Abstract
Background
In modern obstetrical practice, incidence of induction of labour is on rise for varied maternal and foetal indications. Ultrasound can help obstetricians in counselling patients before induction of labour and explain the probability of successful induction.
Objectives
To study the role of foetal head–perineum distance in predicting successful vaginal delivery and to correlate with other parameters such as cervical length and Bishop score.
Design
This study is a prospective case–control study in a tertiary care teaching hospital.
Population
There were 250 term patients between 37 and 40+ weeks with singleton cephalic presentation with no contraindications for vaginal delivery.
Methods
Prior to induction of labour, transperineal ultrasound was performed to measure foetal head–perineum distance. Simultaneously, cervical length was performed using transvaginal ultrasound probe. Bishop score was determined at the same time by clinical examination.
Main Outcome Measures
Outcome of induction was considered successful when it resulted in vaginal delivery. It was considered to be a failure if patient did not get into active phase of labour or an operative intervention had to be performed because of non-progress of labour in active phase of labour. Cases were excluded if caesarean delivery had to be performed in the event of foetal distress.
Results
It was observed that as the transperineal foetal head–perineum distance decreased, the rate of vaginal delivery increased. Similarly, when foetal head–perineum distance increased, the rate of caesarean delivery increased. At a cut-off ≤ 5.5 cm, foetal head–perineum distance had a maximum predictability (sensitivity 97%, specificity 88.1%).
Conclusion
Transperineal foetal head–distance measured by ultrasound can be used as an important tool to predict vaginal delivery before induction of labour.
Keywords: Induction of labour, Transperineal ultrasound, Foetal head–perineum distance
Introduction
It is every obstetrician’s and patient’s desire to have not only uneventful antenatal period, but also a natural vaginal delivery during labour with no compromise with health of mother and baby. However, not all women get into spontaneous labour and as many as 13–20% require induction of labour for varied indications which include both maternal and foetal causes [1]. Traditionally success of induction is determined by Bishop score, but this score is observer based and significant disagreements have been observed between two resident doctors [2]. This influences the outcome of women chosen for vaginal delivery by induction; many of them end up in operative delivery mainly due to non-progress of labour and foetal distress. This contributes to increasing trend of caesarean deliveries and complications associated with emergency caesareans are well known [3]. There are added short-term and long-term risks and also cost associated with operative delivery. Many times, the patient ends up in second-stage emergency caesarean delivery for a deeply impacted head in pelvis which can result in substantial blood loss during surgery, uterine extensions, bladder injuries, broad ligament haematomas, and one should not forget the risk of foetal injuries, especially after difficult extraction [4]. Even the post-operative period can be morbid due to post-partum fever and wound infection.
There are continuous efforts to standardise labour prediction models using intrapartum ultrasound which nullifies subjective errors of digital pelvic examination. All the components of Bishop score such as cervical length, dilatation, position, consistency and station of foetal head can be studied by ultrasound, and in fact, there are several ultrasound-based prediction systems for determining the success of induction of labour [5]. In addition, new ultrasound parameters such as foetal head position with respect to pelvic girdle, foetal spine position, angle of progression, head to symphysis distance and head to perineum distance have been extensively explored [6–8].
One of the important parameters in labour that determines the successful outcome is distance of the presenting part from the outlet. Traditionally, this is determined by the head distance either above or below the ischial spine, which is determined by per vaginal examination. However, digitally assessed head station during intrapartum period many times is erroneous, inaccurate and not consistently reproducible by different examiners [9]. In fact, intrapartum ultrasound examination is more specific and correlates well with different sonographers, and there is a significant disagreement between vaginally performed assessment and ultrasound assessment [10].
Ultrasound has been evolving as an important adjunct tool for the practicing obstetricians to counsel the patients before induction of labour and explain them the probability of successful induction based on imaging findings.
The aim of the present study is to evaluate the role of foetal head–perineum distance as a predictor of successful vaginal delivery using transperineal ultrasound.
Materials and Methods
This is a prospective observational study carried out in the Department of Obstetrics and Gynaecology, in a tertiary care hospital. The project was approved by institutional ethics committee. The study population included term patients between 37 and 40+ weeks, who were induced for various reasons over a period of 2 years. Inclusion criteria were age between 18 and 38 years, gestational age 37–40+ weeks, live singleton pregnancy with cephalic presentation. Patients in labour, previous LSCS, major foetal anomaly were excluded from the study. Women with pre-labour rupture of membranes (PROM) were not considered as a contraindication for enrolment into the study.
Calculated sensitivity of the foetal head to perineum distance for predicting vaginal delivery in labouring women is around 62% [11]. The minimum required sample size is determined by Buderer’s formula:
where N = number of patients, Z1 − α/2 = 1.96 (standard normal deviate value that divides the central 95% of z distribution from 5% in the tails), p = the reported sensitivity (62%, i.e. 0.62), L = absolute precision desired on either side (half width of the confidence interval of the confidence interval) of sensitivity (10% i.e. 0.1).
Accordingly, sample size required was 90, and we enrolled 250 women that can potentially increase the power of the study. As we wanted to compare multiple parameters such as cervical length, Bishop score, birth weight, foetal head position, etc., we recruited more number of cases keeping in mind need for emergency caesarean deliveries not related to foetal head distance (for example, dinoprostone-induced uterine hyperstimulation, foetal distress in labour, sudden cord prolapse, worsening of hypertension, etc.). Larger sample size also allowed subgroup analysis for better interpretation of data and meaningful conclusion.
All eligible women admitted for delivery who were planned for induction of labour underwent imaging procedure. A 3.5-MHz abdominal probe was covered with sterile glove and was placed on the perineal area between two ischial tuberosities and was directed towards the presenting part. The shortest distance from the outer bony limit of foetal skull to skin surface of the perineum in a transverse view was measured to represent FHPD (Fig. 1). Following transperineal scan, transvaginal ultrasound was performed using 5.5-MHz ultrasound probe to measure cervical length. After the scans, pervaginal examination was performed to assess the various components of modified Bishop score (min 0, max 10). If cervix was found unfavourable, induction of labour was using dinoprostone gel 0.5 mg (6 hourly induction, maximum 3 doses, if patient did not get into active labour, then induction was considered unsuccessful) or else oxytocin drops in cases where cervix was nicely favourable. The patients were followed up till delivery.
Fig. 1.

Caliper placement to calculate FHPD
Outcome of induction was considered as successful when it resulted in a vaginal delivery. (Vacuum and forceps delivery were also included.) Outcome was considered unsuccessful when it resulted in caesarean delivery (for reasons like failed induction and non-progress of labour). Caesarean section done for foetal distress was excluded from the study as foetal distress is not related to distance of head from perineum. Failed induction was defined as inability to achieve active phase of labour (as indicated by the cervical dilatation less than 4 cm).
Non-progress of labour was defined according to WHO modified partograph with the following criteria:
Protracted active phase (dilatation line crossing alert line and nearing the action line).
Secondary arrest of cervical dilatation
Secondary arrest of descent
Prolonged second stage
Statistical Package for the Social Science (SPSS-16) was used for evaluation of the predictive factors for FHPD, cervical length and Bishop score and was compared with each other for their accuracy using receiver operating curve (ROC). Sensitivity and specificity for best cut-offs for FHPD, cervical length and Bishop score were also calculated.
Results
Out of 250 patients enrolled for the study, 135 women delivered successfully vaginally and 115 had to undergo caesarean delivery. Of these 115 cases of caesarean delivery, 31 cases were excluded as the operative procedure was performed for indication not related to unsuccessful induction such as occurrence of foetal distress in labour, thick meconium-stained liquor with unfavourable cervix. The final analysis was performed from 219 subjects (135 vaginal births and 84 caesarean births) (Fig. 2).
Fig. 2.
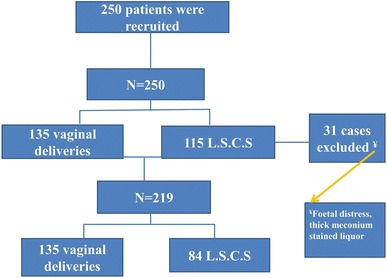
Consort statement
Among these 219 patients, 164 women (74.9%) were primigravida and 55 (25.1%) were multigravida. The majority of the multigravidae had vaginal delivery (83.6%). Nearly 45% of primigravidae required caesarean delivery due to indications like failed induction (73%) and for non-progress of labour (27%). Table 1 shows the maternal characteristics of these 219 women. The Bishop score ranged between 1 and 8. Transcervically measured cervical length spanned between 1.2 and 4 cm. FHPD ranged from 3 to 7 cm.
Table 1.
Patient profile (n = 219)
| Parameters | Mean ± SD (range) |
|---|---|
| Maternal age in years | 26.95 ± 3.5 (18–38) |
| Gestation in weeks | 38.82 ± 1.08 (37–40.4) |
| Height (cm) | 156.26 ± 5.65 (140–177) |
| Weight (kg) | 62.9 ± 8.76 (44–94) |
| Bishop’s score before IOL | 3.92 ± 1.18 (1–8) |
| Cervical length (cm) | 2.89 ± 0.56 (1.2–4) |
| Foetal head–perineum distance (cm) | 5.19 ± 0.92 (3–7) |
| B.M.I (kg/m2) | 25.78 ± 3.5 (16.94–40.16) |
| Baby birth weight (kg) | 2.91 ± 0.41 (1.9–4.1) |
Table 2 shows mode of delivery according to the FHPD categories. With FHPD ≤ 4 cm, everyone had vaginal delivery, and when FHPD was more than 6.1 cm, practically all had caesarean delivery (p < 0.001). ROC analysis was performed to find out which cut-off determines the best predictability. It was found that with FHPD ≤ 5.5 cm there were maximum sensitivity (93%) and specificity (94.4%) (AUC—area under curve of 0.977, p < 0.001). Applying this cut-off, it was found that only 7.1% required caesarean delivery with FHPD ≤ 5.5 cm and that when it was more than 5.5 cm, 95% required caesarean section, and this finding too was found to be statistically significant (p value < 0.001).
Table 2.
Correlation of foetal head–perineum distance (A), cervical length (B) and pre-induction Bishop score (C) with mode of delivery
| Vaginal delivery, n (%) | L.S.C.S, n (%) | |
|---|---|---|
| A. Foetal head–perineum distance (FHPD) in cm | ||
| 3.1–4 | 19 (100) | 0 |
| 4.1–5 | 100 (97.1) | 3 (2.9) |
| 5.1–6 | 16 (28.6) | 40 (71.4) |
| 6.1–7 | 0 | 41 (100) |
| B. Cervical length in cm | ||
| ≤ 2 | 23 (92) | 2 (8) |
| 2.1–3 | 89 (83.2) | 18 (16.8) |
| 3.1–4 | 23 (26.4) | 64 (73.6) |
| C. Pre-induction Bishop score | ||
| 1 | 0 | 2 (100) |
| 2 | 2 (12.5) | 14 (87.5) |
| 3 | 24 (36.9) | 41 (63.1) |
| 4 | 59 (74.7) | 20 (25.3) |
| 5 | 31 (83.8) | 6 (16.2) |
| 6 | 12 (92.3) | 1 (7.7) |
| 7 | 6 (100) | 0 |
| 8 | 1 (100) | 0 |
Chi-square test for correlation between modes of delivery. A. foetal head–perineum distance (p < 0.001), B. cervical length (p < 0.001) and C. Bishop score (p < 0.001)
Relationship between cervical length and mode of delivery is also shown in Table 2. It was observed that with minimum cervical length ≤ 2 cm, vaginal delivery rates were more (92%) and with higher cervical length, caesarean delivery rates are more (73.6%), and this was statistically significant (p < 0.001). Sensitivity and specificity were calculated at different cut-offs ranging from 1 to 4 cm of cervical length, and we found that around ≤ 3 cm of cervical length there were maximum sensitivity (80%) and specificity (80.4%). Area under ROC for prediction of vaginal delivery was 0.786 indicating a strong correlation. It was found that only 15.7% required caesarean section when cervical length was below or equal to 3 cm and when cervical length was more than 3 cm, 76% required caesarean section. This finding was statistically significant by Chi-square test (p < 0.001).
Similarly, Bishop’s score was compared with mode of delivery (Table 2). It was observed that when the Bishop’s score was more, the rate of vaginal delivery increased, whereas when Bishop’s score was less than 3, rate of caesarean section increased. Sensitivity and specificity were calculated at different cut-offs ranging from 1 to 8, and we found that around Bishop’s score of ≥ 3, maximum sensitivity (74%) and specificity (74.4%) could be achieved. Area under ROC for prediction of vaginal delivery was 0.786 and p value was observed to be < 0.001, which was highly significant.
In Table 3, it was observed that predictability of FHPD was higher in all aspects compared to Bishop’s score and cervical length. Multiple comparisons of ROCs (Fig. 3) too proved the same.
Table 3.
Diagnostic accuracy of predictive factors in determining successful vaginal delivery
| Parameters | Cut-off | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | Area under curve |
|---|---|---|---|---|---|---|---|
| FHPD | < 5.5 cm | 97 | 88.1 | 92.9 | 94.9 | 93.6 | 0.977 |
| Cervical length | < 3 cm | 83 | 76.2 | 84.8 | 73.6 | 80.4 | 0.855 |
| Bishop’s score | > 3 | 80.7 | 67.9 | 80.1 | 68.7 | 75.8 | 0.786 |
FHPD foetal head–perineum distance
Fig. 3.
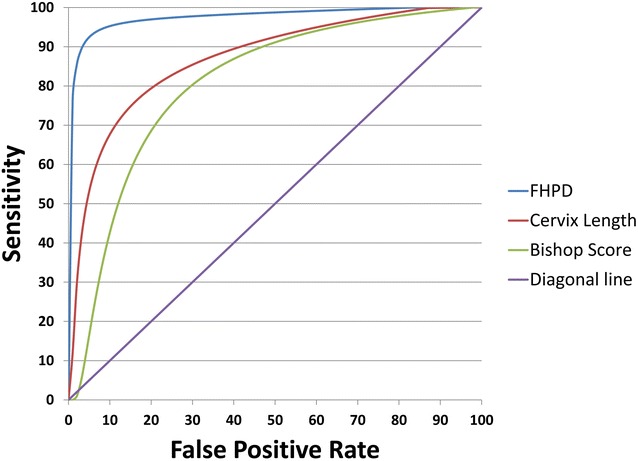
ROC analysis
Discussion
In modern obstetrics, induction of labour has become a routine procedure in high-risk pregnant women, as immediate delivery has potential benefits. Nearly 5–15% of pregnant women undergo routine induction of labour for various maternal and foetal indications [12]. One of the important factors for failure of induction is improperly chosen patient for vaginal delivery. When a case of undiagnosed cephalopelvic disproportion is tried for vaginal delivery, labour may get complicated by failure of cervical dilation and head descent and an emergency operative delivery may be required. As the rate of abdominal deliveries has increased over the period of years and the failure of descent is the second most common indication for performing caesarean section, it is important to evaluate a method to predict successful vaginal delivery. Traditionally success of induction was determined by Bishop score which requires digital pelvic examination, but recent evidence suggests that such an examination is highly erroneous and subjective and does not predict descent of the foetal head during the first and second stages of labour. Ultrasound examination prior to labour has proven to be one of the important aids to the obstetrician in order to decide proper plan of labour. In these days ultrasound machines are easily available, and they are safe and non-invasive, easy to learn and simple to use. The parameters can be easily recorded and analysed. There is increasing evidence that the estimation of FHPD (foetal head–perineum distance) with transperineal ultrasound can predict the success of labour induction. The procedure per say is least time-consuming, has a quick learning curve and can be easily mastered.
Table 4 shows various FHPD cut-offs that successfully indicated vaginal birth by different authors in various labour scenarios. Torkildsen et al. [13] conducted a study in Stavanger university hospital in Norway in 2011 which included 110 patients prior to induction of labour. The cut-off for FHPD obtained in their study was < 4 cm. The sensitivity, specificity and negative predictive value were 62, 85 and 43%. In a study by Ali et al. [14], sensitivity, specificity and negative predictive value of FHPD to predict successful vaginal birth at the cut-off value of < 4.8 cm were 84.7, 84 and 61.8%, which was comparable with our study. Another study in 2014 which involved singleton primigravidae with prolonged first stage of labour by Eggebo and Hassan et al. [15] reported that foetal head–perineum distance measured ultrasonically predicted successful vaginal delivery when the cut-off was ≤ 4 cm. The observed sensitivity and specificity for transperineal distance to predict successful vaginal birth were 69 and 72%. We too found that transperineally assessed foetal head distance showed a better sensitivity of 97%, specificity of 88.1% and accuracy of 93.6% compared to other parameters like cervical length and Bishop’s score.
Table 4.
FHPD cut-off in prediction of successful vaginal births in different labour scenarios
| References | No. of patients (N) | Patient characteristics | Parity | FHPD cut-off (cm) | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|---|---|
| Torkildsen et al. [13] | 110 | Term patients with singleton vertex with prolonged first stage | Primigravidae | < 4 | 62 | 85 | 93 | 43 |
| Mohamed [14] | 180 | Term patient with singleton vertex who underwent induction of labour | Both primigravidae and multigravidae | < 4.8 | 84.7 | 84 | 94.7 | 61.8 |
| Eggebo and Hassan [15] | 150 | Term patients with singleton vertex with prolonged first stage | Primigravidae | < 4 | 69 | 82 | 92 | 48 |
| Yudianto et al. [16] | 319 | Term patient with singleton vertex in active phase of labour | Both primigravidae and multigravidae | < 4.35 | 98 | 80 | 99.6 | 44 |
| Kasbaoui et al. [17] | 659 | Term patient with singleton vertex who had instrumental vaginal delivery | Both primigravidae and multigravidae | < 4 | 73.3 | 47.6 | 23.7 | 88.7 |
| Present study (2018) | 219 | Term patient with singleton vertex who underwent induction of labour | Both primigravidae and multigravidae | ≤ 5.5 | 97 | 88.1 | 92.9 | 94.9 |
FHPD has also been used prior to instrumental vaginal delivery to assess difficult extraction. A study from Indonesia proved that FHPD cut-off point of ≤ 4.35 cm had 98% of sensitivity and 80% of specificity and as much as 89% subjects had successful vaginal delivery (AUC 0.825) [16]. In another study from Strasbourg University, France, with FHPD more than 40 mm, incidence of difficult extraction was more even after adjusting for multiparity, foetal head position and foetal weight (odds ratio 2.38; 95% confidence interval 1.51–3.74; p = 0.0002) [17]. A recent review suggested that medico-legal problems arising from difficult instrumental vaginal extraction can be minimised by adopting ultrasound imaging that offers an objective assessment of foetal pelvic relationships such as foetal weight, foetal head station and foetal position prior to attempted vaginal delivery [18].
In most of the quoted studies, the FHPD is less than 4–4.35 cm, because of the fact that they were conducted in women who were already in labour, having conditions such as prolonged first stage [13, 15], active phase of labour [16] and those who had instrumental vaginal delivery in the second stage of labour [17]. One study [14] had subjects similar to our study who had FHPD measured before induction of labour, and these patients are likely to have relatively high station of head as labour process has not yet begun. They had the FHPD cut-off of 4.8 cm which is closer to our cut-off of 5.5 cm, and this slight difference is maybe because of geographical variation (Egypt vs. India).
Though it appears that transperineal ultrasound assesses head to perineum distance more objectively, it cannot completely replace the role of vaginal examination in labour. Adequacy of pelvis for vaginal delivery, assessment of cephalopelvic disproportion, softness and stretchability of cervix are till today well determined by digital examination. Ultrasound can determine cervical dilatation in latent phase of labour (< 4 cm of cervical dilatation), but thereafter cervical dilatation can be better assessed only by PV examination (> 4–10 cm) in active phase of labour. It is well known that partographic assessment of progress of labour requires regular and periodic assessment of cervical dilatation beyond 4 cm for diagnosis of abnormalities of cervical dilatation, such as protracted active phase and secondary arrest of cervical dilatation. However, many mothers feel vaginal examination is more painful and theoretically it can increase the risk of ascending bacterial infection. By adopting intrapartum ultrasound, one can minimise the number of vaginal examination and can effectively determine the foetal head position in relation to maternal pelvis (occipito-anterior or occipito-posterior positions). At present, it can only be said that ultrasound can be a useful adjunct tool to add more information to digital assessment and helps obstetrician to cross-check his findings and improvise on findings of PV examination.
In this study, transperineal ultrasound examination was performed with ease and in a short time. Pregnant women well tolerated transperineal ultrasound without any discomfort, and same observations have been made by all the studies mentioned so far.
Limitations of the Study
Recently, many other ultrasound parameters such as angle of head progression, head to internal os distance, head position (occipito-anterior or occipito-posterior), foetal head perimeter, public arch angle and posterior cervical angle either as a single or multiple parameter/s have been studied to determine successful labour. There should be adjustment for these confounding variables before one can say FHPD is the stand-alone parameter which influences labour outcome. Further studies are required to know whether incorporation of these parameters improves the efficacy of intrapartum sonography in predicting successful induction.
Conclusion
The foetal head–perineum distance measured by transperineal ultrasound is an easy, simple, reliable, comfortable and non-invasive method for prediction of mode of delivery in women before induction of labour and can be used as an adjunct method for assessment of foetal head descent during labour.
Acknowledgements
Authors would like to thank Manipal Academy of Higher Education for granting seed money to conduct this study.
Dr Jijisha Ali, MBBS, MS
did her MBBS from Pushpagiri Institute of Medical Sciences And Research Centre, Tiruvalla, and MS in Obstetrics and Gynaecology from Kasturba Medical College, Manipal, Karnataka. After her postgraduation, she joined Kasturba Medical College, Manipal, as a senior resident. Currently, she is working as a registrar in Obstetrics and Gynaecology at Mediclinic Welcare Hospital, Garhoud, under Ministry of Health, Government of Dubai.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Statement
The study has been approved by institutional ethical committee of Manipal Academy of Higher Education.
Human and Animal Rights
This study does not involve any research work involving animals and was performed on term pregnant women undergoing induction of labour.
Informed Consent
Informed consent has been obtained from all participating subjects prior to study.
Footnotes
Jijisha Ali is a Registrar in Obstetrics and Gynaecology; Shripad Hebbar is a Professor of Obstetrics and Gynaecology & Unit V Head.
Contributor Information
Jijisha Ali, Email: jijshaji@gmail.com.
Shripad Hebbar, Email: drshripadhebbar@yahoo.co.in.
References
- 1.Al-shaikh GK, Wahabi HA, Fayed AA, et al. Factors associated with successful induction of labor. Saudi Med J. 2012;33(3):298–303. [PubMed] [Google Scholar]
- 2.Garcia-simon R, Oros D, Gracia-cólera D, et al. Cervix assessment for the management of labor induction: reliability of cervical length and Bishop Score determined by residents. J Obstet Gynaecol Res. 2015;41(3):377. doi: 10.1111/jog.12553. [DOI] [PubMed] [Google Scholar]
- 3.Betrán AP, Ye J, Moller AB, et al. The increasing trend in caesarean section rates: global, regional and national estimates: 1990–2014. PLoS ONE. 2016;11(2):e0148343. doi: 10.1371/journal.pone.0148343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gurung P, Malla S, Lama S, et al. Caesarean section during second stage of labor in a tertiary centre. J Nepal Health Res Counc. 2017;15(2):178–181. doi: 10.3126/jnhrc.v15i2.18210. [DOI] [PubMed] [Google Scholar]
- 5.Bajpai N, Bhakta R, Kumar P, et al. Manipal cervical scoring system by transvaginal ultrasound in predicting successful labour induction. J Clin Diagn Res. 2015;9(5):QC04-9. doi: 10.7860/JCDR/2015/12315.5970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dückelmann AM, Bamberg C, Michaelis SA, et al. Measurement of fetal head descent using the ‘angle of progression’ on transperineal ultrasound imaging is reliable regardless of fetal head station or ultrasound expertise. Ultrasound Obstet Gynecol. 2010;35(2):216–222. doi: 10.1002/uog.7521. [DOI] [PubMed] [Google Scholar]
- 7.Youssef A, Maroni E, Ragusa A, et al. Fetal head-symphysis distance: a simple and reliable ultrasound index of fetal head station in labor. Ultrasound Obstet Gynecol. 2013;41(4):419–424. doi: 10.1002/uog.12335. [DOI] [PubMed] [Google Scholar]
- 8.Ahn KH, Oh MJ. Intrapartum ultrasound: a useful method for evaluating labor progress and predicting operative vaginal delivery. Obstet Gynecol Sci. 2014;57(6):427–435. doi: 10.5468/ogs.2014.57.6.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wiafe YA, Whitehead B, Venables H, et al. The effectiveness of intrapartum ultrasonography in assessing cervical dilatation, head station and position: a systematic review and meta-analysis. Ultrasound. 2016;24(4):222–232. doi: 10.1177/1742271X16673124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tutschek B, Torkildsen EA, Eggebø TM. Comparison between ultrasound parameters and clinical examination to assess fetal head station in labor. Ultrasound Obstet Gynecol. 2013;41(4):425–429. doi: 10.1002/uog.12422. [DOI] [PubMed] [Google Scholar]
- 11.Torkildsen EA, Salvesen KÅ, Eggebø TM. Agreement between two- and three-dimensional transperineal ultrasound methods in assessing fetal head descent in the first stage of labor. Ultrasound Obstet Gynecol. 2012;39(3):310–315. doi: 10.1002/uog.9065. [DOI] [PubMed] [Google Scholar]
- 12.Vogel JP, Souza JP, Gülmezoglu AM. Patterns and outcomes of induction of labour in Africa and Asia: a secondary analysis of the WHO global survey on maternal and neonatal health. PLoS ONE. 2013;8(6):e65612. doi: 10.1371/journal.pone.0065612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Torkildsen EA, Salvesen KÅ, Eggebø TM. Prediction of delivery mode with transperineal ultrasound in women with prolonged first stage of labor. Ultrasound Obstet Gynecol. 2011;37(6):702–708. doi: 10.1002/uog.8951. [DOI] [PubMed] [Google Scholar]
- 14.Ali MS, Abdelhafeez MA, Medhat A. The distance from maternal perineum to fetal head distance as a predictive of successful induction of labor. Nat Sci. 2013;11:19–24. [Google Scholar]
- 15.Eggebø TM, Hassan WA, Salvesen KÅ, et al. Sonographic prediction of vaginal delivery in prolonged labor: a two-center study. Ultrasound Obstet Gynecol. 2014;43(2):195–201. doi: 10.1002/uog.13210. [DOI] [PubMed] [Google Scholar]
- 16.Saroyo YB, Danarti MD. Prediction of vaginal delivery using fetal head descent assessed using transperineal ultrasound. Indones J Obstet Gynecol. 2017;5(3):149–153. doi: 10.32771/inajog.v5i3.541. [DOI] [Google Scholar]
- 17.Kasbaoui S, Séverac F, Aïssi G, et al. Predicting the difficulty of operative vaginal delivery by ultrasound measurement of fetal head station. Am J Obstet Gynecol. 2017;216(5):507.e1–507.e9. doi: 10.1016/j.ajog.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 18.Eser A, Köşüş A, Köşüş N. Intrapartum ultrasonography for prediction of vaginal delivery: review. Turkiye Klinikleri J Gynecol Obst. 2016;26(3):146–151. doi: 10.5336/gynobstet.2014-41381. [DOI] [Google Scholar]


