Abstract
Hospital readmission within 30 days of discharge is an important quality measure given that it represents a potentially preventable adverse outcome. Approximately, 20% of Medicare beneficiaries are readmitted within 30 days of discharge. Many strategies such as the hospital readmission reduction program have been proposed and implemented to reduce readmission rates. Prior research has shown that coordination of care could play a significant role in lowering readmissions. Although having a hospital-based skilled nursing facility (HBSNF) in a hospital could help in improving care for patients needing short-term skilled nursing or rehabilitation services, little is known about HBSNFs’ association with hospitals’ readmission rates. This study seeks to examine the association between HBSNFs and hospitals’ readmission rates. Data sources included 2007-2012 American Hospital Association Annual Survey, Area Health Resources Files, the Centers for Medicare and Medicaid Services (CMS) Medicare cost reports, and CMS Hospital Compare. The dependent variables were 30-day risk-adjusted readmission rates for acute myocardial infarction (AMI), congestive heart failure, and pneumonia. The independent variable was the presence of HBSNF in a hospital (1 = yes, 0 = no). Control variables included organizational and market factors that could affect hospitals’ readmission rates. Data were analyzed using generalized estimating equation (GEE) models with state and year fixed effects and standard errors corrected for clustering of hospitals over time. Propensity score weights were used to control for potential selection bias of hospitals having a skilled nursing facility (SNF). GEE models showed that the presence of HBSNFs was associated with lower readmission rates for AMI and pneumonia. Moreover, higher SNFs to hospitals ratio in the county were associated with lower readmission rates. These findings can inform policy makers and hospital administrators in evaluating HBSNFs as a potential strategy to lower hospitals’ readmission rates.
Keywords: hospital-based skilled nursing facilities, readmission rates, coordination of care, vertical integration, resource-based view
What do we already know about this topic?
Given the prior research, we know that many factors such as improper discharge planning, insufficient follow-up, lack of care coordination, and poor communication between providers along the continuum of care could lead to higher hospital readmission rates, and that better coordination of care between acute and post-acute care may exhibit the most potential to reduce readmission rates.
How does your research contribute to the field?
This study explores the relationship between hospital-based skilled nursing facilities and readmission rates using data for years 2007 to 2012 and a methodology that includes generalized estimating equations with state and year fixed effects, and propensity score weights to control for potential selection bias of hospitals having an skilled nursing facility (SNF).
What are the research’s implications toward theory, practice, or policy?
Findings of this study could be used by health care administrators, payers, and policy makers to evaluate the strategies related to their access to post-acute care services through vertical integration and the role of hospital-based skilled nursing facilities in improving the care processes and patients’ transition between various health care settings.
Introduction
Hospital readmissions within 30 days of discharge are an essential quality measure as they represent a potentially preventable adverse outcome.1-4 Readmissions not only drive costs5 but also account, on average, for 20% of the Medicare beneficiaries being readmitted within 30 days of discharge from the hospital.6,7 A variety of strategies such as the hospital readmission reduction program have been proposed and implemented to reduce readmission rates.8-10 These initiatives have tied the hospitals’ reimbursement to their readmission rates. Consequently, many hospitals have been exploring strategies to effectively reduce their readmissions.11
Prior research has identified many factors that could lead to higher readmission rates.12 These factors include poor quality of inpatient care, inadequate staffing,13 inadequate discharge planning and premature discharge, improper transitions of care, insufficient follow-up, lack of care coordination, and poor communication between acute and post-acute care (PAC) providers.10,12,14,15 Several studies have suggested that better coordination of care and communication between acute and PAC providers may have the most potential to reduce readmission rates.6,16-19
Establishing a skilled nursing unit within a hospital, ie, a hospital-based skilled nursing facility (HBSNF), could improve coordination of care5 and quality of PAC.20 HBSNF refers to a facility which is licensed by the state as a skilled nursing facility (SNF), is located inside a hospital, shares its governing board, is financially integrated with the hospital, and the two (hospital and HBSNF) file their Medicare cost reports together.21,22 HBSNFs have also been referred to as “sub-acute care units” and “transitional care units” in the literature.23 For this study, these terms are used interchangeably. In 2010, there were 1058 HBSNFs in the United States with 55 311 patients.24
Among Medicare patients, HBSNFs provide care to those who “need short-term” skilled nursing and/or rehabilitation services after a hospital stay of at least 3 days, are not well enough to go home, and need extended medical supervision or nursing services.8,25-27 HBSNFs can serve as a potential mechanism for better coordination of patient care through improved access to physicians, nurses, therapists, and ancillary services (such as x-ray and laboratory exams), thereby facilitating the transition from acute to PAC, and ultimately into the community.28
Although HBSNFs could play a significant coordinating role in patients’ transition from acute to PAC, little is known about their association with hospitals’ readmission rates. The few studies that have examined this relationship have focused on the effect of HBSNF closures on health care utilization and patient outcomes among Medicare fee-for-service (FFS) beneficiaries,29 differences in patient outcomes of free-standing SNFs and HBSNFs,30 the effect of HBSNF beds reduction on rehospitalizations of free-standing SNFs in the area,31 and differences between hospital patients discharged to a HBSNF versus a free-standing SNF, in terms of SNF use and days spent in the community.32 No study, to our knowledge, has explored the association between the presence of HBSNFs and hospitals’ readmission rates.
The purpose of this article is to examine whether hospitals that have HBSNFs experience lower readmission rates than hospitals that do not have them. This study will allow providers, payers, and policy makers to understand better the role HBSNFs could play in coordinating patients’ care during the transition from acute to PAC or into the community. It would also allow hospital administrators to evaluate whether having an HBSNF could be a viable strategy to achieve lower readmission rates.
Conceptual Framework
As a conceptual framework, this article refers to tenets from the vertical integration literature and the resource-based view (RBV) of the firm to explore the role of HBSNFs in lowering readmission rates for hospitals. Readmissions have often been attributed to the breakdown in communication and coordination of care associated with treating acute episodes and the PAC after the acute episode is over.10,12,14 Due to their potential negative implications for patients’ health status, readmissions are considered an important measure of the quality of care.12,16,33,34
Vertical Integration
The external environment continuously presents organizations with a variety of challenges as well as opportunities.35 Organizations respond to these changes by embracing various strategies to adapt and maintain or improve their performance.36,37 The health care environment has undergone a variety of changes over the years such as the advent of managed care, implementation of reimbursement reforms such as the prospective payment system, and the health care reform efforts with the Affordable Care Act. In response to these changes, hospitals have pursued strategies such as vertical integration to maintain or improve their performance.
In health care, a vertically integrated organization represents “an arrangement whereby the organization offers, either directly or through others, a broad range of patient care and support services operated in a functionally unified manner.”38 This range of services offered may include pre-acute, acute, and PAC organized around a hospital.38 The concept of vertical integration has been used to study various organizational forms or arrangements adopted by health care organizations to deliver care.39,40 Vertically integrated health care organizations have the potential to achieve clinical integration, defined as “the extent to which patients’ care services are coordinated across people, functions, activities, processes, and operating units to maximize the value of services delivered.”41 Tighter linkages, arising from integration between different levels of care under one organizational umbrella, could allow for better control of patient flow, greater access to patients’ health information, standardization of care processes, increased efficiency, and better coordination of care along the continuum.42,43 For instance, HBSNFs can facilitate clinical integration and transitions in care from acute to PAC through the use of organizational resources, such as electronic health records (EHRs) and team-based care. Better clinical integration, in turn, may result in lower readmission rates.
Resource-Based View of the Firm
RBV of the firm seeks to explain the link between internal characteristics of an organization and its performance. More specifically, it examines the differences in the performance of organizations (firms) and the relationship of these differences with the variation in their resources and capabilities.44 Firm resources are those that are controlled by the firm and allow it to conceive and implement value-creating strategies.45,46 Examples of firm resources include all tangible and intangible assets, capabilities, firm attributes, and knowledge.45 Integration of acute, transitional, and PAC in the form of an HBSNF within an acute care hospital represents a tangible resource which could influence the performance of the hospital.
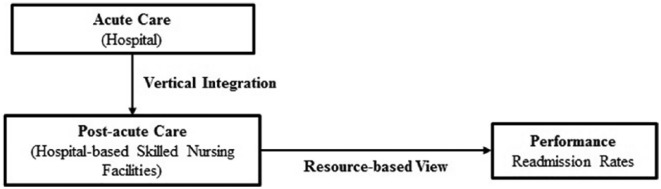
HBSNFs could prove valuable to hospitals by facilitating delivery of higher quality patient care through improved communication and better coordination among care providers. However, this process involves coordination among different care providers, and between care providers and various organizational resources, or coordinating bundles of resources needed to provide appropriate patient care. According to Lawrence and Lorsch,35 it is easier to coordinate the use of resources and build capabilities within an organization than among multiple organizations. Therefore, vertical integration could facilitate the enhancement of organizational capabilities by reducing the difficulties in coordination of resources.47 The theoretical framework (Figure 1) summarizes the relationships conceptualized in this article by showing how a vertical integration strategy of having an HBSNF (a tangible resource) would be linked to organizational performance (readmission rates).
Figure 1.
Theoretical framework to study whether hospitals with hospital-based skilled nursing facilities have lower readmission rates than hospital without.
Rahman and colleagues47 found that stronger hospital-SNF referral linkages were associated with lower readmission rates.31,47 Some of the factors that may allow HBSNFs to better coordinate care for patients include improved access to treating physicians, greater availability of nursing resources per patient, and immediate and timely availability of resources, such as emergency services and equipment.25,41,48-50 Similarly, the use of the same EHRs platform could minimize errors during transitions between acute and PAC settings, as well as improve the quality of services delivered at each point in the process.38 Therefore, having an HBSNF could allow hospitals to develop unique resources to better monitor and control the quality of care delivered to its patients,25 thereby potentially lowering their readmission rates. Therefore, this article hypothesizes the following:
Hypothesis: Hospitals with HBSNFs experience lower readmissions rates than the hospitals without them.
Methods
Data Sources
Data for this study were derived from 4 sources: the American Hospital Association (AHA) Annual Survey, the Area Health Resources Files (AHRF), Center for Medicare and Medicaid Services (CMS) Medicare Cost Reports, and CMS Hospital Compare. The AHA survey includes information on the organizational characteristics of hospitals and their inpatient and outpatient utilization.51 The AHRF data set contains county-level information on socioeconomic status, population demographics, and environmental characteristics.52 The CMS Medicare Cost Reports is a public access data set that contains the financial information for all hospitals accepting Medicare patients.53 The Hospital Compare data set includes information on the 30-day risk-adjusted readmission rates for acute myocardial infarction (AMI), congestive heart failure (CHF), and pneumonia.54
The study sample consisted of all nonfederal, medical/surgical, acute-care hospitals (n = 24 556 hospital-year observations) operating in the United States between 2007 and 2012. As only the cases with complete information were utilized in the regression analyses, the final analytic samples were 8357 hospital-year observations for AMI, 13 464 hospital-year observations for CHF, and 14 114 hospital-year observations were for pneumonia. The study protocol was approved by the University of Alabama at Birmingham’s Institutional Review Board (IRB).
Measures
Dependent variables
The dependent variables represent the 30-day risk-adjusted readmission rates for AMI, CHF, and pneumonia. It measures the rate of unplanned readmissions for AMI, CHF, or pneumonia to any acute-care hospital within 30 days of discharge from hospitalization. It includes Medicare beneficiaries aged 65 years or more who were enrolled in traditional FFS Medicare for an entire 12 months prior to their hospitalization as well as those who were admitted to Veteran’s Health Administration (VA) hospitals. The readmission rates are risk-adjusted for patient characteristics (gender, age, past medical history, and other comorbidities), which could increase the risk of readmission among the patients irrespective of the quality of care provided by the hospital.54
Independent variable
The independent variable represents the presence or absence of an HBSNF in a hospital. It was created based on the number of HBSNF beds reported by the hospital in the AHA survey and Medicare Cost Reports. It was assigned the value of “1” if the number of HBSNF beds was greater than 0 in either AHA database or Medicare cost reports and “0” if it was 0 HBSNF beds or missing (1 = have HBSNF, and 0 = do not have HBSNF).
Control variables
The analysis controlled for organizational and market factors that have been found to be associated with readmissions55-59 and hospitals’ quality of care.60-62 The organizational control variables included hospital system affiliation, network participation, teaching status, ownership status (for-profit, not-for-profit, government hospitals), location (urban vs rural), hospital size (setup and / or staffed beds), length of stay (Medicare inpatient days / Medicare discharges), occupancy rate ([total inpatient days × 100] / [total number of staffed beds × 365]), payer mix (percentage of Medicare patients and percentage of Medicaid patients), and registered nurse (RN) staffing intensity (full-time equivalent RNs per 1000 inpatient days). The market-level control variables included competition among acute care hospitals, Medicare Advantage (managed care) penetration, SNF to hospital ratio in the county, number of primary care physician per 1000 population, poverty, and unemployment rate. Competition was measured by Herfindahl-Hirschman Index (HHI).63 HHI is defined as the sum of squares of an individual hospital’s market share. Scores close to “0” indicate a highly competitive market while scores of “1” indicate a monopolistic market.
Analysis
The bivariate analysis was performed to assess the differences in the organizational and market characteristics between hospitals with and without HBSNFs. Generalized estimating equation (GEE) models with state and year fixed effects were used to examine the effect of HBSNFs on the overall variation in hospitals’ readmissions. GEE models take into account the within-subject correlation characteristic of longitudinal panel data. The state fixed effects controlled for interstate differences, including regulations, which could influence the hospitals’ readmission rates, while year fixed effects accounted for time trends.
To address potential selection bias of hospitals with a SNF, we used propensity score weighting of the GEE models. To estimate the propensity score, a logistic regression model was used where HBSNF status was regressed on the baseline control variables: hospital size (total beds), length of stay (Medicare), occupancy rate, percentage of Medicaid patients, RN staffing, system affiliation, ownership, market competition, poverty, and unemployment rate. Then, the inverse of the propensity score—a propensity score weight—was calculated and included in the models.
Sensitivity analysis, using the independent variable with 3 groups (hospitals that never had SNF, hospitals that changed their SNF status, and hospitals that always had SNF), was performed to examine the robustness of the results. The results were interpreted as significant for P value ≤.05. SAS 9.3 and STATA 13 were used to conduct the data management and analyses.
Findings
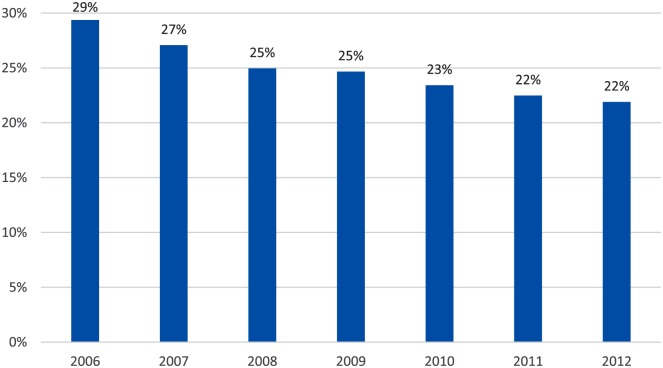
Figure 2 shows the proportion of hospitals with a SNF over the study period. There was a 7% decrease in the proportion of hospitals with a SNF, from 29% of hospitals having a SNF in 2006 to 22% in 2012.
Figure 2.
Proportion of hospitals with skilled nursing facilities over the study period (2006-2012).
Table 1 presents the descriptive statistics for this study with independent-samples t tests for continuous variables and chi-square for categorical variables. Hospitals with HBSNFs had lower pneumonia 30-day readmission rates (mean = 17.97) compared to those without a HBSNF (mean = 18.08; P < .001). The hospitals that had HBSNFs were less likely to be a teaching hospital (5%) or for-profit hospital (9%), but more likely to be located in rural areas (8%). Moreover, the hospitals that had HBSNFs were, on average, larger (200 beds), had higher occupancy rate (62%), and longer lengths of stay for their Medicare patients (7.7) than the hospitals without HBSNFs. However, compared to hospitals without HBSNFs, hospitals with one had lower RN staffing intensity (5.8), a lower percentage of Medicare patients (44%), and a higher percentage of Medicaid (27%). Finally, hospitals with HBSNFs were located in markets characterized by a lower competition (0.8) and a lower percentage of people in poverty (16.3%).
Table 1.
Descriptive Analysis of Variables (Means and Percentages) (N = 24 556).
| Variable | Have HBSNFs (n = 5863)a Mean (SD)/n (percentages) |
Do not have HBSNFs (n = 18 693)a Mean (SD)/n (percentages) |
P value |
|---|---|---|---|
| Thirty-day readmission rate for AMI (%) | 19.26 (0.03) | 19.22 (0.02) | .291 |
| Thirty-day readmission rate for CHF (%) | 24.04 (0.03) | 24.06 (0.02) | .516 |
| Thirty-day readmission rate for pneumonia (%) | 17.97 (0.02) | 18.08 (0.01) | <.001 |
| System affiliation | <.001 | ||
| No | 2940 (50.14) | 7606 (40.69) | |
| Yes | 2923 (49.86) | 11 087 (59.31) | |
| Network participation | .147 | ||
| No | 2422 (55.64) | 7566 (56.90) | |
| Yes | 1931 (44.36) | 5732 (43.10) | |
| Teaching hospital | <.001 | ||
| No | 5593 (95.39) | 17 420 (93.19) | |
| Yes | 270 (4.61) | 1273 (6.81) | |
| Ownership status | <.001 | ||
| For-profit | 539 (9.19) | 3774 (20.19) | |
| Not-for-profit | 3955 (67.46) | 11 001 (58.85) | |
| Government | 1369 (23.35) | 3918 (20.96) | |
| Location | <.001 | ||
| Rural | 484 (8.27) | 987 (5.28) | |
| Urban | 5368 (91.73) | 17 698 (94.72) | |
| Hospital size | 200.60 (2.36) | 163.20 (1.27) | <.001 |
| Length of stay (Medicare) | 7.66 (0.08) | 5.28 (0.03) | <.001 |
| Occupancy rate (%) | 61.72 (0.25) | 52.86 (0.15) | <.001 |
| Percentage of Medicare patients (%) | 43.94 (0.27) | 53.18 (0.12) | <.001 |
| Percentage of Medicaid patients (%) | 27.45 (0.28) | 16.13 (0.08) | <.001 |
| RN staffing intensity | 5.76 (0.06) | 10.46 (0.26) | <.001 |
| Market competition (HHI) | 0.80 (0.01) | 0.73 (0.01) | <.001 |
| Medicare managed care penetration (%) | 21.98 (0.19) | 22.21 (0.11) | .290 |
| SNF to hospital ratio (%) | 1.81 (0.02) | 1.78 (0.01) | .336 |
| Poverty (%) | 16.33 (0.07) | 16.74 (0.04) | <.001 |
| Unemployment rate (%) | 8.01 (0.04) | 7.94 (0.02) | .093 |
| PCP per 1000 population | 0.70 (0.01) | 0.71 (0.01) | .041 |
Note. HBSNFs = hospital-based skilled nursing facilities; AMI = acute myocardial infarction; CHF = congestive heart failure; HHI = Herfindahl-Hirschman index; RN = registered nurse; SNF = skilled nursing facility; PCP = primary care physician.
Hospital-year observations (2007-2012).
The propensity score weighted GEE model with state and year fixed results showed that the hospitals with HBSNFs, as compared to the ones without HBSNF, were associated with lower readmission rates for AMI (β = −0.19, P < .05) and pneumonia (β = −1.04, P < .001) (Table 2). This provides partial support to our hypothesis.
Table 2.
Generalized Estimating Equations with State and Year Fixed Effects Regression Results for the Relationship between Presence of HBSNFs and 30-Day Readmission Rates of AMI, CHF, and Pneumonia.
| AMI (n = 8357)a |
CHF (n = 13 464)a |
Pneumonia (n = 14 114)a |
|
|---|---|---|---|
| Variables | Coefficient | Coefficient | Coefficient |
| Independent variable | |||
| HBSNF status | |||
| No | reference | reference | reference |
| Yes | −0.1857* | 0.0354 | −1.0348*** |
| Control variables | |||
| Organizational factors | |||
| System affiliation | |||
| No | reference | reference | reference |
| Yes | 0.1981*** | −1.3029*** | −1.1984*** |
| Network participation | |||
| No | reference | reference | reference |
| Yes | −0.5205*** | 0.0679 | −0.3346*** |
| Teaching hospital | |||
| No | reference | reference | reference |
| Yes | 0.0128 | 0.0738 | −0.2809 |
| Ownership status | |||
| For-profit | reference | reference | reference |
| Not-for-profit | −0.0807 | 0.0027 | −0.4002*** |
| Government | −0.0434 | −1.0519*** | −0.7071*** |
| Location | |||
| Rural | reference | reference | reference |
| Urban | −0.3124 | 0.9428*** | −1.8661*** |
| Hospital size | −0.0003* | 0.0010** | 0.0016*** |
| Length of stay (Medicare) | 0.0154 | −0.0400*** | −0.0363*** |
| Occupancy rate | 0.0077*** | 0.0406*** | 0.0170*** |
| Proportion of Medicare patients | −0.0039*** | 0.0188*** | 0.0161*** |
| Proportion of Medicaid patients | 0.0017 | 0.0104*** | 0.0272*** |
| RN staffing intensity | 0.0083*** | 0.0608*** | 0.0170*** |
| Market factors | |||
| Market competition (HHI) | 0.2869*** | 0.9772*** | 0.1675*** |
| Medicare managed care penetration | 0.0226*** | 0.0361*** | 0.0558*** |
| SNF to hospital ratio | −0.0188 | −0.0968*** | −0.0767*** |
| Poverty | −0.0057 | −0.0082 | −0.0060 |
| Unemployment rate | −0.0018 | −0.2413*** | −0.2122*** |
| PCP per 1000 population | 0.1207 | −0.6360*** | 0.0289 |
Note. HBSNFs = hospital-based skilled nursing facilities; AMI = acute myocardial infarction; CHF = congestive heart failure; RN = registered nurse; HHI = Herfindahl-Hirschman index; SNF = skilled nursing facilities; PCP = primary care physician.
Hospital-year observations (2007-2012).
P ≤ .05. **P ≤ .01. ***P ≤ .001.
Among the control variables, the system-affiliated hospitals, as compared to the hospitals without affiliation, were associated with lower readmission rates for CHF (β = −1.30, P < .001) and pneumonia (β = −1.20, P < .001). However, this association was positive for AMI; system-affiliated hospitals were associated with higher AMI readmission rates (β = 0.20, P < .001). The hospitals that participated in networks were associated with lower readmission rates for AMI (β = −0.52, P < .001) and pneumonia (β = −0.34, P < .001). Hospital ownership status was also related to readmission rates for CHF and pneumonia. Government hospitals, compared with for-profit hospitals, were associated with lower readmission rates for CHF (β = −1.05, P < .001) and pneumonia (β = −0.71, P < .001). Furthermore, not-for-profit hospitals, compared with for-profit hospitals, were associated with lower pneumonia readmission rates (β = −0.40, P < .001). The effect of hospital location on readmission rates was mixed. Hospitals that were located in urban areas, in comparison with the ones in rural areas, were associated with higher readmission rate for CHF (β = 0.94, P < .001) but lower readmission rate for pneumonia (β = −1.87, P < .001). Likewise, the effects of hospital size and the proportion of Medicare patients had mixed results. Size was negatively correlated with AMI readmission rate (β = −0.0003, P < .05) while positively correlated with CHF (β = 0.001, P < .01) and pneumonia (β = 0.002, P < .001) readmission rates. The proportion of Medicare patients was also negatively correlated with AMI readmission rate (β = −0.004, P < .001), yet positively correlated with CHF (β = 0.02, P < .001) and pneumonia (β = 0.02, P < .001) readmission rates. Furthermore, the length of stay was associated with lower readmission rates for CHF (β = −0.04, P < .001) and pneumonia (β = −0.04, P < .001). Similarly, a higher proportion of SNFs to hospitals in the county had a significant association with lower readmission rates for CHF (β = −0.10, P < .001) and pneumonia (β = −0.08, P < .001).
On the contrary, occupancy rate had a significant association with higher readmission rates for AMI (β = 0.01, P < .001), CHF (β = 0.04, P < .001), and pneumonia (β = 0.02, P < .001). A greater Medicare managed care penetration in the market was also associated with a higher readmission rates for AMI (β = 0.02, P < .001), CHF (β = 0.04, P < .001), and pneumonia (β = 0.06, P < .001). Similarly, higher RN staffing levels had a significant association with higher readmission rates for AMI (β = 0.01, P < .001), CHF (β = 0.06, P < .001), and pneumonia (β = 0.02, P < .001). Last, hospitals located in less competitive markets had higher readmission rates for AMI (β = 0.29, P < .001), CHF (β = 0.98, P < .001), and pneumonia (β = 0.17, P < .001).
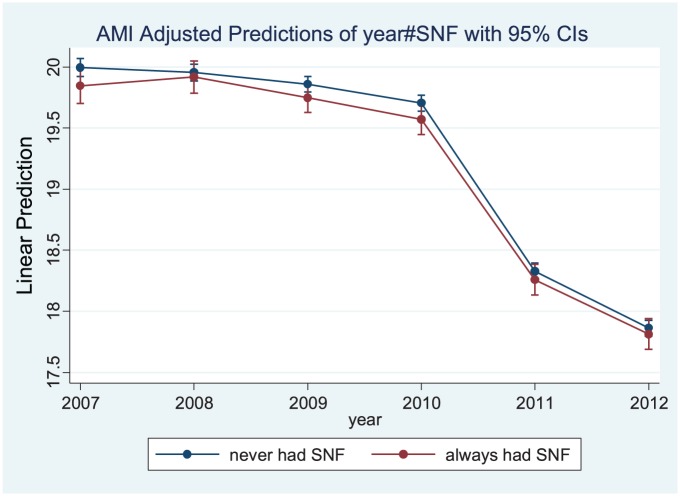
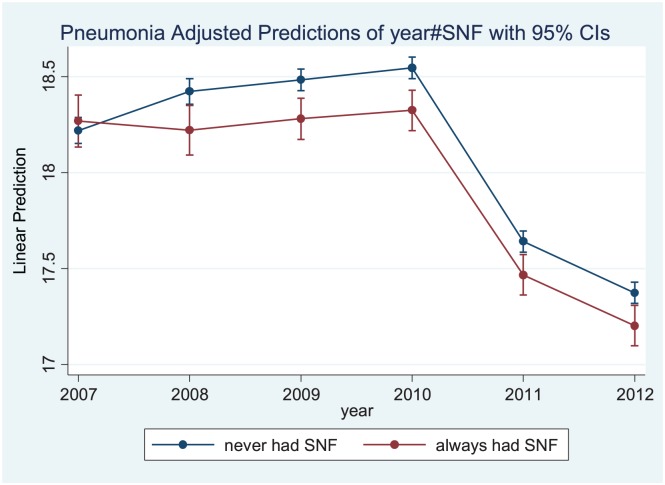
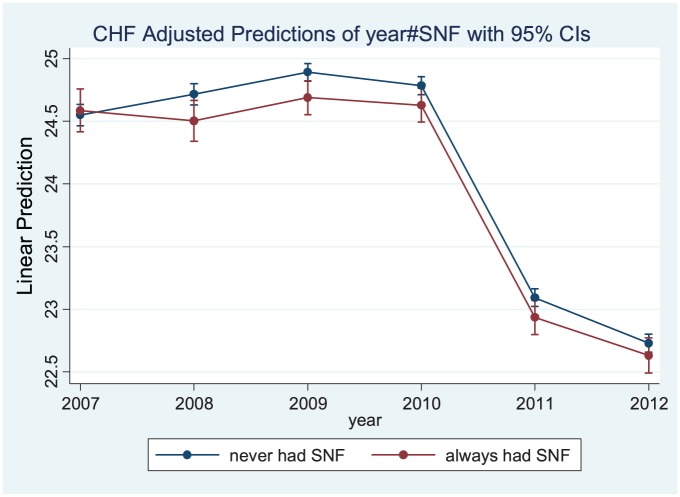
The marginal effects of the HBSNF status over time on readmission rates for AMI, CHF, and pneumonia indicated that the hospitals that always had HBSNFs experienced more significant reductions in their readmission rate compared with those that never had one, as shown in Table 3 and Figures 3 to 5.
Table 3.
Generalized Estimating Equations with State and Year Fixed Effects Regression Results for the Relationship between Hospital SNF Status and 30-Day Readmission Rates of AMI, CHF, and Pneumonia.
| AMI (n = 8358)a |
CHF (n = 13 465)a |
Pneumonia (n = 14 115)a |
|
|---|---|---|---|
| Variables | Coefficient | Coefficient | Coefficient |
| Independent variable | |||
| HBSNF status | |||
| Never had SNF | reference | reference | reference |
| Changed SNF status | −0.0751 | −0.0278 | −0.1327* |
| Always had SNF | −0.1553** | −0.1853** | −0.2490*** |
| Control variables | |||
| Organizational factors | |||
| System affiliation | |||
| No | reference | reference | reference |
| Yes | 0.0249 | −0.0353 | −0.0169 |
| Network participation | |||
| No | reference | reference | reference |
| Yes | −0.0342 | −0.0508 | −0.0162 |
| Teaching hospital | |||
| No | reference | reference | reference |
| Yes | 0.0414 | 0.3749** | 0.1358 |
| Ownership status | |||
| For-profit | reference | reference | reference |
| Not-for-profit | −0.2722*** | −0.3731*** | −0.2957*** |
| Government | −0.1485* | −0.2365** | −0.2063** |
| Location | |||
| Rural | reference | reference | reference |
| Urban | −0.0510 | −0.2892** | −0.2422** |
| Hospital size | 0.0001 | −0.0005* | 0.0005** |
| Length of stay (Medicare) | −0.0121 | −0.0230*** | −0.0083 |
| Occupancy rate | 0.0037** | 0.0058*** | 0.0046*** |
| Proportion of Medicare patients | 0.0023 | 0.0034* | 0.0029* |
| Proportion of Medicaid patients | 0.0045* | 0.0044* | 0.0031* |
| RN staffing intensity | −0.0030** | −0.0054** | −0.0033 |
| Market factors | |||
| Market competition (HHI) | 0.0582 | 0.2181** | 0.0085 |
| Medicare managed care penetration | 0.0045* | 0.0055* | 0.0054** |
| SNF to hospital ratio | −0.0250 | −0.0527** | −0.0204 |
| Poverty | 0.0083 | 0.0251*** | 0.0147*** |
| Unemployment rate | 0.0369* | 0.0518*** | 0.0488*** |
| PCP per 1000 population | 0.0919 | −0.0469 | 0.0419 |
Note. HBSNFs = hospital-based skilled nursing facilities; SNF = skilled nursing facilities; AMI = acute myocardial infarction; CHF = congestive heart failure; RN = registered nurse; HHI = Herfindahl-Hirschman index; PCP = primary care physician.
Hospital-year observations (2007-2012).
P ≤ .05. **P ≤ .01. ***P ≤ .001.
Figure 3.
Marginal effects of AMI readmission rates over the study period (2007-2012).
Note. AMI = acute myocardial infarction; SNF = skilled nursing facilities; CI = confidence interval.
Figure 5.
Marginal effects of pneumonia readmission rates over the study period (2007-2012).
Note. SNF = skilled nursing facilities; CI = confidence interval.
Figure 4.
Marginal effects of CHF readmission rates over the study period (2007-2012).
Note. CHF = congestive heart failure; SNF = skilled nursing facilities; CI = confidence interval.
Discussion
The purpose of this study was to evaluate the association between the presence of HBSNFs in hospitals and their readmission rates, using tenets from the of vertical integration literature and RBV. This article hypothesized that hospitals with HBSNFs would experience lower readmission rates, through better coordination of patient care, given that poor communication and care coordination among providers has been identified as one of the most common causes for higher readmission rates.10,12 The GEE model revealed that the presence of HBSNFs was associated with lower readmission rates for AMI and pneumonia. However, no significant association was observed for CHF. This result can be attributed to the difference between CHF and AMI/pneumonia. While AMI and pneumonia are considered acute illnesses, CHF is a chronic condition. It may be more difficult to tease out a significant relationship for a chronic condition due to many potential confounding factors.
The observed relationship between the presence of HBSNF and lower readmissions rates could be attributed to better integration of acute, transitional, and PAC for patients admitted to a HBSNF. Therefore, HBSNFs may lower hospitals’ readmission rates by facilitating better communication between providers and easier access to resources such as technology needed for care of medically complex patients. Rahman and colleagues31 also suggested that the HBSNFs may be more effective in reducing specifically the early readmissions (bounce backs) due to greater access to physicians and other medical resources. In a recent study, Rahman and colleagues32 found that patients who were discharged to HBSNFs spent fewer days in SNFs and more days in the community. Even though the study was based on a cross-sectional 2009 data, the use of instrumental variable to control for differential selection of individuals into HBSNF versus free-standing SNF has made the study findings important and relevant to our findings. Especially when one considers that HBSNFs tend to have separate administration, the synergy and care coordination achieved between hospitals and HBSNFs is worth exploring further to understand the underlying mechanisms that lead to such better patient outcomes.
However, the study results cannot be attributed solely to the presence of HBSNFs in a hospital. For instance, delay in placement of Medicare patients in the SNFs leads to longer length of stay and poor patient outcomes for the hospitals.40 To ensure timely access to skilled nursing services and reduction in adverse patient outcomes, hospitals may develop interorganizational exchange relationships with SNFs in the market instead of owning a HBSNF.31 The significant association of a greater proportion of SNFs to hospitals in the county with lower readmission rates for AMI and CHF in this study may reflect such a relationship.
Among the organizational control variables, higher RN staffing intensity was associated with higher readmission rates in both models, which is counter to the findings of prior studies.57,64,65 For instance, Joynt and Jha57 found that hospitals with high RN staffing ratios had lower readmission rates. The results of this study also show that higher occupancy rate is associated with higher readmission rates for AMI, CHF, and pneumonia. These results are similar to those of Erdem et al,66 who found that readmission rates increased with hospitals’ occupancy rate. This increase may result from the premature discharge of patients from hospitals to free up the beds for additional patients.
Among the market-level control variables, greater Medicare managed care penetration was associated with higher readmission rates for all 3 conditions. As our readmission measure captures only FFS Medicare patients, the observed positive relationship between higher Medicare managed care penetration and FFS readmissions may be a result of Medicare managed care attracting healthier beneficiaries. This may result in FFS inpatients having more complicated health problems, which may increase the likelihood of readmissions.
We also found that increased market competition results in lower readmission rates. This finding parallels those of prior studies showing that increased market competition is associated with better hospital quality of care.61,67 Given public reporting of readmission rates, hospitals in more competitive markets may have a greater incentive to invest in quality improvement67 and transition in care activities, which may ultimately lead to lower readmissions.
Limitations
Outcomes of this study were influenced by several limitations. First, the independent variable is dichotomous which only conveys the information related to the presence or absence of HBSNFs in hospitals. It does not capture the information related to the extent to which the hospitals that have HBSNFs utilize its services or the nature of coordination. Second, the dependent variable (readmissions rates) is calculated using the hospitals’ discharge data for 3 years and includes hospitalizations only for Medicare beneficiaries, 65 years and above of age, who were enrolled in a traditional FFS Medicare for entire 12 months prior to their hospitalization. Third, the study utilizes secondary data, which limited the scope of the study to the variables available in the data sets.
Given these limitations, there are some directions for future research regarding the relationship between hospitals with HBSNFs and various patient outcomes utilizing more detailed data about HBSNFs. Availability of details about HBSNFs, such as their utilization and staffing, could allow for a better evaluation of the potential role of HBSNFs in the continuum of patient care. The processes related to care coordination among health care providers and patients’ transition between acute and PAC settings could also be included in future studies. Assessing the care coordination processes may also assist in the better evaluation of the association between the presence of HBSNFs and improvement in measures of quality of care and patient satisfaction.
Historically, there have been minimal incentives for hospitals to manage care after an acute episode. However, changes in the reimbursement system, such as Medicare’s hospital readmission reduction program, bundled payments, and accountable care organizations, are creating incentives for acute and PAC management by holding providers accountable for the quality of acute and PAC delivered to patients. Poor information exchange, communication, and coordination of care have been identified as the primary causes of poor patient outcomes such as avoidable readmissions. For instance, hospitals incur reimbursement penalties for “excess” readmissions with the implementation of the hospital readmission reduction program33,68,69 Therefore, hospitals will need to build tighter linkages and collaborations across the continuum of care to achieve superior patient outcomes and avoid the penalties.8,70 Greater access to HBSNFs or free-standing SNFs in the markets could allow the hospitals to better coordinate transitions between different health care settings for their patients and reduce their readmission rates.9
Conclusion
Overall, the findings of this study could be used by health care organizations to evaluate strategies related to their access to PAC services through either HBSNFs or free-standing SNFs operating in their market and the role these strategies could play in improving patient outcomes. For instance, a potential strategy for hospitals to reduce readmission rates may be to improve information exchange processes between providers through a shared EHR platform between the acute and post-acute setting. Similarly, policy makers could utilize the findings of this study to evaluate the policies that promote and incentivize the vertical or horizontal integration between providers, thereby improving the care processes related to patients’ transition between various health care settings.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Robert Weech-Maldonado was supported in part by the Agency for Healthcare Research and Quality (R01HS023345).
ORCID iDs: Shivani Gupta  https://orcid.org/0000-0003-3562-4561
https://orcid.org/0000-0003-3562-4561
Robert Weech-Maldonado  https://orcid.org/0000-0002-5005-0909
https://orcid.org/0000-0002-5005-0909
References
- 1. Cykert S. Improving care transitions means more than reducing hospital readmissions. N C Med J. 2012;73(1):31-33. [PubMed] [Google Scholar]
- 2. Medicare Hospital Compare. https://www.medicare.gov/hospitalcompare/Data/30-day-measures.html. Published 2012. Accessed December 6, 2018.
- 3. MedPAC. Report to the Congress: Medicare Payment Policy. http://www.medpac.gov/docs/default-source/reports/Mar07_EntireReport.pdf. Published March 2007. Accessed December 6, 2018.
- 4. van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: A systematic review. CMAJ. 2011;183(7):E391-E402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Anderson MA, Tyler D, Helms LB, Hanson KS, Sparbel KJ. Hospital readmission from a transitional care unit. J Nurs Care Qual. 2005;20(1):26-35. [DOI] [PubMed] [Google Scholar]
- 6. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: A systematic review. Ann Intern Med. 2011;155(8):520-528. [DOI] [PubMed] [Google Scholar]
- 7. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. [DOI] [PubMed] [Google Scholar]
- 8. Dummit LA. Medicare’s bundling pilot: Including post-acute care services. Issue Brief No. 841, National Health Policy Forum, The George Washington University, Washington DC; March 28, 2011. [PubMed] [Google Scholar]
- 9. Ouslander JG, Diaz S, Hain D, Tappen R. Frequency and diagnoses associated with 7-and 30-day readmission of skilled nursing facility patients to a nonteaching community hospital. J Am Med Dir Assoc. 2011;12(3):195-203. [DOI] [PubMed] [Google Scholar]
- 10. Stone J, Hoffman GJ. Medicare hospital readmissions: Issues, policy options and PPACA. Congressional Research Service Report for Congress, September 21, 2010; 1-37. [Google Scholar]
- 11. Sood N, Huckfeldt PJ, Escarce JJ, Grabowski DC, Newhouse JP. Medicare’s bundled payment pilot for acute and postacute care: Analysis and recommendations on where to begin. Health Aff (Millwood). 2011;30(9):1708-1717. doi: 10.1377/hlthaff.2010.0394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Minott J. Reducing hospital readmissions. Academy Health. Published November 2008;23(2):1-10. Accessed on December 6, 2018. [Google Scholar]
- 13. Thomas KS, Mor V, Tyler DA, Hyer K. The relationships among licensed nurse turnover, retention, and rehospitalization of nursing home residents. Gerontologist. 2013;53(2):211-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. DeCoster V, Ehlman K, Conners C. Factors contributing to readmission of seniors into acute care hospitals. Educ Gerontol. 2013;39(12):878-887. doi: 10.1080/03601277.2013.767615. [DOI] [Google Scholar]
- 15. Kirsebom M, Wadensten B, Hedström M. Communication and coordination during transition of older persons between nursing homes and hospital still in need of improvement. J Adv Nurs. 2013;69(4):886-895. [DOI] [PubMed] [Google Scholar]
- 16. Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med. 2000;160(8):1074-1081. [DOI] [PubMed] [Google Scholar]
- 17. Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: Results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822-1828. [DOI] [PubMed] [Google Scholar]
- 18. Epstein CD, Tsaras G, Amoateng-Adjepong Y, Greiner PA, Manthous C. Does race affect readmission to hospital after critical illness? Heart Lung. 2009;38(1):66-76. [DOI] [PubMed] [Google Scholar]
- 19. King BJ, Gilmore-Bykovskyi AL, Roiland RA, Polnaszek BE, Bowers BJ, Kind AJ. The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J Am Geriatr Soc. 2013;61(7):1095-1102. doi: 10.1111/jgs.12328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rahman M, Norton EC, Grabowski DC. Do hospital-owned skilled nursing facilities provide better post-acute care quality? J Health Econ. 2016;50:36-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Deangelis P., Jr. Hospital based SNFs: An alternative to empty beds. Healthc Financ Manage. 1987;41(8):60-62, 64, 66 passim. [PubMed] [Google Scholar]
- 22. Whitman J, DeAngelis P, Knapp M. Restructuring hospital capacity: The hospital-based skilled nursing facility. Chicago,Ill: Hospital Research and Educational Trus; t; 1986. [Google Scholar]
- 23. Smith CA. Discharge destination and cost of care in an acute care unit versus a hospital-based skilled nursing unit. Doctoral dissertation: University of New Mexico; 1996. [Google Scholar]
- 24. American Health Care Association. The State Long-Term Health Care Sector: Characteristics, Utilization and Government Funding: 2011 Update. Reimbursement and Research Department American Health Care Association, Washington, DC: Published 2011. Accessed 24 February, 2014. [Google Scholar]
- 25. McDowell TN., Jr. The subacute care patient: Hospital responses to the challenge. J Health Hosp Law. 1990;23(10):289-294. [PubMed] [Google Scholar]
- 26. Murad Y. Skilled nursing facilities and post-acute care. J Gerontol Geriatr Res. 2011;1(101):1-4. [Google Scholar]
- 27. MedPAC. Report to the Congress: Medicare Payment Policy. http://www.medpac.gov/docs/default-source/reports/mar14_entirereport.pdf. Published March 2014. Accessed November 28, 2018.
- 28. Joseph JA. A study of hospitals’ changes in length of stay and number of discharges as a result of changes in financial incentives related to medicare exempt status for hospital-based skilled nursing care [dissertation]. Pittsburgh, PA: University of Pittsburgh; 1998. [Google Scholar]
- 29. White C, Seagrave S. What happens when hospital-based skilled nursing facilities close? A propensity score analysis. Health Serv Res. 2005;40(6 Pt 1):1883-1897. doi: 10.1111/j.1475-6773.2005.00434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Stearns SC, Dalton K, Holmes GM, Seagrave SM. Using propensity stratification to compare patient outcomes in hospital-based versus freestanding skilled-nursing facilities. Med Care Res Rev. 2006;63(5):599-622. doi: 10.1177/1077558706290944. [DOI] [PubMed] [Google Scholar]
- 31. Rahman M, Zinn JS, Mor V. The impact of hospital-based skilled nursing facility closures on rehospitalizations. Health Serv Res. 2013;48(2 Pt 1):499-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rahman M, Norton EC, Grabowski DC. Do hospital-owned skilled nursing facilities provide better post-acute care quality? J Health Econ. 2016;50:36-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: Paying for coordinated quality care. JAMA. 2011;306(16):1794-1795. [DOI] [PubMed] [Google Scholar]
- 34. Medicare Program. Hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system and FY 2012 rates; hospitals’ FTE resident caps for graduate medical education payment: Final rules. Federal Register. 2011;76(160):51660-51676. [PubMed] [Google Scholar]
- 35. Lawrence PR, Lorsch JW. Organization and environment: Managing differentiation and integration. Boston, MA: Irwin; 1967. [Google Scholar]
- 36. Child J. Organizational structure, environment and performance: The role of strategic choice. Sociology. 1972;6(1):1-22. [Google Scholar]
- 37. Donaldson L. American Anti-Management Theories of Organization: A critique of paradigm proliferation. Vol. 25 Cambridge: Cambridge University Press; 1995. [Google Scholar]
- 38. Conrad DA, Dowling WL. Vertical integration in health services: Theory and managerial implications. Health Care Manage Rev. 1990;15(4):9-21. [DOI] [PubMed] [Google Scholar]
- 39. Robinson JC. Administered pricing and vertical integration in the hospital industry. J Law Econ. 1996;39:357-378. [Google Scholar]
- 40. Lehrman S, Shore KK. Hospitals’ vertical integration into skilled nursing: A rational approach to controlling transaction costs. Inquiry. 1998;35(3):303-314. [PubMed] [Google Scholar]
- 41. Shortell SM, Gillies RR, Anderson DA, Erickson KM, Mitchell JB. Remaking health care in America. Hosp Health Netw. 1996;70(6):43-44. [PubMed] [Google Scholar]
- 42. Conrad D, Shortell S. Integrated health systems: Promise and performance. Front Health Serv Manage. 1996;13(1):3-40. [PubMed] [Google Scholar]
- 43. Zingmond DS. A description of the vertical integration of acute and post-acute care and its impact on patients with stroke in California, 1997 to 1998 [Dissertation]. Los Angeles, CA: University of California, Los Angeles. UCLA; 2002. [Google Scholar]
- 44. Short JC, Palmer TB, Ketchen DJ., Jr. Resource-based and strategic group influences on hospital performance. Health Care Manage Rev. 2002;27(4):7-17. [DOI] [PubMed] [Google Scholar]
- 45. Barney J. Firm resources and sustained competitive advantage. J Manag. 1991;17(1):99-120. [Google Scholar]
- 46. Daft R. Organization theory and design. New York, NY: West; 1983. [Google Scholar]
- 47. Rahman M, Foster AD, Grabowski DC, Zinn JS, Mor V. Effect of hospital–SNF referral linkages on rehospitalization. Health Serv Res. 2013;48(l Pt 1):1898-1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Shaughnessy P, Schlenker R, Brown K, Yslas I. Case mix and surrogate indicators of quality of care over time in freestanding and hospital-based nursing homes in Colorado. Public Health Rep. 1983;98(5):486-492. [PMC free article] [PubMed] [Google Scholar]
- 49. Bailis S, Shannon J. Subacute’s place in the capitated scene. Provider. 1995;21(11):29-30. [PubMed] [Google Scholar]
- 50. Tuch H, Hiep P, Robinson BE. Postacute care in the 1990s. J Fla Med Assoc. 1994;81:631-634. [PubMed] [Google Scholar]
- 51. American Hospital Association. AHA Annual Survey Database Fiscal Year 2010. http://www.ahadata.com/academics-researchers/. Published 2018. Accessed December 6, 2018.
- 52. HRSA, US Department of Health and Human Services: Health Resources and Services Administration. National County-Level Health Resource Information Database: Overview. https://data.hrsa.gov/topics/health-workforce/ahrf. Published 2011. Accessed December 6, 2018.
- 53. Centers for Medicare & Medicaid Services. Research Data and Systems. https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Cost-Reports/. Published 2014. Accessed November 28. 2018.
- 54. Medicare.gov Hospital Compare. 30-day unplanned readmission and death measures. https://www.medicare.gov/hospitalcompare/Data/30-day-measures.html. Published 2012. Accessed December 6, 2018.
- 55. Experton B, Ozminkowski RJ, Pearlman DN, Li Z, Thompson S. How does managed care manage the frail elderly? The case of hospital readmissions in fee-for-service versus HMO systems. Am J Prev Med. 1999;16(3):163-172. [DOI] [PubMed] [Google Scholar]
- 56. Heggestad T. Do hospital length of stay and staffing ratio affect elderly patients’ risk of readmission? A nation-wide study of Norwegian hospitals. Health Serv Res. 2002;37(3):647-665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes. 2011;4(1):53-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Rich MW, Freeland KE. Effect of DRGs on three-month readmission rate of geriatric patients with congestive heart failure. Am J Public Health. 1988;78:680-682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Aiken LH, Clarke SP, Sloane DM. Hospital staffing, organization, and quality of care: Cross-national findings. Nurs Outlook. 2002;50(5):187-194. [DOI] [PubMed] [Google Scholar]
- 61. Propper C, Burgess S, Green K. Does competition between hospitals improve the quality of care? Hospital death rates and the NHS internal market. J Publ Econ. 2004;88(7):1247-1272. [Google Scholar]
- 62. Shah A, Fennell M, Mor V. Hospital diversification into long-term care. Health Care Manage Rev. 2001;26(3):86-100. [DOI] [PubMed] [Google Scholar]
- 63. Cutler DM, Morton FS. Hospitals, market share, and consolidation. JAMA. 2013;310(18):1964-1970. [DOI] [PubMed] [Google Scholar]
- 64. McHugh MD, Berez J, Small DS. Hospitals with higher nurse staffing had lower odds of readmissions penalties than hospitals with lower staffing. Health Aff. 2013;32(10):1740-1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. McHugh MD, Ma C. Hospital nursing and 30-day readmissions among Medicare patients with heart failure, acute myocardial infarction, and pneumonia. Med Care. 2013;51(1):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Erdem E, Fout BT, Korda H, Abolude AO. Hospital readmission rates in Medicare. J Hosp Admin. 2014;3(4):109-118. [Google Scholar]
- 67. Chou SY, Deily ME, Li S, Lu Y. Competition and the impact of online hospital report cards. J Health Econ. 2014;34:42-58. [DOI] [PubMed] [Google Scholar]
- 68. Axon RN, Williams MV. Hospital readmission as an accountability measure. JAMA. 2011;305(5):504-505. [DOI] [PubMed] [Google Scholar]
- 69. Centers for Medicare & Medicaid Services. Readmissions Reduction Program. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Published 2014. Accessed November 28, 2018.
- 70. Maly MB, Lawrence S, Jordan MK, et al. Prioritizing partners across the continuum. J Am Med Dir Assoc. 2012;13(9):811-816. [DOI] [PubMed] [Google Scholar]