Abstract
Purpose
To characterize preschool and school services for children who are hard of hearing (CHH), we described service setting, amount, and configuration and analyzed the relationship between service receipt and student hearing levels and language scores. Characteristics of professionals providing services were described and then used to predict level of comfort with skills supporting listening and spoken language. The amount of provider communication with children's audiologists was also investigated.
Method
Participants included parents of CHH (preschool n = 174; school n = 155) and professionals (preschool n = 133; school n = 104) who completed interviews and questionnaires as part of a longitudinal study. Children's hearing, speech, and language data were collected from annual testing and analyzed in relation to service data.
Results
A majority (81%) of preschool-age CHH received services. Children were more likely to be in a preschool for children who are deaf or hard of hearing (CDHH) or exceptional children than a general education preschool. By elementary school, 70% received services, nearly all in general education settings. Sessions averaged twice a week for a total of approximately 90 min. Children who no longer received services performed significantly better on speech/language measures than those who received services, regardless of service setting. Professionals were primarily speech-language pathologists (SLPs) and teachers of CDHH. SLPs reported significantly less comfort with skills involving auditory development and hearing technologies and less frequent communication with the child's audiologists than teachers of CDHH. Overall communication with audiologists was more frequent in the preschool years.
Conclusions
As preschool-age CHH transition into school, the majority continue to qualify for services. Congruent with national trends, school-age CHH in the Outcomes of Children with Hearing Loss study were most often in general education settings. Without specialized preprofessional or postgraduate training, SLPs and teachers of CDHH did not report comfort with all the skills critical to developing listening and spoken language. This finding supports the need for increased implementation of interprofessional practice among SLPs and teachers of CDHH, as well as audiologists, to best meet the needs unique to this population.
With the implementation of newborn hearing screening, a confluence of factors changed the landscape for children who are hard of hearing (CHH) and their families. These factors included earlier diagnosis and fitting of hearing aids, improving access to the auditory signal, and earlier intervention services for families of infants. The degree to which these factors have altered the longer term intervention needs of this group of children is unclear. There is documentation that the intervention/resource needs of CHH are often underestimated in school settings (Antia, Jones, Reed, & Kreimeyer, 2009; Davis, Elfenbein, Schum, & Bentler, 1986). CHH may display language/communication deficits that are subtle, and related service needs may go unrecognized. Some states require that children demonstrate significant delays on norm-referenced measures (i.e., −1.5 SDs) in order to qualify for services, which may restrict service access. Recent data from the Outcomes of Children with Hearing Loss (OCHL) study showed that a large group of preschoolers who are hard of hearing performed within the average range on norm-referenced language measures but were nearly a full standard deviation behind children with normal hearing matched on age and socioeconomic status (Tomblin, Harrison, et al., 2015). The OCHL research team has argued that the needs of CHH will continue to be underestimated unless their performance is considered relative to the characteristics of classmates with whom they are typically compared (Moeller, Tomblin, & OCHL Collaboration, 2015). Furthermore, considerable variation in the outcomes of this group on norm-referenced measures suggests that a subgroup of CHH is especially at risk for significant language and literacy delays (Ambrose, Walker, Unflat-Berry, Oleson, & Moeller, 2015; Tomblin, Harrison, et al., 2015). Although recent findings have advanced our understanding of the needs of CHH, little is known about their current service access or the characteristics of services beyond early intervention. Describing the services that CHH currently receive is a critical first step in determining if their needs are recognized and met in this contemporary era. The primary purpose of this article is to describe the services that preschool- and school-age CHH receive and the professionals that provide those services. Further analyses are conducted to examine differences in service receipt and in professional practice.
Trends in Service Provision
Beginning with the Education for All Handicapped Children Act (1975) and subsequent legislation, there has been a steady increase in the flow of students away from separate educational programs to inclusive educational settings. The latest report of the annual survey conducted by the Research Support and International Affairs (2014) described educational placements for 23,731 students up to 21 years of age. Respondents were allowed to select more than one setting per student. Fifty-one percent were placed in general education classrooms with hearing students, 30% were educated in special schools, and 24% received instruction in self-contained classrooms within general education settings. The Gallaudet Research Institute study included children with severe and profound levels of hearing, as well as children with additional disabilities, whose language and educational needs typically differ from the CHH with mild to moderately severe hearing levels who were enrolled in the OCHL research study.
Blackorby and Knokey (2006) studied the educational placements of CHH and reported that almost 70% of children with mild to moderately severe hearing levels were placed in general education classrooms (including resource support) rather than a self-contained classroom or a school for children who are deaf or hard of hearing (CDHH). Placement of the 30% of CHH in specialized settings or self-contained classrooms may be due to increased intervention needs for CHH who exhibit significant delays or have additional disabilities or because of specific communication requirements. Children who have age-appropriate language abilities may be more likely to receive services in general education settings rather than a school for CDHH.
Very few studies have attempted to quantify educational intervention or link intervention to child characteristics. The National Early Intervention Longitudinal Study (SRI International, 2000) investigated early intervention for children with a wide range of disabilities in a variety of settings. One portion of that large study investigated the relationship between the level of spending on services and the outcomes of the children receiving those services when they exited early intervention at 36 months of age (Hebbler, Levin, Perez, Lam, & Chambers, 2009). The authors found that the higher the expenditure for services, the poorer child outcomes were. They explained that this finding reflected the fact that the initial assessment of severity of the child's condition dictated the level of services allocated. Thus, children with more significant challenges cost more to serve but achieved less optimal outcomes than those with less severe diagnoses. This finding was echoed in a study by Sininger, Grimes, and Christensen (2010) that investigated the factors influencing auditory-based communication outcomes in CDHH. They reported that more services were provided to children most in need of them, and yet these children often had poorer outcomes. The authors concluded that the relationship between intervention and outcomes is complex and challenging to characterize.
Professionals Providing Services
As services shift from family centered to child centered at 36 months of age, it is important for CHH to have access to providers with knowledge and skills related to serving them. Those professionals need additional expertise specifically related to managing amplification and communication in complex listening environments, such as classrooms, in order to provide an auditory environment optimal for learning. In general education settings, speech-language pathologists (SLP) and teachers of CDHH are likely to provide services to CHH. The preprofessional education of SLPs prepares them to diagnose and provide intervention for a wide range of communication disorders across the life span; however, the certification requirement for knowledge and skills in the area of hearing loss (HL) can be met by only a few hours of supervised hearing screening and as little as one academic course. In contrast, the preprofessional education of teachers of CDHH is focused upon understanding and ameliorating the effects of HL on cognition, communication, and psychosocial development. As a result of differences in preparation, professionals may bring distinct skill sets in regard to service delivery for preschool- and school-age CHH. It is not clear which providers are serving CHH at the preschool- and school-age level and whether both specialists and generalist providers are involved. Given that the needs of CHH have been underestimated in the past, it is important to determine the degree to which preschool- and school-age children are accessing providers with specialized knowledge and confidence in their skills.
Previous survey research revealed that SLPs perceived themselves to be well prepared in normal speech and language processes but needed more preparation in evaluation of speech and language skills of children with HL (Moseley, Mashie, Brandt, & Fleming, 1994). In addition, they did not feel prepared to manage hearing devices in either general education classrooms or school settings designed for students with HL (Compton, Tucker, & Flynn, 2009; Richburg & Knickelbein, 2011). Houston and Perigoe (2010) emphasized that, in order to be effective, intervention providers must be knowledgeable about advanced hearing technology (e.g., digital hearing aids, cochlear implants, and FM/DM systems) and the potential impact such technologies have on developing appropriate language abilities. Collaboration with audiologists could help SLPs become more knowledgeable about hearing technologies. In addition, this interprofessional partnership could support a better understanding of the child's audiogram, the benefit provided by hearing technologies, and the influence of the auditory environment on listening and learning. However, communicating with the child's audiologist might be difficult due to limited access to educational audiologists in the school district or overall geographic area, large caseload sizes for the SLPs and the audiologists, or other demands limiting time for contact. Furthermore, providers may not know when it is appropriate to contact the audiologist (Compton et al., 2009). Identifying interdisciplinary communication patterns is a first step toward overcoming obstacles to creating and maintaining relationships between providers.
Research Questions
This study aims to provide a description of service delivery to CHH and to explore characteristics of professionals that may affect speech-language and educational services in the preschool- and school-age years. The following research questions are addressed:
What are the service characteristics (setting, amount, and configuration) for CHH at preschool and elementary school ages?
What is the relationship between receipt of services, service setting, and students' hearing levels and language scores?
What is the professional preparation and experience of individuals providing services to CHH?
Do differences in professional preparation and experience predict level of comfort regarding working with CHH?
What are the characteristics of providers who regularly collaborate with audiologists?
Method
The primary goal of the OCHL study was to identify factors that affect the outcomes of infants and preschool- and school-age children who have permanent, bilateral, mild-to-severe hearing levels. Children with a confirmed sensorineural, mixed, or permanent conductive bilateral HL with pure-tone average hearing levels between 25 and 75 dB were included in the study. All had at least one parent or primary caregiver who spoke English in the home. Children with major developmental disabilities in addition to HL were not included. These inclusion criteria allowed the research team to control for the effects that the presence of developmental disabilities or language differences might exert on outcomes. Families were recruited by three study sites, the University of Iowa, Boys Town National Research Hospital in Nebraska, and the University of North Carolina–Chapel Hill. Approval was obtained from the institutional review board at each research center. A full description of the study methodology can be found in Tomblin, Walker, et al. (2015). This study investigates aspects of service provision for preschool- and school-age children enrolled in the OCHL study.
Participants
Participants resided in 16 states and included (a) preschool- and school-age children and their parents and (b) the professionals providing speech-language and educational services to the children. The preschool children (n = 174) ranged from 41 to 72 months of age (M = 50.5, SD = 7.9). Those in elementary school (n = 155) were between 66 and 114 months (M = 81.2, SD = 13.8 months). School placements ranged from the first year of preschool through fourth grade of elementary school. During the course of this longitudinal study, 78 children advanced from preschool to school placements; thus, the total number of unique children is 251. Because data for the two age groups are analyzed independently, these children are represented in both groups.
A majority of the children had better ear pure-tone averages (BEPTA) between 45 and 65 dB HL with a mean of 48.4 dB HL (SD = 14.8). In 25 instances (10%), children's BEPTA fell outside the criterion range (25 to 75 dB HL). Of these 25 children, 15 had BEPTA below 25 dB HL, and 10 were above 75 dB HL. These cases were discussed by the research team and were included either because of prior clinical assessments with thresholds in the qualifying range or because of audiologic or medical circumstances (e.g., HL in low or high frequencies only or mixed HL with fluctuation due to otitis media with effusion).
At the initial research study visit, parents reported results of the newborn hearing screen and ages at which children were first identified with HL, had it confirmed, and were fitted with hearing aids. Seventy-one percent of children in the current study were early identified through newborn hearing screening, with a mean BEPTA of 50.3 dB HL (SD = 13.6, Mdn = 50.0). Twenty-nine percent of children were later identified, having a mean BEPTA of 46.9 dB HL (SD = 17.5, Mdn = 47.5). Children who were early identified had HL confirmed on average at 7.4 months (SD = 12.4, Mdn = 3.0) and a mean age at hearing aid fitting of 11.8 months (SD = 15.1, Mdn = 6.0). Children who were later identified had HL confirmed roughly 3 months after identification at an average age of 31.7 months (SD = 16.8, Mdn = 30.0) and hearing aid fitting at a mean age of 32.6 months (SD = 17.3, Mdn = 30.5). A description of the etiologies of the children's HLs is beyond the scope of this article. However, a manuscript (Judge et al., 2018) that describes etiologies of approximately one third of the CHH who participated in the outcomes study has been submitted for publication.
A summary of participant demographics is shown in Table 1. Almost all of the mothers who participated in the OCHL study had completed high school or equivalent. Fifty-two percent (n = 90) of the mothers of preschoolers and 56% (n = 87) of the mothers of school-age children had earned a bachelor's degree or higher. In contrast, the 2016 U.S. Census reported that 29% of women in the United States had completed high school or the equivalent, and 32% had a college degree or higher (U.S. Census Bureau, 2016). Although the outcomes research study includes families with a wide range of maternal education, the sample is skewed in the direction of higher maternal education than the general population.
Table 1.
Description of children who are hard of hearing as reported in the preschool- and school-age family interviews.
| Demographic and background characteristics | Preschool (n = 174) |
School age (n = 155) |
||
|---|---|---|---|---|
| n | % | n | % | |
| Child gender | ||||
| Male | 96 | 55.2 | 81 | 52.3 |
| Female | 78 | 44.8 | 74 | 47.7 |
| Child ethnicity | ||||
| African American | 13 | 7.5 | 9 | 5.8 |
| Asian Pacific | 4 | 2.3 | 4 | 2.6 |
| Hispanic or Latino | 5 | 2.9 | 8 | 5.2 |
| Multiracial | 8 | 4.6 | 9 | 5.8 |
| White | 140 | 80.3 | 120 | 77.4 |
| Other | 2 | 1.2 | 4 | 2.6 |
| Undisclosed | 2 | 1.2 | 1 | 0.6 |
| Maternal education: highest level completed | ||||
| High school degree or less | 24 | 13.8 | 24 | 15.5 |
| Some postsecondary education | 59 | 33.8 | 42 | 27.1 |
| College graduate | 41 | 23.6 | 43 | 27.7 |
| Postgraduate work | 49 | 28.2 | 44 | 28.4 |
| Undisclosed | 1 | 0.6 | 2 | 1.3 |
| Timing of identification | ||||
| HL identified at newborn screen | 134 | 77.0 | 102 | 65.8 |
| HL identified later | 40 | 23.0 | 53 | 34.2 |
| Service enrollment at last interview | ||||
| Children receiving services | 141 | 81.0 | 109 | 70.3 |
| Children not receiving services | 33 | 19.0 | 46 | 29.7 |
Note. HL = hearing loss.
CHH were included in the outcomes research study if the primary language used in the home was spoken English. However, some families reported the use of signs in addition to spoken language in the child's educational environment. When families were asked how preschool service providers and teachers communicated with their child, 81% (n = 141) selected spoken language or spoken language plus fewer than 50 signs; 19% (n = 33) indicated spoken language and more than 50 signs. When asked the same question, 92% (n = 142) of families of school-age children indicated the service providers and teachers in their child's educational program used spoken language or spoken language plus fewer than 50 signs, and 8% (n = 13) indicated spoken language plus more than 50 signs. Parents were not specifically queried in the Family Interview whether the educational programs were considered total communication or not.
A total of 133 preschool professionals including SLPs (n = 68), teachers of CDHH (n = 58), special educators (n = 5), early childhood educators (n = 1), and an SLP assistant (n = 1) participated. School-age professionals (n = 104) included SLPs (n = 55), teachers of CDHH (n = 47), special educators (n = 1), and an SLP assistant (n = 1).
Measures
Family Interview
In addition to standardized speech and language assessments, members of the research team developed interview and survey instruments, including a Family Interview and an online Service Provider Survey (SPS). The National Early Intervention Longitudinal Study Interview (SRI, 2000) was the basis for the Family Interview. However, extensive changes were made to tailor the interview for families of CHH. Three versions of the Family Interview were designed: birth to 3 years, preschool, and school age. An experienced research assistant conducted all of the Family Interviews via telephone approximately 6 months after each child's study visit. Data from the preschool- and school-age versions were used in the current study. Items related to family demographics, whether or not the child received services, and, if so, the setting(s) in which services were delivered were analyzed. Unless otherwise indicated, data from the most recent Family Interview per age group are used. In the preschool group, five families who had two children participating in the study completed separate Family Interviews. In the school age group, three families with two children completed individual interviews for their children. The Family Interviews are available at www.ochlstudy.org.
SPS
Three versions (birth to 3, preschool, and school age) of an online SPS were also developed. This instrument was designed to elicit information from professionals who provided speech and language services or educational support for the children participating in the OCHL research study. The SPS includes questions on characteristics of services, caseload composition, provider preparation, professional experience, and interactions with other professionals. For these questions, professionals were asked to include all children with any degree of HL, not just CHH. In addition, providers indicated their level of comfort with skills related to providing services for CDHH on a 4-point Likert scale ranging from expert to none. Although a majority of the skill items are identical in the preschool and school lists, characteristics unique to the needs of the two age groups resulted in the development of separate preschool- and school-age lists.
A majority of all respondents (96.2%; n = 209) were either an SLP or a teacher of CDHH. The remaining respondents (3.8%; n = 9) were from a range of professions, including special education, early childhood education, and SLP assistant. The number of individuals representing each of these professions was very small and, thus, could not be considered representative of a profession. As a result, their responses were excluded in the analyses of caseload characteristics, professional experience, and comfort with professional skills. When a respondent served both age groups of children, which occurred for 19 providers, his or her most recent preschool and school SPS were used to provide a comprehensive description of the professionals and services for each age group.
Audiologic Measures
At each research study visit, participants completed a hearing evaluation that included otoscopy, pure-tone audiometry, and tympanometry. Hearing thresholds were obtained using insert earphones with foam tips, supra-aural headphones, or insert earphones with the child's earmolds. Sound field thresholds were obtained if ear-specific thresholds could not be measured. A four-frequency BEPTA was calculated at 0.5, 1, 2, and 4 kHz. If an audiogram could not be completed at the visit, the most recent clinical audiogram was obtained and used for the purposes of the study.
Speech and Language Measures
Results from a subset of norm-referenced measures from the OCHL test protocol were used in this study to compare speech and language abilities of the children across educational/service settings. The speech and language measures selected for this study are frequently used to evaluate children for services provided in preschool or elementary school. These included (a) the Goldman-Fristoe Test of Articulation–Second Edition (GFTA-2) Sounds-in-Words subtest (Goldman & Fristoe, 1999), (b) the Word Structure subtest of the Clinical Evaluation of Language Fundamentals–Fourth Edition (Semel, Wiig, & Secord, 2004), (c) the Comprehensive Assessment of Spoken Language (CASL; Carrow-Woolfolk, 1999) Core and Syntax subtests, (d) the Wechsler Preschool and Primary Scale of Intelligence–Third Edition Vocabulary subtest (Wechsler, 2002), and (e) the Wechsler Abbreviated Scale of Intelligence–Second Edition Vocabulary subtest (Wechsler & Hsiao-Pin, 2011).
Results
Receipt of Services, Service Setting, and Student Characteristics
Research Questions 1 and 2 aimed to describe (a) the settings, amount, and how services were received (individually, in a group, or a combination of the two) by CHH and (b) the relationships between receipt of services, service setting, and characteristics of the children during the preschool and early school years. Thirty-three (19%) families reported that their preschool children did not receive services. The remaining 141 children were seen in six different service settings, including general education preschools, preschools for CDHH, preschools for children with exceptional needs (e.g., multicategorical needs preschools), clinics or therapists' offices, child care centers, and at home. Three settings, general education preschools (32.6%), preschools for CDHH (31.2%), and preschools for children with exceptional needs (17.0%), collectively accounted for 81% (n = 114) of the service settings for CHH. Children in preschools for CDHH spent more time in services (M = 476.6 min/week) than those in preschools for children with exceptional needs (M = 79.4 min/week), general education preschools (M = 46.5 min/week), clinic or therapist's office (M = 44.3 min/week), child care (M = 62.4 min/week), or services in the home (M = 38.9 min/week). Preschool-age children receiving services from an SLP were seen an average of 1.92 times/week averaging 35.8 min (SD = 26.5) per session. Children receiving services from a teacher of CDHH were seen on average 2.5 times/week for 88.6 min per session (SD = 96.0). Across all settings, 51% (n = 72) of preschool children received services individually. Forty percent (n = 56) received services in a combination of individual and group therapy, and 9% (n = 13) received services only in a group.
At school age, parents reported that 30% (n = 46/155) of the children were not receiving services. Among the children who did have services, 83% (n = 91/109) received them in a general education setting. Similar to the preschool results, CHH attending a school for CDHH spent the most time in services, averaging 162.5 min, or slightly more than 2.5 hr of services per week. School-age CHH in general education settings averaged 79.6 min/week of intervention with an SLP or teacher of children who are deaf or hard of hearing, and those in a therapist's clinic averaged 61.6 min/week. When services were provided by an SLP, school-age students were seen an average of 1.7 times per week for 30.7 min per session (SD = 14.0). Teachers of CDHH provided services on average 1.75 times per week. Each session was an average of 46.9 min in duration (SD = 52.4). Most of the children in general education settings (84.6%, n = 77) received individual or combined (individual + group) therapy. The remaining children (n = 14) were seen in a group only. Service configuration information was not provided for three participants who were seen in a general education setting. Table 2 shows the configuration of service delivery by setting and age group.
Table 2.
Configuration of service delivery by setting for preschool- and school-age children who are hard of hearing.
| Tx configuration |
Service setting (%) |
|||||
|---|---|---|---|---|---|---|
| Preschool | General ed. preschool n = 46 |
Preschool for CDHH n = 44 |
Preschool for CE n = 24 |
Office or clinic n = 20 |
Childcare n = 4 |
Home n = 3 |
| Individual Tx | 60.9 | 27.3 | 27.3 | 85.0 | 75.0 | 100.0 |
| Group Tx | 4.3 | 9.1 | 13.6 | 5.0 | 0 | 0 |
| Combination |
34.8 |
63.6 |
59.1 |
10.0 |
25.0 |
0 |
|
School |
General ed. school
n = 91 |
School for CDHH
n = 6 |
School for CE
n = 0 |
Office or clinic
n = 11 |
Childcare
n = 0 |
Home
n = 1 |
| Individual Tx | 37.5 | 0 | 0 | 77.8 | 0 | 100.0 |
| Group Tx | 12.5 | 0 | 0 | 0 | 0 | 0 |
| Combination | 50.0 | 100.0 | 0 | 22.2 | 0 | 0 |
Note. Tx = Therapy; ed. = education; CDHH = children who are deaf or hard of hearing; CE = children with exceptionalities; combination = individual + group therapy.
Audiologic Characteristics by Service Setting
We utilized analyses of variance (ANOVAs) for both preschool- and school-age service settings to test for differences between mean BEPTA, mean age at identification of HL, and mean age at hearing aid fitting.
Five preschool settings were used in the analysis: (a) general education preschools (n = 46), (b) preschools for CDHH (n = 44), (c) preschools for children with exceptional needs (n = 24), (d) clinic or therapists' offices (n = 20), and (e) “no services” (n = 33). Because so few preschool children received services in child care (n = 4) or at home (n = 3), they were not included in these analyses. There were no statistically significant mean differences between preschool service settings for BEPTA, F(4, 162) = 1.42, p = .23, age at identification of HL, F(4, 160) = 0.83, p = .511, nor age at hearing aid fit, F(4, 159) = 0.59, p = .672.
The four school-age settings included (a) general education schools (n = 91), (b) schools for CDHH (n = 6), (c) clinic or therapist's offices (n = 11), and (d) no services (n = 46). Among school-age children, the mean BEPTA difference between service settings was statistically significant, F(3, 150) = 4.55, p = .004. Post hoc pairwise comparisons using Bonferroni adjustments were performed to determine which specific service settings were significantly different from one another. These tests revealed that children who received services in general education school settings had significantly poorer hearing thresholds (M = 50.22, SD = 14.5, p = .012) than children who were not in services (M = 41.91, SD = 12.6). No other pairwise comparisons yielded significant differences. No statistically significant main effects were yielded between school-age service settings for age at identification of HL, F(3, 149) = 1.5, p = .217, or age at hearing aid fit, F(3, 142) = 1.79, p = .153.
Speech-Language Characteristics by Service Setting
Next, we utilized ANOVAs to assess differences in articulation, language, and definitional vocabulary abilities between service settings for the preschool- and school-age CHH. Table 3 shows the mean scores for the preschool- and school-age settings. Significant differences between preschool service settings were found on combined receptive and expressive language via the CASL Core Composite (4, 114) = 6.82, p < .001, and for Syntax, F(4, 132) = 5.21, p < .001. Post hoc comparisons using a Bonferroni multiple comparisons adjustment showed significant differences in CASL composite scores between no services (M = 110.0, SD = 18.2) and three preschool settings, including general education preschools (M = 90.6, SD = 18.2, p = .001), preschools for CDHH (M = 87.6, SD = 16.7, p < .001), and preschools for exceptional children (M = 88.4, SD = 17.2, p = .002). On the preschool syntax measures, significant differences existed between no services (M = 102.5, SD = 16.0) and the same three settings: general education preschools (M = 89.4, SD = 16.6, p = .017), preschools for CDHH (M = 86.5, SD = 15.6, p = .002), and preschools for children with exceptionalities (M = 84.4, SD = 15.6, p = .003). There were no significant differences in the performance of preschool CHH receiving services in a clinic or therapist's office and any of the other preschool settings. Significant main effects were not detected for preschool outcomes on the GFTA-2 Sounds-in-Words subtest, F(4, 45) = 1.62, p = .187, nor for the Wechsler Preschool and Primary Scale of Intelligence–Third Edition Vocabulary subtest, F(4, 75) = 1.52, p = .203.
Table 3.
Mean performance for children who are hard of hearing on speech and language measures by service setting.
| Measures |
Service settings: M (SD) |
||||
|---|---|---|---|---|---|
| Preschool | No services | General ed. preschool | Preschool for CDHH | Preschool for CE | Office or clinic |
| GFTA-2 (n = 50) | 105.0 (10.5) | 90.1 (20.7) | 88.2 (18.7) | 88.2 (18.8) | 92.9 (14.2) |
| Syntax a (n = 136) | 102.5 (16.0) | 89.4 (16.6) | 86.0 (14.7) | 84.4 (15.6) | 92.1 (17.7) |
| CASL Core Composite (n = 119) | 110.0 (18.2) | 90.6 (18.2) | 87.6 (16.7) | 88.4 (17.2) | 98.3 (18.2) |
| WPPSI-III Vocabularyb (n = 80) |
9.9 (2.4) |
8.3 (3.1) |
7.9 (2.6) |
8.0 (3.1) |
7.6 (3.2) |
|
School |
No services |
General ed. school |
School for CDHH |
School for CE |
Office or clinic |
| GFTA-2 (n = 77) | 105.2 (8.7) | 93.2 (12.7) | 83.7 (29.7) | — | 96.0 (11.6) |
| Syntax a (n = 118) | 112.3 (17.0) | 93.1 (17.5) | 74.4 (29.8) | — | 92.8 (17.3) |
| CASL Core Composite (n = 60) | 117.5 (17.0) | 103.1 (23.5) | 69.5 (7.8) | — | 109.2 (10.6) |
| WASI Vocabulary c (n = 105) | 56.9 (10.6) | 47.5 (9.5) | 33.5 (2.1) | — | 45.3 (6.1) |
Note. Em dashes indicate data not applicable. Ed. = education; CDHH = children who are deaf or hard of hearing; CE = children with exceptionalities; GFTA-2 = Goldman-Fristoe Test of Articulation–Second Edition; CASL = Comprehensive Assessment of Spoken Language; WPPSI-III = Wecshler Preschool and Primary Scale of Intelligence–Third Edition; WASI = Wechsler Abbreviated Scale of Intelligence.
Syntax consists of either the CASL Syntax subtest or the Clinical Evaluation of Language Fundamentals–Fourth Edition Word Structure subtest. In the four instances where participants were administered both subtests in the same year, the higher of the two scores was used.
The WPPSI-III Vocabulary subtest utilizes scaled scores with a range of 1–19 and a mean of 10 (50th percentile).
The WASI Vocabulary subtest utilizes t scores with a range of 20–80 and a mean of 50 (50th percentile).
Similarly, we utilized ANOVAs to assess differences in articulation, language, and definitional vocabulary abilities of CDHH across the school-age settings. Again, CHH with no services consistently demonstrated the highest mean scores on all measures compared with school-age students in any of the service settings. Statistically significant main effects were detected for the GFTA-2 Sounds-in-Words subtest, Welch's F(3, 7) = 6.30, p = .020. Post hoc comparisons using a Bonferroni multiple comparisons adjustment showed significant differences in standard scores between no services (M = 105.2, SD = 8.7) and the general education setting (M = 93.2, SD = 12.7, p = .002) and schools for CDHH (M = 83.7, SD = 29.7, p = .035). CASL composite scores of global language also returned a significant main effect, F(3, 56) = 3.88, p = .014, and post hoc comparisons revealed significant group differences between no services (M = 117.5, SD = 17.07) and schools for CDHH (M = 69.5, SD = 7.8, p = .021). For school-age syntactic abilities, a significant main effect, F(3, 116) = 11.71, p < .001, was also found. Pairwise comparisons determined statistically significant differences between no services (M = 112.3, SD = 17.0) and three settings including general education (M = 93.1, SD = 17.5, p < .001), schools for CDHH (M = 74.4, SD = 29.8, p < .001), and therapist's office/clinic (M = 92.8, SD = 17.3, p = .020). Definitional vocabulary abilities, as measured by the Wechsler Abbreviated Scale of Intelligence–Second Edition Vocabulary subtest, yielded a statistically significant main effect between standard t scores, F(3, 101) = 8.95, p < .001. Bonferroni comparisons detected significant group differences between no services (M = 56.9, SD = 10.6), general education settings (M = 47.6, SD = 9.5, p < .001), schools for CDHH (M = 33.5, SD = 2.1, p = .007), and therapist's office/clinic (M = 45.3, SD = 6.1, p = .030). Statistically significant ANOVAs and post hoc comparisons for preschool- and school-age children are shown in Table 4.
Table 4.
Statistically significant analyses of variance (ANOVAs) and post hoc t tests comparing type of service location to outcomes for preschool- and school-age children who are hard of hearing.
| Group | Measures | Post hoc comparisons |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| ANOVA main effects |
95% familywise CI |
||||||||
| df | F | p | M difference a | p adjusted b | r | Lower bound | Upper bound | ||
| Preschool | |||||||||
| Syntax c | 4, 132 | 4.90 | .001 | ||||||
| No services X general ed. preschool | 13.18 | .017 | .37 | 1.82 | 24.54 | ||||
| No services X preschool for CDHH | 16.08 | .002 | .47 | 4.60 | 27.56 | ||||
| No services X preschool for CE | 18.12 | .003 | .50 | 4.58 | 31.66 | ||||
| CASL Core Composite | 4, 114 | 6.82 | < .001 | ||||||
| No services X general ed. preschool | 19.40 | .001 | .47 | 5.85 | 32.95 | ||||
| No services X preschool for CDHH | 22.43 | < .001 | .54 | 9.31 | 35.55 | ||||
| No services X preschool for CE | 21.61 | .002 | .52 | 6.23 | 36.00 | ||||
| School | |||||||||
| BEPTA | 3, 150 | 4.55 | .004 | ||||||
| No services X general ed. school | −8.31 | .012 | −.29 | −15.19 | −1.43 | ||||
| GFTA-2 Sounds-in-Words d | 3, 7 | 6.30 | .020 | ||||||
| No services X general ed. school | 11.98 | .002 | .48 | 3.66 | 20.29 | ||||
| No services X school for CDHH | 21.51 | .035 | .44 | 1.59 | 41.43 | ||||
| Syntax c | 3, 116 | 11.71 | < .001 | ||||||
| No services X general ed. school | 19.20 | < .001 | .49 | 9.29 | 29.12 | ||||
| No services X school for CDHH | 37.91 | < .001 | .62 | 15.42 | 60.41 | ||||
| No services X office/clinic | 19.51 | .020 | .49 | 2.57 | 36.46 | ||||
| CASL Core Composite d | 3, 56 | 3.88 | .014 | ||||||
| No services X school for CDHH | 48.00 | .021 | .88 | 6.27 | 89.73 | ||||
| WASI Vocabulary | 3, 101 | 8.95 | < .001 | ||||||
| No services X general ed. school | 9.34 | < .001 | .42 | 3.77 | 14.92 | ||||
| No services X school for CDHH | 23.40 | .007 | .84 | 5.07 | 41.72 | ||||
| No services X office/clinic | 11.61 | .030 | .56 | 1.06 | 22.17 | ||||
Note. CI = confidence interval; CDHH = children who are deaf or hard of hearing; CASL = Comprehensive Assessment of Spoken Language; CE = children with exceptionalities; BEPTA = better-ear pure-tone average; ed. = education; GFTA-2 = Goldman-Fristoe Test of Articulation–Second Edition; WASI = Wechsler Abbreviated Scale of Intelligence.
M difference = M (no services) – M (intervention setting).
Bonferroni adjustment for multiple comparisons.
Depending on age at testing, syntax was either assessed with the CASL Syntax subtest or the Clinical Evaluation of Language Fundamentals–Fourth Edition Word Structure subtest.
Welch's F-ratio was utilized to address heterogeneity of variance in GFTA-2 scores.
Although each of the settings were contrasted with one another for preschool- and school-age CHH, only significant differences existed among CHH without services and those with services regardless of setting. Statistically significant differences were not found among the settings where children did receive services. These results suggest that children with no services demonstrated consistently better outcomes (i.e., group means) than those who did. Further, CHH who received services performed similarly to one another, regardless of setting.
Professionals Providing Services
The information presented in this section is based upon the online SPS completed by the professionals providing preschool (n = 133) and/or school (n = 104) services related to hearing and communication for children in the current study. Nineteen of the professionals completed both a preschool- and school-age SPS during the course of the study. Unless specifically noted, each provider's most recent response completed per age group was used in the information reported for that group.
Degrees, Certifications, and Continuing Education
All but seven of the professionals working with preschool- and school-age CHH were either an SLP or teachers of CDHH. Their degrees ranged from associate to doctoral; however, 87% (n = 115/133) of the professionals serving preschool children held at least a master's degree. Eighty-six out of 104 (83%) of the professionals providing services to school-age children had earned a master's or doctoral degree. The degrees earned by professionals providing services to both age groups are shown in Table 5.
Table 5.
Characteristics of preschool- and school-age speech-language pathologist (SLP) and teacher of children who are deaf or hard of hearing (CDHH) professionals.
| Professional characteristics | Preschool |
School age |
||
|---|---|---|---|---|
| SLP (n = 68) |
TODHH (n = 58) |
SLP (n = 55) |
TODHH (n = 47) |
|
| Degree level: n (%) | ||||
| Bachelor's | 0 | 14 (24.1) | 0 | 14 (34.1) |
| Master's | 66 (97) | 43 (74.2) | 55 (100) | 30 (63.8) |
| Ed.S. | 1 (1.5) | 1 (1.7) | 0 | 2 (2.1) |
| PhD | 1 (1.5) | 0 | 0 | 0 |
| Continuing education: n (%) | ||||
| None | 7 (10.3) | 23 (39.6) | 6 (10.9) | 19 (40.4) |
| Day-long in-service | 10 (14.7) | 12 (20.7) | 8 (14.6) | 4 (8.5) |
| One- to 2-week course | 4 (5.9) | 4 (6.9) | 2 (3.6) | 8 (17.0) |
| Semester-long course or more | 47 (69.1) | 19 (32.8) | 39 (70.9) | 16 (34.1) |
| Professional experience: n (%) | ||||
| 0 to 5 years | 32 (45.6) | 22 (37.9) | 18 (32.7) | 8 (17.0) |
| 6 to 10 years | 14 (20.6) | 13 (22.4) | 11 (20.0) | 10 (21.3) |
| 11 to 15 years | 14 (20.6) | 6 (10.3) | 12 (21.8) | 8 (17.0) |
| > 15 years | 8 (13.2) | 17 (29.3) | 14 (25.5) | 21 (44.7) |
| Caseload | ||||
| Total students on caseload: M (SD) | 34.4 (15.9) | 14.7 (10.2) | 40.7 (18.2) | 17.1 (9.9) |
| Total caseload range | 5–80 | 4–50 | 5–87 | 4–45 |
| % of caseload with CDHH a : M (SD) | 29.0 (0.4) | 94.0 (0.2) | 21.5 (0.3) | 97.7 (0.1) |
| % range of CDHH on caseload a | 1.8–100 | 11.4–100 | 1.1–100 | 45.8–100 |
Note. Em dashes indicate data not [obtained/reported/available]. TODHH = teacher of children who are deaf or hard of hearing; Ed.S. = education specialist degree; PhD = doctor of philosophy; CDHH = children who are deaf or hard of hearing.
Of the 68 preschool SLPs, one provided the total caseload amount but did not report the percentage of caseload with CDHH.
Each professional was also asked to indicate any certifications they had earned in addition to those associated with their primary degree. For this investigation, professionals who possessed dual certifications as a teacher of CDHH and SLP were considered to have attained additional certification because the combination of the two certifications created unique, specialized preparation to serve CHH. Results for the SLPs (n = 68) and teachers of CDHH (n = 58) providing services to preschool children were similar. Sixty (88%) of the SLPs and 51 (88%) of the teachers of CDHH reported no additional certifications. Eight (12%) of SLPs and seven (12%) teachers of CDHH reported additional certifications, including SLP (n = 2), teacher of CDHH (n = 2), listening and spoken language specialist (n = 7), special education (n = 2), reading specialist (n = 1), and administration (n = 1). Of the seven service providers from other professions, only one special educator reported an additional certification as a sign language interpreter.
Among professionals serving school-age children, 45 (82%) of the SLPs and 44 (92%) of the teachers of CDHH reported having no additional certifications. These were the only two professions reporting additional certifications, which included SLP (n = 1), teachers of CDHH (n = 3), listening and spoken language specialist (n = 4), special education (n = 2), reading specialist (n = 1), and administration (n = 2). For the 19 professionals who completed both a preschool- and school-age SPS, two possessed dual SLP/teacher of CDHH credential.
The amount of continuing education specifically related to HL was also queried. The range of reported continuing education for both SLPs and teachers of CDHH is shown in Table 5. For professionals serving both age groups, 89% of SLPs reported continuing education related to childhood HL compared with 60% of the teachers of CDHH.
Years of Experience and Caseloads
Overall, school-age providers (M = 13.5, SD = 9.6) had more years of experience working with CDHH than preschool providers (M = 10.7, SD = 9.5). Teachers of the deaf or hard of hearing (M = 15.8, SD = 10.3), on average, had 4 more years of experience compared with SLPs (M = 11.5, SD = 8.6), a statistically significant difference, t(100) = 2.37, p = .020. As shown in Table 5, nearly half of all preschool SLPs were within the first 5 years of their career.
Providers also reported the number of children on their caseloads. If a professional completed more than one annual survey for the preschool or school years, an average was calculated based on their repeated responses for both total number of children and percent of CDHH on their caseload. The total caseload ranges and means were higher for SLPs than for teachers of CDHH regardless of the ages of the children. For preschool professionals, SLPs total caseloads averaged 34.4 (SD = 15.9) students and 14.7 (SD = 10.2) for teachers of CDHH. At school age, the total caseloads for SLPs averaged 40.7 (SD = 18.2) students and 17.1 (SD = 9.9) for teachers of CDHH. However, the percentage CDHH on those caseloads was considerably higher for the teachers in both age groups. On average, preschool teachers of CDHH had caseloads that were primarily composed of CDHH (M = 94%, SD = 0.43). In contrast, CDHH made up only 29% (SD = 0.43) of the SLPs' caseloads. Similarly, caseloads for school teachers of CDHH consisted of 98% (SD = 0.082) CDHH, whereas SLP caseloads had 22% (SD = 0.33). SLPs (n = 8) who had certification as a teacher of CDHH or a listening and spoken language specialist were exceptions to these findings. Using Pearson correlation, dual certification of SLP plus teacher of CDHH or listening and spoken language specialist was positively correlated (r = .38; p = .004) with the percentage of CDHH on SLP caseloads. Dual certification was not significantly correlated with caseload composition for teachers of CDHH (r = .12; p = .416). In addition, there was not a statistically significant linear relationship between preschool providers' years of experience and percentage of CDHH on caseloads (r = .16, p = .072). For school professionals, there was a statistically significant correlation, although the linear relationship is considered weak (r = .22, p = .028).
Provider Self-Assessment of Comfort
Each respondent indicated their level of comfort with skills associated with providing services to CDHH. A comparison of the professionals' reported comfort levels is shown in Table 6. Significant differences were found between the two professions for a majority of the skills. A Fisher's exact test was used to compare the comfort level that SLPs and teachers of CDHH reported for each skill. This nonparametric method was used rather than a Pearson chi-square test of independence because many cells contained five or fewer responses.
Table 6.
A comparison of comfort levels with significant differences between speech-language pathologists (SLPs) and teachers of children who are deaf or hard of hearing (TODHH) at preschool and school ages.
| Skill area | Preschool |
School |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SLP |
TODHH |
SLP |
TODHH |
|||||||||||||
| n | M | SD | n | M | SD | p | r | n | M | SD | n | M | SD | p | r | |
| Assessing speech | 68 | 1.50 | 0.50 | 57 | 1.76 | 0.51 | .006 | −.25 | 54 | 1.28 | 0.45 | 44 | 2.20 | 0.79 | < .001 | −.58 |
| Assessing language | 68 | 1.49 | 0.53 | 58 | 1.26 | 0.48 | .018 | .22 | 54 | 1.35 | 0.48 | 47 | 1.62 | 0.59 | .022 | −.24 |
| Assessing communication approach | 68 | 1.78 | 0.59 | 57 | 1.33 | 0.47 | < .001 | .39 | — | — | — | — | — | — | — | — |
| Designing therapy goals | 68 | 1.56 | 0.55 | 58 | 1.20 | 0.45 | < .001 | .34 | 54 | 1.45 | 0.50 | 47 | 1.43 | 0.5 | .429 | .02 |
| Developing sign language | 67 | 2.24 | 0.81 | 58 | 1.93 | 1.03 | .061 | .16 | 55 | 1.94 | 0.81 | 41 | 1.31 | 0.47 | < .001 | .43 |
| Carryover of speech therapy to home | 68 | 1.59 | 0.61 | 56 | 1.63 | 0.65 | .738 | −.03 | 54 | 1.50 | 0.5 | 41 | 2.20 | 0.86 | < .001 | −.45 |
| Carryover of speech therapy to class | — | — | — | — | — | — | — | — | 54 | 1.51 | 0.51 | 41 | 2.02 | 0.82 | .002 | −.35 |
| Expanding vocabulary through play | 68 | 1.27 | 0.44 | 58 | 1.11 | 0.31 | .023 | .21 | — | — | — | — | — | — | — | — |
| Building language through play | 68 | 1.27 | 0.48 | 58 | 1.09 | 0.29 | .001 | .22 | — | — | — | — | — | — | — | — |
| Promoting language in routines | 68 | 1.33 | 0.51 | 58 | 1.07 | 0.26 | < .001 | .31 | 54 | 1.43 | 0.53 | 47 | 1.82 | 0.74 | .009 | −.29 |
| Carryover of language therapy to home | 68 | 1.56 | 0.58 | 57 | 1.31 | 0.54 | .020 | .22 | 53 | 1.49 | 0.50 | 46 | 1.80 | 0.79 | .046 | −.23 |
| Promoting participation in discussions | — | — | — | — | — | — | — | — | 54 | 1.56 | 0.72 | 47 | 1.31 | 0.47 | .033 | .20 |
| Promoting early literacy / literacy | 68 | 1.85 | 0.71 | 58 | 1.17 | 0.38 | < .001 | .51 | 53 | 1.79 | 0.60 | 47 | 1.48 | 0.70 | .031 | .23 |
| Supporting academic development | — | — | — | — | — | — | — | — | 55 | 1.67 | 0.51 | 47 | 1.34 | 0.48 | .003 | .32 |
| Promoting accommodations in school | — | — | — | — | — | — | — | — | 54 | 2.32 | 1.03 | 47 | 1.08 | 0.28 | < .001 | .63 |
| Developing self-advocacy | — | — | — | — | — | — | — | — | 53 | 1.71 | 0.56 | 47 | 1.31 | 0.53 | < .001 | .34 |
| Developing listening skills | 67 | 2.13 | 0.87 | 58 | 1.27 | 0.49 | < .001 | .52 | 55 | 2.07 | 0.80 | 47 | 1.48 | 0.56 | < .001 | .39 |
| Using Ling sounds | 68 | 2.43 | 1.24 | 56 | 1.11 | 0.37 | < .001 | .58 | 55 | 2.45 | 1.24 | 46 | 1.08 | 0.37 | < .001 | .60 |
| Inserting earmolds | 67 | 2.19 | 0.93 | 58 | 1.09 | 0.29 | < .001 | .62 | 55 | 2.54 | 0.84 | 47 | 1.71 | 0.75 | < .001 | .46 |
| Daily hearing aid checks | 68 | 2.22 | 1.00 | 58 | 1.05 | 0.23 | < .001 | .63 | 55 | 2.28 | 1.09 | 46 | 1.05 | 0.23 | < .001 | .62 |
| Troubleshooting hearing devices | 68 | 2.66 | 0.95 | 58 | 1.37 | 0.52 | < .001 | .64 | 55 | 2.66 | 0.99 | 47 | 1.37 | 0.49 | < .001 | .64 |
| Using FM | 67 | 2.15 | 0.84 | 58 | 1.22 | 0.42 | < .001 | .57 | 55 | 1.98 | 0.79 | 47 | 1.22 | 0.42 | < .001 | .51 |
Note. Participants rated their comfort on a 4-point scale with lower scores indicating more comfort with a particular skill. Em dashes indicate that a particular skill was not queried on either the preschool or school survey.
At the preschool level, no difference in comfort level was found between SLPs (n = 68) and teachers of CDHH (n = 58) for developing sign language and carryover of speech therapy to home. Preschool SLPs reported being significantly more comfortable assessing speech than teachers of CDHH (p = .005). Teachers of CDHH reported significantly more comfort than SLPs (p s < .001) with six items related to the use of hearing instruments, as well as with assessing communication approach, promoting early literacy, promoting language in routines, and designing therapy goals.
Among the list of skills related to school-age children, no differences in comfort scores were found between the two professional groups on five of the identified skills. These included designing therapy goals and four skills associated with language development: promoting complex language, promoting social language in school, promoting language with peers, and expanding vocabulary. SLPs of school-age children were more comfortable than teachers of CDHH with three items related to speech, as well as promoting language in routines and carryover of language goals to the home. Teachers of CDHH reported more comfort than SLPs (p s < .001) with the six skills involving hearing technologies and auditory development, as well as developing sign language skills and promoting adequate accommodations for students who are deaf or hard of hearing. As shown in Table 6, the teachers of CDHH were significantly more comfortable than SLPs with four other skills, including promoting participation in discussions, promoting literacy, developing self-advocacy, and supporting academic development.
Next, we analyzed whether SLPs with additional certifications as teachers of CDHH or as listening and spoken language specialists differed in comfort levels from SLPs without. Preschool SLPs with these certifications reported being significantly more comfortable inserting earmolds (p = .031), conducting daily listening checks (p = .030), using Ling sounds (p = .007; Ling, 1989), troubleshooting hearing devices (p = .027), and developing listening skills (p = .002). Similarly, SLPs serving school-age children were more comfortable with three skills necessary for device management, including inserting earmolds (p = .003), conducting daily hearing aid checks (p = .007), and troubleshooting devices (p < .001).
Relationship of Experience and Caseload to Comfort With Skills
Research Question 4 sought to examine if professional characteristics predicted self-reported comfort levels regarding essential skills for working with CHH. Predictors were chosen based on variables used in Harrison et al. (2016) to analyze comfort among professionals working with CHH aged birth to 3 years. Initially, a five-predictor logistic regression model was proposed. The most parsimonious model consisted of three variables to determine how the (a) number of CDHH on a caseload, (b) percent of CDHH on a caseload, and (c) providers' years of experience working with CDHH are related to the log odds of considering oneself an expert in the various rated areas of expertise. Two of the five proposed variables, amount of communication with an audiologist and professional discipline, were excluded due to strong interrelationships with the remaining variables. For these analyses, we dichotomized comfort ratings into expert and less than expert. This was done because few people chose the very little or none categories.
For professionals working with preschool CHH, both years of experience and the percent of CDHH on a caseload were significant predictors of comfort ratings for a majority of the skill areas. While more years of experience were modestly associated with increases in comfort, greater proportions of CDHH on a provider's caseload often yielded high odds that the professional was more likely to self-report as an expert. The odds of identifying oneself as an expert on skills related to managing hearing technology and developing listening skills were very high (odds ratios ranging from 7.8 to 146.5) when the professional had greater proportions of their caseload consisting of CDHH. This was the case for both preschool- and school-age providers. The concordance statistics for these particular skills indicated a strong goodness of fit with most values above 0.8, ranging from .768 to .957. At preschool, higher proportions of CDHH on caseloads strongly predicted expertise for promoting literacy (b = 3.017, p < .001), promoting language in routines (b = 2.248, p = .004), assessing communication approach (b = 2.117, p < .001), and designing therapy goals (b = 1.906, p = .001). Aside from hearing-related skills, promoting self-advocacy (b = 1.587, p = .027) was the only skill where caseload makeup was a strong predictor of expertise. All significant predictors and associated skill areas are shown in Table 7. The total number of CDHH on a caseload was not a significant predictor for any skills at the preschool level and was a modest predictor of expertise for designing therapy goals (b = −0.066, p = .003), promoting complex language (b = −0.035, p = .048), expanding vocabulary (b = −0.045, p = .021), and promoting language with peers (b = −0.044, p = .016) for school professionals.
Table 7.
Statistically significant logistic regression results showing the likelihood of professionals reporting high levels of clinical skill comfort with caseload characteristics and more years of experience.
| Skill area (c-statistic) and predictors | Estimate | χ2 | p | Odds ratio |
|---|---|---|---|---|
| Preschool a | ||||
| Assessing language (.738) | ||||
| Percent of CDHH on caseload | 1.521 | 7.072 | .008 | 4.575 |
| Years of experience | 0.081 | 8.483 | .004 | 1.084 |
| Assessing communication approach (.776) | ||||
| Percent of CDHH on caseload | 2.117 | 12.464 | < .001 | 8.309 |
| Years of experience | 0.091 | 11.481 | < .001 | 1.095 |
| Designing therapy goals (.773) | ||||
| Percent of CDHH on caseload | 1.906 | 10.189 | .001 | 6.724 |
| Years of experience | 0.114 | 12.192 | < .001 | 1.121 |
| Promoting language in routines (.760) | ||||
| Percent of CDHH on caseload | 2.248 | 8.431 | .004 | 9.464 |
| Years of experience | 0.075 | 4.276 | .039 | 1.079 |
| Building language through play (.721) | ||||
| Percent of CDHH on caseload | 1.760 | 5.198 | .023 | 5.815 |
| Expanding vocabulary (.734) | ||||
| Percent of CDHH on caseload | 1.715 | 5.524 | .019 | 5.554 |
| Years of experience | 0.089 | 5.330 | .021 | 1.093 |
| Developing oral language (.690) | ||||
| Percent of CDHH on caseload | 1.396 | 6.012 | .014 | 4.037 |
| Years of experience | 0.047 | 3.88 | .049 | 1.048 |
| Promoting literacy (.828) | ||||
| Percent of CDHH on caseload | 3.017 | 22.250 | < .001 | 20.438 |
| Years of experience | 0.089 | 8.448 | .004 | 1.093 |
| Carryover of speech therapy to home (.660) | ||||
| Years of experience | 0.054 | 6.564 | .010 | 1.056 |
| Carryover of language therapy to home (.740) | ||||
| Years of experience | 0.108 | 12.884 | < .001 | 1.114 |
| Inserting earmolds (.872) | ||||
| Percent of CDHH on caseload | 4.051 | 29.208 | < .001 | 57.478 |
| Daily hearing aid checks (.909) | ||||
| Percent of CDHH on caseload | 4.451 | 28.221 | < .001 | 93.781 |
| Years of experience | 0.081 | 4.737 | .030 | 1.085 |
| Use Ling sounds (.913) | ||||
| Percent of CDHH on caseload | 4.381 | 26.764 | < .001 | 79.889 |
| Troubleshooting hearing devices (.818) | ||||
| Percent of CDHH on caseload | 2.924 | 17.364 | < .001 | 18.612 |
| Using FM (.768) | ||||
| Percent of CDHH on caseload | 2.057 | 12.653 | < .001 | 7.822 |
| Developing listening skills (.820) | ||||
| Percent of CDHH on caseload | 2.941 | 22.518 | < .001 | 18.934 |
| Years of experience | 0.060 | 5.084 | .024 | 1.062 |
| School b | ||||
| Assessing speech (.718) | ||||
| Percent of CDHH on caseload | −2.326 | 9.124 | .003 | 0.098 |
| Assessing language (.659) | ||||
| Years of experience | 0.054 | 4.915 | .027 | 0.055 |
| Designing therapy goals (.813) | ||||
| Number of CDHH on caseload | −0.066 | 9.174 | .003 | 0.936 |
| Years of experience | 0.120 | 13.510 | < .001 | 1.128 |
| Promoting speech (.674) | ||||
| Percent of CDHH on caseload | −1.781 | 5.327 | .021 | 0.168 |
| Promoting complex language (.739) | ||||
| Number of CDHH on caseload | −0.035 | 3.922 | .048 | 0.965 |
| Years of experience | 0.069 | 6.962 | .008 | 1.071 |
| Expanding vocabulary (.795) | ||||
| Number of CDHH on caseload | −0.045 | 5.290 | .021 | 0.956 |
| Years of experience | 0.122 | 12.047 | < .001 | 1.130 |
| Promoting language with peers (.715) | ||||
| Number of CDHH on caseload | −0.044 | 5.781 | .016 | 0.957 |
| Years of experience | 0.063 | 6.735 | .009 | 1.065 |
| Encourage participation (.757) | ||||
| Years of experience | 0.076 | 7.967 | .005 | 1.079 |
| Self-advocacy (.806) | ||||
| Percent of CDHH on caseload | 1.587 | 4.867 | .027 | 4.889 |
| Promoting literacy (.819) | ||||
| Years of experience | 0.088 | 10.237 | .001 | 1.092 |
| Carryover of speech therapy to class (.664) | ||||
| Years of experience | 0.068 | 8.179 | .004 | 1.071 |
| Carryover of language therapy to class (.708) | ||||
| Years of experience | 0.063 | 6.822 | .009 | 1.065 |
| Carryover of speech therapy to home (.608) | ||||
| Years of experience | 0.046 | 3.862 | .049 | 1.047 |
| Developing sign language (.837) | ||||
| Years of experience | 0.058 | 4.264 | .039 | 1.060 |
| Inserting earmolds (.907) | ||||
| Percent of CDHH on caseload | 3.581 | 16.815 | < .001 | 35.581 |
| Daily hearing aid checks (.931) | ||||
| Percent of CDHH on caseload | 4.845 | 16.899 | < .001 | 127.144 |
| Using Ling sounds (.957) | ||||
| Percent of CDHH on caseload | 4.987 | 16.900 | < .001 | 146.459 |
| Troubleshooting hearing devices (.833) | ||||
| Percent of CDHH on caseload | 3.686 | 13.189 | < .001 | 39.894 |
| Using FM (.784) | ||||
| Percent of CDHH on caseload | 3.309 | 15.437 | < .001 | 27.351 |
| Developing listening skills (.796) | ||||
| Percent of CDHH on caseload | 2.312 | 8.311 | .004 | 10.091 |
| Supporting academic development (.797) | ||||
| Years of experience | 0.077 | 7.858 | .005 | 1.079 |
Note. CDHH = children who are deaf or hard of hearing.
For preschool professionals, there were no statistically significant predictors of clinical comfort for the skill areas assessing speech (.579) or developing sign language (.729).
For school professionals, there were no statistically significant predictors of clinical comfort for the skill areas promoting language (.701), promoting social language in school (.666), carryover of language therapy to home (.606), or promoting accommodations in school (.777).
Communication With Audiologists
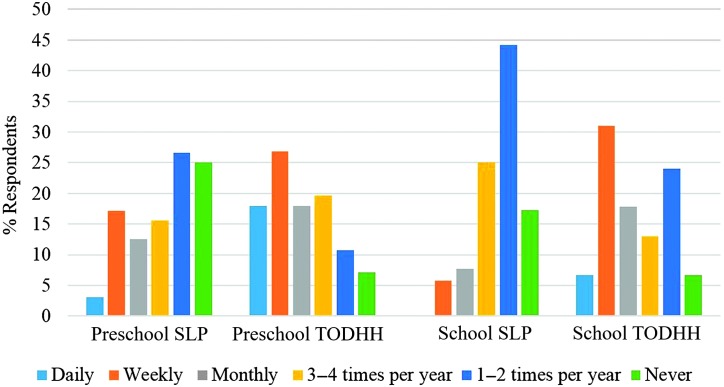
Although frequency of contact with audiologists was too interrelated to be included as a factor in the statistical analysis on provider comfort level above, interprofessional communication by age group and provider profession are described here. In the SPS, both preschool and elementary school providers were asked how often they communicated with the participating child's audiologist. Responses included (a) daily, (b) weekly, (c) monthly, (d) 3–4 times per year, (e) 1–2 times per year, and (f) never. Overall, professionals providing services to preschool children had more frequent contact with audiologists compared with those providing services to school-age children. Seventy-one percent (n = 89/126) of preschool providers communicated with audiologists on at least a monthly basis compared with 35% (n = 36/102) of school-age providers.
Communication with audiologists was also examined by professional discipline as shown in Figure 1. Teachers of CDHH reported more frequent contact with audiologists. Across the preschool and school years, 57% (n = 60/105) of the teachers of CDHH reported at least monthly contact. In contrast, 22.3% of the SLPs (n = 28/123) reported monthly or more frequent contact.
Figure 1.
Frequency of communication with audiologist by profession. SLP = speech-language pathologist; TODHH = teacher of children who are deaf or hard of hearing.
Discussion
As CHH transition from family-centered, home-based Part C services to a child-centered service delivery model, it is considered best practice that their continuing services are provided by knowledgeable professionals during the preschool and elementary school years. Previous work by Harrison et al. (2016) showed that early intervention professionals who have experience working with CDHH are more confident than inexperienced professionals with skills associated with providing services for CHH. The current study sought to characterize both the intervention settings and providers for preschool- and school-age CHH as a step toward understanding how services are accessed after the age of 3 years.
Our first goal was to document the receipt and nature of services for preschool- and school-age CHH, including setting of service provision, frequency/amount of intervention, and provider profession. Harrison et al. (2016) found that over 93% of the OCHL participants received Part C services during the birth to 3 years. In the present cohort, 81% of preschoolers and 70% of school-age CHH received Part B services. Although there is a gradual reduction in the receipt of services, the majority of participants continued to rely on support into elementary school. The present findings suggest a higher reliance of school-based services for CHH than historically reported. Davis et al. (1986) reported that 50% to 60% of school-age children with mild and sloping mild–moderate hearing levels were enrolled in services in Iowa. With greater awareness of the potential to prevent or minimize communicative delays related to permanent childhood HL, increases in service provision might be expected in the postnewborn hearing screening era. Consistent with this view, Vohr et al. (2012) reported that 100% of preschool CDHH in Rhode Island, with hearing levels ranging from unilateral mild to profound bilateral, were documented to have received intervention services. While the resource needs of CHH are more likely to be addressed in educational settings now compared to 30 years ago, further research would be worthwhile to explore why some children still do not receive services.
Greater numbers of preschool participants received services in preschools for CDHH and those for children with exceptionalities than at school age, when the overwhelming majority of CHH were seen in general education settings. At age 3 years, many CHH have just begun to consistently wear their hearing aids and, thus, have experienced reduced acoustic and linguistic access (Walker, McCreery, et al., 2015). It is plausible that a greater proportion of CHH at preschool rely on specialized settings and support to address greater speech and language delays and less consistent hearing aid use than demonstrated by school (Tomblin, Harrison, et al., 2015; Walker, McCreery, et al., 2015). The shift toward service provision in inclusive settings by school age may be a function of children's improved language abilities and/or the trend toward inclusion of students with mild to moderately severe hearing levels within general education settings (Blackorby & Knokey, 2006).
Of the CHH receiving intervention, nearly all were seen by a certified SLP and/or a teacher of CDHH on a regular basis. On average, intervention sessions for preschool-age children lasted approximately 36 min when seen by an SLP or 90 min with a teacher of CDHH and occurred 2–2.5 times per week. School-aged children received intervention 30 min/session when seen by an SLP or 47 min/session with a teacher of CDHH and occurred 1.7 times per week. Although sessions with a teacher of CDHH were longer than those provided by SLPs at both preschool and school age, this difference was notably larger at preschool. This may have been due to more participants receiving services from a teacher of CDHH in a specialized preschool setting.
Services for both age groups were provided either individually or both individually and in a group. Group-only service delivery was not a primary provision model for any setting or age. Representing less than 10% of the CHH participants, group services occurred most often in preschools for children with exceptional needs and school-age general education settings. Research is needed to address whether group therapy in these educational settings appropriately addresses the needs of CHH who do not have resource needs beyond speech and language, and it remains an empirical question whether frequency and context (individual vs. group intervention) influence outcomes for CHH.
Our second research question focused on whether or not there is a relationship between a child's hearing levels, language scores, and service receipt and setting. Previous research has shown that preschool children with all degrees of HL are at risk for language delays (Tomblin, Harrison, et al., 2015; Tomblin, Oleson, Ambrose, Walker, & Moeller, 2014; Vohr et al., 2012). Although this study found that school-age children with better hearing were less likely to receive services than those with greater degrees of HL, it is important to consider that children with mild HL may still exhibit delays compared with their peers with normal hearing (Walker, Holte, et al., 2015). These researchers found significant variance in the amount of time 5- and 7-year-old children with mild HL wore their hearing aids, and that higher amounts of daily hearing aid use predicted higher vocabulary and grammar abilities.
Regardless of hearing level, results indicate that children with better language abilities are less likely to receive services compared with those with lower language skills. In preschool, performance on global measures of receptive and expressive language and grammar differed between children with and without services, suggesting they may be sensitive indicators of children's intervention needs at this age. In elementary school, syntax, vocabulary, and articulation skills differed among children receiving services across settings. Of specific note, children receiving intervention at schools for CDHH performed below average across all language areas (i.e., global receptive/expressive, syntax, vocabulary, and articulation), whereas children receiving services at other locations performed in the low average range. Children with the lowest language abilities, especially at school age, are more likely to receive services in a specialized school setting. These results showed that the children with the greatest language intervention needs were in the most specialized/restrictive educational settings.
While there is a relationship between receipt of service and language ability, determining the exact nature of the relationship is complicated by factors that could influence both language and eligibility for quality intervention (e.g., family's socioeconomic status, availability of specialized programs for CDHH, concentration of qualified intervention providers in a geographic area). The CHH included in this study were all from homes in which at least one parent spoke English and none of the children had significant development disabilities in addition to their HL. Thus, the results presented here may not generalize to the wider population of CHH. Further research is needed to better explain how the presence of coexisting conditions, the language spoken in the home, and socioeconomic status influence the receipt and quality of services. These important questions were beyond the scope of the current investigation and our somewhat advantaged group of families. In addition, the influence of intensity and quality of intervention on outcomes for CHH remains unclear and is in need of further research.
The third goal of this study was to characterize the professionals working with the preschool- and school-age CHH in the OCHL study. Most of the children received services from an SLP and/or teacher of CDHH. Unlike the birth-to-3 period (Harrison et al., 2016), few early childhood educators, special educators, or other professionals provided communication services for preschool- and school-age CHH. This shift may reflect differing service delivery models from Part C to Part B services. The majority of CHH in the current study were served by SLPs and teachers of CDHH who had earned a master's degree. With the exception of a small group with certification as listening and spoken language specialists or who were dually certified as an SLP and a teacher of CDHH, most did not have additional certifications related to HL. Participation in continuing education relevant to working with CDHH was more frequently reported for SLPs (89%) compared with teachers of CDHH (60%), ranging from day-long in-service to several semester-long courses. SLPs may have pursued continuing education specific to working with CHH because it is an area where they often lack preprofessional preparation. Providers with more preprofessional or professional education regarding CDHH, whether a teacher of CDHH or SLP with listening and spoken language specialist certification, had a higher proportion of CDHH on their caseloads compared with providers with less preprofessional or professional preparation. It should be noted that some of the SLPs who participated in this study were employed in specialized centers for CDHH; thus, the high percentage of children on their caseloads may not be representative of SLPs who serve CDHH in general education settings.
Our fourth research question investigated whether provider background/preparation related to reported levels of comfort on skills specific to working with CHH. Based on previous research on birth-to-3 providers (Harrison et al., 2016), we expected that expertise would align with discipline-specific professional training. Teachers of CDHH and SLPs with dual certification reported higher levels of comfort on hearing and device-related knowledge and skills, and SLPs reported higher levels of comfort specifically in the area of speech. Although both SLPs and teachers of CDHH have specialized strengths when working with CHH, neither group claimed expertise with skills related to both device maintenance and speech/language, suggesting the value of interprofessional collaboration.
Similar to Harrison et al. (2016), experience working with CDHH makes a difference in provider's self-efficacy with hands-on device troubleshooting and promoting optimal audibility/listening with hearing aids. Both preschool- and school-age providers with a high percentage of CDHH on their caseloads and many years of professional experience reported being comfortable with device-specific skills, such as inserting earmolds, daily listening checks, using the Ling sounds, troubleshooting hearing aids, and using FM. As experience with the population increases, professionals may have opportunities to gain the relevant knowledge and skills to serve CHH. However, given that comfort was self-reported, it is unclear if years of experience is also related to quality of service provision, suggesting the need for further research.
It has been proposed that increased interprofessional training with audiologists is needed to support efficacy in troubleshooting hearing devices for SLPs and teachers of CDHH at both preschool- and school-age levels (Brackett, 1997; Nelson, Poole, & Muñoz, 2013; Richburg & Knickelbein, 2011). Our findings support that communication between audiologists and other service providers could be improved, especially for school-age SLPs, many of whom contact the audiologist only once or twice per year. The teachers of CDHH reported more frequent contact with audiologists compared with SLPs. This may be because they are more likely to be employed by specialized programs for CDHH that also employ educational audiologists.
Pediatric audiologists are suited to convey the importance of consistent hearing device use, monitoring use (i.e., data logging and journaling), and the influence that audibility has on communication development and speech perception, learning, and behavior in the classroom. Collaboration among professionals can facilitate individualized listening, speech, and language therapy and support classroom teachers in adapting teaching strategies for CDHH (Blair, EuDaly, & Benson, 1999). Further research is needed to identify barriers to communication and means of increasing collaboration between intervention providers (e.g., audiologists, SLPs, teachers of CDHHs, and educators) serving CHH.
Clinical Implications
Several clinical implications may be drawn from the results of the current study. First, providers varied by professional discipline in their level of comfort with age-appropriate treatment/intervention for CDHH. This suggests the need for interprofessional or continuing education focused on evaluating speech and language for teachers of CDHH or managing hearing technology for SLPs to ensure CHH are receiving optimal auditory access with properly functioning devices. Another option is to provide specialized interprofessional education that prepares SLPs, audiologists, and teachers to work with CDHH when graduate programs co-occur within the same institution. These complementary skill sets are both necessary in order to develop and assess progress toward Individualized Education Program goals.
Furthermore, it is important that service providers have specialized knowledge and skills in using appropriate assessment tools and methods to identify delays in language domains known to be at risk (e.g., phonology, grammar, and listening in noise) for CHH (Tomblin, Harrison, et al., 2015; Walker, McCreery, et al., 2015). As argued by the OCHL research team, reliance on norm-referenced measures rather than a comparison with peers or classmates with similar background characteristics to determine that a child has “caught up” may underestimate the support needs of CHH, especially in noisy classroom settings (Blair, Peterson, & Viehweg, 1985; Moeller et al., 2015; Moeller & Tomblin, 2015). Future research is needed to address whether children who do not have services have unmet needs, especially as they progress to more academically challenging grades.
When delays are identified, there is a need to provide intervention that addresses the unique resource needs of CHH. Compared with group service delivery, it is possible that individual services occur in quieter acoustic environments (Brackett, 1997), which may confer advantages, given that CHH require more audibility of speech to listen and learn. It remains an empirical question whether individual versus group intervention influences outcomes for CHH. Further research is required to confirm this hypothesis.
Encinas and Plante (2016) demonstrated that techniques such as auditory bombardment, provision of high linguistic variability in the input, and recasting resulted in reducing morpheme errors in children with cochlear implants. Evidence-based interventions like these can be applied in individual sessions to provide focused stimulation (higher rates of auditory-based practice and response) in an auditory environment that is conducive to learning for CHH. In terms of broader support needs, preschoolers may need more technical/equipment support than school-age children who are more apt to troubleshoot independently and report when devices malfunction (Kobylas, 2016). Older children may need different supports that help them become independent and responsible in regard to device care/use and to advocate for their listening and learning needs in the classroom.
For inexperienced providers (those with a low percentage of CDHH on their caseload or only a few years of experience working with CDHH), collaborative service delivery or training with partnering professionals (teachers of CDHH, SLP, audiologist) would be ideal to support best practice in serving preschool- and school-age CHH with their language and technology needs. An alternative would be to offer preprofessional cross-training or credentialing in order to share expertise across disciplines. This method of cross-training in graduate programs has been shown to be effective for students preparing to work with CDHH (Bondurant, Lartz, & Meehan, 2016) For university programs lacking staff to provide preprofessional cross-training opportunities, Pakulski (2011) described a service-learning model that pairs students with providers in the community as an effective, collaborative learning experience. In this way, professionals and educators may better support CHH in receiving needed educational resources.
In conclusion, the majority of CHH in the OCHL study received intervention services in preschool and early elementary school provided by certified SLPs and/or teachers of CDHH. Children most at risk of language delay and those with higher degrees of HL were likely to be enrolled in school services. In contrast, children with milder degrees of HL and those with better language abilities were less likely to be. Despite being well prepared to meet the expected standards in their preprofessional programs, some professionals providing services may not be knowledgeable or proficient in the skills needed to support the auditory and language development of CDHH. Ideally, providers working with CDHH should be skilled not only in managing devices and supporting auditory development but also in promoting complex language skills where children demonstrate delays. Our results indicate that, without specialized preprofessional or postgraduate training, providers are unlikely to report confidence in both of these areas, especially if they do not have experience working with CDHH.
Acknowledgments
The authors have no financial relationships relevant to this article to disclose. This work was supported by the National Institute on Deafness and Other Communication Disorders Grant 5 R01DC009560 awarded to the University of Iowa (co-PIs: J. Bruce Tomblin [University of Iowa] and Mary Pat Moeller [Boys Town National Research Hospital]). The content of this project is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Deafness and Other Communication Disorders or the National Institutes of Health. The authors are grateful to each of the families and professionals who participated in this study, as well as Barbara Peterson, who conducted the family interviews.
Funding Statement
The authors have no financial relationships relevant to this article to disclose. This work was supported by the National Institute on Deafness and Other Communication Disorders Grant 5 R01DC009560 awarded to the University of Iowa (co-PIs: J. Bruce Tomblin [University of Iowa] and Mary Pat Moeller [Boys Town National Research Hospital]).
References
- Ambrose S. E., Walker E. A., Unflat-Berry L. M., Oleson J. J., & Moeller M. P. (2015). Quantity and quality of caregiver's input to 18–month-old and 3-year-old children who are hard of hearing. Ear and Hearing, 36(Suppl. 1), 48S–59S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antia S. D., Jones P. B., Reed S., & Kreimeyer K. H. (2009). Academic status and progress of deaf and hard of hearing students in general education classrooms. Journal of Deaf Studies and Deaf Education, 14(3), 293–311. [DOI] [PubMed] [Google Scholar]
- Blackorby J., & Knokey A. M. (2006). A national profile of students with hearing impairments in elementary and middle school: A special topic report from the Special Education Elementary Longitudinal Study. Menlo Park, CA: SRI. [Google Scholar]
- Blair J. C., EuDaly M., & Benson P. V. A. (1999). The effectiveness of audiologists' information sources for classroom teachers. Language, Speech, and Hearing Services in Schools, 30(2), 173–182. [DOI] [PubMed] [Google Scholar]
- Blair J. C., Peterson M. D., & Viehweg S. H. (1985). The effect of mild hearing loss on academic performance of young school-age children. The Volta Review, 87(2), 87–93. [Google Scholar]
- Bondurant L., Lartz M., & Meehan T. (November, 2016). Preparing audiologists & SLPs to collaborate in early intervention for children with hearing loss. Poster presented at the annual convention of the American Speech-Language-Hearing Association, Philadelphia, PA. [Google Scholar]
- Brackett D. (1997). Intervention for children with hearing impairment in general education settings. Language, Speech, and Hearing Services in Schools, 28(4), 355–361. [DOI] [PubMed] [Google Scholar]
- Carrow-Woolfolk E. (1999). Comprehensive Assessment of Spoken Language. Circle Pines, MN: AGS. [Google Scholar]
- Compton M. V., Tucker D. A., & Flynn P. F. (2009). Preparation and perceptions of speech-language pathologists working with children with cochlear implants. Communication Disorders Quarterly, 30(3), 142–154. [Google Scholar]
- Davis J. M., Elfenbein J., Schum R., & Bentler R. A. (1986). Effects of mild and moderate hearing impairments on language, educational, and psychosocial behavior of children. Journal of Speech and Hearing Disorders, 51(1), 53–62. [DOI] [PubMed] [Google Scholar]
- Education for All Handicapped Children Act, 20 U.S.C.S. § 140 et seq. (1975).
- Encinas D., & Plante E. (2016). Feasibility of a recasting and auditory bombardment treatment with young cochlear implant users. Language, Speech, and Hearing Services in Schools, 47(2), 157–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman R., & Fristoe M. (1999). Goldman-Fristoe Test of Articulation–Second Edition. Circle Pines, MN: AGS. [Google Scholar]
- Harrison M., Page T. A., Oleson J. J., Spratford M., Unflat-Berry L., Peterson B., … Moeller M. P. (2016). Factors affecting early services for children who are hard of hearing. Language, Speech, and Hearing Services in Schools, 47(1), 16–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebbler K., Levin J., Perez M., Lam I. M., & Chambers J. G. (2009). Expenditures for early intervention services. Infants and Young Children, 22(2), 76–86. [Google Scholar]
- Houston K. T., & Perigoe C. (2010). Speech-language pathologists: Vital listening and spoken language professionals. The Volta Review, 110(2), 219–230. [Google Scholar]
- Judge P. D., Jorgensen E., Lopez-Vazquez M., Roush P., Page T. A., Moeller M. P., … Buchman C. (2018). Medical referral patterns and etiologies for children with mild to severe hearing loss. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed]
- Kobylas M. M. (2016). Is this thing on? An investigation of school-based speech-language pathologists' knowledge of hearing technology (Senior independent study thesis 7151). Retrieved from http://openworks.wooster.edu/independentstudy/7151
- Ling D. (1989). Foundations of spoken language for the hearing-impaired child. Washington, DC: Alexander Graham Bell Association for the Deaf. [Google Scholar]
- Moeller M. P., & Tomblin J. B. (2015). An introduction to the Outcomes of Children with Hearing Loss study. Ear and Hearing, 36(Suppl. 1), 4S–13S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller M. P., Tomblin J. B., & OCHL Collaboration. (2015). Epilogue: Conclusions and implications for research and practice. Ear and Hearing, 36(Suppl. 1), 92S–98S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moseley M. J., Mashie J. J., Brandt F. D., & Fleming L. F. (1994). A survey of professionals delivering speech-language services to children with hearing loss. Language, Speech, and Hearing Services in Schools, 25, 100–104. [Google Scholar]
- Nelson L. H., Poole B., & Muñoz K. (2013). Preschool teachers' perception and use of hearing assistive technology in educational settings. Language, Speech, and Hearing Services in Schools, 44(3), 239–251. [DOI] [PubMed] [Google Scholar]
- Pakulski L. A. (2011). Addressing qualified personnel shortages for children who are deaf or hard of hearing with an interdisciplinary service learning program. American Journal of Audiology, 20(2), S203–S219. [DOI] [PubMed] [Google Scholar]
- Research Support and International Affairs. (2014, September). Regional and national summary report of data from 2013-2014 Annual Survey of Deaf and Hard of Hearing Children and Youth (Report). Washington, DC: Research Support and International Affairs. [Google Scholar]
- Richburg C. M., & Knickelbein B. A. (2011). Educational audiologists: Their access, benefit, and collaborative assistance to speech-language pathologists in schools. Language, Speech, and Hearing Services in the Schools, 42(4), 444–460. [DOI] [PubMed] [Google Scholar]
- Semel E., Wiig E., & Secord W. (2004). Clinical Evaluation of Language Fundamentals–Fourth Edition. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Sininger Y. S., Grimes A., & Christensen E. (2010). Auditory development in early amplified children: Factors influencing auditory-based communication outcomes in children with hearing loss. Ear and Hearing, 31(2), 166–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SRI International. (2000). National Early Intervention Longitudinal Study (NEILS). Menlo Park, CA: SRI. [Google Scholar]
- Tomblin J. B., Harrison M., Ambrose S. E., Walker E. W., Oleson J. J., & Moeller M. P. (2015). Language outcomes in young children with mild to severe hearing loss. Ear and Hearing, 36(Suppl. 1), 76S–91S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin J. B., Oleson J. J., Ambrose S., Walker E., & Moeller M. P. (2014). The influence of hearing aids on the speech and language development of children with hearing loss. JAMA Otolaryngology—Head & Neck Surgery, 140(5), 403–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin J. B., Walker E. W., McCreery R. W., Arenas R. M., Harrison M., & Moeller M. P. (2015). Outcomes of children with hearing loss: Data collection and methods. Ear and Hearing, 36(Suppl. 1), 14S–23S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2016). Educational attainment in the United States: 2016. Retrieved from https://www.census.gov/data/tables/2016/demo/education-attainment/cps-detailed-tables.html
- Vohr B., Topol D., Girard N., Pierre L. S., Watson V., & Tucker R. (2012). Language outcomes and service provision of preschool children with congenital hearing loss. Early Human Development, 88(7), 493–498. [DOI] [PubMed] [Google Scholar]
- Walker E. A., Holte L., McCreery R. W., Spratford M., Page T. A., & Moeller M. P. (2015). The influence of hearing aid use on outcomes of children with mild hearing loss. Journal of Speech, Language, and Hearing Research, 58(5), 1611–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker E. A., McCreery R. W., Spratford M., Oleson J. J., Van Buren J., Bentler R., Roush P., & Moeller M. P. (2015). Trends and predictors of longitudinal hearing aid use for children who are hard of hearing. Ear and Hearing, 36(Suppl. 1), 38S–47S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. (2002). The Wechsler Preschool and Primary Scale of Intelligence–Third Edition. San Antonio, TX: Harcourt Assessment. [Google Scholar]
- Wechsler D., & Hsiao-Pin C. (2011). Wechsler Abbreviated Scale of Intelligence–Second Edition. San Antonio, TX: Pearson. [Google Scholar]