Abstract
The tibial nerve intraneural ganglion cyst—which presents with fluid accumulated inside the nerve epineurium—is a rare etiology of tarsal tunnel syndrome. We report a case with insidious onset of numbness over his left medial ankle. Ultrasound imaging revealed that the tibial nerve was encircled by crescent-shaped anechoic substances, spanning from the distal leg to the sole. Magnetic resonance imaging disclosed a thickened tibial nerve wrapped by hyperintense materials in the tarsal tunnel. Some effusion was observed besides the tibialis posterior and flexor digitorum tendons as well. The patient underwent a surgical treatment and an intraneural ganglion cyst was confirmed. This report elaborated the clinical and imaging presentations of a tibial nerve intraneural ganglion cyst and highlighted the usefulness of ultrasound in exploring the cause of compressive neuropathy at the ankle region.
Keywords: Tibial nerve, Ultrasound, Ganglion, Tarsal tunnel
Sommario
La cisti del ganglio intraneurale del nervo tibiale—che si presenta con presenza di liquido all’interno del nervo epineurico—è una rara causa di sindrome del tunnel tarsale. Segnaliamo un caso con insidiosa insorgenza di intorpidimento a livello della caviglia mediale sinistra. L’ecografia ha rivelato che il nervo tibiale era circondato da sostanze anecoiche a forma di mezzaluna, che si estendevano dalla gamba distalmente fino in zona plantare. La risonanza magnetica ha rivelato un nervo tibiale ispessito ed avvolto da materiali iperintensi nel tunnel tarsale. È stato osservato un certo versamento perifericamente ai tendini del tibiale posteriore e del flessore delle dita. La paziente è stata sottoposta a un trattamento chirurgico ed è stata confermata una cisti gangliare intraneurale. Questo caso clinico ha valutato le presentazioni cliniche e di imaging di una cisti del ganglio intraneurale del nervo tibiale e ha evidenziato l’utilità degli ultrasuoni nella valutazione della causa della neuropatia compressiva nella regione della caviglia.
Introduction
Ankle pain has become prevalent due to an increased population of sport participation and it mostly occurs at the lateral ligamentous complex following inversion injuries. Medial ankle pain is much less prevalent and may be associated with neurological complaints, termed as tarsal tunnel syndrome (TTS). The syndrome is induced by compression of the tibial nerve as it travels through the tarsal tunnel. Its causes are miscellaneous, such as hypertrophic flexor retinaculum, tendinopathy, neuroma, hematoma, osteophytes and ganglions [1]. The symptoms may be misrecognized as lumbar radiculopathy pertaining to L4, L5 or S1 nerve roots [2]. Differential diagnosis relies on electrophysiological [3] and imaging studies like magnetic resonance imaging [4] and high-frequency ultrasound (US) [5]. The latter has emerged as a useful tool for its excellence in identifying peripheral nerve lesions [6]. Herein, we report a case with TTS whereby US imaging was used to identify the rare underlying etiology, i.e., tibial nerve intraneural ganglion cyst.
Case report
A 49-year-old healthy male, without any traumatic history, visited our clinic because of gradual onset of numbness over the medial ankle and plantar area for some weeks. The numbness was accentuated by vigorous activity like playing basketball. Neither radicular pain nor lower limb weakness was present. He had received treatments like nonsteroidal anti-inflammatory drugs and physical modalities which could have not relieved his symptoms.
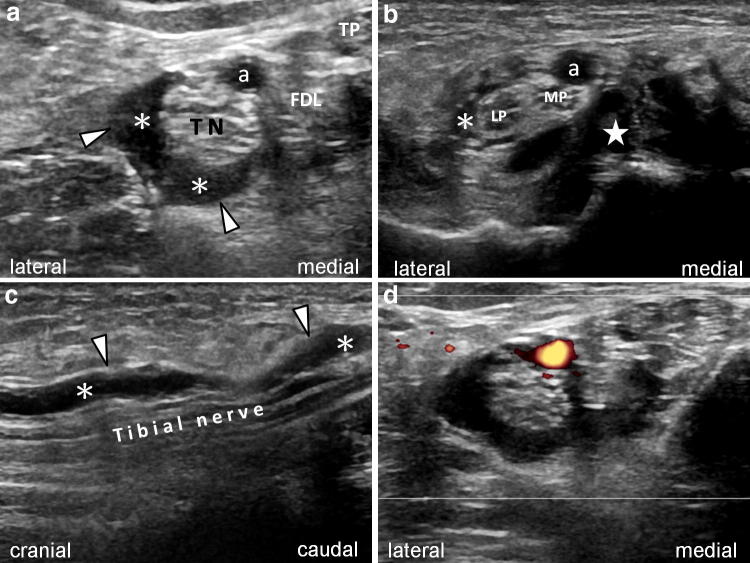
Physical examination did not show any pes cavus/planus, intrinsic muscle atrophy, sensory loss at the medial ankle or gait disturbance. A positive Tinel sign was detected on the tarsal tunnel. Ankle US examination was performed by an 18 MHz linear transducer (Ascendus, Hitachi, Ltd., Tokyo, Japan) according to EURO-MUSCULUS/USPRM scanning protocol for the ankle and foot [7]. When placing the transducer over the inlet of the tarsal tunnel, some anechoic lesions with posterior enhancement around the tibial nerve were noticed. In the short axis, the fluid was confined in a crescent-shape area within a hyperechoic capsule, likely to be the perineurium of the tibial nerve (Fig. 1a). The lesion extended from the distal leg to bifurcation of the medial and lateral plantar nerves and was mildly compressible without direct connection with the subtalar joint (Fig. 1b, c). No hypervascularity was noted around the lesion on the power Doppler imaging (Fig. 1d). A positive sono-tinel sign was noted, indicating possible tibial nerve entrapment. Dynamic imaging showed no tendon subluxation or ligament laxity.
Fig. 1.
a Ultrasound imaging at the tarsal tunnel (axial, proximal) shows anechoic fluid (asterisks) surrounding the tibial nerve (TN) within its epineurium (arrowheads). FDL flexor digitorum longus tendon, TP tibialis posterior tendon, a posterior tibial artery. b. Ultrasound imaging at the tarsal tunnel (axial, distal) shows the fluid (asterisk) next to the lateral plantar nerve (LP). Star indicates the subtalar fluid. MP medial plantar nerve, a posterior tibial artery. c Ultrasound imaging at the tarsal tunnel (longitudinal) shows the anechoic fluid (asterisks) around the tibial nerve within its epineurium (arrowheads). d Power Doppler imaging shows no signals other than the posterior tibial artery
Magnetic resonance imaging (MRI) with contrast medium was arranged. Thickening of the tibial nerve in the tarsal tunnel was noted. The tibialis posterior and flexor hallucis longus tendons revealed moderate peritendinous effusion, indicating tenosynovitis. The hyperintense lesions extended from the distal leg to bifurcation of the medial and lateral plantar nerves at T2-weighted imaging (Fig. 2a). The tibial nerve was swollen with loss of fascicular architecture and displaying a ‘sausage appearance’, i.e., with a clear entrapped site (Fig. 2a). Some hyperintense substances filled the space inside the epineurium (Fig. 2b), but the nervous fascicles were not separated from the lesion. He underwent a surgery (tibial nerve neurolysis and ablation of the ganglion cyst) during which multiple lobulated ganglion cysts infiltrating the tibial nerve were confirmed. After the surgery, the pain and numbness fully subsided without recurrence.
Fig. 2.
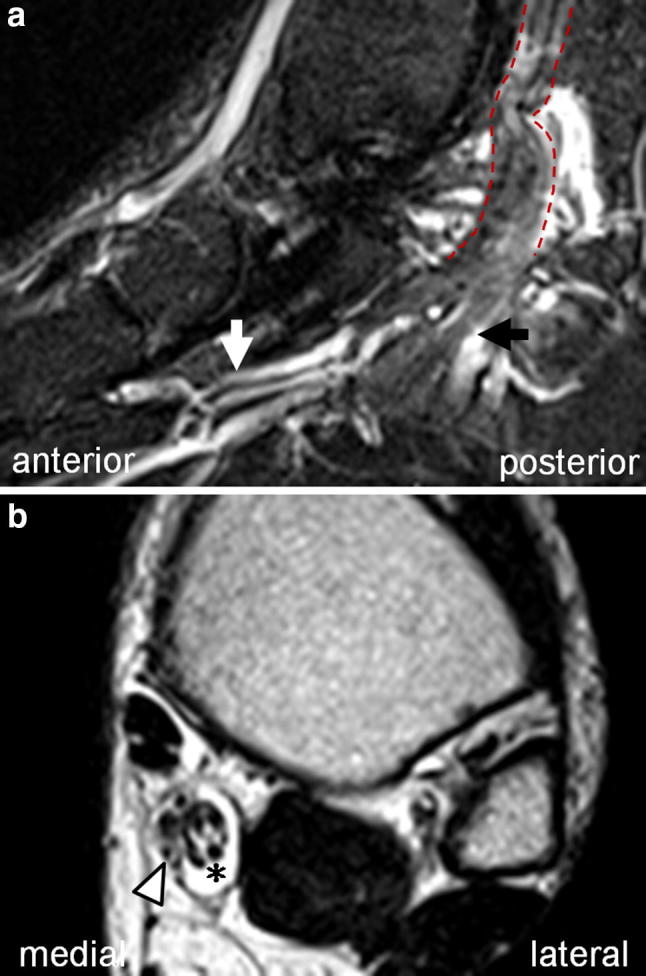
Magnetic resonance imaging of at tarsal tunnel level. a Saggital view shows thickening of the tibial nerve (red dashed line). Black arrow shows the medial plantar nerve and white arrow shows the lateral plantar nerve. b Coronal view shows the swollen nerve (arrowhead) with fluid (asterisk) around it
Discussion
The tibial nerve arises from the sciatic nerve and travels through the popliteal fossa to the posterior side of medial malleolus. Before entering the tarsal tunnel, it gives off the medial calcaneal branch and then divides into the medial and lateral plantar nerves [5]. TTS refers to entrapment of the tibial nerve or its terminal branches when passing underneath the flexor retinaculum. The patients usually present with pain, paresthesia, weakness, and atrophy of the innervated area [8, 9].
The etiology can be traumatic reasons like tibial bone fracture, severe ankle sprain [10], hematoma, or iatrogenic damage to the nerves [11]. Also the tibial neuroma, tenosynovitis of surrounding tendons and other space occupying lesions (ganglion cysts being the most frequent causes) [12] will induce the syndrome. Extraneural ganglions originating from the nearby tendons are common; however, intraneural ones are rare and are seen as tibial nerve schwannomas, i.e., a hypoechoic mass located eccentrically besides the nerve [13]. The pathology comprises thick mucinous fluid collected inside the fibrous capsule of the nerve epineurium [14]. The cysts mostly affect the tibial nerve [15] and are more common among men in the third and fourth decades of life [16]. It usually results from perineural connective tissue degeneration due to chronic irritation or repeated injury [17]. A less frequent cause is expansion of the synovial joint fluid along the articular nerve branches [18–20].
With advance in US techniques and scanning skills, the validation of etiology in TTS is easier. The sonographic hallmark for an intraneural cyst is fluid accumulation between the epineurium and fascicles without blood flow signals, namely the crescent sign [21]. The tibial nerve may become swollen proximal to the entrapment site and is usually normal in size distal to the site of compression. US-guided cyst aspiration can be used initially for symptom relief. Because the synovial joint fluid may expand along the articular branches of the tibial nerve which are very difficult to find through US examination [22]. Of note, the fluid may reaccumulate and a surgery for removing the ganglion and tibial nerve articular branch might be necessary [14, 19, 23].
In our case, the suspicion of an intraneural ganglion cyst was first confirmed through the US imaging. The following MRI scrutinized whether the lesion extended underneath the bone [24]. After the surgery, US imaging would again be suitable for close/convenient follow-up for recurrence and MRI might be needed if the involvement of the tibial nerve’s articular branch is suspected.
Conclusion
As in other regions, high-resolution US appears as a reliable imaging modality to conveniently explore the presence (and the relevant etiologies) of nerve entrapment syndromes at the ankle and foot. Although the intraneural ganglion cyst is an uncommon cause of TTS, the symptoms can be successfully relieved through the early diagnosis and accurate treatment.
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from the patient for being included in the study.
References
- 1.Ahmad M, Tsang K, Mackenney PJ, Adedapo AO. Tarsal tunnel syndrome: a literature review. Foot Ankle Surg. 2012;18(3):149–152. doi: 10.1016/j.fas.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Zheng C, Zhu Y, Jiang J, et al. The prevalence of tarsal tunnel syndrome in patients with lumbosacral radiculopathy. Eur Spine J. 2016;25(3):895–905. doi: 10.1007/s00586-015-4246-x. [DOI] [PubMed] [Google Scholar]
- 3.Alan U, Sendromu H. Tarsal tunnel syndrome in a patient on long-term peritoneal dialysis: case report. Turk Neurosurg. 2007;17(4):283–285. [PubMed] [Google Scholar]
- 4.Moholkar S, Sawhney JS, Bhatt R. Imaging benign soft tissue lesions of the foot. Appl Radiol. 2009;38(10):10. [Google Scholar]
- 5.Hung CY, Hsiao MY, Ozcakar L, et al. Sonographic tracking of the lower limb peripheral nerves: a pictorial essay and video demonstration. Am J Phys Med Rehabil. 2016;95(9):698–708. doi: 10.1097/PHM.0000000000000463. [DOI] [PubMed] [Google Scholar]
- 6.Kara M, Özçakar L, De Muynck M, Tok F, Vanderstraeten G. Musculoskeletal ultrasound for peripheral nerve lesions. Eur J Phys Rehabil Med. 2012;48(4):665–674. [PubMed] [Google Scholar]
- 7.Özçakar L, Kara M, Chang K, et al. EURO-MUSCULUS/USPRM basic scanning protocols for ankle and foot. Eur J Phys Rehabil Med. 2015;51(5):647–653. [PubMed] [Google Scholar]
- 8.Patel P, Schucany WG (2012) A rare case of intraneural ganglion cyst involving the tibial nerve. In: Baylor University Medical Center Proceedings 2012 Apr 1, vol 25, No. 2, p 132 [DOI] [PMC free article] [PubMed]
- 9.Chalian M, Soldatos T, Faridian-Aragh N, et al. 3T magnetic resonance neurography of tibial nerve pathologies. J Neuroimaging. 2013;23(2):296–310. doi: 10.1111/j.1552-6569.2011.00676.x. [DOI] [PubMed] [Google Scholar]
- 10.Kim DH, Cho Y-J, Ryu S, Tiel RL, Kline DG. Surgical management and results of 135 tibial nerve lesions at the Louisiana State University Health Sciences Center. Neurosurgery. 2003;53(5):1114–1125. doi: 10.1227/01.NEU.0000089059.01853.47. [DOI] [PubMed] [Google Scholar]
- 11.Fantino O. Role of ultrasound in posteromedial tarsal tunnel syndrome: 81 cases. J Ultrasound. 2014;17(2):99–112. doi: 10.1007/s40477-014-0082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takakura Y, Kitada C, Sugimoto K, Tanaka Y, Tamai S. Tarsal tunnel syndrome. Causes and results of operative treatment. Bone Joint J. 1991;73(1):125–128. doi: 10.1302/0301-620X.73B1.1991745. [DOI] [PubMed] [Google Scholar]
- 13.Judd T, Jones T, Thornberry L. Schwannoma of the posterior tibial nerve: case study. J Am Podiatr Med Assoc. 2014;104(5):539–543. doi: 10.7547/0003-0538-104.5.539. [DOI] [PubMed] [Google Scholar]
- 14.Silveira CRS, Vieira CGM, Pereira BM, Pinto Neto LH, Chhabra A. Cystic degeneration of the tibial nerve: magnetic resonance neurography and sonography appearances of an intraneural ganglion cyst. Skelet Radiol. 2017;46(12):1763–1767. doi: 10.1007/s00256-017-2753-z. [DOI] [PubMed] [Google Scholar]
- 15.Desy NM, Wang H, Elshiekh MAI, et al. Intraneural ganglion cysts: a systematic review and reinterpretation of the world’s literature. J Neurosurg. 2016;125(3):615–630. doi: 10.3171/2015.9.JNS141368. [DOI] [PubMed] [Google Scholar]
- 16.Spinner RJ, Mokhtarzadeh A, Schiefer TK, Krishnan KG, Kliot M, Amrami KK. The clinico-anatomic explanation for tibial intraneural ganglion cysts arising from the superior tibiofibular joint. Skelet Radiol. 2007;36(4):281–292. doi: 10.1007/s00256-006-0213-2. [DOI] [PubMed] [Google Scholar]
- 17.Kannus P, Jozsa L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. JBJS. 1991;73(10):1507–1525. doi: 10.2106/00004623-199173100-00009. [DOI] [PubMed] [Google Scholar]
- 18.Spinner RJ, Hébert-Blouin M-N, Maniker AH, Amrami KK. Clock face model applied to tibial intraneural ganglia in the popliteal fossa. Skelet Radiol. 2009;38(7):691–696. doi: 10.1007/s00256-009-0651-8. [DOI] [PubMed] [Google Scholar]
- 19.Spinner RJ, Atkinson JL, Tiel RL. Peroneal intraneural ganglia: the importance of the articular branch. A unifying theory. J Neurosurg. 2003;99(2):330–343. doi: 10.3171/jns.2003.99.2.0330. [DOI] [PubMed] [Google Scholar]
- 20.Spinner RJ, Amrami KK, Wolanskyj AP, et al. Dynamic phases of peroneal and tibial intraneural ganglia formation: a new dimension added to the unifying articular theory. J Neurosurg. 2007;107:296–307. doi: 10.3171/JNS-07/08/0296. [DOI] [PubMed] [Google Scholar]
- 21.Spinner RJ, Luthra G, Desy NM, Anderson ML, Amrami KK. The clock face guide to peroneal intraneural ganglia: critical “times” and sites for accurate diagnosis. Skelet Radiol. 2008;37(12):1091–1099. doi: 10.1007/s00256-008-0545-1. [DOI] [PubMed] [Google Scholar]
- 22.Jacobson JA, Wilson TJ, Yang LJS. Sonography of common peripheral nerve disorders with clinical correlation. J Ultrasound Med. 2016;35(4):683–693. doi: 10.7863/ultra.15.05061. [DOI] [PubMed] [Google Scholar]
- 23.Spinner RJ, Dellon AL, Rosson GD, Anderson SR, Amrami KK. Tibial intraneural ganglia in the tarsal tunnel: is there a joint connection? J Foot Ankle Surg. 2007;46(1):27–31. doi: 10.1053/j.jfas.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 24.Chung W, Chung H, Shin M, et al. MRI to differentiate benign from malignant soft-tissue tumours of the extremities: a simplified systematic imaging approach using depth, size and heterogeneity of signal intensity. Br J Radiol. 1018;2012(85):e831–e836. doi: 10.1259/bjr/27487871. [DOI] [PMC free article] [PubMed] [Google Scholar]