Abstract
Objective
The objective of the study was to assess the fetal outcome after receiving intrauterine transfusion (IUT) in Rh-isoimmunized pregnancy in a tertiary care center.
Study Design
This was a retrospective observational descriptive study in which all Rh-negative gravidas with isoimmunization warranting IUTs (40 patients) were analyzed during the period from January 1, 2010 to October 31, 2015. Primary outcome variables were fetal outcomes and procedural-related factors.
Results
Forty pregnancies (13—hydropic, 27—non-hydropic) required 74 IUTs. IUT was performed at gestational age of 15.4–33 weeks when indicated. The amount of blood transfused ranged from 4 to 110 ml. There were two sudden intrauterine fetal deaths during the procedure, four post-procedure intrauterine fetal deaths in fetuses with severe hydrops, and three neonatal deaths. The overall survival rate was found to be 77.5%.
Conclusion
IUT was found to be an effective therapy in correcting anemia in fetuses of Rh isoimmunized mothers. Early diagnosis of fetal anemia and intrauterine blood transfusion by an experienced fetal medicine specialist is very important for the perinatal outcome.
Keywords: Rh isoimmunization, Fetal anemia, Intrauterine blood transfusion, Fetal outcome
Introduction
Maternal isoimmunization occurs when a pregnant woman has an immunologic response to a paternally derived red-cell antigen inherited by the fetus. The antibodies may cross the placenta, bind to antigens present in the fetal erythrocytes, and cause hemolysis, hydrops fetalis, and fetal death [1]. Intrauterine transfusions (IUT) have been the mainstay of treatment of fetal isoimmunization since the early 1980s [2]. Previously, alloimmune hemolytic disease was the most important cause of perinatal mortality. Nowadays, perinatal survival rates can exceed 90% if anemia is diagnosed and treated in early stages in experienced centers [3–5].
An intrauterine blood transfusion under the guidance of ultrasound was done to replace fetal red blood cells being destroyed by the Rh-sensitized mother’s immune system causing fetal hemolytic anemia [6]. This treatment is meant to keep the fetal hemoglobin near optimum level until the baby is mature enough to be delivered.
Ultrasound-directed intrauterine transfusions can be done through intraperitoneal and intravascular routes. The umbilical vein at the insertion of cord into placenta and intrahepatic vein are the two safest sites for intrauterine transfusion. Intravascular transfusion enables accurate replacement with preprocedure and post-procedure fetal hematocrit estimation and is effective immediately. Intraperitoneal route administration is not immediately effective. In cases of hydropic fetuses, it is ineffective as intraperitoneal blood is not absorbed [7]. In India, few centers offer the expertise for conducting IUTs in high-risk Rh isoimmunized pregnancies with good prognosis.
This study measures the usefulness of intrauterine transfusion retrospectively in terms of the overall survival rate of fetus, need for exchange transfusion after birth, complications associated with the procedure, gestational age at delivery, and mode of delivery.
Materials and Methods
Study Design
This was a retrospective observational descriptive study in which all Rh-negative gravidas with isoimmunization warranting intrauterine transfusion (40 patients) were analyzed.
Setting
The study was conducted at Seth G.S. Medical College and Nowrosjee Wadia Maternity Hospital, Mumbai, which is a tertiary care hospital from January 1, 2010 to October 31, 2015.
Participants
Rh-negative pregnant women with age between 20 and 40 years, husbands having Rh-positive blood group, single fetus, Rh-isoimmunized pregnancy confirmed by Rh titers who had undergone intrauterine transfusion were included in the study.
Women with multifetal pregnancy and those with of any major structural abnormality in fetus on ultrasonography (USG) were excluded from the study.
Study Procedure
In this study, the indoor papers of all the participants who were included in our study from January 1, 2010 to October 31, 2015 were reviewed from our medical record department. Forty patients fulfilled our inclusion criteria and were included in study after getting the ethical clearance from the institutional review board. Waiver consent was taken. The results were expressed in terms of appropriate proportion and percentage. The overall survival rate of fetus, need for exchange transfusion after birth, complications associated with the procedure, gestational age at delivery, and mode of delivery were analyzed.
In our institute, the following protocol is used for investigation and management of Rh-sensitized pregnancy. Rh titer of all Rh-negative pregnant patients with Rh-positive husband was done. In all patients with Rh titer positive, fetal antenatal monitoring was done by Color Doppler examination. Color Doppler ultrasonography (USG) is performed to determine the middle cerebral artery peak systolic velocity (MCA PSV) meticulously using the technique described by Mari et al. [8] [Figures 1, 9] for determination of fetal anemia and its severity. Also features of ascites, pleural effusion, pericardial effusion, were assessed in all cases for determination of hydrops fetalis. Peak systolic velocity was plotted on Mari’s normograms at corresponding gestational age. Action was taken as per the following:
If peak systolic velocity was in Zone A Immediate IUT
Zone B IUT or weekly Doppler
Zone C weekly color Doppler studies performed.
Fig. 1.
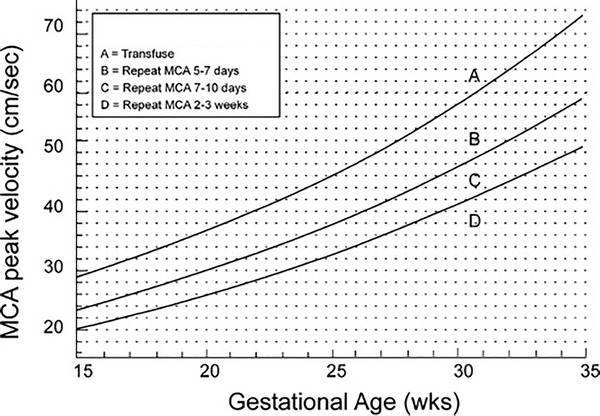
Mari chart for MCA-PSV middle cerebral artery and severity of fetal anemia
Source: Modified from Mari et al. [9]. Reproduced with permission
Intravascular route was preferred for transfusion usually at the placental end of the cord insertion. If cord was inaccessible, intrahepatic vein was used for transfusion. Intraperitoneal transfusion was done in case of difficulty in access or in case of complications or very early transfusion before 18 weeks or in combination with intravascular transfusion in order to prolong the time interval for the next transfusion. Post-transfusion hematocrit was determined after intravascular transfusion. Occasionally, sufficient sample was not obtained for post-transfusion hematocrit and monitoring was done by color Doppler as an indirect method. Color Doppler was performed 1–3 weeks starting at 15 weeks till abnormal MCA is encountered. After the first transfusion, color Doppler was performed weekly till delivery.
Technique of IUT
Written, informed, and valid consent was taken before each IUT procedure. The procedure was done under ultrasound guidance with real-time equipment with transabdominal 3.5 MHz curvilinear transducer under strict sterile technique. The fetus was paralyzed using intramuscular pancuronium 0.3 mg/kg of estimated fetal weight through spinal needle number 20 inserted into fetal thigh or buttock or intravenous vecuronium 0.1 mg/kg into cord insertion under ultrasonography guidance.
Double-packed Rh O negative blood freshly collected (less than 5 days old) cross-matched with mother’s blood was used for transfusion. Blood was transfused slowly in 10 cc aliquots using a three-way and extension tubing to connect the intravascular tubing of blood bag to spinal needle. Dose of blood required was calculated according to the fetal hematocrit, donor hematocrit, and gestational age using Nicolaides graphs [10]. Fetal heart was monitored continuously during the transfusion with a Doppler or direct ultrasound visualization and cascade observed throughout the procedure by ultrasonography at the distal end of the spinal needle. Post-transfusion blood was collected for hemoglobin and hematocrit estimation.
After the procedure, the mother was shown the cardiac activity of fetus and informed about absence of fetal movements for about 8 h due to fetal paralysis. Antenatal monitoring was done by weekly MCA-PSV measurement and biophysical profile. Antenatal steroid was given (Injection Betamethasone 12 mg IM two doses 24 h apart) to achieve lung maturity at 28–30 weeks in anticipation of preterm labor.
Delivery was conducted electively by cesarean section in most pregnancies. After delivery, cord blood was collected for hemoglobin, serum bilirubin, blood group, and direct Coombs tests.
Post-delivery newborn was kept in intensive care unit for monitoring of anemia, jaundice, prematurity and treated using intravenous immunoglobulin, phototherapy, or exchange transfusions on a case to case basis.
Statistical Analysis
No statistical package was used in the study and no comparison was done in the study. The results were expressed in terms of appropriate proportion and percentage. The overall survival rate of fetus, need for exchange transfusion after birth, complications associated with the procedure, gestational age at delivery, and mode of delivery were analyzed.
Results
There were 40 Rh isoimmunized pregnancies of which 13 fetuses were hydropic and the remaining 27 were non-hydropic. Patients who were included in the study ranged from 24 to 37 years with mean age of 30 years. Majority of the patients are in age-group of 26–30 years. Sixteen cases were diagnosed with Rh isoimmunization at an earlier stage of 28 weeks of gestation, nine(22.5%) between 28 and 30 weeks, seven (17.5%) between 30 and 32 weeks, and eight (20%) after 32 weeks. Intrauterine transfusion was performed 74 times in 40 cases. Site of transfusion depends upon numerous factors like gestational age, accessibility of the site of transfusion, and presence or absence of hydrops. The most attempted site of transfusion (52) in the study was through intraumbilical site (Table 1). The amount of blood transfused ranged from 4 to 110 ml depending upon the weeks of gestation, pretransfusion fetal hemoglobin, and presence or absence of hydrops (Table 2). During this procedure, two cases had intrauterine fetal demise.
Table 1.
Site of transfusion in IUT
| Site | No. | Percentage |
|---|---|---|
| Intraumbilical | 52 | 70.2 |
| Intraperitoneal | 13 | 17.5 |
| Intrahepatic | 9 | 12.1 |
| Total | 74 | 100 |
Table 2.
Amount of blood transfused at IUT
| Amount of blood transfused | No. of patients | Percentage |
|---|---|---|
| < 30 ml | 4 | 5.4 |
| 30–50 ml | 9 | 12.1 |
| 50–100 ml | 39 | 52.7 |
| > 100 ml | 22 | 29.7 |
| Total | 74 | 100 |
Intrauterine transfusions supported pregnancies to be carried on successfully for a period of 34–36 weeks in 45% of cases. Half of the patients, i.e., 47.5%, did not reach term gestation and either delivered or had to be delivered in view of their worsening clinical profile
Mode of delivery was by cesarean section in 30 cases (75%) (26 elective and four emergency caesarian section) and by vaginal delivery in ten cases (25%). Twenty-five percentage of babies had a birth weight of more than 2.5 kg and 67.5% of babies weighted more than 2 kg. The commonest encountered complication of neonate was related to its Rh-isoimmunized status. Neonatal jaundice occurred in majority of neonates (97%). One had cholestatic jaundice. Depending upon jaundice severity, treatment was given. About 88% of neonates received phototherapy and supportive measures but did not require exchange transfusion. However in the next line it is stated otherwise that 73.5% neonates required intervention in the form of exchange transfusion. In two neonates, the level of hemolysis was severe enough to warrant more than two exchange transfusions (Table 3).
Table 3.
Treatment of neonatal jaundice
| Modality | No. | Percentage |
|---|---|---|
| Phototherapy | 30 | 88.2 |
| Intravenous immunoglobulin | 16 | 47 |
| Exchange transfusion | 25 | 73.5 |
| 1 time | 9 | |
| 2 time | 5 | |
| 3 time | 2 |
Nearly 73.5% of the neonates required a week stay in NICU. Six neonates (17%) required prolonged stay of more than 12 days (Table 4).
Table 4.
Duration of NICU stay
| Duration of NICU stay | No. | Percentage |
|---|---|---|
| < 4 days | 12 | 35.2 |
| 4–8 days | 13 | 38.2 |
| 8–12 days | 3 | 8.8 |
| > 12 days | 6 | 17.6 |
| Total | 34 | 100 |
Fetal and neonatal outcome in the 13 hydropic fetuses showed that there was one intrauterine death (7.6%), four intrauterine fetal deaths after intrauterine transfusion (30.7%), and three neonatal deaths (23%), with five living babies at discharge with a survival rate in hydropic babies of 38.4%. In the 27 non-hydropic fetuses, only one death was noted after intrauterine transfusion with a survival rate of 96% (Table 5).
Table 5.
Perinatal outcome of the study
| Outcome | No. | Percentage |
|---|---|---|
| IUFD (intra- + post-procedure) | 6 | 15 |
| NND | 3 | 7.5 |
| Went home alive | 31 | 77.5 |
| Total | 40 | 100 |
Discussion
Management of moderate to severe fetal anemia with ultrasonography and by intrauterine blood transfusions has dramatically improved the survival rate of babies in Rh-isoimmunized mothers. It is, however, a difficult procedure associated with fetal mortality (4.8%) [11, 12].
The present study was conducted on 40 Rh-isoimmunized pregnant women of age-group ranging from 24 to 37 years. The results of the study did not show any specific age-related predominance for Rh isoimmunisation. A total of 74 ultrasound-guided intravascular transfusions were performed during 15.4–33 weeks of gestational period in patients with severe fetal anemia in which 31 cases had shown survival rate (77.5%). In the study by Sampson et al., 288 intrauterine transfusions were done for 78 fetuses and the overall survival rate was 75.6% [13].
In this study, out of 40, 13 were hydropic fetuses and 27 were non-hydropic. The average number of intrauterine transfusions in both the groups was found to be two times per patient. In study by Deka et al. [14] in 102 women, a total of 303 intrauterine transfusions were given with an average of 2.9 transfusion per patient. Transfusion amount ranged from 4 to 110 ml. On an average, half the patients required intrauterine transfusion ranging from 50 to 100 ml depending upon the weeks of gestation, pretransfusion fetal hemoglobin, and presence or absence of hydrops. Intravascular transfusion can be given earliest by 18–20 weeks. In severely isoimmunized mothers, hydrops can occur even before this gestational age. Prophylactic intraperitoneal transfusion given at the earliest time when MCA PSV demonstrates moderate to severe anemia is lifesaving for these fetuses. In this study (17.5%), fetuses were given intraperitoneal transfusion. The volume transfused is typically small. Forty-five percentage of the fetuses were delivered at near-term gestation (34–36 weeks), thus minimizing the morbidity and mortality due to prematurity. Vatsala et al. [12] reported 30% of the fetuses were delivered at near-term gestation.
Mode of delivery was decided based upon the severity of fetal anemia, Bishop’s score, pelvic adequacy, and presentation. Most of the cases (65%) were delivered by elective cesarean. Due to favorable cervix in multiparous women, vaginal delivery with intrapartum electronic monitoring was successful in 25% cases. Vatsala et al. [12] in their study reported an incidence of vaginal delivery by 32.5%.
In this study, the common complication perceived in 33 neonates was neonatal jaundice. Majority, i.e., 88.2%, received phototherapy and other supportive measures. On an average, the duration of phototherapy was 4 days. The type of phototherapy employed was single-surface phototherapy or double-surface phototherapy depending upon the level of bilirubin. Significantly high bilirubin levels were seen in 73.5% of neonates. Such neonates were treated in the form of exchange transfusions. Also 47% were given IV IgG to minimize the number of exchange transfusions. This observation was in accordance with the studies of Bujandric N in which exchange transfusions were done for treating neonatal jaundice [15].
NICU stay depended on the condition of baby at birth, level of bilirubin, and other complication of the newborn. On an average, nearly three-fourth of the neonates required a week stay in NICU for therapeutic and supportive care. Six neonates, i.e., nearly 17% required prolonged stay of more than 12 days.
In 13 hydropic fetuses, there were five intrauterine transfusion fetal deaths and three neonatal deaths, and in 27 non-hydropic fetuses who received intrauterine transfusions, only one intrauterine fetal death was recorded. Five of hydropic fetuses and 26 of non-hydropic fetuses were alive, and the survival rate was 38 and 96%, respectively. According to Vatsala et al. [12], the survival rate was 88 and 83% in hydropic and non-hydropic cases, respectively.
Thus, survival rate is more in non-hydropic neonates as compared to hydropic neonates. Survival rate in hydrops depends upon its severity, the weeks of gestation at its first presentation, and prompt intervention [3].
Conclusion
Intrauterine blood transfusion plays a very significant role in the treatment of Rh-isoimmunized pregnancies. Early detection of this problem definitely improves the perinatal outcome, particularly in case of non-hydropic compared to hydropic fetuses. Late referrals, severe Rh alloimmunization, volume overload, delay in IUT because of non-availability of blood were thought to be reasons for the poor outcome.
About the Author
Dr. Omkar Shankar Potdar is an Assistant Professor in the Department of Obstetrics and Gynecology at Government Medical College, Miraj. He graduated from B. J. Medical College, Pune (2012). He completed his Postgraduation as M.S. (Obstetrics and Gynecology) from Seth G. S. Medical College and Wadia Maternity Hospital, Mumbai in 2016. Later he joined as an Assistant Professor at GMC, Miraj. He also received D.N.B. in Obstetrics and Gynecology. He holds Fellowship in Minimal Access Surgery and Fellowship in Assisted Reproductive Techniques from World Laparoscopy Hospital, Gurgaon (2017). He has special interest in the field of Infertility and Gynecological Endoscopy.
Authors’ Contributions
PRS designed the study model, performed IUT, and reviewed the article; HRN assisted in the IUT, wrote the article, and helped in compilation and analysis of data; and OP assisted in the IUT, compiled and analyzed the data, and helped in article write-up.
Conflict of interest
The authors have no conflicts of interest.
Ethical Approval
For this type of study, formal consent is not required and waiver consent was obtained.
Human and Animal Rights
Retrospective observation study analyzes records of Rh-sensitized women in pregnancy.
Informed Consent
Waiver consent was taken.
Footnotes
Dr. Omkar Potdar MD is a Registrar in the Department of Obstetrics and Gynecology, Seth G S Medical College, Nowrosjee Wadia Maternity Hospital, Parel, Mumbai, 400012, India; Dr. Hemraj R Narkhede MD is a Assistant Professor in the Department of Obstetrics and Gynecology, Seth G S Medical College, Nowrosjee Wadia Maternity Hospital, Parel, Mumbai, 400012, India; Dr. Purnima R. Satoskar MD, DNB, FRCOG is a Professor in the Department of Obstetrics and Gynecology, Seth G S Medical College, Nowrosjee Wadia Maternity Hospital, Parel, Mumbai, 400012, India.
References
- 1.Bowman JM. Haemolytic disease of the fetus (Erythroblastsis fetalis) In: Creasy RK, Rensnik R, editors. Maternal-fetal medicine. 7. Philadelphia: W.B. Saunders; 2014. pp. 558–568. [Google Scholar]
- 2.Badran EF, Al-lawama M, Masri A, et al. Fetal intrauterine transfusion therapy: neonatal outcomes. J Blood Lymph. 2013;3:112. [Google Scholar]
- 3.Zwiers C, Lindenburg ITM, Klumper FJ, et al. Complications of intrauterine intravascular blood transfusion: lessons learned after 1678 procedures. Ultrasound Obstet Gynecol. 2017;50(2):180–186. doi: 10.1002/uog.17319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moise KJ., Jr Management of rhesus alloimmunization in pregnancy. Obstet Gynecol. 2008;112(1):164–176. doi: 10.1097/AOG.0b013e31817d453c. [DOI] [PubMed] [Google Scholar]
- 5.Tiblad E, Kublickas M, Ajne G, et al. Procedure-related complications and perinatal outcome after intrauterine transfusions in red cell alloimmunization in Stockholm. Fetal Diagn Ther. 2011;30(4):266–273. doi: 10.1159/000328683. [DOI] [PubMed] [Google Scholar]
- 6.Urbaniak SJ, Greiss MA. RhD haemolytic disease of the fetus and the newborn. Blood Rev. 2000;14(1):44–61. doi: 10.1054/blre.1999.0123. [DOI] [PubMed] [Google Scholar]
- 7.Alec Mc Ewan . Red cell alloimmunization. In: Pavord S, Hunt B, editors. The obstetric hematology manual. New York: Cambridge University Press; 2010. pp. 73–88. [Google Scholar]
- 8.Wong KS, Connan K, Rowlands S, et al. Antenatal immunoglobulin for fetal red blood cell alloimmunization. Cochrane Database Syst Rev. 2013;5:CD008267. doi: 10.1002/14651858.CD008267.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mari G, Adrignolo A, Abuhamad AZ, et al. Diagnosis of fetal anemia with Doppler ultrasound in the pregnancy complicated by maternal blood group immunization. Ultrasound Obstet Gynecol. 1995;5(6):400–405. doi: 10.1046/j.1469-0705.1995.05060400.x. [DOI] [PubMed] [Google Scholar]
- 10.Pasman SA, Claes L, Lewi L, et al. Intrauterine transfusion for fetal anemia due to red blood cell alloimmunization: 14 years’ experience in Leuven. Facts Views Vis ObGyn. 2015;7(2):129–136. [PMC free article] [PubMed] [Google Scholar]
- 11.Lindenburg IT, Smits-Wintjens VE, van Klink JM, et al. Long-term neurodevelopmental outcome after intrauterine transfusion for hemolytic disease of the fetus/newborn: the LOTUS study. Am J Obstet Gynecol. 2012;206(2):141. doi: 10.1016/j.ajog.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 12.Vatsla D, Deepika D, Sumana G, et al. Treatment of fetal anemia in Rh isoimmunized pregnancies with intrauterine fetal blood transfusion. J Obstet Gynaecol India. 2010;60(2):135–140. doi: 10.1007/s13224-010-0019-y. [DOI] [Google Scholar]
- 13.Altunyurt S, Okyay E, Saatli B, et al. Neonatal outcome of fetuses receiving intrauterine transfusion for severe hydrops complicated by Rhesus hemolytic disease. Int J Gynecol Obstet. 2012;117:153–156. doi: 10.1016/j.ijgo.2011.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Deka D, Dadhwal V, Sharma AK, et al. Perinatal survival and procedure-related complications after intrauterine transfusion for red cell alloimmunization. Arch Gynecol Obstet. 2016;293(5):967–973. doi: 10.1007/s00404-015-3915-7. [DOI] [PubMed] [Google Scholar]
- 15.Bujandric N, Grujic J. Exchange Transfusion for Severe Neonatal Hyperbilirubinemia: 17 years’ experience from Vojvodina, Serbia. Indian J Hematol Blood Transfus. 2016;32(2):208–214. doi: 10.1007/s12288-015-0534-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


