Abstract
Significant evidence demonstrates the powerful effects social determinants have on health-related perceptions, behaviors, and health outcomes. However, these factors are often studied out of context, despite the acknowledgement that social determinants of health are place based. This research aimed to demonstrate that health-related perceptions are dependent on where one lives. Via a community-based participatory study, participants were randomly selected from 3 residential regions varying distances from a freight railyard (nearest n = 300, middle n = 338, farthest n = 327), all mostly low-income, predominately Latino areas. Interview-administered surveys with adults were collected by bilingual trained community members (87% response) in English/Spanish. Adjusted-logistic regression models assessed residential region as a predictor of stressors (perceptions of community safety, community noise disturbance, health care access, food insecurity) and buffers (3 neighborhood cohesion variables), after adjusting for household income, race/ethnicity, gender, and age. Each region experienced a unique amalgam of stressors and buffers. In general, the region closest to the railyard experienced more stressors (odds ratio [OR] = 1.58; 95% CI 1.12-2.20) and less buffers (OR = 0.69; 95% CI 0.49-0.96) than the region furthest from the railyard. More than half of participants in each region reported 2 or more stressors and 2 or more buffers. In this seemingly homogenous study population, place remained important in spite of traditionally used socioeconomic factors, such as household income and race/ethnicity. Social determinants of health should be studied with regard to their environmental context, which will require interdisciplinary collaboration to improve multilevel research methods. Including the study of social buffers will also promote sustainable, positive change to reduce health disparities.
Keywords: social determinants, environmental determinants, interdisciplinary, stressors, buffers, perceptions, health determinant disparities
Introduction
Social, economic, and the physical environments account for 50% of the factors attributable to health status and life expectancy in the United States.1 Consequently, disparities among social-, economic-, and physical-environmental health determinants largely contribute to the health disparities that persist today.2,3
Studying the health effects from such social factors has been difficult because these “upstream” factors are often contingent on other factors. For example, health literacy may be based on educational attainment of the individual, but educational attainment is often related to parental socioeconomic status (SES).3 Increasingly, researchers argue that economic factors, psychosocial stressors or health buffers are too often studied out of context, when in reality they are place based or affected by the physical environment.4 Therefore, social determinants of health research in the United States has been shifting to include place-based concepts, such as studying where people were born, grew up or live to better understand factors affecting health outcomes.5
Despite the recognition that social determinants are place based, this concept of including a measure of geography within health-predictive models remains underutilized. When geography is considered, it is often in the form of clustering and comparing larger regions, such as by county or zip code. In studies such as these, researchers may or may not have6 been able to adjust for place/geography in their health-predictive models. In addition, clustering place by zip code has limitations such as boundary lines changing over time and the imposed concept of land-use continuity (some zip codes may be more representative of uninhabited land or of business-sectors than of residences).7 In the present study, we used a different clustering of place by sampling residential household addresses within a relatively small area, in an urban, predominantly low-income region encompassing a 6-mile radius around a point-source environmental hazard.
The aim of this research was to explore if, even within relatively homogenous SES regions, living next to a known pollution source is associated with additional social-environmental stressors and buffers known to affect health.
Methods
Study Population
San Bernardino County, in the inland region of Southern California, is a region of vulnerable populations in the context of both social and environmental determinants, largely because of its lower cost of living compared with nearby Los Angeles. Not only is San Bernardino County one of the most underfunded regions in the state, but residents continuously exhibit higher chronic disease morbidity than California state counterparts.8 In addition to its geography-related routine poor air quality, the metropolitan area of San Bernardino9 is home to an inland goods movement network, the San Bernardino Railyard (SBR), with diesel-powered locomotives and trucks operating 24/7.10,11 San Bernardino is also known for its high number of violent crime offences,12 large number of gang members,13 evidence of historic neighborhood segregation,13 and in 2012 for its economic downturn as the United States’ second bankrupt city.14
Based in the San Bernardino metropolitan area, we conducted the Environmental Railyard Research Impacting Community Health (ENRRICH) Project, a mixed-methods, community-based participatory research study, to characterize the community health burden of disease in 2011-2012.15 The study included a community engagement qualitative research project,16 followed by a quantitative research study which included administration of interview-administered household surveys of adult participants.
Study participants were sampled from 1 of 3 defined regions (A, B, and C). The location and spatial configuration of the sampling regions are depicted and are described in more detail elsewhere.13,17 In short, the 3 regions were designed to model decreasing levels of air pollution exposure in relation to the railyard from highest (A) to lowest (C). Region A was defined by delineating a 350-m buffer around the perimeter of the railyard facility; then every house within region A was considered for sampling. Within sampling regions B and C, ENRRICH investigators used digital street and cadastral maps of the target neighborhoods and selected households for interviews using a GIS (geographic information system)-based random number generator tool.
There were 965 participants who participated in the study (300 in region A, 338 in region B, 327 in region C). The response rate was 87%. This research study was approved by Loma Linda University Institutional Review Board. All participants provided informed written consent prior to participation in the study.
Place (Residential Region)
Community and neighborhood are some of the commonly used terms to describe place. The term “community” is broadly defined as where individuals and/or families socialize or form a shared connection with others, which can exist beyond a geographic region. The term neighborhood refers to a relatively small, non-specific in size, area where people live.18 Often, place has been clustered and compared by state, county, zip code, or as small as census-blocks. Here we grouped place by residential (household) regions at three distances away from an environmental hazard, a freight railyard. While this was originally to be in line with the primary purpose of the ENRRICH study, to study the health effects associated with proximity to the railyard, we have chosen to maintain these groupings here as it represents a common, point-source neighborhood “problem.” This also combines the definitions of community and neighborhood by centering community around an environmental hazard and maintaining household residence as “place.” Households in residential regions A, B, and C were an average of 0.18 miles (283 m), 1.9 miles (3057 m), and 4.6 miles (7320 m) away from the railyard, respectively.
To best describe the economic differences between the residential regions, we obtained household income measures at the census-block group level from the 2011 U.S. Census Bureau. We individually assigned Census variables to each participant by geocoding latitude and longitude coordinates for each household in arcGIS for desktop version 10.5.
Survey
A bilingual—English and Spanish—interview instrument was developed17 to gather information in a culturally competent and linguistically appropriate manner, and was based on qualitative research of relevant questions from the affected population, as well as from existing literature.16 Survey administration, in a personal interview format, was delivered by trained bilingual community health workers from the study’s local community partner, a nonprofit environmental justice organization.15
Stressors
Individual-level perceived stressors were defined as well-researched health predictors that could have a biological effect on health through the chronic (toxic) stress (ie, inflammatory) pathway. Four categories of stressors18 (social, physical, health care services, and economic) were a priori chosen based on availability within the data set and relative importance to the study population.
Community Safety
Participants were asked to agree along a 5-point scale to the following statements: “I feel safe walking in my community, day or night” and “Violence or crime is not a problem in my community.” For ease of interpretation, responses to each question were dichotomized by collapsing strongly disagree and disagree and collapsing neutral, agree, strongly agree.
Noise
Similarly, participants were asked to agree along a 5-point scale to the following statement: “The noise from my community keeps me awake or wakes me up in the middle of the night.” Responses were dichotomized by collapsing strongly agree and agree and collapsing neutral, disagree, strongly disagree.
Health Care Services
Two questions were chosen to best represent current access to healthcare services. “Within the past 12 months were there medical services you needed but could not get?” and “Within the past 12 months were there prescription medications you needed but could not get?” Responses were yes or no.
Food Insecurity
Two food insecurity questions were asked on the ENRRICH survey: “The food that we bought just didn’t last and we didn’t have money to get more” and “My family couldn’t afford to eat balanced meals.” Participants were asked to answer if the statement was “often true, sometimes true, or never true” for their household based on the past 12 months.
Social Buffers
Individual-level perceived buffer questions were created based on a bottom-up approach.16 They were: “Participants in my community generally get along with each other,” “People in my community can be trusted,” and “I often see children playing outside in the community.” Participants were asked to agree along a 5-point scale. Responses were dichotomized by collapsing strongly agree and agree and collapsing neutral, disagree, strongly disagree.
Statistical Analysis
Imputation of missing values was conducted for a small number of missing data using multiple-imputation with chained equations: RStudio 1.1.423, the mice package. For descriptive statistics, we computed frequencies for categorical variables, mean and standard deviation for age, and median and quartiles for Census income variables. To test differences between regional groupings, we computed chi-square tests for categorical variables, an F test for age, and Kruskal-Wallis test for Census income variables.
To test for an association between the social-environmental factors and residential region we computed adjusted logistic and ordinal logistic (for food insecurity outcomes) regression models. Ordinal logistic models met the proportional odds assumption. Covariates (household income, race/ethnicity, gender, and age) were a priori selected. The number of confounding covariates was intentionally kept minimal for the purpose of simplicity—to represent the most often used covariates in health-predictive statistical models. Household income and race/ethnicity were chosen to represent SES variables. Asian and “other” race categories were collapsed with white due to small counts Education was not included as a confounder because it was highly associated with both income and race/ethnicity (P < .0001) and did not vary by residential region (P = .427). Analyses were performed using RStudio 1.1.423 (mice and devtools packages) and SAS 9.4.
Results
Study Population Characteristics
Overall, the ENRRICH study population was relatively young (mean age of 44 years, standard deviation 14 years) and predominantly female (67%), Hispanic (76%), married (57%), and had never smoked (69%). It was, overall, a low-SES population of which subjects were mainly high school educated or less (63%), unemployed (47%), had low health insurance coverage (43%), and an annual average household income of less than $50 000 (93%) with 3 or more people living in the household (85%). Calculated from Census data, the median household income of the study population was $40 843 and the median per capita income was $14 098. Most (94%) had lived at the sampled residence for more than 1 year. Region A was the lowest income region followed by regions B and C (Table 1).
Table 1.
Individual-Level and Household Characteristics of ENRRICH Study Population by Place (Residential Region).a
| Characteristics | Total (n = 965) | Residential Region | |||
|---|---|---|---|---|---|
| A (n = 300) | B (n = 338) | C (n = 327) | P b | ||
| Individual-level characteristics | |||||
| Age (years) | 44.4 (14.6) | 44.8 (15.7) | 43.7 (14.0) | 44.7 (14.1) | .538 |
| Gender | |||||
| Female | 646 (66.9) | 185 (61.7) | 240 (71.0) | 221 (67.6) | .042 |
| Male | 319 (33.1) | 115 (38.3) | 98 (29.0) | 106 (32.4) | |
| Race/Ethnicity | |||||
| Hispanic, Latino | 731 (75.8) | 259 (86.3) | 242 (71.6) | 230 (70.3) | <.001 |
| African American, Black | 113 (11.7) | 21 (7.0) | 54 (16.0) | 38 (11.6) | |
| White/Asian/Other | 121 (12.5) | 20 (6.7) | 42 (12.4) | 59 (18.0) | |
| Per capita income (USD) | 14 098 (12 504, 17 421) | 12 504 (9959, 14 098) | 14 757 (13 304, 20 266) | 15 701 (13 144, 17 762) | <.0001 |
| Educational achievement | |||||
| Grade school or less | 271 (28.1) | 79 (26.3) | 105 (31.1) | 87 (26.6) | .427 |
| High school | 332 (34.4) | 116 (38.7) | 108 (32.0) | 108 (33.0) | |
| Some college, vocational, business, or trade | 278 (28.8) | 81 (27.0) | 93 (27.5) | 104 (31.8) | |
| ≥Associates degree | 84 (8.7) | 24 (8.0) | 32 (9.5) | 28 (8.6) | |
| Current employment status | |||||
| Unemployed | 456 (47.3) | 146 (48.7) | 158 (46.7) | 152 (46.5) | .838 |
| Employed/retired/student | 509 (52.7) | 154 (51.3) | 180 (53.3) | 175 (53.5) | |
| Marital status | |||||
| Never married/widowed/divorced | 420 (43.5) | 134 (44.7) | 152 (45.0) | 134 (41.0) | .520 |
| Married/live together | 545 (56.5) | 166 (55.3) | 186 (55.0) | 193 (59.0) | |
| Self-reported general health | |||||
| Excellent/Good | 527 (54.6) | 145 (48.3) | 199 (58.9) | 183 (66.0) | .024 |
| Fair/Poor | 438 (45.4) | 155 (51.7) | 139 (41.1) | 144 (44.0) | |
| Behavior | |||||
| Ever regularly smoked cigarettes, cigars, or a pipe | |||||
| Current smoker | 194 (20.1) | 55 (18.3) | 77 (22.8) | 62 (19.0) | .390 |
| Past smoker | 106 (11.0) | 33 (11.0) | 31 (9.2) | 42 (12.8) | |
| Never smoker | 665 (68.9) | 212 (70.7) | 230 (68.0) | 223 (68.2) | |
| Household-level characteristics | |||||
| Health care insurance type | |||||
| None | 414 (42.9) | 149 (49.7) | 138 (40.8) | 127 (38.8) | .005 |
| Private, HMO/Military/Other | 225 (23.3) | 52 (17.3) | 78 (23.1) | 95 (29.1) | |
| Medicare, Medicaid, Medical | 326 (33.8) | 99 (33.0) | 122 (36.1) | 105 (32.1) | |
| Average annual household income (USD) | |||||
| <10 000 | 331 (34.3) | 123 (41.0) | 110 (32.5) | 98 (30.0) | <.001 |
| 11 000-19 000 | 230 (23.8) | 89 (29.7) | 70 (20.7) | 71 (21.7) | |
| 20 000-29 000 | 180 (18.7) | 45 (15.0) | 62 (18.3) | 73 (22.3) | |
| 30 000-49 000 | 161 (16.7) | 30 (0.0) | 72 (21.3) | 59 (18.0) | |
| ≥50 000 | 63 (6.5) | 13 (4.3) | 24 (7.1) | 26 (8.0) | |
| Median household income (USD) | 40 843 (29 235, 54 127) | 31 427 (27 063, 40 843) | 43 631 (31 943, 51 802) | 51 911 (37 064, 62 517) | <.0001 |
| Number of household members | |||||
| 1-2 persons | 141 (14.6) | 49 (16.3) | 40 (11.8) | 52 (15.9) | .364 |
| 3-5 persons | 523 (54.2) | 164 (54.7) | 191 (56.5) | 168 (51.4) | |
| ≥6 persons | 301 (31.2) | 87 (29.0) | 107 (31.7) | 107 (32.7) | |
| Duration at current residence (years) | |||||
| 11+ | 263 (27.3) | 108 (36.0) | 60 (17.8) | 95 (29.1) | <.001 |
| 1-10 | 641 (66.4) | 173 (57.7) | 244 (72.2) | 224 (68.5) | |
| <1 | 61 (6.3) | 19 (6.3) | 34 (10.1) | 8 (2.4) | |
Data shown represents n (%) for categorical variables, mean (standard deviation) for age, and median (1st, 3rd quartile) for per capita income and median house income. Slash (/) denotes collapsed nominal categories. A = closest to San Bernardino Railyard; B = intermediate; C = farthest distance.
P values computed from chi-square statistic for categorical variables, F test for age, and Kruskal-Wallis test for per capita income and median house income.
The self-reported general health of the population was quite low—45% reported their general health to be fair or poor and varied by residential region; a higher proportion of participants living in region A reported fair/poor health (52%) compared with B (41%) and C (44%) (Table 1).
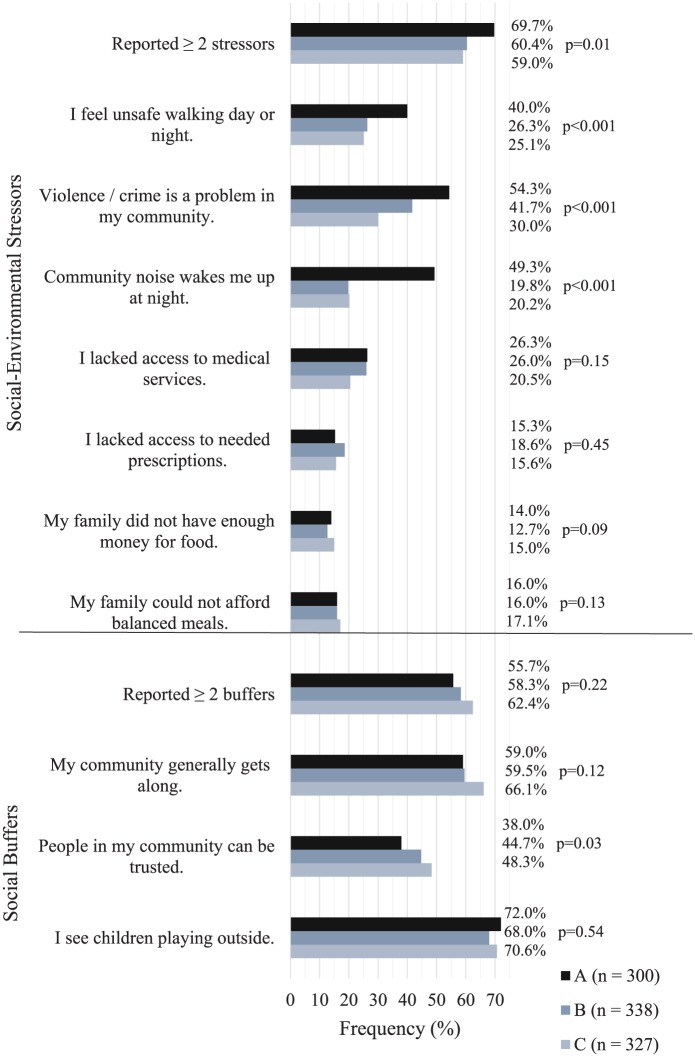
Social-Environmental Stressors
Both stressors and buffers were highly prevalent. Four out of 5 (84.5%) ENRRICH study participants reported at least 1 stressor and two-thirds (66.6%) reported 2 or more stressors. The most prevalent stressor in the study population was perceiving violence or crime to be a problem in their community (42.4%) followed by feeling unsafe walking in their community (30.4%). The least prevalent was experiencing food insecurity often over the previous 12 months (Figure 1). However, about half of the study population reported food insecurity to be often or sometimes true (50.9% did not have enough money to buy food; 46.2% could not afford to eat balanced meals).
Figure 1.
Prevalence of stressors and buffers in the ENRRICH study population by place (residential region).
Food insecurity questions prompted 3 responses and the response “often true” is presented here. All other stressors and buffers presented here were dichotomous.
Multivariate results showed that residential region was associated with community safety, noise, and food insecurity stressors surveyed in the ENRRICH study population independent of household income, race/ethnicity, gender, or age (Figure 2; Table 2). Specifically, adults living in region A, the lowest SES region, had twice the odds of reporting feeling unsafe walking in their community compared to regions B and C, 3 times the odds of perceiving violence or crime to be a problem in their community compared to region C, and 4 times the odds to be kept awake at night due to community noise compared with regions B and C. Also, participants in regions A and B were less likely to report that their family did not have enough money for food compared to region C. Overall, participants of region A had twice the odds of reporting 2 or more stressors compared with region C (Table 2). Age was not associated with any stressor.
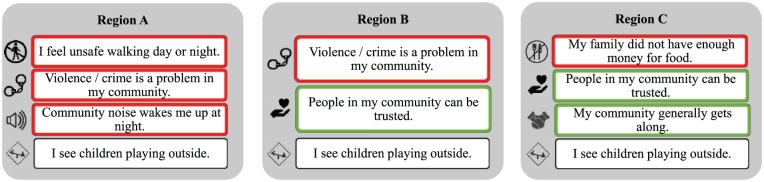
Figure 2.
Summary of stressors and buffers by place in the ENRRICH study population.
Social-environmental stressors (red) and social buffers (green), details in Tables 2 and 3, that were significantly different by residential region, after adjustment for income, race/ethnicity, gender and age. In each region, the social buffer of seeing children playing outside was extremely prevalent but did not significantly (P < .05) differ by region.
Table 2.
The Relationship Between Social-Environmental Stressor Outcomes and Placea (Residential Region) in the ENRRICH Study Population.
| Odds Ratio (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|
| I feel unsafe walking day or night | Violence /crime is a problem in my community | Community noise wakes me at night | I lacked access to medical services | I lacked access to needed prescriptions | My family did not have enough money for food | My family could not afford balanced meals | Two or more stressors reported | |
| Region A | 2.14 (1.49, 3.07) | 2.98 (2.11, 4.22) | 3.91 (2.69, 5.68) | 1.28 (0.86, 1.91) | 0.92 (0.58, 1.45) | 0.63 (0.46, 0.87) | 0.75 (0.54, 1.00) | 1.58 (1.12, 2.20) |
| Region B | 1.17 (0.82, 1.68) | 1.74 (1.25, 2.42) | 0.96 (0.65, 1.42) | 1.32 (0.91, 1.93) | 1.23 (0.81, 1.87) | 0.75 (0.56, 1.02) | 0.82 (0.61, 1.10) | 1.06 (0.77, 1.50) |
| Region C | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Region A vs B | 1.83 (1.29, 2.59) | 1.71 (1.23, 2.40) | 4.07 (2.81, 5.89) | 0.97 (0.67, 1.40) | 0.74 (0.48, 1.16) | 0.83 (0.60, 1.20) | 0.91 (0.65, 1.30) | 0.80 (0.39, 1.60) |
| <$10 000 | 3.49 (1.50, 8.12) | 1.33 (0.74, 2.38) | 1.33 (0.67, 2.64) | 4.66 (1.60, 13.56) | 1.93 (0.78, 4.77) | 2.93 (1.63, 5.26) | 3.05 (1.64, 5.70) | 2.69 (1.49, 4.90) |
| $11 000-$19 000 | 3.05 (1.30, 7.16) | 1.10 (0.60, 2.01) | 0.72 (0.35, 1.47) | 5.30 (1.81, 15.48) | 2.06 (0.82, 5.17) | 2.24 (1.22, 4.13) | 2.39 (1.24, 4.60) | 1.73 (0.94, 3.20) |
| $20 000-$29 000 | 2.97 (1.23, 7.17) | 0.96 (0.51, 1.80) | 0.86 (0.42, 1.76) | 4.43 (1.52, 12.96) | 1.19 (0.46, 3.13) | 2.29 (1.23, 4.26) | 2.57 (1.33, 5.00) | 1.81 (0.96, 3.40) |
| $30 000-$49 000 | 2.58 (1.05, 6.30) | 0.87 (0.46, 1.64) | 0.81 (0.39, 1.71) | 2.95 (0.99, 8.81) | 1.17 (0.44, 3.09) | 1.36 (0.73, 2.54) | 1.86 (0.95, 3.60) | 1.18 (0.63, 2.20) |
| ≥$50 000 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Black | 0.68 (0.41, 1.14) | 1.35 (0.87, 2.12) | 1.29 (0.78, 2.13) | 1.44 (0.90, 2.31) | 1.18 (0.68, 2.05) | 2.35 (1.58, 3.49) | 3.03 (2.02, 4.60) | 1.44 (0.91, 2.30) |
| White/other | 1.59 (1.01, 2.50) | 1.91 (1.25, 2.92) | 1.16 (0.71, 1.88) | 0.88 (0.52, 1.48) | 0.90 (0.51, 1.59) | 0.91 (0.60, 1.38) | 1.67 (1.10, 2.50) | 1.31 (0.85, 2.00) |
| Hispanic | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
Logistic regression models: Stressor = region + average annual household income + race/ethnicity + gender + age; all variables except for region were self-reported. A = closest to San Bernardino Railyard, B = intermediate, C = farthest distance.
Values which are statistically significant at P < 0.05 are boldfaced.
Values which are statistically significant at P < 0.1 are bold-italicized.
Social Buffers
In the ENRRICH study population, witnessing children playing outside was the most reported buffer (70.8%), followed by perceiving their community members to get along with each other (61.4%) and trust of community members (42.4%). Approximately 58% of participants reported 2 or more buffers (Figure 1).
In the multivariable models, those living in the highest SES region (region C) had higher odds to perceive that people generally got along with each other in their community compared with regions A and B, respectively. Participants living in regions B and C had 1.52 and 1.72, respectively, times the odds to perceive that people can be trusted in their community compared to those living in region A. Those living in region A had 1.37 times the odds to report seeing children playing outside in their community compared to those in region B (Table 3). Increasing age had a mild/moderate positive association with experiencing a social buffer for each of the 3 buffers analyzed.
Table 3.
The Relationship Between Social Buffer Outcomes and Placea (Residential Region) in the ENRRICH Study Population.
| Odds Ratio (95% CI) | ||||
|---|---|---|---|---|
| My community generally gets along | People in my community can be trusted | I see children playing outside | Two or more buffers reported | |
| Region A | 0.68 (0.48, 0.96) | 0.58 (0.41, 0.82) | 1.16 (0.81, 1.7) | 0.69 (0.49, 0.96) |
| Region B | 0.72 (0.52, 1.00) | 0.88 (0.64, 1.21) | 0.85 (0.61, 1.2) | 0.82 (0.60, 1.13) |
| Region C | 1.00 | 1.00 | 1.00 | 1.00 |
| Region A vs B | 0.94 (0.68, 1.31) | 0.66 (0.47, 0.93) | 1.37 (0.96, 2.0) | 0.84 (0.60, 1.16) |
| <$10 000 | 0.90 (0.47, 1.74) | 0.46 (0.25, 0.84) | 0.64 (0.33, 1.2) | 0.87 (0.47, 1.62) |
| $11 000-$19 000 | 0.79 (0.41, 1.52) | 0.46 (0.24, 0.86) | 0.69 (0.35, 1.4) | 0.71 (0.38, 1.33) |
| $20 000-$29 000 | 0.95 (0.49, 1.84) | 0.53 (0.28, 1.03) | 0.93 (0.44, 2.0) | 0.86 (0.45, 1.65) |
| $30 000-$49 000 | 0.99 (0.49, 1.98) | 0.59 (0.30, 1.14) | 1.03 (0.50, 2.1) | 1.07 (0.55, 2.07) |
| ≥$50 000 | 1.00 | 1.00 | 1.00 | 1.00 |
| Black | 0.87 (0.56, 1.35) | 0.36 (0.22, 0.58) | 1.55 (0.93, 2.6) | 0.77 (0.50, 1.18) |
| White/other | 0.51 (0.34, 0.78) | 0.44 (0.28, 0.68) | 0.90 (0.58, 1.4) | 0.50 (0.33, 0.75) |
| Hispanic | 1.00 | 1.00 | 1.00 | 1.00 |
Logistic regression models: Buffer = region + average annual household income + race/ethnicity + gender + age; all variables except for region were self-reported. A = closest to San Bernardino Railyard, B = intermediate, C = farthest distance.
Values which are statistically significant at P < 0.05 are boldfaced.
Values which are statistically significant at P < 0.1 are bold-italicized.
Discussion
The ENRRICH Study participants were overall a low SES adult population; representative of the region from which it was drawn.19 In this research, we explored how 3 residential regions surrounding a point-source environmental hazard at increasing distances away from the railyard would differ in its social-ecological presentations. In general, region A experienced more stressors than buffers and region C experienced more buffers than stressors compared with the other regions. However, each region experienced a unique amalgam of stressors and buffers (Figure 2). Understanding how social-environmental stressors are affected by a person’s residential context is critical. Indeed, it has been previously shown that neighborhood physical characteristics,20 neighborhood social structural characteristics,21 and neighborhood perceptions affect chronic health outcomes,22 potentially through a chronic (also referred to as toxic) stress (ie, inflammatory process) pathway.23
There is much heterogeneity in the health factors in populations that were otherwise thought to be quite homogenous, that is, in income and race/ethnic composition. This study’s results go a step beyond, “Your zip code is a better predictor of your health than your genetic code.”24 We were able to show that, even in a small geographic area with populations that differed only slightly by SES makeup, differences existed among the common types of social-environmental determinants reported. It has been suggested that multiple levels of social determinant measurement should be considered.25 Unfortunately, many studies continue to focus solely on income and race/ethnicity as factors that influence health disparities.
Our finding that residents of region A, the region nearest to the freight railyard, were more likely to report sleep disturbance due to community noise more than the other 2 regions was the least surprising as this stressor was based on the physical environment. Many social-environmental studies continue to focus on income as a primary social determinant26,27; and while income remained as a significant predictor for many stressors in this study, it was not, however, a predictor for perceiving violence/crime or noise to be a problem in one’s community. This is important to note because income alone may not account for a variety of stressors a person perceives, and we have previously found that a lack of perceived community safety, and not low-income, was associated with adverse health outcomes, findings which are further supported by others.28
It was unexpected to find that residents of region C, the highest income region, were more likely to report food insecurity compared with residents in regions A and B. A possible reason for this finding may be that residents in regions A and B had access to welfare services helping them to afford enough food, whereas residents in region C may have been a part of the working poor, who do not have such supports. A limitation on our survey tool was that we did not specifically ask for information on welfare services received as this is an extremely politically laden issue in high immigrant, Spanish-speaking populations. Another reason could be a true difference in perception—that residents of region C perceived to not have enough money for food or for balanced meals, possibly due to family size, knowledge/past experience, or income needed elsewhere such as for cost of housing; while those at lower income had managed to make do with what they had, therefore not perceiving it to be as much of a challenge.
Residents of region A reported lesser social buffers than residents of region C. Neighborhood trust is a crucial component of neighborhood social cohesion and is influenced by poverty density and racial composition29 as we have also found here. Furthermore, lack of social cohesion is associated with poor health.30 Residents of region A reported to see children playing outside more than residents of region B. This is likely due to a large park made up of soccer fields that are frequently occupied by men or children playing soccer games and entire families attending the games. The presence of a (somewhat) maintained community green space may serve as this community’s social cohesion buffer.
Our most relevant finding is that each region had a unique set of experiences made up of different stressors and social buffers. This has implications for future research and interventions because there are various ways communities may experience and express social cohesion. This makes social cohesion difficult to measure without utilizing a bottom-up research approach.31
Determining the frequency and distribution of social-environmental determinants is the first step toward studying their more complex nature within the casual web of health outcomes.32 Our work uniquely points to the fact that social-environmental experiences vary, even within geographically tight spaces among populations of seemingly similar SES. Moreover, those living most closely to a point-source of pollution are clearly different from apparently similar groups who live further away. As part of the hypothesized causal web, social-environmental stressors and social buffers may also be moderated by one another, which may in turn increase or weaken the impact each determinant has on health.33 For instance, low social cohesion communities are often associated with more crime/violence.29,34
Limitations and Strengths
Like many other environmental studies, our research had some limitations. The ENRRICH study was cross-sectional and temporality between place of residence and stressors/buffers cannot be determined; although, the majority (93%) of residents had lived at their current location for more than a year. It is possible that we oversampled women; nevertheless, some households were interviewed during early evening hours and weekends as interviews could not be conducted after dark because of safety concerns.
Despite our limitations, our study has notable strengths. It is an advantage to be able to assess perceptions measured at an individual-level rather than solely relying on census block-level or administrative data.35 In addition, sampled households were randomly selected. Data were collected by trained bilingual community members using a community-based participatory research approach,15 which contributed to a high response rate (87%), a notable strength, in a majorly Latino, low-income target population, where immigration challenges are common.
Furthermore, the consideration of the community member’s concerns as a guide for the survey tool used, by use of the ENRRICH project’s mixed-methods design, lends itself to 2 strengths. First, we analyzed identified salient social stressors and buffers for this community, which reduced confounding by other hypothesized, less-salient perceptions.35 Second, because the experience and “voices” of community members are crucial for successful place-based interventions,18 this study will be more easily translatable to public health practice in populations that are also socially and economically vulnerable.
Recommendations
Within a relatively small geographic region and among a population that seemed relatively socially and economically homogenous, we found differences in the social-environmental stressors and social buffers experienced by adult community members who lived in different residential neighborhoods. Perceptions of the social-environmental context are place-based and methodologies and interpretations to study multiple determinants of health and spatial dependence in health models should continue to be refined. Nonetheless, in order to contribute to the big picture understanding, it is currently useful to use well-established methodologies to show prevalence, geographic distributions, and associations between various known determinants of health, as we have shown here. Clearly, there is an intersection of the social, economic, and physical environmental context of where people live. The contribution of multiple determinants of health requires thought of the interconnectedness of these determinants.
Public health interventions may prove cost-efficient and effective by capitalizing on the promotion of social cohesion as a preventive health determinant.36 This would require a multistakeholder approach in which both community members and community leaders do their part. For example, while city officials focus on improving safety and reducing crime, community members themselves could be encouraged to create community events that foster social cohesion. The community members themselves will choose the best approach for their community, such as church potluck events to get to know and appreciate one another, a neighborhood watch program to foster trust, or creating safe times for children to play together at a local park.
Conclusions
In conclusion, when studying social determinants of health, the environmental context is a critical consideration. Place as a measure is important over and above the most commonly used SES factors, namely household income and race/ethnicity. Contextualizing social determinants of health will require interdisciplinary collaboration to translate multilevel research into effective and efficient community-based solutions to reduce health disparities.
Acknowledgments
We also acknowledge the contribution of the study participants, the hard work from the trained community health workers, and Jan Irene Lloren and Andrew Mashchak for their statistical assistance with RStudio.
Author Biographies
Kristen N. Arthur, PhD, MPH, is a recent epidemiology graduate from Loma Linda University School of Public Health. Her research interest is the social-cultural contexts of medicine and health in health disparity settings. Some of her previously published work includes complementary and alternative medicine use, and she’s worked in public health practice for local (minority, recidivism, cancer) and international (rural, HIV/TB, adolescent) vulnerable population groups.
Synnøve F. Knutsen, MD, PhD, MPH, was the program director of the PhD in Epidemiology program at Loma Linda University School of Public Health, has served on numerous dissertations committees, and is co-investigator for the Adventist Health Study-2. Her research focuses on lifestyle, air pollution and chronic disease.
Rhonda Spencer-Hwang, DrPH, MPH, an associate professor in the School of Public in the Center for Community Resilience at Loma Linda University, is an environmental epidemiologist whose research identifies adverse health outcomes associated with environmental exposures to support vulnerable populations. She has appeared in multiple international documentaries discussing her findings, given presentations around the world and was the recipient of millions in funding from various government agencies (i.e. AQMD, First 5 Riverside Commission) to promote resiliency and a culture of health.
David Shavlik, PhD, MSPH, is the program director for a master’s graduate program in epidemiology at the School of Public Health, Loma Linda University. He works on projects that range from environmental to nutritional epidemiology.
Susanne Montgomery, MS, MPH, PhD, the associate dean for Research in the School of Behavioral Health, Loma Linda University, is a social/behavioral epidemiologist who is committed to conducting translational health disparities research. She has received funding from NIH, CDC, State and private funders using mainly mixed method and community-based participatory approaches like the one this paper features. Her research topics range from environmental research in local communities, breast and prostate cancer in African Americans, to diabetes and weight control in Latinos and cultural issues, most involving structural access issues for the underserved.
Footnotes
Authors’ Note: In memoriam: Dr Samuel Soret (1962-2016). Samuel Soret, PhD, MPH, Associate Dean for Research and Executive Director of the Center for Community Resilience at Loma Linda University School of Public Health and a Co-Principal Investigator on this research passed away on August 23, 2016 from a heart attack while on a trip in his home-country of Spain. Dr Soret faithfully served the School of Public Health for 21 years and lived his motto: “Compassion must fuel everything we do.”
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: The research study was approved by Loma Linda University Institutional Review Board (IRB #5110054). All participants provided informed written consent prior to participation in the study.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the South Coast Air Quality Management District/BP West Coast Products Oversight Committee, LLC, Grant #659005 and also supported by National Institutes of Health #1P20MD006988.
ORCID iD: Kristen N. Arthur  https://orcid.org/0000-0001-9161-8452
https://orcid.org/0000-0001-9161-8452
References
- 1. National Association of Community Health Centers. Powering Healthier Communities: Community Health Centers Address the Social Determinants of Health. https://stepup.ucsf.edu/sites/stepup.ucsf.edu/files/CHCs%20and%20the%20Social%20Determinants%20of%20Health_1.pdf. Accessed February 19, 2019.
- 2. Centers for Disease Control and Prevention. CDC Health Disparities and Inequalities Report—United States, 2013. Atlanta, GA: US Department of Health and Human Services; 2013. [Google Scholar]
- 3. Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(suppl 2):19-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Diez Roux AV. Neighborhoods and health: what do we know? what should we do? Am J Public Health. 2016;106:430-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123(suppl 3):S174-S184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Samuelson MB, Chandra RK, Turner JH, Russell PT, Francis DO. The relationship between social determinants of health and utilization of tertiary rhinology care. Am J Rhinol Allergy. 2017;31:376-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grubesic TH, Matisziw TC. On the use of ZIP codes and ZIP code tabulation areas (ZCTAs) for the spatial analysis of epidemiological data. Int J Health Geogr. 2006;5:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. California Asthma Quality Improvement Initiative. San Bernardino County asthma profile. https://www.cdph.ca.gov/Programs/CCDPHP/DEODC/EHIB/CPE/CDPH%20Document%20Library/County%20profiles/San%20Bernardino%202016%20profile.pdf. Accessed February 18, 2019.
- 9. American Lung Association. State of the Air. Washington, DC: American Lung Association; 2013. [Google Scholar]
- 10. Hricko A, Rowland G, Eckel S, Logan A, Taher M, Wilson J. Global trade, local impacts: lessons from California on health impacts and environmental justice concerns for residents living near freight rail yards. Int J Environ Res Public Health. 2014;11:1914-1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Castaneda H, Yang E, Mahmood A, et al. Health Risk Assessment for the BNSF Railway San Bernardino Railyard. Sacramento, CA: California Air Resources Board; 2008. [Google Scholar]
- 12. Federal Bureau of Investigation. California offenses known to law enforcement by city, 2012. https://ucr.fbi.gov/crime-in-the-u.s/2012/crime-in-the-u.s.-2012/tables/8tabledatadecpdf/table-8-state-cuts/table_8_offenses_known_to_law_enforcement_by_california_by_city_2012.xls. Accessed July 19, 2017.
- 13. Soret S, Montgomery S, Spencer-Hwang R. Project ENRRICH: A Public Health Assessment of Residential Proximity to a Goods Movement Railyard. Loma Linda, CA: Loma Linda University; 2014. [Google Scholar]
- 14. United States Bankruptcy Court Central District of California. City of San Bernardino http://www.cacb.uscourts.gov/case-of-interest/city-san-bernardino. Accessed January 20, 2018.
- 15. Spencer-Hwang R, Soret S, Halstead L, et al. Making human subject protection training community responsive: experiences delivering on the community-based participatory research promise. Prog Community Health Partnersh. 2014;8:215-224. [DOI] [PubMed] [Google Scholar]
- 16. Spencer-Hwang R, Montgomery S, Dougherty M, et al. Experiences of a rail yard community: life is hard. J Environ Health. 2014;77:8-17. [PMC free article] [PubMed] [Google Scholar]
- 17. Arthur KN, Spencer-Hwang R, Knutsen SF, Shavlik D, Soret S, Montgomery S. Are perceptions of community safety associated with respiratory illness among a low-income, minority adult population? BMC Public Health. 2018;18:1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bell J, Rubin V. Why Place Matters: Building a Movement for Healthy Communities. Oakland, CA: Policy Link–The California Endowment; 2007. [Google Scholar]
- 19. United States Census Bureau. Quick facts: San Bernardino city, California; United States. https://www.census.gov/quickfacts/fact/table/sanbernardinocitycalifornia,US/PST045216. Accessed April 22, 2018.
- 20. Wing JJ, August E, Adar SD, et al. Change in neighborhood characteristics and change in coronary artery calcium: a longitudinal investigation in the MESA (Multi-Ethnic Study of Atherosclerosis) Cohort. Circulation. 2016;134:504-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schulz AJ, Zenk SN, Israel BA, Mentz G, Stokes C, Galea S. Do neighborhood economic characteristics, racial composition, and residential stability predict perceptions of stress associated with the physical and social environment? Findings from a multilevel analysis in Detroit. J Urban Health. 2008;85:642-661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yen IH, Yelin EH, Katz P, Eisner MD, Blanc PD. Perceived neighborhood problems and quality of life, physical functioning, and depressive symptoms among adults with asthma. Am J Public Health. 2006;96:873-879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: development of a measure of neighborhood problems, and associations with socioeconomic status and health. Ann Behav Med. 2001;23:177-185. [DOI] [PubMed] [Google Scholar]
- 24. Goodman M. Keynote address. Paper presented at: First Annual Symposium sponsored by the Department of Biostatistics Summer Program in Quantitative Sciences, Dana Farber Cancer Institute; July 24, 2014; Boston, MA. [Google Scholar]
- 25. Penman-Aguilar A, Talih M, Huang D, Moonesinghe R, Bouye K, Beckles G. Measurement of health disparities, health inequities, and social determinants of health to support the advancement of health equity. J Public Health Manag Pract. 2016;22(suppl 1):S33-S42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health. 2010;100(suppl 1):S186-S196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schmidt S, Sparks PJ. Disparities in injury morbidity among young adults in the USA: individual and contextual determinants. J Epidemiol Community Health. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Scott SB, Munoz E, Mogle JA, et al. Perceived neighborhood characteristics predict severity and emotional response to daily stressors. Soc Sci Med. 2018;200:262-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lameris J, Hipp JR, Tolsma J. Perceptions as the crucial link? The mediating role of neighborhood perceptions in the relationship between the neighborhood context and neighborhood cohesion. Soc Sci Res. 2018;72:53-68. [DOI] [PubMed] [Google Scholar]
- 30. Fone D, White J, Farewell D, et al. Effect of neighbourhood deprivation and social cohesion on mental health inequality: a multilevel population-based longitudinal study. Psychol Med. 2014;44:2449-2460. [DOI] [PubMed] [Google Scholar]
- 31. Acket S, Borsenberger M, Dickes P, Sarracino F. Measuring and validating social cohesion: a bottom-up approach. Paper Presented at: the International Conference on Social Cohesion and Development, OECD; January 20-21, 2011; Paris, France. [Google Scholar]
- 32. Philippe P, Mansi O. Nonlinearity in the epidemiology of complex health and disease processes. Theor Med Bioeth. 1998;19:591-607. [DOI] [PubMed] [Google Scholar]
- 33. Cohen S. Social relationships and health. Am Psychol. 2004;59:676-684. [DOI] [PubMed] [Google Scholar]
- 34. Wilkins N, Tsao B, Hertz M, Davis R, Klevens J. Connecting the Dots: An Overview of the Links Among Multiple Forms of Violence. Atlanta, GA/Oakland, CA: National Center for Injury Prevention and Control/Centers for Disease Control and Prevention/Prevention Institute; 2014. [Google Scholar]
- 35. Shmool JL, Kubzansky LD, Newman OD, Spengler J, Shepard P, Clougherty JE. Social stressors and air pollution across New York City communities: a spatial approach for assessing correlations among multiple exposures. Environ Health. 2014;13:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kim ES, Hawes AM, Smith J. Perceived neighbourhood social cohesion and myocardial infarction. J Epidemiol Community Health. 2014;68:1020-1026. [DOI] [PMC free article] [PubMed] [Google Scholar]