Abstract
Motivated by the observation that medical care explains only a relatively small part of the SES-health gradient, we present a life-cycle model that incorporates several additional behaviours that potentially explain (jointly) a large part of observed disparities. As a result, the model provides not only a conceptual framework for the SES-health gradient but more generally an improved framework for the production of health. We derive novel predictions from the theory by performing comparative dynamic analyses. More generally, our comparative dynamic method can be applied to models of similar form, e.g., human capital, health deficits, firm investment, to name a few.
Keywords: socioeconomic status, health, human capital, health behaviour
JEL Codes: D91, I10, I12, I14, J24
Disparities in health across socioeconomic status (SES) groups – often called the SES-health gradient – are substantial. For example, Case and Deaton (2005) show how in the United States, a 20 year old low-income (bottom quartile of family income) male, on average, reports to be in similar health as a 60 year old high-income (top quartile) male. In cross sectional data the disparity in health between low and high SES groups appears to increase over the life cycle until ages 50–60, after which it narrows. These patterns exist across a wide range of measures of SES, such as education and wealth, and across all indicators of health, including the onset of chronic diseases, disability and mortality (e.g., Adler et al., 1994; Marmot, 1999). The pattern is also remarkably similar between countries with relatively low levels of protection from loss of work and health risks, such as the U.S., and those with stronger welfare systems, such as the Netherlands (Case and Deaton, 2005; Smith, 2007; Van Kippersluis et al., 2010).
Recent significant contributions to the understanding of socioeconomic disparities in health have concentrated on the identification of causal effects, but have stopped short of uncovering the underlying mechanisms that produce the causal relationships. For example, education is found to have a causal protective effect on mortality (Lleras-Muney, 2005) but it is not known exactly how the more educated achieve their health advantage (Cutler and Lleras-Muney, 2010).
Case and Deaton (2005) argue that it is extremely difficult to understand the relationships between health, education, income, wealth and labor-force status without some guiding theoretical framework. Integrating the roles of proposed mechanisms and their long-term effect into a theoretical framework allows researchers to disentangle the differential patterns of causality and assess the interaction between mechanisms. Such understanding is essential in designing effective policies to reduce disparities (Deaton, 2002). It is no surprise then that several authors (e.g., Case and Deaton, 2005; Cutler, Lleras-Muney and Vogl, 2011) have pointed to the absence of a theory of SES and health over the life cycle and have emphasised the importance of developing one.
This paper develops a conceptual framework for health and SES in which the SES-health gradient is the outcome of rational (constrained) individual choices made over the life cycle. The paper makes two main contributions. The first main contribution is of a fundamental nature and consists of extending the canonical human-capital model for the demand for health (Grossman, 1972a,b) in two ways. First, we employ a relatively straightforward extension by allowing for decreasing returns to scale in health investment of the health-production process (see Galama and Kapteyn, 2011; Galama and Van Kippersluis, 2013, and Galama, 2015, for the reasoning behind this extension). Second, motivated by the observation that differences in medical care usage explain only a small part of the health gradient (e.g., Adler et al., 1993), we conduct an extensive review of the literature from multiple disciplines to identify the most important mechanisms through which socioeconomic characteristics such as wealth, earnings, and education, interact with health. We then include several additional decisions regarding health (besides health investment), such as choices regarding lifestyle (exercise, healthy/unhealthy consumption), working conditions, labor-force participation, and longevity, as mechanisms generating disparities in health. In doing so, we develop a comprehensive theory of the SES-health gradient, by integrating the most important interactions between health, longevity, health behaviour, and SES (wealth, education, and earnings) during adulthood.1
Because of the inclusion of a rich set of endogenous health behaviours, endogenous health, and endogenous longevity, the theory can be employed to analyze the value of health as well as the value of life. Previous papers employing a life-cycle model for the value of life include Rosen (1988), Ehrlich (2000), Becker (2007), and Kuhn et al. (2015). In contrast to these papers, but in line with Murphy and Topel (2006), we distinguish between the value of health and the value of longevity. We go beyond Murphy and Topel (2006) by treating health and longevity endogenously: individuals seek to optimise both health and longevity. We find that the value of health and the value of life are distinct concepts that vary with age and by SES in distinct ways. For example, calibrated simulations suggest the value of life decreases near the end of life whereas the value of health increases. Assessments of the value of a statistical life generally involve investigating how much individuals need to be paid for taking a certain risk of death (usually in a setting of hazardous work). In practice, such estimates may capture the monetary value (compensating variation) of both the effect of changes in health and changes in longevity. In our theory, individuals are willing to engage in a certain amount of unhealthy consumption or job hazards for the instantaneous benefits it provides, as long as these benefits outweigh the associated health cost: the reduction in life-time utility due to health loss. Our theory suggests that unhealthy job conditions as well as risky health behaviours may be used in empirical work to evaluate both the value of health and the value of life.
Our second main contribution consists of deriving detailed predictions from the theory by performing comparative dynamic analyses of the effects of wealth, earnings, education, and health on health behaviour and longevity. We are the first to perform such analyses analytically for a comprehensive theory with multiple health behaviours (to better model health) and multiple dimensions of SES (to model disparities in health for several measures of SES).2 The comparative dynamic analyses not only deliver novel predictions regarding the SES-health gradient (see below), but more generally provide an alternative and complementary method to calibration and / or estimation in exploring model characteristics. They provide a method for researchers to explore their own research questions of interest. The method can be applied to models of similar form, for example, human capital, health deficits, firm investment, rational addiction, habit formation, and resource extraction, to name a few. This work is therefore potentially also relevant to these and other areas of economics.
The comparative dynamic analyses provide insight into the mechanisms through which SES and health interact, and generate novel testable predictions. We highlight a few here and discuss these and several others more extensively in section 3.
First, wealth, earnings, and education affect health behaviour by increasing the marginal value of health relative to the marginal value of wealth. Intuitively, wealth, earnings, and the higher earnings associated with education relax the budget constraint. At higher levels of wealth, and hence consumption, only limited marginal utility is gained from additional consumption and it is not beneficial to consume more. In contrast, health extends length of life, providing additional time during which consumption, leisure, and health can be enjoyed. This leads higher SES individuals to place a higher value on their health and to invest more in it (Becker, 2007; Hall and Jones, 2007).
A higher marginal value of health, in turn, increases the marginal benefits of healthy consumption, and the marginal costs of unhealthy working (and living) environments, and unhealthy consumption. This leads to healthier behaviour and gradually to greater health advantage with age. The more rapidly worsening health of low SES individuals may lead to early withdrawal from the labour force and associated lost earnings, further widening the gradient in early- and mid-age. The model allows for a subsequent narrowing of the SES-health gradient, due to mortality selection and potentially because low SES individuals increase their health investment and improve their health behaviour faster as a result of their more rapidly worsening health. Our model is thus able to replicate the life-cycle patterns of the SES-health gradient.
Second, we predict a central role for our concept of a “health cost” of unhealthy behaviours. The health cost is the marginal value (in terms of life-time utility) of health lost due to detrimental health behaviours. It takes into account all future consequences of current health behaviour. As a result of differences in the health cost, our theory predicts that high SES individuals are more likely to drink moderately but less likely to drink heavily (Van Kippersluis and Galama, 2014); and that individuals are willing to accept unhealthy working conditions in mid-life, given the high monetary benefits during those years, but that their willingness declines later in life due to an increasing health cost. Thus, the concept of a health cost has potential for explaining variation in health behaviours over the life cycle and across SES groups.3
Third, we predict that the ability to postpone death (endogenous longevity) is crucial in explaining observed associations between SES and health. Absent the ability to extend life (fixed horizon), associations between SES and health are small. If, however, life can be extended, SES and health are positively associated and the greater the degree of life extension, the greater is their association. The intuition behind this result is that the horizon (longevity) is a crucial determinant of the return to investments in health. This suggests that in settings where it is difficult for wealthier, higher income and higher educated individuals to increase life expectancy (e.g., due to a high disease burden, competing risks, low efficiency of health investment, etc.), health disparities across socioeconomic groups would be smaller.
These are just a few examples of how the theory can be used as a conceptual framework in conjunction with the comparative dynamic analyses to generate testable predictions for the complex relationships between SES and health. The theory is rich, and it is impossible to produce an exhaustive list of its possible uses. Researchers can use the theory and detailed comparative dynamic analyses presented here as a template to study their own questions of interest.
The paper is organised as follows. Section 1 reviews the literature on health disparities by SES to determine the essential components required in a theoretical framework. Developing a theory requires simplification and a focus on the essential mechanisms relating SES and health. To keep the model relatively simple we focus on explaining health disparities in adulthood.4 We highlight potential explanations for the SES-health gradient that a) explain a large part of the gradient and b) are relatively straightforward to include in our theoretical framework. Based on these principles we develop our theoretical formulation in section 2. Section 3 presents dynamics and calibrated simulations, section 4 presents comparative dynamic analyses and makes predictions, and section 5 summarises and concludes.
1 Components of a Theory of the Gradient
In this section we review the empirical literature to determine the essential components of a theory of health disparities by SES in adulthood. Based on these findings we present our theoretical formulation.
A significant body of research across multiple disciplines (including epidemiology, sociology, demography, psychology, evolutionary biology, and economics) has been devoted to documenting and explaining the substantial disparity in health between low and high SES groups. The pathways linking the various dimensions of SES to health are diverse: some cause health, some are caused by health and some are jointly determined with health (e.g., Cutler et al., 2011). Several key findings can be identified.
Medical care
Utilization of medical services and access to care explain only a relatively small part of the association between SES and health (e.g., Adler et al., 1993). Therefore, additional mechanisms, besides medical care, have to be included in the model.
Work environment and lifestyle
Epidemiological research highlights the importance of lifestyles (e.g., smoking, drinking, caloric intake, and exercise), psychosocial and environmental risk factors, neighborhood social environment, acute and chronic psychosocial stress, social relationships and supports, sense of control, fetal and early childhood conditions, and physical, chemical, and psychosocial hazards and stressors at work (e.g., House et al., 1994; Lynch, Kaplan and Shema, 1997).
During adulthood, two of those mechanisms appear to be of particular importance: (i) working conditions, and (ii) lifestyles. Using three different datasets from the U.K. and the U.S., House et al. (1994) find that features of the psychosocial working environment, social circumstances outside work, and health behaviour jointly account for much of the social gradient in health. Some epidemiological studies suggest that around two thirds of the social gradient in health deterioration could be explained by working environment and lifestyle factors alone (Borg and Kristensen, 2000). Low SES individuals more often perform risky, manual labour than high SES individuals, and their health deteriorates faster as a consequence (Marmot et al., 1997; Ravesteijn et al., 2013). Case and Deaton (2005) find that those who are employed in manual occupations have worse health than those who work in professional occupations and that the health effect of occupation operates at least in part independently of the personal characteristics of the workers. Extensive research further suggests an important role of lifestyle factors, particularly smoking, in explaining SES disparities in health (Mackenbach et al., 2004). Fuchs (1986) argues that in developed countries, it is personal lifestyles that cause the greatest variation in health.
Education
Education appears to be a key dimension of SES and studies suggest education has a causal protective effect on health and mortality (Lleras-Muney, 2005; Conti et al., 2010; Van Kippersluis et al., 2011).5 Education increases wages (e.g., Mincer, 1974), thereby enabling purchases of health investment goods and services (though higher wages also increase the opportunity cost of time). Education potentially increases the efficiency of medical and preventive care usage and time inputs into the production of health investment (Grossman, 1972a; 1972b). The higher educated are also better able at managing their diseases (Goldman and Smith, 2002), and benefit more from new knowledge and new technology (Lleras-Muney and Lichtenberg, 2005; Glied and Lleras-Muney, 2008).
Financial measures of SES
Financial measures of SES may have a more limited impact on health than education. Smith (2007) finds no effect of financial measures of SES (income, wealth, and change in wealth) on changes in health. Cutler, Lleras-Muney and Vogl (2011) provide an overview of empirical findings and conclude that the evidence points to no, or a very limited, impact of income or wealth on health (see also Michaud and Van Soest, 2008). Yet, this view is not unequivocally accepted. For example, Lynch, Kaplan and Shema (1997) suggest that accumulated exposure to economic hardship causes bad health, and Herd, Schoeni and House (2008) argue that there might be causal effects of financial resources on health at the bottom of the income or wealth distribution. Income and wealth enable purchases of medical care and thereby potentially allow for better health maintenance. Further, more affluent workers may choose safer working and living environments since safety is a normal good (Viscusi, 1978). But, higher wages are also associated with higher opportunity costs, which would reduce the amount of time devoted to health maintenance.
Health and labor-force withdrawal
In the other direction of causality, studies have shown that perhaps the most dominant causal relation between health and dimensions of SES in adulthood is the causal impact that poor health has on one’s ability to work and hence produce income and wealth (e.g., Case and Deaton, 2005; Smith, 2007). Healthy individuals are also more productive and earn higher wages (Currie and Madrian, 1999).
Joint determination
Fuchs (1986) has argued that the strong correlation between SES and health may be due to differences in the time preferences of individuals, which affects investments in both education and health. Cutler and Lleras-Muney (2008) argue that differences in individual preferences (risk aversion and discount rates) appear to explain only a small portion of the SES-health gradient, but they also note that preferences are difficult to measure, and that preferences with respect to health may differ from preferences with respect to finance. Other third factors known to contribute to the correlation between SES and health are cognitive and non-cognitive skills, in particular conscientiousness and self-esteem (Auld and Sidhu, 2005; Chiteji, 2010; Conti et al., 2010; Savelyev, 2014).
Gradient over the life cycle
Health inequalities are largest in mid-life and narrow in later life. The literature provides competing explanations for this pattern. The cumulative advantage hypothesis states that health inequalities emerge by early adulthood and subsequently widen as economic and health advantages of higher SES individuals accumulate (House et al., 1994; Ross and Wu, 1996; Lynch, 2003). Any apparent narrowing of SES inequalities in late life is largely attributed to mortality selection, i.e., lower SES people are more likely to die which results in an apparently healthier surviving disadvantaged population.6 The competing age-as-leveler hypothesis maintains that later in life deterioration in health becomes more closely associated with age than with any other predictor, i.e. through a greater equalization of health risks (House et al., 1994), with the result that the SES-health gradient narrows.
2 Theory
2.1 Theoretical Formulation
In this section we formalise the above discussion on the features of a theoretical framework for the SES-health gradient over the life cycle. The aim is to understand the SES-health gradient as the outcome of rational constrained individual behaviour.
A natural starting point for a theory of the relation between health and SES is a model of life cycle utility maximization. Our model is based on the Grossman model of the demand for health (Grossman, 1972a; 1972b; 2000) in continuous time (see also Wagstaff, 1986a; Ehrlich and Chuma, 1990; Zweifel and Breyer, 1997; Galama, 2015). The Grossman model provides a framework for the interrelationship between health, financial measures of SES (wealth, wages, and earnings), the demand for consumption, the demand for medical goods and services, and the demand for time investments in health (e.g., visits to the doctor, exercise). Health increases earnings (through reduced sick time) and provides utility. We add six additional features to the model.
First, we assume decreasing-returns-to-scale (DRTS) in investment of the health-production process. This addresses the degeneracy of the solutions for investment and health that characterises commonly employed linear investment models (Ehrlich and Chuma, 1990; Galama, 2015). It is further attractive in that the health-production process is generally thought of as being subject to diminishing returns (Wagstaff, 1986b).
Second, individuals choose their level of “job-related health stress”, which can be interpreted broadly, ranging from physical working conditions (e.g., hard or risky labor) to psychosocial aspects of work (e.g., low social status, lack of control, repetitive work, etc.) that are detrimental to health. Individuals may accept risky and/or unhealthy work environments, in exchange for higher pay (Muurinen, 1982; Case and Deaton, 2005), i.e. a compensating wage differential (Smith, 1776; Viscusi, 1978).
Third, we allow consumption patterns to affect the health deterioration rate (Grossman, 1972b; Forster, 2001; Case and Deaton, 2005; see Cawley and Ruhm, 2012, for a review of theoretical models of health behaviours). We distinguish healthy consumption (such as the consumption of healthy foods, sports and exercise) from unhealthy consumption (such as smoking, excessive alcohol consumption). Healthy consumption provides utility, and is associated with health benefits in that it lowers the health deterioration rate. We interpret healthy consumption broadly to include decisions regarding housing and neighborhood.7 Unhealthy consumption provides consumption benefits (utility) but increases the health deterioration rate.
Fourth, the effect of education on income is included in a straightforward manner by assuming a Mincer-type wage relation, in which earnings are increasing in the level of education and in the level of experience of workers (e.g., Mincer, 1974).
Fifth, individuals endogenously optimise length of life (Ehrlich and Chuma, 1990). Longevity is an important health outcome and differential mortality by SES may explain part of the narrowing of the gradient in late life. Moreover, length of life is an essential horizon that determines the duration over which the benefits of health investments and healthy behaviours can be reaped.
Last, we include leisure, which jointly with sick time and time inputs into health investment and into health behaviour allows for the modelling of an implicit retirement decision. As health declines, increased sick time and increased demand for time inputs into health investment and healthy behaviour reduce the amount of time that can be devoted to work, capturing possible reverse causality from health to labour force participation, and thereby financial measures of SES.
Individuals maximise the life-time utility function
| (1) |
where time t is measured from the time an individual has completed her education and joined the labour force (e.g., around age 25 or so), T denotes total lifetime (endogenous), β is a subjective discount factor, and individuals derive utility U(t) ≡ U[Ch(t), Cu(t), L(t), H(t)] from healthy consumption Ch(t), unhealthy consumption Cu(t), leisure L(t), and health H(t). Utility is assumed to be strictly concave and increasing in its arguments.
Healthy Ch(t) and unhealthy Cu(t) consumption are produced following a Becker (1965) home-production model by combining goods, Xh(t) and Xu(t), purchased in the market and own time inputs, and
| (2) |
| (3) |
where and are (exogenous) efficiency factors.
The objective function (1) is maximised subject to three constraints. The first relates to the production of health capital
| (4) |
Health H(t) can be improved through health production I[m(t), τm(t); E]. Goods and services m(t) (e.g., medical care) as well as own time inputs τm(t) (e.g., exercise, time spent visiting a doctor, etc.) are used in the production of health I[m(t), τm(t); E]. We assume the following functional form
| (5) |
where the efficiency of the health-production process μI (t;E) is assumed to be a function of the consumer’s stock of knowledge E as the more educated are assumed to be more efficient consumers and producers of health (Grossman, 1972a; 1972b). The health-production function I[m(t), τm(t), E] is assumed to exhibit DRTS (0 < αI + βI < 1).
Health (equation 4) deteriorates at the health deterioration rate d(t) ≡ d[t, Ch(t), Cu(t), z(t), H(t); ξ(t)]. The health deterioration rate depends endogenously on healthy consumption Ch(t), unhealthy consumption Cu(t), job-related health stress z(t), and health H(t).8 Consumption can be healthy (∂d/∂Ch ≤ 0; e.g., healthy foods, healthy neighborhood) or unhealthy (∂d/∂Cu > 0; e.g., smoking). Greater job-related health stress z(t) accelerates the “aging” process (∂d/∂z > 0). The deterioration rate depends in a flexible way on health, instead of the usual assumption of a linear relationship d(t) = δ(t)H(t) as in Grossman (1972a;b) and the related literature (but see Dalgaard and Strulik, 2014, for an exception), and ξ(t) denotes a vector of exogenous environmental conditions. Last, we have a fixed initial H(0) = H0 and a fixed end condition H(T) = Hmin for health.9
The second constraint is the total time budget Ω,
| (6) |
where the total time available in any period Ω is the sum of all possible uses τw(t) (work), L(t) (leisure), τm(t) (health investment), (healthy consumption), (unhealthy consumption) and s[H(t)] (sick time).
The third constraint concerns the dynamic relation for financial assets:
| (7) |
Assets A(t) provide a return r (the return on capital), increase with income Y (t) and decrease with purchases in the market of healthy consumption goods Xh(t), unhealthy consumption goods Xu(t), and medical care m(t), at prices , , and pm(t), respectively. We have a fixed initial A(0) = A0 and a fixed end condition A(T) = AT for wealth, and assume that individuals face no borrowing constraints.10
Income Y (t) ≡ Y [H(t), z(t); E, x(t)] is assumed to be an increasing function of health H(t) (∂Y/∂H > 0) and of job-related health stress z(t) (∂Y/∂z > 0; Case and Deaton, 2005). We follow Grossman (1972b,a; 1972b,a; 2000) and model income Y (t) as the product of the wage rate w(t) and time spent working τw(t),
| (8) |
Individuals receive wages w(t) ≡ w[t, z(t); E, x(t)], which are a function of job-related health stress z(t)
| (9) |
where γw ≥ 0 and w*(t) ≡ w*[E, x(t)] represents the “stressless” wage rate, i.e., the wage rate associated with the least job-related health stress z(t) = 0.11 The stressless wage rate w*(t) is a function of the consumer’s education E and experience x(t) (e.g., Mincer, 1974),
| (10) |
where education E is expressed in years of schooling, x(t) is years of working experience, and ρE, βx and are coefficients, assumed to be positive.
Thus, we have the following optimal control problem: the objective function (1) is maximised with respect to the control functions L(t), Xh(t), , Xu(t), , m(t), τm(t), z(t), the parameter T, and subject to the constraints (4), (6) and (7).
The Hamiltonian (see, e.g., Seierstad and Sydsaeter, 1987) of this problem is:
| (11) |
where qH(t) is the marginal value of remaining life-time utility (from t onward) derived from additional health capital
| (12) |
and qA(t) is the marginal value of remaining life-time utility derived from additional financial capital
| (13) |
T* denotes optimal length of life, and U(∗) denotes the maximised utility function (see, e.g., Caputo, 2005).
The condition for optimal longevity T follows from the dynamic envelope theorem (e.g., Caputo, 2005, p. 293):
| (14) |
The marginal value of life extension is given by . When dividing by the marginal value of wealth, one obtains a measure for the monetary value of life, . The monetary value of life is similar to the expressions obtained in Rosen (1988) (his equation 16) and Murphy and Topel (2006) (their equations 7 and 8), for health-neutral consumption. Our measure is richer since it additionally takes into account asset accumulation and health depreciation.
2.2 First-Order Conditions
In this section we discuss the first-order conditions for optimization. We assume that an interior solution to the optimization problem exists. Detailed derivations are provided in Appendix A. The first-order condition for health investment is given by
| (15) |
where qh/a(t) represents the marginal benefit of health investment, defined as the ratio of the marginal value of health, qH(t), to the marginal value of wealth, qA(t) (throughout the paper we refer to qh/a(t) as the relative marginal value of health):
| (16) |
and πI(t) represents the marginal cost of health investment,
| (17) |
The marginal benefit of health investment increases in the marginal value of health qH(t) and decreases in the marginal value of wealth qA(t). If the marginal value of health is high individuals invest more in health, and if the marginal value of wealth is high individuals invest less, consume less, and save more.
For the functional form (5) we can express the marginal cost of health investment πI(t) as follows (see Appendix B for detail)
| (18) |
| (19) |
The marginal cost of health investment πI(t) increases with the level of health investment goods and services m(t) and time inputs τm(t) due to decreasing returns to scale 0 < αI + βI < 1,12 with the price of medical goods and services purchased in the market pm(t), and with the opportunity cost of time w(t), where the latter is a function of job-related health stress, z(t).
The first-order condition for leisure is
| (20) |
a standard result equating the marginal utility of leisure ∂U/∂L to the marginal cost of leisure, which is a function of the marginal value of initial wealth qA(0), the individual’s wage rate w(t), and the difference between the time preference rate β and the return on capital r.
The first-order condition for healthy consumption is
| (21) |
where is the marginal monetary cost of healthy consumption Ch(t)
| (22) |
and is the marginal health benefit of healthy consumption
| (23) |
The marginal monetary cost of healthy consumption (equation 22) is a function of the price of healthy consumption goods and services and the opportunity cost of time w(t), and represents the direct monetary cost of consumption. The marginal health benefit of healthy consumption (equation 23), is equal to the product of the relative marginal value of health qh/a(t) and the “amount” of health saved ∂d/∂Ch, and represents the marginal value of health saved.
Similarly, the first-order condition for unhealthy consumption is
| (24) |
where is the marginal monetary cost of unhealthy consumption Cu(t) (direct monetary cost)
| (25) |
and is the marginal health cost of unhealthy consumption (marginal value of health lost)
| (26) |
The first-order condition for unhealthy consumption (24) is similar to the condition for healthy consumption (21). The difference lies in the marginal health cost (rather than health benefit) of unhealthy consumption, which has to be added rather than subtracted from the marginal monetary cost of unhealthy consumption .
Last, the first-order condition for job-related health stress is
| (27) |
where φz(t) ≡ φz[t, H(t), z(t); E, x(t)] is the marginal production benefit of job-related health stress
| (28) |
reflecting the notion that job-related health stress is associated with a compensating wage differential (greater earnings), and πdz(t) ≡ πdz[t, H(t), Ch(t), Cu(t), z(t); E, x(t), ξ(t)] is the marginal health cost of job-related health stress (marginal value of health lost)
| (29) |
2.3 The Health Cost and Health Benefit of Health Behaviour
From the first-order conditions follows that lifestyle decisions regarding consumption and occupation provide utility (directly or indirectly), and are associated with a monetary cost and with an opportunity cost. However, in contrast to conventional economic models, in our theory, these lifestyle decisions are additionally associated with a “health benefit” or a “health cost”. The health cost (benefit) is given by
| (30) |
where the variable x represents the relevant health behaviour (e.g., unhealthy consumption, or hard physical labor), and the definition of qh/a(t) is given by (12), (13), and (16). From (16), (43) and (44) follows
| (31) |
The health cost (benefit) is the amount of health “lost” (“saved”) due to the health behaviour ∂d/∂x times the relative marginal value of health qh/a(t) (the “price” or “value” of health, measured in life-time monetary units [e.g., US dollars] per unit of health, see 31). In simple terms, unhealthy consumption worsens health, and the health cost is the value one attaches to the lifetime consequences of reduced health. These lifetime consequences consist of the discounted additional (marginal) utility (qA(0)−1 ∂U/∂He−(β−r)s in 31) plus the additional earnings (production benefit) derived from better health (∂Y/∂H in 31), over the remainder of life (from t till T). They are discounted at the rate r+∂d/∂H, where ∂d/∂H represents the cost of holding the stock of health and r represents the opportunity cost (i.e. one could alternatively invest in assets).
There are assymetries between health costs and health benefits. For healthy consumption the time investments and monetary costs are incurred today (and so is utility, if any, from its consumption), while the health benefits are reaped in the future. For unhealthy consumption the opposite holds: it provides pleasure (and requires time investments and monetary costs) today, while the health costs occur in the future. This implies that discount rates matter, as well as information on the healthiness or unhealthiness of the good ∂d/∂x. Individuals who discount the future heavily (large β in 31) or who underestimate the health consequences, will engage more in unhealthy consumption. Likewise, individuals who discount the future or underestimate the health gains from healthy consumption will engage less in healthy consumption.
Assessments of the value of a statistical life (VSL, see Viscusi and Aldy, 2003, for a review) generally involve investigating the risk of death that people are willing to take (usually in a setting of hazardous work) and how much they should be paid for taking these risks. An analogous concept is captured in, e.g., the first-order condition for job-related health stress (27), which weighs the wage premium of engaging in unhealthy / risky jobs today with the costs in terms of the lifetime consequences of reduced health (and associated longevity). In our theory, individuals are also willing to engage in a certain amount of unhealthy consumption for the utility it provides, as long as this benefit outweighs the associated health cost: the reduction in life-time utility due to health loss associated with unhealthy consumption. Thus, our theory provides a framework for determining the value of life and the value of health in settings outside of hazardous work, e.g., by exploiting unhealthy behaviours.
As we discuss in the remainder of the paper, the health cost and health benefit of behaviour are promising concepts for understanding a wide range of health behaviours, as well as the socioeconomic disparities in these behaviours.
2.4 Assumptions
Apart from the earlier mentioned assumptions of diminishing returns to scale (DRTS) of investment m(t), τm(t), in the health-production function I[m(t), τm(t); E] (0 < αI +βI < 1), and diminishing marginal utilities of healthy Ch(t) and unhealthy consumption Cu(t), of leisure L(t), and of health H(t), we further assume:
- Diminishing marginal production benefit of health ∂2Y/∂H2 < 0, diminishing marginal production benefit of job-related health stress ∂2Y/∂z2 < 0, diminishing marginal health benefit of healthy consumption , and diminishing returns to longevity (see 14)
where T* denotes optimal length of life and U(∗) denotes the maximised utility function (see, e.g., Caputo, 2005).(32) Increasing or constant returns to scale in the marginal health cost of unhealthy consumption (as in Forster, 2001)13 and in the marginal health cost of job-related health stress ∂2d/∂z2 ≥ 0.
- Cobb-Douglas CRTS relations between the inputs (goods/services purchased in the market and own-time) and the outputs healthy consumption Ch(t), and unhealthy consumption , and , where , are the elasticities of the outputs with respect to goods and services, and , are the elasticities of the outputs with respect to time inputs. As a result we have (see equations 22 and 25):
(33) (34) -
First-order direct effects dominate higher-order indirect effects for control variables. For example, wealth affects healthy consumption directly, but also indirectly through its effect on unhealthy consumption, since unhealthy consumption affects healthy consumption through its effect on utility and on health deterioration. The assumption, in this particular example, is that the direct effect of wealth on healthy consumption dominates any indirect wealth effect that operates through unhealthy consumption or through any other control variable.
Second- and higher-order terms are often ignored since they tend to be quantitatively less important (e.g., first-order Taylor series approximations). Moreover, additively separable utility functions are fairly conventional in the literature (e.g., Zeckhauser, 1970; Gjerde et al., 2005; Hall and Jones, 2007), and assuming that utility is additively separable, and that the health deterioration rate is additively separable, would lead to similar results. The difference is that we require second-order terms to be small, not that they are identical to zero, and we do not make the assumption for state variables since small differences can grow large over time. Thus, e.g., the marginal utility of healthy consumption is still a function of health (e.g., Finkelstein et al., 2013). Therefore, our assumption is less restrictive than the fairly conventional assumption of functions being additively separable in their arguments. We provide more detail in Appendix D.
In addition to these four assumptions, we need further information to be able to conduct the comparative dynamic analyses (section 4). In particular, we need the sign of ∂d/∂H, ∂qA(t)/∂A(t), and ∂qA(t)/∂H(t). For this reason, in the next section, we calibrate a simple version of the model to establish which signs are plausible. We obtain these as our “benchmark” relationships. From the calibrated model we have
∂d/∂H > 0,
∂qA(t)/∂A(t) < 0; ∂qA(t)/∂wE < 0; ∂qA(t)/∂E < 0,
∂qA(t)/∂H(t) < 0.
The calibrated model suggests that health increases aging at a diminishing rate, i.e. ∂d/∂H ≥ 0 and ∂2d/∂H2 ≤ 0. This suggests that the health of healthy individuals deteriorates faster in absolute terms (since they have more of it) but not in relative terms (as a percentage of total health). Further, the calibrated model suggests diminishing returns to wealth , i.e. poorer individuals derive greater benefits from an additional increment of wealth than wealthier individuals. Finally, the calibrated model suggests unhealthier individuals derive greater benefits from an additional increment of wealth ).14 This suggests health and wealth are to some extent substitutable in financing consumption and leisure (e.g., Muurinen, 1982; Case and Deaton, 2005).15
In the Appendix we also explicitly investigate the sensitivity of our predictions to the opposite signs of the above relations to assess the robustness of our results.
3 Dynamics and Numerical Calibration
In this section we begin with a study of the life-cycle profiles of health and health investment. Theoretically, the model’s predictions for these life-cycle patterns are ambiguous. We therefore calibrate a simple version of the model to investigate whether for a realistic set of parameter values it is able to reproduce empirical stylised facts. We then use findings from the calibrated simulations to make predictions for the life-cycle trajectories of healthy and unhealthy consumption and job-related health stress.
3.1 Health Investment and Health Over the Life Cycle
A quick glance at the first-order conditions in section 2.2 shows that the relative marginal value of health qh/a(t) is an important driver of health investment (and more generally of health behaviour). Specifically, note that from (15), (18) and (19) we obtain
| (35) |
| (36) |
Thus, health investment increases with the marginal value of health. Hence, to understand health investment we first investigate the dynamics of the relative marginal value of health qh/a(t) and of health H(t). We then discuss the implications of these dynamic patterns for health behaviours.16
Individuals start life generally in good health at H(0) = H0, while the terminal health stock H(T) is constrained to the minimum health level Hmin, below which life cannot be sustained. This implies that health decreases over the life cycle. Indeed, empirical evidence suggests that health falls over the life cycle, first slowly and then more rapidly in old age (e.g., Deaton and Paxson, 1998; Van Kippersluis et al., 2009; Dalgaard and Strulik, 2014).
The evolution of the relative marginal value of health qh/a(t) is given by
| (37) |
(combine equations 43 and 44 of Appendix A). Recall that the relative marginal value of health qh/a(t) is the ratio of the marginal value of health qH(t) and the marginal value of wealth qA(t). The marginal value of wealth depreciates with age at the rate of return on capital r (see 43). The marginal value of health qH(t) however, may increase or decrease with age. As long as qH(t) appreciates, or depreciates more slowly than qA(t), the relative marginal value of health qh/a(t) will increase with age.
Empirical evidence suggests that health investments increase with age: medical expenditures peak in the final phase of life (Zweifel, Felder and Meiers, 1999),17 and other components of health investment either increase or stay relatively flat with age (Podor and Halliday, 2012). This suggests that the relative marginal value of health increases with age (see 15).
Theoretically our model allows for these patterns, but does not unambiguously predict them. In the next section, therefore, we resort to calibrated simulations to investigate whether our model, for a realistic set of parameter values, is able to reproduce these empirical stylised facts.
3.2 Calibrated Simulations
Our calibrated simulations proceed in several steps. First, we compute five-year averages for a health index and for health investment and treat these as the data “moments” for our calibration. Following Poterba, Venti and Wise (2011; 2013), we construct a health index using 1999–2013 U.S. Panel Study of Income Dynamics (PSID) data of a rich set of health measures, including: (i) a binary indicator of poor self-reported health; (ii) diseases such as acute myocardial infarctions (AMI), arthritis, asthma, cancer, diabetes, heart conditions, high blood pressure, learning disorders, lung disease, and stroke; (iii) mental health problems, (iv) activities of daily living (ADLs), and (v) body-mass index (BMI). We arbitrarily scale this health index such that initial health is equal to 100 and health at age 80 is equal to 15. We obtained age profiles for health investment from Halliday et al. (2017) who computed health investment expenditures from the U.S. Medical Expenditure Survey (MEPS). Figure 1 shows the life-cycle patterns of health and health investment, where the dots indicate the average of the health index and of health investment in 5 year age groups. As the Figure shows, health declines in a concave manner over the life cycle, while health investment increases rapidly in old age. These are stylised facts our model of health production ought to reproduce.
Figure 1.
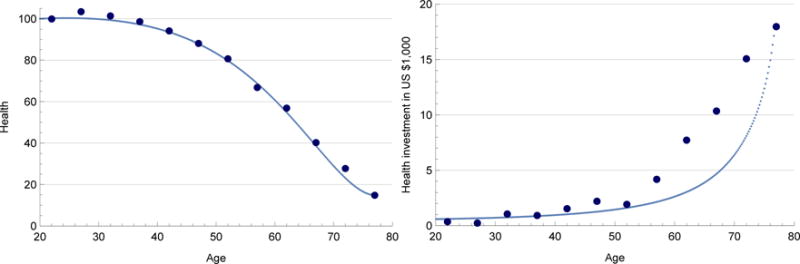
Model simulation of health (left figure) and health investment (right figure) using calibrated parameter values in Table 1. The solid lines indicate the model simulations, and the dots indicate the empirical data moments constructed from PSID (health) and MEPS (health investment).
Second, we estimate the hourly wage profile using the PSID data and a Mincer equation of log hourly wages on dummies for each educational level and a quadratic polynomial in age. The estimated parameters are as follows
| (38) |
where D is a dummy for a college degree, t measures age, and we multiply by 2 to obtain the yearly wages in thousands of dollars (assuming individuals work for 40 hours, 50 weeks per year). This Mincer-type wage equation for a college graduate starts with annual wages of $30, 000 per year at age t = 20 and peaks at $45, 000 per year at age t = 50 after which wages gradually decline.
Third, we numerically simulate a simplified version of our model (see Appendix C for details). Since the aim is to investigate whether our model is capable of reproducing the stylised facts regarding the life-cycle profiles of health and health investment, we omit the time inputs into consumption and health investment, omit the distinction between healthy and unhealthy consumption, and omit job-related health stress.
We assume a constant relative risk aversion (CRRA) utility function with scale parameter μU of the form
| (39) |
where 0 ≤ ζ ≤ 1 is the relative “share” of consumption versus health, ρ is the coefficient of relative risk aversion, and B is a constant to ensure that utility is positive (Hall and Jones, 2007). We follow Scholz and Seshadri (2016) in modelling sick time as , and use a flexible functional form for health production
| (40) |
where 0 < α < 1, and following Cropper (1981) and Wagstaf (1986a). This functional form is flexible enough to capture various possible relationships between the deterioration rate ( ) and health. For example, ν = 1 represents the Grossman case, while ν < 0 is akin to the health-deficit model by Dalgaard and Strulik (2014), in which the health of unhealthy individuals deteriorates faster. The functional form also depends in a flexible way on calendar age t.
No consensus exists over what causes aging with many theories attempting to explain what drives it. Two important classes of theories are prominent. The first class consists of “deficit-based theories”, where aging occurs predominantly as a result of the accumulation of deficits (or “damage”). For example, Arking (2006) advocates a theory of aging in which health decline is independent of calendar age, depending solely on the level of health, i.e. as in a model of aging due to wear and tear (see also Dalgaard and Strulik, 2014). The second class consists of “programmed theories of aging”, where aging is predominantly the result of genetically regulated or predetermined processes (Longo et al., 2005, de Magalhaes 2003, 2011, 2014). Such processes exhibit “pure” calendar age effects. De Magalhaes (2011) writes for example: ‘… it is now largely recognised that ageing (…) is not primarily the result of damage to irreplaceable body parts’ and that there is a role for ‘… genetically regulated processes or predetermined mechanisms’ (de Magalhaes, 2011). Further, Longo et al. (2005) provide evidence for genetic programming ‘that regulates the level of protection against stochastic damage, and therefore the length of time an organism remains healthy’. Finally, so-called aging-clock theory, which also falls within the programmed theories, stipulates that ‘Aging is programmed into our bodies, like a clock ticking away from the moment of conception’ (Moody and Sasser, 2014). The two classes of theories are not mutually exclusive; and there is in fact wide recognition that aging exhibits genetic programming or predetermined, and accumulated deficits aspects, with disagreement about their relative importance. We therefore choose to remain agnostic about the aging process, using a specification that is flexible enough to encompass both deficits as well as calendar age aspects of aging. In essence, we ask the data which aspects of aging are important in our model for a good fit. We find that both calendar age and deficits features are needed.
Fourth, we fix a large number of model parameters by taking values from the literature (see Table 1 in section C). In particular, we set α = 0.75 in line with Hugonnier et al. (2013, 2016) who use values of 0.69 and 0.77, respectively. We follow Scholz and Seshadri (2016), setting A0 = AT = 0, ρ = 3, ζ = 0.7 and γ = 1.7.18 We follow Blau (2008) and DeNardi et al. (2016), setting the time preference rate β = 0.03, and the interest rate r equal to β. We further normalise prices of consumption and health investment and the efficiency of consumption to 1. The remaining parameters to be calibrated are ν, μI, μU, and the parameters a and b of the deterioration rate .
Given the data moments and our model solutions, we calibrate the parameters ν, μI, μU, a and b using a Method of Simulated Moments (MSM) approach (see Appendix C for details). Admittedly, this parameter space leaves many degrees of freedom. We do not claim our parametrization is unique. See for example Dalgaard and Strulik (2014) for an alternative framework using health deficits that is also able to reproduce the life-cycle profiles for health and health investment. Our aim is more modest: to illustrate that for a realistic set of parameter values the model can reproduce the empirical stylised facts. Table 1 in Appendix C provides the fixed and calibrated parameter values, and Figure 1 shows the resulting simulated profiles (solid lines) alongside the empirical moments (dots). For this realistic set of parameter values, the fit of our simulated profiles is fairly accurate. The model can generate empirically plausible trajectories.19
The calibrated simulations provide three additional pieces of information. First, the calibrated simulations suggest an optimal length of life of T = 76.8 years.
Second, our calibration establishes a benchmark for the sign of relationships we require to obtain comparative dynamic results. The parameter value ν = 0.3 in equation (40) is consistent with ∂d/∂H ≥ 0 and ∂2d/∂H2 ≤ 0. Further, in counterfactual simulations where we increase A0 and H0 by a small amount, we obtain ∂qA(0)/∂A0 < 0 and ∂qA(0)/∂H0 < 0 (see Table 2 in Appendix C).
Third, the calibrated model demonstrates that while health declines, the relative marginal value of health increases, with age. We will use these life-cycle patterns to derive from theory the implied life-cycle profiles for healthy and unhealthy consumption and job-related health stress in the general model.
3.3 Health Behaviour Over the Life-Cycle
As illustrated by the calibrated simulations, for plausible parameter values, the relative marginal value of health qh/a(t) increases with age. This would suggest that the health cost of unhealthy consumption and of job-related health stress and the health benefit of healthy consumption increase with age.20 Smoking rates are 8.9% among the 65+ compared to 21.6% among the 25–44 (US DHHS, 2014), and intake of fruit and vegetables increases with age (Serdula et al., 2004; Pearson et al., 2005). These patterns are consistent with the notion that the health benefit of healthy behaviour and the health cost of unhealthy behaviour increase with age: individuals start caring more about their health when they get older.
With declining health H(t) and an increasing marginal value of health qh/a(t) with age we obtain the following life-cycle patterns for health behaviours. Early in life, individuals are generally healthy and therefore plausibly value health less (see Table 2 in Appendix C and propositions 5 and 7, section 4.3). As a result, they invest less in their health (equation 15), engage more in unhealthy consumption (see 24), and less in healthy consumption (see 21). As individuals age, declining health becomes a burden as poor health reduces utility and increased sick time reduces earnings. As a result, the benefits of health increase and individuals invest more in health, shift toward healthier consumption, and reduce the level of job-related health stress. This general trend of improved health behaviour may be partially reversed in mid life, as wages peak, leading to a higher opportunity cost of time. This may result in a reduction in health investment and healthy consumption in mid life, relative to a general trend of improved health behaviours with age.
The pattern for job stress is distinct. Early in life the health cost of job stress qh/a(t) [∂d/∂z] is low, but so is the marginal benefit of job stress ∂Y/∂z (see 27). As wages increase, the benefit of job-stress increases. After mid age, declining health reduces the marginal benefit of job-stress, as sick time reduces the time available for work and wages plateau or even decrease. This suggests a pattern in which job stress initially increases as the marginal benefit of job-stress increases due to wage growth, followed by a decline in job stress due to plateauing or declining wages, increasing sick time, and an increasing health cost of job stress with age.
Prediction 1
Individuals in mid life plausibly accept unhealthy working conditions as they value the associated wage premium, but as they age they seek to engage in healthier work.
4 Variation in Health behaviour by SES and Health
Comparative dynamic analyses allow exploration of the effect of SES and health on the life-cycle trajectories of the control and state variables. We investigate the change in the optimal trajectory in response to variation in initial conditions or other model parameters, by comparing the “perturbed” optimal trajectory with respect to the “unperturbed” (or original) trajectory. Comparative dynamic analysis is an alternative to numerical simulation that has the benefit of being less restrictive by allowing for quite general functional forms (i.e. that utility be concave rather than, e.g., CRRA). Moreover, as Dalgaard and Strulik (2015, p.2) put it: ‘A purely numerical analysis entails a danger of neglecting general properties and implications of the model’.
Our emphasis is on exploring differences in constraints related to SES and health.21 Common measures of SES employed in empirical research are wealth, earnings (income), and education. Here we provide an intuitive discussion of the comparative dynamic results, supported by a number of propositions, whose formal proof we relegate to the Appendix.
The effect of variation in an initial condition or other model parameter δZ, where we are particulary interested in Z = {A0, wE, E, H0}, on any control or state variable g(t) can be separated into two components22
| (41) |
where the first term on the right-hand side (RHS) represents the response to variation in Z for constant T and the second term on the RHS represents the additional response due to the associated variation in T.
4.1 Variation in Initial Wealth, δA0
Let us focus first on the hypothetical case where length of life T is fixed. Contrasting the fixed T case with the general case where T is free provides us with useful insights regarding the properties of the model. This scenario may represent a developing nation with a high disease burden (where there may be lack of access to medical or public health technology, and competing risks from many diseases), the developed world, if it were faced with diminishing ability to further extend life, or individuals with a disease that severely limits longevity, such as Huntington’s disease (Oster, Shoulson and Dorsey, 2013).
-
◦
PROPOSITION 1: Absent ability to extend life, wealthy individuals, ceteris paribus, value health only marginally more than less wealthy individuals. For proof see Appendix D.1.
For fixed length of life T, additional wealth δA0 increases the relative marginal value of health initially, , but eventually the relative marginal value of wealth decreases with respect to the unperturbed path, . This result is illustrated in Figure 2, where the thick solid line labelled “Unperturbed” represents the unperturbed trajectory of the relative marginal value of health qh/a(t) versus age t, and the dotted line labelled “T fixed” represents the perturbed path for fixed T. Note that both curves end at t = T. The intuition is that the relative marginal value of health cannot be higher at all times, as this would be associated with higher health investment, improved health behaviour (see the first-order conditions in section 2.2), and a longer life, violating the condition that end of life occurs at t = T (fixed) at the minimum health level H(T) = Hmin. Indeed, simulations confirm this pattern: in the calibrated model, for individuals with higher initial wealth, the marginal value of health is higher up to age 70 and lower thereafter.23 The response to additional wealth is thus muted as the individual is forced to invest less later in life in order not to extend life. Hence, the first term on the RHS of equation (41) is small for variation in wealth A0.
Figure 2.
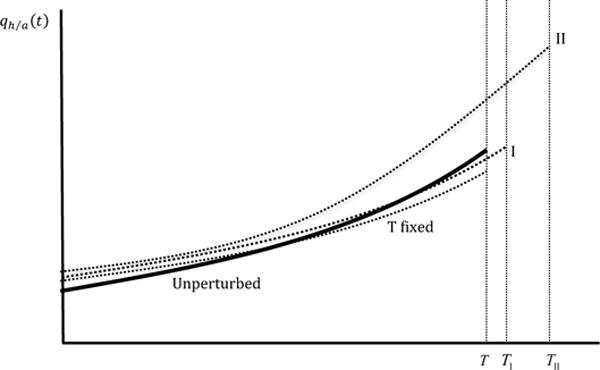
Evolution of the relative marginal value of health qh/a(t) with age due to variation in A0. The solid thick line, labelled “Unperturbed”, represents the unperturbed path. The perturbed paths are shown for the T fixed case (dotted line, labelled “T fixed”), scenario I, associated with small life extension TI (dotted line, labelled “I”), and scenario II, associated with large life extension TII (dotted line labelled “II”).
Let us now turn to the more interesting case where individuals can optimally choose T; they not only invest in the quality of life but also in the quantity of life.
Individuals optimally choose longevity T such that the marginal value of life extension is zero at this age, (see 14),
| (42) |
where for reasons of exposition we have divided by qA(T). As (42) shows, the marginal benefit of extending life consists of the additional utility from consumption and health. The marginal costs consist of the increasingly binding wealth and health constraints, due to declining wealth and declining health near the end of life.24 With declining health, the utility U(t) gained over the extra years decreases, and thereby the marginal benefit of life extension. The calibrated simulation shows that qh/a(t) increases rapidly with age as health declines, suggesting that the marginal cost of life extension does too. Eventually, the depreciation of health and decumulation of assets render additional life extension non-optimal.
As we will see, ability to extend life changes the picture dramatically as life extension increases the return to health investment by increasing the period over which a multitude of benefits of health can be accrued. The results can be summarised by propositions 2 and 3.
-
◦
PROPOSITION 2: Wealthy individuals live longer: ∂T/∂A0 > 0. For proof see Appendix D.2.
-
◦
PROPOSITION 3: Wealthy individuals value health more and are healthier at all ages. The more life can be extended, the stronger is the increase in the value of health in response to additional wealth. For proof see Appendix D.3.
Intuitively, at high values of wealth (and hence consumption), individuals prefer investing in health over consuming, since health extends life, the period over which they can enjoy the benefits of health, leisure and consumption, whereas additional consumption per period would yield only limited marginal utility due to diminishing utility of consumption (see also Becker, 2007; Hall and Jones, 2007). With sufficient wealth one starts caring more about other goods, in particular health. Wealthier individuals value health more relative to wealth, invest more, are healthier, and live longer (propositions 2 and 3).
The second part of proposition 3 is best understood by its visual representation in Figure 2. The extent to which individuals are able to extend life, ∂T/∂A0, depends on the model’s parameters r, α, μI, etc. These parameters are in turn determined by biology, medical technology, and environmental factors. If these factors are unfavorable to life extension (scenario I; small life extension), then individuals value health more early in life, but value health less later in life (the perturbed path starts higher, but eventually crosses the unperturbed path). This is the case we observe in our calibrated simulations. The pattern of initially higher investment, and subsequently lower investment, closely resembles that of the fixed T case (see proposition 1).
In contrast, if additional wealth affords considerable life extension (scenario II), the relative marginal value of health is higher at all times. Life extension raises the return to health investment and healthy behaviours. Further, utility from leisure and consumption can be enjoyed with additional years of life. Health also generates additional wealth from work, reinforcing the effect of the initial endowment of wealth δA0. Together, these various benefits substantially raise the value of health, leading to improved health behaviours, better health throughout life, and greater longevity. This leads to the following prediction.
Prediction 2
Health disparities are larger in environments where the wealthy can effectively use their resources to extend life.
Propositions 2 and 3 also allow gauging the predicted response of an increase in wealth on health behaviours. A higher relative marginal value of health directly increases the health benefit of healthy behaviour, and the health cost of unhealthy behaviour. Plausibly, this represents the dominant effect,25 consistent with wealthy individuals behaving healthier (e.g., Cutler and Lleras-Muney, 2010; Cutler, Lleras-Muney and Vogl, 2011; Cawley and Ruhm, 2012), and consistent with less affluent individuals responding more strongly to an unanticipated wealth shock (Van Kippersluis and Galama, 2014).
Prediction 3
Wealthy individuals shift consumption toward healthy consumption: they consume more healthy and moderately unhealthy consumption goods and services, but fewer severely unhealthy consumption goods and services.
The comparative dynamic effect of wealth on healthy consumption can be decomposed into a “direct” and an “indirect” wealth effect. The direct wealth effect is positive: an increase in wealth affords more healthy consumption (see Table 2 in Appendix C). Yet, wealth also has an indirect effect: an increase in wealth leads to a higher relative marginal value of health qh/a(t) (proposition 3), which increases the health benefit of healthy consumption [−qh/a(t)∂d/∂Ch]. Both the direct and indirect effects operate in the same direction, and wealthy individuals engage more in healthy consumption: ∂Ch(t)/∂A0 > 0, at least initially.26
Similar to healthy consumption, additional wealth enables purchases of more unhealthy consumption goods – the direct wealth effect is positive. Yet, additional wealth also increases the marginal health cost of unhealthy consumption qh/a(t)∂d/∂Cu (the indirect wealth effect), through a higher relative marginal value of health qh/a(t). The indirect wealth effect competes with the direct wealth effect.
While we cannot a priori sign the relation between unhealthy consumption and wealth, the two competing effects predict an interesting pattern of behaviour. The health cost increases in the severity of its impact on health, (the degree of “unhealthiness” of the consumption good). This suggests that for moderately unhealthy goods the direct wealth effect would dominate, while for severely unhealthy goods the indirect wealth effect would dominate.
4.2 Variation in Wages, δwE, and education δE
-
◦
PROPOSITION 4: Permanently higher wages and education operate in a similar manner to an increase in wealth δA0 (propositions 1 through 3), with some differences: (i) the wealth effect is muted by the increased opportunity cost of time, (ii) permanent wages wE and education E also raise the production benefit of health, and (iii) education raises the efficiency of health investment. For proof see Appendix D.4.
It is important to distinguish between an evolutionary wage change and permanent differences in the wage rate w(t), i.e. permanent income. In our model of perfect certainty and perfect capital markets, an evolutionary increase in the wage rate w(t) raises the opportunity cost of time but does not affect the marginal value of wealth qA(t) (i.e. the life-cycle trajectory is unchanged). In contrast, if wages are permanently higher, i.e. larger wE in (10), earnings are higher over the entire life cycle,27 and in addition to the opportunity cost of time effect, there is also a wealth effect (operating by decreasing the marginal value of wealth qA(t); see Table 2 in Appendix C). Further, the production benefit of health is higher as higher wages increase the value of health in reducing sick time.
There are reasons to believe that the wealth effect and the effect of a higher production benefit of health dominate the opportunity cost of time effect. First, this is consistent with the result by Dustmann and Windmeijer (2000) and Contoyannis, Jones and Rice (2004) that a permanent wage change affects health positively, while a transitory wage increase affects health negatively. Second, it is consistent with the rich literature on SES and health that consistently finds that high-income individuals are generally in better health than low-income individuals.
Permanently higher wages due to education E (see equation 10) are also associated with an increased opportunity cost of time effect, a wealth effect, and higher production benefits. But, education also increases the efficiency μI(t; E) of health investment, as the educated are assumed to be more efficient consumers and producers of health. The efficiency effect of education has two implications. First, it increases total health investment I[m(t), τm(t); E]. However, improved efficiency implies that fewer inputs are required to obtain a certain level of investment, potentially reducing the market m(t) and time inputs τm(t) devoted to health investment (e.g., Grossman, 1972a;b). Second, it could potentially explain the stronger evidence for an effect of education on health and the weaker evidence for effects of income and wealth on health, since the efficiency effect does not operate for income and wealth (see section 1). Thus, among the socioeconomic indicators, education improves health behaviours and health potentially the most.
4.3 Variation in Initial Health, δH0
-
◦
PROPOSITION 5: Absent ability to extend life, healthy individuals, ceteris paribus, value health cumulatively less, . For proof see Appendix D.5.
For fixed length of life T, when starting off with a higher level of health, cumulatively the relative marginal value of health has to be lower over the life cycle, leading to cumulatively unhealthier behaviour and lower health investment, in order to arrive at Hmin over the same duration of life T. The calibrated model simulations confirm this pattern and Figure 3 illustrates it: the perturbed fixed T path (dotted line) lies below the unperturbed curve, and both end at t = T.28
Figure 3.
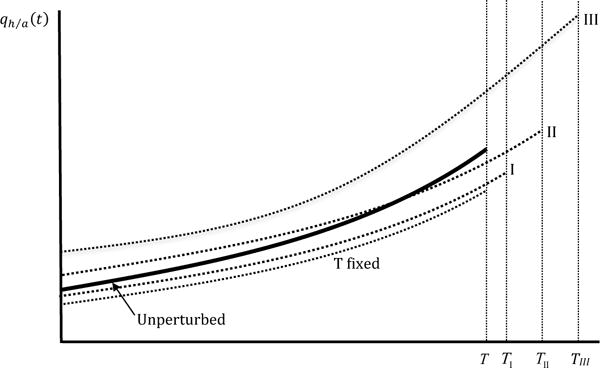
Evolution of the relative marginal value of health qh/a(t) with age due to variation in H0. The solid thick line, labelled “Unperturbed”, represents the unperturbed path. The perturbed paths are shown for the T fixed case (dotted line, labelled “T fixed”), scenario I, associated with small life extension TI (dotted line, labelled “I”), scenario II, associated with intermediate life extension TII (dotted line labelled “II”), and scenario III, associated with large life extension (dotted line labelled “III”).
-
◦
PROPOSITION 6: Healthy individuals live longer ∂T/∂H0 ≥ 0. For proof see Appendix D.6.
-
◦
PROPOSITION 7: Individuals with greater endowed health are healthier at all ages, ∂H(t)/∂H0 > 0, ∀t. For small life extension, they cumulatively value health less , for intermediate life extension they value health cumulatively more , and for large life extension they value health more at all ages, ∂qh/a(t)/∂H0 > 0, ∀t. For proof see Appendix D.7.
When T can be optimally chosen, individuals with greater endowed health are healthier throughout life, and live longer (proposition 6 and 7).29 We distinguish between three scenarios: “small”, “intermediate”, and “large” life extension, as illustrated in Figure 3 (see Appendix section D.7 and Figure 10 for more detail). For small life extension, healthier individuals value health more than in the fixed T case, but cumulatively still less than for the unperturbed path, and life is extended to TI. For intermediate life extension, the relative marginal value of health is cumulatively higher compared with the unperturbed path, but health is still valued less in old age. Life is extended to TII. For large life extension, the relative marginal value of health is higher at all ages, and life is extended to TIII. In such a scenario, healthy individuals care more about their health as for them investment pays off in terms of a longer lifespan over which the benefits of health, consumption, and leisure may be enjoyed. Since health investment increases in the value of health (see 15 and 17) it follows similar patterns in these three scenarios.
Which scenario is more plausible depends on the extent to which medical technology, institutional, and environmental factors, allow for endowed health to extend life (∂T/∂H0): in developed countries with few competing risks from diseases, universal access to health care, and cutting-edge medical technology, or in developing nations where large gains in longevity can potentially be achieved with relatively low cost interventions such as provision of clean water and improving sanitation. In our calibrated simulations for an average U.S. college graduate, we find ∂qh/a(t)/∂H(t) < 0 for all ages (see Table 2 in section C), which would be consistent with the “small” life extension scenario TI (see Figure 3 and for more detail Figure 10 in Appendix section D.7), and is consistent with the empirical regularity that healthy individuals consume less medical care (Van de Ven and Van der Gaag, 1982; Wagstaff, 1986a; Erbsland, Ried and Ulrich, 2002).30
4.4 Variation in Work, Leisure, and Retirement by SES and Health
Important variation exists across individuals both in the type of work and in the amount of time spent working, during a day and over the life cycle. We first discuss variation in the type of work, then turn to time spent working.
Work and job-related health stress
A higher relative marginal value of health qh/a(t) induced by wealth (proposition 3) increases the health cost of job-related health stress (see 29). Eventually, however, wealth leads to better health (proposition 3) and better health increases the marginal benefit ∂Y/∂z of job-related health stress through reduced sick time. Permanently higher wages, e.g., through better education, are also associated with the above competing wealth and health effects. In addition, the marginal benefit of job-related health stress ∂Y/∂z increases directly with the wage rate. Empirical evidence suggests that high SES individuals on average work in less demanding occupations (e.g., Ravesteijn, van Kippersluis and van Doorslaer, 2013). This suggests that higher SES increases the marginal costs of job-related health stress more than it increases its marginal benefits.
The effect of health on job-related health stress is plausibly positive. Better health reduces sick time, which increases the marginal benefit of job-related health stress. Further, if the relative marginal value of health decreases in health (proposition 5 and 7), then healthier individuals will have lower marginal costs of engaging in job-related health stress. With higher benefits and lower costs, we expect the healthy to engage in unhealthy jobs, consistent with empirical evidence (Kemna, 1987).
Leisure and retirement
To analyze retirement, we informally treat a small amount of time devoted to work τw(t), i.e. below a certain threshold, say τR, as a retirement phase. With declining health, time spent working τw(t) (see 6) gradually decreases, as a result of increasing sick time and the increasing demand for time devoted to health investment. Hence, the model produces a phase of life in old age that naturally qualifies as retirement. During working life, individuals divide their time between work, leisure, and time inputs into consumption and health investment (see 6). Therefore, we can infer the effect on the time spent working by investigating effects on leisure and time inputs.
Wealth increases the demand for leisure, for (time inputs into) healthy and unhealthy consumption, and for (time devoted to) health investment, through a “direct” wealth effect, reducing the marginal value of wealth qA(t), and an “indirect” value of health effect, increasing the relative marginal value of health (proposition 3). This leads wealthier individuals, ceteris paribus, to work less (see 6), and hence retire earlier, in line with empirical evidence (Imbens, Rubin and Sacerdote, 2001; Brown, Coile and Weisbenner, 2010).31 Permanently higher wages, e.g., through education, are also associated with the above wealth and value of health effects, but higher wages also increase the cost of time inputs, i.e. of leisure, of healthy and unhealthy consumption, and of health investment (see sections D.8.2 and D.8.3 in the Appendix). The higher opportunity cost of not working encourages higher educated individuals to retire later. Thus, the wealthy retire earlier, but the higher educated and those with higher permanent wages may retire later.
Healthier individuals spend more time working, as good health reduces sick time and reduces the demand for (time inputs into) health investment (proposition 5 and 7). This encourages healthier individuals to work more and retire later (see 6). However, health is also associated with a wealth effect, reducing the marginal value of wealth qA(t) (see Table 2 in Appendix C), which increases the demand for leisure, and for (time inputs into) healthy and unhealthy consumption, and thereby encourages early retirement.32 While the net effect is therefore ambiguous, it seems plausible that the direct effect of health on reducing sick time, and reducing time inputs into health investment, outweighs the indirect effect of health on leisure by relaxing the wealth constraint. This is consistent with an extensive literature showing quantitatively large effects of health on labour force participaton, with unhealthier individuals retiring earlier (e.g., Currie and Madrian, 1999; Smith, 2007).
Prediction 4
Under plausible assumptions, healthier individuals retire later. This, combined with an effect of health on earnings, leads to reverse causality as healthier individuals accumulate more wealth by earning more and retiring later.
5 Discussion and Conclusions
We have developed a theory of the relation between health and SES over the life-cycle. Our life-cycle model incorporates health, longevity, wealth, earnings, education, work, job-related physical and psychosocial health stressors, leisure, health investment (e.g., exercise, medical care), and healthy and unhealthy consumption (including housing, neighborhood social environment). Our review of the literature identifies these as essential mechanisms in the formation and evolution of disparities in health.
The theory is capable of reproducing stylised facts regarding the life-cycle profiles of health and health investment, as illustrated by calibrated simulations of the model. The theory is further able to reproduce stylised facts characteristic of the SES-health gradient. We find that greater SES, as measured by wealth, earnings, and education, induces a healthy lifestyle: it encourages investment in health, encourages healthy consumption, discourages unhealthy consumption, and protects individuals from the health risks of physically and psychosocially demanding working conditions. The healthier lifestyle of high SES individuals causes the health trajectories of high and low SES individuals to diverge. As a result they are healthier and live longer (propositions 2 to 4). In addition, health generates earnings and the worsening health of low SES individuals potentially leads to early withdrawal from the labour force (prediction 4). This reverse causality from health to financial measures of SES potentially reinforces the widening of the SES-health gradient, as documented in empirical studies (e.g., Smith, 2007).
In middle to late life the divergence of health trajectories potentially slows as lower levels of health encourages low SES individuals to invest more in health and engage in healthier behaviour in order to slow down their health deterioration (propositions 3 and 4). Also, mortality selection, i.e. the least healthy among lower SES individuals die sooner, results in an apparently healthier surviving disadvantaged population, potentially narrowing the gradient in late age.33 Thus, the theory is capable of reproducing the characteristic life cycle patterns of the SES-health gradient.
Apart from providing a framework to interpret stylised facts, the theory also makes novel testable predictions and provides new intuition. In particular, we emphasise the importance of our concept of a health cost (benefit) of unhealthy (healthy) behaviours, in explaining health behaviour. Individuals make decisions regarding health by taking into account not just monetary prices and preferences, but additionally the life-time health consequences of their choices, as embodied by the health cost (benefit). Variation in the health cost over the life cycle and across SES potentially explains several empirical phenomena.
For example, we predict that individuals in mid life, particularly the healthy and poor, engage in work associated with unhealthy working conditions as they value the associated wage premium. However, as individuals age they engage in healthier work, as the health cost of unhealthy working conditions increase with declining health (prediction 1). Another implication of our concept of a health cost is a pattern in which high SES individuals consume more of moderately unhealthy consumption goods (e.g., moderate alcohol consumption) and less of severely unhealthy consumption goods (e.g., cigarettes, high alcohol consumption, illicit drugs) than do lower SES individuals (prediction 3). Greater wealth permits more consumption but also increases the health cost. This could provide an explanation for the observation that high SES individuals are less likely to smoke cigarettes (bad for health) but are more likely to be moderate drinkers (moderately bad) than low SES individuals (e.g., Cutler and Lleras-Muney, 2008).
Another insight is that (endogenous) longevity is crucial in explaining observed associations between SES and health (cf. propositions 1, 3, and 4, and prediction 2). Absent ability to extend life (fixed horizon), the association between SES and health is small (proposition 1). If, however, life can be extended, SES and health are positively associated and the greater the degree of life extension afforded by SES, the greater is their association (propositions 3 and 4). Thus, health disparities are larger in environments where higher SES individuals can effectively use their resources to extend life (prediction 2). For example, if the latest medical technology is more easily accessible to higher SES individuals, health disparities across SES groups may be larger.
In deriving predictions from the comparative dynamic analyses we have made a number of assumptions, most of which are conventional, such as diminishing marginal utility and Cobb-Douglas production functions. Our calibrated model corroborated other necessary relations. However, one assumption we had to make is that first-order effects dominate second-order effects (assumption 4 in section 2.4). Future work could investigate the sensitivity of results to this assumption, although it is less restrictive than the fairly conventional assumption of functions being additively separable in their arguments, and other (potentially stronger) assumptions are likely needed to derive unambiguous predictions from the comparative dynamic analyses.
Future work may also extend the model to incorporate the joint determination of SES and health (e.g., Chiteji, 2010; Conti et al., 2010), the evolution of child health (e.g., Case, Lubotsky and Paxson, 2002; Currie and Stabile, 2003; Heckman, 2007), and the impact of fetal and early-childhood conditions on health in adulthood (e.g., Barker et al., 1993; Case, Fertig and Paxson, 2005).34 Early childhood could be included modelling the production of health by the family, similar to, e.g., Jacobson (2000) and Bolin, Jacobson and Lindgren (2001). We do not explicitly take into account the influence of the wider social context and social relationships of the family or neighborhood on health (e.g., Kawachi and Berkman, 2003), or of social capital on health (e.g., Bolin et al., 2003). Insights from the behavioural-economic and psychological literature regarding myopia and lack of self-control (e.g., Blanchflower, Oswald, and van Landeghem, 2009) might be incorporated following Laibson (1998). Uncertainty (e.g., health shocks) could be included similar to, e.g., Cropper (1977), Dardanoni and Wagstaff (1990), Liljas (1998), and Ehrlich (2000).
Acknowledgments
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Numbers K02AG042452, R01AG037398, R01AG030824, R01AG055654, P30AG012815 and P01AG022481. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Van Kippersluis thanks Netspar (Health and Income, Work and Care across the Life cycle II), and the Netherlands Organization of Scientific Research (NWO Veni grant 016.145.082) for support. Galama is grateful to the School of Economics of Erasmus University Rotterdam for a Visiting Professorship in the Economics of Human Capital. We thank the Editor, two anonymous reviewers, Mauricio Avendano, Megan Beckett, Dan Belsky, Jan Brinkhuis, Eileen Crimmins, Michael Grossman, Bas Jacobs, Arie Kapteyn, Valter Longo, Joao Pedro Magalhaes, Erik Meijer, Owen O’Donnell, Rosalie Pacula, Bastian Ravesteijn, Peter Savelyev, Eddy van Doorslaer, Tom Van Ourti, Arthur van Soest, and participants in the Health Inequality Network (HINet) meeting at the University of Chicago, the 8th iHEA World Congress on Health Economics in Toronto, the 12th Viennese Workshop on Optimal Control, Dynamic Games and Nonlinear Dynamics, the 9th Annual SHESG Conference at the University of Memphis and the 2011 RAND Conference on Health, Aging and Human Capital, as well as seminar participants at Erasmus University, the Harvard Center for Population and Development Studies, the London School of Economics, the RAND Corporation, the University of Chicago, the University of Lausanne, the University of Southern California and the University of Tilburg, for useful discussions and comments. We thank Timothy Halliday and Hui He for generously sharing their health investment estimates from the Medical Expenditure Panel Survey.
A First-Order Conditions
Associated with the Hamiltonian (equation 11) we have the following conditions:
| (43) |
| (44) |
| (45) |
| (46) |
| (47) |
| (48) |
| (49) |
| (50) |
| (51) |
| (52) |
Equation (50) and (51) provide the first-order condition for health investment (15). Equation (45) provides the first-order condition for leisure (20). Equations (46) and (47) provide the first-order condition for healthy consumption (21). Equations (48) and (49) provide the first-order condition for unhealthy consumption (24). Last, equation (52) provides the first-order condition for job-related health stress (equation 27).
B Functional Relations
| (53) |
and hence
| (54) |
Use (54) to substitute τm(t) into (5) to obtain
| (55) |
and, likewise, use (54) to substitute m(t) into (5) to obtain
| (56) |
Use (55) to substitute I[m(t), τm(t); E] into (53) to obtain (18). Likewise, use (56) to substitute I[m(t), τm(t); E] into (53) to obtain (19). Use (55) to substitute m(t) into (53), or alternatively, use (56) to substitute τm(t) into (53), to obtain
| (57) |
where we have used (15), and where
| (58) |
C Calibrated Simulations
For the calibrated simulations, we resort to discrete time. In the simplified version of our model discussed in section 3.2, individuals maximise the life-time utility function
| (59) |
where individuals live for T (endogenous) periods, β is a subjective discount factor and individuals derive utility U(Ct, Ht) from consumption Ct and from health Ht.
The objective function (59) is maximised subject to the dynamic constraints:
| (60) |
| (61) |
with , wages wt are given by (38), , and initial and end conditions: H0, HT, A0 and AT are given. Individuals live for T periods and die at the end of period T − 1. Life cannot be sustained below a minimum health level Hmin, and the individual dies when HT = Hmin.
The Lagrangian of this problem is:
| (62) |
where is the adjoint variable associated with the dynamic equation (60) for the state variable health Ht, and is the adjoint variable associated with the dynamic equation (61) for the state variable assets At.
Associated with the Lagrangian we have the following conditions:
| (63) |
| (64) |
| (65) |
| (66) |
We start with the initial condition for health, H0. Initial consumption C0 then follows from the first-order condition for consumption (65), which, for the assumed utility function (39) in section 3.2, can be written as
| (67) |
where χ ≡ (1 + ρζ − ζ)/ρ. Initial consumption C0 is a function of initial health H0, the utility share of consumption ζ, the price of goods and services pC, the efficiency of the consumption production process μC, and the marginal value of initial wealth .
Next, the initial level of health investment m0 follows from the initial relative marginal value of health (see 66). In particular,
| (68) |
The initial level of health investment m0 is a function of the price of goods and services pm, the effectiveness and efficiency of health investment, α and μI, and the initial marginal value of wealth and of health .
Health in the next period H1 is determined by the dynamic equation (60). Assets in the next period A1 follow from the initial condition for assets A0 and the dynamic equation for assets (61).
Using the functional form for the utility function, sick time, and the deterioration rate in section 3.2, the relative marginal value of health is updated according to
| (69) |
The solutions for consumption Ct, health investment mt, health Ht, and wealth At, for every period t are functions of the initial marginal values of wealth and health . In the final period, the end conditions for health HT = Hmin and for assets AT determine and
We employ the downhill simplex method (Nelder and Mead, 1965) to iteratively determine the initial marginal value of wealth and of health that satisfy the end conditions AT and HT. We use the usual values αNM = 1, γNM = 2, ρNM = 0.5 and σNM = 0.5 for the reflection, expansion, contraction and shrink coefficients, respectively. We use a period step size of one fifth of a year.
The optimal control problem presented so far is formulated for a fixed length of life T. To allow for differential longevity one needs to optimise over all possible lengths of life T. We achieve this by first solving the problem conditional on length of life T, inserting the optimal solutions , into the “indirect utility function”
| (70) |
and maximizing VT with respect to T by evaluating VT for different values of T.35
The parameters used in the calibration are presented in Table 1, and are motivated in section 3.2. The parameters to be calibrated are μI, μU, ν, the health deterioration parameters a and b, and optimal length of life T. In the calibration, to minimise the curse of dimensionality in calibrating six parameters, we first choose six values that produce a reasonable fit. We then define a six-dimensional discrete grid between 0.75 and 1.25 of the initial parameter values (i.e. 3 to 5 parameter values between 25% smaller and 25% larger than the original value).36 For each value in this six-dimensional grid, we compute the sum of the absolute deviation between the simulated moments and the data moments consisting of the 5-year averages of health and health investment shown in Figure 1, where the deviations are scaled by the value of each observed moment so that the deviations from health and health investment receive equal weight. The parameter values that jointly produce the lowest deviation are presented in Table 1, and the corresponding life-cycle profiles for health and health investment are shown in Figure 1.
Next we use our calibrated simulations to perform several counterfactual experiments regarding the signs of ∂qA(0)/∂x, and ∂qh/a(0)/∂x for x = A0, w, E, H0, where we increase x by a small amount and observe the change in the optimal co-state variable. The resulting signs are presented in Table 2. All relations are valid for fixed T and free T. To get a feel for the magnitude of these effects in the calibrated model, we also compute elasticities. However, since A0 is zero at baseline, it is not possible to compute an elasticity for A0. For the remaining initial conditions, we compute elasticities by increasing the value of the relevant initial condition by 1%. Increasing wages by 1%, the observed elasticity for qA(0) is −1.82, and the elasticity for qh/a(0) is 0.45. For education, it is not straightforward to compute elasticities, since education influences both wages and the efficiency of health investment. First, we solely increase the efficiency of health investment μI by 1%, and obtain very small elasticities of 0.005 and −0.005 for qA(0) and qh/a(0), respectively. When we make the restrictive assumption that a 1% increase in education increases both wages as well as the efficiency of health investment by 1%, the resulting elasticities are −2.18 and 0.13 for qA(0) and qh/a(0) respectively. Finally, the elasticity with respect to initial health H0 of qA(0) is −0.91 and of qh/a(0) is −0.44. Reassuringly (not shown in the Table), we also find ∂H(t)/∂x > 0, and ∂T/∂x > 0 for all parameters x = A0, wE, E, and H0.
Table 1.
Parameter Values for the Calibrated Simulations
| Parameter | Description | Value |
|---|---|---|
| Parameters taken from the literature | ||
| α | Effectiveness of health investment | 0.75 |
| r | Interest rate | 0.03 |
| β | Time preference rate | 0.03 |
| γ | Power law relation sick time and health | 1.7 |
| ρ | Coefficient of relative risk aversion | 3 |
| ζ | Utility share of consumption vs health | 0.7 |
| μC | Efficiency of consumption | 1 |
| pm | Price of medical care | 1 |
| pc | Price of consumption | 1 |
| A0, AT | Assets | 0 |
| Calibrated parameters | ||
| μI | Efficiency of health investment | 0.25 |
| μU | Scale parameter utility | 0.00001 |
| ν | Dependency of depreciation on health | 0.3 |
| a | Deterioration rate intercept | −3.6 |
| b | Deterioration rate slope | 1/17 ≈ 0.059 |
| T | Length of life | 76.8 |
Table 2.
Sign of the Effect on Co-states qA(0) and qh/a(0) of Perturbations in Initial Conditions
| Initial condition x | ∂qA(0)/∂x | ∂qh/a(0)/∂x |
|---|---|---|
| A0 | − | + |
| wE | − | + |
| E | − | + |
| H0 | − | − |
Note: All signs are valid for both fixed T and free T.
D Proofs of Propositions
D.1 Proof of Proposition 1
Absent ability to extend life, wealthy individuals, ceteris paribus, value health only marginally more than less wealthy individuals.
The dynamic equation for the relative marginal value of health is given by (37). The dynamic equation for health can be rewritten (see 57) as
| (71) |
The comparative dynamic effect of initial wealth on the relative marginal value of health, keeping length of life T fixed, is obtained by taking the derivate of (37) with respect to intial wealth A0
| (72) |
Likewise, for the health stock, the comparative dynamic effect of A0, keeping length of life T fixed, is obtained by taking the derivative of equation (71) with respect to A0
| (73) |
One can develop similar relations for the comparative dynamic effect of initial wealth on the controls: L(t), Ch(t), Cu(t), and z(t) (see section D.8). These too are expressed in terms of variation in controls, in health, in the marginal value of initial wealth and in the relative marginal value of health.
Pontryagin’s maximum principle (e.g., Caputo 2005) informs us that the solution of the optimal control problem is no longer a function of the controls and can be fully expressed in the state and co-state functions. Indeed, one can substitute the expressions for variation in the control variables, , , , and , into one another such that the final result (not shown) are comparative dynamic expressions in terms of the variation in state and co-state functions but no longer contain variation in control functions. These expressions however are unwieldy with a cumbersome mix of opposite-sign coefficients from which it is hard to draw firm conclusions. Therefore, we assume that first-order (direct) effects dominate higher-order (indirect) effects (assumption 4 in section 2.4).
As an example, wealth affects the rate of change of variation in the relative marginal value of health directly (first term on the right-hand side [RHS] of 72), but also indirectly through, for example, the effect that wealth has on healthy consumption, and healthy consumption in turn has on (third term on the RHS of 72). The comparative dynamic effect of wealth on healthy consumption is given by (94). Combining (94) with (72), we obtain the combined wealth effect
where the first term, 1, in the large term in brackets represents the first-order (direct) effect of wealth, and the second term represents the second-order (indirect) effect operating through healthy consumption. The assumption is that the direct effect of wealth dominates any indirect wealth effect that operates through healthy consumption or through any other control variable. This simplifies the expressions considerably. We have:
| (74) |
and
| (75) |
Figure 4 shows the phase diagram for the motion paths of the variation of the relative marginal value of health with respect to initial wealth (y-axis) versus the variation of health with respect to initial wealth (x-axis). Conditional on our assumptions in section 3.4 and the signs for relations (a), (b), and (c) obtained from the calibrated model, we obtain a two-dimensional phase diagram. The boundaries between regimes, the so-called null-clines, are shown by the thick lines in the figure and are obtained by setting the derivatives and to zero. While the null-clines may vary over time, the properties of the comparative dynamic phase diagrams do not change: the null-cline (∂/∂t)(∂H/∂A0) will always slope upward and cross the origin, and the null-cline (∂/∂t)(∂qh/a/∂A0) will always slope downward and cross the y-axis above the origin. Hence, the “steady state” is always above and to the right of the origin. Note that the unperturbed path corresponds with the origin (where variations are equal to zero at all ages). The phase diagram allows us to explore how changes in model parameters dynamically shift the optimal path with respect to the unperturbed life-cycle trajectory (represented by the origin).
We know the signs of most of the coefficients in (74) and (75), for example ∂2U/∂H2 < 0, ∂2Y/∂H2 < 0 (assumption 1). However, two relationships are a priori unknown: and ∂d/∂H. We proceed as follows. We obtain our preferred sign for these relationships from the calibrated simulations in section 3.2. We estimated the parameter ν in equation (40) at 0.3, which implies ∂d/∂H > 0. Further, we varied initial wealth by a small amount δA0 to obtain the sign of the change in the marginal value of initial wealth in response to variation in initial wealth for fixed T and find that (see Table 2 in Appendix C). These coefficients, based on the calibrated model, represent our benchmark case in the comparative dynamics below. Next, we investigate the robustness of these results to the opposite sign of these two relationships. We find the results to be robust.
Benchmark case
With all coefficients known, we can predict the sign of and in the four dynamic regions of the phase diagram, defined by the null-clines. The block arrows indicate the direction of motion in each of the four dynamic regions and the dotted lines provide example trajectories.37
Since both initial health H(0) = H0 and end-of-life health H(T) = Hmin are fixed, it follows that . Thus, in the phase diagram all admissible paths start and end at the vertical axis.
Consider a path that starts at the vertical axis, but below the horizontal axis . Such a path will move toward the South-West, and stay there indefinitely, as illustrated by the dotted line (c). Similarly, a path starting at the vertical axis, but above the null-cline, will move toward the North-East and stay there indefinitely, never returning to the vertical axis in finite time, as illustrated by trajectory (a).
Now consider a path starting at the vertical axis, between the null-cline and the origin. This path is associated with , and returns to the vertical axis in finite time if it crosses the horizontal axis and enters dynamic region IV at some point over the life cycle. This path satisfies all conditions, and an example trajectory (b) is shown for illustrative purposes.38
We conclude from this (see trajectory b) that wealth increases the relative marginal value of health initially, but decreases it eventually. In a model with a fixed life span T, health is higher at all ages, ∀t (trajectory a lies to the right of the vertical axis), except for t = 0 and t = T. Q.E.D.
Figure 4.
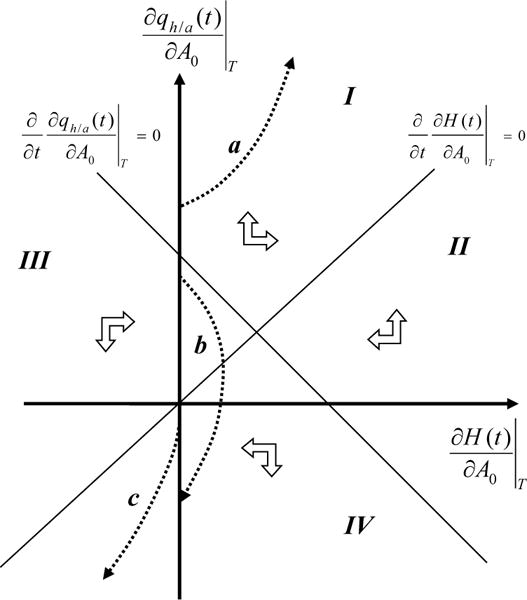
Phase diagram of the deviation from the unperturbed path, resulting from variation in initial wealth δA0, of the relative marginal value of health and of the health stock , for fixed T.
Sensitivity to the sign of ∂d/∂H
Consider the case where ∂d/∂H < 0, consistent with the health-deficit approach of Dalgaard and Strulik (2014). Further, r + ∂d/∂H > 0, since a negative sign would necessarily imply an ever decreasing relative marginal value of health and therefore ever decreasing health investment over the life cycle (see equation 37). This is inconsistent with empirical evidence and with our calibrated simulations. The null-cline for (∂/∂t)(∂qh/a/∂A0) still slopes downward, but the null-cline for (∂/∂t)(∂H/∂A0) now also slopes downward. Depending on which slope is steeper we have two scenarios, as shown in Figure 5. Recall that for fixed T all trajectories start and end at the vertical axis, since initial and terminal health are fixed, and so . In both figures the only feasible trajectory b is identical to the case where ∂d/∂H > 0. That is, ∂qh/a(0)/∂A0 > 0 and ∂qh/a(T)/∂A0 < 0, and ∂H(t)/∂A0 ≥ 0 for 0 < t < T. Therefore, reassuringly, our main predictions regarding the effect of wealth on health investment and health are insensitive to the sign of ∂d/∂H.
Sensitivity to the sign of
Figure 6 shows the phase diagram for the case where .
Here, once more trajectory b is the only path that satisfies all conditions. However, in this case, health is lower at all ages ∀t, except for t = 0 and t = T. Moreover, the path is associated with , which implies that length of life is reduced (as we explore in the next section D.2). Finally, (healthy) consumption is reduced (see equation 94). Hence, for the model predicts that increases in wealth lead to worse health, less consumption, and a shorter life, which is inconsistent with optimizing behaviour (see Ehrlich and Chuma, 1990, for a similar argument), with our calibrated model and with empirical stylised facts. Therefore, we dismiss the case where .
Figure 5.
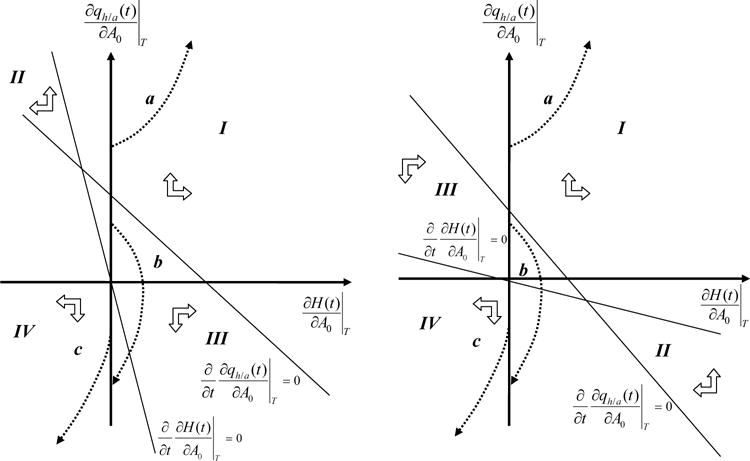
Phase diagram of the deviation from the unperturbed path, resulting from variation in initial wealth δA0, of the relative marginal value of health and of the health stock , for fixed T. The left panel represents the situation where the nullcline is steeper than the nullcline and the right panel represents the opposite case.
D.2 Proof of Proposition 2: Wealthy individuals live longer: ∂T/∂A0 > 0
Taking into account that in the optimum the condition has to be satisfied (see 14), we have
| (76) |
where denotes variation in an endogenous function g(t) with respect to initial wealth A0, keeping length of life T fixed, and denotes variation in an endogenous function g(t) with respect to T, keeping A0 fixed
The change in life expectancy due to an increase in initial wealth ∂T/∂A0 can then be identified from the identity
| (77) |
Using the expression for the Hamiltonian (11) we obtain
| (78) |
where ℂ(t) denotes the vector of control variables, ℂ(t) = [Ch(t), Cu(t), L(t), m(t), τm(t), z(t)]. In the derivations we have used , which follows from the first-order conditions, and , since A(T) and H(T) are fixed.
Note that we distinguish in notation between , which represents the derivative with respect to time t at time t = T, and , which represents variation with respect to the parameter T at time t = T.
Using (77) and (78), and assuming diminishing returns to life extension (cf. assumption 1 in section 2.4), wealth increases longevity ∂T/∂A0 > 0 if . In (78), both and are negative since health declines near the end of life as it approaches Hmin from above, and assets decline near the end of life in absence of a strong bequest motive. For diminishing returns to wealth (see the proof of proposition 1 in section D.1), a sufficient requirement for length of life to increase in response to positive variation in wealth is . As one can see from Figure 4, indeed , and thus ∂T/∂A0 > 0. Q.E.D.
Figure 6.
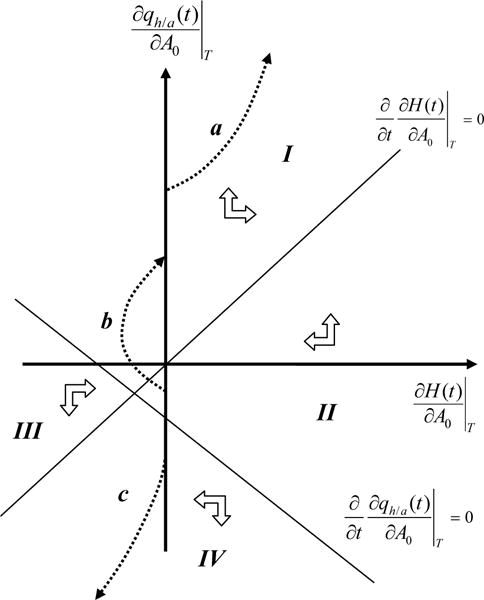
Phase diagram of the deviation from the unperturbed path, resulting from variation in initial wealth δA0, of the relative marginal value of health and of the health stock , for fixed T with .
D.3 Proof of Proposition 3
Wealthy individuals value health more and are healthier at all ages. The more life can be extended, the stronger is the increase in the value of health in response to additional wealth.
In the previous section D.2, we showed that wealthy individuals live longer. We are now interested in understanding the full comparative dynamic response of the relative marginal value of health qh/a(t) and the health stock H(t) to an increase in initial wealth, employing the full model with optimally chosen T. The total differentials
| (79) |
| (80) |
consist of the effect of variation in wealth keeping T fixed (first term on the RHS in 79 and in 80), which we explored in section D.1, and the effect that operates through responses in the optimal length of life T, keeping initial wealth A0 fixed (second term on the RHS in 79 and in 80).
The coefficients in the comparative dynamic expressions for the response in the relative marginal value of health and the health stock to variation in length of life T, holding initial wealth A0 constant, are identical to the coefficients derived for the response to variation in initial wealth A0, holding length of life T fixed, shown in (74) and (75). That is, we simply have to replace the partial differentials with their total differentials, i.e. with ∂qA(0)/∂T, with ∂qh/a(t)/∂T, and with ∂H(t)/∂T, in (74) and (75) to obtain the total comparative dynamic effect.
There is, however, one important difference compared to the previous case in which we explored variation with respect to A0 for fixed T: the terminal value of the variation in health with respect to T, for fixed A0, is positive, . Thus the total differential with respect to wealth A0 is too, ∂H(T)/∂A0 > 0, implying that all admissible paths end to the right of the vertical axis in the phase diagram (and not on the vertical axis as is the case for fixed T in section D.1). This can be seen as follows. First, solve the state equation for health (4):
| (81) |
Then take the derivative of (81) with respect to T to obtain
| (82) |
Now take the derivative of (81) with respect to T for t = T
| (83) |
The derivative of health with respect to time at t = T is negative since we approach Hmin from above. Thus we have
Intuitively, if length of life is extended to T + δT the health stock has to be higher at the previous point of death T, and it is higher by exactly the change in health over a small period of time. Thus, .
Figure 7 presents the comparative dynamic results. The initial condition ∂H(0)/∂A0 = 0, implies that all admissible paths start on the vertical axis, and the end-condition ∂H(T)/∂A0 > 0, implies that all admissible paths end to the right of the vertical axis, at ∂H(T)/∂A0 (indicated by the four dotted vertical lines in the figure). As the phase diagram shows, trajectories a, b, c and d, corresponding to four different levels of ∂H(T)/∂A0, are feasible. This implies that ∂H(t)/∂A0 > 0 ∀t (except for t = 0), ∂qh/a(t)/∂A0 > 0 initially, and while potentially the relative marginal value is lower ∂qh/a(t)/∂A0 < 0 after some t = t† (as for trajectory d, but not for a, b or c), cumulatively it is higher , which proves the first part op proposition 3.
Consider equation (80) for t = T. In proposition 1, section D.1, we established that for fixed T, . Thus the value of the total differential ∂H(T)/∂A0 is determined by the second term on the RHS of (80). Since (compare with 83), it is the same for all four scenarios as it re presents the negative of the derivate with respect to time t at t = T of the unperturbed (unchanged) path. Thus the end point ∂H(T)/∂A0 is proportional to the degree of life extension afforded by additional wealth ∂T/∂A0: it thus lies further to the right in the phase diagram (vertical dotted lines) for greater ∂T/∂A0.
In scenario d (see Figure 7), if life extension due to additional wealth is small, wealthier individuals will value health more cumulatively, but not necessarily at all times, the relative marginal value of health increases less rapidly over the life cycle, compared to the unperturbed path (less steep increase), and the trajectory eventually crosses the unperturbed path. Moving from scenario d to c to b and finally to a, the marginal value of health increases progressively and so does life extension. This proves the second part of proposition 3. In all four scenarios individuals value health more cumulatively but they may value health less at certain ages (for example in scenario d individuals value health less late in life, compared to the unperturbed path). Q.E.D.
Figure 7.
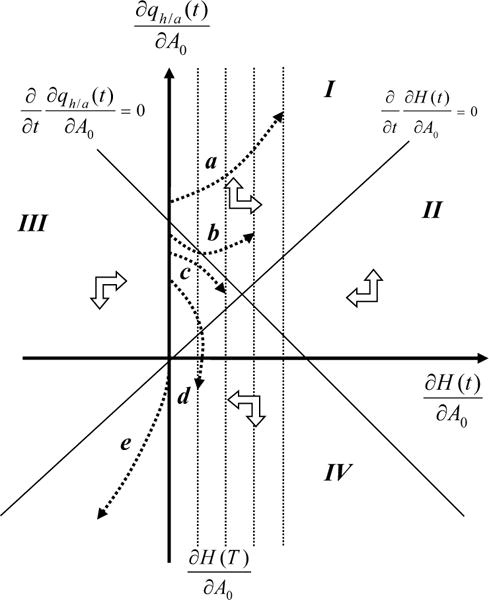
Phase diagram of the deviation from the unperturbed path, resulting from variation in initial wealth δA0, of the relative marginal value of health ∂qh/a(t)/∂A0 and of the health stock ∂H(t)/∂A0, allowing length of life T to be optimally chosen. The four vertical dotted lines represent different potential values for the end point ∂H(T)/∂A0.
D.4 Proof of Proposition 4
Permanently higher wages and education operate in a similar manner to an increase in wealth δA0 (propositions 1 through 3), with some differences: (i) the wealth effect is muted by the increased opportunity cost of time, (ii) permanent wages wE and education E also raise the production benefit of health, and (iii) education raises the efficiency of health investment.
Permanent wages wE
The comparative dynamic effect of a permanent increase in the wage rate w(t), through, e.g., an increase in the parameter wE in (10), on the relative marginal value of health qh/a(t) can be obtained by taking the derivate of (37) with respect to wE and keeping first-order terms (total differentials, free T):
| (84) |
The first term on the RHS of (84) represents a wealth effect. Permanently higher wages raise the production benefit of health, as health is more valuable in reducing sick time (freeing time for work) when wages are higher. In addition there is the usual wealth effect (second term on the RHS). Both wealth terms are negative since sick time decreases with health ∂s/∂H < 0, and because wE raises lifetime earnings (permanent income) and relaxes the budget constraint (7), see also Table 2 in section C. Variation in permanent wages δwE is thus distinct from variation in wealth δA0 in that it not only raises the consumption benefit of health (as is the case for variation in δA0) but also the production benefit of health (which is not the case for variation in δA0).
Likewise, the comparative dynamic effect of a permanent increase in the wage rate on health H(t) is obtained by taking the derivative of (71) with respect to wE and keeping first-order terms:
| (85) |
where the first term on the RHS of equation (85) represents the negative effect of the opportunity cost of time on health investment, and in turn on health.
The corresponding phase diagram is shown in Figure 8. It is nearly identical to the phase diagram for variation in initial wealth δA0 (Figure 7), except that the (∂/∂t)(∂H(t)/∂wE) null cline crosses the vertical ∂qh/a(t)/∂wE axis at qh/a(t)(1 −κI)/wE and not at the origin. This term represents the effect of a permanent increase in wages wE on the opportunity cost of investing time in health. The (∂/∂t)(∂qh/a(t)/∂wE) null cline crosses the vertical ∂qh/a(t)/∂wE axis at . This expression represents a wealth, or permanent income, effect: permanently higher wages increase the production benefit of health (first term) and increases wealth, thereby raising the consumption benefit of health (second term; operating through ∂qA(0)/∂wE < 0). In the scenario depicted in Figure 8, it is assumed that the opportunity cost of time effect is small compared to the wealth / permanent income effect.
Following similar steps as in sections D.1 and D.3 for variation in wealth, we first need to establish whether length of life is extended as a result of a permanent increase in income. This can be accomplished by considering the fixed T case. The comparative dynamic effect of a permanent increase in the wage rate wE on longevity can be obtained by replacing A0 with wE in (76), (77), and (78). Since (see Table 2 in section C), it follows that, similar to the case for variation in initial wealth δA0 (see section D.2), a sufficient condition for life extension in response to positive variation in permanent wages is .
For fixed T all admissible paths in the phase diagram have to start and end at the vertical axis, since H(0) and H(T) are fixed. Trajectory e in the phase diagram of Figure 8 is consistent with these conditions and the trajectory is characterised by . Thus length of life is extended ∂T/∂wE > 0.
Considering the T free case, the reasoning is identical to the discussions for propositions 3 and 4 in sections D.2 and D.3. Following the logic outlined there, we find that trajectories a, b, c, and d are consistent with life extension. The greater life is extended as a result of greater permanent income, the further to the right is the trajectory’s end point ∂H(T)/∂wE. Example trajectory a is associated with a large increase in the marginal value of health ∂qh/a(t)/∂wE and in health ∂H(t)/∂wE, compared to the unperturbed trajectory, and this trajectory is associated with the greatest gain in longevity ∂T/∂wE. Trajectory b and c represent an intermediary case and trajectory d a case of limited response, the latter most closely resembles the fixed T case, represented by trajectory e. Trajectory f is incompatible with live extension and ruled out. Q.E.D.
These results rely on our assumption that the opportunity cost effect is smaller than the wealth / permanent income effect. If, however, the opportunity cost effect is substantial, the ∂H(t)/∂wE null cline is shifted further upward in the phase diagram of Figure 8 than shown. A trajectory similar to e might then end up above the ∂H(t)/∂wE axis with a positive end value of , in which case we cannot unambiguously establish that length of life increases.39
If the opportunity cost is very high, outweighing the wealth / permanent income effect, the ∂H(t)/∂wE null cline could even cross the vertical ∂qh/a(t)/∂wE axis above the location where the ∂qh/a(t)/∂wE null cline crosses the vertical ∂qh/a(t)/∂wE axis. In such a scenario (not shown), for fixed T, any admissible trajectory is characterised by , and we cannot unambiguously establish that length of life increases. While theoretically we cannot rule out the scenario where the opportunity cost effect outweighs the wealth effect, empirical evidence suggests that a permanent wage change affects health positively, while a transitory wage increase affects health negatively (e.g., Contoyannis, Jones and Rice 2004), and that high-income individuals are generally in better health than low-income individuals. Thus, in practice it appears the opportunity cost effect is not large.
Education E
The comparative dynamic effect of an increase in education E (see 9 and 10), on the relative marginal value of health qh/a(t) is obtained by taking the derivate of (37) with respect to E and keeping first-order terms (total differentials, free T):
| (87) |
Likewise, the comparative dynamic effect of an increase in education on health H(t) is obtained by taking the derivative of (71) with respect to E and keeping first-order terms:
| (88) |
where we have used (58). Contrasting the results of the comparative dynamics for education E (equations 87 and 88) with those obtained for permanent income wE (equations 84 and 85) we observe that permanent wages wE and education E operate in the same way. This should come as no surprise, as they both operate by increasing permanent wages. There is however one important difference: the first term on the RHS of (88) represents both the effect of education on the efficiency of health investment ∂μI/∂E (the educated are assumed to be more efficient producers and consumers of health) and the effect of education on the opportunity cost of time ρE(1 − κI). The efficiency effect of education reduces the opportunity cost of time effect. The phase diagram for the effect of variation in education δE is essentially the same as for variation in permanent income wE, shown in Figure 8, and replacing wE by E (for this reason we do not provide a separate phase diagram). Given strong empirical support for a positive association between education and health, it could be that the efficiency effect dominates, in which case the (∂/∂t)(∂H(t)/∂E) null cline would cross the vertical ∂qh/a(t)/∂E axis below instead of above the origin. This would make the case for variation in education δE stronger (compared to the case for variation in permanent wages wE) in ensuring that the condition is obtained and hence length of life is extended.
Figure 8.
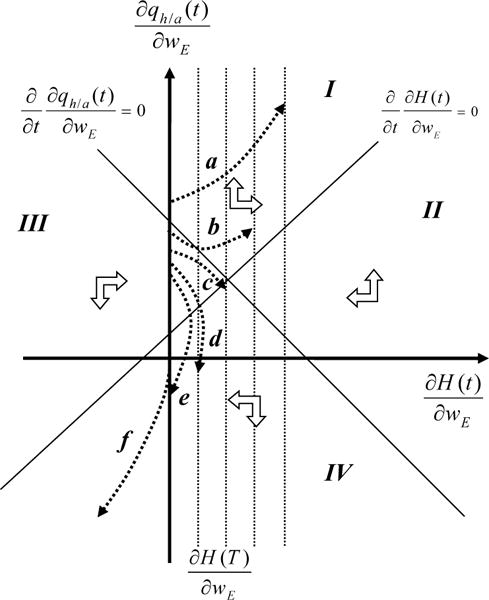
Phase diagram of the deviation from the unperturbed path, resulting from variation in permanent wages δwE, of the relative marginal value of health ∂qh/a(t)/∂wE and of the health stock ∂H(t)/∂wE, allowing length of life T to be optimally chosen. The four vertical dotted lines represent different potential values for the end point ∂H(T)/∂wE.
D.5 Proof of Proposition 5
Absent ability to extend life, healthy individuals, ceteris paribus, value health cumulatively less,
The comparative dynamic effect of variation in initial health δH0 on the relative marginal value of health, keeping length of life T fixed, is obtained by taking the derivative of (37) with respect to initial health H0 and keeping first-order terms. Likewise, the comparative dynamic effect of initial health on health, keeping length of life T fixed, is obtained by taking the derivate of (71) with respect to intial health H0 and keeping first-order terms:
| (89) |
and
| (90) |
Thus, the coefficients in (89) and (90) are identical to the coefficients in the comparative dynamic relations (74) and (75) for variation with respect to wealth δA0.
A-priori we don’t know the sign of . First, consider the scenario where health reduces the marginal value of wealth, , consistent with results obtained for our calibrated model (see Table 2 in section C). In this case the phase diagram for variation in initial health δH0, shown in Figure 9, is similar to the phase diagram for variation in initial wealth δA0, shown in Figure 4. Importantly, the null-cline crosses the vertical axis above the origin. While any admissible path has to end on the vertical axis, an important difference with wealth is that any admissible path has to start at , which for t = 0 is identical to 1. We don’t know a-priori where is located with respect to the steady state (where the two null-clines cross) and we show one case where the initial point lies to the left (vertical dashed line to the left) and another case where it lies to the right (vertical dashed line to the right) of the steady state (Figure 9).
In case is located to the left of the steady state, we can rule out trajectory a as it does not end on the vertical axis. For the same reason we can also eliminate trajectory e in case is located to the right of the steady state.
Trajectories b, c and f represent an initial increase, followed by a subsequent decrease, in the marginal value of health qh/a(t), with respect to the unperturbed path. Trajectories d and g represent solutions where the relative marginal value of health is lower at all times. Also for these solutions health is higher at all times (except t = T) and the individual uses the additional health δH0 to shift resources from health to other uses. For these solutions better health reduces the demand for health investment and healthy behaviour at all times.
Those trajectories that are feasible (that are consistent with the begin and end conditions), i.e. b, c, d, f and g, all involve a cumulatively lower marginal value of health as initially higher health δH0 requires lower health investment and less healthy behaviour over the life cycle in order for health to reach the minimum health level Hmin within the same length of life T.40 Q.E.D.
Figure 9.
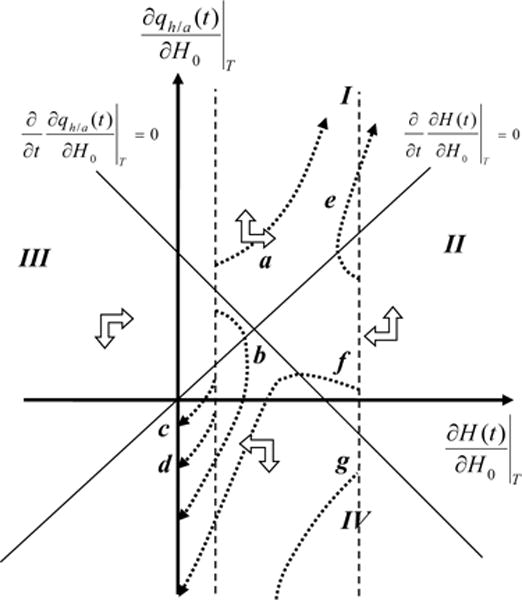
Phase diagram of the deviation from the unperturbed path, resulting from variation in initial wealth δH0, of the relative marginal value of health and of the health stock , for fixed T.
Sensitivity to the sign of ∂d/∂H
Using similar reasoning and procedures as in Appendix section D.1 we find that the results remain valid for the opposite sign of ∂d/∂H.
Sensitivity to the sign of
Now consider the scenario where health raises the marginal value of wealth, . In this scenario the null-cline shifts downward, crossing the null cline to the left of and below the origin. In this case (not shown), all admissible trajectories start with a lower relative marginal value of health and either end with a higher relative marginal value of health , in which case life is not extended but reduced ∂T/∂H0 < 0 as a result of greater health (see 91), or end with a lower relative marginal value of health , in which case we cannot unambiguously establish that life is extended. While we cannot rule out this scenario in the general case, our calibrated simulations show that a small increase in initial health δH0 leads to a reduction in the marginal value of wealth, which is consistent with ∂qA(0)/∂H0 < 0 (see Table 2 in section C). Therefore, we favor the scenario where health reduces the marginal value of wealth, which is consistent with empirical evidence that worse childhood health is associated with shorter lives (Currie, 2009), and it has a natural intuitive interpretation that health and wealth are to some extent substitutable in financing consumption (e.g., Muurinen, 1982; Case and Deaton, 2005).
D.6 Proof of Proposition 6: Healthy individuals live longer ∂T/∂H0 ≥ 0
The comparative dynamic effect of variation in initial health δH0 on length of life T can be obtained by following the same steps as in section D.2. The result is identical to replacing A0 with H0 in conditions (76), (77) and (78). Assuming diminishing returns to life extension (cf. assumption 1 in section 2.4), length of life is extended ∂T/∂H0 > 0, if:
| (91) |
As argued before in section D.2, in (91), both and are negative since health declines near the end of life as it approaches Hmin from above, and assets decline near the end of life in absence of a very strong bequest motive. Further, we have . Note that all admissible scenarios b, c, d, f and g, end with negative values for variation in the relative marginal value of health with respect to initial health . Thus, length of life is extended ∂T/∂H0 > 0. Q.E.D.
D.7 Proof of Proposition 7
Individuals with greater endowed health are healthier at all ages, ∂H(t)/∂H0 > 0, ∀t. For small life extension healthy individuals cumulatively value health less , for intermediate life extension they value health cumulatively more , and for large life extension they value health more at all ages, , ∀t.
Having established that length of life is extended, ∂T/∂H0 > 0, now consider the more interesting case where T is free. Analogous to the discussion in section D.3 we have
Thus, .
Figure 10 presents the comparative dynamic results for free T. The phase diagram on the left shows feasible trajectories a through g for the case where the starting point ∂H(t)/∂H0 = 1 is located to the left of the steady state, and the phase diagram on the right shows feasible trajectories a through f for the case where the starting point ∂H(t)/∂H0 = 1 is located to the right of the steady state (the starting values are indicated by the dashed vertical lines in both phase diagrams). The initial condition ∂H(t)/∂H0 = 1 for t = 0, and the end-condition ∂H(T)/∂H0 > 0, imply that all admissible paths start and end to the right of the vertical axis. Three example end values ∂H(T)/∂H0 are indicated by the three dotted vertical lines in both figures.
All feasible trajectories for health lie to the right of the vertical axis. Thus individuals with greater endowed health are healthier at all ages, ∂H(t)/∂H0 > 0, ∀t. Further, as the result shows, also for health the greater life is extended, the further is the end point ∂H(T)/∂H0 located to the right in the phase diagram. While both phase diagrams are quite complicated, they clearly show that for end points ∂H(T)/∂H0 (the vertical dotted lines) that lie further to the right (i.e. those associated with a greater degree of life extension), the variation in the value of health ∂qh/a(t)/∂H0 becomes more and more positive, with some scenarios even allowing for the possibility that healthy individuals value health more at every age. Whereas for end points ∂H(T)/∂H0 that lie more to the left (i.e. those associated with a smaller degree of life extension), the variation in the value of health ∂qh/a(t)/∂H0 becomes more and more negative. These latter cases more closely resemble the fixed T case (proposition 7). Q.E.D.
Figure 10.
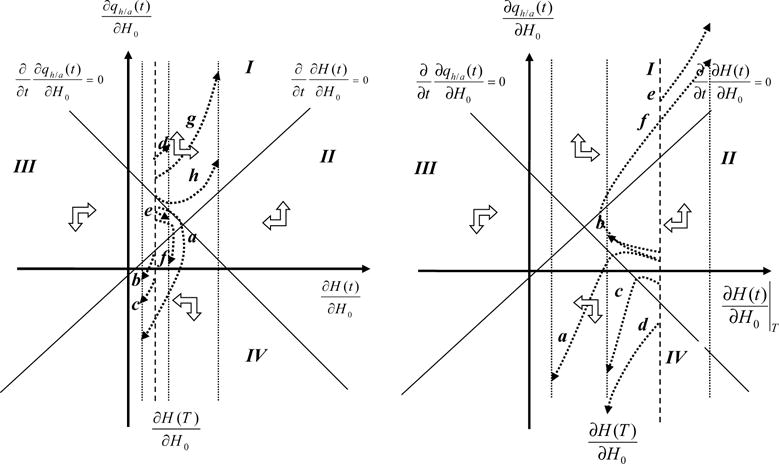
Phase diagram of the deviation from the unperturbed path, resulting from variation in initial health δH0, of the relative marginal value of health ∂qh/a(t)/∂H0 and of the health stock ∂H(t)/∂H0, for free T. The left shows feasible trajectories a through g for the case where the starting point ∂H(t)/∂H0 = 1 is located to the left of the steady state, and the phase diagram on the right shows feasible trajectories a through f for the case where the starting point ∂H(t)/∂H0 = 1 is located to the right of the steady state (the starting values are indicated by the dashed vertical lines in both phase diagrams).
D.8 Comparative Dynamics of the Controls
D.8.1 Variation in initial wealth, δA0
In signing the following comparative dynamic results we rely on assumptions 1 to 4 and propositions 1 to 7.
Health investment
For the control variable health investment the comparative dynamic effect of initial wealth A0 is obtained from (15), 18 and (19)
| (92) |
| (93) |
where we assume that first-order effects dominate and we focus on the total differential (full model with free T). Since ∂m(t)/∂A0 and ∂τm(t)/∂A0 are proportional to ∂qh/a(t)/∂A0, they will mimic the pattern of the variation in the response to wealth of the relative marginal value of health (see propositions 1 and 3).
Healthy and unhealthy consumption
For the control variable healthy consumption the comparative dynamic effect of initial wealth A0 is obtained from (21):
| (94) |
The direct wealth effect (first term on the RHS of 94) as well as the effect of an increase in the relative marginal value of health (second term on the RHS) is positive.41 The sign of the third term is undetermined, since the sign of ∂2d/∂H∂Ch is not known. One could imagine that healthier individuals benefit less from healthy consumption, but one could also imagine the opposite scenario. Since the effect of wealth on health ∂H(t)/∂A0 is gradual and not immediate, the third term is initially small compared to the first two terms. As a result, an increase in endowed wealth increases the demand for healthy consumption, ∂Ch(t)/∂A0 > 0, initially.
Likewise, for unhealthy consumption the comparative dynamic effect of initial wealth is obtained from (24):
| (95) |
For unhealthy consumption, the effect is ambiguous. While the direct wealth effect is positive (first term on the RHS of 95), the effect of an increase in the marginal health cost (last two terms on the RHS) is negative.
Job-related health stress
The comparative dynamic effect of initial wealth A0 on job-related health stress is obtained from (27):
| (96) |
where the coefficient of ∂z(t)/∂A0 is positive under assumptions 1 and 2, but the coefficient of ∂H(t)/∂A0 cannot be signed. Initially, the term in ∂H(t)/∂A0 is small as the effect of wealth on health is gradual.
Leisure
The comparative dynamic effect of variation in initial wealth A0 on leisure is obtained from (20):
| (97) |
For diminishing utility of leisure ∂2U/∂L2 < 0, diminishing returns to wealth ∂qA(0)/∂A(0) < 0 (see Table 2 in section C), the demand for leisure is initially higher as a result of greater wealth. But wealth eventually leads to better health, and if leisure and health are complements in utility ∂2U/∂H∂L > 0, we have ∂L(t)/∂A0 > 0, ∀t. If, however, health and leisure are substitutes in utility, then the demand for leisure is initially higher but could be reduced eventually with improved health.
D.8.2 Variation in the permanent wage rate, δwE
Health investment
For the control variable health investment the comparative dynamic effect of the wage rate wE is obtained from (92) replacing A0 by wE, and adding the term −(1 −κI)/wE on the RHS.
Healthy and unhealthy consumption
For the control variable healthy consumption the comparative dynamic effect of the wage rate wE is obtained from (94) replacing A0 by wE and adding the term on the RHS.
Likewise, for unhealthy consumption the comparative dynamic effect of the wage rate wE is obtained from (95) replacing A0 by wE and adding the term on the RHS.
Job-related health stress
The comparative dynamic effect of wE on job-related health stress is obtained from (96) replacing A0 by wE and adding the term {(∂w/∂z)/wE}τw(t) on the RHS.
Leisure
The comparative dynamic effect of the wage rate on leisure is obtained from (97) by replacing A0 by wE and adding the term qA(0)(w(t)/wE)e(β−r)t on the RHS.
D.8.3 Variation in education, δE
Health investment
For the control variable health investment the comparative dynamic effect of education E is obtained from (92) replacing A0 by E, and adding the term {−ρE(1 −κI) + (1/μI(E)) (∂μI/∂E)} on the RHS.
Healthy and unhealthy consumption
For the control variable healthy consumption the comparative dynamic effect of education E is obtained from (94) replacing A0 by E, and adding the term
on the RHS. Likewise, for unhealthy consumption the comparative dynamic effect of education is obtained from (95) replacing A0 by E and adding the term
on the RHS.
Job-related health stress
The comparative dynamic effect of education E on job-related health stress is obtained from (96) replacing A0 by E, and adding the term ρE (∂Y/∂z) on the RHS.
Leisure
The comparative dynamic effect of education on leisure is obtained from (97) by replacing A0 by E and adding the term ρEqA(0)w(t)e(β−r)t on the RHS.
D.8.4 Variation in initial health, δH0
The comparative dynamics of the control variables with respect to H0 can be directly obtained by using the comparative dynamics for initial wealth in (92) to (97), replacing A0 by H0.
Footnotes
Several papers contain components of our generalised theory of health. The Grossman model (Grossman, 1972a;b) contains health and health investment and interactions with earnings, and wealth, but lacks other health behaviours. Ehrlich and Chuma (1990) were the first to introduce endogenous longevity, but their model does not include other decisions besides health investment. Forster (2001) models the relation between health, longevity, healthy consumption, and unhealthy consumption but does not model health investment, wealth accumulation, or job conditions. Case and Deaton (2005) include unhealthy consumption as well as physical effort on the job, but do not model longevity. In work independently developed around the same time as our theory, Dalgaard and Strulik (2014), Strulik (2015) and Dalgaard and Strulik (2017) present so-called health-deficit models that contain health and health investment and interactions with earnings, labor-force participation and wealth, but lack other health behaviours. Strulik (2016) calibrates a related theoretical model in which health behaviour and SES influence health and longevity, but he does not model job conditions.
Ehrlich and Chuma (1990) generate a set of directional predictions (their Table 3), based on a pioneering comparative dynamic analysis of the Grossman model with endogenous longevity. However, while they are able to generate the sign of the effects (broadly whether an effect is more or less likely to be positive or negative), they do not present dynamic results. Further, they do not consider other health behaviours besides health investment. Ried (1998) presents a comparative dynamic analysis of the Grossman model, but his model is limited to the linear case, which has distinct properties (e.g., Ehrlich and Chuma, 1990; Galama, 2015). Eisenring (1999) presents a comparative dynamic analysis of a simple model without consumption, wealth accumulation, or health behaviours.
While the concept of a health cost (benefit) of unhealthy (healthy) behaviour is not new, explicit theoretical modelling is, and so is our formal definition of the concept. The literature on the value of a statistical life (e.g., Viscusi and Aldy, 2003) focuses on the cost of reductions in life (mortality) rather than in health (morbidity) as in our theory. Even the seminal theory of rational addiction (Becker and Murphy, 1988), while arguing conceptually for an effect of unhealthy addictive consumption on health, does not explicitly model this effect (see Jones et al., 2014, for an exception). To the best of our knowledge, only Forster (2001), Case and Deaton (2005), Strulik (2016), and Schuenemann et al. (2017) have previously explicitly modelled behaviour as a choice variable affecting health. Case and Deaton’s (2005) model, however, focuses on the linear case, which has distinct properties (e.g., Ehrlich and Chuma 1990; Galama 2015). And while Forster (2001), Strulik (2016) and Schuenemann et al. (2017) model a health cost / health benefit by allowing consumption to affect health, our comparative dynamic analyses allow us to formally define, discuss and analyze the concept, investigate how it influences various health behaviours and the health gradient, and make predictions.
James Heckman and colleagues have emphasised the role of childhood cognitive and non-cognitive abilities in determining both education and health outcomes in later life (e.g., Heckman, 2007; Cunha and Heckman, 2007; Conti et al., 2010; Campbell et al., 2014; see also Almond and Currie, 2011), and there is strong evidence that parental, especially maternal, SES influences the evolution of child health (Currie, 2009), suggesting that part of the SES-health gradient may be determined very early in life.
Yet, see, e.g., Albouy and Lequien (2009) and Clark and Royer (2013) who could not establish a causal effect of education on mortality.
Beckett (2000) and Baeten, van Ourti and van Doorslaer (2013), however, have demonstrated that the convergence in health inequalities in later life cannot be explained entirely, or even mostly, by mortality selection.
Living in an affluent neighborhood is an expensive, yet health-promoting and utility-generating choice. It is a constrained choice: low SES individuals cannot afford to live in more affluent areas.
We follow Grossman (1972a,b) in distinguishing between the production of health I[m(t), τm(t); E] and the deterioration of health d(t) and in allowing the deterioration rate d(t) to be a function of health H(t). We follow Case and Deaton (2005) in modelling health behaviours as operating through the deterioration rate d(t). These choices are somewhat arbitrary. Mathematically, however, they are equivalent, with the exception that with our current choice, investment is not a direct function of health or health behaviour since the production process does not explicitly depend on them.
In Grossman’s original formulation (Grossman, 1972a; 1972b) length of life T is determined by a minimum health level Hmin below which life cannot be sustained. If health reaches this level H(t) = Hmin an individual dies, hence H(T) ≡ Hmin.
Imperfect capital markets itself could be a cause of socioeconomic disparities in health if low income individuals face greater borrowing constraints and therefore cannot optimally invest in health.
We associate z(t) = 0 with the least amount of job-related health stress possible in employment, and since there is no obvious scale to job stress we employ the simple relationship shown in equation (9).
Intuitively, at higher levels of investment, due to concavity of the health-production function I[m(t), τm(t); E], an additional increment of investment m(t), τm(t) produces a smaller improvement in health. Thus, the effective ‘price’ πI(t) increases with the level of investment m(t), τm(t).
While it seems plausible that the health benefits of health investment and healthy consumption exhibit diminishing returns to scale, the health costs of unhealthy consumption and job-related health stress plausibly exhibit increasing returns to scale. In simple terms: whereas after a certain point more health investment, exercise, or consumption of healthy foods, does not prevent eventual aging, escalating risky behaviour (e.g., illicit drug use) or dangerous work can lead to rapid health deterioration.
Where T* denotes optimal length of life and U(*) denotes the maximised utility function (see 13).
Intuitively, health is a resource and having more of it relaxes the dynamic constraint for wealth: being in better health reduces the need for health investment and health provides earnings. Both health and wealth are resources that enable consumption and leisure.
After solving the optimal control problem, the model’s solutions can be fully expressed in the state and co-state functions. For this reason it is useful to start with an analysis of the dynamics of the co-state function qh/a(t) and the state function H(t).
DeNardi et al., (2016) decompose medical expenditures into different components, and show that the rapidly increasing expenditures in old age can largely be attributed to long-term and nursing home care.
Scholz and Seshadri (2016) use γ = 0.17, we multiply with 10 to account for the difference in scaling between their and our health variable.
The calibration suggests that a model where health depreciation depends only implicitly on age through the health stock H(t), i.e. and ν < 0 is able to fit the health profile very accurately. However, this model cannot reproduce the quasi-exponentially increasing profile for health investment. Our understanding from the calibration exercise is that there are two different ways in which one can reproduce the empirical life-cycle profiles of health and health investment: (i) a Grossman-style health accumulation model with health depreciation that depends explicitly on age as well as implicitly on the health stock, e.g., , with 0 < ν < 1; and (ii) a health-deficit model in the style of Dalgaard and Strulik (2014).
However, it is unclear whether ∂d/∂x, for x = Ch, Cu, z increases or decreases with age. Since health decreases with age, and since ∂d/∂H > 0 (since ν > 0 in our calibrated simulations), a declining health stock decreases the aging rate d(t) with age. Depending on the sign of ∂2d/∂H∂Ch, ∂2d/∂H∂Cu, and ∂2d/∂H∂z, this effect may be either reinforced or mitigated. As outlined in assumption 4, we assume these second-order effects are quantitatively less important.
Part of the SES-health gradient may be explained by differences in individual’s preferences. A lower rate of time preference β operates in a similar manner to wealth, earnings and education. A lower rate of time preference may also lead to greater investment in education (not part of our theory) and hence lead to joint determination of health and education (e.g., Fuchs, 1986).
Note that we can restart the problem at any time t, taking A(t) and H(t) as the new initial conditions. Thus the comparative dynamic results derived for, e.g., variation in initial wealth δA0 and initial health δH0 have greater validity, applying to variation in wealth δA(t) and in health δH(t) at any time t ∈ [0, T).
Note that it can be understood that the opposite pattern, one of disinvestment early in life and increased investment later in life, is inferior as it would be associated with lower health at all ages and therefore a reduced consumption benefit.
Both and are negative since health approaches Hmin from above, and assets decline near the end of life as poor health reduces earnings.
An indirect effect operates through the effect that wealth has on health, and health in turn has on the deterioration rate. It is not clear what the signs of these effects are, since signing these terms requires assumptions on the signs of ∂d2/∂H∂Cu, ∂d2/∂H∂Ch, etc. As outlined in assumption 4, we assume these second-order effects are quantitatively less important. The effect of wealth on health is gradual and is therefore at least initially unlikely to drive the effect of wealth on health behaviours.
If wealth enables limited life extension (scenario I in proposition 3), it is possible that the health benefit decreases late in life, since wealth reduces qh/a(t) late in life compared to the unperturbed path.
Earnings Y (t) are a function of the wage rate w(t) times the amount of time spent working τw(t) (see equation 8). A higher wage rate wE implies that the individual has higher earnings Y (t) because the direct effect of higher wages is to increase earnings. There are also two secondary effects. First, individuals may work more because of the higher opportunity cost of not working (substitution effect). Second, individuals may work fewer hours to spend their increased income on leisure or consumption (income effect). Empirical studies suggest that the substitution and income effects are of the same magnitude (e.g., Blundell and MaCurdy, 1999) and hence that the direct effect of a wage increase is to increase earnings, while the secondary effect is small, consisting of two competing effects that roughly cancel out. Thus, a higher wage rate translates into higher earnings.
Cases are also possible where the relative marginal value of health is initially higher but eventually lower. See Appendix section D.5 and Figure 9 for more detail.
If, in contrast to our benchmark scenario, ∂qA(0)/∂H0 > 0, then theoretically we cannot rule out that ∂T/∂H0 < 0 and that ∂H(t)/∂H0 < 0 after some age t (see Appendix D.5). This case would represent an extreme scenario in which the complementarity between consumption and health in utility is so strong that healthier individuals choose to spend much more on consumption and much less on health investment, living shorter lives. This scenario is inconsistent with empirical stylised facts, e.g., that healthier people live longer lives, and with our calibrated simulations.
However, after accounting for the endogeneity of health, Galama et al. (2012) find that the effect of health on medical care use becomes statistically insignificant, suggesting the negative association obtained in empirical studies may not be sufficiently robust.
However, wealthy individuals are healthier (proposition 3), which reduces sick time and increases the benefit of work (earnings). The disparity in health grows over time, so that eventually the effect of better health among the wealthy may become important in the retirement decision.
The amount of time devoted to work further depends on whether leisure, consumption, and health are complements or substitutes in utility.
The narrowing of the gradient due to unhealthier individuals engaging in healthier behaviour would represent an economic variant of the age-as-leveller hypothesis, while the narrowing of the gradient due to mortality selection would be consistent with a process of cumulative advantage (House et al., 1994; Ross and Wu, 1996; Lynch, 2003).
See Galama and Van Kippersluis (2015) and Strulik (2016) for theories of endogenous education and health.
When the optimal parameter value is at a corner of the grid, we define a new grid with the previous corner solution as its middle point.
While the null clines are functions of age and shift over time the nature of the diagram is essentially unchanged, for the assumed signs of the coefficients in (74) and (75). That is, there are always four dynamic regions, the null-cline is always downward sloping and intersects the x-axis to the right of the origin, and the null cline is always upward sloping and intersects the origin.
More complicated paths are possible (given that the null clines shift with time) that may temporarily enter regions I and/or II, but only those paths that start on the vertical axis above the horizontal axis and that eventually end on the vertical axis below the horizontal axis are admissible, producing broadly similar patterns, and leading to the same conclusions.
| (86) |
Note that health is higher at all times (all trajectories stay to the right of the origin), except for t = T (in the fixed T case eventual disinvestment is required to enforce that health reaches the minimum level H(t) = Hmin at t = T).
Scenarios are possible in which the effect of wealth on the relative marginal value of health eventually becomes negative after some age. The initial response however is always positive.
Contributor Information
Titus J. Galama, University of Southern California, Dornsife Center for Economic and Social Research (CESR), USA
Hans van Kippersluis, Erasmus School of Economics, Erasmus University Rotterdam, The Netherlands; Tinbergen Institute, The Netherlands; Department of Economics, Chinese University of Hong Kong, Hong Kong SAR.
References
- Adler NE, Boyce T, Chesney M, Folkman S, Syme L. Socioeconomic inequalities in health: No easy solution. Journal of the American Medical Association. 1993;269:3140–3145. [PubMed] [Google Scholar]
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, Syme SL. Socioeconomic status and health: The challenge of the gradient. American Psychologist. 1994;49(1):15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Albouy V, Lequien L. Does compulsory education lower mortality? Journal of Health Economics. 2009;28(1):155–168. doi: 10.1016/j.jhealeco.2008.09.003. [DOI] [PubMed] [Google Scholar]
- Almond D, Currie J. Killing Me Softly: The Fetal Origins Hypothesis. Journal of Economic Perspectives. 2011;25(3):153–172. doi: 10.1257/jep.25.3.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arking R. Biology of aging: observations and principles. Oxford University Press; 2006. [Google Scholar]
- Auld MC, Sidhu N. Schooling, cognitive ability, and health. Health Economics. 2005;14(10):1019–1034. doi: 10.1002/hec.1050. [DOI] [PubMed] [Google Scholar]
- Baeten S, Van Ourti T, van Doorslaer E. The socioeconomic health gradient across the life cycle: What role for selective mortality and institutionalization? Social Science and Medicine. 2013;97:66–74. doi: 10.1016/j.socscimed.2013.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker D, Gluckman PD, Godgrey KM, Harding JE, Owens JA, Robinson JS. Fetal nutrition and cardiovascular disease in adult life. Lancet. 1993;341(8850):938–941. doi: 10.1016/0140-6736(93)91224-a. [DOI] [PubMed] [Google Scholar]
- Becker G. A Theory of the Allocation of Time. The Economic Journal. 1965;75(299):493–517. [Google Scholar]
- Becker G. Health as human capital: synthesis and extensions. Oxford Economic Papers. 2007;59(3):379–410. [Google Scholar]
- Becker G, Murphy K. A Theory of Rational Addiction. Journal of Political Economy. 1988;96(4):675–700. [Google Scholar]
- Beckett M. Converging Health Inequalities in Later Life: An Artifact of Mortality Selection? Journal of Health and Social Behavior. 2000;41:106–119. [PubMed] [Google Scholar]
- Blanchflower DG, Oswald AJ, van Landeghem B. Imitative Obesity and Relative Utility. Journal of the European Economic Association. 2009;7:528–538. [Google Scholar]
- Blau DM. Retirement and consumption in a life cycle model’. Journal of Labor Economics. 2008;26(1):35–71. [Google Scholar]
- Blundell R, MaCurdy T. Labor Supply. In: Ashenfelter Orley, Card David., editors. Handbook of Labor Economics. Amsterdam: North-Holland; 1999. [Google Scholar]
- Bolin K, Jacobson L, Lindgren B. The family as the producer of health-when spouses are Nash bargainers. Journal of Health Economics. 2001;20:349–362. doi: 10.1016/s0167-6296(00)00086-2. [DOI] [PubMed] [Google Scholar]
- Bolin K, Lindgren B, Lindstrom M, Nystedt P. Investments in social capital – implications of social interactions for the production of health. Social Science & Medicine. 2003;56(12):2379–2390. doi: 10.1016/s0277-9536(02)00242-3. [DOI] [PubMed] [Google Scholar]
- Borg V, Kristensen TS. Social class and self-rated health: can the gradient be explained by differences in life style or work environment? Social Science & Medicine. 2000;51:1019–1030. doi: 10.1016/s0277-9536(00)00011-3. [DOI] [PubMed] [Google Scholar]
- Brown JR, Coile CC, Weisbenner SJ. The Effect of Inheritance Receipt on Retirement. Review of Economics and Statistics. 2010;92(2):425–434. [Google Scholar]
- Caputo MR. Foundations of Dynamic Economic Analysis. Cambridge University Press; 2005. [Google Scholar]
- Campbell F, Conti G, Heckman JJ, Moon SH, Pinto R, Pungello E, Pan Y. Early childhood investments substantially boost adult health. Science. 2014;343(6178):1478–1485. doi: 10.1126/science.1248429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, Lubotsky D, Paxson C. Economic status and health in childhood: The origins of the gradient. American Economic Review. 2002;92:1308–1334. doi: 10.1257/000282802762024520. [DOI] [PubMed] [Google Scholar]
- Case A, Fertig A, Paxson C. The lasting impact of childhood health and circumstance. Journal of Health Economics. 2005;24(2):365–389. doi: 10.1016/j.jhealeco.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Cawley J, Ruhm C. Handbook of Health Economics. Vol. 2. Elsevier; 2012. The Economics of Risky Health Behaviors. [Google Scholar]
- Case A, Deaton A. Broken Down by Work and Sex: How our Health Declines. In: Wise David A., editor. Analyses in the Economics of Aging. The University of Chicago Press; Chicago: 2005. pp. 185–212. 2005. [Google Scholar]
- Chiteji N. Time Preference, Noncognitive skills and Well Being across the Life Course: Do Noncognitive Skills Encourage Healthy Behavior? American Economic Review: Papers & Proceedings. 2010;100:200–204. doi: 10.1257/aer.100.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark D, Royer H. The Effect of Education on Adult Mortality and Health: Evidence from Britain. American Economic Review. 2013;103(6):2087–2120. doi: 10.1257/aer.103.6.2087. [DOI] [PubMed] [Google Scholar]
- Conti G, Heckman JJ, Urzua S. The education-health gradient. American Economic Review Papers and Proceedings. 2010;100:234–238. doi: 10.1257/aer.100.2.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contoyannis P, Jones AM, Rice N. The dynamics of health in the British Household Panel Survey. Journal of Applied Econometrics. 2004;19(4):473–503. [Google Scholar]
- Cropper ML. Health, investment in health, and occupational choice. Journal of Political Economy. 1977;85:1273–1294. [Google Scholar]
- Cropper ML. Measuring the benefits from reduced morbidity. American Economic Review. 1981;71(2):235–240. [PubMed] [Google Scholar]
- Cunha F, Heckman JJ. The technology of skill formation. American Economic Review. 2007;97(2):31–47. [Google Scholar]
- Currie J, Madrian BC. Health, Health Insurance and the labour market. In: Ashenfelter O, Card D, editors. Handbook of labour economics. Vol. 3. Amsterdam: Elsevier Science B.V; 1999. pp. 3309–3415. [Google Scholar]
- Currie J, Stabile M. Socioeconomic status and child health: why is the relationship stronger for older children? American Economic Review. 2003;93:1813–1823. doi: 10.1257/000282803322655563. [DOI] [PubMed] [Google Scholar]
- Currie J. Healthy, wealthy, and wise: Socioeconomic status, poor health in childhood, and human capital development. Journal of Economic Literature. 2009;47(1):87–122. [Google Scholar]
- Cutler DM, Lleras-Muney A. Education and Health: Evaluating Theories and Evidence. In: Schoeni Robert F, et al., editors. Making Americans Healthier: Social and Economic Policy As Health Policy. National Poverty Center Series on Poverty and Public Policy; 2008. [Google Scholar]
- Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. Journal of Health Economics. 2010;29(1):1–28. doi: 10.1016/j.jhealeco.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler DM, Lleras-Muney A, Vogl T. Socioeconomic Status and Health: Dimensions and Mechanisms. Oxford Handbook of Health Economics 2011 [Google Scholar]
- Dalgaard CJ, Strulik H. Optimal aging and death: understanding the Preston curve. Journal of the European Economic Association. 2014;12(3):672–701. [Google Scholar]
- Dalgaard CJ, Strulik H. The Economics of Health Demand and Human Aging: Health Capital vs. Health Deficits. University of Goettingen; 2015. (Discussion Paper). [Google Scholar]
- Dalgaard CJ, Strulik H. The Genesis of the Golden Age - Accounting for the Rise in Health and Leisure. Review of Economic Dynamics. 2017 forthcoming. [Google Scholar]
- Dardanoni V, Wagstaff A. Uncertainty and the demand for medical care. Journal of Health Economics. 1990;9:23–38. doi: 10.1016/0167-6296(90)90039-6. [DOI] [PubMed] [Google Scholar]
- Deaton A, Paxson C. Aging and inequality in income and health. American Economic Review. 1998;88(2):248–253. [Google Scholar]
- Deaton A. Policy implications of the gradient of health and wealth. Health Affairs. 2002;21(2):13–30. doi: 10.1377/hlthaff.21.2.13. [DOI] [PubMed] [Google Scholar]
- DeNardi M, French E, Bailey Jones J, McCauley J. Medical spending of the U.S. elderly. Fiscal Studies. 2016;37(3–4):717–747. doi: 10.1111/j.1475-5890.2016.12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Magalhaes JP. Is mammalian aging genetically controlled? Biogerontology. 2003;4(2):119–120. doi: 10.1023/a:1023356005749. [DOI] [PubMed] [Google Scholar]
- De Magalhaes JP. The Biology of Ageing: A Primer. In: Stuart-Hamilton I, editor. An Introduction to Gerontology. Cambridge University Press; Cambridge, UK: 2011. pp. 21–47. [Google Scholar]
- De Magalhaes JP. senescence.info. 2014 http://www.senescence.info’.
- DHHS. Current cigarette smoking among adults - United States, 2005–2012. US Department of Health and Human Services, MMWR. 2014;63(2):29–46. [PMC free article] [PubMed] [Google Scholar]
- Dustmann C, Windmeijer F. Wages and the Demand for Health – A Life Cycle Analysis. Germany: 2000. (IZA Discussion Paper 171). [Google Scholar]
- Eisenring C. Comparative dynamics in a health investment model. Journal of Health Economics. 1999;18(5):655–660. doi: 10.1016/s0167-6296(99)00003-x. [DOI] [PubMed] [Google Scholar]
- Ehrlich I, Chuma H. A Model of the Demand for Longevity and the Value of Life Extension. Journal of Political Economy. 1990;98(4):761–782. doi: 10.1086/261705. [DOI] [PubMed] [Google Scholar]
- Ehrlich I. Uncertain lifetime, life protection, and the value of life saving. Journal of Health Economics. 2000;19(3):341–367. doi: 10.1016/s0167-6296(99)00030-2. [DOI] [PubMed] [Google Scholar]
- Erbsland M, Ried W, Ulrich V. Econometric Analysis of Health Data. John Wiley & Sons, Ltd; 2002. Health, health care, and the environment: econometric evidence from German micro data; pp. 25–36. [DOI] [PubMed] [Google Scholar]
- Finkelstein A, Luttmer EF, Notowidigdo MJ. What good is wealth without health? The effect of health on the marginal utility of consumption. Journal of the European Economic Association. 2013;11(s1):221–258. [Google Scholar]
- Forster M. The meaning of death: some simulations of a model of healthy and unhealthy consumption. Journal of Health Economics. 2001;20:613–638. doi: 10.1016/s0167-6296(01)00080-7. [DOI] [PubMed] [Google Scholar]
- Fuchs VR. The Health Economy. Harvard University Press; Cambridge, MA: 1986. [Google Scholar]
- Galama TJ, Kapteyn A. Grossman’s missing health threshold. Journal of Health Economics. 2011;30(5):1044–1056. doi: 10.1016/j.jhealeco.2011.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galama TJ, Hullegie P, Meijer E, Outcault S. Is there empirical evidence for decreasing returns to scale in a health capital model? Health Economics. 2012;21(9):1080–1100. doi: 10.1002/hec.2843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galama TJ, vanKippersluis H. Health Inequalities through the Lens of Health Capital Theory: Issues, Solutions, and Future Directions. In: Bishop John., editor. Research on Economic Inequality. 2013. (Volume 21: Health and Inequality). Eds: Pedro Rosa Dias, Owen O’Donnell. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galama TJ. (CESR Schaeffer Working Paper 2015-004).A Contribution to Health Capital Theory. 2015 [Google Scholar]
- Galama TJ, van Kippersluis H. (CESR-Schaeffer Working Paper Series 2015-001).A Theory of Education and Health. 2015 [Google Scholar]
- Gjerde J, Grepperud S, Kverndokk S. On adaptation and the demand for health. Applied Economics. 2005;37(11):1283–1301. [Google Scholar]
- Glied S, Lleras-Muney A. Technological Innovation and Inequality in Health. Demography. 2008;45(3):741–761. doi: 10.1353/dem.0.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman DP, Smith JP. Can Patient Self-Management Help Explain the SES Health Gradient? Proceedings of the National Academy of Science. 2002;99:10929–10934. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman M. The Demand for Health - A theoretical and Empirical Investigation. New York: National Bureau of Economic Research; 1972a. [Google Scholar]
- Grossman M. On the Concept of Health Capital and the Demand for Health. Journal of Political Economy. 1972b;80(2):223–255. [Google Scholar]
- Grossman M. The Human Capital Model. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. Vol. 1. Elsevier Science; 2000. pp. 347–408. [Google Scholar]
- Hall RE, Jones CI. The Value of Life and the Rise in Health Spending. The Quarterly Journal of Economics. 2007;122(1):39–72. [Google Scholar]
- Halliday TJ, He H, Ning L, Zhang H. Health Investment over the Life-Cycle. Macroeconomic Dynamics. 2017 forthcoming. [Google Scholar]
- Heckman JJ. The economics, technology, and neuroscience of human capability formation. Proceedings of the national Academy of Sciences. 2007;104(33):13250–13255. doi: 10.1073/pnas.0701362104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herd P, Schoeni RF, House JS. Upstream solutions: does the supplemental security income program reduce disability in the elderly? Milbank Quarterly. 2008;86(1):5–45. doi: 10.1111/j.1468-0009.2007.00512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Lepkowski JM, Kinney AM, Mero RP, Kessler RC, Regula Herzog A. The Social Stratification of Aging and Health. Journal of Health and Social Behavior. 1994;35(3):213–234. [PubMed] [Google Scholar]
- Hugonnier J, Pelgrin F, St-Amour P. Health and (Other) Asset Holdings. The Review of Economic Studies. 2013;80(2):663–710. [Google Scholar]
- Hugonnier J, Pelgrin F, St-Amour P. Closing down the shop: Optimal health and wealth dynamics near the end of life. Faculty of Business and Economics (HEC), University of Lausanne; 2016. Jul, Manuscript. [DOI] [PubMed] [Google Scholar]
- Imbens G, Rubin D, Sacerdote B. Estimating the Effect of Unearned Income on Labor Supply, Earnings, Savings and Consumption: Evidence from a Survey of Lottery Players. American Economic Review. 2001;91(4):778–794. [Google Scholar]
- Jacobson L. The family as producer of health - an extension of the Grossman model. Journal of Health Economics. 2000;19:611–637. doi: 10.1016/s0167-6296(99)00041-7. [DOI] [PubMed] [Google Scholar]
- Jones A, Laporte A, Rice N, Zucchelli E. A synthesis of the Grossman and Becker-Murphy models of health and addiction: theoretical and empirical implications. Centre for Health Economics, University of York; 2014. (Working paper). [Google Scholar]
- Kawachi I, Berkman L, editors. Neighborhoods and health. Oxford, U.K.: Oxford University Press; 2003. [Google Scholar]
- Kemna H. Working conditions and the relationship between schooling and health. Journal of Health Economics. 1987;6:189–210. doi: 10.1016/0167-6296(87)90008-7. [DOI] [PubMed] [Google Scholar]
- Kuhn M, Wrzaczek S, Prskawetz A, Feichtinger G. Optimal choice of health and retirement in a life-cycle model. Journal of Economic Theory. 2015;158:186–212. [Google Scholar]
- Laibson D. Life-cycle consumption and hyperbolic discount functions. European Economic Review. 1998;42:861–871. [Google Scholar]
- Liljas B. The demand for health with uncertainty and insurance. Journal of Health Economics. 1998;17(2):153–170. doi: 10.1016/s0167-6296(97)00021-0. [DOI] [PubMed] [Google Scholar]
- Lleras-Muney A, Lichtenberg F. The Effect of Education on Medical Technology Adoption: Are the More Educated More Likely to Use New Drugs. (special issue in memory of Zvi Griliches, No 79/80).Annales d’Economie et Statistique. 2005 [Google Scholar]
- Lleras-Muney A. The relationship between education and adult mortality in the United States. Review of Economic Studies. 2005;72(1):189–221. [Google Scholar]
- Longo VD, Mitteldorf J, Skulachev VP. Programmed and altruistic ageing. Nat Rev Genet. 2005;6(11):866–872. doi: 10.1038/nrg1706. [DOI] [PubMed] [Google Scholar]
- Lynch JW, Kaplan GA, Shema SJ. Cumulative Impact of Sustained Economic Hardship on Physical, Cognitive, Psychological, and Social Functioning. New England Journal of Medicine. 1997;337(26):1889–1895. doi: 10.1056/NEJM199712253372606. [DOI] [PubMed] [Google Scholar]
- Lynch SM. Cohort and Life-Course Patterns in the Relationship between Education and Health: A Hierarchical Approach. Demography. 2003;40:309–331. doi: 10.1353/dem.2003.0016. [DOI] [PubMed] [Google Scholar]
- Mackenbach JP, Huisman M, Andersen O, Bopp M, Borgan JK, Borrell C, et al. Inequalities in lung cancer mortality by the educational level in 10 European populations. European Journal of Cancer. 2004;40(1):126–135. doi: 10.1016/j.ejca.2003.10.018. [DOI] [PubMed] [Google Scholar]
- Marmot M, Ryff CD, Bumpass LL, Shipley M, Marks NF. Social inequalities in health: next questions and converging evidence. Social Science & Medicine. 1997;44(6):901–910. doi: 10.1016/s0277-9536(96)00194-3. [DOI] [PubMed] [Google Scholar]
- Marmot M. Multi-level approaches to understanding social determinants. In: Berkmanm Lisa, Icawachi Ichiro., editors. Social Epidemiology. Oxford: Oxford University Press; 1999. [Google Scholar]
- Michaud PC, van Soest A. Health and wealth of elderly couples: Causality tests using dynamic panel data models. Journal of Health Economics. 2008;27:1312–1325. doi: 10.1016/j.jhealeco.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mincer JA. Schooling, Experience, and Earnings. Columbia University Press; 1974. [Google Scholar]
- Moody HR, Sasser . Aging: Concepts and controversies. 8th SAGE publications; 2014. [Google Scholar]
- Muurinen JM. Demand for health: a generalized Grossman model. Journal of Health Economics. 1982;1:5–28. doi: 10.1016/0167-6296(82)90019-4. [DOI] [PubMed] [Google Scholar]
- Murphy KM, Topel RH. The value of health and longevity. Journal of Political Economy. 2006;114(5):871–904. [Google Scholar]
- Nelder JA, Mead R. A simplex method for function minimization. The Computer Journal. 1965;7(4):308–313. [Google Scholar]
- Oster E, Shoulson I, Dorsey ER. Limited Life Expectancy, Human Capital and Health Investments. American Economic Review. 2013;103(5):1977–2002. doi: 10.1257/aer.103.5.1977. [DOI] [PubMed] [Google Scholar]
- Pearson T, Russell J, Campbell MJ, Barker ME. Do ’food deserts’ influence fruit and vegetable consumption? - A cross-sectional study. Appetite. 2005;45(2):195–197. doi: 10.1016/j.appet.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Podor M, Halliday TJ. Health Status and the Allocation of Time. Health Economics. 2012;21:514–527. doi: 10.1002/hec.1725. [DOI] [PubMed] [Google Scholar]
- Poterba JM, Venti SF, Wise DA. Investigations in the Economics of Aging. University of Chicago Press; 2011. Were They Prepared for Retirement? Financial Status at Advanced Ages in the HRS and AHEAD Cohorts; pp. 21–69. [Google Scholar]
- Poterba J, Venti S, Wise DA. Health, Education, and the Postretirement Evolution of Household Assets. Journal of Human Capital. 2013;7(4):297–339. doi: 10.1086/673207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravesteijn B, Van Kippersluis H, Van Doorslaer E. The contribution of occupation to health inequality. In: Dias Pedro Rosa, ODonnell Owen., editors. Research on Economic Inequality, Volume 21: Health and Inequality. Emerald Group Publishing; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ried W. Comparative dynamic analysis of the full Grossman model. Journal of Health Economics. 1998;17:383–425. doi: 10.1016/s0167-6296(97)00038-6. [DOI] [PubMed] [Google Scholar]
- Rosen S. The value of changes in life expectancy. Journal of Risk and Uncertainty. 1988;1:285–304. [Google Scholar]
- Ross CE, Wu CL. Education, Age, and the Cumulative Advantage in Health. Journal of Health and Social Behavior. 1996;37:104–20. [PubMed] [Google Scholar]
- Savelyev P. Socioemotional Skills, Education, and Longevity of High-Ability Individuals. Vanderbilt University; 2014. (Working Paper). [Google Scholar]
- Scholz JK, Seshadri A. Health and Wealth In a Lifecycle Model. University of Wisconsin-Madison; 2016. (working paper July 2016). [Google Scholar]
- Schuenemann J, Strulik H, Trimborn T. The Gender Gap in Mortality: How Much is Explained by Behavior? Journal of Health Economics. 2017 doi: 10.1016/j.jhealeco.2017.04.002. forthcoming. [DOI] [PubMed] [Google Scholar]
- Seierstad A, Sydsaeter K. Optimal Control Theory With Economic Applications. In: Bliss CJ, Intriligator MD, editors. Advanced Texbooks in Economics. Vol. 24. Elsevier; North Holland: 1987. Series Editors. [Google Scholar]
- Serdula MK, Gillespie C, Kettel-Khan L, Farris R, Seymour J, Denny C. Trends in fruit and vegetable consumption among adults in the United States: behavioral risk factor surveillance system, 1994–2000. American Journal of Public Health. 2004;94(6):1014–1018. doi: 10.2105/ajph.94.6.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A. In: An inquiry into the nature and causes of the wealth of nations. Campbell Roy H, Skinner Andrew S., editors. Oxford: Clarendon Press; 1776. 1976. [Google Scholar]
- Smith JP. The impact of socioeconomic status on health over the life course. Journal of Human Resources. 2007;42(4):739–764. [Google Scholar]
- Strulik H. Frailty, Mortality, and the Demand for Medical Care. Journal of the Economics of Ageing. 2015;6:5–12. [Google Scholar]
- Strulik H. (Cege Discussion Paper 293).The Return to Education in Terms of Wealth and Health. 2016 [Google Scholar]
- Van de Ven W, van der Gaag J. Health as an unobservable: A MIMIC-model of the demand for health care. Journal of Health Economics. 1982;1:157–183. doi: 10.1016/0167-6296(82)90013-3. [DOI] [PubMed] [Google Scholar]
- Van Kippersluis H, Van Ourti T, ODonnell OA, van Doorslaer E. Health and income across the life cycle and generations in Europe’. Journal of Health Economics. 2009;28(4):818–830. doi: 10.1016/j.jhealeco.2009.04.001. [DOI] [PubMed] [Google Scholar]
- Van Kippersluis H, O’Donnell O, van Doorslaer E, Van Ourti T. Socioeconomic Differences in Health over the Life Cycle in an Egalitarian Country. Social Science and Medicine. 2010;70(3):428–438. doi: 10.1016/j.socscimed.2009.10.020. [DOI] [PubMed] [Google Scholar]
- Van Kippersluis H, Galama TJ. Wealth and health behavior: Testing the concept of a health cost. European Economic Review. 2014;72:197–220. doi: 10.1016/j.euroecorev.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viscusi KW. Wealth Effects and Earnings Premiums for Job Hazards. Review of Economics and Statistics. 1978;60:408–416. [Google Scholar]
- Viscusi KW, Aldy JE. The value of a statistical life: a critical review of market estimates throughout the world. Journal of risk and uncertainty. 2003;27(1):5–76. [Google Scholar]
- Wagstaff A. The demand for health: Some new empirical evidence. Journal of Health Economics. 1986a;5:195–233. doi: 10.1016/0167-6296(86)90015-9. [DOI] [PubMed] [Google Scholar]
- Wagstaff A. The demand for health: Theory and applications. Journal of Epidemiology and Community Health. 1986b;40:1–11. doi: 10.1136/jech.40.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeckhauser R. Medical insurance: A case study of the tradeoff between risk spreading and appropriate incentives. Journal of Economic Theory. 1970;2(1):10–26. [Google Scholar]
- Zweifel P, Breyer F. Health Economics. Oxford University Press; New York: 1997. [Google Scholar]
- Zweifel P, Felder S, Meiers M. Ageing of population and health care expenditures: a red herring? Health Economics. 1999;8(6):485–496. doi: 10.1002/(sici)1099-1050(199909)8:6<485::aid-hec461>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]


