Abstract
Eagle syndrome is a rare cause of stroke and results as a complication of the elongated styloid process (ESP), which can cause carotid dissection and consequent ischemic stroke. We report a case of a 42-year-old woman with a past medical history of rheumatoid arthritis who developed left hemispheric ischemic stroke after deep tissue massage. Imaging studies revealed an intimal tear of the left carotid artery bulb and bilaterally ESPs, measuring approximately 6 cm on the right and 4.5 cm on the left. It seems that direct vascular compromise by the anomalous styloid process was the cause of her carotid artery dissection and stroke. Moreover, neck manipulation may have been a contributing factor.
Keywords: Eagle syndrome, styloid process, carotid artery dissection
Introduction
Eagle syndrome is named after Watt W. Eagle who in 1937 described elongation of the styloid process or calcification of the stylohyoid ligament.1 The styloid process is a slender bony prominence projecting from the inferior surface of the temporal bone between the internal and the external carotid arteries.2–4 The styloid process is a derivative of Reichert cartilage which originates from the second branchial arch. Multiple theories exist to describe this anomaly and include persistence of precursors causing congenital styloid process elongation, ossification of the stylohyoid ligament, reactive hyperplasia or metaplasia secondary to trauma, congenital anatomical variation, and age-related calcification.2,5-7 Although the incidence of elongated styloid process (ESP) is contested, majority of researchers report an incidence between 4% and 7%, but there is a consensus that only a small minority of patients become symptomatic from ESP.3,6,8-13 Presence of ESP should not imply causation in ischemic stroke, and other underlying conditions should be ruled out, such as connective tissue disorders, which may cause an ESP and concomitantly increase the risk of carotid artery dissection (CAD).14 Generally, a length >3 cm is abnormal.3,6,8,15
There are a number of symptoms that may occur which are thought to be dependent on the length, width, and angulations of the styloid process. The classic presentation as described by Watt Eagle is a sensation of throat pain, otalgia, dysphagia, and a sensation of pharyngeal foreign body.3,15 A less common variant, stylocarotid syndrome, is associated with vascular compromise of the internal or external carotid arteries. This can present with headaches, transient ischemic attack, or stroke. Additionally, mechanical insult to the carotid artery leading to dissection may occur.3,9,15
Case Report
A 42-year-old woman with a past medical history of rheumatoid arthritis was referred to our stroke clinic for the evaluation of ischemic stroke. The patient was recently on a cruise ship when she developed right-sided hemiparesis and facial weakness and aphasia. The patient had received a deep tissue massage prior to the onset of her symptoms. She was transferred to an outside hospital but did not receive tissue plasminogen activator or endovascular intervention, as she was outside the treatment time window for such therapy. The patient did not have typical vascular risk factors such as hypertension, hyperlipidemia, diabetes mellitus, tobacco abuse, and her stroke workup including hypercoagulation workup, echocardiography, and cardiac monitoring for atrial fibrillation was unremarkable. Diagnostic studies revealed an abrupt occlusion of the left middle cerebral artery (MCA; M1 portion) and an intimal tear and dissection of left internal carotid artery (ICA) bulb (Figure 1). The patient had a left basal ganglia ischemic stroke (Figure 2). Further studies revealed bilateral ESPs, approximately 6 cm on the right side and 4.5 cm on the left side (Figure 3).
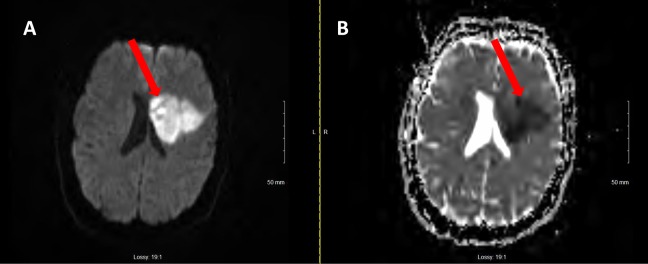
Figure 1.
Magnetic resonance angiography of the head (axial sequence) showing left internal carotid artery (ICA) dissection (arrow).
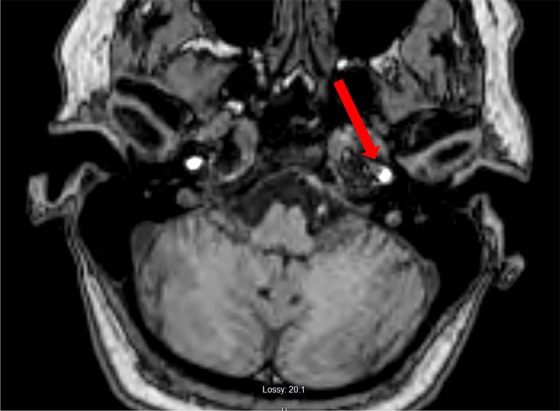
Figure 2.
A, Magnetic resonance imaging (MRI) brain, diffusion-weighted imaging sequence showing area of restricted diffusion in the left middle cerebral artery (MCA) distribution. B, Magnetic resonance imaging brain, apparent diffusion coefficient (ADC) sequence showing corresponding areas of hypointensity.
Figure 3.
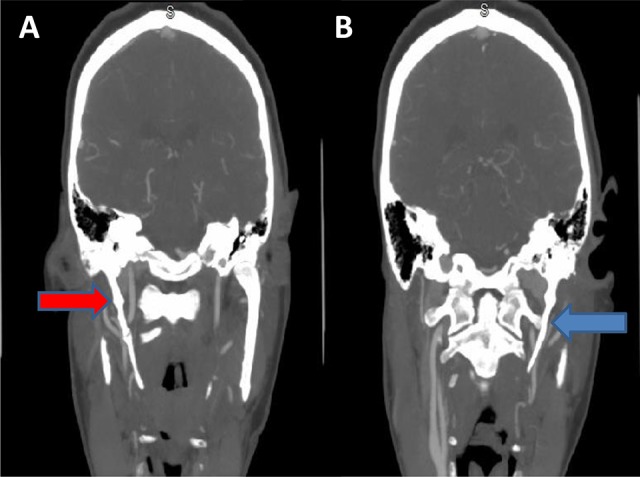
Computed tomography angiography (CTA) of the head and neck (coronal sequence) showing elongated right (A, red arrow) styloid process measuring 6 cm and left (B, blue arrow) styloid process measuring 4.5 cm.
Cardiovascular risk factor modification was addressed. Dual antiplatelet was initiated prior to her evaluation at our institution. It was stopped, and monotherapy only with aspirin was continued. The patient was discharged to continue physical and occupational therapy. She was also seen by a vascular surgery team, and surgical intervention was not recommended for elongation of the styloid process. The patient was educated to avoid hyperextension or hyperrotation of the neck. The patient’s follow-up imaging after 3 months revealed recanalization of left MCA.
The patient’s history of rheumatoid arthritis and receiving a massage may increase the risk of arterial dissection, but these potential risk factors typically cause vertebral artery dissection. Also, spontaneous or traumatic CAD is more common in younger individuals. However, in the absence of traditional stroke risk factors, we believe direct vascular contact by ESP associated with Eagle syndrome alone or possibly in combination with neck manipulation is the likely cause of CAD and the consequent left M1 embolic stroke which lead to left basal ganglia infarction. At this juncture, the patient continues to recover. Her modified Rankin scale was 2 at a 3-month follow-up visit.
Discussion
Watt W. Eagle described 2 versions of this syndrome associated with the neurovascular structures compromised by the styloid process.15,16 More common of the 2 is the classic form, which is associated with neck pain, dysphagia, odynophagia, and a referred otalgia. In the less commonly seen “stylocarotid artery syndrome,” internal and external carotid arteries and the accompanying periarterial nerve plexus are compromised by an elongated or abnormally angulated styloid process. These patients can experience eye and facial pain, cephalalgia, transient ischemic symptoms, syncope, or rarely a CAD.3,6 Our patient did not report these symptoms prior to being diagnosed with CAD and ischemic stroke.
Eagle syndrome is not commonly recognized as a cause of CAD. While the incidence of symptomatic ESP is still low, we have noticed a recent increase in published case reports of CAD caused by Eagle syndrome, including 3 cases at a single institution within a year which may raise awareness of this disease entity.11–13,17–19 Cerebrovascular complications including stroke have been reported with this entity related to elongation of the styloid process leading to an intimal tear, artery to artery embolism, and MCA occlusion with subsequent infarction such as in our case. Studies have suggested styloid-ICA distance along with styloid process length as risk factors for CAD.14,20 One study reported mean styloid process length in CAD to be longer than in controls (3.03 cm vs 2.66 cm), suggesting a 4-fold increase in risk for CAD associated with ESPs.14 In our case, the styloid process length was 4.5 cm on the affected side. Furthermore, another study reported mean styloid–carotid distance calculated at midpoint of ICA to be significantly shorter in patients with CAD compared to controls (56 mm vs 66.5 mm on the right and 57.5 mm vs 74.5 mm on the left).20 Styloid–ICA distance in our case was approximately 6.5 mm on the right and 1.7 mm on the left, which is significantly lower than the mean distances previously reported.
Therefore, this syndrome should be included in the differential diagnosis when evaluating CAD and ensuing cerebrovascular sequelae. Other associated conditions to consider include connective tissue and collagen vascular disorders, history of smoking or trauma, history of migraine, and hypertension.3,7,17 Proper examination including palpation of the tonsillar fossa and radiological studies may be valuable diagnostic adjuncts. However, the value of palpation of the tonsillar fossa remains to be further defined in this entity.6
Recent reports of Eagle syndrome suggest direct vascular compromise by the anomalous styloid process. Also, neck manipulation may affect the degree of vascular compression.17 This was likely the case in our patient who had CAD and stroke soon after receiving a massage. Imaging may be useful in the evaluation of Eagle syndrome. Plain radiographs may be obtained to evaluate styloid process anatomy. However, computed tomography scan is the study of choice to evaluate anatomical variations in the styloid process and stylohyoid ligament.7 In case of stylocarotid syndrome, 3-D computed tomography angiography is considered the gold standard for assessing vascular compromise secondary to angulation or length of the styloid process.7,17,21
Treatment guidelines for CAD secondary to a mechanical insult by an ESP have not been established, but short-term anticoagulation (3-6 months) and antiplatelet medications such as aspirin are considered reasonable treatment approaches.3,17 Patients who fail medical management and experience recurrent strokes or refractory pain symptoms can be considered for styloid process resection. Surgical dissection is typically performed via an intraoral or a cervical approach.7,21
Acknowledgments
The patient described in this case report provided consent for publication.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Eagle WW. Elongated styloid processes: report of two cases. Arch Otolaryngol. 1937;25(5):584–587. [Google Scholar]
- 2. Cawich S, Gardner M, Johnson P, Shetty R, Wolf K. The clinical significance of an elongated styloid process. Internet J Fam Pract. 2008;6(1):3. [Google Scholar]
- 3. Smoot TW, Taha A, Tarlov N, Riebe B. Eagle syndrome: a case report of stylocarotid syndrome with internal carotid artery dissection. Interv Neuroradiol. 2017;23(4):433–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Han MK, Kim DW, Yang JY. Non surgical treatment of Eagle’s syndrome—a case report. Korean J Pain. 2013;26(2):169–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moon CS, Lee BS, Kwon YD, et al. Eagle’s syndrome: a case report. J Korean Assoc Oral Maxillofac Surg. 2014;40(1):43–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Piagkou M, Anagnostopoulou S, Kouladouros K, Piagkos G. Eagle’s syndrome: a review of the literature. Clin Anat. 2009;22(5):545–558. [DOI] [PubMed] [Google Scholar]
- 7. Badhey A, Jategaonkar A, Anglin Kovacs AJ, et al. Eagle syndrome: a comprehensive review. Clin Neurol Neurosurg. 2017;159:34–38. [DOI] [PubMed] [Google Scholar]
- 8. Gallaway E, Bayoumi S, Hammond D, Halsnad M. Case report: an atypical presentation of Eagle syndrome. J Surg Case Rep. 2017;2017(8):rjx152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. David J, Lieb M, Rahimi SA. Stylocarotid artery syndrome. J Vasc Surg. 2014;60(6):1661–1663. [DOI] [PubMed] [Google Scholar]
- 10. Eagle WW. Elongated styloid process: symptoms and treatment. AMA Arch Otolaryngol. 1958;67(2):172–176. [DOI] [PubMed] [Google Scholar]
- 11. Esiobu PC, Yoo MJ, Kirkham EM, Zierler RE, Starnes BW, Sweet MP. The role of vascular laboratory in the management of Eagle syndrome. J Vasc Surg Cases Innov Tech. 2018;4(1):41–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jelodar S, Ghadirian H, Ketabchi M, Ahmadi Karvigh S, Alimohamadi M. Bilateral ischemic stroke due to carotid artery compression by abnormally elongated styloid process at both sides: a case report. J Stroke Cerebrovasc Dis. 2018;27(6):e89–e91. [DOI] [PubMed] [Google Scholar]
- 13. Subedi R, Dean R, Baronos S, Dhamoon A. Carotid artery dissection: a rare complication of Eagle syndrome. BMJ Case Rep. 2017;2017:bcr2016218184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Raser JM, Mullen MT, Kasner SE, Cucchiara BL, Messe SR. Cervical carotid artery dissection is associated with styloid process length. Neurology. 2011;77(23):2061–2066. [DOI] [PubMed] [Google Scholar]
- 15. Eagle WW. Symptomatic elongated styloid process report of two cases of styloid process-carotid artery syndrome with operation. Arch Otolaryngol. 1949;49(5):490–503. [DOI] [PubMed] [Google Scholar]
- 16. Eagle WW. Elongated styloid process: further observations and a new syndrome. Arch Otolaryngol. 1948;47(5):630–640. [DOI] [PubMed] [Google Scholar]
- 17. Ogura T, Mineharu Y, Todo K, Kohara N, Sakai N. Carotid artery dissection caused by an elongated styloid process: three case reports and review of the literature. NMC Case Rep J. 2015;2(1):21–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Aldakkan A, Dunn M, Warsi NM, Mansouri A, Marotta TR. Vascular Eagle’s syndrome: two cases illustrating distinct mechanisms of cerebral ischemia. J Radiol Case Rep. 2017;11(8):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kavi T, Lahiri S. Teaching neuroimages: Eagle syndrome: cerebrovascular complications. Neurology. 2016;87(2):e17–e17. [DOI] [PubMed] [Google Scholar]
- 20. Renard D, Azakri S, Arquizan C, Swinnen B, Labauge P, Thijs V. Styloid and hyoid bone proximity is a risk factor for cervical carotid artery dissection. Stroke. 2013;44(9):2475–2479. [DOI] [PubMed] [Google Scholar]
- 21. Razak A, Short JL, Hussain SI. Carotid artery dissection due to elongated styloid process: a self-stabbing phenomenon. J Neuroimaging. 2014;24(3):298–301. [DOI] [PubMed] [Google Scholar]