Abstract
We performed a retrospective analysis to evaluate treatment outcomes and the risk of fatal hemorrhage by tumor regression when definitive concurrent chemo-radiotherapy (CCRT) was delivered to patients with non–small cell lung cancer (NSCLC) invading adjacent great vessels on radiological findings. We selected 37 unresectable NSCLC patients with adjacent great vessel invasion (GVI) by carefully reviewing each patient’s images. The criteria of definite GVI were as follows: irregular indentation at the tumor–vessel contact border, slit-like narrowing of adjacent great vessels by the tumor, presence of intra-luminal mass formation, tumors contacting >5 cm of adjacent great vessel and obliteration of the intervening fat plane between tumor and adjacent great vessel, and/or tumors contacting more than half of the circumference of the aortic wall. All of the patients completed the CCRT, of which the median dose was 66.0 Gy (range, 59.4–72.0 Gy) with 1.8 or 2.0 Gy per fraction. The 2-year overall survival (OS) rate for total patients was 48.2%. Early nodal staging (P = 0.006) and good performance status (P = 0.044) were identified as independent prognostic factors associated with better OS. There was no fatal complication related to the GVI, such as a sudden death or massive hemoptysis due to vascular rupture after CCRT. We concluded that definitive CCRT for NSCLC patients with GVI on radiological findings has a low risk of fatal complication and it can benefit long-term survival when treated with CCRT in patients with early nodal staging or good performance status.
Keywords: chemoradiation, non–small cell lung carcinoma, great vessel invasion, complication
INTRODUCTION
Non–small cell lung cancer (NSCLC) with great vessel invasion (GVI) is classified into T4 stage according to the American Joint Committee on Cancer (AJCC) [1]. Although the survival benefits of complete surgical resection have been reported in several studies [2–4], the majority of patients in this category are managed by non-surgical treatments widely ranging from only supportive care to chemotherapy and/or radiation therapy (RT).
RT is frequently given to these patients and plays a role in treatments with both palliative and curative intent. While RT with moderate dose (30–40 Gy) is usually used for symptom palliation, higher dose RT with >60 Gy is needed for local tumor control. Concurrent chemo-radiotherapy (CCRT) has been claimed to yield long-term survival benefits in patients with T4 NSCLC based on the results from randomized trials for Stage IIIB NSCLC [5, 6]. However, T4 NSCLC contains diverse groups of patients; in particular, there is no published data on the clinical result of CCRT in the subgroup of T4 NSCLCs with adjacent GVI. NSCLC invading adjacent great vessels has been considered to have a high risk of massive hemorrhage during or after CCRT because rapid tumor regression or necrosis by CCRT may generate defects in tumor-invaded vessels, without allowing time for healing the defects. Many patients in this group have therefore been treated with more conservative treatment modalities than the standard recommendations for Stage IIIB NSCLC, such as sequential chemotherapy and RT, RT alone, or palliative chemotherapy only. On the other hand, this group of patients still belongs to localized Stage IIIB, and certain subgroups, such as patients with good performance status or younger age, may have a better chance of longer survival or even cure with more aggressive treatment options. Therefore, selective patients with NSCLC with GVI have also been treated with CCRT. However, there is little data regarding fatal complications after CCRT and there are no universally accepted treatment guidelines for these patients. We, therefore, performed a retrospective analysis to evaluate treatment outcomes and the risk of fatal complications in NSCLC patients with adjacent GVI on radiological findings after definitive CCRT.
MATERIALS AND METHODS
Study design and patient selection
Between August 1996 and March 2015, 278 patients were registered as having T4 NSCLC with radiological GVI at our institution. All medical records and imaging studies of these patients were reviewed retrospectively. The treatment modalities were determined according to the performance status, patients’ preference, or multidisciplinary team approaches. The inclusion criteria were as follows: (i) presence of histologically confirmed NSCLC, (ii) fulfilled the radiological criteria of GVI on computed tomography (CT) or magnetic resonance image (MRI) as described in the following section, (iii) tumor judged unresectable by at least one thoracic surgeon, (iv) absence of any distant metastasis, (v) completion of the treatment course with definitive CCRT. Of the 278 patients, 241 patients were excluded, and the inclusion flow is summarized in Fig 1. Finally, 37 of the 278 patients were included in the current analysis. This study was approved by the Samsung Medical Center Institutional Review Board (2017-10-076).
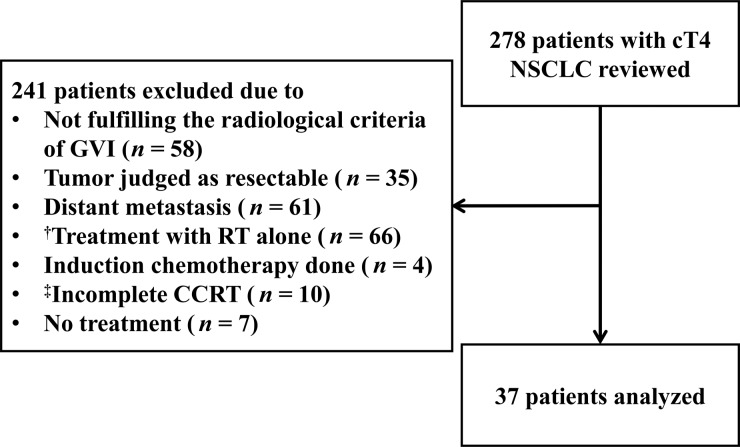
Fig. 1.
Flow diagram of patient inclusion. NSCLC = non–small cell lung cancer, GVI = great vessel invasion, RT = radiation therapy, CCRT = concurrent chemo-radiotherapy. †All of the patients in this group received palliative RT alone, with a total dose of 20–48 Gy, of which the doses per fraction were 2.5–4 Gy. ‡The reasons for incomplete CCRT were disease progression during the CCRT (n = 2), poor performance status (n = 3), patients’ refusal (n = 2), and comorbidities such as lung abscess (n = 2) and pneumonia (n = 1).
Great vessel invasion
There are no universally accepted criteria to define GVI by NSCLC on CT or MRI. Therefore, we defined it as radiological findings indicating definite tumor invasion to the great vessels, based on the previous literature [7–9] as follows: (i) irregular indentation at the tumor–vessel contact border, (ii) slit-like narrowing of adjacent great vessels by the tumor, (iii) presence of an intra-luminal mass formation, (iv) tumors contacting >5 cm of adjacent great vessel and obliteration of the intervening fat plane between tumor and adjacent great vessel, (v) tumors contacting more than half of the circumference of the aortic wall. The GVI was categorized according to five sites as follows: (i) pulmonary artery (PA), (ii) superior vena cava (SVC), (iii) aortic arch (AA), (iv) descending aorta (DA), and (v) heart (H) invasion. Representative images of the GVIs are shown in Fig. 2.
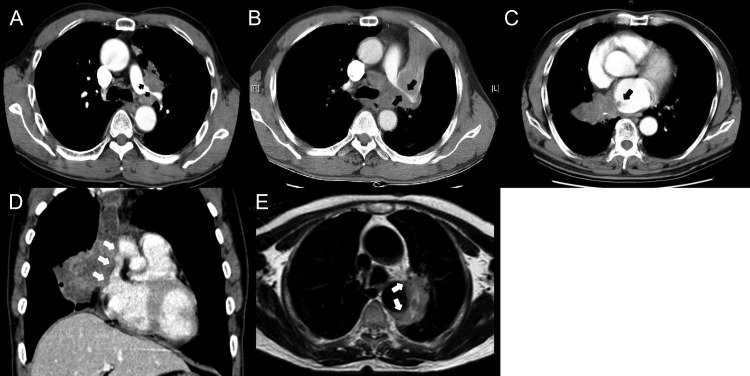
Fig. 2.
Representative images of great vessel invasions (GVIs): (A) irregular indentation at the tumor and left pulmonary artery contact border (black arrows), (B) slit-like narrowing of left pulmonary artery contact border by the tumor (black arrows), (C) presence of intra-luminal mass formation (black arrows), (D) tumor contacting >5 cm of adjacent great vessel and obliteration of the intervening fat plane between tumor and adjacent great vessel (white arrows), and (E) tumor contacting more than half of the circumference of the aortic wall (white arrows).
Pre-treatment evaluation
Pathologic confirmation of NSCLC was performed in all patients by bronchoscopy or percutaneous needle aspiration and biopsy. The diagnostic and staging work-ups included a complete history-taking and physical examination, simple chest X-rays, chest CT scans that routinely covered the liver and adrenal glands, bronchoscopic evaluation with biopsy or washing cytology, blood tests and whole-body bone scans. Chest MRI was performed for three patients.18F-deoxy-glucose positron emission tomography (FDG-PET) or PET/CT was performed in 12 patients.
Treatment
CCRT with a median dose of 66.0 Gy (range, 59.4–72.0 Gy) and 1.8 or 2.0 Gy per fraction was administered over 6–7 weeks. Cisplatin-based chemotherapy was delivered to 35 patients concurrently with docetaxel (n = 16), paclitaxel (n = 11), etoposide (n = 6), vinorelbine (n = 1) or genexol (n = 1). Two patients received carboplatin-based chemotherapy concurrently with docetaxel (n = 1) or paclitaxel (n = 1).
RT planning
In all patients, contrast-enhanced CT scans were performed in a supine position for 3D planning. CT images with 2.5–5.0 mm thickness were obtained during free breathing. The clinical target volume (CTV) was delineated with a 3–5 mm margin around the gross tumor volume (GTV) for consideration of microscopic tumor extension. The elective nodal irradiation was omitted. The planning target volume (PTV) was generated with an additional margin of 0.5 cm around the CTV to compensate for respiratory movement and set-up uncertainty. The beam margin was 1 cm around the PTV. Radiation dose was prescribed at the isocenter, with correction for tissue heterogeneity. Three or four beam arrangements were typically used to adequately cover the target volume and minimize the dose to normal tissues such as lung, spinal cord, and esophagus.
Statistical analysis
The actuarial survival rate was determined by the Kaplan–Meier method. The duration of survival was calculated from the date of initiation of RT to the date of the last follow-up or death. The duration of local control (LC) was calculated from the date of initiation of RT to the date of the local failure or last follow-up. Survival differences between groups were compared by the log-rank test, and the Cox proportional hazards regression model was used for multivariate analysis. A P-value of <0.05 was considered statistically significant.
RESULTS
Patient characteristics
Patient characteristics are present in Table 1. The median age of all patients was 63 years (range, 34–80 years). Eleven patients (30%) were N0 stage. AA invasion was developed in 4 patients, DA in 3, PA in 13, SVC in 10, and H invasion in 11. Simultaneous tumor invasions of 2 great vessels were shown in 4 patients. PA and SVC invasion was shown in 2 patients, and PA and H invasions in 2 patients. No patient received the anticoagulant or anti-angiogenesis drug during the treatment and the follow-up. The distribution in characteristics of the GVI of the tumor according to the radiologic criteria is also summarized in Table 1. Tumors in 19 patients fulfilled two or more radiological criteria for GVI.
Table 1.
Characteristics of patients (N= 37)
| Characteristics | Number of patients (%) |
|---|---|
| Age | |
| <65 years | 21 (57) |
| ≥65 years | 16 (43) |
| Sex | |
| Male | 35 (95) |
| Female | 2 (5.4) |
| ECOG status | |
| 0 | 3 (8.1) |
| 1 | 31 (84) |
| 2 | 3 (8.1) |
| N staging | |
| 0 | 11 (30) |
| 1 | 2 (5.4) |
| 2 | 12 (32) |
| 3 | 12 (32) |
| Histology | |
| Squamous cell carcinoma | 21 (57) |
| Adenocarcinoma | 11 (30) |
| Not specified | 5 (13) |
| Invasion site | |
| Aortic arch | 4 (11) |
| Descending aorta | 3 (8.1) |
| Pulmonary artery | 13 (35) |
| Superior vena cava | 10 (27) |
| Heart | 11 (30) |
| Radiological criteria for GVI* | |
| 1 | 24 (65) |
| 2 | 18 (49) |
| 3 | 6 (16) |
| 4 | 2 (5.4) |
| 5 | 10 (27) |
ECOG = European Cooperative Oncology Group, N = nodal, GVI = great vessel invasion.
*Radiological criteria for GVI is as follow: 1. irregular indentation at the tumor–vessel contact border, 2. slit-like narrowing of adjacent great vessels by the tumor, 3. presence of intra-luminal mass formation, 4. tumors contacting >5 cm of adjacent great vessel and obliteration of the intervening fat plane between tumor and adjacent great vessel, and 5. tumors contacting more than half of the circumference of the aortic wall.
Treatment outcome
At the time of analysis, 24 of the 37 patients (65%) had died. Nineteen patients died of disease progression, and 2 patients died of community-acquired pneumonia and septic shock at 1 month after the completion of CCRT. Treatment-related death occurred in one patient, who died of acute respiratory distress syndrome at 4 months after the completion of CCRT. One of the remaining 2 patients died of aspiration pneumonia due to an esophagobronchial fistula at 5 months after the completion of CCRT, and the other died of hypovolemic shock due to adrenal bleeding at 7 months after the completion of CCRT. The median follow-up period of the living patients was 17 months (range, 2–88 months). Twenty-four patients (65%) have survived over 1 year. The 2-year and 5-year overall survival (OS) rate for the total population of patients was 48.2% and 22.6%, respectively (Fig. 3A). The median OS was 24 months [95% confidence interval (CI), 0.862–47.138 months] for all patients. Univariate and multivariate analysis for OS is summarized in Table 2. By univariate analysis, early N stage (0–1), and good European Cooperative Oncology Group performance status (0–1) were significantly associated with better OS. Invasion site, however, was not associated with OS.
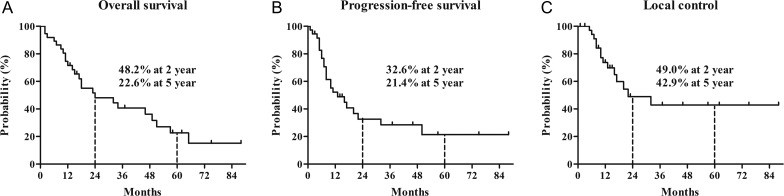
Fig. 3.
Kaplan–Meier curves of (A) overall survival, (B) progression-free survival, and (C) local control.
Table 2.
Univariate and multivariate analyses of overall survival
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| 2 year OS rate (%) | P value | Hazard ratio (95% CI) | P value | |
| Age | ||||
| <65 years | 53.2 | 0.455 | 0.90 (0.35–2.33) | 0.823 |
| ≥65 years | 40.1 | |||
| Sex | ||||
| Male | 47.9 | 0.423 | 2.68 (0.22–32.61) | 0.440 |
| Female | 50.0 | |||
| N staging | ||||
| 0–1 | 80.8 | <0.001 | 0.10 (0.02–0.53) | 0.006 |
| 2–3 | 32.4 | |||
| ECOG PS | ||||
| 0–1 | 53.2 | 0.035 | 0.20 (0.043–0.96) | 0.044 |
| 2 | 0.0 | |||
| Histology | ||||
| Squamous cell carcinoma vs | 45.8 | 0.544 | 2.49 (0.44–14.16) | 0.303 |
| Adenocarcinoma vs | 45.5 | 0.669 | 1.49 (0.32–6.99) | 0.617 |
| Not specified vs | 60.0 | 0.770 | NA | NA |
| Invasion site | ||||
| Aortic arch vs | 75.0 | 0.065 | 0.058 (0.002–2.25) | 0.127 |
| Descending aorta vs | 33.3 | 0.189 | 3.60 (0.30–43.02) | 0.312 |
| Pulmonary artery vs | 51.9 | 0.883 | 0.53 (0.074–3.73) | 0.520 |
| Superior vena cava vs | 62.5 | 0.579 | 0.16 (0.008–3.31) | 0.235 |
| Heart vs | 24.5 | 0.218 | 1.94 (0.24–15.75) | 0.537 |
OS = overall survival, CI = confidence interval, N = nodal, ECOG = European Cooperative Oncology Group, PS = Performance status, NA = Not analyzed.
At the time of analysis, 23 patients (62%) had experienced recurrence. The patterns in failures are summarized in Fig. 4. The progression-free survival (PFS) rates at 2 and 5 years were 32.6% and 21.4%, respectively (Fig. 3B). The LC rates at 2 and 5 years were 49.0% and 42.9%, respectively (Fig. 3C).
Fig. 4.
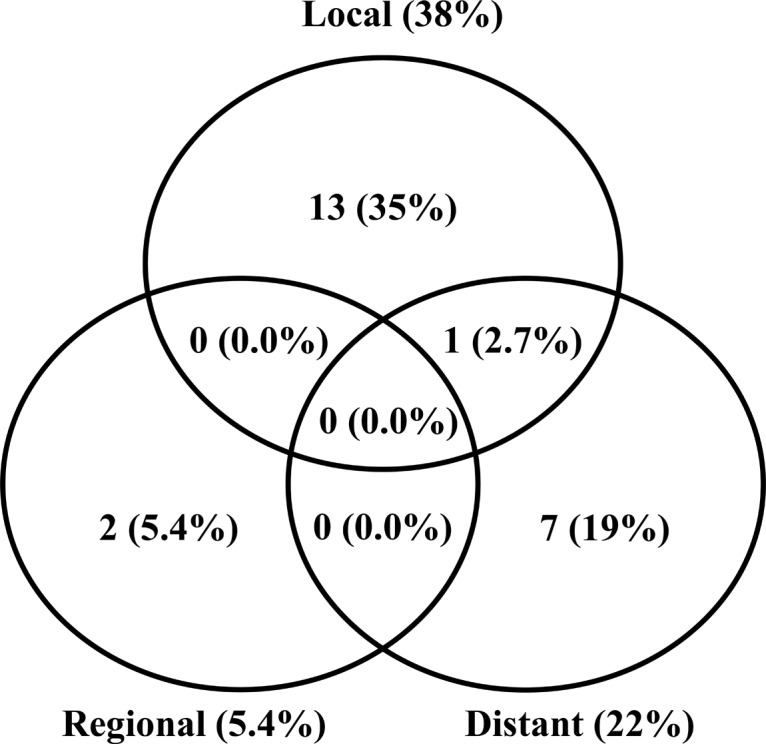
Patterns of failure.
Critical events accompanying hemoptysis occurred in two patients during the follow-up period. One patient was a 68-year-old male and he had a tumor invading the left PA (Fig. 5A). He received CCRT of 66 Gy in 33 fractions with weekly cisplatin and taxotere. He experienced hemoptysis at 17 months after CCRT and underwent the emergent angiography, which revealed a hemorrhage in the bronchial artery. Then, embolization of the bronchial artery was performed. At the time, there was no evidence of a left PA rupture in the CT scan (Fig. 5B). He died of progressed disease at 44 months after CCRT. The other patient was a 66-year-old male and he had a tumor with a heart invasion (Fig. 5C). He received CCRT of 63 Gy in 35 fractions with cisplatin and etoposide. He experienced hemoptysis at 2 months after CCRT. He underwent close observation and supportive care in an intensive care unit. At 2 months after the onset of hemoptysis, there was no evidence of the heart rupture in the follow-up CT scan (Fig. 5D). He died of progressed disease at 55 months after CCRT. Otherwise, there was no fatal complication related to the vascular rupture, and there was no sudden death due to great vessel rupture by rapid tumor regression or necrosis after CCRT.
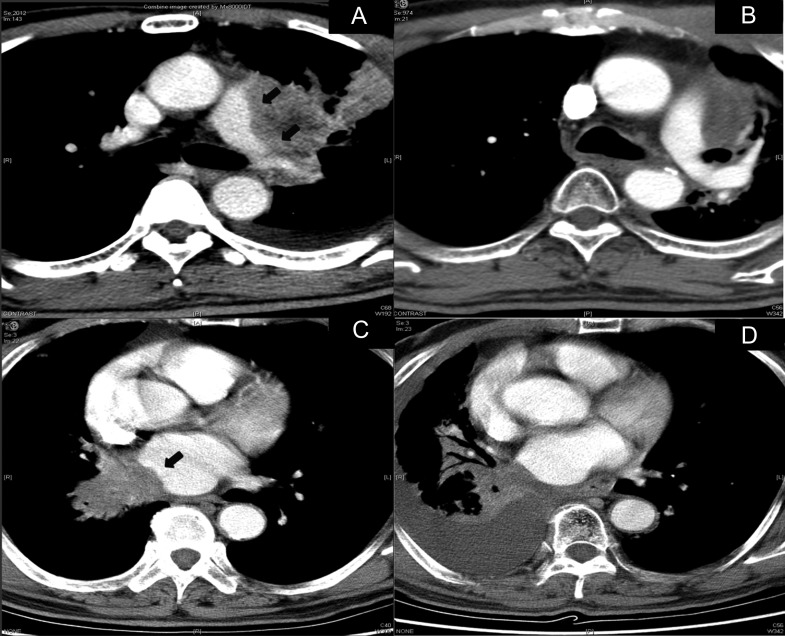
Fig. 5.
Computed tomography (CT) scans of patients who experienced critical events. (A) CT scan of 68-year-old male patient with tumor invading left pulmonary artery (black arrows) before concurrent chemo-radiotherapy (CCRT), (B) CT scan at 17 months after CCRT, when he experienced hemoptysis. There was no evidence of any left pulmonary artery rupture. (C) CT scan of 66-year-old male patient with tumor invading heart (black arrows) before CCRT, (D) CT scan at 2 months after the onset of hemoptysis at 2 months after CCRT. There is no evidence of any rupture in the heart.
DISCUSSION
The management of T4 NSCLC with adjacent GVI is challenging. Although aggressive surgery has been performed in selected patients [2–4, 10], it is generally considered unresectable, and CCRT has yielded the best outcome so far, based on the results from randomized trials for Stage IIIB NSCLC [5, 6]. However, there is a concern about the risk of leakage of great vessels after tumor regression caused by CCRT and there is limited published data on this issue. The current study showed that there was no fatal hemorrhagic event among 37 patients who were treated with CCRT for NSCLC with adjacent GVIs, and there was a treatment outcome with 2-year and 5-year OS rates of 45.5% and 21.4%, respectively—more favorable than that of total T4 NSCLCs [11]. This finding suggests that CCRT with a curative aim rather than just a palliative aim may be feasible in these patients, especially when they have good performance status or early N stage.
Surgery is also selectively recommended for NSCLC invading great vessels, and favorable outcomes have been reported [2–4, 10, 12, 13]. However, the surgical resection often results in an increased risk of postoperative complications, such as vascular leakage or hemodynamic dysfunction, because the anastomosis of involved great vessels or vascular grafts is frequently required. Furthermore, curative surgery for such patients is frequently not possible after thoracotomy due to the discovery of additional disease extension such as unresectable N3 disease or pleural metastases. Various studies showed that incomplete resection (R1 or R2 resection) had a worse OS [14–18]. Therefore, CCRT may be more appropriate than surgery for this type of patient if there is no increased risk of fatal complications due to the CCRT.
There are few studies reporting the fatal complications after definitive RT or CCRT for NSCLC with adjacent GVI. Lee et al. reported late complications in patients who received ≥66 Gy for unresectable Stage III NSCLC [19]. Two cases of fatal hemoptysis were observed, one of which had Stage IIB (T4N1) disease and developed massive hemoptysis at 4 months after the completion of RT. The original site of the hemoptysis, however, could not be identified by autopsy. Cho et al. [20] conducted a phase II study of concomitant boost to the GTV with concurrent chemotherapy for patients with unresectable stage III NSCLC. They reported two cases of sudden death with hemoptysis during RT in patients with T4 lesions with involvement of great vessels and concluded that rapid shrinkage of tumors due to the use of accelerated RT (daily 2.4 Gy) concurrently with chemotherapy might have caused perforations of the great vessels. They recommended conventional RT rather than an accelerated schedule for tumors that invade great vessels. Since we did not experience any fatal hemoptysis or hemorrhage after CCRT for NSCLC with GVI using conventional fractionation, the fraction size of the daily RT when combined with chemotherapy may be of concern. In more recent studies, the clinical outcomes of RT for NSCLC with PA invasions that were graded according to the proximities and invasiveness of the tumor to the PA on radiological finding were evaluated [9, 21]. The investigators observed sudden death from massive hemorrhage in 10.5–50% after definitive RT for tumors invading the PA extensively, with signs of vessel wall damage. The authors also argued that severe PA invasion and large PA volume irradiated with a high dose appeared to be associated with inferior OS. Those studies, however, did not present the correlation between massive hemorrhage and the damage to a particular great vessel, explicitly. As in the current study, the possibility that the hemorrhage after the completion of definitive RT resulted from the rupture of another vessel such as bronchial artery rather than invaded PA, cannot be excluded.
This obscurity in the causality between massive hemorrhage and PA damage is due to several reasons, as follows. First, the autopsy or radiological data regarding the cause of the massive hemorrhage is almost impossible to obtain after the sudden death of the patient. Although the current study utilized the CT scan and angiography and revealed that the causes of the hemoptysis were ruptures of bronchial artery, in other studies the precise locations of the hemorrhage were not evaluated. Second, in spite of using strict criteria for GVI, it is difficult to prove whether there is true GVI inducing the defect and hemorrhage in the invading site after definitive CCRT because of the lack of histologic data that can validate the radiological criteria. Therefore, we cannot exclude the possibility that images strongly indicating GVI might not correspond to true GVI. The accuracy of diagnostic images in indicating GVI has been reported rarely, and the optimal imaging modality for diagnosis of GVI by thoracic tumor has not yet been determined. Uramoto et al. evaluated the accuracy of diagnosis of aortic invasion of lung cancer, and the authors observed no true aortic invasion in intraoperative assessment, even though the radiologic finding strongly suggested the likelihood of aortic invasion [8]. Other studies reported that cine MRI might improve the accuracy in detection of GVI by intrathoracic tumors [22, 23]. The sample numbers of these studies, however, were extremely small. Therefore, further large-scaled studies which compare the radiological finding with operative or histological findings are necessary.
Nevertheless, in the current situation, in which only diagnostic images are available, our results suggest that definitive CCRT might not elevate the risk of great vessel rupture in the patients who are considered to have definite GVI by NSCLC according to the radiological criteria. However, as the previous studies have suggested, particular caution would be required in the selection of the dose regimen and the RT planning to reduce the high dose volume in the great vessels [9, 20, 21].
The present study has several limitations. By its retrospective nature, there is inevitably selection bias in the present study. The sample size of the study patients is also too small to confirm the low risk of definitive CCRT in great vessel rupture. Although prospective study is required, such study is difficult to perform due to the rarity of the disease. Therefore, a larger retrospective study will be needed to verify our results.
In conclusion, definitive CCRT for patients with unresectable clinical T4 NSCLC invading adjacent great vessels on radiological findings may have a low risk of fatal complications related to the rupture or leakage of the involved vessels; those patients with good performance status may have to be treated rather actively with CCRT and may show long-term survival.
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
FUNDING
The authors received no specific funding for this work.
REFERENCES
- 1. Edge SB, Byrd DR, Compton CC et al. AJCC Cancer Staging Manual. 7th edn New York: Springer, 2010. [Google Scholar]
- 2. McCloskey E, Selby P, de Takats D et al. Effects of clodronate on vertebral fracture risk in osteoporosis: a 1-year interim analysis. Bone 2001;28:310–5. [DOI] [PubMed] [Google Scholar]
- 3. Yang HX, Hou X, Lin P et al. [Postoperative survival comparison of non–small cell lung cancer between disease with peripheral direct adjacent invasion and resectable T4 disease with mediastinal structures invasion]. Zhonghua Yi Xue Za Zhi 2009;89:1770–3. [PubMed] [Google Scholar]
- 4. Wu L, Xu Z, Zhao X et al. Surgical treatment of lung cancer invading the left atrium or base of the pulmonary vein. World J Surg 2009;33:492–6. [DOI] [PubMed] [Google Scholar]
- 5. Curran WJ Jr, Paulus R, Langer CJ et al. Sequential vs concurrent chemoradiation for stage III non–small cell lung cancer: randomized phase III trial RTOG 9410. J Natl Cancer Inst 2011;103:1452–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Furuse K, Fukuoka M, Kawahara M et al. Phase III study of concurrent versus sequential thoracic radiotherapy in combination with mitomycin, vindesine, and cisplatin in unresectable stage III non-small-cell lung cancer. J Clin Oncol 1999;17:2692–9. [DOI] [PubMed] [Google Scholar]
- 7. Herman SJ, Winton TL, Weisbrod GL et al. Mediastinal invasion by bronchogenic carcinoma: CT signs. Radiology 1994;190:841–6. [DOI] [PubMed] [Google Scholar]
- 8. Uramoto H, Iijima Y, Nakajima Y et al. Accurate diagnosis of aortic invasion in patients with lung cancer. Anticancer Res 2016;36:2391–5. [PubMed] [Google Scholar]
- 9. Han CB, Wang WL, Quint L et al. Pulmonary artery invasion, high-dose radiation, and overall survival in patients with non–small cell lung cancer. Int J Radiat Oncol Biol Phys 2014;89:313–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chambers A, Routledge T, Bille A et al. Does surgery have a role in T4N0 and T4N1 lung cancer? Interact Cardiovasc Thorac Surg 2010;11:473–9. [DOI] [PubMed] [Google Scholar]
- 11. Groome PA, Bolejack V, Crowley JJ et al. The IASLC Lung Cancer Staging Project: validation of the proposals for revision of the T, N, and M descriptors and consequent stage groupings in the forthcoming (seventh) edition of the TNM classification of malignant tumours. J Thorac Oncol 2007;2:694–705. [DOI] [PubMed] [Google Scholar]
- 12. Yang HX, Hou X, Lin P et al. Postoperative survival comparison of non–small cell lung cancer between disease with peripheral direct adjacent invasion and resectable T4 disease with mediastinal structures invasion. Zhonghua Yi Xue Za Zhi 2009;89:1770–3. [PubMed] [Google Scholar]
- 13. Misthos P, Papagiannakis G, Kokotsakis J et al. Surgical management of lung cancer invading the aorta or the superior vena cava. Lung Cancer 2007;56:223–7. [DOI] [PubMed] [Google Scholar]
- 14. Collaud S, Bongiovanni M, Pache JC et al. Survival according to the site of bronchial microscopic residual disease after lung resection for non–small cell lung cancer. J Thorac Cardiovasc Surg 2009;137:622–6. [DOI] [PubMed] [Google Scholar]
- 15. Kim D, Kim HK, Choi YS et al. Central lung cancer management: impact of bronchial resection margin length. Thorac Cardiovasc Surg 2015;63:583–8. [DOI] [PubMed] [Google Scholar]
- 16. Tomaszek SC, Kim Y, Cassivi SD et al. Bronchial resection margin length and clinical outcome in non–small cell lung cancer. Eur J Cardiothorac Surg 2011;40:1151–6. [DOI] [PubMed] [Google Scholar]
- 17. Sawabata N, Ohta M, Matsumura A et al. Optimal distance of malignant negative margin in excision of nonsmall cell lung cancer: a multicenter prospective study. Ann Thorac Surg 2004;77:415–20. [DOI] [PubMed] [Google Scholar]
- 18. El-Sherif A, Fernando HC, Santos R et al. Margin and local recurrence after sublobar resection of non–small cell lung cancer. Ann Surg Oncol 2007;14:2400–5. [DOI] [PubMed] [Google Scholar]
- 19. Lee CB, Stinchcombe TE, Moore DT et al. Late complications of high-dose (≥66 Gy) thoracic conformal radiation therapy in combined modality trials in unresectable stage III non–small cell lung cancer. J Thorac Oncol 2009;4:74–9. [DOI] [PubMed] [Google Scholar]
- 20. Cho KH, Ahn SJ, Pyo HR et al. A Phase II study of synchronous three-dimensional conformal boost to the gross tumor volume for patients with unresectable Stage III non-small-cell lung cancer: results of Korean Radiation Oncology Group 0301 study. Int J Radiat Oncol Biol Phys 2009;74:1397–404. [DOI] [PubMed] [Google Scholar]
- 21. Ma JT, Sun L, Sun X et al. Is pulmonary artery a dose-limiting organ at risk in non–small cell lung cancer patients treated with definitive radiotherapy? Radiat Oncol 2017;12:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Uramoto H, Kinoshita H, Nakajima Y et al. Easy diagnosis of aortic invasion in patients with lung cancer using cine magnetic resonance imaging. Case Rep Oncol 2015;8:308–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ried M, Hnevkovsky S, Neu R et al. Impact of surgical evaluation of additional cine magnetic resonance imaging for advanced thymoma with infiltration of adjacent structures: the thoracic surgeon’s view. Thorac Cardiovasc Surg 2017;65:244–9. [DOI] [PubMed] [Google Scholar]