Abstract
Digital manufacturing, all-ceramics, and adhesive dentistry are currently the trendiest topics in clinical restorative dentistry. Tooth- and implant-supported fixed restorations from computer-aided design (CAD)/computer-aided manufacturing (CAM)–fabricated high-strength ceramics—namely, alumina and zirconia—are widely accepted as reliable alternatives to traditional metal-ceramic restorations. Most recent developments have focused on high-translucent monolithic full-contour zirconia restorations, which have become extremely popular in a short period of time, due to physical strength, CAD/CAM fabrication, and low cost. However, questions about proper resin bonding protocols have emerged, as they are critical for clinical success of brittle ceramics and treatment options that rely on adhesive bonds, specifically resin-bonded fixed dental prostheses or partial-coverage restorations such as inlays/onlays and veneers. Resin bonding has long been the gold standard for retention and reinforcement of low- to medium-strength silica-based ceramics but requires multiple pretreatment steps of the bonding surfaces, increasing complexity, and technique sensitivity compared to conventional cementation. Here, we critically review and discuss the evidence on resin bonding related to long-term clinical outcomes of tooth- and implant-supported high-strength ceramic restorations. Based on a targeted literature search, clinical long-term studies indicate that porcelain-veneered alumina or zirconia full-coverage crowns and fixed dental prostheses have high long-term survival rates when inserted with conventional cements. However, most of the selected studies recommend resin bonding and suggest even greater success with composite resins or self-adhesive resin cements, especially for implant-supported restorations. High-strength ceramic resin-bonded fixed dental prostheses have high long-term clinical success rates, especially when designed as a cantilever with only 1 retainer. Proper pretreatment of the bonding surfaces and application of primers or composite resins that contain special adhesive monomers are necessary. To date, there are no clinical long-term data on resin bonding of partial-coverage high-strength ceramic or monolithic zirconia restorations.
Keywords: adhesives, CAD, cement, clinical outcomes, esthetic dentistry, prosthetic dentistry/prosthodontics
Introduction
High-strength ceramic materials, such as alumina and zirconia, are typically fabricated with computer-aided design (CAD)/computer-aided manufacturing (CAM) technologies and were developed to eliminate metal-alloy frameworks for restorations that are exclusively made from ceramics for optical, physical, and biologic reasons. Especially for full-coverage crowns, clinical success rates are comparable to traditional metal-ceramic restorations (Takeichi et al. 2013; Ozer et al. 2014). Consequently, the popularity and range of clinical applications of high-strength ceramics have increased considerably at an unexpected pace. Initially designed for copings and frameworks for porcelain-veneered bilayer all-ceramic restorations (Ozer et al. 2014), current high-translucent zirconia ceramics are extensively used in private practice for monolithic full-contour restorations (Blatz et al. 2016; Zhang et al. 2016). Digital workflows, CAD/CAM fabrication, and elimination of work-intensive porcelain layering procedures have made monolithic ceramic restorations more predictable and cost-effective. However, the scientific world has been largely unable to keep pace with the rapid and widespread implementation of these materials in clinical practice: sound clinical studies are scarce, not just on the materials themselves but even more so on their clinical handling and suggested cementation protocols. Resin bonding is a necessity for low- and medium-strength silica-based ceramics that are not supported by a core or framework to provide reinforcement and adhesion. Discussions on cementation versus resin bonding for high-strength ceramics have been going on for almost 2 decades, but clinical recommendations mainly rely on in vitro studies. Bonding protocols for high-strength oxide ceramics differ fundamentally from the ones established for silica-based ceramics and are based on early bond-strength studies to alumina.
Over the past decade, alumina was progressively replaced by zirconia in clinical practice. Nevertheless, clinical data on alumina ceramics and how bonding affects their clinical performance are critical in the development and understanding of more current high-strength ceramics.
Therefore, this article reviews and critically discusses the clinical evidence on resin bonding as it relates to long-term success of high-strength ceramic restorations.
High-Strength Dental Ceramics
When categorized by microstructure, “high-strength dental ceramics” include the following non-glass-based ceramic systems: crystalline-based systems with glass fillers (e.g., glass-infiltrated alumina) and polycrystalline solids (e.g., alumina and zirconia). Glass-infiltrated alumina (In-Ceram Alumina; Vita Zahnfabrik) became popular in the mid-1990s and incorporates a dry-sintered alumina core, which is infused with molten glass (Paul et al. 1995). With a flexural strength of 450 MPa, it is indicated for full-coverage crowns and short-span fixed dental prostheses (FDPs). Feldspathic porcelain can be applied as a veneer to improve esthetics (Giordano et al. 1995). The slightly weaker glass-infiltrated spinel ceramic (In-Ceram Spinell; Vita Zahnfabrik) offered better optical properties (Paul et al. 1995) with high clinical success (Fradeani et al. 2002).
Densely sintered high-purity aluminum-oxide (>99.9%) ceramic (Procera Alumina; Nobel Biocare) was developed around the same time but is fabricated by a CAD/CAM-process. With a flexural strength of 610 MP, it does not contain any silica (Odén et al. 1998). Densely sintered alumina single-crown cores and multiunit frameworks must be veneered with feldspathic ceramics.
In the meantime, alumina has been largely replaced by zirconium-dioxide ceramics (zirconia, yttria-stabilized tetragonal zirconia polycrystal, Y-TZP) in clinics (Sadan et al. 2005a, 2005b). Conventional zirconia is indicated as a core and framework material for full-coverage crowns (Blatz 2002), resin-bonded FDPs (RBFDP) and conventional FDPs (McLaren 1998), implant abutments (Yildirim et al. 2000), endodontic posts (Koutayas and Kern 1999), tooth- and implant-supported frameworks, overdenture bars, FDPs, and full-mouth reconstructions (Kern 2005). Zirconia has a monoclinic crystal structure at room temperature and a tetragonal and cubic structure at increasing temperatures. Formulations used in dentistry contain mainly tetragonal crystals that are partially stabilized with yttrium oxide (Y2O3) and have a flexural strength of 900 to 1,400 MPa, a modulus of elasticity of 210 GPa, and a fracture toughness of 10 MPa/m0.5. Properties termed active crack resistance or transformation toughening (Guazzato et al. 2004) are unique to this material: external stresses and cracks cause transformation of the tetragonal particle into a monoclinic one with greater volume (approximately 3% to 5%), subjecting a crack under compressive stresses and impeding its growth. However, the actual effects of this phase transformation on ultimate strength and its role in an accelerated aging process (low-temperature surface degradation) are discussed controversially.
Restorations are typically milled from green-stage or presintered (white-stage) zirconia blocks before full sintering. Only very few CAD/CAM systems mill from fully sintered blocks, which have a significantly higher hardness and flexural strength, making the milling process time-consuming and taxing on the milling equipment. First-generation conventional zirconia copings and frameworks are veneered with feldspathic ceramic (porcelain-fused-to-zirconia, PFZ) for esthetic reasons since they are rather opaque and monochromatic white. Early studies indicate a high incidence of veneer fractures and chippings (Sailer et al. 2006; Sailer et al. 2007). The development of veneering ceramics that better matched the thermal (coefficient of thermal expansion [CTE]) and physical properties of zirconia as well as firing and cooling protocols to control internal thermal stresses significantly increased reliability of PFZ restorations (Ozer et al. 2014). More recent investigations show long-term success rates of PFZ crowns that are not different from metal-ceramics (Takeichi et al. 2013; Ozer et al. 2014). Nevertheless, concerns about possible veneering ceramic fractures made monolithic full-contour restorations the predominant all-ceramic choice. A fully digital CAD/CAM process has made full-contour zirconia (FCZ) restoration fabrication highly predictable and cost-effective. Second-generation zirconia materials have a higher translucency and slightly lower flexural strength than conventional zirconia. A customized, tooth-like appearance is created through infiltration of liquid dyes in a green or presintered stage and firing of stains and glazes after sintering. Some manufacturers offer preshaded and even multilayer zirconia blanks that mimic natural tooth appearance and can be further customized.
The latest generation of zirconia features significantly greater light transmission with optical properties suitable even for anterior teeth. The higher translucency is achieved by slight changes of the Y2O3 content (5 mol-% or more instead of 3 mol-%), resulting in a higher amount of cubic-phase particles (Zhang 2014; Zhang et al. 2016). However, the flexural strength (between 550 and 800 MPa) is significantly lower than that of conventional zirconia but still considerably higher than any silica-based ceramic. Some clinicians have begun using FCZ for resin-bonded partial-coverage inlays/onlays and laminate veneers (Ma et al. 2013).
Ceramic Resin Bonding
Characteristic physical properties and inherent brittleness of ceramic restorations make handling and cementation critical for their clinical success (Burke et al. 2002). Low- to medium-strength silica-based ceramics rely on resin bonding for reinforcement and support, especially for minimally invasive restorations and preparation designs that provide little retention (Blatz 2002). Acid etching with hydrofluoric acid and silane coupling agent application provide very high bond strengths to silica-based ceramic. Conventional shear and tensile bond strength tests typically cause cohesive fractures in the ceramic, meaning that bond strengths may even exceed the tensile strength of the ceramic (Blatz et al. 2004).
Adhesive bonding with composite resins requires multiple steps to prepare the bonding surfaces of the tooth and the restoration. As these are time-consuming, technique sensitive, and susceptible to contamination, clinicians widely prefer conventional cementation with zinc-phosphate, glass ionomer, or resin-modified glass ionomer cements. These do not require specific pretreatment steps or application of bonding agents but provide little or no adhesion at all. Current self-adhesive resin cements offer a compromise: moderate bond strength values to teeth and indirect dental materials without additional primers or bonding agents (Blatz et al. 2010). They are, however, not sufficient for restorations or materials that rely on resin bonding (Blatz et al. 2010).
Acid etchants for silica-based ceramics do not roughen metal-oxide ceramic surfaces (Awliya et al. 1998). Air-particle abrasion with Al2O3 is both effective and practical to provide long-term durable bond strengths to high-strength ceramics (Kern and Thompson 1994). Silica/silane coating (e.g., Rocatec or CoJet; 3M ESPE) has also been recommended (Özcan et al. 2001; Blatz et al. 2007) and includes air-particle abrasion steps that form a silica layer and application of a silane-coupling agent (Frankenberger et al. 2000).
Conventional silane coupling agents cannot form chemical bonds to metal-oxide ceramics (Dérand and Dérand 2000). A composite resin cement (e.g., Panavia 21; Kuraray Noritake) or ceramic primer (e.g., Clearfil Ceramic Primer; Kuraray Noritake) that contains special adhesive monomers is recommended (Wegner and Kern 2000; Blatz, Sadan, Arch, et al. 2003; Blatz et al. 2016). One such monomer that chemically bonds to metal oxides is 10-methacryloyloxydecyl dihydrogenphosphate (MDP). Auto-polymerizing or dual-polymerizing composites are recommended due to the opacity of the ceramic (Sadan et al. 2005b).
In vitro studies and systematic reviews are in strong agreement that a combined micromechanical and chemical pretreatment is necessary for long-term durable resin bonds (Blatz et al. 2007; Koizumi et al. 2012; Inokoshi et al. 2014; Özcan and Bernasconi 2015). Figures 1 to 3 illustrate the effects of adequate surface pretreatment for optimal adhesion to high-strength ceramics. Dual-beam focused ion beam (DB FIB) technology followed by scanning electron microscopy (SEM) was used to visualize the undisturbed bonding interface of a composite resin luting agent to zirconia (Fig. 1), without preparation artifacts often seen after mechanical sample preparation. Without any surface pretreatment, the resin-ceramic interface reveals wide-open gaps (Fig. 2). Air-particle abrasion with alumina (50 µm to 60 µm at 2 bar for 5 s) and application of an MDP-containing primer provide an optimized adhesive interface (Fig. 3).
Figure 1.

Dual-beam focused ion beam technology followed by scanning electron microscopy facilitates visual assessment of the bonding interface between a composite resin luting agent (left) and zirconia ceramic (right) without preparation artifacts.
Figure 3.
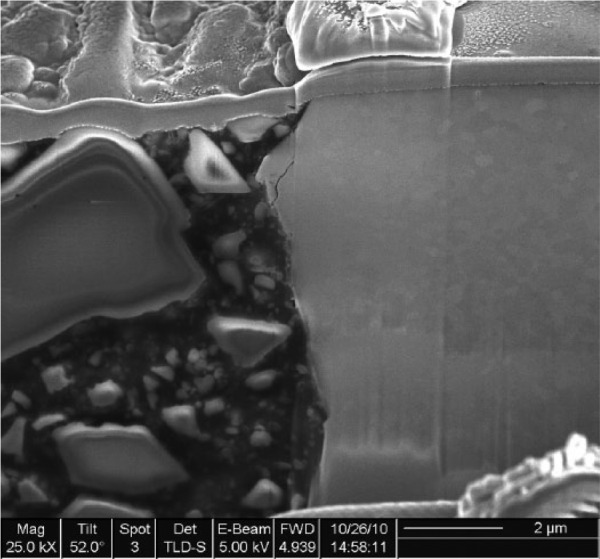
Air-particle abrasion of the zirconia surface with alumina particles (50 µm at 2 bar for 5 s) and application of a ceramic primer that contains phosphate monomers that chemically bond to oxide ceramics provide an optimized adhesive interface (×25,000 magnification).
Figure 2.

Without any surface pretreatment, the resin-zirconia bonding interface reveals wide-open gaps and only limited adhesion (×35,000 magnification).
High-strength ceramic full-coverage restorations with adequate thickness and retention offer mechanical strength that exceeds natural chewing forces and can, therefore, be cemented conventionally (Tinschert et al. 2001; Blatz et al. 2008). Resin bonding is recommended in cases of compromised retention, adhesive treatment options (e.g., laminate veneers and RBFDPs), high dislodging forces, minimal ceramic thickness, and low inherent strength (Burke et al. 2002; Blatz, Sadan, and Kern 2003; Kern 2005).
Resin-bonding protocols for silica-based ceramics are universally known and accepted. However, despite its high popularity, most practitioners are still unsure about proper bonding techniques and materials for zirconia. Therefore, a simplified zirconia-bonding concept that summarizes the 3 critical steps of air-particle abrasion, primer application, and composite resin luting agents (the “APC Concept”) was recently introduced in the clinical literature (Blatz et al. 2016).
Long-Term Clinical Studies
To ensure a comprehensive overview and limit bias in the selection and assessment of the literature, an electronic database search of PubMed and Cochrane Library was conducted for English-language clinical studies published between 1990 and 2016 and pertaining to bonding to high-strength ceramics. The MeSH terms zirconium, aluminum oxide, and dental bonding and the free text words zirconium, zirconia, zirconium oxide, zirconium dioxide, Y-TZP, aluminum oxide or alumina, dental bonding, adhesion, resin bonding or cement, and clinical were used. Clinical studies that met the following criteria were included: 1) studies related to resin-bonded alumina and zirconia restorations; 2) prospective, retrospective, or randomized controlled trials conducted in humans; 3) studies with a dropout rate of less than 30%; and 4) long-term studies with a follow-up of at least 5 y. The electronic search was complemented by a manual search. All titles obtained were screened for additional relevant studies.
The initial search revealed 974 titles. Of the 49 articles selected by title and abstract, 8 duplicates were identified. Full-text screening was carried out for 41 studies, yielding 16 articles that complied with the inclusion criteria (Tables 1 and 2).
Table 1.
Long-Term Clinical Studies on Resin-Bonded Alumina Restorations.
| Author (Year) | Study Design | Restoration Type | Restoration Material | No. of Restorations and Cement Type | Mean Follow-up, mo | Cumulative Survival Rate, % |
|---|---|---|---|---|---|---|
| Galiatsatos and Bergou (2014) | Prospective | Two-retainer RBFDP | Glass-infiltrated alumina | 54 composite resin | 96 | 85.2 |
| Kern (2005) | Prospective | Two-retainer RBFDP | Glass-infiltrated alumina | 16 composite resin | 75.8 | 73.9 |
| Single-retainer RBFDP | Glass-infiltrated alumina | 21 composite resin | 51.7 | 92.3 | ||
| Kern and Sasse (2011) | Prospective | Two-retainer RBFDP | Glass-infiltrated alumina | 16 composite resin | 120.2 | 73.9 |
| Single-retainer RBFDP | Glass-infiltrated alumina | 22 composite resin | 111.1 | 94.4 | ||
| Selz et al. (2014) | Prospective randomized split-mouth | Tooth-supported crown | Glass-infiltrated alumina | 59 composite resin A62 composite resin B | 6060 | 88.782.8 |
| 28 glass ionomer | 60 | 80.1 | ||||
| Sorrentino, Galasso, et al. (2012) | Retrospective | Tooth- and implant-supported crown | Densely sintered alumina | 109 composite resin | 72 | 98.6 |
| 100 zinc phosphate | 72 | 96.7 |
RBFDP, resin-bonded fixed dental prosthesis.
Table 2.
Long-Term Clinical Studies on Resin-Bonded Zirconia Restorations.
| Author (Year) | Study Design | Restoration Type | Restoration Material | Restoration Numbers and Cement Type | Mean Follow-up, mo | Cumulative Survival Rate, % |
|---|---|---|---|---|---|---|
| Burke et al. (2013) | Observational | FDP | Zirconia | 33 self-adhesive resin | 60 | 97 |
| Dogan et al. (2017) | Prospective | Crown | Zirconia | 20 self-adhesive resin | 58.7 | 100 |
| Chaar and Kern (2015) | Prospective | IRFDP | Zirconia | 30 composite resin | 64.4 | 95.8 |
| Larsson and Von Steyern (2013) | Pilot | Complete-arch FDP | Zirconia | 9 composite resin | 96 | 100 |
| Molin and Karlsson (2008) | Prospective | FDP | Zirconia | 19 composite resin | 60 | 100 |
| Ortorp et al. (2012) | Retrospective | Tooth-supported crown | Zirconia | 143 zinc phosphate cement self-adhesive resin |
60 | 88.8 12.5% debonded 6.6% debonded |
| Sailer et al. (2007) | Prospective | FDP | Zirconia | 33 composite resins | 53.4 | 73.9 |
| Sasse and Kern (2013) | Prospective | Single-retainer RBFDP | Zirconia | 30 composite resin | 64.2 | 100 |
| Sasse and Kern (2014) | Prospective | Single-retainer RBFDP | Zirconia | 42 composite resin | 61.8 | 100 |
| Sax et al. (2011) | Prospective | FDP | Zirconia | 57 composite resin | 128.4 | 67 (FDP) 91.5 (framework) |
| Sorrentino, De Simone, et al. (2012) | Prospective | FDP | Zirconia | 48 self-adhesive resin | 60 | 100 |
FDP, fixed dental prosthesis; IRFDP, inlay-retained fixed dental prosthesis; RBFDP, resin-bonded fixed dental prosthesis.
Alumina Restorations
The selected long-term studies on the effect of resin bonding on clinical performance of alumina restorations evaluated glass-infiltrated alumina tooth-supported crowns and RBFDPs as well as tooth-and implant-supported densely sintered alumina crowns (Table 1). Studies on multiunit FDPs and partial-coverage restorations could not be identified.
In a prospective, randomized clinical split-mouth study, 5-y success rates of posterior glass-infiltrated alumina crowns inserted with 1 of 2 composite resin or glass-ionomer cements ranged between 81% and 88% and were not significantly different among cements (Selz et al. 2014).
Sorrentino and coworkers followed anterior and posterior densely sintered alumina (Procera Alumina) single crowns on natural teeth and implant abutments for 6 y (Sorrentino, Galasso, et al. 2012). Cumulative survival and success rates were 95.2% and 90.9%, respectively. Resin bonding with a composite-resin luting agent revealed slightly better success than cementation with zinc-phosphate cement.
A study of densely sintered alumina crowns (Zitzmann et al. 2007) reported a cumulative survival rate of 100% for anterior and 98.8% for posterior crowns after 55 mo, irrespective of tooth position or cement type (composite resin or glass-ionomer cement).
These studies suggest that all cement types provide high success rates for alumina crowns, with a slight advantage of resin bonding over zinc-phosphate cement.
A clinical pilot study by Kern and Strub (1998) indicated high success rates of glass-infiltrated alumina RBFDPs. Kern (2005) then compared the long-term survival of 2-retainer versus single-retainer all-ceramic RBFDPs. Of 37 anterior In-Ceram alumina RBFDPs, 16 were inserted with a conventional 2-retainer design and 21 with a cantilever single-retainer design. Mean observation times were 75.8 and 51.7 mo, respectively. None of the restorations debonded. In the 2-retainer group, 1 restoration fractured after 3 mo at both connectors and 1 restoration was lost in an accident. Also, four 2-retainer RBFDPs fractured within 15 mo after insertion at 1 connector. However, the pontics remained in situ as a cantilever RBFDP for several years. In the single-retainer group, only 1 FDP fractured and was lost 48 mo after insertion. The 5-y survival rate was 73.9% in the 2-retainer and 92.3% in the single-retainer group. After 10 y, the 2-retainer RBFDPs had a survival rate of 73.9% and single-retainer ones of 94.4% (Kern and Sasse 2011). MDP-containing composite-resin luting agents were used after either silica coating and silanization or air-particle abrasion with alumina only.
These studies indicate that single-retainer cantilever all-ceramic RBFDPs perform significantly better than 2-retainer RBFDPs in the anterior region.
Galiatsatos and Bergou (2014) reported an 85.18% survival rate of 54 anterior alumina RBFDPs with a 2-retainer design after 8 y. These restorations rely on strong adhesive resin bonds since there is no mechanical retention. Given the clinical simplicity and minimally invasive nature of this treatment option, the very high success rates are impressive and make this a viable alternative to implant-supported, full-coverage fixed, or removable prostheses in select cases (Saker et al. 2014). Failures can be easily rebonded, repaired, replaced, or followed by more invasive treatment if needed.
Zirconia Restorations
Studies identified for resin-bonded zirconia-based restorations included tooth-supported conventional and resin-bonded as well as implant-supported FDPs (Table 2).
In a retrospective practice-based study of 143 mostly posterior zirconia crowns followed up for 5 y, 126 did not reveal any complications, indicating a cumulative survival rate of 88.8% (Ortorp et al. 2012). Crown loosening occurred in 12.5% of crowns cemented with zinc-phosphate and in only 6.6% of crowns inserted with self-adhesive resin cement.
Twenty anterior maxillary crowns with customized copings luted with self-adhesive resin cement revealed no coping fractures or loss of retention after 5 y (100% survival), excluding minor veneer chippings (Dogan et al. 2017).
A short-term study of PFZ crowns in predoctoral dental education clinics and inserted with self-adhesive resin cement showed a survival rate of 89% after 46.6 mo (Näpänkangas et al. 2015).
According to these studies, self-adhesive resin cements are adequate for PFZ crowns. Zinc-phosphate cement seems less suitable.
No clinical studies were found on monolithic FCZ crowns. Since conventional zirconia core and full-contour materials are similar, the differences should be minor. However, the effects of resin bonding on clinical outcomes may be quite different with high-translucent FCZ materials, which have a significantly lower flexural strength. Here, minimal material thickness requirements and reinforcement through resin bonding may be critical to prevent fractures and ensure long-term clinical success, but clinical studies are missing.
The first long-term study on tooth-supported posterior PFZ FDPs revealed a success rate of zirconia frameworks of 97.8% after 5 y (Sailer et al. 2007). However, overall survival rate of zirconia FDPs, fabricated with a prototype CAD/CAM system, was only 73.9%. Most prevalent complications were marginal caries and veneer porcelain chipping. Fourteen FDPs were resin bonded with Variolink (Ivoclar Vivadent) and 20 with Panavia TC. Overall survival and the occurrence of marginal discrepancies were not different between the 2 resin cements.
Ten-year clinical outcomes of the same patient population revealed an overall FDP survival rate of only 67%, due to technical and biological complications (Sax et al. 2011). Survival rate for zirconia frameworks was 91.5%. The authors attributed the most common adverse effects, chipping and marginal deficiencies, to the prototype status of the CAD/CAM system.
Zirconia-based 3-unit premolar and molar FDPs with anatomically designed frameworks were more promising, with a 100% survival rate after 5 y (Molin and Karlsson 2008). One complication was registered at the 1-y follow-up due to loss of retention and despite being bonded with composite resin. The FDP was recemented with the same material, and no further complications were registered. None of the restorations revealed chipping of the veneering ceramic at 5-y follow-up.
Similarly, Sorrentino and coworkers reported 100% cumulative survival of 3-unit PFZ FDPs after 5 y (Sorrentino, De Simone, et al. 2012). Cumulative success rates for patients having 1 and 2 FDPs were 91.9% and 95.4%, respectively. All restorations were luted with a universal self-adhesive resin cement without any retention loss. Minor porcelain chipping was detected in 3 restorations.
A 5-y clinical evaluation of zirconia-based FDPs (Lava; 3M ESPE) in patients in UK general dental practices revealed 97% success (Burke et al. 2013). All zirconia frameworks were intact and without debondings after insertion with self-adhesive resin cement.
In early studies, PFZ FDPs showed a relatively high incidence of chippings in the veneering ceramic. More supportive framework designs, proper selection of veneering ceramics, and slow cooling after porcelain layering significantly diminished the prevalence of such failures (Ozer et al. 2014).
For these types of full-coverage restorations with a preparation design that features at least some mechanical retention, self-adhesive resin cements provide high clinical success rates.
Several studies have reviewed clinical success of zirconia RBFDPs (Kern 2015) and the influence of different framework designs (Wei et al. 2016).
Sasse and Kern published 2 studies on single-retainer zirconia-based RBFDPs (Sasse and Kern 2013; Sasse and Kern 2014). In the first study, anterior zirconia RBFDPs were adhesively bonded with either MDP-containing composite resin cement (Panavia 21; n = 16) or an adhesive bonding system with a phosphoric acid acrylate primer (Multilink-Automix with Metal-Zirconia Primer; Ivoclar Vivadent; n = 14). After 64.2 mo, 1 debonding occurred in each cement group. Both RBFDPs were rebonded successfully, providing 100% survival rates at 5 y.
In the other study, 42 zirconia RBFDPs with a cantilever single-retainer design were inserted with Panavia 21 TC after alumina air-particle abrasion (Sasse and Kern 2014). Two RBFDPs debonded during the 61.8-mo observation but were successfully rebonded. Six-year success rate was 91.1%.
Anterior single-retainer zirconia RBFDPs have excellent clinical survival rates when adhesively bonded with the proper protocols and materials (Koizumi et al. 2012; Inokoshi et al. 2014; Özcan and Bernasconi 2015).
To replace posterior teeth with minimal abutment tooth preparations, Chaar and Kern (2015) followed 30 three-unit zirconia inlay-retained FDPs (IRFDPs) over 64.4 mo. The restorations, bonded with an adhesive composite resin after air-particle abrasion, had a survival rate of 95.8%. The authors concluded that, depending on proper case selection, IRFDPs may be a reliable treatment option to replace posterior single teeth (Chaar and Kern 2015).
A short-term study on posterior zirconia all-ceramic IRFDPs showed far less promising results, with a high incidence of technical complications, independent of type of resin cement (Ohlmann et al. 2008).
Kolgeci and coworkers followed implant-supported zirconia-based prostheses for up to 7 y (Kolgeci et al. 2014). Twenty-five of 193 crowns and short-span FDPs were resin bonded onto the zirconia abutments with composite resin (Panavia F). The overall cumulative survival rate was 96.4%. Three prostheses needed to be recemented.
Full-arch implant-supported zirconia-based frameworks and reconstructions have become very popular. Clinical studies, however, are scarce. A clinical pilot study assessed 8-y performance of 10 full-arch zirconia-based mandibular FDPs, each supported by 4 implants (Larsson and Von Steyern 2013). The FDPs were resin bonded to individually prepared titanium abutments with resin composite (Panavia F 2.0). Success rate was 100%, and none of the restorations debonded.
In a short-term study, Pozzi and coworkers reported 100% survival of full-arch implant FDPs with lithium disilicate crowns bonded to CAD/CAM zirconia frameworks after 49.3 mo (Pozzi et al. 2015).
Consequently, resin bonding does not only play a role in tooth-supported and short-span restorations but, in fact, may be critical for the long-term success of implant-supported high-strength ceramic reconstructions. The same ceramic bonding protocols applied in clinics are carried out in the dental laboratory, where, especially for implant reconstructions, the combination of different ceramics and materials offers a plethora of new prosthetic options.
Limited esthetic properties restricted most alumina and zirconia ceramics to cores and frameworks. Except for early glass-infiltrated alumina formulations, it took until high-translucent FCZ became available that high-strength ceramics could also be used for partial-coverage laminate veneers and inlays/onlays. No clinical studies could be found on partial-coverage high-strength ceramic restorations.
Summary and Outlook
High-strength ceramic restorations are used in clinics in a variety of indications. Despite high success rates, alumina-based restorations were, over the years, largely replaced by zirconia. While in vitro studies indicate a significant increase in flexural strength of high-strength ceramic restorations after resin bonding (Blatz et al. 2008), the evidence on the exact influence of the cementation medium on clinical performance is limited. For full-coverage high-strength ceramic crowns and FDPs and based on the specific clinical situation, the clinician can choose between resin bonding with composite resins, insertion with a self-adhesive resins, or conventional cementation with zinc-phosphate, glass ionomer, or resin-modified glass ionomer cement. Zinc-phosphate cement was, in the few studies that evaluated it, not as successful, while self-adhesive resin appeared to be the most common. For restoration types that rely on adhesion, however, composite resins and adequate resin-bonding pretreatment steps are critical and not optional. With the increasing popularity of high-strength ceramics, there is a strong need to further evaluate the correlation between cement and clinical success. We could not find any long-term clinical studies on monolithic FCZ crowns or partial-coverage restorations. The differences between first- and second-generation zirconia materials are minor, and clinical recommendations as well as suggested bonding protocols should not differ substantially. However, the latest generation of high-translucent, more cubic zirconia has significantly different properties and lower flexural strength. There seems to be a lack of understanding of how these properties affect clinical outcomes. Following manufacturers’ minimal thickness recommendations and proper cementation or resin bonding protocols are critical in strengthening high-translucent FCZ and to prevent failures. This is especially important for minimal-invasive partial-coverage restorations, which are becoming increasingly popular in practice, even with zirconia and despite the complete lack of in vivo scientific support.
Conclusions
Clinical long-term studies indicate that porcelain-veneered alumina or zirconia full-coverage crowns and fixed dental prostheses have high survival rates when inserted with conventional cements. However, most of the selected studies recommend resin bonding and suggest even greater success with composite resins or self-adhesive resin cements, especially for implant-supported restorations. High-strength ceramic RBFDPs have high long-term clinical success rates, especially when designed as a cantilever with only 1 retainer. Proper pretreatment of the bonding surfaces and application of primers or composite resins that contain special adhesive monomers are necessary. To date, there are no clinical long-term data on resin bonding of partial-coverage high-strength ceramic or monolithic zirconia restorations.
Author Contributions
M.B. Blatz, contributed to conception, design, data analysis, and interpretation, drafted and critically revised the manuscript; M. Vonderheide, contributed to data acquisition and analysis, drafted the manuscript; J. Conejo, contributed to data acquisition, analysis, and interpretation, drafted the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Acknowledgments
The authors express their appreciation for the contributions of Drs. Lolita Rotkina, Tomohiro Tagagaki, and Christoph Zbaeren to the FIB technology and SEM illustrations and Pat Heller for assistance with the literature search.
Footnotes
The authors received no financial support and declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Awliya W, Oden A, Yaman P, Dennison JB, Razzoog ME. 1998. Shear bond strength of a resin cement to densely sintered high-purity alumina with various surface conditions. Acta Odontol Scand. 56(1):9–13. [DOI] [PubMed] [Google Scholar]
- Blatz MB. 2002. Long-term clinical success of all-ceramic posterior restorations. Quintessence Int. 33(6):415–426. [PubMed] [Google Scholar]
- Blatz MB, Alvarez M, Sawyer K, Brindis M. 2016. How to bond to zirconia: the APC concept. Compend Contin Educ Dent. 37(9):611–618. [PubMed] [Google Scholar]
- Blatz MB, Sadan A, Arch GH, Jr, Lang BR. 2003. In vitro evaluation of long-term bonding of procera AllCeram alumina restorations with a modified resin luting agent. J Prosthet Dent. 89(4):381–387. [DOI] [PubMed] [Google Scholar]
- Blatz MB, Sadan A, Kern M. 2003. Resin-ceramic bonding: a review of the literature. J Prosthet Dent. 89(3):268–274. [DOI] [PubMed] [Google Scholar]
- Blatz MB, Sadan A, Maltezos C, Blatz U, Mercante D, Burgess JO. 2004. In vitro durability of the resin bond to feldspathic ceramics. Am J Dent. 17(3):169–172. [PubMed] [Google Scholar]
- Blatz MB, Chiche G, Holst S, Sadan A. 2007. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int. 38(9):745–753. [PubMed] [Google Scholar]
- Blatz MB, Oppes S, Chiche GJ, Holst S, Sadan A. 2008. Influence of cementation technique on fracture strength and leakage of alumina all-ceramic crowns after cyclic loading. Quinessence Int. 39(1):23–32. [PubMed] [Google Scholar]
- Blatz MB, Phark JH, Ozer F, Mante FK, Saleh N, Bergler M, Sadan A. 2010. In vitro comparative bond strength of contemporary self-adhesive resin cements to zirconium oxide ceramic with and without air-particle abrasion. Clin Oral Investig. 14(2):187–192. [DOI] [PubMed] [Google Scholar]
- Burke FJ, Crisp RJ, Cowan AJ, Lamb J, Thompson O, Tulloch N. 2013. Five-year clinical evaluation of zirconia-based bridges in patients in UK general dental practices. J Dent. 41(11):992–999. [DOI] [PubMed] [Google Scholar]
- Burke FJ, Fleming GJ, Nathanson D, Marquis PM. 2002. Are adhesive technologies needed to support ceramics? An assessment of the current evidence. J Adhes Dent. 4(1):7–22. [PubMed] [Google Scholar]
- Chaar MS, Kern M. 2015. Five-year clinical outcome of posterior zirconia ceramic inlay-retained FDPs with a modified design. J Dent. 43(12):1411–1415. [DOI] [PubMed] [Google Scholar]
- Dérand P, Dérand T. 2000. Bond strength of luting cements to zirconium oxide ceramics. Int J Prosthodont. 13(2):131–135. [PubMed] [Google Scholar]
- Dogan S, Raigrodski AJ, Zhang H, Mancl LA. 2017. Prospective cohort clinical study assessing the 5-year survival and success of anterior maxillary zirconia-based crowns with customized zirconia copings. J Prosthet Dent. 117(2):226–232. [DOI] [PubMed] [Google Scholar]
- Fradeani M, Aquilano A, Corrado M. 2002. Clinical experience with In-Ceram Spinell crowns: 5-year follow-up. Int J Periodontics Restorative Dent. 22(6):525–533. [PubMed] [Google Scholar]
- Frankenberger R, Kramer N, Sindel J. 2000. Repair strength of etched vs silica-coated metal-ceramic and all-ceramic restorations. Oper Dent. 25(3):209–215. [PubMed] [Google Scholar]
- Galiatsatos AA, Bergou D. 2014. Clinical evaluation of anterior all-ceramic resin-bonded fixed dental prostheses. Quintessence Int. 45(1):9–14. [DOI] [PubMed] [Google Scholar]
- Giordano RA, Pelletier L, Campbell S, Pober R. 1995. Flexural strength of an infused ceramic, glass ceramic, and feldspathic porcelain. J Prosthet Dent. 73(5):411–418. [DOI] [PubMed] [Google Scholar]
- Guazzato M, Albakry M, Ringer SP, Swain MV. 2004. Strength, fracture toughness and microstructure of a selection of all-ceramic materials: Part II. zirconia-based dental ceramics. Dent Mater. 20(5):449–456. [DOI] [PubMed] [Google Scholar]
- Inokoshi M, De Munck J, Minakuchi S, Van Meerbeek B. 2014. Meta-analysis of bonding effectiveness to zirconia ceramics. J Dent Res. 93(4):329–334. [DOI] [PubMed] [Google Scholar]
- Kern M. 2005. Clinical long-term survival of two-retainer and single-retainer all-ceramic resin-bonded fixed partial dentures. Quintessence Int. 36(2):141–147. [PubMed] [Google Scholar]
- Kern M. 2015. Bonding to oxide ceramics-laboratory testing versus clinical outcome. Dent Mater. 31(1):8–14. [DOI] [PubMed] [Google Scholar]
- Kern M, Sasse M. 2011. Ten-year survival of anterior all-ceramic resin-bonded fixed dental prostheses. J Adhes Dent. 13(5):407–410. [DOI] [PubMed] [Google Scholar]
- Kern M, Strub JR. 1998. Bonding to alumina ceramic in restorative dentistry: clinical results over up to 5 years. J Dent. 26(3):245–249. [DOI] [PubMed] [Google Scholar]
- Kern M, Thompson VP. 1994. Sandblasting and silica coating of a glass-infiltrated alumina ceramic: volume loss, morphology, and changes in the surface composition. J Prosthet Dent. 71(5):453–461. [DOI] [PubMed] [Google Scholar]
- Koizumi H, Nakayama D, Komine F, Blatz MB, Matsumura H. 2012. Bonding of resin-based luting cements to zirconia with and without the use of ceramic priming agents. J Adhes Dent. 14(4):385–392. [DOI] [PubMed] [Google Scholar]
- Kolgeci L, Mericske E, Worni A, Walker P, Katsoulis J, Mericske-Stern R. 2014. Technical complications and failures of zirconia-based prostheses supported by implants followed up to 7 years: a case series. Int J Prosthodont. 27(6):544–552. [DOI] [PubMed] [Google Scholar]
- Koutayas SO, Kern M. 1999. All-ceramic posts and cores: the state of the art. Quintessence Int. 30(6):383–392. [PubMed] [Google Scholar]
- Larsson C, Vult Von Steyern P. 2013. Implant-supported full-arch zirconia-based mandibular fixed dental prostheses: eight-year results from a clinical pilot study. Acta Odontol Scand. 71(5):1118–1122. [DOI] [PubMed] [Google Scholar]
- Ma L, Guess PC, Zhang Y. 2013. Load-bearing properties of minimal-invasive monolithic lithium disilicate and zirconia occlusal onlays: finite element and theoretical analyses. Dent Mater. 29(7):742–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaren EA. 1998. All-ceramic alternatives to conventional metal-ceramic restorations. Compend Contin Educ Dent. 19(3):307–308, 310, 312 passim; quiz 326. [PubMed] [Google Scholar]
- Molin MK, Karlsson SL. 2008. Five-year clinical prospective evaluation of zirconia-based denzir 3-unit FPDs. Int J Prosthodont. 21(3):223–227. [PubMed] [Google Scholar]
- Näpänkangas R, Pihlaja J, Raustia A. 2015. Outcome of zirconia single crowns made by predoctoral dental students: a clinical retrospective study after 2 to 6 years of clinical service. J Prosthet Dent. 113(4):289–294. [DOI] [PubMed] [Google Scholar]
- Odén A, Andersson M, Krystek-Ondracek I, Magnusson D. 1998. Five-year clinical evaluation of Procera AllCeram crowns. J Prosthet Dent. 80(4):450–456. [DOI] [PubMed] [Google Scholar]
- Ohlmann B, Rammelsberg P, Schmitter M, Schwarz S, Gabbert O. 2008. All-ceramic inlay-retained fixed partial dentures: preliminary results from a clinical study. J Dent. 36(9):692–696. [DOI] [PubMed] [Google Scholar]
- Ortorp A, Kihl ML, Carlsson GE. 2012. A 5-year retrospective study of survival of zirconia single crowns fitted in a private clinical setting. J Dent. 40(6):527–530. [DOI] [PubMed] [Google Scholar]
- Özcan M, Alkumru HN, Gemalmaz D. 2001. The effect of surface treatment on the shear bond strength of luting cement to a glass-infiltrated alumina ceramic. Int J Prosthodont. 14(4):335–339. [PubMed] [Google Scholar]
- Özcan M, Bernasconi M. 2015. Adhesion to zirconia used for dental restorations: a systematic review and meta-analysis. J Adhes Dent. 17(1):7–26. [DOI] [PubMed] [Google Scholar]
- Ozer F, Mante FK, Chiche G, Saleh N, Takeichi T, Blatz MB. 2014. A retrospective survey on long-term survival of posterior zirconia and porcelain-fused-to-metal crowns in private practice. Quintessence Int. 45(1):31–38. [DOI] [PubMed] [Google Scholar]
- Paul SJ, Pietrobon N, Schärer P. 1995. The new In-Ceram Spinell system—a case report. Int J Periodontics Restorative Dent. 15(6):520–527. [PubMed] [Google Scholar]
- Pozzi A, Tallarico M, Barlattani A. 2015. Monolithic lithium disilicate full-contour crowns bonded on CAD/CAM zirconia complete-arch implant bridges with 3 to 5 years of follow-up. J Oral Implantol. 41(4):450–458. [DOI] [PubMed] [Google Scholar]
- Sadan A, Blatz MB, Lang B. 2005. a. Clinical considerations for densely sintered alumina and zirconia restorations: part 1. Int J Periodontics Restorative Dent. 25(3):213–219. [PubMed] [Google Scholar]
- Sadan A, Blatz MB, Lang B. 2005. b. Clinical considerations for densely sintered alumina and zirconia restorations: part 2. Int J Periodontics Restorative Dent. 25(4):343–349. [PubMed] [Google Scholar]
- Sailer I, Fehér A, Filser F, Gauckler LJ, Lüthy H, Hämmerle CH. 2007. Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont. 20(4):383–388. [PubMed] [Google Scholar]
- Sailer I, Fehér A, Filser F, Lüthy H, Gauckler LJ, Schärer P, Franz Hämmerle CH. 2006. Prospective clinical study of zirconia posterior fixed partial dentures: 3-year follow-up. Quintessence Int. 37(9):685–693. [PubMed] [Google Scholar]
- Saker S, El-Fallal A, Abo-Madina M, Ghazy M, Özcan M. 2014. Clinical survival of anterior metal-ceramic and all-ceramic cantilever resin-bonded fixed dental prostheses over a period of 60 months. Int J Prosthodont. 27(5):422–424. [DOI] [PubMed] [Google Scholar]
- Sasse M, Kern M. 2013. CAD/CAM single retainer zirconia-ceramic resin-bonded fixed dental prostheses: clinical outcome after 5 years. Int J Comput Dent. 16(2):109–118. [PubMed] [Google Scholar]
- Sasse M, Kern M. 2014. Survival of anterior cantilevered all-ceramic resin-bonded fixed dental prostheses made from zirconia ceramic. J Dent. 42(6):660–663. [DOI] [PubMed] [Google Scholar]
- Sax C, Hämmerle CH, Sailer I. 2011. 10-year clinical outcomes of fixed dental prostheses with zirconia frameworks. Int J Comput Dent. 14(3):183–202. [PubMed] [Google Scholar]
- Selz CF, Strub JR, Vach K, Guess PC. 2014. Long-term performance of posterior InCeram alumina crowns cemented with different luting agents: a prospective, randomized clinical split-mouth study over 5 years. Clin Oral Investig. 18(6):1695–1703. [DOI] [PubMed] [Google Scholar]
- Sorrentino R, De Simone G, Tetè S, Russo S, Zarone F. 2012. Five-year prospective clinical study of posterior three-unit zirconia-based fixed dental prostheses. Clin Oral Investig. 16(3):977–985. [DOI] [PubMed] [Google Scholar]
- Sorrentino R, Galasso L, Tetè S, De Simone G, Zarone F. 2012. Clinical evaluation of 209 all-ceramic single crowns cemented on natural and implant-supported abutments with different luting agents: a 6-year retrospective study. Clin Implant Dent Relat Res. 14(2):184–197. [DOI] [PubMed] [Google Scholar]
- Takeichi T, Katsoulis J, Blatz MB. 2013. Clinical outcome of single porcelain-fused-to-zirconium dioxide crowns: a systematic review. J Prosthet Dent. 110(6):455–461. [DOI] [PubMed] [Google Scholar]
- Tinschert J, Natt G, Mautsch W, Augthun M, Spiekermann H. 2001. Fracture resistance of lithium disilicate-, alumina-, and zirconia-based three-unit fixed partial dentures: a laboratory study. Int J Prosthodont. 14(3):231–238. [PubMed] [Google Scholar]
- Wegner SM, Kern M. 2000. Long-term resin bond strength to zirconia ceramic. J Adhes Dent. 2(2):139–147. [PubMed] [Google Scholar]
- Wei YR, Wang XD, Zhang Q, Li XX, Blatz MB, Jian YT, Zhao K. 2016. Clinical performance of anterior resin-bonded fixed dental prostheses with different framework designs: a systematic review and meta-analysis. J Dent. 47:1–7. [DOI] [PubMed] [Google Scholar]
- Yildirim M, Edelhoff D, Hanisch O, Spiekermann H. 2000. Ceramic abutments—a new era in achieving optimal esthetics in implant dentistry. Int J Periodontics Restorative Dent. 20(1):81–91. [PubMed] [Google Scholar]
- Zhang F, Inokoshi M, Batuk M, Hadermann J, Naert I, Van Meerbeek B, Vleugels J. 2016. Strength, toughness and aging stability of highly-translucent Y-TZP ceramics for dental restorations. Dent Mater. 32(12):e327–e337. [DOI] [PubMed] [Google Scholar]
- Zhang Y. 2014. Making yttria-stabilized tetragonal zirconia translucent. Dent Mater. 30(10):1195–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zitzmann NU, Galindo ML, Hagmann E, Marinello CP. 2007. Clinical evaluation of Procera AllCeram crowns in the anterior and posterior regions. Int J Prosthodont. 20(3):239–241. [PubMed] [Google Scholar]


