Abstract
Objective
To characterise the contributing factors that affect medical students’ subspecialty choice and to estimate the extent of influence of individual factors on the students’ decision-making process.
Design
Systematic review and meta-analysis.
Methods
A systematic search of the Cochrane Library, ERIC, Web of Science, CNKI and PubMed databases was conducted for studies published between January 1977 and June 2018. Information concerning study characteristics, influential factors and the extent of their influence (EOI) was extracted independently by two trained investigators. EOI is the percentage level that describes how much each of the factors influenced students’ choice of subspecialty. The recruited medical students include students in medical school, internship, residency training and fellowship, who are about to or have just made a specialty choice. The estimates were pooled using a random-effects meta-analysis model due to the between-study heterogeneity.
Results
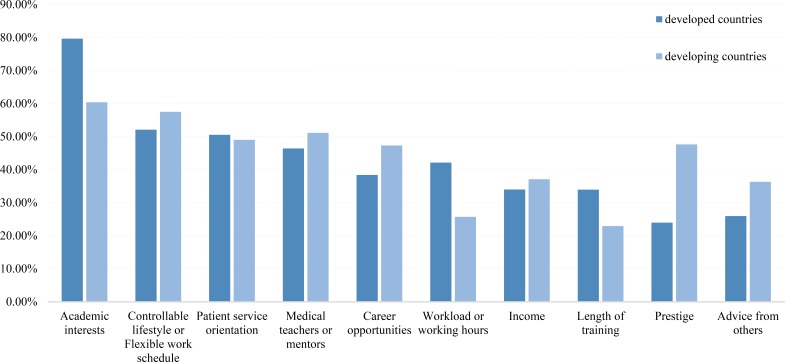
Data were extracted from 75 studies (882 209 individuals). Overall, the factors influencing medical students’ choice of subspecialty training mainly included academic interests (75.29%), competencies (55.15%), controllable lifestyles or flexible work schedules (53.00%), patient service orientation (50.04%), medical teachers or mentors (46.93%), career opportunities (44.00%), workload or working hours (37.99%), income (34.70%), length of training (32.30%), prestige (31.17%), advice from others (28.24%) and student debt (15.33%), with significant between-study heterogeneity (p<0.0001). Subgroup analyses revealed that the EOI of academic interests was higher in developed countries than that in developing countries (79.66% [95% CI 70.73% to 86.39%] vs 60.41% [95% CI 43.44% to 75.19%]; Q=3.51, p=0.02). The EOI value of prestige was lower in developed countries than that in developing countries (23.96% [95% CI 19.20% to 29.47%] vs 47.65% [95% CI 34.41% to 61.24%]; Q=4.71, p=0.01).
Conclusions
This systematic review and meta-analysis provided a quantitative evaluation of the top 12 influencing factors associated with medical students’ choice of subspecialty. Our findings provide the basis for the development of specific, effective strategies to optimise the distribution of physicians among different departments by modifying these influencing factors.
Keywords: medical students, career choice, meta-analysis
Strengths and limitations of this study.
This is the first study that provides a systematic estimate of the factors associated with medical students’ subspecialty choices.
A large number of studies conducted in varied populations have been included.
The differences in the characteristics of country, survey years, specialty, the type of data used and sample size across studies represent a major limitation of our study.
Introduction
Because of the population ageing, increased workload on doctors through increased number of consultations and in managing patients with multimorbidity, the demand for physicians continues to increase; however, an imbalance in the supply of physicians in different subspecialties has become a growing concern in both developed and developing countries.1–5 Some specialties and subspecialties, such as family medicine and palliative medicine,6 7 are experiencing a desperate shortage of physicians, whereas other specialties and subspecialties, such as cardiology, ophthalmology and ear, nose and throat surgery, are highly competitive specialties with low success rate for candidates.8 9
Specialty choice is the product of a complex interconnection of student expectation, department expectation and competition for available spots, and student choice is where the choice begins.10 Previous studies have suggested that medical students’ choice of subspecialty is essential to the maintenance of an adequate medical workforce and a balanced development of the medical system.11 12 However, the influencing factors underlying students’ subspecialty choice have not been systemically reviewed. Recent changes in the training and practice environment may influence medical students’ career choice.13 Additionally, the variability in preferences over time and in students’ attitudes towards career choices can further complicate this assessment. For example, a study in the UK indicated that half of the medical students made a definitive subspecialty choice during their first year of medical school.14 However, students were prone to changing their subspecialty preference during medical school and internship.15 Notably, students may also reject certain subspecialties during their medical school training, even those they have previously seriously considered.16 Therefore, identifying the factors that influence students’ choice of subspecialty will enable a better understanding of the current shortage/overload of physicians in specific fields and contribute to policy-building and decision-making to improve the training and recruitment of students in the future.
We thus conducted a systematic review and a meta-analysis to investigate the influencing factors and the extent of their influence on the choice of subspecialty training among medical students. More specifically, we focused on the following questions. First, can we gain a better understanding of students’ preferences for medical specialty according to the primary influencing factor? Second, do the subgroups according to world region and survey years examined in this study differ significantly with regard to the weight that students place on the identified influencing factor?
Methods
We developed a review protocol (registration number: PROSPERO CRD42017053781) prior to commencing the study. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines was used to ensure the reporting quality of this review (see online supplementary figure S1).17
bmjopen-2018-022097supp001.pdf (2.1MB, pdf)
Search strategy and study eligibility
We performed a literature search in June 2018 using the Cochrane Library, Medline, Web of Science, CNKI and ERIC databases without language restrictions. Articles were screened by title, abstract and reference list, and by correspondence with study investigators. Potentially relevant papers were first identified by reviewing the titles and abstracts, and the full text of each retrieved article was then assessed. A detailed example of search strategy for Medline/PubMed is shown in online supplementary methods S1. Studies were included if they were systematic review or cross-sectional studies, reported data on medical students, were published in peer-reviewed journals and used a validated method to assess the extent of their influence (EOI) on the choice of subspecialty, such as paediatric gastroenterology and vascular surgery, or its corresponding specialty, such as paediatrics and surgery. Because of the differences between medical education systems in the world, the medical students we recruited include the students in medical school, internship, residency training and fellowship, students who are about to make a specialty choice and students who have just made a specialty choice. A guide to medical specialty, available at https://www.abms.org/member-boards/specialty-subspecialty-certificates/, was used to identify the medical specialty and subspecialty of our research. We also conducted an additional search using OpenGrey. However, no additional articles were further included. All searches were performed using Google chrome (V.54.0.2840).
Data extraction and quality assessment
Each article was reviewed by two trained investigators (YY and JL) and the following information was independently extracted from each selected article using a standardised form: study design, geographic location, years of survey, journal, sample size, average age of the participants, the number and percentage of male participants and the influencing factors and the extent of their influence. A third investigator was consulted if disagreements occurred. Each study may involve one or several influencing factors. An 11-item checklist which was recommended by Agency for Healthcare Research and Quality (AHRQ), used for cross-sectional studies,18 available at https://www.ncbi.nlm.nih.gov/books/NBK35156/, was used to assess the quality of the studies. All discrepancies were resolved via discussion and consensus.
Statistical analysis
As considerable heterogeneity was expected because of the multiple sources of variances, a random effects meta-analysis model was used to estimate the influencing factors and the extent of their influence.19 Between-study heterogeneity was assessed using the Cochran’s Q-test, and was quantified with the I2 statistic, which was calculated to describe the percentage of total variation caused by heterogeneity across studies, with ≥50% indicating considerable heterogeneity.20 21 Potential sources of heterogeneity were identified using meta-regression.22 Four categorical covariates were defined as potential sources of heterogeneity by examining the studies conducted in the USA versus the studies conducted in other countries, the studies conducted before 2010 versus those conducted after 2010, the studies concerning subspecialty only versus those that were not specific to a subspecialty, and the studies with a sample size <200 versus the studies with a sample size ≥200. Subgroup analyses were performed for each factor in the studies in developed countries versus developing countries and studies conducted before 2010 versus after 2010. The EOI value of competencies in developing countries was not statistically significant (81.21% [95% CI 75.27% to 86.51%], p=0.1436), and no studies on the influence of student debt in developing countries were found. The Q-test based on the analysis of variance was used to compare the subgroups, with a significance threshold of 5%.23 The influence of individual studies on the overall EOI value was explored by serially excluding each study in a sensitivity analysis. Publication bias was investigated using a funnel plot test and Egger’s test.24 25 Fill and trim approach, which imputes estimates from hypothetical negative unpublished reports,26 was also used to investigate the publication bias if the Egger’s test was significant. All analyses were performed using R (V.3.3.1, The R Foundation, Vienna, Austria). The statistical tests were two-sided with a significance threshold of p<0.05.
Patient and public involvement
Patients and the public were not involved in development of the research question and outcome measures, nor the study design. The study does not involve patient recruitment, and patients were not involved in conduct of the study. We plan to liaise closely with patients, special interest groups and charities in the dissemination of our results in printed and electronic media.
Results
Study characteristics
Seventy-five cross-sectional studies involving a total of 882 209 individuals that were published between January 1977 and May 2018 were included in the present research (table 1). Thirty-four studies were conducted in North America, twenty-four in Europe, seven in Asia, five in Oceania, three in Africa and two in South America. The median number of participants per study was 243 (range 37–29 227). Fourteen studies included students who had already selected subspecialties, whereas 61 did not. The influencing factors were ranked according to the frequency of occurrence and each factor was identified when at least five papers were available describing it. The influencing factors for subspecialty choice were then classified according to 17 aspects, including academic interests, controllable lifestyle or flexible work schedule (defined as flexibility that allows physicians to control the number of hours devoted to practising the specialty), competencies, patient service orientation, medical teachers or mentors, career opportunities, workload or working hours (characterised by the physician’s time spent on professional responsibilities), income, prestige, length of training, advice from others (advice from family, friends and other students), student debt, experience with the subject, working environment, personality, gender and job security. Personality and gender are common factors that affect the choice of subspecialty among medical students, but most of the relevant literature has not reported on the extent of these factors’ influence. Moreover, the funnel plots were clearly asymmetrical with regard to experience with the subject, the working environment and job variety, indicating the existence of publication bias. Thus, the analysis of the remaining 12 influencing factors were shown in this paper. Studies assessed for influencing factors using questionnaires validated to medical students asking the extent of certain factors the studies investigated. Quality assessment scores for the included studies are listed in table 1. None of the studies received a point for the second AHRQ quality indicator, which requires studies to list the inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications, since no comparison studies were referenced in the analysed articles. For the remaining 10 criteria, 6 studies received nine points, 8 studies received eight points, 17 studies received seven points, 33 studies received six points, 9 studies received 5 points and 2 studies received four points (scores for individual studies are presented in online supplementary table S1).
Table 1.
Selected characteristics of the 75 studies included in this systematic review and meta-analysis
| First author, year | Country | Survey years | Sample size | Average age | Men, No. (%) | Scores |
| Smith et al,43 2015 | UK | 2012 | 2978 | NR | NR | 6 |
| Cochran et al,44 2005 | USA | 2002 | 408 | 27.2 | 214 (52.45) | 5 |
| Hauer et al,45 2008 | USA | 2007 | 1177 | NR | NR | 6 |
| Johnson et al,46 2012 | USA | 2012 | 622 | NR | NR | 6 |
| Kiolbassa et al,47 2011 | Germany | 2010 | 1114 | 24.1 | 408 (36.62) | 5 |
| Klingensmith et al,48 2015 | USA | 2013 | 792 | NR | 539 (68.06) | 6 |
| Lee et al,49 2012 | USA | 2012 | 100 | NR | 58 (58) | 7 |
| Macdonald et al,50 2012 | New Zealand | 2011 | 134 | NR | 79 (58.96) | 7 |
| Parsa et al,39 2010 | Iran | 2006–2007 | 137 | 27.34 | 49 (35.77) | 7 |
| Paiva et al,51 1982 | USA | 1982 | 144 | NR | NR | 6 |
| Ni Chroinin et al,52 2013 | UK | 2009–2011 | 274 | NR | 112 (40.89) | 7 |
| Newton et al,34 2005 | USA | 1998–2004 | 1258 | NR | 642 (51.03) | 8 |
| Rogers et al,53 1990 | USA | 1989 | 266 | NR | 205 (77.07) | 6 |
| Abendroth et al,54 2014 | Germany | 2007–2012 | 45 | NR | 14 (31) | 7 |
| Alawad et al,55 2015 | USA | 2010–2011 | 45 | NR | 36 (80) | 8 |
| Azizzadeh et al,56 2003 | USA | 2002 | 130 | NR | NR | 6 |
| Celenza et al,57 2012 | Australia | 2009 | 216 | NR | 121 (56.02) | 8 |
| Dolan-Evans et al,58 2014 | Australia | 2013 | 419 | NR | 215 (51.31) | 8 |
| Boyd et al,59 2009 | USA | 2005–2006 | 5848 | NR | 2982 (50.99) | 8 |
| Egerton et al,60 1985 | Ireland | 1977–1981 | 134 | 30 | 82 (61.19) | 6 |
| Diderichsen et al,61 2013 | Sweden | 2006–2009 | 372 | 27 | 157 (42.20) | 6 |
| Ferrari et al,62 2013 | Italy, UK | 2009–2011 | 45 | 25 | NR | 9 |
| Freire et al,63 2011 | Brazil | 2006–2008 | 290 | 23 | 102 (35.17) | 7 |
| Buddeberg-Fischer et al,64 2006 | Switzerland | 2001–2003 | 522 | 31.1 | 241 (46.17) | 9 |
| Dorsey et al,65 2005 | USA | 2003 | 11 029 | NR | 4964 (45.01) | 6 |
| Ekenze et al,66 2013 | Nigeria | 2009–2010 | 96 | 25.9 | NR | 7 |
| Barikani et al,67 2012 | Australia | 2008–2009 | 49 | 21.7 | NR | 6 |
| Bittaye et al,68 2012 | Gambia | 2011 | 106 | 24.1 | 48 (45.28) | 6 |
| Bonura et al,69 2016 | USA | 2015 | 590 | NR | 321 (54.40) | 9 |
| Al-Fouzan et al,70 2012 | Kuwait | 2011–2012 | 144 | NR | NR | 7 |
| AlKot et al,71 2015 | Egypt | 2013 | 451 | 21.8 | NR | 7 |
| Borges et al,72 2009 | USA | 2001–2005 | 341 | NR | NR | 5 |
| Budd et al,73 2011 | UK | 2011 | 870 | 22 | NR | 7 |
| Corrigan et al,74 2007 | Ireland | 2007 | 222 | NR | 142 (63.96) | 7 |
| Davis et al,75 2016 | UK | 2016 | 173 | NR | 76 (43.93) | 7 |
| Deutsch et al,76 2015 | Germany | 2011 | 659 | 27.9 | NR | 8 |
| Gardner et al,77 2014 | Australia | 1993–2005 | 631 | NR | NR | 7 |
| Dias et al,78 2013 | UK | 2013 | 495 | NR | 438 (88.48) | 5 |
| Goltz et al,79 2013 | USA | 2012 | 102 | 24.5 | 34 (33.33) | 6 |
| Gupta et al,80 2013 | India | 2013 | 243 | NR | 179 (73.36) | 6 |
| Hanzlick et al,81 2008 | USA | 2006 | 161 | NR | NR | 6 |
| Harris et al,82 2005 | USA | 1991–2002 | 104 | NR | 53 (50.96) | 6 |
| Hauer et al,83 2008 | USA | 2008 | 80 | NR | NR | 6 |
| Labiris et al,84 2014 | Greece | 2014 | 111 | 23.6 | 55 (49.54) | 6 |
| Lambert et al,85 2008 | UK | 2007 | 17 393 | NR | NR | 6 |
| Shah et al,86 2012 | USA | 2011 | 892 | NR | NR | 6 |
| Lefevre et al,87 2010 | USA | 2008 | 1555 | NR | 589 (37.88) | 6 |
| Vicente et al,88 2013 | Chile | 2013 | 30 | NR | NR | 6 |
| Wiesenfeld et al,892014 | Canada | 2013 | 60 | NR | NR | 7 |
| Lam et al,90 2016 | Hong Kong | 2015 | 228 | 23 | NR | 9 |
| Hartung et al,91 2005 | USA | 2004 | 192 | 20.59 | 74 (38.54) | 4 |
| Girasek et al,92 2011 | Hungary | 2011 | 536 | NR | NR | 5 |
| Zuccato et al,93 2015 | Canada | 2012 | 37 | NR | 24 (65) | 6 |
| Wilbanks et al,94 2015 | USA | 2011–2013 | 29 227 | NR | 15 164 (51.99) | 9 |
| West et al,95 2009 | USA | 2005–2007 | 14 890 | NR | 8700 (58.43) | 6 |
| Watmough et al,96 2007 | UK | 2005 | 116 | NR | 66 (56.90) | 4 |
| Thakur et al,97 2001 | USA | 2001 | 56 | NR | 53 (95) | 8 |
| Scott et al,98 2011 | Canada | 2002–2004 | 1542 | NR | NR | 6 |
| Schnuth et al,99 2003 | USA | 2002 | 203 | NR | 72 (53.47) | 6 |
| Richards et al,100 2009 | UK | 2009 | 150 | NR | 108 (72.00) | 5 |
| Reed et al,101 2009 | USA | 2008 | 2022 | NR | 1354 (66.96) | 9 |
| de Souza et al,102 2015 | Portugal | 2012 | 1303 | NR | NR | 7 |
| Pikoulis et al,103 2010 | Greece | 2006–2007 | 87 | NR | NR | 6 |
| Ozer et al,104 2015 | Turkey | 2013 | 98 | 27.7 | 26 (26.53) | 6 |
| Noble et al,105 2004 | Canada | 2004 | 21 296 | NR | NR | 8 |
| Noble et al,106 2010 | Canada | 2007 | 120 | NR | NR | 5 |
| Newton et al,34 2005 | USA | 2004 | 1286 | NR | NR | 6 |
| Moore et al,107 2012 | USA | 2011 | 337 | 26 | 179 (53.12) | 6 |
| Momen et al,108 2015 | Iran | 2014–2015 | 38 | 35.6 | 11 (29) | 6 |
| Mehmood et al,109 2012 | Saudi Arabia | 2012 | 550 | NR | 348 (63.27) | 6 |
| Loriot et al,110 2010 | France | 2007 | 44 | NR | 17 (39) | 7 |
| Lefevre et al,111 2010 | France | 2008 | 522 | 23.8 | 198 (37.93) | 7 |
| Vo et al,112 2017 | Canada | 2017 | 90 | 22.5 | 52 (57.78) | 5 |
| Grasreiner et al,113 2018 | Germany | 2014–2016 | 181 | 24 | 33 (18.10) | 6 |
| Alkhannen et al,114 2018 | Saudi Arabia | 2017 | 436 | NA | 250 (57.00) | 5 |
Footnotes, scores: quality score of the AHRQ scale.
Primary analysis
A meta-analysis was performed on the 12 influencing factors (table 2): academic interests (see online supplementary figure S2), competencies (see online supplementary figure S3), controllable lifestyle or flexible work schedule (see online supplementary figure S4), patient service orientation (see online supplementary figure S5), medical teachers or mentors (see online supplementary figure S6), career opportunities (see online supplementary figure S7), workload or working hours (see online supplementary figure S8), income (see online supplementary figure S9), length of training (see online supplementary figure S10), prestige (see online supplementary figure S11), advice from others (see online supplementary figure S12) and student debt (see online supplementary figure S13). All the factors were significant with evidence of between-study heterogeneity (p<0.0001). A sensitivity analysis, in which the meta-analysis was serially repeated after the exclusion of each study, demonstrated that no individual study affected the overall extent of a factor’s influence.
Table 2.
Meta-analyses of the factors influencing medical students’ choice of subspecialty
| Factor | No. of studies | Total no. of participants | EOI value (%) | 95 CI% of extent of influence value | Cochran’s Q | I2 (%) | τ2 | P value | |
| Lower | Upper | ||||||||
| Academic interests | 38 | 82 366 | 75.29 | 66.93 | 82.11 | 14 719.76 | 99.70 | 1.60 | <0.0001 |
| Competencies | 17 | 76 515 | 55.15 | 33.63 | 74.90 | 23 572.74 | 99.90 | 3.44 | <0.0001 |
| Controllable lifestyle or flexible work schedule | 44 | 1 01 001 | 53.00 | 47.90 | 58.03 | 8624.46 | 99.50 | 0.45 | <0.0001 |
| Patient service orientation | 37 | 46 572 | 50.04 | 44.65 | 55.43 | 2668.79 | 98.70 | 0.41 | <0.0001 |
| Medical teachers or mentors | 32 | 85 071 | 46.93 | 37.77 | 56.30 | 15 216.32 | 99.80 | 1.14 | <0.0001 |
| Career opportunities | 38 | 81 923 | 44.00 | 32.26 | 48.78 | 13 553.20 | 99.70 | 1.15 | <0.0001 |
| Workload or working hours | 20 | 22 051 | 37.99 | 29.59 | 47.19 | 584.81 | 98.30 | 0.69 | <0.0001 |
| Income | 50 | 1 09 791 | 34.70 | 28.36 | 41.62 | 16 952.48 | 99.70 | 1.09 | <0.0001 |
| Length of training | 18 | 42 046 | 32.30 | 27.61 | 37.37 | 917.21 | 98.10 | 0.20 | <0.0001 |
| Prestige | 26 | 30 629 | 31.17 | 26.32 | 37.69 | 1464.67 | 98.30 | 0.52 | <0.0001 |
| Advice from others | 18 | 82 692 | 28.24 | 22.26 | 34.23 | 7679.73 | 99.80 | 0.02 | <0.0001 |
| Student debt | 8 | 38 917 | 15.33 | 10.96 | 21.03 | 574.81 | 98.80 | 0.27 | <0.0001 |
Meta-regression and subgroup analysis
We performed meta-regression to identify the potential sources of heterogeneity using common instructions when at least five studies were available and at least two studies were in each comparator subgroup (table 3). Some of the heterogeneities observed among the 12 factors can be partially explained by country, survey years, specialty and sample size.
Table 3.
Meta-regression of the extent of influence value stratified by study-level characteristics
| Factor | Estimate | 95 CI% of estimate | P value | |
| Lower | Upper | |||
| Academic interests | ||||
| Country | −0.2314 | −1.1575 | 0.6946 | 0.6302 |
| Survey years | 0.3811 | −0.3580 | 1.1202 | 0.2711 |
| Specialty | −0.4892 | −1.5345 | 0.5562 | 0.4008 |
| Sample size | 0.2362 | −0.5488 | 1.0212 | 0.6537 |
| Competencies | ||||
| Country | 0.6946 | −1.1461 | 0.8938 | 0.8376 |
| Survey years | −1.0418 | −2.0950 | 0.0114 | 0.0151 |
| Specialty | 0.0904 | −1.5786 | 1.7594 | 0.9398 |
| Sample size | −0.5720 | −1.8606 | 0.7166 | 0.5823 |
| Controllable lifestyle or flexible work schedule | ||||
| Country | −0.1261 | −1.1461 | 0.8938 | 0.9614 |
| Survey years | −0.0001 | −0.4052 | 0.4051 | 0.9822 |
| Specialty | −0.8989 | −1.4979 | −0.3000 | 0.0035 |
| Sample size | −0.0518 | −0.4396 | 0.3361 | 0.7203 |
| Patient service orientation | ||||
| Country | −0.6238 | −1.3118 | 0.0642 | 0.0833 |
| Survey years | −0.0414 | −0.6912 | 0.6083 | 0.8524 |
| Specialty | −1.5982 | −2.5227 | −0.6737 | 0.0010 |
| Sample size | −0.1157 | −0.7473 | 0.5159 | 0.6358 |
| Medical teachers or mentors | ||||
| Country | 0.7395 | 0.3117 | 1.1674 | 0.0007 |
| Survey years | 0.1133 | −0.3580 | 0.5845 | 0.6376 |
| Specialty | 0.0605 | −0.4441 | 0.5652 | 0.8141 |
| Sample size | −0.1202 | −0.5567 | 0.3163 | 0.5894 |
| Career opportunities | ||||
| Country | 0.1075 | −0.7030 | 0.9179 | 0.5828 |
| Survey years | 0.3284 | −0.3913 | 1.0480 | 0.7546 |
| Specialty | −0.9292 | −1.8015 | −0.0570 | 0.0077 |
| Sample size | 0.3654 | 0.1156 | 1.5478 | 0.0081 |
| Workload or working hours | ||||
| Country | −0.4535 | −1.5086 | 0.6016 | 0.3981 |
| Survey years | 0.4624 | −0.5417 | 1.4665 | 0.3922 |
| Specialty | −0.9878 | −2.1727 | 0.1972 | 0.1070 |
| Sample size | 0.0982 | −0.8589 | 1.0553 | 0.8205 |
| Income | ||||
| Country | 0.1058 | −0.4665 | 0.6781 | 0.7390 |
| Survey years | 0.0999 | −0.4379 | 0.6377 | 0.8774 |
| Specialty | −0.6457 | −1.3267 | 0.0352 | 0.0480 |
| Sample size | 0.0523 | −0.4826 | 0.5872 | 0.6786 |
| Length of training | ||||
| Country | −0.1559 | −1.2782 | 0.9664 | 0.7854 |
| Survey years | −0.2158 | −1.4089 | 0.9772 | 0.7229 |
| Specialty | 0.3959 | −0.9585 | 1.7502 | 0.5667 |
| Sample size | 0.1565 | −0.6631 | 0.9761 | 0.7082 |
| Prestige | ||||
| Country | −0.3346 | −1.0799 | 0.4106 | 0.3485 |
| Survey years | −0.4513 | −1.1378 | 0.2352 | 0.0950 |
| Specialty | −1.0112 | −1.8980 | −0.1244 | 0.0172 |
| Sample size | 0.0355 | −0.6013 | 0.6723 | 0.5214 |
| Advice from others | ||||
| Country | −0.0097 | −0.0722 | 0.0529 | 0.9328 |
| Survey years | −0.0861 | −0.1471 | −0.0251 | 0.0057 |
| Specialty | −0.2017 | −0.2790 | −0.1244 | <0.0001 |
| Sample size | 0.2125 | 0.1309 | 0.2941 | <0.0001 |
| Student debt | ||||
| Country | 2.7853 | 2.0544 | 3.5162 | 0.0001 |
| Survey years | −0.1567 | −0.6707 | 0.3573 | 0.5502 |
| Sample size | −0.5248 | −1.0108 | −0.0388 | 0.0343 |
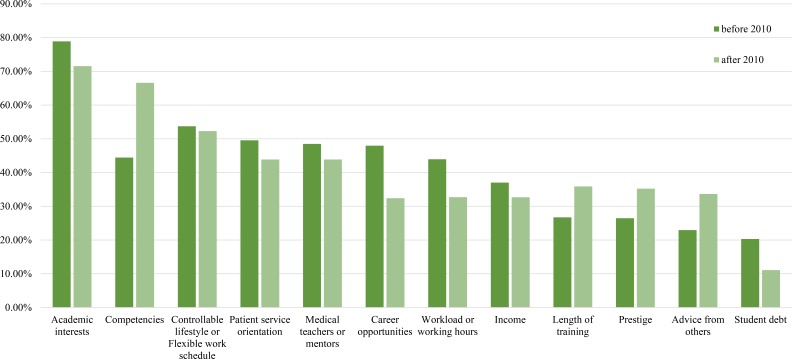
EOI values were further analysed by subgroup (see online supplementary table S2) according to world region (figure 1) and survey year (figure 2). The EOI value of academic interests in developed countries was higher than that in developing countries (79.66% [95% CI 70.73% to 86.39% vs 60.41% [95% CI 43.44% to 75.19%]; Q=3.51, p=0.02). Conversely, a lower EOI value of prestige was found in studies conducted in developed countries than in developing countries (23.96% [95% CI 19.20% to 29.47%] vs 47.65% [95% CI 34.41% to 61.24%]; Q=4.71, p=0.01). No statistically significant subgroup differences in the EOI values of the other influencing factors were noted between developed countries and developing countries. In addition, no statistically significant differences in the EOI values of the influencing factors were observed when subgroup analysis was performed by survey year.
Figure 1.
Bar graph of the meta-analyses of the factors influencing medical students’ choice of subspecialty stratified by region.
Figure 2.
Bar graph of the meta-analyses of the factors influencing medical students’ choice of subspecialty stratified by survey year.
Assessment of publication bias
We generated a funnel plot with proportion as the abscissa and SE as the ordinate. A visual inspection of the funnel plots revealed minimal asymmetry among the various influencing factors (see online supplementary figure S14), and the results were concentrated in the narrow upper part of the graph. There was evidence of small study effect in the meta-analysis of ‘patient service orientation’ (Egger’s test, p=0.02). However, the trim-and-fill method showed the publication bias-corrected estimate remained statistically significant (63.79%, 95% CI 58.20% to 69.04%).
Discussion
Implications
This systematic review and meta-analysis involved 75 studies with 882 209 medical students. Twelve influencing factors were analysed. These factors can be classified into two categories: economic factors and non-economic factors. We found that the EOI of the economic factors, including income (34.70%) and student debt (15.33%), may not depend on the region’s level of economic development. However, income remained a major influencing factor in the process of choosing a specialty or subspecialty. In the USA, 15% of full-time family medicine physicians earned less than $100 000 in 2004, which is significantly less than the income earned by invasive cardiologists (median income=$427 815), neurosurgeons (median income=$211 094) and orthopaedists (median income=$335 646).27 This economic inequality made family medicine less attractive to medical school graduates.28 Benefits such as health insurance and tuition reimbursement have been shown to be the most common economic incentives used to attract applicants.29
The non-economic factors can be divided into individual factors, specialty-related factors and others. First, individual factors, including academic interest and competencies, have a considerable impact on students’ subspecialty choice, with EOI values of 75.29% and 55.15%, respectively. In addition, in the subgroup analysis, although academic interests were less influential in developing countries than in developed countries (79.66% [95% CI 70.73% to 86.39% vs 60.41% [95% CI 43.44% to 75.19%]; Q=3.51, p=0.02), they were still the most influential of the 12 factors regardless of regional economic level. These findings indicate that subspecialties with a shortage of manpower may attract more students by increasing students’ interests and improving the quality of education. Previous studies indicated that early specialty exposure in medical education may arouse students’ academic interest and improve their clinical competence.28 30 For example, an elective extracurricular programme designed to facilitate early contact with family medicine physicians was found to significantly improve students’ interest and clinical skills, especially communication skills, in family medicine.31 Furthermore, dispelling myths and espousing the positive aspects of a discipline may provide a better understanding of certain specialties; this approach could also be effective in increasing students’ academic interest.32 For instance, family medicine is often considered a discipline that requires less professional skills and knowledge. This misconception demotivates students from choosing family medicine as their future career specialty, and this trend may eventually lead to a shortage of family physicians.32 Eliminating such prejudices may help students pay greater attention to the areas in short supply and restore their interests in other specialties.
Second, the specialty-related factors included controllable lifestyle/flexible work schedule (EOI of 53.00%), career opportunities (EOI of 44.00%), workload (EOI of 37.99%) and training length (EOI of 32.30%). Of these factors, lifestyle varied between different areas. Additionally, although certain specialties, such as general surgery, seem to have an adequate number of surgeons on a per capita basis in the USA, there is still a poor geographic distribution within the surgical workforce according to the type of surgical practice.33 The inflexible lifestyle is a common reason that students perceive surgery to be less attractive.33 Reorganisation of expected work hours within shared practices and the increased use of physician extenders and technologies such as electronic medical records may give physicians more flexibility in work schedules.34 Moreover, providing promotion opportunities and shortening the length of training are possible strategies to recruit new staff in subspecialties that require a long period of postgraduate residency training, such as neurosurgery.35
Finally, other factors such as service orientation (EOI of 50.74%), medical teachers or mentors (EOI of 46.93%), prestige (EOI of 34.68%) and advice from others (EOI of 28.24%) also contribute to the decision-making process of medical students. For example, the desire to care for patients with end-stage diseases contributed to the decision to enter palliative medicine in 86% of the medical students.7 Additionally, exposure to mentors in a particular clinical field such as internal medicine has been strongly associated with medical students’ choice of clinical field.36 Moreover, improving the occupational prestige of areas such as family medicine, pathology and radiology may help reshape the distribution of the workforce.30 37 38
In our study, several findings are especially noteworthy. First, interest was far more important than income in deciding subspecialty. In our study, interest was the top-ranked influencing factor (EOI of 75.29%) of subspecialty choice, while income was ranked lower (EOI of 34.70%). This finding argues against the possible default belief that raising physician’s wages alone could solve the uneven distribution of clinicians among subspecialties. Our findings highlight that cultivating and stimulating students’ professional interests may help improve the maldistribution of medical resources in a more efficient and cost-saving manner.
Second, improving abilities in a certain subspecialty of interest can greatly affect medical students’ professional choice. In our study, competencies ranked second in influence, which may reflect the impact of admission conditions on students’ choice of subspecialty. Hence, to reduce the risk that students are restricted to the subspecialty of their interest due to a lack of personal skills, medical education should focus more on enhancing students’ personal competencies in addition to their academic interests.
Third, balancing medical resources is a complex process in practical terms, as the influencing factors are not mutually exclusive. The shortage of physicians in certain subspecialties may increase physician workload, resulting in less time for teaching. Hence, the quality of teaching cannot be guaranteed, and students may tend to avoid choosing these subspecialties, thus worsening the imbalance in the medical workforce. Additionally, some of the 12 factors identified are not amenable to practical interventions. For example, prestige cannot be immediately increased using interventional strategies.37 Overall, effective strategies must be multipronged and incorporate several different aspects, and maldistribution in the workforce should not be tackled through a simple adjustment of one influencing factor.
Interpretations of the results of this meta-analysis
Our meta-regression stratified by the study-level characteristics found that country, survey years, subspecialty and sample size may contribute to the heterogeneity between studies. There was no significant difference in the sensitivity analysis, which indicated that the results of the meta-analysis were convincing. The funnel plots and Egger’s tests revealed that most of the publication bias was small (p>0.05), except for the meta-analysis of ‘patient service orientation’. Moreover, the majority of the studies collected in the database were from developed countries rather than developing countries.
Limitations
Several limitations should be considered when interpreting the findings of this study. First, the students involved in our study included medical students at different stages of their medical education. Students’ perception about different subspecialties may change during medical training until the students applies for specialty training. For example, compared with an intern, a freshman student may place greater emphasis on income and prestige when considering a career choice.39 A subgroup analysis stratified by the stages of medical education and a secondary meta-analysis of longitudinal studies may better reflect changes in influencing factors and the extent of their influence over time. Second, our meta-analysis summarised the data from different geographic regions around the world, and the general conclusions may not be appropriate to guide policy development in each region. Enhanced effort is needed to develop specific intervention strategies according to the specific economic level, religious beliefs, healthcare system, educational system and endemic diseases of different countries and regions. Subgroup analysis stratified by organisational and medical training factors would provide more information of the factors influencing subspecialty choice among medical students. Third, the surveys in the various studies were also conducted using different methods. Most of the questionnaires used a Likert scale. Therefore, when we converted the results to a percentage representing the extent of a factor’s influence, the Likert scale items were treated as interval data.40–42 Consequently, there may have been differences in the conversion process. Finally, the analysis relied on aggregated published data. A multicentre prospective study would provide more accurate estimate of the influencing factors and the extent of their influence on medical students’ choice of subspecialty.
Conclusion
In conclusion, this systematic review and meta-analysis provided a summary evaluation of 12 influencing factors and the extent of their influence on the choice of subspecialty training among medical students. Understanding students’ attitudes toward their subspecialty decision-making process could provide the basis for developing strategies to increase the attractiveness of subspecialties experiencing a shortage of manpower, thereby balancing the distribution of medical recourses.
Supplementary Material
Footnotes
Contributors: HL contributed to the conceptualising and design of the study and to research funding, coordinated the research and oversaw the project. YY, JL and XW contributed to data collection and interpretation, and to data analysis. JW, YZ, CC and WL contributed to the design of the study. All authors contributed to the drafting and revision of the paper and approved the final manuscript for publication.
Funding: The principal investigator of this study (Haotian Lin) is currently supported by National key R & D project (2018YFC010302), the Key Research Plan for the National Natural Science Foundation of China Cultivation Project (91546101), the National Natural Science Foundation of China (81770967), the Fundamental Research Funds for the Central Universities (16ykjc28), the Guangdong Provincial Natural Science Foundation for Distinguished Young Scholars of China (2014A030306030), the Guangdong Province Universities and Colleges Youth Pearl River Scholar Funded Scheme (2016), the Clinical Research and Translational Medical Center of Pediatric Cataract in Guangzhou City (201505032017516) and Ministry of Science and Technology of China Grants (2015CB964600).
Disclaimer: These sponsors and funding organisations had no role in the design or performance of this study.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Extracted data are available upon request to the corresponding author.
Patient consent for publication: Not required.
References
- 1. Zurn P, Dal Poz MR, Stilwell B, et al. Imbalance in the health workforce. Hum Resour Health 2004;2:13 10.1186/1478-4491-2-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Diallo K, Zurn P, Gupta N, et al. Monitoring and evaluation of human resources for health: an international perspective. Hum Resour Health 2003;1:3 10.1186/1478-4491-1-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson GF, Hussey PS. Population aging: a comparison among industrialized countries. Health Aff 2000;19:191–203. 10.1377/hlthaff.19.3.191 [DOI] [PubMed] [Google Scholar]
- 4. Hobbs FDR, Bankhead C, Mukhtar T, et al. Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007-14. Lancet 2016;387:2323–30. 10.1016/S0140-6736(16)00620-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reeve J, Blakeman T, Freeman GK, et al. Generalist solutions to complex problems: generating practice-based evidence--the example of managing multi-morbidity. BMC Fam Pract 2013;14:112 10.1186/1471-2296-14-112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bodenheimer T. Primary care--will it survive? N Engl J Med 2006;355:861–4. 10.1056/NEJMp068155 [DOI] [PubMed] [Google Scholar]
- 7. Legrand SB, Heintz JB. Palliative medicine fellowship: a study of resident choices. J Pain Symptom Manage 2012;43:558–68. 10.1016/j.jpainsymman.2011.04.018 [DOI] [PubMed] [Google Scholar]
- 8. Kim YY, Kim UN, Kim YS, et al. Factors associated with the specialty choice of Korean medical students: a cross-sectional survey. Hum Resour Health 2016;14:8 10.1186/s12960-016-0141-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McNally SA. Competition ratios for different specialties and the effect of gender and immigration status. J R Soc Med 2008;101:489–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Reed VA, Jernstedt GC, Reber ES. Understanding and improving medical student specialty choice: a synthesis of the literature using decision theory as a referent. Teach Learn Med 2001;13:117–29. 10.1207/S15328015TLM1302_7 [DOI] [PubMed] [Google Scholar]
- 11. Al-Ansari SS, Khafagy MA. Factors affecting the choice of health specialty by medical graduates. Journal of Family & Community Medicine 2015;13:119–23. [PMC free article] [PubMed] [Google Scholar]
- 12. Leduc N, Vanasse A, Scott I, et al. The career decision-making process of medical students and residents and the choice of specialty and practice location: how does Postgraduate Medical Education fit in? 2011.
- 13. Delamothe T. Modernising medical careers: final report. BMJ 2008;336:54–5. 10.1136/bmj.39455.401817.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Goldacre MJ, Laxton L, Harrison EM, et al. Early career choices and successful career progression in surgery in the UK: prospective cohort studies. BMC Surg 2010;10:11 10.1186/1471-2482-10-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Weissman C, Zisk-Rony RY, Schroeder JE, et al. Medical specialty considerations by medical students early in their clinical experience. Isr J Health Policy Res 2012;1:13 10.1186/2045-4015-1-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jackson C, Ball J, Hirsh W, et al. Informing choices: the need for career advice in medical training. Cambridge: National institute for careers Education and Counseling, 2003. [Google Scholar]
- 17. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 18. Rostom A, Dube C, Cranney A, et al. Celiac disease. Evid Rep Technol Assess 2004;104:1–6. [PMC free article] [PubMed] [Google Scholar]
- 19. Borenstein M, Hedges LV, Higgins JP, et al. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 2010;1:97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 20. Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 22. Sterne JA, Jüni P, Schulz KF, et al. Statistical methods for assessing the influence of study characteristics on treatment effects in ’meta-epidemiological' research. Stat Med 2002;21:1513–24. 10.1002/sim.1184 [DOI] [PubMed] [Google Scholar]
- 23. Borenstein M, Hedges LV, Higgins J, et al. Criticisms of meta‐analysis. Introduction to meta-analysis 2009:377–87. [Google Scholar]
- 24. Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 2001;54:1046–55. [DOI] [PubMed] [Google Scholar]
- 26. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000;56:455–63. 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- 27. Bodenheimer T, Berenson RA, Rudolf P. The primary care-specialty income gap: why it matters. Ann Intern Med 2007;146:301–6. 10.7326/0003-4819-146-4-200702200-00011 [DOI] [PubMed] [Google Scholar]
- 28. Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff 2010;29:799–805. 10.1377/hlthaff.2010.0026 [DOI] [PubMed] [Google Scholar]
- 29. Association AH. The hospital workforce shortage: Immediate and future. Trend Watch 2001;3:1–8. [Google Scholar]
- 30. Compton MT, Frank E, Elon L, et al. Changes in U.S. medical students' specialty interests over the course of medical school. J Gen Intern Med 2008;23:1095–100. 10.1007/s11606-008-0579-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Indyk D, Deen D, Fornari A, et al. The influence of longitudinal mentoring on medical student selection of primary care residencies. BMC Med Educ 2011;11:27 10.1186/1472-6920-11-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gill H, McLeod S, Duerksen K, et al. Factors influencing medical students' choice of family medicine: effects of rural versus urban background. Can Fam Physician 2012;58:E649–E57. [PMC free article] [PubMed] [Google Scholar]
- 33. Richardson JD. Workforce and lifestyle issues in general surgery training and practice. Arch Surg 2002;137:515–20. 10.1001/archsurg.137.5.515 [DOI] [PubMed] [Google Scholar]
- 34. Newton DA, Grayson MS, Thompson LF. The variable influence of lifestyle and income on medical students' career specialty choices: data from two U.S. medical schools, 1998-2004. Acad Med 2005;80:809–14. 10.1097/00001888-200509000-00005 [DOI] [PubMed] [Google Scholar]
- 35. Orrico K. Ensuring an adequate neurosurgical workforce for 21st century. Surgeons AAoN 2012. [Google Scholar]
- 36. Wright S, Wong A, Newill C. The impact of role models on medical students. J Gen Intern Med 1997;12:53–6. 10.1007/s11606-006-0007-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Glazer GM, Ruiz-Wibbelsmann JA. Decades of perceived mediocrity: prestige and radiology. Radiology 2011;260:311–6. 10.1148/radiol.11110596 [DOI] [PubMed] [Google Scholar]
- 38. Schwartzbaum AM, McGrath JH, Rothman RA. The perception of prestige differences among medical subspecialities. Soc Sci Med 1973;7:365–71. 10.1016/0037-7856(73)90045-0 [DOI] [PubMed] [Google Scholar]
- 39. Parsa S, Aghazadeh A, Nejatisafa AA, et al. Freshmen versus interns' specialty interests. Arch Iran Med 2010;13:509–15. doi:010136/AIM.0011 [PubMed] [Google Scholar]
- 40. Komorita SS. Attitude content, intensity, and the neutral point on a likert scale. J Soc Psychol 1963;61:327–34. 10.1080/00224545.1963.9919489 [DOI] [PubMed] [Google Scholar]
- 41. Baggaley AR, Hull AL. The effect of nonlinear transformations on a Likert scale. Eval Health Prof 1983;6:483–91. 10.1177/016327878300600408 [DOI] [PubMed] [Google Scholar]
- 42. Norman G. Likert scales, levels of measurement and the "laws" of statistics. Adv Health Sci Educ Theory Pract 2010;15:625–32. 10.1007/s10459-010-9222-y [DOI] [PubMed] [Google Scholar]
- 43. Smith F, Lambert TW, Goldacre MJ. Factors influencing junior doctors' choices of future specialty: trends over time and demographics based on results from UK national surveys. J R Soc Med 2015;108:396–405. 10.1177/0141076815599674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cochran A, Melby S, Neumayer LA. An Internet-based survey of factors influencing medical student selection of a general surgery career. Am J Surg 2005;189:742–6. 10.1016/j.amjsurg.2005.03.019 [DOI] [PubMed] [Google Scholar]
- 45. Hauer KE, Durning SJ, Kernan WN, et al. Factors associated with medical students' career choices regarding internal medicine. JAMA 2008;300:1154–64. 10.1001/jama.300.10.1154 [DOI] [PubMed] [Google Scholar]
- 46. Johnson AL, Sharma J, Chinchilli VM, et al. Why do medical students choose orthopaedics as a career? J Bone Joint Surg Am 2012;94:e78–1. 10.2106/JBJS.K.00826 [DOI] [PubMed] [Google Scholar]
- 47. Kiolbassa K, Miksch A, Hermann K, et al. Becoming a general practitioner--which factors have most impact on career choice of medical students? BMC Fam Pract 2011;12:7 10.1186/1471-2296-12-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Klingensmith ME, Cogbill TH, Luchette F, et al. Factors influencing the decision of surgery residency graduates to pursue general surgery practice versus fellowship. Ann Surg 2015;262:449–55. 10.1097/SLA.0000000000001435 [DOI] [PubMed] [Google Scholar]
- 49. Lee JY, Kerbl DC, McDougall EM, et al. Medical students pursuing surgical fields have no greater innate motor dexterity than those pursuing nonsurgical fields. J Surg Educ 2012;69:360–3. 10.1016/j.jsurg.2011.11.005 [DOI] [PubMed] [Google Scholar]
- 50. Macdonald C, Cawood T. Factors influencing career decisions in internal medicine. Intern Med J 2012;42:918–23. 10.1111/j.1445-5994.2012.02793.x [DOI] [PubMed] [Google Scholar]
- 51. Paiva RE, Vu NV, Verhulst SJ. The effect of clinical experiences in medical school on specialty choice decisions. J Med Educ 1982;57:666–74. 10.1097/00001888-198209000-00002 [DOI] [PubMed] [Google Scholar]
- 52. Ní Chróinín D, Cronin E, Cullen W, et al. Would you be a geriatrician? Student career preferences and attitudes to a career in geriatric medicine. Age Ageing 2013;42:654–7. 10.1093/ageing/aft093 [DOI] [PubMed] [Google Scholar]
- 53. Rogers LQ, Fincher RM, Lewis LA. Factors influencing medical students to choose primary care or non-primary care specialties. Acad Med 1990;65(9 Suppl):S47–8. 10.1097/00001888-199009000-00038 [DOI] [PubMed] [Google Scholar]
- 54. Abendroth J, Schnell U, Lichte T, et al. Motives of former interns in general practice for speciality-choice--results of a cross-sectional study among graduates 2007 to 2012. GMS Z Med Ausbild 2014;31 10.3205/zma000903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Alawad AA, Khan WS, Abdelrazig YM, et al. Factors considered by undergraduate medical students when selecting specialty of their future careers. Pan Afr Med J 2015;20:6 10.11604/pamj.2015.20.102.4715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Azizzadeh A, McCollum CH, Miller CC, et al. Factors influencing career choice among medical students interested in surgery. Curr Surg 2003;60:210–3. 10.1016/S0149-7944(02)00679-7 [DOI] [PubMed] [Google Scholar]
- 57. Celenza A, Bharath J, Scop J. Improving the attractiveness of an emergency medicine career to medical students: An exploratory study. Emerg Med Australas 2012;24:625–33. 10.1111/j.1742-6723.2012.01607.x [DOI] [PubMed] [Google Scholar]
- 58. Dolan-Evans E, Rogers GD. Barriers for students pursuing a surgical career and where the Surgical Interest Association can intervene. ANZ J Surg 2014;84:406–11. 10.1111/ans.12521 [DOI] [PubMed] [Google Scholar]
- 59. Boyd JS, Clyne B, Reinert SE, et al. Emergency medicine career choice: a profile of factors and influences from the Association of American Medical Colleges (AAMC) graduation questionnaires. Acad Emerg Med 2009;16:544–9. 10.1111/j.1553-2712.2009.00385.x [DOI] [PubMed] [Google Scholar]
- 60. Egerton EA. Choice of career of doctors who graduated from Queen’s University, Belfast in 1977. Med Educ 1985;19:131–7. 10.1111/j.1365-2923.1985.tb01153.x [DOI] [PubMed] [Google Scholar]
- 61. Diderichsen S, Johansson EE, Verdonk P, et al. Few gender differences in specialty preferences and motivational factors: a cross-sectional Swedish study on last-year medical students. BMC Med Educ 2013;13:8 10.1186/1472-6920-13-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ferrari S, Reggianini C, Mattei G, et al. International study of student career choice in psychiatry (ISoSCCiP): results from Modena, Italy. Int Rev Psychiatry 2013;25:450–9. 10.3109/09540261.2013.804402 [DOI] [PubMed] [Google Scholar]
- 63. Freire MC, Jordao LM, de Paula Ferreira N, et al. Motivation towards career choice of Brazilian freshman students in a fifteen-year period. J Dent Educ 2011;75:115–21. [PubMed] [Google Scholar]
- 64. Buddeberg-Fischer B, Klaghofer R, Abel T, et al. Swiss residents' speciality choices--impact of gender, personality traits, career motivation and life goals. BMC Health Serv Res 2006;6:137 10.1186/1472-6963-6-137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Dorsey ER, Jarjoura D, Rutecki GW. The influence of controllable lifestyle and sex on the specialty choices of graduating U.S. medical students, 1996-2003. Acad Med 2005;80:791–6. 10.1097/00001888-200509000-00002 [DOI] [PubMed] [Google Scholar]
- 66. Ekenze SO, Ugwumba FO, Obi UM, et al. Undergraduate surgery clerkship and the choice of surgery as a career: perspective from a developing country. World J Surg 2013;37:2094–100. 10.1007/s00268-013-2073-y [DOI] [PubMed] [Google Scholar]
- 67. Barikani A, Afaghi M, Barikani F, et al. Perception of the medical students on their future career in Qazvin University of Medical Sciences. Glob J Health Sci 2012;4:176–80. 10.5539/gjhs.v4n4p176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Bittaye M, Odukogbe AT, Nyan O, et al. Medical students' choices of specialty in The Gambia: the need for career counseling. BMC Med Educ 2012;12:72 10.1186/1472-6920-12-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Bonura EM, Lee ES, Ramsey K, et al. Factors influencing internal medicine resident choice of infectious diseases or other specialties: a National Cross-sectional Study. Clin Infect Dis 2016;63:155–63. 10.1093/cid/ciw263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Al-Fouzan R, Al-Ajlan S, Marwan Y, et al. Factors affecting future specialty choice among medical students in Kuwait. Medical Education Online 2012;17:19587 10.3402/meo.v17i0.19587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. AlKot MM, Gouda MA, KhalafAllah MT, et al. Family Medicine in Egypt From Medical Students' Perspective: a Nationwide Survey. Teach Learn Med 2015;27:264–73. 10.1080/10401334.2015.1044654 [DOI] [PubMed] [Google Scholar]
- 72. Borges NJ, Manuel RS, Duffy RD, et al. Influences on specialty choice for students entering person-oriented and technique-oriented specialties. Med Teach 2009;31:1086–8. 10.3109/01421590903183787 [DOI] [PubMed] [Google Scholar]
- 73. Budd S, Kelley R, Day R, et al. Student attitudes to psychiatry and their clinical placements. Med Teach 2011;33:e586–e592. 10.3109/0142159X.2011.610836 [DOI] [PubMed] [Google Scholar]
- 74. Corrigan MA, Shields CJ, Redmond HP. Factors influencing surgical career choices and advancement in Ireland and Britain. World J Surg 2007;31:1921–9. 10.1007/s00268-007-9175-3 [DOI] [PubMed] [Google Scholar]
- 75. Davis CR, Trevatt AEJ, McGoldrick RB, et al. How to train plastic surgeons of the future. Journal of Plastic, Reconstructive & Aesthetic Surgery 2016;69:1134–40. 10.1016/j.bjps.2016.05.001 [DOI] [PubMed] [Google Scholar]
- 76. Deutsch T, Lippmann S, Frese T, et al. Who wants to become a general practitioner? Student and curriculum factors associated with choosing a GP career--a multivariable analysis with particular consideration of practice-orientated GP courses. Scand J Prim Health Care 2015;33:47–53. 10.3109/02813432.2015.1020661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Gardner SP, Roberts-Thomson KF. The effect of a change in selection procedures on students' motivation to study dentistry. Aust Dent J 2014;59:2–8. 10.1111/adj.12141 [DOI] [PubMed] [Google Scholar]
- 78. Dias MS, Sussman JS, Durham S, et al. Perceived benefits and barriers to a career in pediatric neurosurgery: a survey of neurosurgical residents. J Neurosurg Pediatr 2013;12:422–33. 10.3171/2013.7.PEDS12597 [DOI] [PubMed] [Google Scholar]
- 79. Goltz CJ, Bachusz RC, Mancini E, et al. Medical student career survey--vascular surgery awareness initiative. Ann Vasc Surg 2013;27:225–31. 10.1016/j.avsg.2012.02.012 [DOI] [PubMed] [Google Scholar]
- 80. Gupta NB, Khadilkar SV, Bangar SS, et al. Neurology as career option among postgraduate medical students. Ann Indian Acad Neurol 2013;16:478–82. 10.4103/0972-2327.120427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Hanzlick R, Prahlow JA, Denton S, et al. Selecting forensic pathology as a career: a survey of the past with an eye on the future. Am J Forensic Med Pathol 2008;29:114–22. 10.1097/PAF.0b013e318174f0a9 [DOI] [PubMed] [Google Scholar]
- 82. Harris MC, Marx J, Gallagher PR, et al. General vs subspecialty pediatrics: factors leading to residents' career decisions over a 12-year period. Arch Pediatr Adolesc Med 2005;159:212–6. 10.1001/archpedi.159.3.212 [DOI] [PubMed] [Google Scholar]
- 83. Hauer KE, Fagan MJ, Kernan W, et al. Internal medicine clerkship directors' perceptions about student interest in internal medicine careers. J Gen Intern Med 2008;23:1101–4. 10.1007/s11606-008-0640-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Labiris G, Vamvakerou V, Tsolakaki O, et al. Perceptions of Greek medical students regarding medical profession and the specialty selection process during the economic crisis years. Health Policy 2014;117:203–9. 10.1016/j.healthpol.2014.04.009 [DOI] [PubMed] [Google Scholar]
- 85. Lambert TW, Goldacre MJ, Bron AJ. Career choices for ophthalmology made by newly qualified doctors in the United Kingdom, 1974-2005. BMC Ophthalmol 2008;8:9 10.1186/1471-2415-8-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Shah HH, Jhaveri KD, Sparks MA, et al. Career choice selection and satisfaction among US adult nephrology fellows. Clin J Am Soc Nephrol 2012;7:1513–20. 10.2215/CJN.01620212 [DOI] [PubMed] [Google Scholar]
- 87. Lefevre JH, Roupret M, Kerneis S, et al. Career choices of medical students: a national survey of 1780 students. Med Educ 2010;44:603–12. 10.1111/j.1365-2923.2010.03707.x [DOI] [PubMed] [Google Scholar]
- 88. Vicente B, Rosel L. Challenges for psychiatric recruitment and training in Chile. Int Rev Psychiatry 2013;25:413–8. 10.3109/09540261.2013.822348 [DOI] [PubMed] [Google Scholar]
- 89. Wiesenfeld L, Abbey S, Takahashi SG, et al. Choosing psychiatry as a career: motivators and deterrents at a critical decision-making juncture. Can J Psychiatry 2014;59:450–4. 10.1177/070674371405900808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Lam CY, Cheung CS, Hui AS. Factors influencing the career interest of medical graduates in obstetrics and gynaecology in Hong Kong: a cross-sectional questionnaire survey. Hong Kong Med J 2016;22:138–43. 10.12809/hkmj154650 [DOI] [PubMed] [Google Scholar]
- 91. Hartung PJ, Taber BJ, Richard GV. The physician values in practice scale: construction and initial validation. Journal of Vocational Behavior 2005;67:309–20. 10.1016/j.jvb.2004.05.008 [DOI] [Google Scholar]
- 92. Girasek E, Molnár R, Eke E, et al. The medical career choice motivations — Results from a Hungarian study. Open Med 2011;6:502–9. 10.2478/s11536-011-0034-0 [DOI] [Google Scholar]
- 93. Zuccato JA, Kulkarni AV. The impact of early medical school surgical exposure on interest in neurosurgery. Can J Neurol Sci 2016;43:410–6. 10.1017/cjn.2015.332 [DOI] [PubMed] [Google Scholar]
- 94. Wilbanks L, Spollen J, Messias E. Factors Influencing Medical School Graduates Toward a Career in Psychiatry: analysis from the 2011-2013 Association of American Medical Colleges Graduation Questionnaire. Acad Psychiatry 2016;40:255–60. 10.1007/s40596-015-0287-z [DOI] [PubMed] [Google Scholar]
- 95. West CP, Drefahl MM, Popkave C, et al. Internal medicine resident self-report of factors associated with career decisions. J Gen Intern Med 2009;24:946–9. 10.1007/s11606-009-1039-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Watmough S, Taylor D, Ryland I. Using questionnaires to determine whether medical graduates' career choice is determined by undergraduate or postgraduate experiences. Med Teach 2007;29:830–2. 10.1080/01421590701551755 [DOI] [PubMed] [Google Scholar]
- 97. Thakur A, Fedorka P, Ko C, et al. Impact of mentor guidance in surgical career selection. J Pediatr Surg 2001;36:1802–4. 10.1053/jpsu.2001.28842 [DOI] [PubMed] [Google Scholar]
- 98. Scott I, Gowans M, Wright B, et al. Determinants of choosing a career in surgery. Med Teach 2011;33:1011–7. 10.3109/0142159X.2011.558533 [DOI] [PubMed] [Google Scholar]
- 99. Schnuth RL, Vasilenko P, Mavis B, et al. What influences medical students to pursue careers in obstetrics and gynecology? Am J Obstet Gynecol 2003;189:639–43. 10.1067/S0002-9378(03)00886-X [DOI] [PubMed] [Google Scholar]
- 100. Richards JM, Drummond R, Murray J, et al. What proportion of basic surgical trainees continue in a surgical career? A survey of the factors which are important in influencing career decisions. Surgeon 2009;7:270–5. 10.1016/S1479-666X(09)80003-6 [DOI] [PubMed] [Google Scholar]
- 101. Reed CE, Vaporciyan AA, Erikson C, et al. Factors dominating choice of surgical specialty. J Am Coll Surg 2010;210:319–24. 10.1016/j.jamcollsurg.2009.11.016 [DOI] [PubMed] [Google Scholar]
- 102. Correia Lima de Souza L, Mendonça VR, Garcia GB, et al. Medical specialty choice and related factors of brazilian medical students and recent doctors. PLoS One 2015;10:15 10.1371/journal.pone.0133585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Pikoulis E, Avgerinos ED, Pedeli X, et al. Medical students' perceptions on factors influencing a surgical career: the fate of general surgery in Greece. Surgery 2010;148:510–5. 10.1016/j.surg.2010.01.013 [DOI] [PubMed] [Google Scholar]
- 104. Ozer U, Ceri V, Carpar E, et al. Factors affecting the choice of psychiatry as a specialty and satisfaction among turkish psychiatry residents. Acad Psychiatry 2016;40:299–303. 10.1007/s40596-015-0346-5 [DOI] [PubMed] [Google Scholar]
- 105. Noble J, Hechter FJ, Karaiskos N, et al. Motivational factors and future life plans of orthodontic residents in the United States. Am J Orthod Dentofacial Orthop 2010;137:623–30. 10.1016/j.ajodo.2008.03.034 [DOI] [PubMed] [Google Scholar]
- 106. Noble J. Factors influencing career choice in ophthalmology. Can J Ophthalmol 2006;41:596–9. 10.1016/S0008-4182(06)80029-3 [DOI] [PubMed] [Google Scholar]
- 107. Moore HB, Moore PK, Grant AR, et al. Future of acute care surgery: a perspective from the next generation. J Trauma Acute Care Surg 2012;72:94–9. 10.1097/TA.0b013e31823b990a [DOI] [PubMed] [Google Scholar]
- 108. Momen AA, Shakurnia A. Factors influencing pediatric specialty choice among pediatric residents of ahvaz jundishapur university of medical sciences. International Journal of Pediatrics-Mashhad 2015;3:701–6. [Google Scholar]
- 109. Mehmood SI, Kumar A, Al-Binali A, et al. Specialty preferences: trends and perceptions among Saudi undergraduate medical students. Med Teach 2012;34:S51–60. 10.3109/0142159X.2012.656753 [DOI] [PubMed] [Google Scholar]
- 110. Loriot Y, Albiges-Sauvin L, Dionysopoulos D, et al. Why do residents choose the medical oncology specialty? Implications for future recruitment--results of the 2007 French Association of Residents in Oncology (AERIO) Survey. Ann Oncol 2010;21:161–5. 10.1093/annonc/mdp294 [DOI] [PubMed] [Google Scholar]
- 111. Lefèvre JH, Karila L, Kerneis S, et al. Motivation of French medical students to pursue surgical careers: results of national survey of 1742 students. J Visc Surg 2010;147:e181–6. 10.1016/j.jviscsurg.2010.08.004 [DOI] [PubMed] [Google Scholar]
- 112. Vo A, McLean L, McInnes MDF. Medical specialty preferences in early medical school training in Canada. Int J Med Educ 2017;8:400–6. 10.5116/ijme.59f4.3c15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Grasreiner D, Dahmen U, Settmacher U. Specialty preferences and influencing factors: a repeated cross-sectional survey of first- to sixth-year medical students in Jena, Germany. BMC Med Educ 2018;18:103 10.1186/s12909-018-1200-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Alkhaneen H, Alhusain F, Alshahri K, et al. Factors influencing medical students' choice of emergency medicine as a career specialty-a descriptive study of Saudi medical students. Int J Emerg Med 2018;11:14 10.1186/s12245-018-0174-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-022097supp001.pdf (2.1MB, pdf)