Abstract
Objectives
To test the application of a clinical definition of life-threatening complications in pregnancy and determine the level of near miss maternal morbidity and mortality.
Methods
A prospective observational study was conducted in the obstetrics and gynaecology department, NRS Medical College, Kolkata, India, to identify life-threatening complications using a modification of the Mantel’s criteria. The main outcome measures were validity of identification criteria, main causes and incidence of life-threatening complications in pregnancy, maternal near miss: case fatality rates, morbidity–mortality index and use rate of effective interventions.
Results
In total, 177 maternal near miss and 23 maternal deaths were identified in the screened 4400 women. The incidence of near miss was 4.02%. Main causes of maternal mortality were hypertensive disorders (43%) and renal failure (21%). Main causes of near miss were hypertensive disorders (55%), ectopic pregnancy (19%). Near miss mortality index was 7.7:1.
Conclusions
A high proportion of women with life-threatening complications and all women who died were referred from peripheral hospitals. This signals that there may have been important failures in the referral system relating to maternal care and there is a need for further investigation.
Keywords: Life-threatening complications, Obstetric near miss, Maternal mortality, Severe maternal morbidity, Severe acute maternal morbidity
Introduction
In 2010, India recorded 56,000 maternal deaths, the highest for any country in the world, and the progress in reduction in maternal mortality is slow [1, 2]. Maternal death is just the tip of the iceberg. Very severe obstetric events are thought to be more common than maternal deaths. For every woman who dies from maternal complications in the Americas, PAHO/WHO estimates that 20 others—around 1.2 million each year—suffer a life-threatening complication [3]. Many women who survive death and suffer from severe morbidity are referred to as “near misses”.
Maternal mortality is used as only indicator for the woman’s health status for a long time, but now the concept of SAMM (severe acute maternal morbidity)/near miss has emerged. Population-based studies show that the burden of overall maternal morbidity is high and that monitoring of maternal morbidity is important for improving maternal health. However, there is debate surrounding what constitutes the optimum definition of severe obstetric morbidity. A number of terms are in use to describe incidents of severe maternal ill health including life-threatening complications, severe maternal morbidity, severe acute maternal morbidity (SAMM) or near misses. The development of criteria to identify life-threatening condition is challenged by the absence of a gold standard for severe maternal morbidity. In addition, the identification of near miss cases is always retrospective, i.e. the woman needs to survive the life-threatening complication in order to be considered as a near miss case.
Three types of approaches have been proposed for defining life-threatening obstetric complications and near miss events. These approaches include definitions based on (a) management, (b) clinical signs and symptoms and (c) organ systems.
Of the 287,000 maternal deaths which occurred worldwide in 2010, India accounted for 19%, i.e. about 56,000 maternal deaths [1]. The MMR status at all India level is at 167 in 2011–13. India is unlikely to achieve the target level of 109 per 1,00,000 live births by 2015 [2]. As per the historical trend, MMR is likely to reach the level of 140 maternal deaths by 2015 [2]. West Bengal is an agriculture-dependent state in eastern India. It is India’s fourth most populous state with over 91 million inhabitants (as of 2011) [4]. The MMR in our institution was 579 in 2010 which is much higher than the state MMR of 113 in 2011–13 [5]. Studies on near misses have been scarce in India, despite the high maternal death burden. To the best of our knowledge, few studies are published in journals, none of which are conducted in eastern India. The specific objectives of this study were to test the application of a clinical definition of life-threatening complications in pregnancy and to determine the level of near miss maternal morbidity and mortality due to life-threatening obstetrical complications.
Materials and Methods
A prospective observational study was conducted in the Department of Obstetrics and Gynaecology, Nil Ratan Sircar Medical College and Hospital, Kolkata, India. This is a tertiary care hospital located in the heart of the city and well connected with suburban areas by railways and roads. The hospital provides free reproductive and child health services, and comprehensive emergency obstetric care. The antenatal clinic provides antenatal care to 12,000 women annually coming from both from urban and rural areas. The greater referral areas include three districts namely Murshidabad, Nadia and Purba Midnapore. The hospital is equipped with 300 beds with round the clock ultrasonography and laboratory facilities for blood parameters examination, nephrology department with haemodialysis facilities, one surgical intensive care unit containing three beds which are shared by both obstetrics and surgery departments and blood bank with round the clock availability of blood and blood products.
For the identification of maternal life threatening complications, a local modification of the criteria was made (Table 1) in relation with the criteria used in a similar low resource setting in Indonesia (modified Mantel's criteria) [6].
Table 4.
Mode of termination of pregnancy and perinatal outcome in women with life-threatening complications in pregnancy
| Variables | Women with life-threatening complications | Maternal deaths | Maternal near miss |
|---|---|---|---|
| N = 200 (%) | N = 23 (%) | N = 177 (%) | |
| Mode of termination of pregnancy | |||
| Caesarean delivery | 92 (46) | 12 (52.17) | 80 (45.19) |
| Vaginal delivery | 69 (34.5) | 7 (30.43) | 62 (35.02) |
| Laparotomy for ectopic | 35 (17.5) | 1 (4.34) | 34 (19.2) |
| Abortion | 4 (2) | 3 (13) | 1 (.56) |
| Caesarean section ratea | 57.15 | 63.15 | 56.33 |
| Perinatal outcome | n = 161 (%) | n = 19 (%) | n = 142 (%) |
| Live birth | 128 (79.5) | 14 (73.68) | 114 (80.28) |
| Still birth | 20 (12.4) | 4 (21) | 16 (11.26) |
| Neonatal death | 7 (4.34) | 0 | 7 (4.92) |
| Intrauterine foetal death | 6 (3.73) | 1 (5.26) | 5 (3.5) |
aCaesarean section rate—lscs/total no of deliveries
The cross-sectional study conducted in Indonesia showed a prevalence of near miss range of 4.2% in private set-up and 17% in public set-up [6]. As no study was available in our set-up, considering 4.2% as the prevalence of life-threatening complications, we calculated that we need to screen around 4700 women to identify 200 women with life-threatening complications in pregnancy.
Women in pregnancy or in puerperium till 42 days from delivery admitted at hospital were screened. All participants provided written informed consent before enrolment. Institutional Ethics Committee approved the protocol. Women suffering from chronic diseases with life-threatening complications even before the onset of pregnancy were excluded, and women who suffered from life-threatening complications arising out of accidental and incidental causes like suicide, burn injury were also excluded.
During the data collection period (between April 2013 and October 2014), daily visits were made to the wards of the hospital where patients with severe morbidity due to pregnancy, whether antepartum intrapartum or post-partum were admitted and treated. During the daily visit, the attending nursing staff and doctors were contacted and the medical charts of hospitalized women were screened for the study inclusion criteria. The staff responsible for the woman’s hospital care were not told that the woman had been identified for the presence of life-threatening complication in the study in order to avoid possible biases in conduct.
The data were collected on a pre-coded form specially developed for this purpose. After resolution of each case, the consistency and availability of the information on the form were reviewed by the senior obstetrician and the data were inserted into a database using Microsoft Excel software. The study was conducted while maintaining all confidentiality. Openepi software was used for statistical calculations.
The main outcome measures were validity of identification criteria, incidence of life-threatening complications in pregnancy, causes of life-threatening complications in pregnancy, maternal near miss, case fatality rates, morbidity–mortality index and effective intervention’s use rate.
Results
During the study period, 4400 women were screened with modified Mantel’s criteria (Table 1) and 200 women with life-threatening complications were identified of which 177 resulted in near miss and 23 ended in maternal mortality (Fig. 1). During the study period, 4081 women had live births and the incidence of life-threatening complications was calculated as 4.54% (200/4400); 95% CI [3.94–5.20] or 49 per 1000 live births and the incidence of near miss was 4.02% (177/4400); 95% CI [3.46–4.65] or 43 per 1000 live births.
Table 1.
Criteria for inclusion of cases with life-threatening complications.
(modified Mantel's criteria)
| Clinical diagnosis | Organ dysfunction | Management-based criteria |
|---|---|---|
| Eclampsiaa | Cardiac dysfunction—Pulmonary oedema, cardiac arrestd, cardiac failure | Intensive care admission |
| Ectopic pregnancyb | Pulmonary embolism | Emergency hysterectomy |
| Rupture uterusc | Vascular dysfunction—hypovolaemia requiring two or more units of blood, blood loss with hypovolaemic shock (systolic blood pressure < 90 mmHg or pulse rate > 120 bpm) | Anaesthetic accident |
| Immunological dysfunction—septic shocke | ||
| Respiratory dysfunction—intubation or ventilation for reasons other than general anaesthesia, oxygen saturation on pulse oximetry < 90% leading to ventilation | ||
| Renal dysfunction—oliguria < 30 ml per hour or < 400 ml per 24 h, shock not responsive to intravascular rehydration or diuresis, haemodialysis urea/creatinine raised | ||
| Liver dysfunction—Jaundice in pre-eclampsia, bilirubin ≥ 6 mg/dl | ||
| Cerebral dysfunction—Comafincluding metabolic coma, cerebral oedema, seizures other than eclampsia |
aEclampsia is defined as the presence of hypertension associated with proteinuria and fits. Hypertension is defined as a blood pressure > 140/90 mm. Proteinuria is defined as excretion of > 300 mg protein/24 h urine or > 1+ on a dipstick
bEctopic—clinically suspected ectopic pregnancy, haemoperitoneum confirmed on laparotomy
cUterine rupture is defined as the complete rupture of a uterus during labour, confirmed on laparotomy
dCardiac arrest is defined as loss of consciousness and absence of pulse or heartbeat
eSeptic shock—shock in the presence of sepsis; sepsis is defined as a clinical sign of infection and any three of the following: temperature > 38 °C or < 36 °C, respiration rate > 20/min, pulse rate > 90/min, WBC > 12,000
fComa—unconsciousness lasting > 12 h defined as a profound alteration of mental state that involves complete or near-complete lack of responsiveness to external stimuli or Glasgow Coma Scale
Fig. 1.
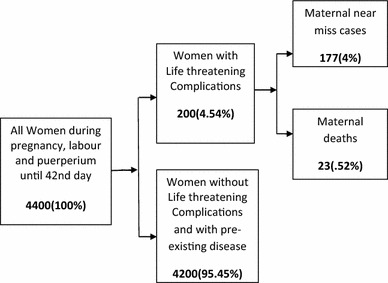
Flow chart showing events in the reproductive process
The modified Mantel’s criteria that we used identified all the 23 out of 23 women who died there by having 100%; 95% CI 85.18–100 sensitivity and also a high specificity of 95.9%; 95% CI 99.9–100. Though the positive predictive value remains low 11.5%; 95% CI 7.43–16.75, the negative predictive value is 100%; 95% CI 99.9–100.
Sensitivity was highest for organ dysfunction 95.65%; 95% CI 78.05–99.89 but was not 100% for any component. But on combination of the three components, the sensitivity was 100% (Table 2).
Table 2.
Distribution of women with life-threatening complications according to modified Mantel’s criteria
| Variables | Total casesa | Near missa | MMa |
|---|---|---|---|
| N = 200 (%) | N = 177 (%) | N = 23 (%) | |
| Clinical diagnosis (CD) only | 95 (47.5) | 94 (53.1) | 1 (4.34) |
| Organ dysfunction criteria (OD) only | 50 (25) | 38 (21.46) | 12 (52.17) |
| Management-based (MBC) only | 2 (1) | 2 (1.12) | – |
| Clinical diagnosis + organ dysfunction | 42 (21) | 34 (19.2) | 8 (34.78) |
| Organ dysfunction + management-based criteria | 7 (3.5) | 7 (3.95) | – |
| Clinical diagnosis + organ dysfunction + management-based criteria | 4 (2) | 2 (1.12) | 2 (8.69) |
| Clinical diagnosis (CD) criteria | N = 141 | N = 130 | N = 11 |
|---|---|---|---|
| Ectopic | 35 | 34 (26.15) | 1 |
| Eclampsia | 105 | 95 (73.07) | 10 |
| Rupture uterus | 1 | 1 (.7) | – |
| Organ dysfunction (OD) criteria | n = 102b | n = 80b | n = 22b |
|---|---|---|---|
| Cardiac dysfunction | 2 | 1 | 1 |
| Pulmonary embolism | Nil | Nil | Nil |
| Vascular dysfunction | 64 | 62 | 2 |
| Immunological dysfunction | 5 | 1 | 4 |
| Respiratory dysfunction | Nil | Nil | Nil |
| Renal dysfunction | 22 | 13 | 9 |
| Liver dysfunction | 7 | 5 | 2 |
| Coagulation dysfunction | 5 | Nil | 4 |
| Cerebral dysfunction | 2 | Nil | 2 |
| Management-based (MBC) criteria | N = 15 | N = 13 | N = 2 |
|---|---|---|---|
| ICU | 5 | 3 | 2 |
| Hysterectomy | 8 | 8 | – |
| Resuscitation | 1 | 1 | – |
| Anaesthetic accident | 1 | 1 | – |
aSum exceeds the total as one case could be identified with more than one criteria
bSum exceeds the total as some women had more than one organ dysfunction
Of the 200 women with life-threatening complications 165, 82% were referred from some other hospital, and of them, 23 died. Only 35 women who were directly admitted developed life-threatening complications, and none of them died.
Demographic characteristics of the women with life-threatening complications are shown in Table 3. Among pregnancies with more than 28-week gestation, 57.15% (92/161) had caesarean section and 83.2% women had live births (Table 4).
Table 3.
Socio-demographic characteristics of women with life-threatening complications in pregnancy
| Variables | Women with life-threatening complications | Maternal deaths | Maternal near miss |
|---|---|---|---|
| N = 200 (%) | N = 23 (%) | N = 177 (%) | |
| Age (years) | |||
| < 20 | 35 (17.5) | 3 (13) | 32 (18) |
| 20−35 | 161 (80.5) | 20 (86.9) | 141 (79.66) |
| > 35 | 4 (2) | 0 | 4 (2.26) |
| Parity | |||
| P 0 | 115 (57.5) | 12 (52.17) | 103 (58.19) |
| P 1 | 58 (29) | 7 (30.43) | 51 (28.81) |
| P 2 | 27 (13.5) | 4 (17.39) | 23 (12.99) |
| Religion | |||
| Hindu | 115 (57.5) | 10 (43.47) | 105 (59.32) |
| Muslim | 85 (42.5) | 13 (56.52) | 72 (40.67) |
| Antenatal check-up (n = 161)a | |||
| Booked (at least three check-ups) | 108 (67) | 12 (63.15) | 96 (67.6) |
| Unbooked | 53 (33) | 7 (36.84) | 46 (32.39) |
| Gestational age at presentation | |||
| < 28 weeks | |||
| Ectopic | 35 (17.5) | 1 (4.34) | 34 (19.2) |
| Abortion | 4 (2) | 3 (13) | 1 (.56) |
| 28–37 weeks | 49 (24.5) | 4 (17.4) | 45 (25.4) |
| Term (> 37 weeks) | 68 (34) | 3 (13) | 65 (36.7) |
| Post-partum | 44 (22) | 12 (52.17) | 32 (18.07) |
aWomen with abortion and ectopic pregnancy were excluded
The leading causes of the life-threatening complications in pregnancy were the hypertensive disorders in pregnancy (53%), ectopic pregnancy (17.5%), haemorrhage in pregnancy (15%) and acute renal failure (6.5%). The leading cause of death was the complications arising out of hypertensive disorders (eclampsia) (43.47%) and acute renal failure (21.74% deaths) (Table 5).
Table 5.
Causes of life-threatening complications in pregnancy
| Main causes | Specific causes | Women with life-threatening complications | Maternal mortality MM | Maternal near miss |
|---|---|---|---|---|
| N = 200 (%) | N = 23 (%) | N = 177 (%) | ||
| Abortion | 4 (2) | 3 (13.04) | 1 (.56) | |
| Haemorrhagic Disorders | Antepartum haemorrhage | 10 (5) | Nil | 10 (5.649) |
| Uterine rupture | 1 (.5) | Nil | 1 (.56) | |
| Post-partum haemorrhage | 15 (7.5) | Nil | 15 (8.47) | |
| Morbid adherent placenta | 4 (2) | Nil | 4 (2.25) | |
| Hypertensive disorders | Eclampsia | 105 (52.5) | 10 (43.47) | 95 (55.56) |
| HELLP syndrome | 1 (.5) | Nil | 1 (.56) | |
| Sepsis | Puerperal sepsis | 6 (3) | 3 (13) | 3 (1.69) |
| Others | ||||
| Ectopic pregnancy | 35 (17.5) | 1 (4.34) | 34 (19.2) | |
| Acute renal failure | 13 (6.5) | 5 (21.74) | 8 (4.5) | |
| Jaundice | 3 (1.5) | 1 (4.34) | 2 (1.13) | |
| Others | 3 (1.5) | Nil | 3 (1.69) |
The morbidity–mortality indices were high for ectopic pregnancy (34:1) and hypertensive disorders (9.6:1). The specific case fatality rate was highest for septic abortion complications 75% (3/4); 95% CI 9.41–99.37 followed by puerperal sepsis 50% (3/6); 95% CI [11.81–88.19] and acute renal failure 38% (5/13); 95% CI [13.86–68.42] (Table 6). Severe maternal outcome ratio was high with 49 per 1000 live births. Near miss ratio was 43 per 1000 live births. A high mortality index of 11.5 (23/200) was noted in the study.
Table 6.
Morbidity–mortality index and case fatality rate for MM and MNM causes
| Causes | MM (maternal mortality) | MNM (maternal near miss) | Near miss mortality index | Case fatality rate % (95% CI) |
|---|---|---|---|---|
| Septic abortion complications | 3 | 1 | .33:1 | 75 (19.41–99.37) |
| Puerperal sepsis | 3 | 3 | 1:1 | 50 (11.81–88.19) |
| Haemorrhagic disorders | Nil | 30 | – | 0 |
| hypertensive disorders | 10 | 96 | 9.6:1 | 9.43 (4.62–16.67) |
| Ectopic pregnancy | 1 | 34 | 34:1 | 2.85 (.72–14.92) |
| Acute renal failure | 5 | 8 | 1.6:1 | 38.46 (13.86–68.42) |
| Others | 1 | 5 | 5:1 | 16.67 (.42–64.12) |
| All causes | 23 | 177 | 7.7:1 | 11.5 (7.43–16.75) |
All women routinely received 10u oxytocin via intramuscular route immediately after delivery of foetus as part of routine active management of third stage of labour. Standard quality of care with 100% overall use rate was noted (Table 7).
Table 7.
Process and outcome indicators related to specific conditions
| Indicators | Number | Percentage (%) |
|---|---|---|
| 1. Treatment of severe post-partum haemorrhage | ||
| Target population: women with severe PPH | 19 | 9.5 |
| Medical management | 19 | 100 |
| Blood | 19 | 100 |
| Removal of retained products | 6 | 31.5 |
| Artery ligation | Nil | |
| Hysterectomy | 5 | 26.31 |
| Mortality | Nil | |
| 2. Anticonvulsants for eclampsia | ||
| Target population: women with eclampsia | 105 | 52.5 |
| Magnesium sulphate | 105 | 100 |
| Other anticonvulsant | 1 | .95 |
| Mortality | 10 | 9.52 |
| 3. Prevention of caesarean section-related infection | ||
| Target population: women undergoing caesarean section at NRS itself | 66 | |
| Prophylactic antibiotic during caesarean section | 66 | 100 |
| 4. Treatment for sepsis | ||
| Target population: women with sepsis | 10 | 5 |
| Parenteral therapeutic antibiotics | 10 | 100 |
| Mortality | 6 | 60 |
| 5. Ruptured uterus | ||
| Target population: women with ruptured uterus | 1 | .5 |
| Laparotomy | 1 | 100 |
| Mortality | Nil | |
| Overall use rate | 135 | 100 |
Discussion
To the best of our knowledge, this is the first study to document life-threatening complications in pregnancy in a tertiary care hospital in eastern India and among the few studies conducted in India. We adopted our criteria from the modified form of Mantel’s criteria used in a study conducted in Indonesia to suit the low-resource setting of the nation [6]. However, we added some modifications to these criteria to suit our set-up (Table 1).
The sensitivity, specificity and negative predictive value of our combined criteria was high, but the positive predictive value (PPV) − 11.5%; 95% CI [7.43–16.75] was low. When different criteria are used to diagnose life-threatening complications in pregnancy, a study has shown that clinical criteria are not suitable for a definitive diagnosis of maternal near miss in view of their low PPV, but they seem adequate as a first approach in investigating maternal near miss [7].
The incidence of life-threatening complication in our study was 4.54% (49 per 1000 live births) which falls within the incidence of life-threatening complications in pregnancy mentioned in different studies, i.e. 8–17.3% [6, 8–12]. A wide variation in incidence or prevalence of near miss cases is likely be due to regional variations, different set-up facilities and most importantly due to different criteria used for near miss case identification. A quiet high incidence of life-threatening complications in pregnancy in our study is likely due to two reasons: (1) we used some clinical criteria for identification of cases and (2) a large number of women were referred (80% of near miss and 100% of the women died) to our hospital in serious condition from three adjacent districts and local hospitals. In a study conducted in Indonesia, the majority of near miss in public hospitals arrived in the hospitals in a state of emergency, strongly suggesting delays in reaching the hospitals [6].
45% (80/177) of the near miss women and 52% (12/23) of the maternal deaths were delivered by caesarean sections. A high caesarean section rate has been noted among the near miss women (56%) and maternal deaths (63%) (Table 4). Fifty-nine out of 105 of the women suffering from eclampsia, i.e. 56% were delivered by caesarean section. In a study conducted in our institute over a period of 2001–2005 on 480 women with eclampsia, caesarean section rate was 19.7% and maternal mortality was 5% [13]. Caesarean delivery rate in our institute at that period (2001–2005) was 22–25 and 36.6% during the study period. Although there is an increase in caesarean section rate in our institution from 22 to 36% over a period of one decade, there is disproportionate increase (19–56%) in caesarean section rate in delivery of eclampsia mothers. However, the current literature does not enable us to assess the link between maternal mortality and rates of caesarean section above 30% [14].
The leading cause of maternal death in our study was eclampsia (43.47%, 10/23), followed by acute renal failure 21.74% (5/23), septic abortion 13% (3/23) and puerperal sepsis 13% (3/23). The overall use rate of known effective interventions to prevent or treat the main causes of maternal death and maternal near miss was 100% (Table 6). If we look at the specific causes of maternal mortality, there was no maternal death from haemorrhage which is a leading cause of maternal mortality throughout the world, and only one woman with ectopic pregnancy died. These findings support the fact that our institute being a tertiary care centre with teaching activities, evidence-based protocols with standard care were followed. However, if we consider overall near miss indicators, maternal near miss—mortality ratio was 7.69:1 which means in every eight women with life-threatening complication, one woman died and mortality index was 11.5 which means life-threatening complication was often deadly even when the women received standard care (Table 7). 80% of near miss women and all women who died were referred from peripheral hospitals. These results are consistent with most studies in developing countries, which have shown that the majority of patients are admitted to hospitals in a critical condition [12], thus suggesting that there is a delay in reaching adequate medical assistance.
The greater reference areas of our hospital included three districts namely Murshidabad, Nadia and Purba Midnapore. The Murshidabad district has a population of 71,03,807 and located at a distance of 227.5 km from Kolkata. Nadia district has population of 51,67,600 and located at a distance of 115 km from Kolkata, and Purba Midnapore district has a population of 50,95,875 and located at a distance of 126.6 km from Kolkata Our results are in agreement with the concept that the main preventive factors in decreasing maternal mortality are delays in the care process, from symptom identification by the patient to the provision of adequate treatment by healthcare professionals [15]. This is in agreement with recent knowledge that severe pregnancy complications occur practically in the same frequency in all countries and regions, regardless of the level of development and availability of resources. In fact, the varying factor is mortality, which is always higher in contexts of lower development and scarce resources, as currently demonstrated [15].
Conclusions
Our study estimated a high incidence of life-threatening complication in pregnancy. The criteria used to identify life-threatening complications were found to be useful in screening. Eclampsia was the leading cause of both near misses and maternal death. Maternal near miss mortality ratio was low despite a satisfactory overall use rate of known effective interventions to reduce maternal deaths. A high proportion of women with life-threatening complications and all women who died were referred from peripheral hospitals. This signals that there may have been important failures in the referral system relating to maternal care and that there is a need for further investigation. In addition, life-threatening complications were strongly associated with adverse perinatal outcomes which imply that efforts directed at maternal health will inadvertently lead to reduction in child mortality.
Acknowledgements
We are grateful to all women, the doctors, nurses, trainees and other staffs of our hospital without whose collaboration this study would not have been possible.
Dr. Snehamay Chaudhuri
has published more than 35 original research publications in various national and international journals. He has contributed to many chapters in textbooks for postgraduate and undergraduate students. He is the recipient of JOGI Erach Roustom Erani Research Prize for the year 2008 and FOGSI Corion award 2015. He is an author of a monograph entitled “Selected research works in obstetrics and Gynecology” and a textbook entitled “Essentials in Gynecology for undergraduate medical students”.
Author contribution
Dr. SC was involved in conception and design, analysis and interpretation of data, drafting the article, revising it critically for important intellectual content and final approval of the version to be published. Dr. SN took part in conception and design, acquisition of data, analysis and interpretation of data, drafting the article, revising it critically for important intellectual content and final approval of the version to be published.
Conflict of interest
There was nothing to disclose regarding financial, personal, political, intellectual or religious interests. There is no conflict of interest.
Ethical Approval
The study was conducted after approval by Institutional Ethics Committee of NRS Medical College, and informed consent was obtained before enrolment.
Footnotes
Dr. Snehamay Chaudhuri, MD, DNB, is an Associate Professor, Department of Obstetrics and Gynecology, at the NRS Medical College and Department of Obstetrics and Gynecology, at the Midnapore Medical College; Dr. Sumana Nath, MD is a Postgraduate Trainee, Department of Obstetrics and Gynecology at the NRS Medical College and Senior resident, Bankura Samiilani Medical College.
References
- 1.WHO, Unicef, UNFPA, and the World Bank estimates . Trends in maternal mortality: 1990 to 2010. Geneva: World Health Organization; 2012. [Google Scholar]
- 2.Millennium development goals India Country report (2015) Ministry of statistics and programme implementation. http://mospi.nic.in/sites/default/files/publication_reports/mdg_2july15_1.pdf. Accessed 4 May 2017.
- 3.PAHO/WHO urges countries to take a closer look at life-threatening complications of pregnancy and childbirth (2014). http://www.paho.org/hq/index.php?option=com_content&view=article&id=9651&Itemid=2&lang = en. Accessed 7 Oct 2014.
- 4.West Bengal Wikipidia. https://en.wikipedia.org/wiki/West_Benga. Accessed 4 May 2015.
- 5.Maternal mortality ratio (MMR) (per 1000 live births) Niti. http://niti.gov.in/content/maternal-mortality-ratio-mmr-100000-live-births. Accessed 4 May 2015.
- 6.Adisasmita A, Deviany PE, Nandiaty F, Stanton C, Ronsmans C. Obstetric near miss and deaths in public and private hospitals in Indonesia. BMC Pregnancy Childbirth. 2008;8:10. doi: 10.1186/1471-2393-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lobato G, Nakamura Pireira M, Mendes Sylvia W. Comparing different diagnostic approaches to severe maternal morbidity and near-miss: a pilot study in a Brazilian tertiary hospital. Eur J Obsterics Gynaecol Reprod Biol. 2013;167(1):24–28. doi: 10.1016/j.ejogrb.2012.10.030. [DOI] [PubMed] [Google Scholar]
- 8.Karolinski A, Mercer R, Micone P, Ocampo C, Mazzoni A, Fontana O, et al. The epidemiology of life-threatening Complications associated with reproductive process in public hospitals in Argentina. BJOG. 2013 doi: 10.1111/1471-0528.12395. [DOI] [PubMed] [Google Scholar]
- 9.Moraes PA, Barreto SM, AzeredoPasso VM, Golino PS, Costa JA, Vasconcelos MX. Incidence and main causes of severe maternal morbidity in São Luís, Maranhão, Brazil: a longitudinal study. Sao Paulo Med J. 2011;129(3):146–152. doi: 10.1590/S1516-31802011000300005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shaheen F, Begum A. Maternal “Near-Miss”. J Rawalpindi Med Coll (JRMC) 2014;18(1):130–132. [Google Scholar]
- 11.Rana A, Baral G, Dangal G. Maternal near-miss: a multicenter surveillance in Kathmandu Valley. J Nepal Med Assoc. 2013;52(190):299–304. doi: 10.31729/jnma.256. [DOI] [PubMed] [Google Scholar]
- 12.PS R, Verma S, Rai L, et al. Near-miss obstetric events and maternal deaths in a tertiary care hospital: an audit. J Pregnancy. 2013;2013:5. Article ID 393758. [DOI] [PMC free article] [PubMed]
- 13.Roy Chowdhury J, Chaudhuri S, Bhattachryya N, Biswas PK, Panpalia M. Comparison of intramuscular magnesium sulfate with low dose intravenous magnesium sulfate regimen for treatment of eclampsia. J Obstet Gynaecol Res. 2009;35(1):119–125. doi: 10.1111/j.1447-0756.2008.00842.x. [DOI] [PubMed] [Google Scholar]
- 14.WHO statement on caesarean section rate World Health Organization (2015). http://apps.who.int/iris/bitstream/10665/161442/1/WHO_RHR_15.02_eng.pdf. Accessed 19 May 2017.
- 15.Hadad SM, Cecatti JG, Souza JP, et al. Applying the maternal near miss approach for the evaluation of quality of obstetric care: a worked sample from a multicentre surveillance study. Biomed Res Int. 2014;2014:10. Article ID 080815. [DOI] [PMC free article] [PubMed]


