Tiwari V.K., Narayanan R.P. Fungal infections in burns: diagnosis and management. Indian J. Plast. Surg. 2010;43(Suppl):S37–S42. doi: 10.4103/0970-0358.70718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ali M., Reza M., Gholipourmalekabadi M., Samadikuchaksaraei A. The prevalence of fungal infections in a level I Iranian burn hospital. 2013;7(6):829–833. [Google Scholar]
- 4.Horvath E., Murray C., Vaughan G., Chung K., Hospenthal D., Wade C. Fungal wound infection (not colonization) is independently associated with mortality in burn patients. Ann. Surg. 2007;245(6):978–985. doi: 10.1097/01.sla.0000256914.16754.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Resch T.R., Main S., Price L.A., Milner S.M. A fungal burn infection. Eplasty. 2014;14:ic4. [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson E.M., Borman A.M. Identification of Aspergillus at the species level the importance of conventional Methods : microscopy and culture. In: Pasqualotto A.C., editor. Aspergillosis: from Diagnosis to Prevention. Springer Science+Business; 2009. [Google Scholar]
- 7.Atiyeh B., Masellis A., Conte C. Optimizing burn treatment in developing low- and middle-income countries with limited health care resources (Part 1) Ann Burn Fire Disasters. 2009;22(3):121–125. [PMC free article] [PubMed] [Google Scholar]
- 8.Lou G., Tan J., Peng Y., Wu J., Huang Y., Peng D. Guideline for diagnosis, prophylaxis and treatment of invasive fungal infection post burn injury in China 2013. Burn Trauma. 2014;2(2):45–52. doi: 10.4103/2321-3868.130182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patterson TF R.T., Iii, Denning D.W., Fishman J.A., Hadley S., Herbrecht R. Practice guidelines for the diagnosis and management of Aspergillosis : 2016 update by the infectious diseases society of America. Clin. Infect. Dis. 2016:1–60. doi: 10.1093/cid/ciw326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ballard J., Edelman L., Saffle J., Sheridan R., Kagan R., Bracco D. Positive fungal cultures in burn patients: a multicenter review. J. Burn Care Res. 2008;29(1):213–221. doi: 10.1097/BCR.0b013e31815f6ecb. [DOI] [PubMed] [Google Scholar]
- 11.Aries P., Hoffmann C., Schaal J.-V., Leclerc T., Donat N., Cirodde A. Aspergillus tamarii: an uncommon burn wound infection. J. Clin. Pathol. 2018;(0):1–2. doi: 10.1136/jclinpath-2017-204858. [DOI] [PubMed] [Google Scholar]
- 12.Prasad P., Fishman J. Impact and cost of the serum galactomannan assay at a tertiary care facility. Transplantation. 2014;98(7):773–780. doi: 10.1097/TP.0000000000000131. [DOI] [PubMed] [Google Scholar]
- 13.Blyth D.M., Chung K.K., Cancio L.C., King B.T., Murray C.K. Clinical utility of fungal screening assays in adults with severe burns. Burns. 2012;39(3):413–419. doi: 10.1016/j.burns.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 14.Mousa H., Al-Bader S., Hassan D. Correlation between fungi isolated from burn wound and burn care units. 1990;25(2):145–147. doi: 10.1016/s0305-4179(98)00148-x. [DOI] [PubMed] [Google Scholar]
- 15.Gupta N., Haque A., Lattif A.A., Narayan R.P., Mukhopadhyay G., Prasad R. Epidemiology and molecular typing of Candida isolates from burn patients. Mycopathologia. 2004;158(4):397–405. doi: 10.1007/s11046-004-1820-x. [DOI] [PubMed] [Google Scholar]
- 16.Guinea J., Viedma DG de, Peláez T., Escribano P., Muñoz P., Klaassen C.H.W. Molecular epidemiology of Aspergillus fumigatus : an in- depth genotypic analysis of isolates involved in an outbreak of invasive aspergillosis. J. Clin. Microbiol. 2011;49(10):3498–3503. doi: 10.1128/JCM.01159-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stone H., Cuzzell J., Kolb L., Moskowitz M., McGowan J.J. Aspergillus infection of the burn wound. J. Trauma. 1979;10(Oct):765–767. doi: 10.1097/00005373-197910000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Warren L., Bhattacharjya S., Abrol N., Russell C., Antony-Olakkengil S. Treatment of invasive Aspergillus-associated wound infection incorporating topical amphotericin B. Wound Pract. Res. 2017;25(2):98–100. [Google Scholar]
- 19.Raja H., Miller A., Pearce C., Oberlies N. Fungal identification using molecular tools: a primer for the natural products research community. J. Nat. Prod. 2017;80(3):756–770. doi: 10.1021/acs.jnatprod.6b01085. [DOI] [PMC free article] [PubMed] [Google Scholar]