Abstract
Monolithic zirconia crowns have become very popular; their surface finish is considered a key factor for restoration longevity. While polishing has shown excellent results in vivo, the surface glass infiltration of zirconia may offer superior damage resistance and aesthetic advantages by using tooth-colored glasses. Thus, the purpose of this study is to evaluate the efficacy of polishing and glass infiltration on the wear behavior of monolithic zirconia crowns. The wear behavior of intact natural molar teeth was investigated as a reference. Zirconia crowns were divided into 3 groups: PolZ—sintered then polished; PolGZ—polished in the presintered state and then glass infiltrated and sintered; NoPolGZ—as machined, glass infiltrated and sintered. Crowns were adhesively bonded to a dentin-like abutment. Zirconia crowns and molar teeth (n = 15) were subjected to contact-slide-liftoff cyclic loading (200 N, 1.25 million cycles) with a steatite sphere (r = 3 mm) as an antagonist in water. Surface and subsurface damages were investigated with optical and scanning electron microscopies. Wear depth and volume loss were determined with micro–computed tomography. PolGZ and NoPolGZ crowns exhibited shallow wear scars, where material loss remained within the glass/zirconia layer with no visible cracks. Meanwhile, PolZ crowns presented no visible wear damage. Volume loss (mm3) in the steatite antagonist was as follows (mean ± SD): PolZ = 0.022 ± 0.007, PolGZ = 0.011 ± 0.004, and NoPolGZ = 0.014 ± 0.006. Molar teeth yielded no measurable wear on the antagonist, while the wear scar on the teeth was greater than that on zirconia crowns, ranging from 0.07 to 0.35 mm3. The combination of polishing and glass infiltration on the occlusal surface of monolithic zirconia crowns yielded reduced wear on both crown and antagonist.
Keywords: ceramics, enamel, mastication, Prosthetic Dentistry, restorative materials, tooth wear
Introduction
The use of 3 mol% yttria-stabilized tetragonal zirconia (3Y-TZP) to fabricate monolithic dental restorations has been proposed as a solution to the high chipping rates associated with porcelain-veneered crowns (Sailer et al. 2015; Kim et al. 2018), as well as the high failure rates in multiunit porcelain-veneered fixed dental prostheses (Rinke et al. 2018). Although high survival rates (up to 98%) were reported for monolithic zirconia crowns and fixed dental prostheses, only a few clinical trials with relatively short follow-up periods (3 to 5 y) are available (Sulaiman et al. 2016; Bomicke et al. 2017). A major concern regarding this type of treatment is the wear of the antagonist tooth due to the superior mechanical properties—most notably, the high hardness and modulus of 3Y-TZP (Tong et al. 2016; Yan et al. 2018; Zhang and Lawn 2018).
Clinical studies showed some controversial wear behavior of monolithic zirconia crowns, which can induce similar (Hartkamp et al. 2017; Lohbauer and Reich 2017; Esquivel-Upshaw et al. 2018) or greater (Mundhe et al. 2015; Stober et al. 2016) wear of natural-enamel antagonist relative to enamel-enamel tooth contact. The restoration surface finish plays an important role in the outcomes of clinical wear studies. A highly polished zirconia occlusal surface can result in much-reduced antagonist enamel wear than that of glazed zirconia (Amer et al. 2014; Stawarczyk et al. 2016). However, the mirror finish of flat zirconia surfaces obtained in vitro is not replicable on the occlusal surface of crowns by using hand-piece polishing tools (Al-Haj Husain et al. 2016). Although glazing does not seem to affect the wear of the antagonist as compared with polished zirconia crowns in vivo (Mundhe et al. 2015; Stober et al. 2016; Hartkamp et al. 2017; Lohbauer and Reich 2017; Esquivel-Upshaw et al. 2018), the glaze is removed within a short period of occlusal function, creating wear-induced defects on the occlusal surface of crowns (Kaizer et al. 2017). Therefore, glazing can be used for aesthetic purposes on the axial walls of the crown, but the occlusal surface should be carefully polished and left unglazed (Lohbauer and Reich 2017).
In this study, we propose a new approach to minimize the drawbacks regarding the wear behavior of zirconia by creating a functionally graded glass/zirconia surface. Glass infiltration on the zirconia surface reduces its elastic modulus and hardness while increasing its resistance to sliding contact (Zhang and Kim 2010; Ren et al. 2011) and flexural damages (Zhang and Ma 2009; Zhang et al. 2010). Therefore, we postulate that the low-modulus and low-hardness glass-infiltrated surface could also benefit the restoration wear behavior. Accordingly, the objective of this study is to evaluate the effect of clinical-like polishing and/or glass infiltration on the wear behavior of monolithic zirconia crowns subjected to mouth-motion cyclic loading in water. The wear behavior of intact natural molar teeth has also been investigated as a reference.
Materials and Methods
A standard die of a mandibular first molar preparation was scanned, and anatomically correct crowns (n = 15) were soft milled from zirconia pucks (Lava Plus; 3M Dental Care) with a CAD/CAM system (LAVA CAD/CAM; 3M Dental Care). The monolithic zirconia crowns were then divided into 3 groups, according to various surface treatments:
PolZ (polished zirconia): crown outer surface was polished after sintering (control).
PolGZ (polished graded zirconia): crowns were presintered, outer surface polished, and then glass infiltrated with concurrent sintering.
NoPolGZ (not polished graded zirconia): crowns were presintered, then the outer surface (as machined) was glass infiltrated with concurrent sintering.
The crowns of the control group (PolZ) were sintered at 1,450 °C for 2 h, according to the zirconia manufacturer’s instructions. Subsequently, the outer surface of these crowns was carefully polished with a clinical zirconia polishing kit (Dialite ZR; Brasseler USA). Two different points were used: a medium followed by a fine polishing point. The outer surface of the crowns was polished with each grade for approximately 5 min with a slow-speed hand piece (5,000 to 10,000 rpm), resulting in a homogeneously glossy and smooth surface. The graded zirconia crowns (PolGZ and NoPolGZ) were produced by infiltrating the outer surface of zirconia with a feldspathic glass developed in-house, as previously described (Zhang and Kim 2009). Briefly, these crowns were initially presintered at 1,350 °C for 1 h. For the PolGZ group, crowns were polished in the presintered state following the same technique for the control group. All presintered crowns (PolGZ and NoPolGZ) subsequently received a thin layer of glass slurry on the outer surface, which was left to dry for several hours. Surface glass infiltration was carried out concurrently with sintering (1,450 °C for 2 h), aided by capillary pressure. The resulting structure consisted of a thin outer surface glass layer (~15 µm thick), followed by a graded glass/zirconia layer (~120 µm thick). The graded layer consisted of ~45 vol.% glass near the interface with the outer surface glass layer. The glass content gradually decreased with depth toward the dense 3Y-TZP interior (Zhang et al. 2012). The elastic modulus and hardness of the outer surface glass were 68 GPa and 8 GPa, respectively. For the graded layer, the modulus and hardness increased from 137 GPa and 11 GPa near the interface of the outer surface glass and graded layer to 213 GPa and 16 GPa near the boundary of the graded layer and homogeneous zirconia core (Zhang and Kim 2009).
All crowns were adhesively bonded to dentin-like abutments (Shembish et al. 2016). These were produced with a resin-based composite (Filtek Z100; 3M Dental Care) and then stored in distilled water at 37 °C for 3 to 5 wk for complete polymerization and hydration. Before cementation, the inner surface of the crowns was air abraded with 50-µm alumina particles at 2-bar pressure for 10 s, and crowns were ultrasonically cleaned in distilled water. Bonding was performed with a primer (Monobond Plus; Ivoclar Vivadent) and resin-based cement (Multilink Automix; Ivoclar Vivadent), following the manufacturer’s recommendations. Specimens were then stored in water at 37 °C for 5 to 7 d prior to wear testing.
Zirconia crowns were subjected to contact-sliding-liftoff mouth-motion cyclic loading, with an electrodynamic fatigue testing machine (Elf 3300, EnduraTEC; TA Instrument). The antagonist slides down the distobuccal cusp toward the central fossa, applying a 200-N load for 1.25 million cycles at a 1,000-N/s loading rate (~2 Hz) in water at room temperature (El Zhawi et al. 2016). The water was stagnant in a chamber and replaced daily. A spherical steatite antagonist (r = 3 mm) was used in this study. Steatite is a magnesium silicate–based ceramic, which has wear characteristics ranging between those of enamel and dental glass-ceramics (Shortall et al. 2002; Preis et al. 2011). Although steatite is widely used in the dental wear literature, its wear behavior relative to enamel is not well known. Therefore, this study included 15 intact human third molars, which were all impacted at the time of extraction. Prior to wear testing, the extracted teeth were stored in saline at 4 °C for 1 to 3 mo. Due to anatomic variations in the teeth, the most symmetrical and prominent cusp was chosen for wear testing.
After the wear test, a qualitative analysis of the surface damage in zirconia crowns, teeth, and antagonists was performed with optical (Leica MZ-APO) and scanning electron microscopes (S3500N; Hitachi). Zirconia crowns were also sectioned across the center of the wear crater along the sliding direction; polished cross sections were analyzed in a scanning electron microscope for subsurface damage evaluation (Renet al. 2011; Kaizer et al. 2017).
Volume loss in the steatite antagonists and teeth was quantified with 3-dimensional (3D) images obtained by a micro–computed tomography scanner (micro-CT 40; Scanco Medical AG). Scanning was performed in high resolution (voxel size: 8 µm) at 70-kVp energy, 114-µA intensity (0.5-mm aluminum filter), and 250-ms integration time. The micro-CT slices were assembled as 3D models with Mimics Research 17.0 software (Materialise) and exported as stereolithography files for volumetric measurements (Geomagic Wrap; 3D Systems). For the antagonists, the original spherical topography was reconstructed by means of mesh editing, and the maximum wear depth and volume loss were obtained by comparing the same 3D models before and after reconstruction. For teeth, micro-CT scans were obtained before and after the wear test, so volume loss was quantified by Boolean subtraction of the intact and worn 3D models.
Volume loss (mm3) and maximum wear depth (mm) data for the steatite antagonists passed the tests for normality and equality of variances. Differences among groups were then investigated with 1-way analysis of variance, and pairwise multiple comparisons were performed with a Tukey’s test. The significance level was set at 5% (α = 0.05) with power of performed analyses >80% (β > 0.8).
Results
Volume loss was not quantified for the zirconia crowns, because material loss was negligible. PolZ crowns showed no repeated sliding contact–induced wear and cracks on the surface, as shown in Figure 1. However, residual machine tool marks were apparent near the base of the cusp, toward the central groove. The surface micrographs of the PolGZ (Fig. 2A) and NoPolGZ (Fig. 3A) crowns showed shallow wear scars at the sliding surface. For both types of graded zirconia crowns, it was possible to observe that the progressive wear of the outer surface glass led to the exposure of the zirconia/glass graded layer. However, a more homogeneous and smooth surface was observed in PolGZ relative to NoPolGZ, where the glass/zirconia graded layer with patches of glass pockets was observed. Further subsurface investigation on the cross-sectioned crowns (Figs. 2B, 3B) revealed that the outer surface glass layer was removed but no near contact–induced cracks were observed in any of the crowns. Note that the cross-sectional images of Figures 2B and 3B clearly reveal depth-dependent structural changes in the graded crowns: an outer surface glass layer followed by a glass/zirconia graded layer.
Figure 1.
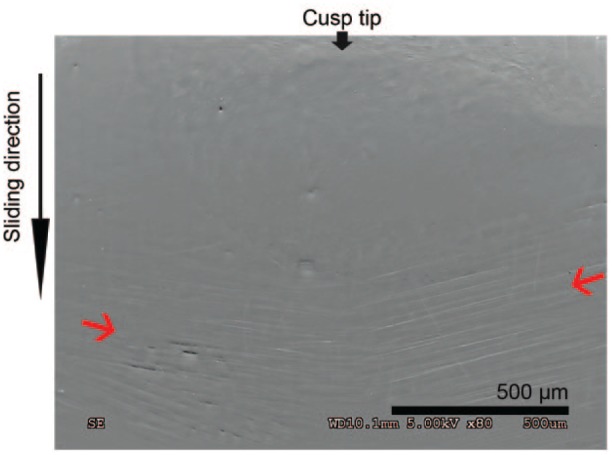
Cusp surface of a PolZ (polished zirconia) crown after wear testing. Note the absence of near contact–induced wear and fracture. The thin red arrows indicate the presence of surface residual machine tool marks near the bottom of the cusp, toward the central groove, which were not removed during polishing.
Figure 2.
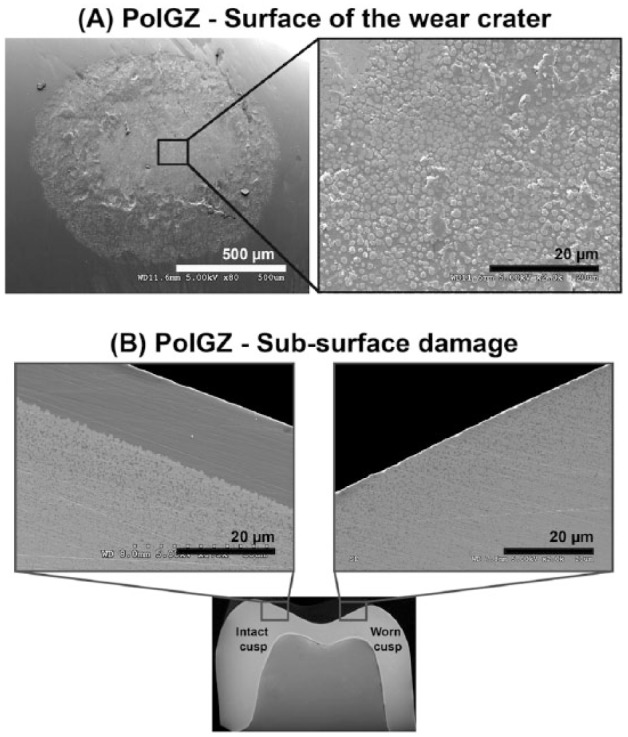
(A) Cusp surface of PolGZ (polished graded zirconia) crown after wear testing. Surface images of the wear scar show that the superficial glass was removed, exposing a smooth zirconia/glass graded layer, which is shown in detail in the magnified image (right). (B) Cross section of the crown shows the graded structure (left) with preserved surface glass on the intact cusp. At the center of the wear crater (right), the surface glass has been worn out, but there are no cyclic contact-induced cracks.
Figure 3.

(A) Cusp surface of NoPolGZ (not polished graded zirconia) crown after wear testing. Surface images of the wear scar show that the superficial glass has been worn down, exposing a small area of a zirconia/glass graded layer with patches of glass pockets, which are shown in detail in the magnified image (right). (B) Cross section of the crown shows the graded structure (left) with preserved surface glass on the intact cusp. At the center of the wear crater (right), surface glass has been worn out, and again, there are no sliding contact-induced cracks.
The wear scar on natural enamel cusps (teeth group) was greater than that observed from zirconia crowns. Thus, it was possible to measure volume loss after the wear test (Fig. 4). However, measurements of volume loss varied significantly among different teeth, ranging from 0.07 to 0.35 mm3 (mean ± SD = 0.19 ± 0.11 mm3). Wear remained within enamel, whereas dentin was not exposed in any of the evaluated teeth. Variations could be related to natural teeth heterogeneity (i.e., the enamel properties, occlusal anatomy, cusp size, and inclination).
Figure 4.
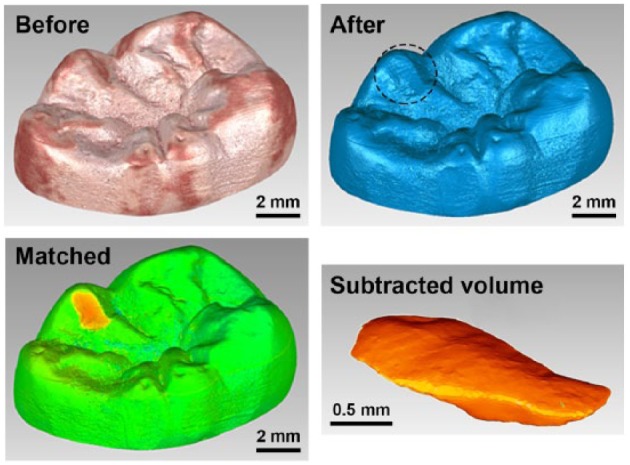
Three-dimensional reconstructions of a representative tooth before and after the wear test, followed by a superimposed image of before-and-after wear testing to highlight the worn volume. The volume loss for this particular tooth was 0.33 mm3.
The 3D volumetric reconstructions of the steatite antagonists after the wear test are represented in Figure 5. The antagonist suffered less wear (PolGZ = 0.011 ± 0.004 mm3) from the polished graded zirconia crowns as compared with the PolZ control group (0.022 ± 0.007 mm3, P = 0.036), while NoPolGZ occupied the middle ground (0.014 ± 0.006 mm3) but was statistically similar to the other 2 groups. Wear depth, however, was statistically similar (P = 0.215) for all 3 groups: PolZ = 0.054 ± 0.015 mm, PolGZ = 0.043 ± 0.009 mm, and NoPolGZ = 0.043 ± 0.006 mm. The chewing motion of steatite against natural enamel (teeth group) resulted in a very shallow wear scar (not measurable), suggesting more of a polishing effect than material loss.
Figure 5.

The graph shows the mean ± SD volume loss (mm3) of steatite antagonists yielded from the 3 zirconia surface finishes after wear testing. Different letters between measurements represent statistical significance, P < 0.05. Representative 3-dimensional volumetric reconstructions of the wear scar on the steatite antagonists are also presented. NoPolGZ, not polished graded zirconia; PolGZ, polished graded zirconia; PolZ, polished zirconia.
It is important to note that under the current test conditions (i.e., a 200-N load applied through a steatite spherical antagonist, r = 3 mm), the initial contact pressure was 1,977, 2,925, and 2,257 MPa in graded zirconia crowns (including both the polished and not-polished groups), polished zirconia crowns, and enamel (molar teeth), respectively. The contact area between the antagonist and crown increased due to the formation of the wear facet, thus decreasing the contact pressure to around 215, 172, and 127 MPa in the aforementioned 3 groups of crowns/teeth at the end of the chewing simulation.
Discussion
This study investigated the wear behavior of graded zirconia crowns relative to the polished monolithic zirconia control. Our findings showed that graded zirconia crowns generated similar or even less wear in their antagonist than that of polished zirconia crowns. Additionally, polishing zirconia in a softer presintered state prior to glass infiltration resulted in a more homogeneous and smoother surface, which was also less abrasive to the antagonist.
For the monolithic zirconia control group, no repeated sliding contact–induced wear damage was observed on the crown surface. However, a greater volume loss was found in the antagonist. This behavior could be attributed to 3Y-TZP high elastic modulus and hardness (Tong et al. 2016; Zhang and Lawn 2018) and to the quality of the surface finish (Fig. 1). Scratches were present on the surface of polished zirconia crowns due to difficulties in obtaining a uniform smooth surface when polishing was performed on the hard zirconia after sintering. Note that the polishing procedures were performed by an experienced prosthodontist with high-quality polishing tools. The combination of a hard ceramic in addition to the complex geometry of a crown, especially in the occlusal surface, impaired the quality of the surface polishing. Previous studies corroborate these limitations, showing that the existing polishing systems are not able to completely remove machining or bur-made grooves on a sintered zirconia surface and that a nonuniformly smooth surface negatively affects the material wear behavior (Preis et al. 2011; Al-Haj Husain et al. 2016).
On the contrary, tailoring the elastic and mechanical properties of 3Y-TZP with a functionally graded glass/zirconia surface layer resulted in more favorable wear behavior. Considerably shallow wear facets were observed for both graded zirconia groups, in which the thin and soft superficial glass was removed and the zirconia/glass graded layer was exposed. Different from what was reported for glazed monolithic zirconia (Amer et al. 2014; Stawarczyk et al. 2016; Kaizer et al. 2017), the wear of the superficial glass did not directly expose the hard 3Y-TZP interior but, rather, an intermediate layer with graded elastic and mechanical properties (Zhang 2012). It is highly unlikely that the graded layer would be completely worn out in a clinical situation. After 1.25 million chewing cycles with a “hard” steatite antagonist at a relatively high nominal load of 200 N, just the surface glass was worn out (similar to glaze), yet the graded layer was only mildly polished and no measurable depth loss was detected. We would like to emphasize 2 points here: 1) Steatite is harder and more abrasive than enamel, yet it caused minimal wear in graded zirconia; 2) Wear on graded zirconia would progressively expose regions with less glass and more zirconia; thus, the restoration would become even more resistant to wear.
Also, no difference in the antagonist volume loss was observed between polished and unpolished graded zirconia crowns. Nonetheless, the worn surface of the polished graded zirconia was smoother and more homogeneous after the glass layer was removed. This quality of the surface may favor the long-term wear behavior of the crowns, since the superficial glass layer is progressively removed and a larger area of the graded layer is then exposed to the oral environment. Rough occlusal surfaces can increase the coefficient of friction and may result in unwanted damage of the antagonist (Kaizer et al. 2017). In addition, the occlusal surface of a crown should ideally maintain a mild wear condition in the long term for better resistance to sliding contact fracture (Ren and Zhang 2014; Pang et al. 2015). Moreover, polishing the relatively soft presintered zirconia can be carried out quickly and efficiently, not burdening the crown fabrication process.
Another important finding of this study is the absence of contact-induced cracks in the surface and subsurface of the wear scars in zirconia crowns. Previous studies demonstrated that graded glass/zirconia structures have superior resistance to sliding contact damage, comparable to that of monolithic zirconia (Zhang and Kim 2010; Ren et al. 2011). Corroborating our findings, it was predicted that even with a much stiffer and harder tungsten carbide indenter at 200 N load in water, the number of cycles for initiating herringbone cracks in 3Y-TZP and graded zirconia would be much greater than the 1.2 × 106 used in the present study (Zhang and Kim 2010). Additionally, it was reported that only after 10 million sliding cycles a few fine cracks formed in the graded layer and these cracks were arrested by the tough zirconia core, suggesting long-term structural stability (Ren et al. 2011). More significantly, recent studies showed that glass infiltration of high-translucency zirconias is also feasible, resulting in a strengthening effect similar to that observed in 3Y-TZPs while retaining excellent translucency properties (Kaizer and Zhang 2018; Mao et al. 2018).
The use of steatite as a human enamel substitute for wear testing is questionable. Although the coefficient of friction between steatite and enamel surfaces under water lubrication is similar to enamel-to-enamel, steatite has higher hardness (6.7 GPa) and initial roughness than enamel, which has a hardness of 3.5 GPa (Shortall et al. 2002; Preis et al. 2011), which can explain the larger wear scars in the teeth surface as compared with monolithic zirconia crowns. Also, as expected, the heterogeneity of the enamel structure and geometry led to large variation in teeth volume loss (0.07 to 0.35 mm3). In addition, the tooth was worn out, but only a polished appearance of the shallow wear facets was observed in the steatite antagonist, which does not properly simulate the wear behavior of tooth against tooth. Nevertheless, steatite antagonists are still suitable for in vitro wear tests, as they allow the standardization of testing conditions and thus quantification of the wear results (Preis et al. 2011; El Zhawi et al. 2016). Moreover, the mechanical properties of steatite are in the range of glass-ceramics, which is a class of restorative materials widely used in clinical situations (Shortall et al. 2002).
Conclusions
Polished graded zirconia crowns exhibit excellent wear behavior. This is attributed to polishing zirconia in a softer presintered state, followed by glass infiltration, resulting in a restoration resistant to wear damage as well as mild to the antagonist, capable of preserving enamel structure.
Author Contributions
M.R. Kaizer, Y. Zhang, contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; S. Bano, V. Garg, contributed to data acquisition, analysis, and interpretation, drafted the manuscript; M. Borba, contributed to data analysis and interpretation, drafted and critically revised the manuscript; M.B.F. dos Santos, contributed to data acquisition, analysis, and interpretation, critically revised the manuscript.
Footnotes
Funding was provided by the National Institutes of Health / National Institute of Dental and Craniofacial Research (grants R01DE026772, R01DE026279, R01DE017925).
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
ORCID iDs: M.R. Kaizer  https://orcid.org/0000-0002-6308-6089
https://orcid.org/0000-0002-6308-6089
M.B.F. dos Santos  https://orcid.org/0000-0001-5477-4077
https://orcid.org/0000-0001-5477-4077
References
- Al-Haj Husain N, Camilleri J, Özcan M. 2016. Effect of polishing instruments and polishing regimens on surface topography and phase transformation of monolithic zirconia: an evaluation with XPS and XRD analysis. J Mech Behav Biomed Mater. 64:104–112. [DOI] [PubMed] [Google Scholar]
- Amer R, Kurklu D, Kateeb E, Seghi RR. 2014. Three-body wear potential of dental yttrium-stabilized zirconia ceramic after grinding, polishing, and glazing treatments. J Prosthet Dent. 112(5):1151–1155. [DOI] [PubMed] [Google Scholar]
- Bomicke W, Rammelsberg P, Stober T, Schmitter M. 2017. Short-term prospective clinical evaluation of monolithic and partially veneered zirconia single crowns. J Esthet Restor Dent. 29(1):22–30. [DOI] [PubMed] [Google Scholar]
- El Zhawi H, Kaizer MR, Chughtai A, Moraes RR, Zhang Y. 2016. Polymer infiltrated ceramic network structures for resistance to fatigue fracture and wear. Dent Mater. 32(11):1352–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esquivel-Upshaw JF, Kim MJ, Hsu SM, Abdulhameed N, Jenkins R, Neal D, Ren F, Clark AE. 2018. Randomized clinical study of wear of enamel antagonists against polished monolithic zirconia crowns. J Dent. 68:19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartkamp O, Lohbauer U, Reich S. 2017. Antagonist wear by polished zirconia crowns. Int J Comput Dent. 20(3):263–274. [PubMed] [Google Scholar]
- Kaizer MR, Gierthmuehlen PC, Dos Santos MB, Cava SS, Zhang Y. 2017. Speed sintering translucent zirconia for chairside one-visit dental restorations: optical, mechanical, and wear characteristics. Ceram Int. 43(14): 10999–11005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaizer MR, Zhang Y. 2018. Novel strong graded high-translucency zirconias for broader clinical applications. Dent Mater. 31(S1):e140–e141. [Google Scholar]
- Kim J, Dhital S, Zhivago P, Kaizer MR, Zhang Y. 2018. Viscoelastic finite element analysis of residual stresses in porcelain-veneered zirconia dental crowns. J Mech Behav Biomed Mater. 82:202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohbauer U, Reich S. 2017. Antagonist wear of monolithic zirconia crowns after 2 years. Clin Oral Investig. 21(4):1165–1172. [DOI] [PubMed] [Google Scholar]
- Mao L, Kaizer MR, Zhao M, Guo B, Song YF, Zhang Y. 2018. Graded ultra-translucent zirconia (5Y-PSZ) for strength and functionalities. J Dent Res. 97(11):1222–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundhe K, Jain V, Pruthi G, Shah N. 2015. Clinical study to evaluate the wear of natural enamel antagonist to zirconia and metal ceramic crowns. J Prosthet Dent. 114(3):358–363. [DOI] [PubMed] [Google Scholar]
- Pang Z, Chughtai A, Sailer I, Zhang Y. 2015. A fractographic study of clinically retrieved zirconia-ceramic and metal-ceramic fixed dental prostheses. Dent Mater. 31(10):1198–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preis V, Behr M, Kolbeck C, Hahnel S, Handel G, Rosentritt M. 2011. Wear performance of substructure ceramics and veneering porcelains. Dent Mater. 27(8):796–804. [DOI] [PubMed] [Google Scholar]
- Ren L, Janal MN, Zhang Y. 2011. Sliding contact fatigue of graded zirconia with external esthetic glass. J Dent Res. 90(9):1116–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren L, Zhang Y. 2014. Sliding contact fracture of dental ceramics: principles and validation. Acta Biomater. 10(7):3243–3253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinke S, Wehle J, Schulz X, Burgers R, Rodiger M. 2018. Prospective evaluation of posterior fixed zirconia dental prostheses: 10-year clinical results. Int J Prosthodont. 31(1):35–42. [DOI] [PubMed] [Google Scholar]
- Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. 2015. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: single crowns (SCs). Dent Mater. 31(6):603–623. [DOI] [PubMed] [Google Scholar]
- Shembish FA, Tong H, Kaizer M, Janal MN, Thompson VP, Opdam NJ, Zhang Y. 2016. Fatigue resistance of CAD/CAM resin composite molar crowns. Dent Mater. 32(4):499–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shortall AC, Hu XQ, Marquis PM. 2002. Potential countersample materials for in vitro simulation wear testing. Dent Mater. 18(3):246–254. [DOI] [PubMed] [Google Scholar]
- Stawarczyk B, Frevert K, Ender A, Roos M, Sener B, Wimmer T. 2016. Comparison of four monolithic zirconia materials with conventional ones: contrast ratio, grain size, four-point flexural strength and two-body wear. J Mech Behav Biomed Mater. 59:128–138. [DOI] [PubMed] [Google Scholar]
- Stober T, Bermejo JL, Schwindling FS, Schmitter M. 2016. Clinical assessment of enamel wear caused by monolithic zirconia crowns. J Oral Rehabil. 43(8):621–629. [DOI] [PubMed] [Google Scholar]
- Sulaiman TA, Abdulmajeed AA, Donovan TE, Cooper LF, Walter R. 2016. Fracture rate of monolithic zirconia restorations up to 5 years: a dental laboratory survey. J Prosthet Dent. 116(3):436–439. [DOI] [PubMed] [Google Scholar]
- Tong H, Tanaka CB, Kaizer MR, Zhang Y. 2016. Characterization of three commercial Y-TZP ceramics produced for their high-translucency, high-strength and high-surface area. Ceram Int. 42(1 Pt B):1077–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan J, Kaizer MR, Zhang Y. 2018. Load-bearing capacity of lithium disilicate and ultra-translucent zirconias. J Mech Behav Biomed Mater. 88:170–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y. 2012. Overview: damage resistance of graded ceramic restorative materials. J Eur Ceram Soc. 32(11):2623–2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Chai H, Lawn BR. 2010. Graded structures for all-ceramic restorations. J Dent Res. 89(4):417–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Chai H, Lee JJ, Lawn BR. 2012. Chipping resistance of graded zirconia ceramics for dental crowns. J Dent Res. 91(3):311–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Kim JW. 2009. Graded structures for damage resistant and aesthetic all-ceramic restorations. Dent Mater. 25(6):781–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Kim JW. 2010. Graded zirconia glass for resistance to veneer fracture. J Dent Res. 89(10):1057–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Lawn BR. 2018. Novel zirconia materials in dentistry. J Dent Res. 97(2):140–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Ma L. 2009. Optimization of ceramic strength using elastic gradients. Acta Mater. 57(9):2721–2729. [DOI] [PMC free article] [PubMed] [Google Scholar]


