Abstract
There is limited understanding of the relation between insomnia and aspects of eating among college students though available data suggest salient clinical relationships. The present study explored a potential transdiagnostic mechanism in the relation between insomnia symptoms and eating expectancies. Participants were a racially/ethnically diverse sample of 1589 college students (80.4% females; Mage = 22.2 years, SD = 5.27) from an urban university. Primary analysis included three regression-based models of eating expectancies. Insomnia symptoms served as the predictor, and emotion dysregulation served as the indirect (mediator) variable in all models. Results indicated that insomnia symptoms yielded a significant indirect effect through emotion dysregulation on expectancies of eating to help manage negative affect, alleviate boredom, and lead to feeling out of control. Students experiencing insomnia symptoms may be at higher risk for experiencing dysregulated emotions and consequently maladaptive eating expectancies compared to good sleepers.
Keywords: Insomnia, sleep, emotion dysregulation, eating, college
Sleep quantity and quality are often negatively impacted by common stressors faced by college students, including financial stress, academic demands, and living away from home (Galambos, Howard, & Maggs, 2011). When inadequate or unsatisfactory sleep results in impairment of daytime functioning, it is referred to as insomnia (Sateia, Doghramji, Hauri, & Morin, 2000). Insomnia can include difficulty initiating sleep, repeated or lengthy awakenings, early morning awakening, or poor overall quality of sleep (Sateia et al., 2000) and is common among college students. As one illustrative recent example, in a study among 1074 undergraduates, approximately 9.5% of students suffered from clinically significant insomnia (Taylor, Bramoweth, Grieser, Tatum, & Roane, 2013).
Insomnia tends to have a chronic course (Morin et al., 2009) and frequently co-occurs with other problematic health behaviors, including unhealthy eating patterns (Quick et al., 2016). Indeed, extant work has examined the role of insomnia and sleep disturbances more generally on eating patterns and behavior. For example, Quick and colleagues (2016) found that college students who slept less than eight hours per night reported significantly more negative attitudes about eating, poorer internal regulation of food, and greater binge eating compared to students who slept eight or more hours per night. Another investigation found poor sleep quality (a symptom of insomnia) was associated with significantly higher uncontrolled eating among college students (Shoff et al., 2009). These data suggest sleep deprived college students may be more apt to experience unhealthy eating behaviors and attitudes. Yet, little is known overall about the relation between insomnia specifically and clinically significant aspects of eating among college students.
To forward the scientific study of unhealthy eating, researchers have increasingly found merit in applying expectancy theory (Odgen, 2003). Such an approach posits that expectancies reflect learned relations between behaviors and their consequences that become stored in memory and guide future behavioral choices (Fischer, Smith, Anderson, & Flory, 2003). In fact research suggests individuals develop expectancies related to a given behavior through observational and experiential learning (Miller, Smith, & Goldman, 1990). There are a number of distinct expectancies for eating that vary both between and within individuals (e.g. eating helps manage negative affect, eating alleviates boredom, and eating leads to feeling out of control; Hohlstein, Smith, & Atlas, 1998). Expectancy models predict that distinct expectancies may theoretically be related to specific types of clinical outcomes (Fischer, Anderson, & Smith, 2004), including various aspects of problematic eating (Smith, Simmons, Flory, Annus, & Hill, 2007). For example, expectancies of eating to alleviate boredom has been found to be associated with emotional eating (Hennegan, Loxton, & Mattar, 2013), whereas expectancies of eating to lead to feeling out of control has been associated with greater calories consumed (Hearon, Utschig, Smits, Moshier, & Otto, 2013). Furthermore, expectancies of eating to manage negative affect have been found to be associated with binge eating (Della Longa & De Young, 2018; Smith et al., 2007), emotional eating (Hennegan et al., 2013), and bulimic symptoms (Lavender, Happel, Anestis, Tull, & Gratz, 2015). In fact, research suggests eating expectancies are related to a variety of other clinically significant consequences, such as obesity (Hearon et al., 2013), cardiovascular problems (Koo-Loeb, Costello, Light, & Girdler, 2000), other addictive behaviors (Fischer, Settles, Collins, Gunn, & Smith, 2012), mental health problems (Danner, Evers, Stok, van Elburg, & de Ridder, 2012), and lower health-related quality of life (Schulte, Joyner, Potenza, Grilo, & Gearhardt, 2015). Thus, enhancing efforts to understand eating expectancies may facilitate knowledge of unhealthy eating within the context of insomnia. Exploration of the relation between insomnia and eating expectancies in general, and among college students specifically, is nonexistent.
Within a clinical context, it is equally important to evaluate mechanisms that underpin associations between insomnia and eating expectancies. Emotion dysregulation is one construct that may serve to explicate the relation between insomnia symptoms and eating expectancies among college students. Emotion dysregulation reflects difficulties engaging a set of abilities wherein one can observe, understand, evaluate, and differentiate one’s emotions and subsequently access strategies to regulate emotions and control behavioral responses (Gratz & Roemer, 2004; Tull & Aldao, 2015). Experimental work has found that sleep loss directly impacts connections between the medial prefrontal cortex and amygdala, whereby increases in emotional arousal co-occur with deficits in emotional control and monitoring (Yoo, Gujar, Hu, Jolesz, & Walker, 2007). Among college students, available research suggests sleep difficulties are, in fact, related to greater emotion dysregulation (Pickett, Barbaro, & Mello, 2016; Tavernier & Willoughby, 2015).
Theoretically, college students experiencing greater insomnia symptoms may experience more difficulties regulating their emotions. As such, they may respond to such emotion dysregulation in a less adaptive fashion, resulting in unhealthy eating to manage their emotions. As a result, they may learn to expect eating to serve distinct affect-related and self-regulation functions. For example, sleep-deprived college students may be more likely to expect eating to help manage negative affect (Selby, Ward, & Joiner, 2010; Smyth et al., 2007), expect to feel out of control once they start eating (Goossens, Braet, Van Vlierberghe, & Mels, 2009), and that eating can improve their mood (e.g. alleviate boredom; Moynihan et al., 2015). In fact, existing work documents the adverse effect of emotion dysregulation on eating behaviors (Lavender et al., 2014), but it has not explored eating expectancies in the context of insomnia-emotion dysregulation relations. Thus, it is clinically and theoretically important to evaluate whether emotion dysregulation indirectly accounts for the relation between insomnia symptoms and expectancies of eating to help manage negative affect, expectancies of eating to lead to feeling out of control, and expectancies of eating to alleviate boredom.
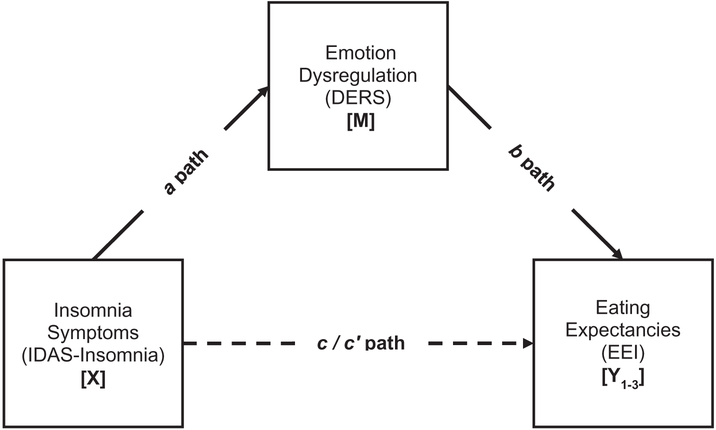
The current study tested the hypothesis that insomnia would exert an indirect effect on eating expectancies via emotion dysregulation (see Figure 1). Specifically, insomnia was expected to be positively associated with emotion dysregulation, which, in turn, would be associated with expectancies of eating to help manage negative affect, expectancies of eating to alleviate boredom, and expectancies of eating to lead to feeling out of control. It was expected that an effect of insomnia symptoms via emotion dysregulation would be evident on all criterion variables over and above variance accounted for by gender, race/ethnicity, and negative affectivity (Croll, Neumark-Sztainer, Story, & Ireland, 2002; Haedt-Matt & Keel, 2011; Lee-Winn, Reinblatt, Mojtabai, & Mendelson, 2016).
Figure 1.
Conceptual model.
Note: a path = Effect of X on M; b paths = Effect of M on Yi; c paths = Total effect of X on Yi; c’ paths = Direct effect of X on Yi controlling for M. Three separate paths were conducted (Y1–3) with the predictor (X). Covariates included gender, race/ethnicity, and negative affectivity.
Methods
Participants
Participants were 1589 college students (80.4% females; Mage = 22.2 years, SD = 5.27). The sample was racially/ethnically diverse and representative of the university’s student body: 29.6% Hispanic (n = 470), 27.2% Asian/Pacific Islander (n = 433), 23.8% White (non-His-panic; n = 378), 14.2% Black (non-Hispanic; n = 226), and 4.7% other race/ethnicities (n = 74). The data were collected from September 2015 through May 2017.
Measures
Demographic questionnaire
A demographic questionnaire was used to collect data including gender, race/ethnicity, and age for descriptive purposes. Gender and race/ethnicity were included as covariates in the current study.
Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988)
The PANAS is a self-report measure that assesses the extent to which participants experienced 20 different feelings and emotions (e.g. excited, distressed) on a Likert-type scale ranging from 1 (Very slightly or not at all) to 5 (Extremely). The measure yields two factors, negative and positive affectivity. The PANAS has demonstrated strong psychometric properties, including high levels of internal consistency across clinical and non-clinical samples (Cronbach’s α = .85–.93; Watson, 2000; Watson et al., 1988) The PANAS-NA demonstrated excellent internal consistency (α = .90).
Inventory of Depression and Anxiety Symptoms (IDAS)
The IDAS is a 64-item self-report assessment of major depression and related anxiety disorders. Respondents are asked to rate the degree to which they have experienced symptoms within the past two weeks, rated on a 5-point Likert-type scale from 1 (not at all) to 5 (extremely). Insomnia symptoms, as in past work (Kauffman, Farris, Alfano, & Zvolensky, 2017), were assessed using the sum of the 6-item insomnia subscale (e.g. “I had trouble falling asleep”), with higher scores representative of greater insomnia symptoms in the past two weeks. The insomnia subscale has strong psychometric properties including, test–retest reliability, internal consistency, and discriminant validity. In the current sample, internal consistency for the insomnia subscale was good (Cronbach’s α = .83).
Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004)
The DERS is a 36-item self-report measure that assesses how often respondents experience dysregulated emotional states. The DERS assesses six subscale facets which can be summed to create a total score with higher values indicating greater emotion dysregulation (possible range = 36–180). Specifically, respondents are asked to rate on a five-point Likert-type scale from 1 (almost never) to 5 (almost always) items related to Non-Acceptance of Emotional Responses, Difficulties Engaging in Goal-Directed Behavior, Impulse Control Difficulties, Lack of Emotional Awareness, Access to Emotion Regulation Strategies, and Lack of Emotional Clarity. The DERS items have strong psychometric properties (Gratz & Roemer, 2004; Whiteside et al., 2007) and internal consistency for the DERS total score was excellent (Cronbach’s α = .93).
Eating Expectancy Inventory (EEI; Hohlstein et al., 1998)
The EEI is a 34-item self-report measure used to assess the cognitive expectancies of eating. Specifically, the EEI assesses five subscale facets: eating helps manage negative affect; eating is pleasurable and useful as a reward; eating leads to feeling out of control; eating enhances cognitive competence; and eating alleviates boredom. Items are rated on a seven-point Likert-type scale ranging from 1 (completely disagree) to 7 (completely agree). The EEI subscales have demonstrated strong psychometric properties among college, clinical, and adolescent samples (Hohlstein et al., 1998; Simmons, Smith, & Hill, 2002). Eating helps manage negative affect (Cronbach’s α = .95), eating alleviates boredom (Cronbach’s α = .73), and eating leads to feeling out of control (Cronbach’s α = .80) were utilized in the current study.
Procedure
The present sample included university students at a large, southwestern university interested in receiving extra credit towards their psychology course as compensation. Participants were recruited via flyers and posting on the extra credit website. Exclusion criteria included being younger than age 18 and non-proficiency in English (to ensure comprehension of study questions). All participants provided informed consent which was completed over the internet before proceeding to the online self-report survey. Quality assurance questions were placed throughout the survey to protect against sporadic responding and ensure the integrity of the data. Identifying information was not retained for each participant; there was no link between each participant’s identity and study responses. This study protocol was approved by the Institutional Review Board at the University of Houston.
Analytic strategy
Data were first checked for quality assurance; no cases of sporadic responding were detected. Sample descriptive statistics and zero-order correlations among study variables were examined. Primary analysis included three regression-based models: (1) expectancies of eating to help manage negative affect, (2) expectancies of eating to alleviate boredom, and (3) expectancies of eating to lead to feeling out of control (y1–3). Insomnia symptoms served as the predictor, and emotion dysregulation served as the indirect variable in all models. Covariates included gender (0 = male, 1 = female), race/ethnicity, and negative affectivity (PANAS-NA); see Figure 1.
Analyses were conducted using bootstrapping techniques through PROCESS, a conditional modeling program that utilizes an ordinary least squares-based path analytical framework to test for both direct and indirect effects (Hayes, 2013). Theoretically our primary interest was in the indirect effect (i.e. the mediation analysis). Thus, a significant total effect was not a prerequisite for testing for the indirect effects (Loeys, Moerkerke, & Vansteelandt, 2014). An indirect effect is the product of path a (the association between the predictor [x] and the proposed explanatory variable [m]) and path b (the association between the proposed mediator variable [m] and the dependent variable [yi] controlling for x). As recommended, the confidence intervals around the point-estimate were subjected to 10,000 bootstrap re-samplings and 95-percent confidence intervals (CIs) were estimated (Hayes, 2009; Preacher & Hayes, 2004, 2008). The effects can be assumed to be statistically significant if the CIs around their product do not include zero (Preacher & Hayes, 2008; Zhao, Lynch, & Chen, 2010). Percent mediated (indirect effect/total effect) was calculated for each outcome variable. Percent mediation was not reported for variables with a non-significant total effect. To further strengthen the interpretation of results, alternative models were tested by reversing the proposed mediator for each of the three significant models (Preacher & Hayes, 2004).
Results
Bi-variate relations
Zero-order correlations among all study variables are presented in Table 1. Average IDAS-Insomnia scores in the current study (M = 13.38, SD = 5.29) were comparable to normative scores for community-recruited individuals (M = 12.7, SD = 5.7; Watson et al., 2007). Insomnia symptoms were positively correlated with emotion dysregulation (r = .382, p < .001) and all criterion variables (r’s = .105–.175, p’s < .001). Similarly, emotion dysregulation was positively correlated with all criterion variables (r’s = .210–.344, p’s < .001).
Table 1.
Descriptive statistics and bivariate correlations between study variables (N = 1589).
| Variable | Mean/n (SD/%) |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Gendera | 1278 (80.4%) | – | |||||||
| 2. Race/Ethnicitya | 378 (23.8%) | .037 | – | ||||||
| 3. Negative Affectivitya | 21.09 (7.83) | −.011 | −.006 | – | |||||
| 4. Insomnia Symptomsb | 13.38 (5.29) | .011 | .025 | .455*** | – | ||||
| 5. Emotion Dysregulationc | 85.94 (23.29) | −.018 | .044 | .614*** | .382*** | – | |||
| 6. Eating Expectancies-Negative Affectd | 57.96 (24.15) | .008 | .030 | .259*** | .175*** | .326*** | – | ||
| 7. Eating Expectancies-Boredomd | 16.36 (5.62) | .057* | .014 | .153*** | .105*** | .210*** | .607*** | – | |
| 8. Eating Expectancies-Controld | 11.55 (5.86) | .001 | −.004 | .246*** | .167*** | .344*** | .467*** | .270*** | – |
Note: Gender: % listed as females (Coded: 0 = male and 1 = female); Race/Ethnicity: % listed as White (non-Hispanic); Negative Affectivity = Positive and Negative Affect Schedule-Negative Affect subscale (Watson et al., 1988); Insomnia Symptoms = Inventory of Depression and Anxiety-Insomnia subscale (Watson, O’Hara, Kotov, et al., 2007); Emotion Dysregulation = Difficulties with Emotion Regulation Scale (Gratz & Roemer, 2004); Eating Expectancies-Negative Affect = Eating Expectancy Inventory-Eating Helps Manage Negative Affect subscale (Hohlstein et al., 1998); Eating Expectancies-Boredom = Eating Expectancy Inventory-Eating Alleviates Boredom subscale (Hohlstein et al., 1998); Eating Expectancies-Control = Eating Expectancy Inventory-Eating Leads to Feeling out of Control subscale (Hohlstein et al., 1998).
p < .001 ;
p < .05;
Covariate.
Predictor.
Mediator.
Criterion.
Indirect effects
Regression results are presented in Table 2. For expectancies of eating to help manage negative affect, the total effects model with insomnia symptoms and covariates in the model accounted for significant variance (R2 =.07, F[4, 1584] = 30.74, p < .001). The full model with emotion dysregulation was significant (R2 =.11, F[5, 1583] = 40.49, p < .001). In the test of the indirect effect, results indicated that insomnia symptoms were associated with expectancies of eating to help manage negative affect, which indirectly occurred through greater levels of emotion dysregulation (a × b = 0.152, SE = 0.034, CI95% = 0.093, 0.226; PM = .473).
Table 2.
Indirect effect of Insomnia symptoms on eating expectancies subscales via emotion dysregulation.
| Y | Path | R2 | b | SE | t | p | CI (l) | CI (u) | PM |
|---|---|---|---|---|---|---|---|---|---|
| 1 | IDAS-IN → DERS (a) | .393 | 0.563 | 0.100 | 5.80 | < .001 | 0.372 | 0.753 | |
| DERS → EEI-NA (b) | .113 | 0.271 | 0.032 | 8.59 | < .001 | 0.209 | 0.332 | ||
| IDAS-IN → EEI-NA (c’) | 0.170 | 0.123 | 1.38 | .167 | −0.071 | 0.411 | |||
| IDAS-IN → EEI-NA (c) | .072 | 0.322 | 0.124 | 2.59 | .010 | 0.078 | 0.566 | ||
| IDAS-IN → DERS → EEI-NA (a × b) | 0.152 | 0.034 | 0.092 | 0.227 | .473 | ||||
| 2 | DERS → EEI-BOR (b) | .049 | 0.044 | 0.008 | 5.83 | < .001 | 0.029 | 0.059 | |
| IDAS-IN → EEI-BOR (c’) | 0.021 | 0.030 | .717 | .434 | −0.037 | 0.079 | |||
| IDAS-IN → EEI-BOR (c) | .029 | 0.460 | 0.030 | 1.56 | .120 | −0.012 | 0.104 | ||
| IDAS-IN → DERS → EEI-BOR (a × b) | 0.030 | 0.006 | 0.014 | 0.039 | |||||
| 3 | DERS → -EEI-CON (b) | .122 | 0.077 | 0.008 | 10.17 | < .001 | 0.062 | 0.092 | |
| IDAS-IN → EEI-CON (c’) | 0.034 | 0.030 | 1.16 | .248 | −0.024 | 0.093 | |||
| IDAS-IN → EEI-CON (c) | .064 | 0.078 | 0.030 | 2.57 | .010 | 0.018 | 0.137 | ||
| IDAS-IN → DERS → EEI-CON (a × b) | 0.044 | 0.009 | 0.027 | 0.064 | .564 |
Note: Path a is equal in all cases Y1–3; therefore, it presented only once to avoid redundancies. N for analyses is 1589 cases. The standard error and 95% CI for the indirect effects (a × b) are obtained through bootstrapping with 10,000 re-samples. a path = Effect of X on M; b paths = Effect of M on Yi; c’ paths = Direct effect of X on Yi controlling for M; c paths = Total effect of X on Yi IDAS-IN = Inventory of Depression and Anxiety-Insomnia subscale; DERS = Difficulties with Emotion Regulation Scale (Gratz & Roemer, 2004); Eating Expectancies-Negative Affect = Eating Expectancy Inventory-Eating Helps Manage Negative Affect subscale (Hohlstein et al., 1998); Eating Expectancies-Boredom = Eating Expectancy Inventory-Eating Alleviates Boredom subscale (Hohlstein et al., 1998); Eating Expectancies-Control = Eating Expectancy Inventory-Eating Leads to Feeling out of Control subscale (Hohlstein et al., 1998). Covariates included gender, race/ethnicity, and negative affectivity.
In terms of expectancies of eating to alleviate boredom, the total effect model accounted for significant variance (R2 =.03, F[4, 1584] = 11.61, p < .001). The model with emotion dysregulation accounted for additional variance for expectancies of eating to alleviate boredom (R2 =.05, F[5, 1583] = 16.27, p < .001). The test of the indirect effect indicated that insomnia symptoms were associated with expectancies of eating to alleviate boredom indirectly through the effect of emotion dysregulation (a × b = 0.030, SE = 0.006, CI95% = 0.014, 0.039).
In regard to expectancies of eating to lead to feeling out of control, the total effects model accounted for significant variance (R2 = .06, F[4, 1584] = 27.18, p < .001). The full model with the addition of emotion dysregulation was significant (R2 = .12, F[5, 1583] = 43.81, p < .001). In the test of the indirect effect through emotion dysregulation, results indicated that insomnia symptoms were associated with expectancies of eating to lead to feeling out of control (a × b = 0.044, SE = 0.009, CI95% = 0.028, 0.064; PM = .564).
Specificity analyses
To further strengthen the interpretation of results, alternative models were tested by reversing the proposed mediator for each of the three models (Preacher & Hayes, 2004); specifically, emotion dysregulation was the predictor, insomnia was the indirect variable, and all three criterion variables remained the same. The indirect effects of the alternate models were non-significant for expectancies of eating to help manage negative affect (a × b = 0.006, SE = 0.005, CI99% = −0.003, 0.017), expectancies of eating to alleviate boredom (a × b = 0.001, SE = 0.001, CI99% = −0.001, 0.003), and expectancies of eating to lead to feeling out of control (a × b = 0.001, SE = 0.001, CI99% = −0.001, 0.004).
Discussion
To our knowledge, this is the first study to empirically examine the indirect explanatory role of emotion dysregulation in the relation between insomnia symptoms and eating expectancies among college students. As hypothesized, results indicated that insomnia symptoms yielded a significant indirect effect through emotion dysregulation for expectancies of eating to help manage negative affect, expectancies of eating to alleviate boredom, and expectancies of eating to lead to feeling out of control. Thus, greater insomnia symptoms were related to increased emotion dysregulation, which in turn, were related to greater expectancies of eating to help manage negative affect, expectancies of eating to alleviate boredom, and expectancies of eating to lead to feeling out of control. The observed indirect effects were evident after adjusting for gender, race/ethnicity, and negative affectivity. Importantly, competing models were non-significant, which provide further empirical support for the proposed model. These findings are broadly consistent with past work that has found emotion dysregulation is related to disordered eating (Ambwani, Slane, Thomas, Hopwood, & Grilo, 2014; Selby et al., 2010).
Notably, there was no significant relationship between insomnia symptoms and expectancies of eating to alleviate boredom. Although broadly discordant with past work (Quick et al., 2016; Shoff et al., 2009), the current findings offer a unique perspective in the understanding of the relation between insomnia symptoms and eating expectancies. The present cross-sectional results suggest that, theoretically, insomnia symptoms in and of itself may not “predispose” college students to evince expectancies of eating to alleviate boredom. Rather, among college students, insomnia symptoms may exacerbate the dysregulation of emotions (Fairholme et al., 2013), and as a result of such dysregulated state, these persons may learn eating can be perceived as helpful in managing negative mood states, lead to feeling out of control, and prevent feeling bored. Future longitudinal modeling of the relations between insomnia, emotion dysregulation, and eating expectancies is warranted. For example, it may be advisable to use time sampling tactics to track daily insomnia in relation to fluctuations in emotion dysregulation and their corresponding impact on eating expectancies.
The results from the present investigation may serve to conceptually inform the development of more targeted weight management or eating education programs for college students experiencing insomnia symptoms. For example, there may be clinical utility in providing psychoeducation about the linkages between insomnia and expectancies about eating. Further, by educating and perhaps targeting emotion dysregulation directly, it may be possible to offset the relative risk of certain high-risk eating expectancies among this group. Consequently, such improvements in emotion regulation may facilitate a reduction in maladaptive eating expectancies and behaviors.
There are several interpretive caveats to the present study. First, given the cross-sectional nature of these data, the directionality of the observed effects cannot be fully explicated. Based upon the present results, future prospective studies are necessary to determine the directional effects of these relations. Second, as the key variables were assessed via self-report, there is the possibility that the observed relations were in part a function of shared method variance. Future research would benefit by employing a multi-method assessment approach to cross-index the nature of the relations observed in the current report. In particular, utilization of an objective measure of sleep such as actigraphy would be helpful to cross-index actual sleep parameters (Edinger & Fins, 1995). Other factors and forms of sleep disturbance (e.g. circadian sleep delays) also contribute to daytime tiredness in older adolescents and young adults (Owens, 2014) and should be explicitly examined in future work. Fourth, we employed the IDAS-insomnia subscale as the primary measure of insomnia symptoms. Future work may benefit from incorporating other validated measures of insomnia symptoms (e.g. Insomnia Severity Index; Bastien, Vallieres, & Morin, 2001). Fifth, although there was a significant indirect effect of insomnia symptoms on eating expectancies through emotion dysregulation, the current study investigated only a single, yet novel, underlying mechanism. Future work should therefore focus on additional explanatory variables that may underlie this association, including other transdiagnostic factors (e.g. anxiety sensitivity, distress intolerance, anhedonia). Finally, 80.4% of the samples were female college students. Future studies may benefit from sampling a larger pool of males from the student population to ensure generalizability of the results to college students.
Overall, the current study found empirical support for the role of emotion dysregulation in the association between insomnia symptoms and certain high-risk eating expectancies among college students. It may be possible that among college students experiencing insomnia symptoms, targeting emotion dysregulation could result in a reduction in clinically relevant eating expectancies and possibly problematic eating behaviors. Future work is needed to replicate and validate the hypothesized model and extend it to include the possible impact on other eating behaviors and disorders as well as obesity related indicators, such as body mass index. Additionally, based on the present findings, further work could examine the nature of specific emotion regulation strategies (i.e. Non-Acceptance of Emotional Responses, Difficulties Engaging in Goal-Directed Behavior, Impulse Control Difficulties, Lack of Emotional Awareness, Access to Emotion Regulation Strategies, and Lack of Emotional Clarity) among college students within the context of insomnia symptoms and eating expectancies.
Footnotes
Disclosure statement
The authors report no conflicts of interest.
References
- Ambwani S, Slane JD, Thomas KM, Hopwood CJ, & Grilo CM (2014). Interpersonal dysfunction and affect-regulation difficulties in disordered eating among men and women. Eating Behaviors, 15(4), 550–554. 10.1016/j.eatbeh.2014.08.005 [DOI] [PubMed] [Google Scholar]
- Bastien CH, Vallieres A, & Morin CM (2001). Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine, 2(4), 297–307. 10.1016/S1389-9457(00)00065-4 [DOI] [PubMed] [Google Scholar]
- Croll J, Neumark-Sztainer D, Story M, & Ireland M (2002). Prevalence and risk and protective factors related to disordered eating behaviors among adolescents: Relationship to gender and ethnicity. Journal of Adolescent Health, 31(2), 166–175. 10.1016/S1054-139X(02)00368-3 [DOI] [PubMed] [Google Scholar]
- Danner UN, Evers C, Stok FM, van Elburg AA, & de Ridder DT (2012). A double burden: Emotional eating and lack of cognitive reappraisal in eating disordered women. European Eating Disorders Review, 20(6), 490–495. 10.1002/erv.2184 [DOI] [PubMed] [Google Scholar]
- Della Longa NM, & De Young KP (2018). Experiential avoidance, eating expectancies, and binge eating: A preliminary test of an adaption of the acquired preparedness model of eating disorder risk. Appetite, 120, 423–430. 10.1016/j.appet.2017.09.022 [DOI] [PubMed] [Google Scholar]
- Edinger JD, & Fins AI (1995). The distribution and clinical significance of sleep time misperceptions among insomniacs. Sleep, 18(4), 232–239. 10.1093/sleep/18.4.232 [DOI] [PubMed] [Google Scholar]
- Fairholme CP, Nosen EL, Nillni YI, Schumacher JA, Tull MT, & Coffey SF (2013). Sleep disturbance and emotion dysregulation as transdiagnostic processes in a comorbid sample. Behaviour Research and Therapy, 51(9), 540–546. 10.1016/j.brat.2013.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer S, Anderson KG, & Smith GT (2004). Coping with distress by eating or drinking: role of trait urgency and expectancies. Psychology of Addictive Behaviors, 18(3), 269–274. 10.1037/0893-164x.18.3.269 [DOI] [PubMed] [Google Scholar]
- Fischer S, Settles R, Collins B, Gunn R, & Smith GT (2012). The role of negative urgency and expectancies in problem drinking and disordered eating: Testing a model of comorbidity in pathological and at-risk samples. Psychology of Addictive Behaviors, 26(1), 112–123. 10.1037/a0023460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer S, Smith GT, Anderson KG, & Flory K (2003). Expectancy influences the operation of personality on behavior. Psychology of Addictive Behaviors, 17(2), 108–114. 10.1037/0893-164X.17.2.108 [DOI] [PubMed] [Google Scholar]
- Galambos NL, Howard AL, & Maggs JL (2011). Rise and fall of sleep quantity and quality with student experiences across the first year of university. Journal of Research on Adolescence, 21(2), 342–349. 10.1111/j.1532-7795.2010.00679.x [DOI] [Google Scholar]
- Goossens L, Braet C, Van Vlierberghe L, & Mels S (2009). Loss of control over eating in overweight youngsters: The role of anxiety, depression and emotional eating. European Eating Disorders Review, 17(1), 68–78. 10.1002/erv.892 [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology & Behavioral Assessment, 26(1), 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Haedt-Matt AA, & Keel PK (2011). Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment. Psychological Bulletin, 137(4), 660–681. 10.1037/a0023660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76(4), 408–420. 10.1080/03637750903310360 [DOI] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach Methodology in the social sciences. New York, NY: The Guilford Press. [Google Scholar]
- Hearon BA, Utschig AC, Smits JAJ, Moshier SJ, & Otto MW (2013). The role of anxiety sensitivity and eating expectancy in maladaptive eating behavior. Cognitive Therapy and Research, 37(5), 923–933. 10.1007/s10608-012-9491-2 [DOI] [Google Scholar]
- Hennegan JM, Loxton NJ, & Mattar A (2013). Great expectations. Eating expectancies as mediators of reinforcement sensitivity and eating. Appetite, 71(Supplement C), 81–88. 10.1016/j.appet.2013.07.013 [DOI] [PubMed] [Google Scholar]
- Hohlstein LA, Smith GT, & Atlas JG (1998). An application of expectancy theory to eating disorders: Development and validation of measures of eating and dieting expectancies. Psychological Assessment, 10(1), 49–58. 10.1037/1040-3590.10.1.49 [DOI] [Google Scholar]
- Kauffman BY, Farris SG, Alfano CA, & Zvolensky MJ (2017). Emotion dysregulation explains the relation between insomnia symptoms and negative reinforcement smoking cognitions among daily smokers. Addictive Behaviors, 72, 33–40. 10.1016/j.addbeh.2017.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koo-Loeb JH, Costello N, Light KC, & Girdler SS (2000). Women with eating disorder tendencies display altered cardiovascular, neuroendocrine, and psychosocial profiles. Psychosomatic Medicine, 62(4), 539–548. 10.1097/00006842-200007000-00013 [DOI] [PubMed] [Google Scholar]
- Lavender JM, Happel K, Anestis MD, Tull MT, & Gratz KL (2015). The interactive role of distress tolerance and eating expectancies in bulimic symptoms among substance abusers. Eating Behaviors, 16(Supplement C), 88–91. 10.1016/j.eatbeh.2014.10.006 [DOI] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Peterson CB, Crosby RD, Engel SG, Mitchell JE, … Berg KC (2014). Dimensions of emotion dysregulation in Bulimia Nervosa. European Eating Disorders Review, 22(3), 212–216. 10.1002/erv.2288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee-Winn AE, Reinblatt SP, Mojtabai R, & Mendelson T (2016). Gender and racial/ethnic differences in binge eating symptoms in a nationally representative sample of adolescents in the United States. Eating Behaviors, 22, 27–33. 10.1016/j.eatbeh.2016.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeys T, Moerkerke B, & Vansteelandt S (2014). A cautionary note on the power of the test for the indirect effect in mediation analysis. Frontiers in Psychology, 5, 1549 10.3389/fpsyg.2014.01549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller PM, Smith GT, & Goldman MS (1990). Emergence of alcohol expectancies in childhood: A possible critical period. Journal of Studies on Alcohol, 51(4), 343–349. 10.15288/jsa.1990.51.343 [DOI] [PubMed] [Google Scholar]
- Morin CM, Belanger L, LeBlanc M, Ivers H, Savard J, Espie CA, … Gregoire JP (2009). The natural history of insomnia. Archives of Internal Medicine, 169(5), 447–453. 10.1001/archinternmed.2008.610 [DOI] [PubMed] [Google Scholar]
- Moynihan AB, van Tilburg WAP, Igou ER, Wisman A, Donnelly AE, & Mulcaire JB (2015). Eaten up by boredom: Consuming food to escape awareness of the bored self. Frontiers in Psychology, 6, 369 10.3389/fpsyg.2015.00369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odgen J (2003). The psychology of eating. Carlton: Blackwell Publishing Ltd. [Google Scholar]
- Owens J (2014). Insufficient sleep in adolescents and young adults: An update on causes and consequences. Pediatrics, 134(3), e921–e932. 10.1542/peds.2014-1696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett SM, Barbaro N, & Mello D (2016). The relationship between subjective sleep disturbance, sleep quality, and emotion regulation difficulties in a sample of college students reporting trauma exposure. Psychological Trauma: Theory, Research, Practice, and Policy, 8(1), 25–33. 10.1037/tra0000064 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36(4), 717–731. 10.3758/bf03206553 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Quick V, Byrd-Bredbenner C, Shoff S, White AA, Lohse B, Horacek T, … Greene G (2016). Relationships of sleep duration with weight-related behaviors of U.S. college students. Behavioral Sleep Medicine, 14(5), 565–580. 10.1080/15402002.2015.1065411 [DOI] [PubMed] [Google Scholar]
- Sateia MJ, Doghramji K, Hauri PJ, & Morin CM (2000). Evaluation of chronic insomnia. An American Academy of Sleep Medicine review. Sleep, 23(2), 243–308. [PubMed] [Google Scholar]
- Schulte EM, Joyner MA, Potenza MN, Grilo CM, & Gearhardt AN (2015). Current considerations regarding food addiction. Current Psychiatry Reports, 17(4), 20 10.1007/s11920-015-0563-3 [DOI] [PubMed] [Google Scholar]
- Selby EA, Ward AC, & Joiner TE (2010). Dysregulated eating behaviors in borderline personality disorder: Are rejection sensitivity and emotion dysregulation linking mechanisms? International Journal of Eating Disorders, 43(7), 667–670. 10.1002/eat.20761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoff S, Nuss E, Horacek T, Boyle C, Lohse B, Patterson J, … Greene G (2009). Sleep quality is associated with eating behavior in 18–24 year old college students. Journal of Nutrition Education and Behavior, 41(4), S8–S9. 10.1016/j.jneb.2009.03.117 [DOI] [Google Scholar]
- Simmons JR, Smith GT, & Hill KK (2002). Validation of eating and dieting expectancy measures in two adolescent samples. International Journal of Eating Disorders, 31(4), 461–473. 10.1002/eat.10034 [DOI] [PubMed] [Google Scholar]
- Smith GT, Simmons JR, Flory K, Annus AM, & Hill KK (2007). Thinness and eating expectancies predict subsequent binge-eating and purging behavior among adolescent girls. Journal of Abnormal Psychology, 116(1), 188–197. 10.1037/0021-843x.116.1.188 [DOI] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, & Engel SG (2007). Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology, 75(4), 629–638. 10.1037/0022-006x.75.4.629 [DOI] [PubMed] [Google Scholar]
- Tavernier R, & Willoughby T (2015). A longitudinal examination of the bidirectional association between sleep problems and social ties at university: The mediating role of emotion regulation. Journal of Youth & Adolescence, 44(2), 317–330. 10.1007/s10964-014-0107-x [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Bramoweth AD, Grieser EA, Tatum JI, & Roane BM (2013). Epidemiology of insomnia in college students: Relationship with mental health, quality of life, and substance use difficulties. Behavior Therapy, 44(3), 339–348. 10.1016/j.beth.2012.12.001 [DOI] [PubMed] [Google Scholar]
- Tull MT, & Aldao A (2015). Editorial overview: New directions in the science of emotion regulation. Current Opinion in Psychology, 3, iv–x. 10.1016/j.copsyc.2015.03.009 [DOI] [Google Scholar]
- Watson D (2000). Mood and temperament. New York, NY: Guilford Press. [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Kotov R, Simms LJ, Chmielewski M, McDade-Montez EA, … Stuart S (2007). Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS). Psychological Assessment, 19(3), 253–268. 10.1037/1040-3590.19.3.253 [DOI] [PubMed] [Google Scholar]
- Whiteside U, Chen E, Neighbors C, Hunter D, Lo T, & Larimer M (2007). Difficulties regulating emotions: Do binge eaters have fewer strategies to modulate and tolerate negative affect? Eating Behaviors, 8(2), 162–169. 10.1016/j.eatbeh.2006.04.001 [DOI] [PubMed] [Google Scholar]
- Yoo S-S, Gujar N, Hu P, Jolesz FA, & Walker MP (2007). The human emotional brain without sleep — A prefrontal amygdala disconnect. Current Biology, 17(20), R877–R878. 10.1016/j.cub.2007.08.007 [DOI] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, & Chen Q (2010). Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research, 37(2), 197–206. 10.1086/651257 [DOI] [Google Scholar]