Abstract
Objective:
The primary outcome of this study is to identify characteristics of study participants in a large opioid treatment program (OTP) for opioid use disorder (OUD) who used take-home naloxone to perform 1 or more opioid overdose (OD) reversal(s) in the community.
Methods:
This 6-month prospective cohort study provided take-home naloxone and opioid OD education for 287 study participants with OUD. Characteristics associated with use of the take-home naloxone were determined from among 16 variables using multivariable logistic regression.
Results:
The study participants who had greater odds of using the take-home naloxone to perform OD reversals, compared to those who did not use the take-home naloxone, (a) received emergency room care themselves for OD (OR = 4.89, 95% CI 1.54–15.52, P = 0.007), (b) previously witnessed someone else OD (OR = 5.67, 95% CI 1.24–25.87, P = 0.025), (c) tested positive for 2 or more illicit substances at their 6-month urine analysis (OR = 5.26, 95% CI 1.58–17.54, P = 0.007) or were missing their 6-month urine analysis (OR = 3.46, 95% CI 1.42–8.43, P = 0.006). In addition, they had greater odds of being (d) less than 30 years old (OR = 2.80, 95% CI 1.02–7.66, P = 0.045), and (e) Hispanic (OR = 3.98, 95% CI 1.41–11.21, P = 0.009).
Conclusions:
This study prospectively identified several characteristics of patients enrolled in an OTP with increased odds of using take-home naloxone in their social networks. Future harm reduction efforts may benefit by using targeted characteristics to identify those most likely to use naloxone in their communities.
Keywords: characteristics, harm reduction, naloxone, opioid, overdose
The opioid crisis is a US public health epidemic (U.S. Department of Health and Human Services, 2018). Drug overdose (OD) deaths exceed all other causes of injury including motor vehicle accidents and gun-related violence (Rudd et al., 2016). The Centers for Disease Control and Prevention (CDC) estimates there are 91 US deaths per day involving opioids. Approximately 3 million Americans suffer from opioid use disorder (OUD), a condition manifested by escalating physical and psychological cravings for opioid analgesics (Schuckit, 2016).
People begin using opioid analgesics for many different reasons: some initially obtain prescription opioids from a medical provider for a diagnosis of acute or chronic pain. Others may begin to use prescription opioids from a friend, a relative or a stranger for the psychoactive feeling of well-being (Schuckit, 2016). Ultimately, the majority of people who develop OUD will switch to heroin because of the lower cost and the accessibility (Cicero et al., 2014; Jones et al., 2015). Polydrug use among people who use heroin, especially the use of alcohol and benzodiazepines is an important contributor to drug OD (Darke and Hall, 2003).
Although self-administration of naloxone is not possible during an OD event, people who OD, especially from heroin, are usually not alone (Galea et al., 2006). Community members present, when trained and supplied with naloxone, can serve as first responders by performing OD reversals on others in their community (Wagner et al., 2010). Community members who perform OD reversals are often reluctant to call emergency medical services due to fear of police (Galea et al., 2006). Other barriers to naloxone access include cost, inadequate first responder training, and lengthy response times, especially in rural communities (Gupta et al., 2016; Rural Health Information Hub, 2016).
This prospective study is an analysis of patients with an OUD treated at an opioid treatment program (OTP) in Albuquerque, New Mexico. Using logistic regression, this study examines characteristics of study participants who use take-home naloxone to perform opioid OD reversal(s) in the community—as compared to study participants who did not use take-home naloxone.
The authors hypothesize that study participants who remain socially connected to people who inject drugs (PWID) may be more likely to perform OD reversals than those who are not socially connected with PWID. It is the authors’ contention that identifying characteristics of those people who might perform OD reversals on others in the community would provide a targeted strategic response to the opioid crisis.
METHODS
Study Population
This study used information collected from patients with a confirmed diagnosis of opioid substance use disorder (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition) being treated at University of New Mexico (UNM) Addiction and Substance Abuse Program (ASAP) (Katzman et al., 2018). Patients eligible for study inclusion were those treated with methadone, buprenorphine or naltrexone between April 4 and October 5, 2016, ages 18 years or older, who were not allergic to naloxone or its inactive ingredients (eg, buffering agents). During the 6-month period, 287 patients were enrolled, and 251 study participants completed their 3- and 6-month follow-up interviews. Forty-four study participants reported performing 65 OD reversals in the community during this 6-month time period. Thirty-six participants were lost to follow-up by the end of 6 months (Fig. 1).
FIGURE 1.
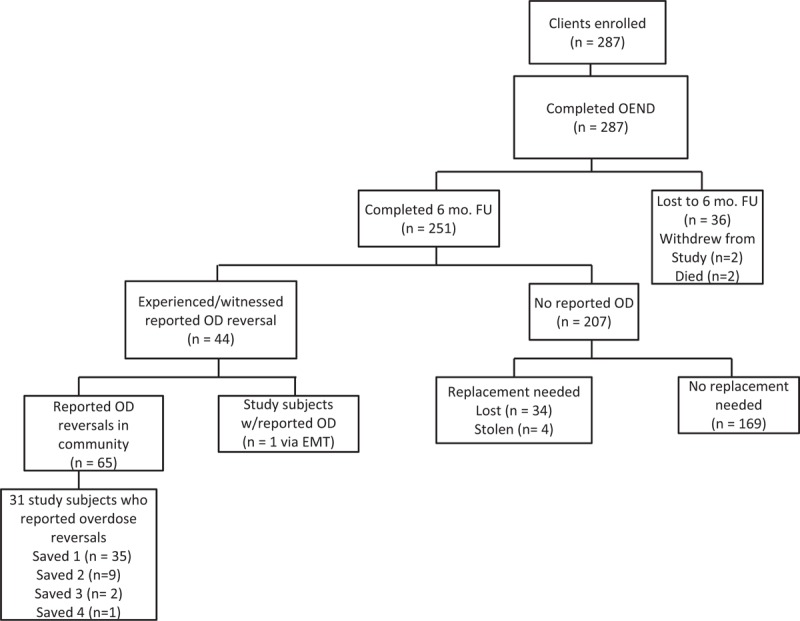
Study participant flow diagram: 6-month follow-up April 4 to October 5, 2016 (EMT, emergency medical technician; FU, follow-up; OD, overdose; OEND, Overdose education and naloxone distribution).
Study Overview
This study analyzes a prospective cohort of study participants with OUD at the ASAP enrolled between April 4 and October 5, 2016. Logistic regression was used to identify characteristics of the OTP participants that reported using naloxone to perform OD reversals on others in their communities for future targeted naloxone provision practices. The authors selected multiple characteristics for analysis based on demographics, study participant personal experiences with OD, routine urine toxicological screens, and participant comorbidities.
Addiction and Substance Abuse Program
Participants enrolled in this study were patients at the ASAP, an OTP for adults, adolescents, and pregnant women receiving Medication-Assisted Treatment (MAT). Because ASAP provides the only comprehensive treatment to women with addictive disorders, ASAP receives referrals throughout New Mexico for pregnant women with OUD. Treating approximately 600 patients per year, 64% of ASAP enrollees on MAT are women, and 11% are pregnant (Katzman et al., 2018).
Study Intervention
Each study participant volunteered to meet with the study coordinator at ASAP for 15 to 20 minutes to determine eligibility and receive opioid OD education. Recruitment for the study involved placing investigational review board-approved notices in the main lobby of the OTP. The study participants received information regarding recognition of an opioid OD as well as appropriate responses such as calling 911, rescue breathing, and staying with the person until EMS arrived. Study participants were then introduced to “Evzio,” an Food and Drug Administration-approved naloxone auto-injector kit and instructed on its use with the help of the “talking trainer” included with the kit (kaléo Inc., 2014). Participants demonstrated proper kit use to the study coordinator. At the end of the enrollment visit, 1 naloxone auto-injector kit (2 naloxone auto-injectors and 1 training auto-injector per kit) was given to each study participant. Every participant was instructed to teach their household members proper indication and use of the naloxone kit. Study participants engaged in a 10- to 15-minute follow-up interview at both 3 and 6 months to asses any new experiences with opioid ODs since study enrollment.
Outcome Variables
The outcome variable is the yes or no response to whether the study participant administered naloxone to perform 1 or more OD reversals. These yes or no responses were recorded at each participant's 3- and 6-month follow-up visits. Participants could also return for a replacement kit at other times during the 6-month period. Reasons for replacement included: having used the kit to perform an OD reversal, or if the kit was lost or stolen. Yes or no responses were also recorded during these intervening visits.
Explanatory Variables
Variables analyzed included demographic characteristics, personal experiences with OD, routine urine toxicological results, and comorbidities. Information was gathered from patient responses as well as medical records.
Patient Response Variables
Variables were age, county, companion presence for naloxone training, education, gender, having overdosed at least once, race/ethnicity, or having witnessed an OD event.
Medical Record Variables
Variables included opioid replacement therapy (ORT) type, prior emergency room care for OD, having been treated for a psychiatric illness or history of suicide (International Classification of Diseases, Ninth Revision [ICD-9]: V62.84), diagnosis of post-traumatic stress disorder (PTSD, ICD-9: 309.81), diagnosis of depressive disorder (ICD-9: 311), diagnosis of hepatitis C (ICD-9: 070.54), recent incarceration, and having no urine toxicological screens or positive urine toxicological screens for 1 or more of the following substances: amphetamines, barbiturates, benzodiazepines, cocaine, and opioids including buprenorphine. Benzodiazepines detected in the urine toxicological screen included chlordiazepixide, clonazepam, demoxepam, desalkylflurazepam, diazepam, and n-desmethyldiazepam. Opioids detected in the urine toxicological screen included codeine, hydrocodone, hydromorphone, morphine, and morphine glucuronide. Study participants were only tested for buprenorphine if their ORT consisted of this medication.
Statistical Analyses
The distribution of each variable was tabulated. Using logistic regression, variable relationships were examined for identification of potential confounders and effect modifiers. Multivariate logistic regression modeling with backward selection at P < 0.05 was used for final model selection of characteristics significantly associated with using naloxone to reverse drug OD in others. The relationship to the study participants of community members who were given naloxone, whether 911 was called, and the number of doses used, were also tabulated. Significant differences in all variable distributions, except urine toxicological screens, between study participants followed for 6 months and those lost to follow-up were examined using chi-squared tests. Analyses were performed using Stata 12 (Stata Corp, College Station, TX).
Institutional Review Board and National Institutes of Health Approval
Institutional Review Board (IRB) approval for this study was obtained through the UNM Human Research Protections Office on March 16, 2016 (ID# 15–616). This study was filed with the National Institutes of Health (NIH) clinical trials on December 21, 2015 (NCT #02669901) with a certificate of confidentiality recorded at NIH.
RESULTS
Baseline Demographics of Study Participants
Table 1 shows the variable distributions of the 251 study participants followed for 6 months. Regarding their demographic characteristics: most were less than 30 years old, female, identified as Hispanic/white, had education less than a high school diploma or general education diploma, and lived in Bernalillo County, consistent with the ASAP patient population. Regarding study participants’ personal experience with opioid OD events: almost half had experienced a prior personal OD event while a few had confirmed emergency room care for OD. Most, however, had witnessed an OD event. Regarding routine urine toxicological results: most study participants were positive for their MAT type, while about half were negative for other illicit substances.
TABLE 1.
Baseline Characteristics of Study Participants
| Patient Response Variables | |||
| Variables | Used Naloxone | Did NOT Use Naloxone | Total |
| Naloxone use: outcome | 44 (18%) | 207 (82%) | 251 (100%) |
| Age, y | |||
| 18–29 | 21 (47.7%) | 82 (39.6%) | 103 (41.0%) |
| 30–44 | 16 (36.4%) | 58 (28.0%) | 74 (29.5%) |
| 45–79 | 7 (15.9%) | 67 (32.4%) | 74 (29.5%) |
| County | |||
| Bernalillo | 38 (86.4%) | 180 (87.0%) | 218 (86.9%) |
| Sandoval | 1 (2.3%) | 12 (5.8%) | 13 (5.2%) |
| Socorro | 1 (2.3%) | 4 (1.9%) | 5 (2.0%) |
| Valencia | 2 (4.5%) | 4 (1.9%) | 6 (2.4%) |
| Not Reported | 2 (4.5%) | 7 (3.4%) | 9 (3.6%) |
| Companion present for naloxone training | |||
| Yes | 5 (11.4%) | 22 (10.6%) | 27 (10.8%) |
| No | 39 (88.6%) | 184 (88.9%) | 223 (88.8%) |
| Not reported | 0 (0%) | 1 (0.5%) | 1 (0.4%) |
| Education | |||
| <High school graduate or GED | 22 (50.0%) | 77 (37.2%) | 99 (39.4%) |
| High school graduate or GED | 13 (29.5%) | 57 (27.5%) | 70 (27.9%) |
| Some college or college degree | 9 (20.5%) | 73 (35.3%) | 82 (32.7%) |
| Gender | |||
| Female | 32 (72.7%) | 146 (70.5%) | 178 (70.9%) |
| Male | 12 (27.3%) | 61 (29.5%) | 73 (29.1%) |
| Overdose at least once | |||
| No | 23 (52.3%) | 114 (55.1%) | 137 (54.6%) |
| Yes | 21 (47.7%) | 93 (44.9%) | 114 (45.4%) |
| Race/ethnicity | |||
| American Indian/Alaska Native | 4 (9.1%) | 9 (4.3%) | 13 (5.2%) |
| Asian | 0 (0%) | 1 (0.5%) | 1 (0.4%) |
| Black or African American | 0 (0%) | 3 (1.4%) | 3 (1.2%) |
| Not reported | 1 (2.3%) | 7 (3.4%) | 8 (3.2%) |
| Hispanic/white | 33 (75.0%) | 122 (58.9%) | 155 (61.8%) |
| Non-Hispanic/white | 6 (13.6%) | 65 (31.4%) | 71 (28.3%) |
| Witnessed someone else overdose | |||
| No | 2 (4.5%) | 43 (20.8%) | 45 (17.9%) |
| Yes | 42 (95.5%) | 164 (79.2%) | 206 (82.1%) |
| Medical Record Variables | |||
| Variables | Used Naloxone | Did NOT Use Naloxone | Total |
| Opioid replacement therapy | |||
| Methadone | 38 (86.4%) | 160 (77.3%) | 198 (78.9%) |
| Buprenorphine | 5 (11.4%) | 38 (18.4%) | 43 (17.1%) |
| Naltrexone | 1 (2.3%) | 4 (1.9%) | 5 (2.0%) |
| None | 0 (0%) | 5 (2.4%) | 5 (2.0%) |
| Emergency room care for overdose | |||
| No | 37 (84.1%) | 195 (94.2%) | 232 (92.4%) |
| Yes | 7 (15.9%) | 12 (5.8%) | 19 (7.6%) |
| Psychiatric illness/suicide | |||
| No | 23 (52.3%) | 103 (49.8%) | 126 (50.2%) |
| Yes | 21 (47.7%) | 104 (50.2%) | 125 (49.8%) |
| PTSD history | |||
| No | 35 (79.5%) | 168 (81.2%) | 203 (80.9%) |
| Yes | 9 (20.5%) | 39 (18.8%) | 48 (19.1%) |
| Depressive disorder history | |||
| No | 31 (70.5%) | 163 (78.7%) | 194 (77.3%) |
| Yes | 13 (29.5%) | 44 (21.3%) | 57 (22.7%) |
| Hepatitis C diagnosis | |||
| No | 33 (75.0%) | 160 (77.3%) | 193 (76.9%) |
| Yes | 11 (25.0%) | 47 (22.7%) | 58 (23.1%) |
| Recent incarceration | |||
| No | 40 (90.9%) | 202 (97.6%) | 242 (96.4%) |
| Yes | 4 (9.1%) | 5 (2.4%) | 9 (3.6%) |
| Urine analysis | |||
| No illicit substances | 15 (34.1%) | 118 (57.0%) | 133 (53.0%) |
| Single substance | 8 (18.2%) | 40 (19.3%) | 48 (19.1%) |
| Two or more substances | 7 (15.9%) | 12 (5.8%) | 19 (7.6%) |
| Not Tested | 14 (31.8%) | 37 (17.9%) | 51 (20.3%) |
Regarding other vulnerabilities or comorbidities: a few of the study participants were recently released from incarceration and some had hepatitis C, PTSD, or a depressive disorder. However, half had previously received treatment for 1 or more severe psychiatric illnesses including depression, bi-polar disorder, schizophrenia, or suicidal ideation (Table 1).
Opioid replacement therapy type was the only variable significantly different (P = 0.002) in distribution between study participants followed for 6 months and those lost to follow-up. Of the 36 lost to follow-up had a greater ratio of patients on buprenorphine to methadone (0.84) compared to those who completed the study for 6 months (0.22). Those lost to follow-up had the following distribution of ORT: 18 (50%) methadone, 15 (42%) buprenorphine, 2 (5%) naltrexone, and 1 (3%) none (Table 1 data illustrates study population who completed 6-month follow up).
Of the 65 community members who were treated with naloxone by the 44 study participants, the majority were friends or family members of the study participants. Almost half of the study participants had 911 called at the time of the naloxone reversal, and more than half had used more than 1 dose of naloxone for the reversal (Table 2).
TABLE 2.
Variable Distributions Regarding Community Members Reversed with the Prescribed Naloxone
| VARIABLE | n | % |
| Number of naloxone doses used | ||
| One | 28 | 43% |
| Two | 35 | 54% |
| Three | 2 | 3% |
| 911 was called | ||
| Yes | 30 | 46% |
| No | 35 | 54% |
| Relationship to study participant | ||
| Acquaintance | 5 | 8% |
| Family member | 11 | 17% |
| Friend | 36 | 55% |
| Significant other | 4 | 6% |
| Stranger | 9 | 14% |
Logistic regression analyses for identification of potential confounders and effect modifiers resulted in education as a potential confounder and no potential effect modifiers. Analyses of the associations between the 16 explanatory variables with the outcome of whether or not naloxone was used to reverse an opioid OD event in another, resulted in 6 variables significantly (P < 0.050) associated with use of the take-home naloxone (Table 3).
TABLE 3.
Logistic Regression between Each Explanatory Variable and Use of Naloxone
| Logistic Regression between Each Explanatory Variable and Use of Naloxone | Final Model (n = 247) | ||||||
| Variable | OR | (95% CI) | P | OR | (95% CI) | P | |
| Urine analysis | + Single substance | 1.57 | (0.62–3.99) | 0.340 | 1.45 | (0.54–3.98) | 0.448 |
| + Two or more substances | 4.59 | (1.56–13.46) | 0.006 | 5.26 | (1.58–17.54) | 0.007 | |
| Not tested | 2.98 | (1.32–6.74) | 0.009 | 3.46 | (1.42–8.43) | 0.006 | |
| Negative all substances | ref | ref | |||||
| ER care for intoxication | Yes | 3.07 | (1.14–8.33) | 0.027 | 4.89 | (1.54–15.52) | 0.007 |
| No | ref | ref | |||||
| Race/ethnicity | Am. Indian/Alaska Native | 4.81 | (1.14–20.41) | 0.033 | 5.09 | (0.96–27.4) | 0.056 |
| Not REPORTED | 1.55 | (0.16–14.77) | 0.704 | 1.37 | (0.13–14.87) | 0.797 | |
| Hispanic/white | 2.93 | (1.17–7.36) | 0.022 | 3.98 | (1.41–11.21) | 0.009 | |
| Non-Hispanic/white | ref | ref | |||||
| Witnessed someone OD | Yes | 5.51 | (1.28–23.66) | 0.022 | 5.67 | (1.24–25.87) | 0.025 |
| No | ref | ref | |||||
| Age, y | 18–29 | 2.45 | (0.98–6.12) | 0.055 | 2.80 | (1.02–7.66) | 0.045 |
| 30–44 | 2.64 | (1.02–6.86) | 0.046 | 2.82 | (1.00–7.95) | 0.050 | |
| 45–79 | ref | ref | |||||
| Recent incarceration | Yes | 4.04 | (1.04–15.71) | 0.044 | |||
| No | ref | ||||||
| Education | <HS grad/GED | 2.31 | (1.00–5.36) | 0.050 | |||
| HS Grad/GED | 1.85 | (0.47–4.63) | 0.189 | ||||
| Some College or Degree | ref | ||||||
| Depressive disorder history | Yes | 1.55 | (0.75–3.22) | 0.236 | |||
| No | ref | ||||||
| ORT type | Buprenorphine | 0.55 | (0.20–1.50) | 0.246 | |||
| Naltrexone | 1.05 | (0.11–9.69) | 0.964 | ||||
| Methadone | ref | ||||||
| County | Sandoval | 0.39 | (0.05–3.13) | 0.379 | |||
| Socorro | 1.18 | (0.13–10.89) | 0.881 | ||||
| Valencia | 2.36 | (0.42–13.40) | 0.330 | ||||
| Bernalillo | ref | ||||||
| OD at least once | Yes | 1.12 | (0.58–2.15) | 0.735 | |||
| No | ref | ||||||
| Hepatitis C diagnosis | Yes | 1.13 | (0.53–2.42) | 0.743 | |||
| No | ref | ||||||
| Psychiatric illness/suicidal ideation | Yes | 0.98 | (0.47–1.73) | 0.762 | |||
| No | ref | ||||||
| Gender | Male | 0.90 | (0.43–1.86) | 0.771 | |||
| Female | ref | ||||||
| PTSD history | Yes | 1.11 | (0.49–2.49) | 0.805 | |||
| No | ref | ||||||
| Companion present for naloxone training | No | 0.93 | (0.33–2.61) | 0.894 | |||
| Yes | Ref | ||||||
95% CI, 95% confidence interval; OR, odds ratio.
Final multivariate model selection resulted in a model with 5 significant explanatory variables. The significant associations with the outcome included being 29 years of age or younger, being Hispanic/white, reporting receiving previous emergency room care for OD, reporting previously witnessing someone OD, and being positive for 2 or more substances in their 6-month urine toxicology screens. These associations had odds ratio point estimates ranging from 2.80 to 5.67 indicating increased odds of using naloxone compared to the reference categories. Study participants in the final selected model included 247 of the 251 6-month follow-up participants with complete records for all 16 explanatory variables included in the initial full model. The 4 study participants not included in the final model were dropped due to very low numbers in the categories of race/ethnicity. Odds ratios in the final selected multivariate logistic regression model listed in Table 3 are unadjusted for education level as differences in the adjusted and unadjusted models were slight.
DISCUSSION
Results from our previous 3-month study suggested that providing opioid OD education and take-home naloxone in an OTP setting may reduce deaths from opioid ODs in others (Katzman et al., 2018). This 6-month prospective cohort study, with an 87% study participant completion rate, evaluated characteristics of those performing OD reversals in the community. Study participants with greater odds of using the take-home naloxone to reverse OD in others were (a) younger than 30 years, (b) Hispanic, (c) had personal experience of emergency room care for OD, (d) had previously witnessed others who have overdosed, and (e) had positive urine toxicology screens for 2 or more illicit substances or (f) no urine toxicology screens.
Urine Toxicology Screens
These urine toxicology results indicate patients who are performing OD reversals in the community tend to have positive or missing urine toxicology screens. This suggests that these study participants are using illicit substances regularly despite receiving MAT. Persistent illegal polydrug use in these study participants may indicate their continued social connectedness to those at high risk for opioid OD. Study participants performed OD reversals on someone they knew 86% of the time, whereas only 14% of the reported OD reversals were performed on a stranger. These findings are in accordance with our hypothesis that those who test positive for urine toxicological screenings may be more connected to PWID and, thus, may be more likely to witness and perform OD reversals on others in their communities.
Only 5 participants (<2%) in this study were prescribed opioid analgesics from a clinician for acute pain, such as a broken bone or postsurgical pain during the study period. In addition, 10 participants (<4%) were prescribed benzodiazepines for anxiety disorders. This suggests that the majority of positive urine toxicological screens are consistent with illicit use.
Witness Overdose in Others
Our study suggests that study participants who reported witnessing others OD in the past have a greater chance of performing an OD in the community. Other recent studies also verify similar characteristics for those performing OD reversals with naloxone. In a study of people receiving take-home naloxone at a San Francisco community-based drug education and naloxone distribution program, people with greater odds of using the naloxone to reverse ODs were those people who witnessed OD in others and who had recently used illicit drugs (Rowe et al., 2015). In an urban New York study of PWID, those found to have greater odds of performing opioid OD reversals in the community were younger, had previously experienced an OD, and had recently experienced withdrawal symptoms (Coffin et al., 2007). The similarity of characteristics of people both at greater odds of personal OD and greater odds of use of take-home naloxone in our study (ie, younger age, having experienced previous OD and current drug use) is not surprising due to social connectedness in those who use illicit substances.
Women and Hispanic Whites in Study Population
This study had a large percentage of participants identified as women (71%) and as Hispanic whites (62%) in the study population. These percentages are not statistically different from the ASAP population. The high percentage of women treated at ASAP is because pregnant women with OUD, and women with newborns with OUD, are given priority access to enroll as a patient in this safety-net clinic. The racial diversity of this clinic population is consistent with the diversity of New Mexico. Being Hispanic was associated with increased odds of performing OD reversals in this study; however, gender was not associated with increased odds of performing OD reversals.
Ethnicity as Social Connectedness
In this study, the associations between Hispanic/white with increased naloxone use may reflect community structure uniqueness. The UNM ASAP and its surrounding community both have majority Hispanic/white populations. The surrounding community of Albuquerque, New Mexico also has a large American Indian community. In this study, being American Indian/Alaskan Native was associated with use of naloxone in the logistic regression final model at P = 0.056. While not statistically significant, this result is based on a relatively low number (13) of American Indian/Alaskan Natives in the study population.
The authors recognize the unique social structure to this study community and realize that other communities around the nation will have similar uniqueness with different ethnic/racial groupings. While we found that Hispanic/white study participants had greater odds of performing OD reversals in our community, other regions may easily find different results depending on their demographics. Our study supports the broader idea that racial/ethnic identity may be an important consideration in take-home naloxone distribution.
Number of Naloxone Doses Given and 911 Called
Of the 65 reported ODs performed, 43% required 1 dose of naloxone, 54% required 2 doses of naloxone and 3% (2 cases) required 3 doses of naloxone. In the 2 cases which needed a third dose of naloxone, the third dose was supplied once by the paramedics when 911 was called, and in the second case, another community bystander had a naloxone kit available. All community members administered naloxone by study participants survived, and all ODs were reported to be due to heroin.
While the data in Table 2 regarding the study subjects who performed OD reversals in the community is patient self-reported, the authors believe this information to be accurate data. The study subjects who perform OD reversals come back to the clinic several times per week for their opioid replacement therapy dosing, and the reporting of the data is felt to be timely and authentic.
The frequency with which 911 was called in our study is similar to other naloxone studies (Koester et al., 2017). In our study, emergency services was called 46% of the time by the study participant performing the OD reversal in the community. Much naloxone literature support the idea that emergency services is contacted less often than needed due to fear of incrimination, the victim awakening, long emergency response time, etc. This is despite the fact that most PWID are aware of the Good Samaritan Law, which is now statute in most states in the US. (Koester et al., 2017).
Limitations
Social Connectedness and Privacy
This study did not directly measure social connectedness between study participants and people who inject drugs, such as the number of partners, friends or acquaintances, perceived social support or time spent with PWID. Because of Health Insurance Portability and Accountability Act (HIPAA), the study was not able to gather protected patient information about the community members who had overdosed. Further investigations may be important to better understand social connectedness and naloxone provision and training practices.
Research demonstrates that education on opioid OD and naloxone distribution significantly reduces opioid OD deaths among OUD patients in active treatment and their social contacts (Doe-Simkins et al., 2014; Fairbairn et al., 2017). Therefore, if naloxone is accessible, more patients treated in an OTP setting can perform OD reversals in the community (Maxwell et al., 2006; Wagner et al., 2014). If social connectedness increases the chance for OD reversals to be performed in the community, then peer trainers in the community may provide the needed harm reduction benefit to people who use drugs together (Marshall et al., 2017) (see Table 2).
Overdose Reversal and Privacy
It should also be noted that when study participants performed an OD reversal in the community, this was a self-report. The study participant gave this information directly to the research coordinator who collected the data. Our study participants reported 38 naloxone kits as “lost/stolen”. It is possible that some of these kits reported as “lost/stolen” may, in fact, have been used for an OD reversal on a community member or the study participant him/herself. However, it is not possible to know the exact percentage of naloxone kits being used to perform OD reversals.
Urine Toxicology Screen Result Limitations
Although we know that the number of patients using prescribed opioids for acute pain (e.g., post-dental procedure), and prescribed benzodiazepines for anxiety was low, future studies will help to elucidate the meaning of these illicit urine toxicology screens and the benefit of providing take-home naloxone to these patients.
Lost to Follow-up
While 36 study participants were lost to follow-up, our study had an excellent 87% completion rate. Two study participants died; however, neither participant death was suspected to be opioid-related.
CONCLUSIONS
Our prior study (Katzman et al., 2018) suggests that providing opioid OD education and take-home naloxone to OTP patients can significantly increase OD reversals in the community. In this study, characteristics of OUD patients with significantly greater odds of performing naloxone OD reversals included: younger age, previously witnessing an opioid OD, receiving emergency room care for OD and having positive urine toxicology screens. By targeting certain patients based on their characteristics, and supplying this patient population with additional support, OD reversals may be increased substantially more in the community. It is possible that this targeted subset of patients may be interested to be trained as “harm reduction peer educators” in their community. This may help to further reduce opioid OD deaths and bridge the gap between clinical and public health efforts related to naloxone distribution.
The findings in this analysis may differ in other regions of the US, or internationally. Because our findings seem to be partly dependent on social variables and connectivity, it may be valuable for other regions around the country to investigate their own OTP populations. They may discover which characteristics increase likelihood of people performing OD reversals in their community.
In future studies, we plan to ask study participants ethnographic, qualitative interview questions regarding their thoughts and feelings surrounding performing OD reversals.
Acknowledgments
The authors are grateful to kaléo, Inc for study support. The authors would also like to thank Kristine Tollestrup, PhD, Kim Page, PhD, Chamron Martin, and the staff and providers at ASAP for their assistance with the study and manuscript.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- Cicero TJ, Ellis MS, Surratt HL, et al. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry 2014; 71:821–826. [DOI] [PubMed] [Google Scholar]
- Coffin PO, Tracy M, Bucciarelli A, et al. Identifying injection drug users at risk of nonfatal overdose. Acad Emerg Med 2007; 14:616–623. [DOI] [PubMed] [Google Scholar]
- Darke S, Hall W. Heroin overdose: research and evidence-based intervention. J Urban Health 2003; 80:189–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doe-Simkins M, Quinn E, Xuan Z, et al. Overdose rescues by trained and untrained participants and change in opioid use among substance-using participants in overdose education and naloxone distribution programs: a retrospective cohort study. BMC Public Health 2014; 14:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbairn N, Coffin PO, Walley AY. Naloxone for heroin, prescription opioid, and illicitly made fentanyl overdoses: challenges and innovations responding to a dynamic epidemic. Int J Drug Policy 2017; 46:172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Worthington N, Piper TM, et al. Provision of naloxone to injection drug users as an overdose prevention strategy: early evidence from a pilot study in New York City. Addict Behav 2006; 31:907–912. [DOI] [PubMed] [Google Scholar]
- Gupta R, Shah ND, Ross JS. The rising price of naloxone—risks to efforts to stem overdose deaths. N Engl J Med 2016; 375:2213–2215. [DOI] [PubMed] [Google Scholar]
- Jones CM, Logan J, Gladden RM, et al. Vital signs: demographic and substance use trends among heroin users—United States, 2002–2013. MMWR Morb Mortal Wkly Rep 2015; 64:719–725. [PMC free article] [PubMed] [Google Scholar]
- kaléo Inc. Patient Information EVZIO (naloxone hydrochloride injection) Auto-Injector. In: kaléo I. ed. Richmond, VA: kaléo, Inc., 2014: 1–7. [Google Scholar]
- Katzman JG, Takeda MY, Bhatt SR, et al. An innovative model for naloxone use within an OTP setting: a prospective cohort study. J Addict Med 2018; 12:113–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koester S, Mueller SR, Raville L, et al. Why are some people who have received overdose education and naloxone retiticent to call Emergency Medical Services in the event of overdose? Int J Drug Policy 2017; 48:115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall C, Perreault M, Archambault L, et al. Experiences of peer-trainers in a take-home naloxone program: results from a qualitative study. Int J Drug Policy 2017; 41:19–28. [DOI] [PubMed] [Google Scholar]
- Maxwell S, Bigg D, Stanczykiewicz K, et al. Prescribing naloxone to actively injecting heroin users: a program to reduce heroin overdose deaths. J Addict Dis 2006; 25:89–96. [DOI] [PubMed] [Google Scholar]
- Rowe C, Santos GM, Vittinghoff E, et al. Predictors of participant engagement and naloxone utilization in a community-based naloxone distribution program. Addiction 2015; 110:1301–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd R, Seth P, David F, et al. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. 2016. Available at: https://www.cdc.gov/mmwr/volumes/65/wr/mm655051e1.htm Accessed June 26, 2017. [DOI] [PubMed] [Google Scholar]
- Rural Health Information Hub. New Mexico. 2016. Available at: https://www.ruralhealthinfo.org/states/new-mexico Accessed February 20, 2018. [Google Scholar]
- Schuckit MA. Treatment of opioid-use disorders. N Engl J Med 2016; 375:357–368. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Huma Services. About the U.S. Opioid Epidemic. Available at: https://www.hhs.gov/opioids/about-the-epidemic/ Accessed February 20, 2018. [Google Scholar]
- Wagner KD, Davidson PJ, Iverson E, et al. “I felt like a superhero”: the experience of responding to drug overdose among individuals trained in overdose prevention. Int J Drug Policy 2014; 25:157–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner KD, Valente TW, Casanova M, et al. Evaluation of an overdose prevention and response training programme for injection drug users in the Skid Row area of Los Angeles, CA. Int J Drug Policy 2010; 21:186–193. [DOI] [PMC free article] [PubMed] [Google Scholar]


