Abstract
OBJECTIVE
We examined the effects of metformin on diabetes prevention and the subgroups that benefited most over 15 years in the Diabetes Prevention Program (DPP) and its follow-up, the Diabetes Prevention Program Outcomes Study (DPPOS).
RESEARCH DESIGN AND METHODS
During the DPP (1996–2001), adults at high risk of developing diabetes were randomly assigned to masked placebo (n = 1,082) or metformin 850 mg twice daily (n = 1,073). Participants originally assigned to metformin continued to receive metformin, unmasked, in the DPPOS (2002–present). Ascertainment of diabetes development was based on fasting or 2-h glucose levels after an oral glucose tolerance test or on HbA1c. Reduction in diabetes incidence with metformin was compared with placebo in subgroups by hazard ratio (HR) and rate differences (RDs).
RESULTS
During 15 years of postrandomization follow-up, metformin reduced the incidence (by HR) of diabetes compared to placebo by 17% or 36% based on glucose or HbA1c levels, respectively. Metformin’s effect on the development of glucose-defined diabetes was greater for women with a history of prior gestational diabetes mellitus (GDM) (HR 0.59, RD −4.57 cases/100 person-years) compared with parous women without GDM (HR 0.94, RD −0.38 cases/100 person-years [interaction P = 0.03 for HR, P = 0.01 for RD]). Metformin also had greater effects, by HR and RD, at higher baseline fasting glucose levels. With diabetes development based on HbA1c, metformin was more effective in subjects with higher baseline HbA1c by RD, with metformin RD −1.03 cases/100 person-years with baseline HbA1c <6.0% (42 mmol/mol) and −3.88 cases/100 person-years with 6.0–6.4% (P = 0.0001).
CONCLUSIONS
Metformin reduces the development of diabetes over 15 years. The subsets that benefitted the most include subjects with higher baseline fasting glucose or HbA1c and women with a history of GDM.
Introduction
The Diabetes Prevention Program (DPP) (1) and its follow-up, the Diabetes Prevention Program Outcomes Study (DPPOS) (2,3), have demonstrated the beneficial effects of the diabetes medication metformin to reduce the risk of developing diabetes. The DPP was conducted in a cohort at high risk for the development of diabetes on the basis of having impaired glucose tolerance, elevated fasting glucose levels, and being at least overweight. In the original DPP trial, analyzed after an average of 2.8 years of follow-up, metformin was of particular benefit in those persons who at baseline had higher fasting glucose levels (110–125 vs. 95–109 mg/dL) or a BMI ≥35 kg/m2 (vs. 24 to <35 kg/m2) (1). In addition, women with a self-reported history of gestational diabetes mellitus (GDM) had a greater benefit from metformin than parous women without such a history (4).
Whether metformin should be used for diabetes prevention requires a careful balance of benefits and risks. The American Diabetes Association has endorsed its use for this purpose, recommending that “metformin therapy for prevention of type 2 diabetes should be considered in those with prediabetes, especially for those with BMI ≥35 kg/m2, those aged <60 years, women with prior gestational diabetes mellitus, and/or those with rising A1C despite lifestyle intervention” (5).
To inform the discussion regarding metformin for prevention, we have analyzed the 15-year results from DPP/DPPOS to determine the longer-term effects of metformin on diabetes prevention and, in particular, prevention in the subgroups that appeared to benefit most from metformin during the DPP. Since glycated hemoglobin (HbA1c) levels are increasingly used to identify persons at risk for or with diabetes (6), rather than fasting glucose and glucose tolerance testing as was used in DPP/DPPOS, we analyzed the effects of metformin on diabetes development in subgroups, as described above, using HbA1c values, applied post hoc, as well as glucose-based diagnostic levels to diagnose diabetes (7).
Research Design and Methods
The design and methods of the DPP and DPPOS have previously been described in detail (1–3,8).
Participants and Procedures
In brief, between 1996 and 1999, the DPP enrolled 3,234 participants aged ≥25 years who were at high risk of developing diabetes based on having impaired glucose tolerance, elevated fasting blood glucose 95 to 125 mg/dL (≤125 mg/dL in the American Indian centers), and a BMI ≥24 kg/m2 (≥22 kg/m2 in Asian Americans). HbA1c was measured throughout DPP and DPPOS but was not an eligibility criterion. Participants were randomly assigned to placebo (n = 1,082), metformin titrated to 850 mg twice daily (n = 1,073), or intensive lifestyle intervention (n = 1,079). All DPP participants randomized to the metformin and placebo treatment groups (total n = 2,155) are considered in this publication (Table 1). Written informed consent was obtained from all participants, and the studies were approved by each clinical center’s institutional review board.
Table 1.
Characteristics of participants in metformin and placebo groups at DPP baseline (1996–1999)
| Cohort for glucose-based diagnoses |
Cohort for HbA1c-based diagnoses |
|||||
|---|---|---|---|---|---|---|
| Total (N = 2,155) | Placebo (N = 1,082) | Metformin (N = 1,073) | Total (N = 1,833) | Placebo (N = 922) | Metformin (N = 911) | |
| Age (yr) | ||||||
| Mean ± SD | 50.6 ± 10.4 | 50.3 ± 10.4 | 50.9 ± 10.3 | 50.3 ± 10.3 | 50.1 ± 10.4 | 50.4 ± 10.2 |
| 25–44 | 642 (29.8) | 324 (29.9) | 318 (29.6) | 562 (30.7) | 283 (30.7) | 279 (30.6) |
| 45–59 | 1,098 (51.0) | 557 (51.5) | 541 (50.4) | 934 (51) | 468 (50.8) | 466 (51.2) |
| ≥60 | 415 (19.3) | 201 (18.6) | 214 (19.9) | 337 (18.4) | 171 (18.5) | 166 (18.2) |
| Female | 1,457 (67.6) | 747 (69.0) | 710 (66.2) | 1,249 (68.1) | 643 (69.7) | 606 (66.5) |
| Parous women | ||||||
| No history of GDM | 951 (80.3) | 487 (80.0) | 464 (80.6) | 818 (80.4) | 422 (80.2) | 396 (80.5) |
| History of GDM | 233 (19.7) | 122 (20.0) | 111 (19.3) | 200 (19.6) | 104 (19.8) | 96 (19.5) |
| Race/ethnicity | ||||||
| Non-Hispanic white | 1,188 (55.1) | 586 (54.2) | 602 (56.1) | 1,087 (59.3) | 539 (58.5) | 548 (60.2) |
| African American | 441 (20.4) | 220 (20.3) | 221 (20.6) | 287 (15.7) | 140 (15.2) | 147 (16.1) |
| Hispanic | 330 (15.3) | 168 (15.5) | 162 (15.1) | 290 (15.8) | 151 (16.4) | 139 (15.3) |
| American Indian | 111 (5.2) | 59 (5.5) | 52 (4.8) | 97 (5.3) | 50 (5.4) | 47 (5.2) |
| Asian/Pacific Islander | 85 (3.9) | 49 (4.5) | 36 (3.4) | 72 (3.9) | 42 (4.6) | 30 (3.3) |
| BMI (kg/m2) | ||||||
| Mean ± SD | 34.0 ± 6.6 | 34.1 ± 6.7 | 33.9 ± 6.6 | 33.7 ± 6.5 | 33.8 ± 6.5 | 33.6 ± 6.4 |
| <30 | 689 (32.0) | 340 (31.4) | 349 (32.5) | 603 (32.9) | 300 (32.5) | 303 (33.3) |
| 30 to <35 | 658 (30.5) | 315 (29.1) | 343 (32.0) | 574 (31.3) | 276 (29.9) | 298 (32.7) |
| ≥35 | 808 (37.5) | 427 (39.5) | 381 (35.5) | 656 (35.8) | 346 (37.5) | 310 (34) |
| Fasting glucose (mg/dL) | ||||||
| Mean ± SD | 106.6 ± 8.4 | 106.7 ± 8.4 | 106.5 ± 8.5 | 105.4 ± 7.4 | 105.6 ± 7.4 | 105.2 ± 7.4 |
| 95–109 | 1,440 (66.8) | 726 (67.1) | 714 (66.5) | 1,324 (72.2) | 663 (71.9) | 661 (72.6) |
| 110–125* | 715 (33.2) | 356 (32.9) | 359 (33.5) | 509 (27.8) | 259 (28.1) | 250 (27.4) |
| 2-h glucose (mg/dL) | ||||||
| Mean ± SD | 164.8 ± 17.2 | 164.5 ± 17.1 | 165.1 ± 17.2 | 164.0 ± 16.9 | 163.8 ± 16.9 | 164.3 ± 17.0 |
| 140–153 | 699 (32.8) | 360 (33.3) | 339 (31.6) | 617 (33.7) | 315 (34.2) | 302 (33.2) |
| 154–172 | 730 (34.3) | 374 (34.6) | 356 (33.2) | 633 (34.5) | 328 (35.6) | 305 (33.5) |
| 173–199 | 726 (33.7) | 348 (32.2) | 378 (35.2) | 583 (31.8) | 279 (30.3) | 304 (33.4) |
| HbA1c | ||||||
| Mean ± SD (%) | 5.9 ± 0.50 | 5.9 ± 0.51 | 5.9 ± 0.50 | 5.8 ± 0.39 | 5.8 ± 0.4 | 5.8 ± 0.4 |
| <6% (42 mmol/mol) | 1,168 (54.3) | 578 (53.6) | 590 (55.1) | 1,161 (63.3) | 576 (62.5) | 585 (64.2) |
| 6–6.4% (42–46 mmol/mL) | 982 (45.7) | 501 (46.4) | 533 (49.7) | 672 (36.7) | 346 (37.5) | 326 (35.8) |
Data are n (%) unless otherwise indicated. yr, years.
*Thirty-eight participants who were recruited prior to the American Diabetes Association change in diagnostic criteria (9) had fasting glucose levels between 125 and 139 mg/dL at baseline.
After DPP ended in 2001, all participants were offered a group-administered version of the lifestyle curriculum. Eighty-six percent (n = 1,861) of the surviving members of the metformin and placebo treatment groups volunteered to continue follow-up in the DPPOS. Placebo was discontinued, and those previously assigned to metformin continued to receive metformin 850 mg twice daily, now unmasked. Metformin was discontinued if diabetes was diagnosed and fasting glucose level was ≥140 mg/dL during DPP (or HbA1c was ≥7% [53 mmol/mol] during DPPOS), which resulted in referral to the participant’s own physician for further management (2). Many such patients were subsequently treated with metformin by their own health care providers.
Measures
Diagnosis of diabetes during DPP and DPPOS was based on the annual oral glucose tolerance test (OGTT) or semiannual fasting plasma glucose (FPG) tests, using the 1997 American Diabetes Association diagnostic criteria (fasting ≥126 mg/dL or 2-h glucose ≥200 mg/dL during a 75-g OGTT), with the diagnosis requiring confirmation with repeat testing (9). In a previous analysis (7), diagnosis of diabetes was also determined post hoc based on HbA1c ≥6.5%. In the analyses with HbA1c as the diagnostic outcome, participants who had diabetes at baseline based on HbA1c ≥6.5% (48 mmol/mol) or fasting glucose 126–139 mg/dL (the original inclusion criteria included a FPG 100–139 mg/dL between 1996 and June 1997 [10], which was subsequently changed to 95–125 mg/dL) were excluded. This leaves 1,833 of the original DPP participants in the combined metformin and placebo treatment groups for the analyses herein that use HbA1c as the diabetes diagnostic outcome (Table 1).
Statistical Analyses
The current analyses cover an average of 15 years of DPP and DPPOS: participants were recruited from 1996–1999 and followed through the end of 2013. We identified subgroups of interest a priori based on sex, race/ethnicity, and baseline age, BMI, and fasting and 2-h postload plasma glucose and HbA1c levels and a self-reported history of GDM in parous women (1,4,7). Time to diabetes defined by glucose levels or by HbA1c compared metformin with placebo on a modified product-limit life table distribution with a log-rank test statistic, overall and within subgroup (11). Follow-up was censored at the participant’s last visit, regardless of DPPOS participation, if diabetes had not developed. Proportional hazards regression models were used to estimate hazard ratios (HRs) and assess heterogeneity. A likelihood ratio test of two models was used with and without the interaction term between treatment assignments and covariates (in continuous form for age, BMI, and glycemia). Rate difference (RD) on an absolute scale between the metformin and placebo groups was expressed in cases per 100 person-years based on treatment-specific crude rates calculated as the number of diabetes events divided by the total number of person-years of follow-up under a doubly homogenous Poisson model. This provides a linearized rate estimate over the total follow-up period (11). Heterogeneity in risk differences among subgroups was assessed using a composite Wald test (11). DPP and DPPOS have generally had low rates of missing data. Visit completion rates (∼87% of those enrolled) did not differ among the three treatment groups, and missing data were assumed to be missing at random. A P ≤ 0.05 was considered significant.
Results
The baseline characteristics of the metformin and placebo-assigned participants (1,082 placebo and 1,073 metformin) and the subset included in the HbA1c analyses are shown in Table 1. The consort diagram for this population followed over time has previously been published (3).
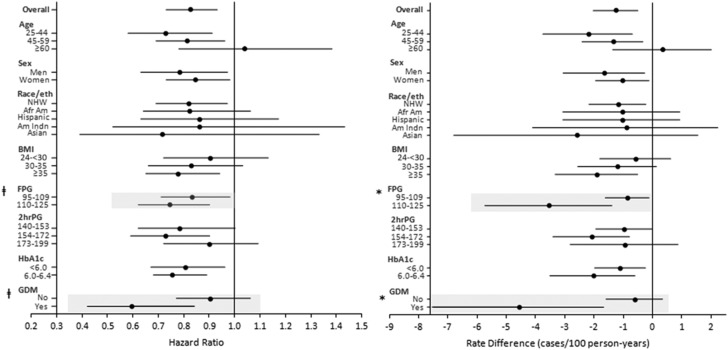
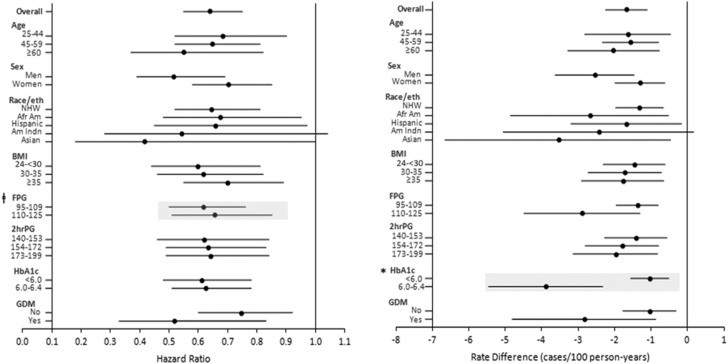
Through 15 years, the mean cumulative exposure to metformin in the original DPP participants assigned to metformin was 8.75 years (9,389.5 years of exposure/1,073 persons = 8.75 years/person) compared with 1.71 years (1,848.5 years/1,082 persons = 1.71 years/person) in the original placebo group (Supplementary Fig. 1). The metformin exposure in the placebo group was almost entirely owing to treatment with nonstudy metformin after the development of diabetes. During this time, the metformin treatment group had a 17% lower incidence of diabetes development than the placebo group (HR 0.83 [95% CI 0.73–0.93], RD −1.25 cases/100 person-years [95% CI −2.01 to −0.49]) based on fasting and/or 2-h glucose results (Fig. 1 and Table 2). With HbA1c used as the diagnostic outcome for diabetes, metformin was associated with a 36% reduction in risk (HR 0.64 [95% CI 0.55–0.75]) or an RD of −1.67 cases/100 person-years (95% CI −2.24 to −1.10) (Fig. 2 and Table 2).
Figure 1.
Forest plot of diabetes HRs and hazard RDs with diabetes defined by glucose levels for metformin vs. placebo over 15 years by subgroups defined at DPP baseline. Point estimates and 95% CIs shown. Highlighted rows show significant treatment-by-group interactions. Group interactions were tested using continuous values for baseline values of age (years), BMI (kg/m2), FPG and 2-h glucose (2hrPG) (mg/dL), and HbA1c (%). Statistically significant (P < 0.05) interactions of metformin treatment by subgroup are indicated by shading and as follows: *FPG-by-treatment interaction P = 0.02, GDM-by-treatment interaction P = 0.01; ‡FPG-by-treatment interaction P < 0.001, GDM-by-treatment interaction P = 0.02. Afr Am, African American; Am Indn, American Indian; eth, ethnicity; GDM, history of prior GDM; NHW, non-Hispanic white.
Table 2.
Metformin treatment effects on diabetes defined by fasting or 2-h postload glucose or by HbA1c ≥6.5%
| Subgroup | N | % | PLAC rate (cases/100 pyr) | MET rate (cases/100 pyr) | HR (95% CI) for MET vs. PLAC | Subgroup-by-MET P | RD (95% CI), cases/100 pyr | Subgroup-by-MET P |
|---|---|---|---|---|---|---|---|---|
| Diabetes defined by fasting or 2-h PG | ||||||||
| Overall | 2,155 | 100.0 | 7.14 | 5.89 | 0.83 (0.73–0.93) | −1.25 (−2.01 to −0.49) | ||
| Age, years | 0.17 | 0.08 | ||||||
| 25 to <45 | 642 | 29.8 | 8.19 | 5.99 | 0.73 (0.58–0.91) | −2.2 (−3.72 to −0.68) | ||
| 45 to <60 | 1,098 | 51.0 | 7.04 | 5.69 | 0.81 (0.69–0.96) | −1.35 (−2.39 to −0.32) | ||
| ≥60 | 415 | 19.3 | 5.93 | 6.28 | 1.04 (0.78–1.38) | 0.35 (−1.33 to 2.02) | ||
| Sex | 0.55 | 0.46 | ||||||
| Men | 698 | 32.4 | 7.49 | 5.85 | 0.78 (0.63–0.97) | −1.64 (−3.03 to −0.26) | ||
| Women | 1,457 | 67.6 | 6.99 | 5.90 | 0.85 (0.73–0.98) | −1.02 (−1.93 to −0.11) | ||
| Race/ethnicity | 0.99 | 0.97 | ||||||
| Non-Hispanic white | 1,188 | 55.1 | 6.52 | 5.34 | 0.82 (0.69–0.97) | −1.18 (−2.15 to −0.22) | ||
| African American | 441 | 20.5 | 8.84 | 7.32 | 0.82 (0.64–1.06) | −1.52 (−3.49 to 0.45) | ||
| Hispanic | 330 | 15.3 | 7.19 | 6.15 | 0.86 (0.63–1.17) | −1.04 (−3.03 to 0.94) | ||
| American Indian | 111 | 5.2 | 6.82 | 5.94 | 0.86 (0.52–1.43) | −0.89 (−4.01 to 2.24) | ||
| Asian/South Pacific Islander | 85 | 3.9 | 8.37 | 5.79 | 0.72 (0.39–1.33) | −2.58 (−6.72 to 1.56) | ||
| BMI, kg/m2 | 0.25 | 0.37 | ||||||
| 24 to <30 | 689 | 32.0 | 5.80 | 5.22 | 0.90 (0.72–1.13) | −0.58 (−1.78 to 0.63) | ||
| 30 to <35 | 658 | 30.5 | 6.83 | 5.64 | 0.83 (0.66–1.03) | −1.19 (−2.53 to 0.14) | ||
| ≥35 | 808 | 37.5 | 8.67 | 6.77 | 0.78 (0.65–0.94) | −1.9 (−3.30 to −0.50) | ||
| FPG, mg/dL | 0.0004 | 0.02 | ||||||
| 95–109 | 1,440 | 66.8 | 5.13 | 4.28 | 0.83 (0.71–0.98) | −0.86 (−1.6 to −0.11) | ||
| ≥110 | 715 | 33.2 | 14.10 | 10.60 | 0.75 (0.62–0.90) | −3.53 (−5.69 to −1.38) | ||
| 2-h PG, mg/dL | 0.60 | 0.37 | ||||||
| 140–153 | 699 | 32.4 | 4.47 | 3.51 | 0.78 (0.62–1.00) | −0.96 (−1.92 to 0) | ||
| 154–172 | 730 | 33.9 | 7.46 | 5.38 | 0.73 (0.59–0.90) | −2.08 (−3.38 to −0.78) | ||
| 173–199 | 726 | 33.7 | 10.7 | 9.74 | 0.90 (0.72–1.09) | −0.95 (−2.78 to 0.88) | ||
| HbA1c, % (mmol/mol) | 0.26 | 0.27 | ||||||
| <6.0 (42) | 1,168 | 62.9 | 5.57 | 4.47 | 0.81 (0.67–0.96) | −1.10 (−1.96 to −0.23) | ||
| 6.0–6.4 (42–46) | 688 | 37.1 | 8.26 | 6.22 | 0.76 (0.68–0.89) | −2.03 (−3.48 to −0.59) | ||
| GDM among parous women | 0.02 | 0.01 | ||||||
| No | 951 | 80.3 | 6.33 | 5.95 | 0.94 (0.78–1.13) | −0.39 (−1.48 to 0.71) | ||
| Yes | 233 | 19.7 | 11.1 | 6.48 | 0.59 (0.42–0.84) | −4.57 (−7.48 to −1.67) | ||
| Diabetes defined by HbA1c ≥6.5% | ||||||||
| Overall | 1,833 | 100.0 | 4.53 | 2.86 | 0.64 (0.55–0.75) | −1.67 (−2.24 to −1.1) | ||
| Age, years | 0.67 | 0.82 | ||||||
| 25 to <45 | 564 | 30.7 | 5.16 | 3.53 | 0.68 (0.52–0.90) | −1.63 (−2.8 to −0.46) | ||
| 45 to <60 | 936 | 51.0 | 4.29 | 2.74 | 0.65 (0.52–0.81) | −1.56 (−2.32 to −0.79) | ||
| ≥60 | 337 | 18.3 | 4.27 | 2.25 | 0.55 (0.37–0.82) | −2.02 (−3.26 to −0.77) | ||
| Sex | 0.08 | 0.06 | ||||||
| Men | 586 | 31.9 | 5.21 | 2.67 | 0.52 (0.39–0.69) | −2.53 (−3.61 to −1.46) | ||
| Women | 1,251 | 68.1 | 4.26 | 2.96 | 0.70 (0.58–0.85) | −1.3 (−1.98 to −0.62) | ||
| Race/ethnicity | 0.86 | 0.46 | ||||||
| Non-Hispanic white | 1,090 | 59.3 | 3.61 | 2.31 | 0.64 (0.52–0.81) | −1.31 (−1.96 to −0.66) | ||
| African American | 288 | 15.7 | 7.91 | 5.23 | 0.67 (0.48–0.95) | −2.67 (−4.82 to −0.52) | ||
| Hispanic | 290 | 15.8 | 4.86 | 3.20 | 0.66 (0.45–0.97) | −1.67 (−3.17 to −0.16) | ||
| American Indian | 97 | 5.3 | 5.39 | 2.96 | 0.54 (0.28–1.04) | −2.42 (−5.01 to 0.17) | ||
| Asian/Pacific Islander | 72 | 3.9 | 5.83 | 2.30 | 0.42 (0.18–1.00) | −3.53 (−6.6 to −0.46) | ||
| BMI (kg/m2) | 0.34 | 0.88 | ||||||
| 24 to <30 | 605 | 32.9 | 3.56 | 2.11 | 0.60 (0.44–0.81) | −1.45 (−2.3 to −0.61) | ||
| 30 to <35 | 575 | 31.3 | 4.39 | 2.68 | 0.62 (0.46–0.82) | −1.71 (−2.71 to −0.71) | ||
| ≥35 | 657 | 35.8 | 5.65 | 3.88 | 0.70 (0.55–0.89) | −1.77 (−2.89 to −0.65) | ||
| FPG, mg/dL | 0.04 | 0.08 | ||||||
| 95–109 | 1,328 | 72.3 | 3.55 | 2.18 | 0.62 (0.50–0.76) | −1.37 (−1.95 to −0.8) | ||
| ≥110 | 509 | 27.7 | 7.92 | 5.04 | 0.66 (0.51–0.85) | −2.88 (−4.46 to −1.3) | ||
| 2-h PG, mg/dL | 0.91 | 0.71 | ||||||
| 140–153 | 619 | 33.7 | 3.64 | 2.23 | 0.62 (0.46–0.84) | −1.41 (−2.26 to −0.56) | ||
| 154–172 | 634 | 34.5 | 4.76 | 2.97 | 0.64 (0.49–0.83) | −1.79 (−2.79 to −0.79) | ||
| 173–199 | 584 | 31.8 | 5.40 | 3.43 | 0.64 (0.49–0.84) | −1.97 (−3.12 to −0.82) | ||
| HbA1c, % (mmol/mol) | 1,161 | 63.3 | 2.70 | 1.67 | 0.057 | 0.001 | ||
| <6.0 (42) | 672 | 36.7 | 9.53 | 5.65 | 0.61 (0.48–0.78) | −1.03 (−1.55 to −0.51) | ||
| 6.0–6.4 (42–46) | 1,161 | 63.3 | 2.70 | 1.67 | 0.63 (0.51–0.78) | −3.88 (−5.43 to −2.32) | ||
| GDM among parous women | 0.21 | 0.13 | ||||||
| No | 818 | 80.4 | 4.14 | 2.97 | 0.73 (0.57–0.92) | −1.17 (−2.01 to −0.34) | ||
| Yes | 200 | 19.6 | 5.80 | 2.97 | 0.52 (0.33–0.83) | −2.82 (−4.78 to −0.87) |
MET, metformin; PG, postload glucose; PLAC, placebo; pyr, person-years.
Figure 2.
Forest plot of diabetes HRs and hazard RDs with diabetes defined by HbA1c levels for metformin vs. placebo over 15 years by subgroups defined at DPP baseline. Point estimates and 95% CIs shown. Highlighted rows show significant treatment-by-group interactions. Group interactions were tested using continuous values for baseline values of age (years), BMI (kg/m2), FPG and 2-h glucose (2hrPG) (mg/dL), and HbA1c (%). Statistically significant (P < 0.05) interactions of metformin treatment by subgroup are indicated by shading and as follows: *HbA1c-by-treatment interaction P = 0.001; ‡FPG-by-treatment interaction P = 0.04. Afr Am, African American; Am Indn, American Indian; eth, ethnicity; GDM, history of prior GDM; NHW, non-Hispanic white.
The analyses of the effects of metformin on diabetes development over 15 years in subgroups are shown for glucose-based diabetes in Table 2 and Fig. 1 and for HbA1c-based diabetes in Table 2 and Fig. 2. Based on RDs and HRs when using glucose levels for diagnosis, there were no significant interactions with baseline age, sex, race/ethnicity, BMI, 2-h plasma glucose, or HbA1c levels. The metformin group had a greater effect at higher baseline FPG (interaction P = 0.02 for RD and P = 0.0004 for HR). Of note, the different effects of metformin by age seen in the original analyses after ∼3 years of DPP were no longer seen by age-group (25–45, 45–59, and ≥60 years of age) (Table 2). With age considered as a continuum, the interaction was not statistically significant (interaction P = 0.08 for the RD). Although the interactions with age were not significant, when considered in isolation the oldest age-group had no benefit with metformin when glucose was used for diagnosis (HR 1.04 [absolute rate was higher in the metformin group by 0.35 cases/100 person-years]) (Fig. 1). By contrast, in the youngest age-group (25–45 years), the HR was 0.73 and the RD was −2.2 cases/100 person-years (Table 2). Similarly, the interactions for the HR and RD were not significant for BMI, indicating no difference in the metformin benefit by BMI. However, considered in isolation, only the highest BMI group had a significant benefit with metformin. History of GDM had a significant interaction with metformin effect on HR (interaction P = 0.03), with a 41% reduction (HR 0.59) in diabetes development for metformin versus placebo in women with a self-reported history of GDM but a nonsignificant 6% reduction (HR 0.94) in parous women who did not report a history of GDM. The GDM-by-treatment interaction was even more pronounced when analyzed by RD, with metformin reducing diabetes incidence by 4.57 cases/100 person-years in women with a history of GDM compared with only 0.38 in women without such a history (interaction P = 0.01).
When the outcome was diabetes defined by HbA1c, there were no statistically significant interactions using HRs of diabetes development with metformin compared with placebo among the subgroups defined by demographic characteristics or any of the preselected clinical variables. Metformin was equally effective in women with or without a history of GDM history (Fig. 2 and Table 2). Therefore, compared with placebo, metformin had comparable beneficial effects by HR across all of the subgroups when HbA1c was used as the outcome. However, while the effect of metformin was nearly identical in those with baseline HbA1c <6.0% (42 mmol/mol) vs. 6.0% to 6.4% (42–46 mmol/mol) based on HRs (0.61 and 0.63, respectively), there was substantial heterogeneity if the absolute difference in cases was used (RDs −1.03 and −3.88 cases/100 person-years, respectively, interaction P = 0.001).
Ideally, we could have explored heterogeneity in various combinations of the baseline factors, but the number of cases and participants in the individual cells were generally too small to allow reliable estimates of the metformin effect for many of the combinations. We therefore restricted these exploratory analyses of baseline factor combinations in those with heterogeneity (namely, GDM status and fasting glucose) and with age (Supplementary Tables 1 and 2).
For example, Fig. 1 and Table 2 show that in those with fasting glucose ≥110 mg/dL, metformin led to a much greater risk difference (RD −3.53 cases/100 person-years) than in those with lower fasting glucose (RD −0.86), and there was a much greater risk difference in women with than those without a history of GDM. These observations raise the question of effects in combinations, such as higher fasting glucose (associated with greater benefit) among women without a history of GDM (associated with less benefit). Supplementary Table 1 suggests approximate additivity of these effects in that the least benefit (RD −0.15) was in women with no history of GDM and lower fasting glucose and the greatest benefit (RD −10.13) occurred in women with a history of GDM and higher fasting glucose. Women in whom one of these factors indicated higher risk and the other indicated lower risk derived intermediate benefit (RD −3.65 or −3.40). These differences in risk differences with metformin were statistically significant (P = 0.008 for interaction of metformin with the subgroups). The interactions of metformin with the other subgroups shown in Supplementary Tables 1 and 2 were not statistically significant, albeit many of the subgroups were small, affording little power for analyses of such combinations.
Conclusions
Previous analyses of the original DPP data supported a particularly powerful effect of metformin in subgroups defined by higher fasting glucose levels, higher BMI, and a history of GDM, when evaluated by percent risk reduction, i.e., the HR for metformin compared with placebo. These results prompted the American Diabetes Association (5), among others (12–16), to suggest that metformin be considered in the prevention of diabetes in people at high risk. The American Diabetes Association specifically recommended that metformin be considered in those subgroups that it concluded had the greatest relative benefit with metformin in the DPP. This recommendation is further supported by the demonstrated cost savings of metformin in diabetes prevention (17).
Examining treatment interactions in terms of the heterogeneity of HRs does not give the full picture needed to decide which sets of persons are likely to derive more or less benefit from the intervention. One should also consider the absolute differences in incidence rates among groups, i.e., RDs. Under homogeneity of treatment effects on HRs, the RDs (metformin vs. placebo) are greater in groups with higher underlying rates and lower in groups with lower underlying rates. For example, in a subgroup with a very low rate of progression to disease, there is little room for improvement in absolute rates even if the HR produced by the treatment is the same as in the high-risk groups. The strongest example of this in the current study is the interaction of baseline HbA1c with diabetes when the outcome is defined by HbA1c (Table 1 and Fig. 1B). There is no heterogeneity using the HR (HRs of 0.61 and 0.63 in the low and high baseline HbA1c groups, respectively), but the treatment effects on an absolute scale differ substantially (RDs due to metformin = −1.03 and −3.88 cases/100 person-years in the two groups, respectively, interaction P = 0.001). By this measure, public health treatment decisions regarding the use of metformin in patients with prediabetes should prioritize those with higher baseline HbA1c.
We observed differences in the absolute rates of diabetes development using glucose-defined versus HbA1c-defined diabetes. During DPP/DPPOS, most diabetes development was diagnosed based on the 2-h glucose level in the OGTT. HbA1c was not yet a generally accepted method of diagnosis during the DPP study period, and we considered it a diabetes-defining outcome only in post hoc analyses. The OGTT, fasting glucose levels, and HbA1c measure different aspects of glucose metabolism. The 2-h glucose level largely reflects glucose disposal into the insulin-sensitive peripheral tissues, predominantly muscle, while the fasting glucose level and HbA1c are measures of hepatic glucose output and overall mean glycemia, respectively. Metformin is known to have its major effects by reducing hepatic glucose production, thereby lowering overnight glycemia and fasting glucose (18), the latter an important contributor to the HbA1c. These effects are consistent with the relatively greater effect of metformin on HbA1c-defined diabetes that we have shown here, including among subgroups that showed somewhat less beneficial effects with glucose-defined diabetes.
Whether the glucose-based results or HbA1c-based results should be given greater credence is complicated. On the one hand, glucose-based results were used for eligibility and outcomes during the study and the selection of participants with baseline HbA1c <6.5% (48 mmol/mol) for the current analyses was performed post hoc. Thus, the participants in our analysis represent a subset of those first selected based on their glucose-defined prediabetes, with HbA1c criteria applied subsequently. This adversely affects the generalizability of the HbA1c results and represents the major limitation of these analyses. On the other hand, in many countries, OGTTs are not used routinely for the identification of persons at high risk for diabetes or with diabetes. Therefore, the HbA1c results may be more clinically relevant.
In summary, regardless of the means by which diabetes is diagnosed, the long-term effects of metformin on diabetes development in DPP/DPPOS suggest that metformin remains effective in this cohort. We have identified specific subgroups where metformin’s effect was enhanced, namely, those with higher baseline fasting glucose or HbA1c and women reporting a history of GDM. These results should help to prioritize those groups at high risk of developing diabetes who will benefit most from being treated with metformin. The conclusions regarding HbA1c must be considered carefully, as our original eligibility and diabetes development criteria were based on glucose and not HbA1c criteria. Continuing the follow-up for other outcomes, including incidence of microvascular disease, cancer, and cardiovascular disease, will provide information on other putative long-term benefits of metformin and whether they are homogeneous across subgroups.
Supplementary Material
Article Information
Acknowledgments. The Diabetes Prevention Program Research Group gratefully acknowledges the commitment and dedication of the participants of the DPP and DPPOS.
Funding and Duality of Interest. During the DPP and DPPOS, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health provided funding to the clinical centers and the Coordinating Center for the design and conduct of the study and collection, management, analysis, and interpretation of the data (U01-DK-048489). The Southwestern American Indian Centers were supported directly by the NIDDK, including its Intramural Research Program, and the Indian Health Service. The General Clinical Research Center Program, National Center for Research Resources, and Department of Veterans Affairs supported data collection at many of the clinical centers. Funding was also provided by the National Institute of Child Health and Human Development; the National Institute on Aging; the National Eye Institute; the National Heart, Lung, and Blood Institute; the National Cancer Institute; the Office of Research on Women’s Health; the National Institute on Minority Health and Health Disparities; the Centers for Disease Control and Prevention; and the American Diabetes Association. LifeScan, Inc.; Health o meter; Hoechst Marion Roussel, Inc.; Merck-Medco Managed Care, Inc.; Merck and Co.; Nike Sports Marketing; Slim Fast Foods Co.; and Quaker Oats Co. donated materials, equipment, or medicines for concomitant conditions. Lipha (Merck-Santé) provided medication and LifeScan, Inc., donated materials during the DPP and DPPOS. This research was also supported, in part, by the Intramural Research Program of the NIDDK. Bristol-Myers Squibb and Parke-Davis provided additional funding and material support during the DPP. McKesson BioServices Corp.; Matthews Media Group, Inc.; and the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., provided support services under subcontract with the Coordinating Center. All authors in the writing group had access to all data. No other potential conflicts of interest relevant to this article were reported.
The sponsor of this study was represented on the Steering Committee and played a part in study design, how the study was done, and publication.
The opinions expressed are those of the investigators and do not necessarily reflect the views of the funding agencies. The funding agencies were not represented on the writing group, although all members of the Steering Committee had input into the report’s contents. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author Contributions. D.M.N. researched data, wrote the first draft of the manuscript, and contributed to discussion. W.C.K., J.P.C., D.D., R.B.G., S.E.K., K.J.M., X.P.-S., G.T., and E.A.W. researched data, contributed to discussion, and reviewed the manuscript. S.L.E. and M.T. researched data, edited and reviewed the manuscript, contributed to discussion, and performed all data analyses. S.L.E. and M.T. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 77th Scientific Sessions of the American Diabetes Association, San Diego, CA, 9–13 June 2017.
Appendix
The writing committee was as follows: David M. Nathan (chair), William C. Knowler, Sharon L. Edelstein, Jill P. Crandall, Dana Dabelea, Ronald B. Goldberg, Steven E. Kahn, Kieren J. Mather, Xavier Pi-Sunyer, Gilda Trandafirescu, Elizabeth A. Walker, and Marinella Temprosa.
Footnotes
Clinical trial reg. nos. NCT00038727 and NCT00004992, clinicaltrials.gov
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc18-1970/-/DC1.
This article is featured in a podcast available at http://www.diabetesjournals.org/content/diabetes-core-update-podcasts.
*A complete list of centers, investigators, and staff can be found in the Supplementary Data online.
A complete list of the members of the writing committee can be found in the Appendix.
See accompanying article, p. 499.
Contributor Information
Collaborators: Diabetes Prevention Program Research Group, David M. Nathan, William C. Knowler, Sharon Edelstein, Jill P. Crandall, Dana Dabelea, Ronald B. Goldberg, Steven E. Kahn, Kieren J. Mather, Gilda Trandafirescu, Elizabeth A. Walker, Marinella Temprosa, George A. Bray, Kishore Gadde, Annie Chatellier, Jennifer Arceneaux, Amber Dragg, Crystal Duncan, Frank L. Greenway, Daniel Hsia, Erma Levy, Monica Lockett, Donna H. Ryan, David Ehrmann, Margaret J. Matulik, Kirsten Czech, Catherine DeSandre, Barry J. Goldstein, Kevin Furlong, Kellie A. Smith, Wendi Wildman, Constance Pepe, Jeanette Calles, Juliet Ojito, Sumaya Castillo-Florez, Anna Giannella, Olga Lara, Beth Veciana, Steven M. Haffner, Helen P. Hazuda, Maria G. Montez, Kathy Hattaway, Carlos Lorenzo, Arlene Martinez, Tatiana Walker, Richard F. Hamman, Lisa Testaverde, Denise Anderson, Alexis Bouffard, Tonya Jenkins, Dione Lenz, Leigh Perreault, David W. Price, Sheila C. Steinke, Edward S. Horton, Catherine S. Poirier, Kati Swift, Enrique Caballero, Barbara Fargnoli, Ashley Guidi, Mathew Guido, Sharon D. Jackson, Lori Lambert, Kathleen E. Lawton, Sarah Ledbury, Jessica Sansoucy, Jeanne Spellman, Brenda K. Montgomery, Wilfred Fujimoto, Robert H. Knopp, Edward W. Lipkin, Ivy Morgan-Taggart, Anne Murillo, Lonnese Taylor, April Thomas, Elaine C. Tsai, Dace Trence, Abbas E. Kitabchi, Samuel Dagogo-Jack, Mary E. Murphy, Laura Taylor, Jennifer Dolgoff, Debra Clark, Uzoma Ibebuogu, Helen Lambeth, Harriet Ricks, Lily M.K. Rutledge, Judith E. Soberman, Mark E. Molitch, Boyd E. Metzger, Mariana K. Johnson, Mimi M. Giles, Diane Larsen, Samsam C. Pen, Mary Larkin, Charles McKitrick, Heather Turgeon, Ellen Anderson, Laurie Bissett, Kristy Bondi, Enrico Cagliero, Kali D’Anna, Linda Delahanty, Jose C. Florez, Valerie Goldman, Peter Lou, Alexandra Poulos, Elyse Raymond, Christine Stevens, Beverly Tsent, Elizabeth Barrett-Connor, Mary Lou Carrion-Petersen, Lauren N. Claravall, Jonalle M. Dowden, Javiva Horne, Diana Leos, Sundar Mudaliar, Jean Smith, Simona Szerdi Janisch, Karen Vejvoda, F. Xavier Pi-Sunyer, Jane E. Lee, Sandra T. Foo, Susan Hagamen, David G. Marrero, Susie M. Kelly, Paula Putenney, Marcia A. Jackson, Gina McAtee, Ronald T. Ackermann, Carolyn M. Cantrell, Edwin S. Fineberg, Angela Hadden, Mario S. Kirkman, Erin O’Kelly Phillips, Paris J. Roach, Robert E. Ratner, Vanita Aroda, Sue Shapiro, Catherine Bavido-Arrage, Peggy Gibbs, Gabriel Uwaifo, Renee Wiggins, Mohammed F. Saad, Karol Watson, Medhat Botrous, Sujata Jinagouda, Maria Budget, Claudia Conzues, Perpetua Magpuri, Kathy Ngo, Kathy Xapthalamous, Neil H. White, Angela L. Brown, Samia Das, Prajakta Khare-Ranade, Tamara Stich, Ana Santiago, Cormarie Wernimont, Christopher D. Saudek, Sherita Hill Golden, Tracy Whittington, Frederick L. Brancati, Jeanne M. Clark, Alicia Greene, Dawn Jiggetts, Henry Mosley, John Reusing, Richard R. Rubin, Shawne Stephens, Evonne Utsey, David S. Shade, Karwyn S. Adams, Claire Hemphill, Penny Hyde, Janene L. Canady, Kathleen Colleran, Ysela Gonzeles, Doris A. Hernandez-McGinnis, Carolyn King, Jill Crandall, Janet O. Brown, Elsie Adorno, Helena Duffy, Angela Goldstein, Jennifer Lukin, Helen Martinez, Dorothy Pompi, Harry Shamoon, Jonathan Scheindlin, Judith Wylie-Rosett, Trevor Orchard, Andrea Kriska, Susan Jeffries, M. Kaye Kramer, Marie Smith, Catherine Benchoff, Stephanie Guimond, Jessica Pettigrew, Debra Rubinstein, Linda Semler, Elizabeth Venditti, Valarie Weinzierl, Richard F. Arakaki, Narleen K. Baker-Ladao, Mae K. Isonaga, Nina E. Bermudez, Marjorie K. Mau, John S. Melish, Robin E. Yamamoto, Norman Cooeyate, Alvera Enote, Mary A. Hoskin, Camille Natewa, Carol A. Percy, Kelly J. Acton, Vickie L. Andre, Roz Barber, Shandiin Begay, Brian C. Bucca, Sherron Cook, Jeff Curtis, Charlotte Dodge, Matthew S. Doughty, Jason Kurland, Justin Glass, Martia Glass, Roberta L. Hanson, Louise E. Ingraham, Kathleen M. Kobus, Jonathan Krakoff, Catherine Manus, Cherie McCabe, Sara Michaels, Tina Morgan, Julie A. Nelson, Christopher Piromalli, Robert J. Roy, Sandra Sangster, Miranda Smart, Darryl P. Tonemah, Rachel Williams, Charlton Wilson, Sarah Fowler, Michael Larsen, Tina Brenneman, Hanna Sherif, Solome Abebe, Julie Bamdad, Melanie Barkalow, Joel Bethepu, Tsedenia Bezebeh, Nicole Butler, Jackie Callaghan, Caitlin E. Carter, Costas Christophi, Gregory M. Dwyer, Mary Foulkes, Yuping Gao, Robert Gooding, Adrienne Gottlieb, Nisha Grover, Heather Hoffman, Ashley N. Hogan, Kathleen Jablonski, Richard Katz, Preethy Kolinjivadi, John M. Lachin, Yong Ma, Qing Pan, Susan Reamer, Alla Sapozhnikova, Elizabeth M. Venditti, Andrea M. Kriska, Linda Semler, Valerie Weinzierl, Santica Marcovina, Greg Strylewicz, John Albers, Judith Fradkin, Stanford Garfield, Christine Lee, Edward Gregg, Ping Zhang, William H. Herman, Michael Brändle, and Morton B. Brown
References
- 1.Knowler WC, Barrett-Connor E, Fowler SE, et al.; Diabetes Prevention Program Research Group . Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diabetes Prevention Program Research Group, Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;14:1677–1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diabetes Prevention Program Research Group Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol 2015;3:866–875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ratner RE, Christophi CA, Metzger BE, et al.; Diabetes Prevention Program Research Group . Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab 2008;93:4774–4779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Diabetes Association 5. Prevention or delay of type 2 diabetes: Standards of Medical Care in Diabetes–2017. Diabetes Care 2017;40(Suppl. 1):S44–S47. [DOI] [PubMed] [Google Scholar]
- 6.International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32:1327–1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diabetes Prevention Program Research Group HbA1c as a predictor of diabetes and as an outcome in the Diabetes Prevention Program: a randomized clinical trial. Diabetes Care 2015;38:51–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diabetes Prevention Program Research Group The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care 1999;22:623–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997;20:1183–1197 [DOI] [PubMed] [Google Scholar]
- 10.American Diabetes Association Screening for diabetes. Diabetes Care 1990;13(Suppl. 1):7–9 [PubMed] [Google Scholar]
- 11.Lachin JM. Biostatistical Methods: The Assessment of Relative Risks, 2nd Edition. New York, John Wiley, 2000, p. 83–87 [Google Scholar]
- 12.Twigg SM, Kamp MC, Davis TM, Neylon EK, Flack JR; Australian Diabetes Society; Australian Diabetes Educators Association . Prediabetes: a position statement from the Australian Diabetes Society and Australian Diabetes Educators Association. Med J Aust 2007;186:461–465 [DOI] [PubMed] [Google Scholar]
- 13.Guzman JR. Documentos Selectos de Posición y Consenso de ALAD (Associatión Lationoamericano de diabetes). Ac Farmacéutica, 2013. Available from https://issuu.com/alad-diabetes/docs/guias_alad_2013. Accessed 13 February 2019 [Google Scholar]
- 14.Ransom T, Goldenberg R, Mikalachki A, Prebtani AP, Punthakee Z; Canadian Diabetes Association Clinical Practice Guidelines Expert Committee . Reducing the risk of developing diabetes. Can J Diabetes 2013;37(Suppl. 1):S16–S19 [DOI] [PubMed] [Google Scholar]
- 15.Alberti KG, Zimmet P, Shaw J. International Diabetes Federation: a consensus on type 2 diabetes prevention. Diabet Med 2007;24:451–463 [DOI] [PubMed] [Google Scholar]
- 16.Türkiye Endokrinoloji ve Metabolizma Dernegi. Díabetes Mellítus Ve Komplíkasyonlarinin TaniI, Tedaví Ve İzlem Kilavizu–2011. Diabetes Mellitus Çalışma ve Eğitim Grubu 2013. Available from https://www.yumpu.com/tr/document/view/10981596/diabetes-mellitus-vekomplikasyonlarnn-tan-tedavi-ve-izlem. Accessed 13 February 2019
- 17.Diabetes Prevention Program Research Group The 10-year cost-effectiveness of lifestyle intervention or metformin for diabetes prevention: an intent-to-treat analysis of the DPP/DPPOS. Diabetes Care 2012;35:723–730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foretz M, Guigas B, Bertrand L, Pollak M, Viollet B. Metformin: from mechanisms of action to therapies. Cell Metab 2014;20:953–966 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.