Abstract
Objectives
To assess the effect of intravenous versus topical tranexamic acid in reducing intraoperative and postoperative blood loss in women with abdominal hysterectomy.
Materials and Methods
The study was a randomized double-blind placebo-controlled trial, carried out in a tertiary university hospital in Egypt, from November 2015 to October 2017. A total of 129 women undergoing abdominal hysterectomy for benign etiology were randomly assigned to three groups: Group I [43 patients received 110 ml normal saline IV just before skin in scion], Group II [43 patients received 1 g tranexamic acid in 100 ml saline IV just before skin in scion], and Group III [43 patients received 2 g topical tranexamic acid applied intra-abdominal after hysterectomy]. The primary outcome was intraoperative, postoperative, and all blood loss estimation.
Results
Both Group II (IV tranexamic acid) and Group III (topical tranexamic acid application) showed great reduction in intraoperative and postoperative blood loss (blood in the intra-abdominal drain) compared with Group I (placebo group), (P = 0.0001, 0.0001, 0.0001, 0.0001), so the overall estimated blood loss in groups II and III showed highly reduction compared with Group I (P = 0.0001, 0.0001).
Conclusion
Intravenous and topical tranexamic acid application is a safe and reliable method to help decrease blood loss during and after abdominal hysterectomy.
Keywords: Tranexamic acid, Randomized controlled trial, Hysterectomy
Introduction
Hysterectomy represents the second most performed surgery in gynecology after the Cesarean section. Worldwide most of the hysterectomies are performed abdominally [1]. One in nine women will undergo a hysterectomy in their lifetime [1]. Surgical blood loss of more than 1000 ml or blood loss that requires a blood transfusion usually defines intraoperative hemorrhage. Intraoperative hemorrhage has been reported in 1–2% of hysterectomy studies [2].
As with any surgical treatment, complications affect the outcomes of hysterectomy. Hemorrhage, which is the most frequent and critical complication, often occurs during surgery. Data from The Danish Hysterectomy and Hysteroscopy Database (DHHD) have revealed a relatively high complication rate of 16–18% from 1998 to 2006, of which perioperative bleeding complications represent the most common cause [3]. From 2004 to 2006, 6–8% of all women undergoing benign hysterectomy in Denmark experienced a bleeding complication [4].
Therefore, adequate hemostatic techniques are essential during abdominal hysterectomy. Currently, surgical hemostasis can be secured by a variety of methods, including mechanical sutures (or clamping), electric coagulation, ultrasonically activated scalpel, or drugs [4].
Moreover, hemostatic medications are also used. Misoprostol, oxytocin, and vasopressin are used to decrease blood loss during hysterectomy [5].
Recently, attention has focused on the use of tranexamic acid (TA) to reduce blood loss if given prophylactically at hysterectomy. This is not a uterotonic agent; TA is an antifibrinolytic agent better known to gynecologists for oral use as treatment of menorrhagia, and to trauma surgeons where it has been shown to reduce blood loss [6].
Traditionally, antifibrinolytic agents have been administered intravenously in surgical settings. Safety concerns associated with intravenous administration of tranexamic acid include thrombosis, increased seizure risk, and renal impairment [7]. Considering the safety concerns with intravenous administration, there has been a growing interest in the topical use of tranexamic acid for the prevention of bleeding associated with major surgical procedures. Although published reports of thromboembolic events with intravenous tranexamic acid are limited and meta-analyses do not suggest an elevated risk, the potential danger of thrombosis warrants investigation of alternative hemostatic strategies [7, 8]. However, among the reported hemostatic strategies, the best strategy for hysterectomy was still unclear.
Topical application of TA provides a high drug concentration at the site of the wound and a low systemic concentration. Studies from cardiac and orthopedic surgery have shown an equal or superior effect of topical application compared with intravenous TA on both bleeding and transfusion requirement. Topical treatment is cost-effective, and adverse effects or drug interactions have not been reported [9]. Topical application of TA to decrease postsurgical bleeding after major surgical procedures is a promising strategy [9].
Given the positive impact of TA on hemostasis in other specialties, perhaps modifications to the intravenous TA dosing and administration regimens may translate to a positive impact on hemostasis during hysterectomy [9].
In the view of limited, good-quality evidence available to inform on the best practices for prevention of bleeding during abdominal hysterectomy our study aimed at evaluating role of adjunctive IV versus topical tranexamic acid application for prevention of hemorrhage in women with abdominal hysterectomy.
Materials and Methods
This study was a randomized double-blind placebo-controlled trial conducted in Aswan university hospital, Egypt, from November 1, 2015, to October 31, 2017. Departmental ethical review board approved the study. Study inclusion criteria were women undergoing total abdominal hysterectomy (TAH) with or without bilateral salpingo-oophorectomy (BSO) due to myoma, menorrhagia, metrorrhagia, chronic pelvic pain, and endometrial hyperplasia. Exclusion criteria were: (1) patients with cardiac, hepatic, renal, or thromboembolic disease; (2) patients with pelvic endometriosis and adnexal mass; (3) patients with endometrial or cervical cancer; (4) patients who had allergy to tranexamic acid.
Eligible Participants
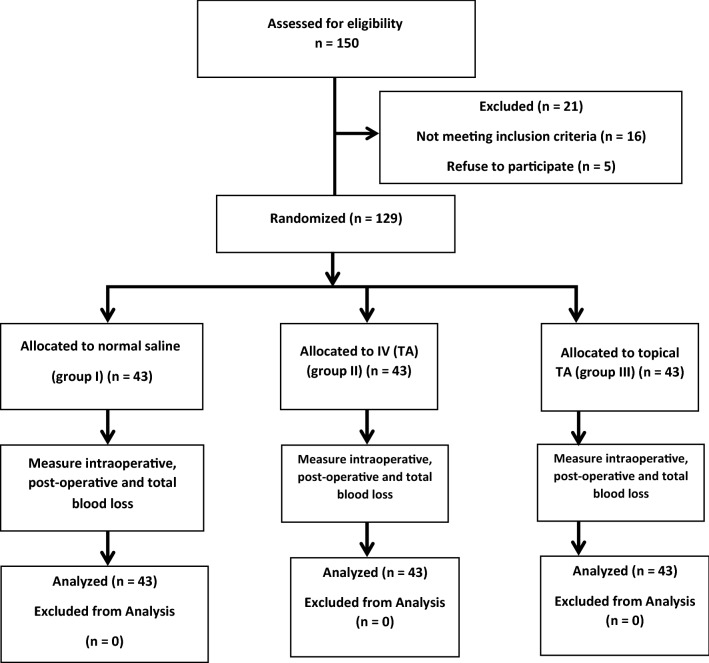
There were 150 patients who were asked to participate, 21 patients were excluded, 16 patients not meeting inclusion criteria, and five patients refuse to participate. Therefore, the remaining 129 patients were included in the study. All participants undergone detailed history, general, abdominal, and vaginal examinations, body mass index (BMI) was calculated, and pelvic ultrasound examination and preoperative hemoglobin were undertaken for all participants (Fig. 1). The participants who fulfilled the eligibility criteria were explained about the study with the beneficial and possible adverse effects of tranexamic acid. Informed consent was obtained from them, after that participants were randomized to three groups: Group I [43 patients received 110 ml normal saline IV just before skin in scion], Group II [43 patients received 1 g tranexamic acid (2 ampoules of kapron 500 mg 5 ml. Amoun company) IV just before skin in scion], and Group III [43 patients received 2 g topical tranexamic acid (4 ampoules of kapron 500 mg 5 ml).
Fig. 1.
Flowchart of the study
Randomization
Patients were randomized to three groups, each comprising of 43 patients according to a three-blocked randomization list which was coded (1 or 2 or 3) at 1:1:1 ratio. The three parallel groups were prepared using a computer-generated randomization system. The allocated groups will be concealed in serially numbered sealed opaque envelopes that will only be opened after recruitment. Patient allocation will be performed prior to the induction of anesthesia by an independent person, who will not otherwise be involved in this study. The trial will be appropriately blinded; the participants, outcome assessors, and the surgeon performing the procedure will be blinded to the medication type, which will be used.
Intervention
In all eligible participants, the hysterectomies were performed by the same operative team. The hemostatic technique during surgery other than TA was done by diathermy coagulation and conventional suture ligature, using vicryl sutures (Vicryl 1–0 polyglactin 910; Egycryl, Taisier CO, Egypt) only.
The abdomen was exposed through Pfannenstiel incision, and after skin incision, the subcutaneous fat and abdominal fascia were opened crosswise, and the rectus muscle was opened on the midline. The parietal peritoneum was opened longitudinally to reach the pelvic cavity. Total hysterectomy with or without bilateral salpingo-oophorectomy was done.
Eligible participants were allocated to one of three groups after induction of spinal anesthesia and immediately prior to the operation and just before skin incision.
Group I patients received 110 ml normal saline (sodium chloride 0.9%.) by slow intravenous injection at an approximate rate of 1 ml per min, and throughout the operation irrigation was done by 60 ml of normal saline, and another 60 ml was left intra-abdominal at the end of the operation. Group II patients received 1-g tranexamic acid (2 ampoules of Capron 500 mg/5 ml; Amoun, Cairo, Egypt) (10 ml) in 100 ml normal saline infusion by slow intravenous injection at an approximate rate of 1 ml per min, and throughout the operation irrigation was done by 60 ml of normal saline, and another 60 ml was left intra-abdominal at the end of the operation. Group III patients received 110 ml normal saline by slow intravenous injection at an approximate rate of 1 ml per min, and throughout the operation irrigation was done by 60 ml of (1 g tranexamic acid (10 ml) diluted in 50 ml of sodium chloride 0.9%). At the end of the operation, another dose of 60 ml of (1 g tranexamic acid (10 ml) diluted in 50 ml of sodium chloride 0.9%) was left intra-abdominal.
An intraperitoneal suction drain was routinely used in all patients. The drains were closed for 3 h postoperative, and after that time the drains were opened and removed on the second postoperative day unless otherwise indicated. To ensure a sufficiently high concentration of topical tranexamic acid, it was diluted only to a volume sufficient to moisten a large wound surface. Twenty milliliters moistens at least 1500 cm2.
Blood Loss Estimation
Intraoperative blood loss was measured by combined methods of estimation of blood loss (both gravimetric and direct methods). Postoperative blood loss was measured through intraperitoneal suction drain which measured every 12 h and on removing the drain. After that, the total blood loss was calculated by the addition of intraoperative and postoperative blood loss.
Study Outcome
The primary outcome was estimation of intraoperative, postoperative, and total blood loss (ml).
The secondary outcome measures included need for blood transfusion, operative time, and period for hospitalization.
Also, hemoglobin concentration was done in all patients 24 h postoperative, and the change in hemoglobin concentration pre- and postoperative were noted. Any side effects such as nausea, vomiting, and diarrhea were recorded.
Statistical Analysis
Data were entered and statistically analyzed using the Statistical Package for Social Sciences (SPSS) version 16. Qualitative data were described as numbers and percentages. Chi-square test and Monte Carlo test were used for comparison between groups, as appropriate. Quantitative data were described as means (SD) or medians, as appropriate. They were tested for normality by Kolmogorov–Smirnov test. In the normally distributed variables, one-way ANOVA with LSD post hoc multiple comparisons test were used for comparison between groups, as appropriate. In the non-normally distributed variables, Mann–Whitney test and Kruskal–Wallis test were used for comparison between groups, as appropriate. Odds ratios and their 95% confidence interval were calculated. “P value ≤ 0.05” was considered to be statistically significant.
Results
Our study started with 150 patients who were asked to participate, 21 patients were excluded, 16 patients did not meet the inclusion criteria, and five patients refused to participate. Therefore, the remaining 129 patients were randomized to three groups, each group comprising of 43 patients. Group I: (received 1 g IV normal saline before skin in scion), Group II: (received 1 g tranexamic acid IV before skin incision), and Group III: (received 2 g topical tranexamic acid).
There was no significant difference between the three groups with respect to their age, weight, Hight, body mass index (BMI), uterine size, indication of hysterectomy, initial hemoglobin and history of previous scar, diabetes mellitus (DM), and hypertension (HTN) (Table 1).
Table 1.
Demographic criteria of the study groups
| Characteristics | Group I (n = 43) | Group II (n = 43) | Group III (n = 43) | Significance |
|---|---|---|---|---|
| Age (years) | 47.3 ± 4.46 | 47.67 ± 4.24 | 47.74 ± 3.98 | 0.873 |
| Weight (kg) | 68.63 ± 6.98 | 68.7 ± 6.2 | 68.77 ± 6.86 | 0.995 |
| Height (cm) | 162.5 ± 4.27 | 163.7 ± 4.44 | 163.7 ± 4.73 | 0.362 |
| BMI | 25.94 ± 2.1 | 25.64 ± 2.17 | 25.6 ± 2.21 | 0.760 |
| Initial hemoglobin | 10.54 ± 0.78 | 10.52 ± 0.71 | 10.52 ± 0.74 | 0.983 |
| DM | 10(23.3) | 9 (20.9) | 11 (25.6) | 0.878 |
| Hypertension | 13(30.2) | 15 (34.9) | 14 (32.6) | 0.900 |
| Uterine size (weeks) | 12.9 ± 3.13 | 12.56 ± 3.002 | 12.88 ± 3.06 | 0.829 |
| Previous scar | 12 (27.9) | 13 (30.2) | 15 (34.9) | 0.776 |
| Indication of hysterectomy | ||||
| Myoma | 13 (30.2%) | 15 (34.9) | 14 (32.6) | 0.991 |
| Chronic pelvic pain | 6 (14.0) | 7 (16.3) | 8 (18.6) | |
| Endometrial hyperplasia | 7 (16.3) | 6 (14.0) | 7 (16.3) | |
| Menorrhagia–metrorrhagia | 17 (39.5%) | 15 (34.9) | 14 (32.6) | |
Variables are presented as mean ± standard deviation and number (percentage)
BMI Body mass index, DM diabetes mellitus, CPP chronic pelvic pain
Statistical significance if P value ≤ 0.05
Both Group II and Group III showed great reduction in intraoperative and postoperative blood loss (blood in the intra-abdominal drain) compared with Group I (P = 0.0001, 0.0001, 0.0001, 0.0001), so the overall estimated blood loss in groups II and III showed highly reduction compared with Group I (P = 0.0001, 0.0001). Also, there was reduction in postoperative bleeding in Group III compared with Group II (P = 0.001). However, no significant difference in intraoperative and overall estimated blood loss between groups II and III (P = 0.631 and 0.804, respectively).
Total blood loss > 500 ml was 69.8% in Group I compared with (14.0%) in Group II and (16.3%) in Group III P = 0.0001 (Table 2).
Table 2.
Primary outcome of the study groups
| Variables | Group I (n = 43) | Group II (n = 43) | Group III (n = 43) | Significance |
|---|---|---|---|---|
| Intraoperative blood loss | 480 (350–700) | 300 (190–620) | 300 (180–650) | 0.0001* 0.0001*/0.0001*/0.631 |
| Postoperative blood loss | 106.16 ± 22.96 | 84.3 ± 16.64 | 70.23 ± 14.39 | 0.0001* 0.0001*/0.0001*/0.001* |
| Total blood loss | 609.19 ± 119.14 | 401.74 ± 121.67 | 395.35 ± 117.61 | 0.0001* 0.0001*/0.0001*/0.804 |
| Total blood loss ≥ 500 ml | 30 (69.8) | 6 (14.0) | 7 (16.3) | 0.0001* 0.0001*/0.0001*/0.763 |
Variables are presented as mean ± standard deviation, median (minimum–maximum) and number (percentage). Statistically significant difference (Group I vs. Group II/Group I vs. Group III/Group II vs. Group III)
*Statistically significant
The mean postoperative hemoglobin concentration was higher in Group II and Group III than in Group I (10.16 ± 0.74 g/dl and 10.17 ± 0.79 vs. 9.71 ± 0.74 g/dl, respectively). P = 0.008 similarly, women in groups II and III had a smaller drop in hemoglobin levels after surgery compared with Group I (0.3 vs. 0.8 g/dl; P = 0.0001).
No significant difference was observed in the requirement for blood transfusions, operation time and duration of hospital stay between the groups (P = 0.499, 0.907, and 0.174, respectively). Also, no significant difference was found between the three groups in relation to the incidence of nausea, vomiting, and diarrhea (P = 0.109, 0.870, and 1.00, respectively) (Table 3).
Table 3.
Secondary outcome of the study groups
| Variables | Group I (n = 43) | Group II (n = 43) | Group III (n = 43) | Significance |
|---|---|---|---|---|
| Postoperative hemoglobin | 9.71 ± 0.74 | 10.16 ± 0.74 | 10.17 ± 0.79 | 0.008* 0.008*/0.007*/0.955 |
| Hemoglobin change | 0.8 (0.5–1.5) | 0.3 (0.2–0.8) | 0.3 (0.2–0.8) | 0.0001* 0.0001*/0.0001*/0.832 |
| Blood transfusion | 4 (9.3) | 1 (2.3) | 2 (4.7) | 0.499 |
| Operative time | 96.84 ± 9.37 | 96.02 ± 10.36 | 96.81 ± 9.34 | 0.907 |
| Hospital stay | 3.7 ± 0.8 | 3.5 ± 0.83 | 3.4 ± 0.85 | 0.174 |
| Nausea | 3 (7.0) | 9 (20.9) | 4 (9.3) | 0.109 |
| Vomiting | 1 (2.3) | 3 (7.0) | 2 (4.7) | 0.870 |
| Diarrhea | 1 (2.3) | 2 (4.7) | 1 (2.3) | 1.00 |
Variables are presented as mean ± standard deviation, median (minimum–maximum) and number (percentage). Statistically significant difference (Group I vs. Group II/Group I vs. Group III/Group II vs. Group III)
*Statistically significant
Discussion
Damage of the endothelial surface during surgery activates the hemostatic system, leading to elevated levels of plasminogen activator. This leads to fibrinolysis, causing destabilization of the fibrin network in blood clots. Elevated levels of plasminogen activator can maintain and prolong bleeding during surgery [10]. This is of interest in gynecologic surgery because the level of fibrinolysis seems to be naturally high in the myometrium, the endometrium, and the cervical glands of the uterus. Furthermore, women with menorrhagia have even higher levels of plasminogen activator and plasmin [10]. Because menorrhagia is one of the most common indications for hysterectomy, these women could have an increased risk of bleeding complications when undergoing uterine surgery. To the best of our knowledge, this research was the first to examine the effect of intravenous versus topical tranexamic acid in reducing blood loss during abdominal benign hysterectomy. Our results indicate that preemptive treatment with TA reduces the overall total blood loss, the incidence of blood loss ≥ 500 ml, postoperative hemorrhage. No incidence of thromboembolic events or death was observed in any of the groups. Furthermore, there was a significant decrease in postoperative hemoglobin in the placebo group.
Regarding benign elective hysterectomy, very few studies were found in the literature for the role of IV TA, and no studies concerning topical TA application to reduce intraoperative blood loss were identified.
Topsoee et al. [6] conducted a randomized controlled trial from April 2013 to October 2014. A total of 332 women undergoing benign abdominal, laparoscopic, or vaginal hysterectomy were included in the trial, randomized to either 1 g of intravenous tranexamic acid or placebo at the start of surgery. Total blood loss was reduced in the group treated with tranexamic acid compared to the placebo group when estimated both subjectively by the surgeon and objectively by weight (98.4 vs. 134.8 ml, P = .006 and 100.0 vs. 166.0 ml, P = .004). The incidence of blood loss ≥ 500 ml was also significantly reduced (6 vs. 21, P = .003), as well as the use of open-label tranexamic acid (7 vs. 18, P = .024). No incidence of thromboembolic events or death was observed in any of the groups.
Essola et al. conducted a prospective, non-randomized study done over 8 months (from January 2013 to August 2013). Patients undergoing a hysterectomy or myomectomy who had a hemoglobin level greater than or equal to 8 g/dl and less than 12 g/dl were included. The estimated blood loss was significantly less (P = 0.0002) in TA group (213.7 ± 131.7 ml) than in non-TA group B (571.6 ± 237.1 ml) [11].
In our study, total blood loss > 500 ml was 69.8% in Group I compared with (14.0%) in Group II and (16.3%) in Group III P = 0.0001.
In our study the irrigation of 60 ml of (1 g tranexamic acid (10 ml) diluted in 50 ml of sodium chloride 0.9%) and another 1 g diluted in 50 ml of sodium chloride 0.9% at the end of the operation reduced intra- and postoperative blood loss, as well as the amount of total blood loss. Hemoglobin level showed a significant decrease in the in the Group I.
Apart from two case reports demonstrating the use of topical tranexamic acid to control bleeding in patients with clotting disorders, there is no study available in the literature addressing the role of topical tranexamic acid during hysterectomy. It is believed that this study may be the first of its kind [12].
One concern regarding the use of TA is the potential for thromboembolic events in a population at already high baseline risk of thrombosis [10]. There were no cases of DVT or pulmonary embolism in our study. However, no long-term follow-up has been maintained.
The WOMAN trial results showed that the effect of TA in postpartum hemorrhage is consistent with the effect recorded in surgery and trauma. There was a significant reduction in death due to bleeding and laparotomy to control postpartum hemorrhage with tranexamic acid and no evidence of increased risk of thromboembolic disease [10].
One limitation of our study was we did not use alkaline hematin method which is a validated method for accurate measurement of blood loss, but we used instead a gravimetric method to measure the amount of blood loss [13]. However, Withanathantrige et al. [13] compared gravimetric and colorimetric methods to quantify surgical blood loss and conclude that estimation of blood loss using a gravimetric method is an accurate and objective tool to evaluate intraoperative blood loss.
The strength of the study lies in its simplicity that a simple easily do-able intervention can result in a clinically significant reduction in intraoperative blood loss.
Conclusion
The results support the hypothesis that intravenous and topical TA application is a safe and reliable method to help decrease blood loss during and after the abdominal hysterectomy. This study indicates the use of topical TA in patients undergone abdominal hysterectomy is associated with decreased blood loss as intravenous TA.
Hany F. Sallam
is a doctor who graduated in 1998 from Mansoura University, Egypt. His experience in obstetrics and gynecology started since 2000 as a Resident Doctor (Registrar) in Mansoura University Hospitals. He obtained MD degree in obstetrics and gynecology in 2010 and has since been Lecturer of Obstetrics and Gynecology, Faculty of Medicine, Aswan University, Egypt. As a part of his job in the university, he teaches for both undergraduates and postgraduates. He is sharing in many researches in the fields of gynecologic oncology, reproductive endocrinology, and maternal–fetal medicine.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
Approval from Ob/Gyn Department at Aswan university hospital was obtained (2-10-2015).
Informed Consent
An informed verbal and written consent of the study subjects to participate in the study was obtained with assurance of confidentiality and anonymity of the data. Subjects participated voluntarily with full right to with draw from the study.
Footnotes
Hany F. Sallam is Lecturer of Obstetrics and Gynecology, Faculty of Medicine, Aswan University, Egypt; Nahla W. Shady is an Associated Professor of Obstetrics and Gynecology, Faculty of Medicine, Aswan University, Egypt.
References
- 1.Clarke-Pearson DL, Geller EJ. Complications of hysterectomy. Obstet Gynecol. 2013;121:654–673. doi: 10.1097/AOG.0b013e3182841594. [DOI] [PubMed] [Google Scholar]
- 2.Parker WH, Wagner WH. Gynecologic surgery and the management of hemorrhage. Obstet Gynecol Clin North Am. 2010;37:427–436. doi: 10.1016/j.ogc.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Hansen CT, Moller C, Daugbjerg S, et al. Establishment of a national Danish hysterectomy database: preliminary report on the first 13,425 hysterectomies. Acta Obstet Gynecol Scand. 2008;87:546–557. doi: 10.1080/00016340802011579. [DOI] [PubMed] [Google Scholar]
- 4.Osler M, Daugbjerg S, Frederiksen BL, et al. Body mass and risk of complications after hysterectomy on benign indications. Hum Reprod. 2011;26:1512–1518. doi: 10.1093/humrep/der060. [DOI] [PubMed] [Google Scholar]
- 5.Biswas J, Chaudhuri P, Mandal A, et al. Effect of a single preoperative dose of sublingual misoprostol on intraoperative blood loss during total abdominal hysterectomy. Int J Gynaecol Obstet. 2013;122:244–247. doi: 10.1016/j.ijgo.2013.03.025. [DOI] [PubMed] [Google Scholar]
- 6.Topsoee MF, Bergholt T, Ravn P, et al. Anti-hemorrhagic effect of prophylactic tranexamic acid in benign hysterectomy-a double-blinded randomized placebo-controlled trial. Am J Obstet Gynecol. 2016;215(1):72-e1. doi: 10.1016/j.ajog.2016.01.184. [DOI] [PubMed] [Google Scholar]
- 7.Ker K, Edwards P, Perel P, et al. Effect of tranexamic acid on surgical bleeding: systematic review and cumulative meta-analysis. BMJ. 2012;344:e3054. doi: 10.1136/bmj.e3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henry DA, Carless PA, Moxey AJ. Anti-fibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev. 2011;1:CD001886. doi: 10.1002/14651858.CD001886. [DOI] [PubMed] [Google Scholar]
- 9.Ipema HJ, Tanzi MG. Use of topical tranexamic acid or aminocaproic acid to prevent bleeding after major surgical procedures. Ann Pharmacother. 2012;46:97–107. doi: 10.1345/aph.1Q383. [DOI] [PubMed] [Google Scholar]
- 10.Roberts I, Fawole B, Chaudhri R, et al. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial WOMAN Trial Collaborators. The Lancet. 2017;389(10084):2105–2116. doi: 10.1016/S0140-6736(17)30638-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Essola L, Kouégnigan Rérambiah L, Obame R, et al. Can venous iron and tranexamic acid reduce the transfusion need? Report on a non-randomized, case control study. Transfus Clin Biol. 2017;24(2):52–55. doi: 10.1016/j.tracli.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Sarris I, Arafa A, Konaris L, et al. Topical use of tranexamic acid to control perioperative local bleeding in gynaecology patients with clotting disorders: two cases. Haemophilia. 2007;13:115–116. doi: 10.1111/j.1365-2516.2006.01386.x. [DOI] [PubMed] [Google Scholar]
- 13.Withanathantrige M, Goonewardene M, et al. Comparison of four methods of blood loss estimation after cesarean delivery. Int J Gynecol Obstet. 2016;135:51–55. doi: 10.1016/j.ijgo.2016.03.036. [DOI] [PubMed] [Google Scholar]