Abstract
Background
Risk of exacerbations in chronic obstructive pulmonary disease (COPD) associated with biomass smoke has not been well addressed, although biomass smoke is similar in composition to tobacco smoke.
Methods
To investigate whether the risk of exacerbations in COPD associated with biomass smoke differs from that in COPD associated with tobacco smoke, we recruited patients with COPD from two Korean multicenter prospective cohorts. In a multiple linear regression model, the standardized regression coefficient (β) of biomass smoke exposure ≥25 years was most similar to that (β′) of tobacco smoke exposure ≥10 pack-years (β = − 0.13 and β′ = − 0.14). We grouped patients with COPD into four categories based on the above cut-offs: Less Tobacco-Less Biomass, Less Tobacco-More Biomass, More Tobacco-Less Biomass, and More Tobacco-More Biomass. The main outcome was the incidence of moderate or severe exacerbations.
Results
Among 1033 patients with COPD, 107 were included in Less Tobacco-Less Biomass (mean age: 67 years, men: 67%), 40 in Less Tobacco-More Biomass (mean age: 70 years, men: 35%), 631 in More Tobacco-Less Biomass (mean age: 68 years, men: 98%), and 255 in More Tobacco-More Biomass (mean age: 69 years, men: 97%). The incidence rates of exacerbations were not significantly different between Less Tobacco-More Biomass and More Tobacco-Less Biomass (adjusted incidence rate ratio, 1.03; 95% confidence interval, 0.56–1.89; P = 0.921). No interaction between sex and tobacco and biomass smoke was observed. When propensity score matching with available covariates including age and sex was applied, a similar result was observed.
Conclusions
Patients with COPD associated with biomass smoke and those with COPD associated with tobacco smoke had a similar risk of exacerbations. This suggests that patients with COPD associated with biomass smoke should be treated actively.
Electronic supplementary material
The online version of this article (10.1186/s12890-019-0833-7) contains supplementary material, which is available to authorized users.
Keywords: Chronic obstructive pulmonary disease, Biomass smoke, Tobacco smoke, Exacerbation
Background
Biomass smoke exposure is an important risk factor for the development of chronic obstructive pulmonary disease (COPD), even though tobacco smoking is the most well-studied COPD risk factor [1–6]. The World Health Organization reported that more than 40% of the world’s population continues to depend on biomass fuels for cooking and heating, and indoor air pollution caused by these activities was responsible for 7.7% of the global mortality in 2012 [7]. Approximately 25% of premature deaths from COPD in low- and middle-income countries are due to exposure to biomass smoke exposure [8].
The clinical characteristics of COPD associated with biomass smoke are different from those associated with tobacco smoke. Patients with COPD associated with biomass smoke are predominantly women, and have worse symptoms and quality of life than do those with COPD associated with tobacco smoke [9, 10]. Recent studies have found phenotypic differences between COPD associated with either biomass or tobacco smoke exposure [10–12]. Biomass smoke exposure is associated with a small airway disease phenotype, whereas tobacco smoke exposure is associated with an emphysema phenotype.
However, only a few longitudinal studies have compared the outcomes between COPD associated with biomass smoke and tobacco smoke [13, 14], and no studies have investigated the risk of exacerbations in patients with COPD exposed to biomass smoke in a prospective study. Exacerbations of COPD are important outcomes in the management of COPD since they negatively impact the health status, hospital admissions and readmissions, disease progression, and mortality [1, 15]. Thus, we aimed to determine whether the risk of exacerbations in COPD associated with biomass smoke differs from that in COPD associated with tobacco smoke. We hypothesized that patients with COPD associated with biomass smoke would have a lower risk of exacerbations than those with COPD associated with tobacco smoke as the rate of FEV1 decline is slower in patients whose COPD was associated with biomass smoke than in those whose COPD was associated with tobacco smoke [14].
Methods
Patients
We recruited participants from two multicenter prospective cohorts in the Republic of Korea: the Korean Obstructive Lung Disease (KOLD) cohort, which comprises participants from 17 centers recruited since 2005 [16], and the Korean COPD Subgroup Study (KOCOSS; NCT02800499) cohort, which comprises participants from 45 centers recruited since 2011 [17]. Major exclusion criteria of the two cohort studies are patients with respiratory diseases other than obstructive lung disease (e.g., previous pulmonary resection, tuberculosis-destroyed lung, and bronchiectasis). All participants in the cohorts provided written informed consent. Participants were eligible for the current study if they were 40 years or older and had post-bronchodilator forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) less than 0.7. Participants with an unknown exposure history to tobacco and/or biomass fuel smoke were excluded. Participants who were followed up for less than 6 months and those who did not have baseline information were also excluded. The present study was approved by the institutional review board of the Seoul National University Hospital (H-1706-079-859) and was conducted in accordance with the tenets of the Declaration of Helsinki.
Definition of exposure groups
At a baseline visit, biomass fuel exposure was determined by using the same questions in both cohorts: “Have you ever burned firewood for cooking or heating by yourself for over a year in your lifetime? If yes, how many years have you burned firewood as fuel?” and “Have you ever used coal briquettes for cooking or heating by yourself for over a year in your lifetime? If yes, how many years have you used coal briquettes as fuel?” We defined the exposure years to biomass fuel smoke in this study as the sum of exposure years to firewood and coal briquettes. In the Republic of Korea, coal briquettes had been used as the major source of fuel for cooking and heating since the 1950s; however, they had been replaced by gas and liquid fuels from the early 1990s, and biomass fuel use is now negligible [18]. To find equivalents of exposure to tobacco and biomass smoke, we applied multiple linear regression in the 1031 cohort participants (mean age, 69 years; 934 men; 55 non-COPD) who were not currently exposed to tobacco and biomass smoke.
In the above equation, Y is post-bronchodilator FEV1/FVC (%) at a baseline visit; X1 is age (0 if age < 60 years and 1 if age ≥ 60 years); X2 is sex (0 if male and 1 if female); X3 is height (cm), X4 is tobacco smoke (0 if < m pack-years and 1 if ≥ m pack-years, where m is an integer); X5 is biomass smoke (0 if < n years and 1 if ≥ n years, where n is an integer); B0, are the intercept terms; B1, to B4, are regression coefficients; and ε, ε′ are the random error terms. The standardized regression coefficient [19] of B4 (β) and that of (β′) were most similar when m was 10 and n was 25 (β = − 0.13 and β′ = − 0.14) (Table 1). Therefore, the tobacco group (More Tobacco) was defined as one with ≥10 pack-years of tobacco smoke, and the biomass group (More Biomass) was defined as one with ≥25 exposure years to biomass smoke. We grouped patients with COPD into four categories based on the above cut-offs: Less Tobacco-Less Biomass, Less Tobrefacco-More Biomass, More Tobacco-Less Biomass, and More Tobacco-More Biomass.
Table 1.
The equivalents of pack-years of tobacco smoke and exposure years to biomass smoke*
| If biomass smoke < n years | If tobacco smoke < m pack-years | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Tobacco smoke (m), pack-years | Exposure to biomass smoke (n), years | B4 | SE | β | P value | SE | β′ | P value | |
| 10 | 10 | −4.22 | 1.79 | −0.12 | 0.019 | −0.15 | 1.87 | −0.01 | 0.937 |
| 15 | −3.48 | 1.48 | −0.10 | 0.019 | 0.37 | 1.83 | 0.02 | 0.840 | |
| 20 | −3.51 | 1.44 | −0.11 | 0.015 | −0.14 | 1.83 | −0.01 | 0.941 | |
| 25 | −4.20 | 1.32 | −0.13 | 0.002 | −3.83 | 1.92 | −0.14 | 0.048 | |
| 30 | −4.12 | 1.30 | −0.13 | 0.002 | −2.24 | 2.00 | −0.08 | 0.263 | |
| 20 | 10 | −4.36 | 1.43 | −0.15 | 0.003 | 0.51 | 1.59 | 0.02 | 0.749 |
| 15 | −3.60 | 1.24 | −0.13 | 0.004 | 0.74 | 1.58 | 0.03 | 0.639 | |
| 20 | −3.62 | 1.21 | −0.13 | 0.003 | 0.38 | 1.60 | 0.02 | 0.811 | |
| 25 | −4.39 | 1.11 | −0.15 | < 0.001 | −3.25 | 1.68 | −0.12 | 0.054 | |
| 30 | −4.01 | 1.09 | −0.14 | < 0.001 | −1.38 | 1.73 | −0.05 | 0.424 | |
*Multiple linear regression adjusting for age (< 60 vs. ≥60 years), sex, and height (cm). The standardized regression coefficient of B4 (β) and that of (β′) were most similar when m was 10 and n was 25 (β = − 0.13 and β′ = − 0.14)
B4 unstandardized regression coefficient for tobacco smoke, unstandardized regression coefficient for biomass smoke, β standardized regression coefficient of B4, β′ standardized regression coefficient of , SE standard error
Measurement of variables and outcomes
All participants underwent detailed interviews by study physicians or trained nurses covering an exposure history to tobacco and biomass smoke; a history of exacerbations during the previous year; and symptom scores, including those for the modified Medical Research Council (mMRC) Questionnaire [20], St. George’s respiratory questionnaire for COPD (SGRQ-C) [21], and COPD assessment test (CAT) [22]. Participants underwent pre- and post-bronchodilator spirometry at baseline. After a baseline visit, participants were followed up every 3 months (the KOLD cohort) or 6 months (the KOCOSS cohort). The use of drugs, including long-acting muscarinic antagonists, long-acting β-agonists, and inhaled corticosteroids at enrollment and the medication possession ratios of those drugs during the follow-up period were recorded.
The main outcome was the incidence of moderate or severe exacerbations. An exacerbation was defined as moderate when any worsening of respiratory symptoms led to treatment with systemic corticosteroids, antibiotics, or both, and severe if it led to hospital admission or emergency department visits [15, 23].
Statistical analysis
Clinical characteristics were compared using independent samples t-tests or one-way analysis of variance for continuous variables. For categorical variables, comparisons were made using either χ2 tests or Fisher’s exact tests. The incidence rates of moderate or severe exacerbations were compared in the four exposure groups by using negative binomial regression models. The time to the first moderate or severe exacerbation was analyzed using the Kaplan–Meier method. Thereafter, we repeated the analyses after propensity score matching. Multivariable logistic regression was used to compute the propensity score for the Less Tobacco-More Biomass group by using available covariates. The Less Tobacco-More Biomass group was matched (1:3 ratio) with the More Tobacco-Less Biomass group by using the nearest neighbor method within a caliper of 0.3 of the propensity score. We also performed sensitivity analysis with four groups of patients (never exposed to tobacco or biomass smoke, exposed to biomass smoke only, exposed to tobacco smoke only, and exposed to both biomass and tobacco smoke). P values less than 0.05 were considered significant. Statistical analyses were performed using Stata statistical software (Version 14.2; StataCorp, College Station, TX).
Results
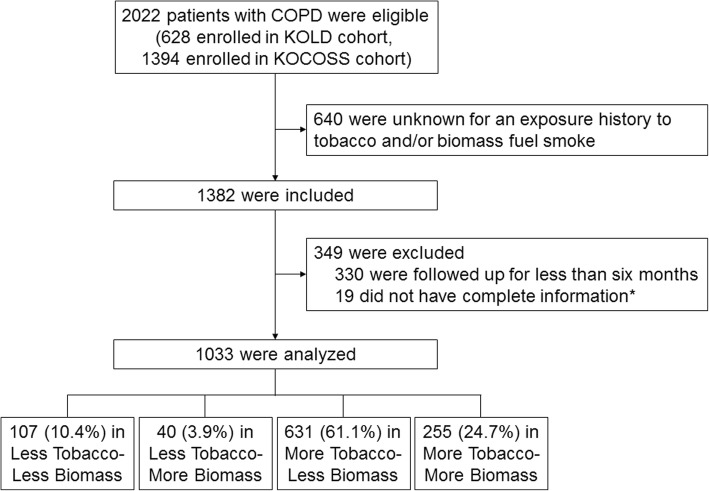
Among the 1033 patients with COPD who were followed up for a mean duration of 3.0 years, 107 (10.4%) were included in the Less Tobacco-Less Biomass group, 40 (3.9%) in the Less Tobacco-More Biomass group, 631 (61.1%) in the More Tobacco-Less Biomass group, and 255 (24.7%) in the More Tobacco-More Biomass group (Fig. 1). Characteristics of the study patients according to exposure are presented in Table 2. Patients in the Less Tobacco-More Biomass group were more likely to be women (65.0 vs. 2.2%; P < 0.001) and older (69.9 ± 6.5 vs. 67.5 ± 7.6 years; P = 0.061) than those in the More Tobacco-Less Biomass group (see Additional file 1: Table S1). Although the mMRC dyspnea scores were similar in the four groups, comprehensive symptom assessment questionnaires showed that the Less Tobacco-More Biomass group had significantly more symptoms. Post-bronchodilator FEV1% predicted was not significantly different across the groups (Table 2).
Fig. 1.
Flowchart illustrating patient selection. *Body mass index, % predicted post-bronchodilator forced expiratory volume in 1 s (FEV1), exacerbation history during the previous year, the modified Medical Research Council dyspnea score, and the St. George’s respiratory questionnaire for COPD score at baseline
COPD chronic obstructive pulmonary disease, KOCOSS Korean COPD Subgroup Study, KOLD Korean Obstructive Lung Disease.
Table 2.
Baseline characteristics of the study patients*
| Less Tobacco-Less Biomass (n = 107) | Less Tobacco-More Biomass (n = 40) | More Tobacco-Less Biomass (n = 631) | More Tobacco-More Biomass (n = 255) | P value | |
|---|---|---|---|---|---|
| Age, years | 67.1 ± 9.3 | 69.9 ± 6.5 | 67.5 ± 7.6 | 69.2 ± 7.1 | 0.007 |
| Age | 0.004 | ||||
| < 60 years | 23 (21.5) | 2 (5.0) | 99 (15.7) | 24 (9.4) | |
| ≥ 60 years | 84 (78.5) | 38 (95.0) | 532 (84.3) | 231 (90.6) | |
| Sex | < 0.001 | ||||
| Male | 72 (67.3) | 14 (35.0) | 617 (97.8) | 248 (97.3) | |
| Female | 35 (32.7) | 26 (65.0) | 14 (2.2) | 7 (2.8) | |
| BMI, kg/m2 | 23.7 ± 3.3 | 23.7 ± 3.3 | 23.0 ± 3.1 | 22.5 ± 3.4 | 0.005 |
| Tobacco smoking | < 0.001 | ||||
| Never-smoker | 70 (65.4) | 31 (77.5) | 0 (0.0) | 0 (0.0) | |
| Former smoker | 32 (29.9) | 9 (22.5) | 447 (70.8) | 165 (64.7) | |
| Current smoker | 5 (4.7) | 0 (0.0) | 184 (29.2) | 90 (35.3) | |
| Tobacco smoke, pack-years | 1.7 ± 2.9 | 0.8 ± 2.1 | 45.8 ± 24.9 | 47.1 ± 25.4 | < 0.001 |
| Biomass smoke, years | 8.9 ± 7.9 | 35.5 ± 8.3 | 5.9 ± 7.5 | 37.9 ± 11.2 | < 0.001 |
| Exacerbation during the previous year | 0.164 | ||||
| No | 79 (73.8) | 25 (62.5) | 485 (76.9) | 199 (78.0) | |
| Yes | 28 (26.2) | 15 (37.5) | 146 (23.1) | 56 (22.0) | |
| mMRC dyspnea score | 1.4 ± 0.9 | 1.7 ± 0.9 | 1.5 ± 0.9 | 1.6 ± 0.9 | 0.083 |
| mMRC dyspnea score | 0.455 | ||||
| < 2 | 63 (58.9) | 19 (47.5) | 367 (58.2) | 139 (54.5) | |
| ≥ 2 | 44 (41.1) | 21 (52.5) | 264 (41.8) | 116 (45.5) | |
| SGRQ-C total score | 32.8 ± 18.3 | 44.4 ± 21.7 | 32.1 ± 18.1 | 36.8 ± 18.3 | < 0.001 |
| SGRQ-C total score | 0.001 | ||||
| < 25 | 44 (41.1) | 9 (22.5) | 269 (42.6) | 77 (30.2) | |
| ≥ 25 | 63 (58.9) | 31 (77.5) | 362 (57.4) | 178 (69.8) | |
| CAT score (n = 780) | 13.9 ± 7.9 | 18.7 ± 10.0 | 14.0 ± 7.8 | 16.2 ± 8.0 | < 0.001 |
| CAT score | < 0.001 | ||||
| < 10 | 30 (28.0) | 6 (15.0) | 156 (24.7) | 30 (11.8) | |
| ≥ 10 | 63 (58.9) | 23 (57.5) | 339 (53.7) | 133 (52.2) | |
| Unknown | 14 (13.1) | 11 (27.5) | 136 (21.6) | 92 (36.1) | |
| Post-bronchodilator FEV1, % predicted | 59.3 ± 18.6 | 63.4 ± 24.2 | 60.3 ± 17.7 | 60.0 ± 19.4 | 0.685 |
| Post-bronchodilator FVC, % predicted | 80.8 ± 17.1 | 84.3 ± 20.7 | 88.6 ± 17.2 | 85.5 ± 18.9 | < 0.001 |
| Post-bronchodilator FEV1/FVC, % | 53.4 ± 10.3 | 53.1 ± 12.5 | 48.3 ± 11.3 | 49.2 ± 11.3 | < 0.001 |
| Bronchodilator response (FEV1, %) | 6.4 ± 11.4 | 8.0 ± 13.7 | 8.5 ± 10.9 | 8.6 ± 9.7 | 0.270 |
| Blood eosinophil, % (n = 868) | 3.6 ± 4.4 | 2.4 ± 1.7 | 3.6 ± 3.4 | 3.7 ± 4.0 | 0.196 |
| Blood eosinophil | < 0.001 | ||||
| ≤ 5% | 68 (63.6) | 35 (87.5) | 409 (64.8) | 180 (70.6) | |
| > 5% | 19 (17.8) | 2 (5.0) | 101 (16.0) | 54 (21.2) | |
| Unknown | 20 (18.7) | 3 (7.5) | 121 (19.2) | 21 (8.2) | |
| Use of LAMA at enrollment | 57 (53.3) | 16 (40.0) | 329 (52.1) | 113 (44.3) | 0.090 |
| Use of LABA at enrollment | 54 (50.5) | 26 (65.0) | 329 (52.1) | 144 (56.5) | 0.273 |
| Use of ICS at enrollment | 38 (35.5) | 22 (55.0) | 263 (41.7) | 114 (44.7) | 0.147 |
*Data are presented as mean ± SD or No. (%)
BMI Body mass index, CAT COPD Assessment Test, COPD chronic obstructive pulmonary disease, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity, ICS inhaled corticosteroid, LABA long-acting β-agonist, LAMA long-acting muscarinic antagonist, mMRC modified Medical Research Council, SGRQ-C St. George’s Respiratory Questionnaire for COPD
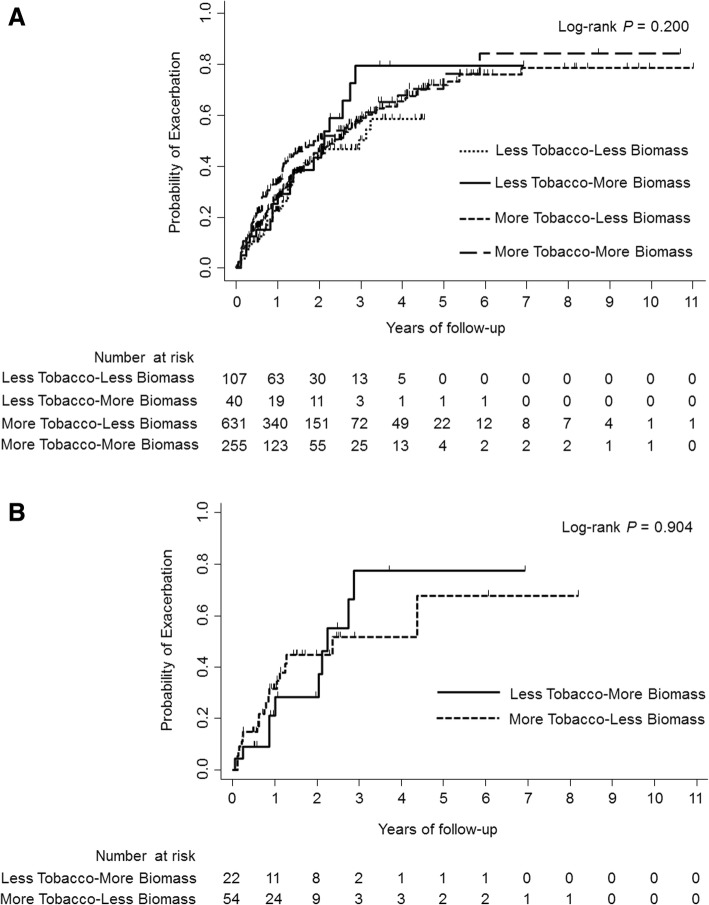
When adjusted for age, sex, body mass index, SGRQ-C total score (< 25 vs. ≥25), exacerbation history during the previous year (yes vs. no), and post-bronchodilator FEV1% predicted, the incidence rates of moderate or severe exacerbations did not differ by groups (Table 3). The adjusted incidence rates were 0.72 (95% confidence interval [CI], 0.31–1.13) in the Less Tobacco-More Biomass group and 0.70 (95% CI, 0.60–0.79) in the More Tobacco-Less Biomass group, resulting in an incidence rate ratio of 1.03 (95% CI, 0.56–1.89; P = 0.921). No interaction between sex and tobacco smoke (< 10 vs. ≥10 pack-years) and biomass smoke (< 25 vs. ≥25 years) was observed (data not shown). In addition, the time to the first moderate or severe exacerbation was not significantly different between the four groups (log-rank P = 0.200) (Fig. 2a).
Table 3.
Adjusted incidence rates of moderate or severe exacerbations by exposure groups
| Adjusted incidence rate* (95% CI) | Adjusted incidence rate ratio* (95% CI) | P value | |
|---|---|---|---|
| More Tobacco-Less Biomass | 0.70 (0.60–0.79) | 1 | |
| Less Tobacco-Less Biomass | 0.51 (0.33–0.68) | 0.73 (0.50–1.05) | 0.092 |
| Less Tobacco-More Biomass | 0.72 (0.31–1.13) | 1.03 (0.56–1.89) | 0.921 |
| More Tobacco-More Biomass | 0.67 (0.54–0.80) | 0.96 (0.76–1.20) | 0.698 |
*Adjusted for age, sex, body mass index, St. George’s Respiratory Questionnaire for COPD (SGRQ-C) total score (< 25 vs. ≥25), exacerbation history during the previous year (yes vs. no), and post-bronchodilator forced expiratory volume in 1 s (FEV1)% predicted
CI confidence interval
Fig. 2.
Kaplan–Meier curves illustrating the time to the first moderate or severe exacerbation in four exposure groups (a) and in two exposure groups after propensity score matching (b)
After propensity score matching, each of 16 participants in the Less Tobacco-More Biomass group was matched with three controls in the More Tobacco-Less Biomass group, whereas each of six participants in the Less Tobacco-More Biomass group was matched with a control in the More Tobacco-Less Biomass group. The clinical characteristics of these matched groups were comparable (see Additional file 1: Figure S1 and Table S1). The incidence rates of exacerbations were not significantly different between the groups (incidence rate ratio, 1.18; 95% CI, 0.53–2.59; P = 0.687) (Table 4). A similar result was observed in the time to the first exacerbation (log-rank P = 0.904) (Fig. 2b).
Table 4.
Incidence rates of moderate or severe exacerbations in the propensity score-matched cohort
| Incidence rate (95% CI) | Incidence rate ratio (95% CI) | P value | ||
|---|---|---|---|---|
| Model 1* | More Tobacco-Less Biomass | 0.58 (0.33–0.83) | 1 | |
| Less Tobacco-More Biomass | 0.68 (0.23–1.13) | 1.18 (0.53–2.59) | 0.687 | |
| Model 2† | More Tobacco-Less Biomass | 0.58 (0.32–0.83) | 1 | |
| Less Tobacco-More Biomass | 0.69 (0.21–1.17) | 1.19 (0.51–2.78) | 0.685 | |
| Model 3‡ | More Tobacco-Less Biomass | 0.56 (0.32–0.79) | 1 | |
| Less Tobacco-More Biomass | 0.65 (0.22–1.07) | 1.16 (0.52–2.58) | 0.721 | |
*Model 1: unadjusted
†Model 2: adjusted for sex
‡Model 3: adjusted for sex, and medication possession ratios of long-acting muscarinic antagonists, long-acting β-agonists, and inhaled corticosteroids during the follow-up period as continuous variables
CI confidence interval
We performed sensitivity analysis with 22 patients who were never exposed to tobacco or biomass smoke and 79 exposed to biomass smoke only and 322 exposed to tobacco smoke only and 610 exposed to both biomass and tobacco smoke. We found no difference in the rates of exacerbations between COPD associated with biomass smoke and that associated with tobacco smoke (see Additional file 1: Table S2). We also applied a propensity score-matched analysis. Forty participants exposed to biomass smoke only were matched with 40 participants exposed to tobacco smoke only. The incidence rates of exacerbations were not significantly different between the groups (incidence rate ratio, 1.05; 95% CI, 0.55–1.98; P = 0.890; see Additional file 1: Table S3).
Discussion
The present study investigated whether the risk of exacerbations differs by exposure to biomass or tobacco smoke. We found no difference in the rates of exacerbations between COPD associated with biomass smoke and that associated with tobacco smoke, even in an analysis with propensity score matching.
When an individual with significant exposures to risk factors, such as tobacco smoke, indoor/outdoor air pollution, and occupational dusts and chemicals, presents appropriate symptoms, a diagnosis of COPD is made on the basis of spirometry, which confirms the presence of persistent airflow limitation [1]. Tobacco smoke continues to be recognized as the most commonly encountered risk factor for COPD. In most clinical studies including large trials, a history of tobacco smoke exposure has been accepted as a major inclusion criterion to define COPD [24–27]. The pathogenesis and pathophysiology of COPD caused by tobacco smoke have been well-studied, and in vivo and in vitro models of cigarette smoke-induced COPD have been widely used [28]. Biomass smoke exposure is now being identified as an important risk factor for persistent airflow limitation. However, translational and clinical research on COPD associated with biomass smoke has been limited, especially from the perspective of comparing exposure to biomass smoke and to tobacco smoke [29]. In a Mexican cohort, the rate of FEV1 decline was slower and more homogeneous in patients whose COPD was associated with biomass smoke than in those whose COPD was associated with tobacco smoke [14]. In the same cohort, no differences were found in survival between the two groups after adjusting for confounders [13]. However, the risk of exacerbations, another important COPD outcome, in the patients exposed to biomass smoke has not been well addressed as a few studies investigated it retrospectively [13, 30].
To our knowledge, ours is the first prospective study comparing the risk of exacerbations between COPD associated with biomass smoke and that associated with tobacco smoke. We recruited 1033 patients with COPD and grouped them into four categories based on the presence of risk factors, biomass and/or tobacco smoke. Patients with COPD exposed to biomass smoke were predominantly women and older, and presented more symptoms even with a similar degree of airflow limitation than did those exposed to tobacco smoke. After adjusting for confounding factors, the rates of moderate or severe exacerbations did not differ by exposure groups. When propensity score matching was applied to compare participants with either biomass or tobacco smoke, a similar result was observed. Biomass and tobacco smoke shares common harmful components [31], and a recent experimental study showed that biomass fuel smoke activated similar pathogenic processes observed in cigarette smoke exposure in both human airway epithelial cells and mice [32]. A considerable amount of evidence, from in vivo and in vitro studies, shows biomass smoke enhances lung inflammation and impairs pulmonary anti-microbial defense, which could lead to exacerbations [31].
Our finding is consistent with that of previous retrospective analyses reporting no differences in exacerbations between patients with COPD associated with tobacco or biomass smoke [13, 30]. On combining our finding with that of the previous cohort study, which demonstrated similar mortality between patients with COPD exposed to the two different smokes [13], we found that clinical and radiological differences between COPD associated with biomass and tobacco smoke may not lead to significant differences in clinical outcomes. Therefore, clinicians should suspect a diagnosis of COPD in any patient with a history of exposure to biomass fuel smoke who has dyspnea, chronic cough, or sputum production, and any patient with COPD associated with biomass smoke should be treated actively.
As the cumulative amounts of exposure to biomass smoke, which are comparable to those of exposure to tobacco smoke, are unknown, the group exposed to biomass smoke has been defined using arbitrary cut-off values of exposure duration in years, especially when an individual’s exposure intensity to biomass smoke is unavailable [30, 33]. Cumulative exposure to biomass smoke expressed as hour-years, which is the product of the number of years cooking with biomass fuels multiplied by the average number of hours spent daily in the kitchen [34], was unavailable in our cohort. Instead, we used the standardized regression coefficient to determine equivalents of the exposure duration (years) to biomass smoke and pack-years of tobacco smoke. The exposure duration to biomass smoke was defined as the sum of exposure years to firewood and coal briquettes. We applied multiple linear regression predicting values of the dependent variable, post-bronchodilator FEV1/FVC (%) at a baseline visit, in the 1031 cohort participants including non-COPD in a cross-sectional design. Upon repeated modeling with variable values, we found that the standardized regression coefficients for each exposure were most similar when the exposure duration to biomass smoke was 25 years and a history of tobacco smoke was 10 pack-years (Table 1). However, there are several limitations in these estimates. First, we thought that a multiple linear regression model predicting values of the dependent variable, not post-bronchodilator FEV1/FVC (%) but diagnosis of COPD, would be ideal for determining comparable cut-off values of exposures. While there were only 5% participants without COPD in the KOLD and KOCOSS cohorts, other prospective cohorts utilizing the same questionnaire on a history of exposure to biomass smoke were not available in Korea. Second, our regression model using the spirometric value as a dependent variable is still limited by the small number of participants without COPD. Third, questions assessing biomass exposure were focused on cooking or heating. However, it is possible that a responder was not a cook, but still had been exposed to biomass smoke. Fourth, the exposure duration to biomass smoke was defined as the simple sum of exposure years to firewood and coal briquettes without weights although the risk of development of COPD was greater for wood burners than for coal users [3]. Fifth, exposure to tobacco and/or biomass smoke under the cut-off values may cause COPD. Sixth, exposure data on other risk factors for COPD, such as indoor/outdoor air pollution and occupational dusts, were lacking in our study.
Sex selection bias is a commonly encountered issue in COPD research associated with biomass smoke [11]. The present study also has the limitation as patients with COPD associated with biomass smoke were predominantly women. To mitigate the bias, we applied a propensity score-matched analysis with available covariates including sex. This approach resulted in the findings consistent with the overall results on COPD exacerbation rates. In addition, no interaction was observed between sex and tobacco and biomass smoke both before and after matching. However, although controversies still arise, women can be more susceptible of the effects of tobacco and biomass smoke then men, leading to more severe disease for the equivalent quantity of smoke [1, 35].
The current study has several limitations, such as its observational design and the small number of patients with COPD associated with biomass smoke. There was a possibility of recall bias as the data regarding exposure to biomass and tobacco smoke were collected at the time of or after the diagnosis of COPD. Although we included participants aged 40 years or older, COPD associated with biomass smoke could be prevalent in younger adults [36].
Conclusions
In conclusion, this study shows that patients with COPD associated with biomass smoke and those with COPD associated with tobacco smoke have a similar risk of exacerbations. This suggests that any patient with COPD associated with biomass smoke should be treated actively. In addition, management strategies should not be confined to pharmacologic treatment, and should be complemented by interventions, such as improvement of kitchen ventilation, introduction of non-polluting cooking stoves, and use of clean fuels, to reduce exposure to smoke from biomass fuels.
Additional file
Online supplement (DOC). Figure S1. Histograms showing propensity score distribution. Table S1. Baseline characteristics of the study patients before and after propensity score matching. Table S2. Adjusted incidence rates of moderate or severe exacerbations by exposure groups (sensitivity analysis). Table S3. Incidence rates of moderate or severe exacerbations in the propensity score-matched cohort (sensitivity analysis) (DOC 117 kb)
Acknowledgements
We thank all investigators of the KOLD and KOCOSS for its contribution on patient enrollment and data acquisition. The KOLD was built with the support of a grant of the Korea Healthcare Technology R&D Project, Ministry for Health and Welfare, Republic of Korea (A102065).
Funding
None declared.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CAT
COPD assessment test
- COPD
chronic obstructive pulmonary disease
- KOCOSS
Korean COPD Subgroup Study
- KOLD
Korean Obstructive Lung Disease
- mMRC
modified Medical Research Council
- SGRQ-C
St. George’s respiratory questionnaire for COPD
Authors’ contributions
CHL. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. JC. and CHL. contributed to the study concept and design, analysis and interpretation of data, and writing and revision of the manuscript. SSH. contributed to data analysis. KUK., SHL., HYP., SJP., KHM., YMO., KHY., and KSJ. contributed to patient enrollment and data acquisition. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The present study was approved by the institutional review board of the Seoul National University Hospital (H-1706-079-859) and was conducted in accordance with the tenets of the Declaration of Helsinki. All participants in the cohorts provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195:557–582. doi: 10.1164/rccm.201701-0218PP. [DOI] [PubMed] [Google Scholar]
- 2.Orozco-Levi M, Garcia-Aymerich J, Villar J, Ramirez-Sarmiento A, Anto JM, Gea J. Wood smoke exposure and risk of chronic obstructive pulmonary disease. Eur Respir J. 2006;27:542–546. doi: 10.1183/09031936.06.00052705. [DOI] [PubMed] [Google Scholar]
- 3.Kurmi OP, Semple S, Simkhada P, Smith WC, Ayres JG. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax. 2010;65:221–228. doi: 10.1136/thx.2009.124644. [DOI] [PubMed] [Google Scholar]
- 4.Hu G, Zhou Y, Tian J, Yao W, Li J, Li B, et al. Risk of COPD from exposure to biomass smoke: a metaanalysis. Chest. 2010;138:20–31. doi: 10.1378/chest.08-2114. [DOI] [PubMed] [Google Scholar]
- 5.Po JY, FitzGerald JM, Carlsten C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax. 2011;66:232–239. doi: 10.1136/thx.2010.147884. [DOI] [PubMed] [Google Scholar]
- 6.Zhou Y, Zou Y, Li X, Chen S, Zhao Z, He F, et al. Lung function and incidence of chronic obstructive pulmonary disease after improved cooking fuels and kitchen ventilation: a 9-year prospective cohort study. PLoS Med. 2014;11:e1001621. doi: 10.1371/journal.pmed.1001621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Statistics. Monitoring health for the SDGs. World Health Organization. 2017;2017 http://www.who.int/gho/publications/world_health_statistics/2017/en/. Accessed Oct 6 2017.
- 8.World Energy Outlook . 2017. 2017. International energy agency publications. [Google Scholar]
- 9.Torres-Duque CA, Garcia-Rodriguez MC, Gonzalez-Garcia M. Is chronic obstructive pulmonary disease caused by wood smoke a different phenotype or a different entity? Arch Bronconeumol. 2016;52:425–431. doi: 10.1016/j.arbres.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Camp PG, Ramirez-Venegas A, Sansores RH, Alva LF, McDougall JE, Sin DD, et al. COPD phenotypes in biomass smoke- versus tobacco smoke-exposed Mexican women. Eur Respir J. 2014;43:725–734. doi: 10.1183/09031936.00206112. [DOI] [PubMed] [Google Scholar]
- 11.Zhao D, Zhou Y, Jiang C, Zhao Z, He F, Ran P. Small airway disease: a different phenotype of early stage COPD associated with biomass smoke exposure. Respirology. 2018;23:198–205. doi: 10.1111/resp.13176. [DOI] [PubMed] [Google Scholar]
- 12.Fernandes L, Gulati N, Fernandes Y, Mesquita AM, Sardessai M, Lammers JJ, et al. Small airway imaging phenotypes in biomass- and tobacco smoke-exposed patients with COPD. ERJ Open Res. 2017;3. [DOI] [PMC free article] [PubMed]
- 13.Ramirez-Venegas A, Sansores RH, Perez-Padilla R, Regalado J, Velazquez A, Sanchez C, et al. Survival of patients with chronic obstructive pulmonary disease due to biomass smoke and tobacco. Am J Respir Crit Care Med. 2006;173:393–397. doi: 10.1164/rccm.200504-568OC. [DOI] [PubMed] [Google Scholar]
- 14.Ramirez-Venegas A, Sansores RH, Quintana-Carrillo RH, Velazquez-Uncal M, Hernandez-Zenteno RJ, Sanchez-Romero C, et al. FEV1 decline in patients with chronic obstructive pulmonary disease associated with biomass exposure. Am J Respir Crit Care Med. 2014;190:996–1002. doi: 10.1164/rccm.201404-0720OC. [DOI] [PubMed] [Google Scholar]
- 15.Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370:786–796. doi: 10.1016/S0140-6736(07)61382-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park TS, Lee JS, Seo JB, Hong Y, Yoo JW, Kang BJ, et al. Study design and outcomes of Korean obstructive lung disease (KOLD) cohort study. Tuberc Respir Dis (Seoul) 2014;76:169–174. doi: 10.4046/trd.2014.76.4.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee JY, Chon GR, Rhee CK, Kim DK, Yoon HK, Lee JH, et al. Characteristics of patients with chronic obstructive pulmonary disease at the first visit to a pulmonary medical Center in Korea: the KOrea COpd subgroup study team cohort. J Korean Med Sci. 2016;31:553–560. doi: 10.3346/jkms.2016.31.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dzioubinski O, Chipman R. Trends in consumption and production: household energy consumption. DESA discussion paper no. 6. United Nations Department of Economic and Social Affairs. 1999. https://sustainabledevelopment.un.org/index.php?page=view&type=400&nr=77&menu=1572. Accessed Oct 18 2017.
- 19.Best H, Wolf C. The SAGE handbook of regression analysis and causal inference. Thousand Oaks, CA: SAGE Publications; 2014. [Google Scholar]
- 20.Fletcher C. Standardised questionnaire on respiratory symptoms: a statement prepared and approved by the MRC Committee on the Aetiology of chronic bronchitis (MRC breathlessness score) BMJ. 1960;2:1665. [Google Scholar]
- 21.Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St. George's respiratory questionnaire. Am Rev Respir Dis. 1992;145:1321–1327. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 22.Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34:648–654. doi: 10.1183/09031936.00102509. [DOI] [PubMed] [Google Scholar]
- 23.Yoon HK, Park YB, Rhee CK, Lee JH, Oh YM. Summary of the chronic obstructive pulmonary disease clinical practice guideline revised in 2014 by the Korean academy of tuberculosis and respiratory disease. Tuberc Respir Dis (Seoul). 2017;80:230–240. doi: 10.4046/trd.2017.80.3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356:775–789. doi: 10.1056/NEJMoa063070. [DOI] [PubMed] [Google Scholar]
- 25.Tashkin DP, Celli B, Senn S, Burkhart D, Kesten S, Menjoge S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359:1543–1554. doi: 10.1056/NEJMoa0805800. [DOI] [PubMed] [Google Scholar]
- 26.Wedzicha JA, Banerji D, Chapman KR, Vestbo J, Roche N, Ayers RT, et al. Indacaterol-Glycopyrronium versus salmeterol-fluticasone for COPD. N Engl J Med. 2016;374:2222–2234. doi: 10.1056/NEJMoa1516385. [DOI] [PubMed] [Google Scholar]
- 27.Vestbo J, Anderson JA, Brook RD, Calverley PM, Celli BR, Crim C, et al. Fluticasone furoate and vilanterol and survival in chronic obstructive pulmonary disease with heightened cardiovascular risk (SUMMIT): a double-blind randomised controlled trial. Lancet. 2016;387:1817–1826. doi: 10.1016/S0140-6736(16)30069-1. [DOI] [PubMed] [Google Scholar]
- 28.Shapiro SD, Ingenito EP. The pathogenesis of chronic obstructive pulmonary disease: advances in the past 100 years. Am J Respir Cell Mol Biol. 2005;32:367–372. doi: 10.1165/rcmb.F296. [DOI] [PubMed] [Google Scholar]
- 29.Silva R, Oyarzun M, Olloquequi J. Pathogenic mechanisms in chronic obstructive pulmonary disease due to biomass smoke exposure. Arch Bronconeumol. 2015;51:285–292. doi: 10.1016/j.arbres.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 30.Golpe R, Sanjuan Lopez P, Cano Jimenez E, Castro Anon O, Perez de Llano LA. Distribution of clinical phenotypes in patients with chronic obstructive pulmonary disease caused by biomass and tobacco smoke. Arch Bronconeumol. 2014;50:318–324. doi: 10.1016/j.arbres.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 31.Olloquequi J, Silva OR. Biomass smoke as a risk factor for chronic obstructive pulmonary disease: effects on innate immunity. Innate Immun. 2016;22:373–381. doi: 10.1177/1753425916650272. [DOI] [PubMed] [Google Scholar]
- 32.Mehra D, Geraghty PM, Hardigan AA, Foronjy R. A comparison of the inflammatory and proteolytic effects of dung biomass and cigarette smoke exposure in the lung. PLoS One. 2012;7:e52889. doi: 10.1371/journal.pone.0052889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gonzalez-Garcia M, Torres-Duque CA, Bustos A, Jaramillo C, Maldonado D. Bronchial hyperresponsiveness in women with chronic obstructive pulmonary disease related to wood smoke. Int J Chron Obstruct Pulmon Dis. 2012;7:367–373. doi: 10.2147/COPD.S30410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Perez-Padilla R, Regalado J, Vedal S, Pare P, Chapela R, Sansores R, et al. Exposure to biomass smoke and chronic airway disease in Mexican women. A case-control study. Am J Respir Crit Care Med. 1996;154:701–706. doi: 10.1164/ajrccm.154.3.8810608. [DOI] [PubMed] [Google Scholar]
- 35.Foreman MG, Zhang L, Murphy J, Hansel NN, Make B, Hokanson JE, et al. Early-onset chronic obstructive pulmonary disease is associated with female sex, maternal factors, and African American race in the COPDGene study. Am J Respir Crit Care Med. 2011;184:414–420. doi: 10.1164/rccm.201011-1928OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Gemert F, Kirenga B, Chavannes N, Kamya M, Luzige S, Musinguzi P, et al. Prevalence of chronic obstructive pulmonary disease and associated risk factors in Uganda (FRESH AIR Uganda): a prospective cross-sectional observational study. Lancet Glob Health. 2015;3:e44–e51. doi: 10.1016/S2214-109X(14)70337-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online supplement (DOC). Figure S1. Histograms showing propensity score distribution. Table S1. Baseline characteristics of the study patients before and after propensity score matching. Table S2. Adjusted incidence rates of moderate or severe exacerbations by exposure groups (sensitivity analysis). Table S3. Incidence rates of moderate or severe exacerbations in the propensity score-matched cohort (sensitivity analysis) (DOC 117 kb)
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.