Abstract
Objectives:
Children who are hard of hearing (CHH) have restricted access to auditory-linguistic information. Remote-microphone (RM) systems reduce the negative consequences of limited auditory access. The purpose of this study was to characterize receipt and use of RM systems in young CHH in home and school settings.
Design:
Through a combination of parent, teacher, and audiologist report, we identified children who received RM systems for home and/or school use by 4 years of age or younger. With cross-sectional surveys, parents estimated the amount of time the child used RM systems at home and school per day.
Study Sample:
Participants included 217 CHH.
Results:
Thirty-six percent of children had personal RMs for home use and 50% had RM systems for school. Approximately half of the parents reported that their children used RM systems for home use for 1–2 hours per use and RM systems for school use for 2–4 hours per day.
Conclusions:
Results indicated that the majority of CHH in the current study did not receive RM systems for home use in early childhood, but half had access to RM technology in the educational setting. High-quality research studies are needed to determine ways in which RM systems benefit preschool-age CHH.
Keywords: remote microphones, pediatrics, assistive technology, newborn hearing screening
INTRODUCTION
Children who are hard of hearing (CHH) have restricted access to acoustic and linguistic information. In most cases, hearing aids (HAs) are the primary approach to improving auditory access for this population. However, HAs are not the only option available for increasing auditory access in CHH. There is clear evidence that CHH need a better signal-to-noise ratio (SNR) to understand speech in complex listening situations compared to their hearing peers (Finitzo-Hieber & Tillman, 1978; Nábělek & Pickett, 1974). Remote-microphone (RM) systems are a common type of hearing-assistive technology that utilize a remote microphone to provide an enhanced auditory signal.1 This enhanced auditory signal reduces the negative effects of noisy, reverberant room acoustics or distance between speakers and listeners (Anderson & Goldstein, 2004; Crandell, 1993; Flexer, 1997). RM systems also increase signal-to-noise ratio (SNR) and improve speech perception (Benoit, 1989; Davies, Yellon, & Purdy, 2001; Moeller, Donaghy, Beauchaine, Lewis, & Stelmachowicz, 1996; Schafer & Thibodeau, 2006).
Much of the research examining RM systems in the pediatric hard-of-hearing population has focused on RM use in elementary and secondary-grade schools, with demonstrations of improvements in speech perception in those settings (Hawkins, 1984; Larsen & Blair, 2008). It is unclear how many preschool-age CHH have access to this assistive technology both in academic settings and outside of the classrooms, at what age children are fit with personal RM for use in home settings, or in what circumstances families utilize RM systems at home. The goal of the current work was to document current practices with RM systems in young CHH, in order to provide insight into the use of assistive technologies with this population.
HAs are designed to provide increased access to acoustic-phonetic components of spoken language. Unfortunately, HAs are limited in their capacity to increase speech audibility in noisy, distant, or reverberant situations. RM hearing-assistive technology devices enhance the SNR and reduce the negative effects of distance and reverberation. Personal RM technology is an example of one such system that is recommended for use with children (Flexer, 1997). A remote microphone and transmitter, worn by a parent or caregiver, transmits the signal to the HA of the listener, via frequency modulation (FM) or digital modulation (DM). The microphone increases the intensity of the signal heard by the listener by reducing the distance from the speaker’s mouth to the listener’s ear. Microphone placement within 4 to 6 inches from the speaker’s mouth, as opposed to 3 to 6 feet from a child’s HA microphone, results in a 15 to 20 dB increase in the intensity of the speech signal and improved SNR at the position of the listener (Madell, 1992).
Because RM systems provide an opportunity to optimize speech perception in adverse listening conditions, they are commonly recommended in classroom settings for school-age children with hearing loss (Crandell & Smaldino, 2000; Johnson, Stein, Broadway, & Markwalter, 1997). RM technology also may be utilized with preschool-age CHH, who are especially vulnerable to the effects of noise, reverberation, and distance (Blaiser, Nelson, & Kohnert, 2015). Given this vulnerability, preschool-age CHH may especially benefit from efforts to improve the classroom listening environment through the use of RM systems. Unfortunately, despite the evidence to support benefits of classroom-based RM use for HA users in this age group (Anderson & Goldstein, 2004; Hawkins, 1984; Thibodeau, 2010), there have been few reports on the actual use of RM systems in preschool settings.
To the best of our knowledge, Nelson, Poole, and Muñoz (2013) conducted the only study that specifically examined educational practices with hearing-assistive technology in preschool classrooms for children who were deaf or hard of hearing. They surveyed 99 professionals who worked with 3- to 5-year-old children with hearing loss in the academic setting. Survey respondents included deaf education teachers, school administrators, speech-language pathologists, and preschool aides. Fifty-eight percent of the professionals indicated they used a sound field FM system in their classroom (also known as classroom audio distribution systems, but referred to as sound field FM by Nelson et al.). Personal FM use in the classroom was lower than sound field FM, ranging from 18% for 3-year-olds to 27% for 5-year-olds. The majority of professionals said they would recommend FM systems in the classrooms (77% for sound field systems and 71% for personal FM systems). A limitation of the study was that the authors did not ask respondents to provide a breakdown of degree of hearing loss or type of device (cochlear implant or HAs) used by the students in their classrooms. Therefore, we lack evidence of how often children with mild-to-severe hearing loss have access to RM systems. Because RM technology would appear to offer significant advantages to children who have residual hearing, it is instructive to know how often this technology is actually being utilized with CHH.
Researchers and audiologists have also recommended personal RM systems for infants, toddlers, and preschoolers in the home setting. However, there is limited information characterizing use of personal RM systems in the home with young children. The few previous studies on this topic have clear restrictions: 1) they utilized technology that is now outdated and 2) the number of participants was very small. Moeller et al. (1996) examined FM system use in home settings in six children with mild-to-severe hearing loss. The children were followed over a two-year period, starting between 2 and 6 years of age. They were instructed to use a personal FM system as often as possible outside of the classroom setting. Parents expressed a preference for using the FM system in specific situations, such as listening to the TV, when there was a primary speaker in a group, or when distance could be an issue (e.g., in the store, parks, or zoos). Both parents and children reported that the FM system could be uncomfortable and cumbersome to use outside of the home. Because of the increased visibility of the FM system compared to HAs, children were reportedly reluctant to use the FM system in public. It should be noted, however, that the study by Moeller and colleagues was conducted in the 1990s when body-worn FM receivers were considerably more bulky compared to current ear-level RM technology. It is possible that more families would express positive attitudes toward RM systems today because the wireless receivers are less obtrusive than the models from two decades ago.
In summary, there are numerous gaps in our knowledge regarding clinical practices with hearing-assistive technology for preschool-age children, specifically how often RM systems are provided to young children, how consistently RM systems are used in the home (i.e., any situation that does not involve daycare or preschool) or at school, and parent perceptions and attitudes towards current RM technology. Such information would be useful for clinical audiologists for several reasons: 1) it may enable them to provide more directed counseling to families who are considering getting an RM system, 2) it may help with making recommendations for improving use for those families who already have RM systems, but are not consistent users and 3) understanding parent perceptions and challenges may provide opportunities for improving family-centered practice. Results could have important public health and educational implications, given that RM systems are costly and sometimes covered through state or local public health or educational funding. If families are not using RM devices consistently, more education may be needed to emphasize the benefits of increased SNR and recognize appropriate environments in which to use RM systems. Additional professional and family education on these topics may support increased RM use, supporting cost-effective treatment.
The purpose of this study was to determine the proportion of CHH who received an RM system for home (defined as any context outside of school or daycare) or preschool. We also examined cross-sectional patterns of RM use at home and school, the primary source of payment for RM systems, as well as parents’ perceived benefits and problems with RM technology use at home.
METHOD
Participants
Participants were selected from a larger sample of CHH (n = 317) who participated in the multicenter, longitudinal Outcomes of Children with Hearing Loss (OCHL) study. Children were recruited from three primary sites: University of Iowa, Boys Town National Research Hospital, and University of North Carolina – Chapel Hill (for additional information about recruitment methods, see Tomblin, Walker et al., 2015). Children who participated in the OCHL study presented with a permanent bilateral hearing loss, with the better-ear pure-tone average (BEPTA) in the mild-to-severe hearing loss range. For all participants, at least one primary caregiver spoke English in the home and used a spoken language communication approach with the children. Children with significant cognitive, visual, or motor impairments were excluded from participation. Participating children were within 1.5 standard deviations of the norm-referenced mean on at least one of the two nonverbal subtests, Block Design and Matrix Reasoning, of the Wechsler Preschool and Primary Scale of Intelligence-3 (WPPSI-3; Wechsler, 2012). Vision was within normal limits or corrected to normal. Children who had motor impairments that precluded completing visual reinforcement audiometry, conditioned play audiometry, or pointing to items on standardized tests (e.g., Peabody Picture Vocabulary Test) were excluded.
The current study included OCHL participants who were preschoolers or younger at their initial testing visit. A cohort of 217 CHH (93 girls and 124 boys) between the ages of 5 months and 4 years, 9 months (M = 30.4 months; SD = 15.1 months) were included. The mean BEPTA of the CHH was 48.07 dB HL (SD = 12.68). Eighty participants had a slight/mild hearing loss (16.25 to 44 dB HL), 93 had a moderate hearing loss (45 to 59 dB HL) and 44 had a moderately-severe/severe hearing loss (60 to 82.50 dB HL).
One hundred and seventy-three children (80%) did not pass their newborn hearing screen or were identified by one month of age. The mean age at confirmation of hearing loss was 5.8 months (median = 3, SD = 8.3), and the mean age at HA fitting was 8.5 months (median = 5, SD = 9.2) for children who referred on the newborn hearing screen. Forty-two children were identified with hearing loss after the newborn period, due to passing the newborn hearing screen, not being screened, or lack of follow-up following the newborn hearing screen referral. Of those 42 later-identified participants, the mean age at confirmation of hearing loss was 22.7 months (median = 25, SD = 14.1), and the mean age at HA fitting was 23.6 months (median = 26, SD = 14.2). Two children’s newborn hearing screen status was unknown. Ninety-four percent of the children received early intervention (EI) services (n = 203/217). For the 14 children who did not receive EI, 12 were older than 3 years at the time of diagnosis and 2 declined to receive services.
Two hundred five children were fitted with acoustic HAs and 10 had bone conduction HAs. Two children did not have HAs. These two children had mild bilateral hearing loss (BEPTAs of 21.25 and 26.25). No children in the current dataset received cochlear implants during the course of the study.
Data collection
All study procedures were approved by the Institutional Review Boards of each institution. As previously described in other articles (e.g., Tomblin, Walker et al., 2015), children participated in two visits a year for children under age 2 and one visit a year for children older than 2 years. At the initial visit, parents completed an intake interview with an examiner that documented demographic characteristics (e.g., maternal education level, sex, age at HA fitting, receipt of RM system). At every visit, parents participated in a face-to-face interview regarding HA use. An RM questionnaire was added to the test battery two years into the study.
Home and Preschool RM use questionnaire.
An examiner conducted an interview pertaining to RM use inside and outside of the school setting. The RM questionnaire can be found online (http://ochlstudy.org/assessment-tools.html). Parents reported whether their child had a personal RM system for home settings. If so, parents indicated how old their child was when he/she received the personal RM system and estimated the average amount of time the child wore the personal RM system outside of the day care or preschool setting. Data regarding average amount of time per use at home were documented as categorical variables: 0 hours, 1–2 hours, 3–4 hours, or 5–6 hours. Examiners asked the caregiver to rate how often the child wore his/her RM system in six different listening environments: in the car, during meal times, during book sharing, on the playground, in public (e.g., at the zoo, in a store), or other. The scale included the following ratings: 0 = never, 1 = rarely, 2 = sometimes, 3 = often, 4 = always, and not applicable. For data reduction purposes regarding frequency of use in each situation, ratings were combined into categories of always/often/sometimes and rarely/never. Parents were also asked to indicate the primary user of the RM system (i.e., which conversational partner used it more than 50% of the time with the child), funding source, whether they believed RM benefitted their child, and frustrations/problems with using the RM system at home. A separate questionnaire addressed the type of RM system and amount of RM use in preschool settings. Data regarding average RM use at preschool are reported as categorical variables: 0 hours, 1–2 hours, 2–4 hours, 4–6 hours, and 6–8 hours. In addition to parent report, we invited service providers to complete online service provider surveys after each visit. The surveys included specific questions regarding whether the children owned RM systems (i.e., “Does this child have a personal FM system for use outside of school?” and “Does this child use FM at school?”). These survey responses were reviewed to ascertain and/or confirm whether children had received RM systems in home and school settings. These surveys can be found online at the OCHL webpage and are described in further detail in Harrison et al. (2016). For two participants, parent report of RM receipt was missing. In these two cases, we examined information provided by the participants’ preschool teachers and audiologists. We found seven cases in which there was disagreement between audiologists, teachers, and/or parents regarding whether or not a child had an RM system. In these cases, we verified RM receipt through educational records for six children. For the one participant who could not be verified through these means, we included the response provided by two out of three respondents (parents and teacher).
Statistical Analysis
Data regarding RM receipt and use were explored descriptively. For home RM use, participants were divided into two age groups: toddlers (6 months-2 years) and preschoolers (3–4 years). Categorizing children in this manner is consistent with previous manuscripts in the OCHL study (Walker et al., 2015; Walker et al., 2013), which have demonstrated that issues pertaining to situational hearing device use with infants/toddlers are different from preschool-age children. Preschool RM use data included children at the 3- and 4-year old visits. If there were repeated measures within an age range (e.g., data at 1 and 2 years), the earliest time point was included in the analysis to avoid repeated measures.
RESULTS
Personal RM systems for home use
Thirty-six percent (n = 79/217) of children received a personal RM for home use, as determined by the OCHL intake form and/or the RM questionnaire. On average, children were fitted with the personal RM at 23.4 months (SD = 10.29, range = 6 to 48). Of the 79 children who had an RM system for home, 23 did not complete the RM questionnaire at any test visit due to time constraints or examiner error. Eleven completed the RM questionnaire subsequent to the 4 year old visit; however, we chose not to include these later responses in the event that the answers did not apply to preschool RM use. There were 45 parents who completed the RM questionnaire when the children were 4 or younger. Table 1 summarizes results regarding primary funding support. The majority of parents reported that their state early hearing detection and intervention (EHDI) program was the primary source of funding for the RM system (59%; n = 29/49; three parents provided different responses across visits; all of their responses are included in the descriptive data). Table 2 summarizes results related to the primary user of the RM transmitter. Mothers were identified as primary users of the RM transmitter most often (71%; n = 29/41), with fathers, grandparents, babysitter, and gymnastics coach identified less frequently.
Table 1.
Descriptive data regarding funding sources for RM systems.
| N=49 | n | % |
|---|---|---|
| EHDI or other birth to three funding program | 29 | 59 |
| Medicaid | 9 | 18 |
| Out of pocket | 7 | 14 |
| School provides RM for use at home | 3 | 6 |
| Private health insurance | 1 | 2 |
Table 2.
Descriptive data regarding primary user of the RM system.
| Who is the primary user (uses more than 50% of the time) of the RM transmitter when used for personal use (e.g., outside of school)? | ||
|---|---|---|
| N=41 | n | % |
| Mother | 29 | 71 |
| Father | 5 | 13 |
| Both parents | 3 | 7 |
| Grandparents | 2 | 5 |
| Babysitter | 1 | 2 |
| Other (gymnastics coach) | 1 | 2 |
Thirty-eight and 32 parents responded to questions regarding benefit and problems with the personal RM system, respectively. Some parents responded to these questions at multiple visits, but only single-test visits are included in the description (i.e., no repetition of subjects). In cases in which participants had more than one survey, the earliest survey that had the most complete information for questions regarding perceived benefits was included. On average, families had owned the RM systems for 15 months (SD = 11) by the time they responded to the survey. The vast majority of parents (95%; n = 36/38) responded that they felt that their child benefitted from the personal RM. Parents cited not having to raise their voice to be heard, gaining and maintaining the child’s attention, ensuring safety by communicating with the child at a distance, behavior management in public, connecting to Bluetooth for phone calls, and the child picking up new words and concepts easier as benefits for using the RM system. Two parents, who had owned the RM system for 17 and 29 months, responded with negative comments. Of the two parents who reported their children did not benefit from the personal RM system, one felt that the personal RM “scared” their child, while the other family reported having difficulty detaching the RM receivers from the HAs.
With respect to problems with the personal RM system, more parents reported experiencing no problems (59%; n = 19/32) compared to parents who reported problems (41%; n = 13/32). Parents who noted that there were problems were also asked to describe the problems. Responses varied and some parents reported more than one problem, but several common themes emerged. Five parents reported having difficulty with the connection between the HAs and RM receivers, five parents noted that the RM system did not appear to be working and/or had to be sent in for repairs, and two parents indicated that the RM system drained the HA batteries too quickly. One parent reported that his/her child did not like the RM system, but did not provide further explanation.
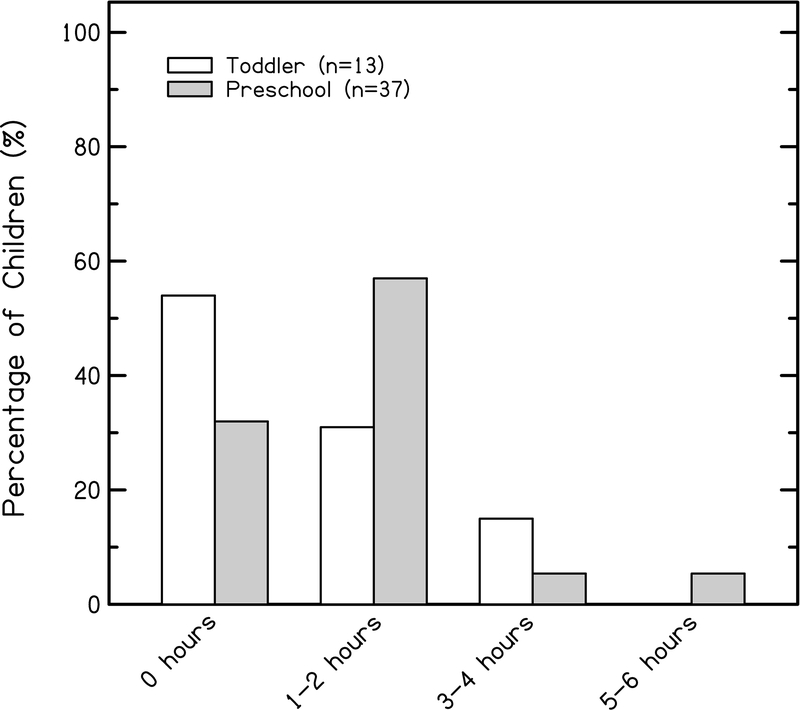
Parents reported the average amount of RM use in home settings on days when the RM was used. Data were divided into two age groups: toddlers (1–2 years; n = 13) and preschoolers (3–4 years; n = 37). As shown in Figure 1, the majority of parents reported 0 hours of use for toddlers (54%; n = 7/13), followed by 31% (n = 4/13) reporting an average of 1–2 hours per use and 15% (n = 2/13) reporting 3–4 hours. When the RM system was used, parents of preschoolers reported longer amounts of time per use of the home RM system compared to toddlers. Fifty-seven percent (n = 21/37) of preschoolers used it 1–2 hours per use, on average. Thirty-two percent (n = 12/37) reportedly used it 0 hours, 5% each (n = 2/37) reported 3–4 hours and 5–6 hours per use.
Figure 1.
Parent-report ratings for daily personal remote microphone use for toddlers (white bars) and preschoolers (gray bars).
To examine variables that may be correlated with RM use, we conducted non-parametric Spearman’s correlations with chronological age or better-ear PTA as independent variables. We included the earliest visit at which parents reported average amount of RM hours per use as the dependent variable. There was no significant association between chronological age and RM use (r = .08, p = .61). Although the association was in the expected positive direction (i.e., poorer hearing > hours of use), there was also no significant relationship between better-ear PTA and RM use (r = .228, p = .14).
Length of experience with the RM system was also calculated. Because the data were skewed in terms of length of RM experience, we conducted a median split of length of experience, which divided the participants into a group of children with 12 months or less of experience (n = 22) and children with 14 to 40 months of experience (n = 21). Of the group with less experience, 55% (n = 13/22) of parents reported 1–2 hours per use, followed by 27.3% (n = 6/22) reporting 0 hours, and 18% (n = 4/22) reporting 3 or more hours. Forty-eight percent (n = 10/21) of the group with greater experience reported using it 0 hours, while another 48% reported 1–2 hours per use. Only one parent reported using it 3 or more hours per use.
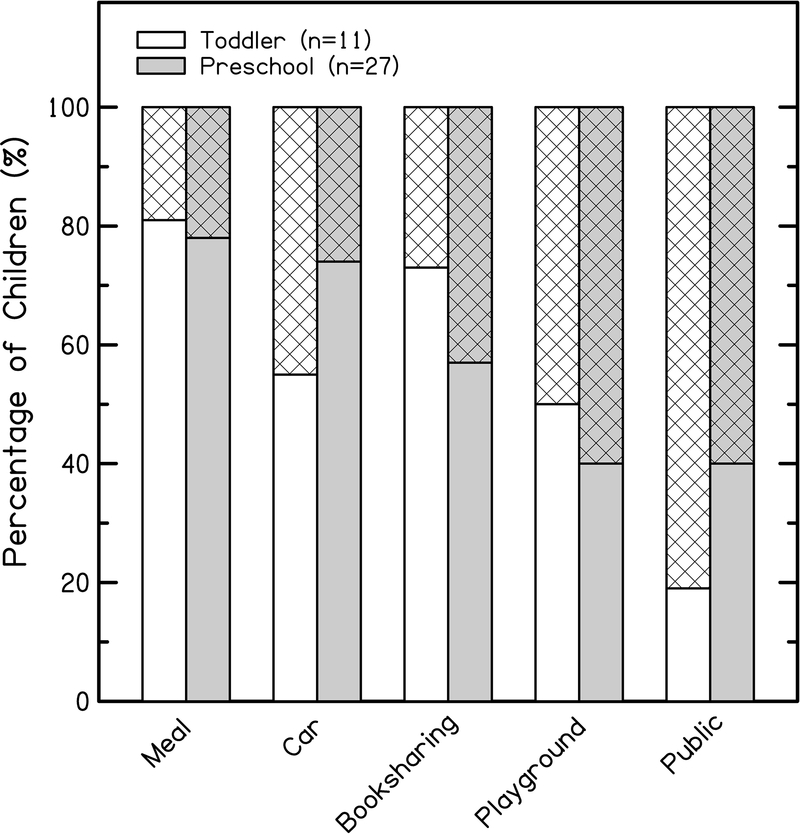
Parents were also queried regarding use of personal RM across different situational contexts, using a 5-point Likert scale (Moeller, Hoover, Peterson, & Stelmachowicz, 2009). Figure 2 shows parent ratings across five listening situations, separated by children’s ages (the number of participants is reduced compared to Figure 1, due to parents not responding to the question or examiners not administering this part of the questionnaire). Parents of toddlers reported using the RM system most often in public situations, with 81% (n = 9/11) reporting that they used it always, often, or sometimes. Parents reported using the RM system the least often at mealtimes, with 81% (n = 9/11) reporting that they used it rarely or never. Shared book reading was another situation in which the majority of parents reported using it rarely or never (73%; n = 8/11). The parents of toddlers were fairly evenly split in their ratings of RM use in the car, at the playground, and at home. Parents of preschoolers reported using the RM system most often in public and at the playground, with 60% using it always, often, or sometimes in both situations (n = 18/30). Consistent with the toddlers, mealtimes were the least frequent context for RM use (78%; n = 21/27).
Figure 2.
Ratings for frequency of remote microphone use for toddlers (white bars) and preschoolers (gray bars) across different situations. Solid regions of the bar graph indicate rarely/never ratings. Hatched regions indicate always/often/sometimes ratings.
RM systems in preschool settings
Data were obtained for 168 3- and 4-year-olds who were enrolled in preschool. Half of the participants (n = 84/168) received an RM system for use in the preschool setting. Forty-three percent (n = 36/84) of the children with an RM system at school had an RM system for home use. Forty parents received the questionnaire regarding the type of RM system used in school. The majority of parents reported that their children used HAs with universal RM receivers (60%; n = 24/40). Twenty percent (n = 8/40) used HAs with integrated RM receivers, 12.5% (n = 5/40) used a classroom audio distribution system, and 7.5% (n = 3/40) used a telecoil and neckloop. The same parents also reported on who paid for the school RM system. In 70% (n = 28/40) of cases, the school system paid for the entire RM system (receiver and transmitter). Twenty-three percent (n = 9/40) of parents provided the entire RM system. Two parents indicated that they provided the receiver and the school provided the transmitter and one parent said that Medicaid paid for the RM system for school.
Thirty-nine parents reported on hours of school RM use. No parents indicated that their child used the RM system 0 hours at school. Fifteen percent (n = 6/39) used it 1–2 hours, 7% (n = 3/39) used it 4–6 hours and 15% (n = 6/30) used it 6–8 hours. The highest percentage of children used the RM system from 2–4 hours (49%; n = 19/39). We did not document amount of hours in preschool throughout the day, so we cannot determine how many of the children were in half-day preschools and how many were in full-day preschool (and therefore, using the RM system during half of the day).
DISCUSSION
The primary objective of this study was to describe service provision related to RM system receipt at home and school for young CHH. The current results indicate that approximately one-third of the sample received a personal RM system for home use and one-half received an RM system (personal or classroom audio distribution) for academic use in the preschool setting. The majority of parents reported benefit from using the RM system at home.
RM receipt and use in home and school settings
This paper is one of the first studies to report on RM receipt and use both inside and outside of the educational setting for younger CHH. Approximately one-third of OCHL participants owned a personal RM system for home use (i.e., non-school settings) by 4 years of age. On average, families obtained the RM system during the toddler years (around 2 years of age), although the range was wide (6 months to 4 years). It is worth mentioning that the sample of this study consists of an economically advantaged cohort of children compared to the U.S. population as a whole (Tomblin, Walker et al., 2015). As a result, the results of the current study may not be generalizable to all children with hearing loss, which would include lower-income families who may have less access to hearing-assistive technology, especially in locations that do not have programs that provide funding support for RM systems. The majority of participants in the study routinely received routine audiological care with experienced pediatric audiologists. In addition, 94% received EI services after identification. This value is a much higher percentage of enrollment than the whole U.S., on average, which is 67% based on 2016 data from the Centers for Disease Control (CDC, 2018). It may be that the results of this study overestimate RM receipt and use in other parts of the country where audiological care and EI/Part C services are more difficult to access (Bush et al., 2015, 2017).
Parents estimated amount of hours per use with the RM, but they indicated that use occurred in specific situations that did not necessarily occur on a daily basis. Therefore, the average amount of hours per RM use reported in this paper should be interpreted with caution. Despite our caution in interpreting the RM usage data, it is also critical to note that a number of families reported 0 hours of use with the RM systems, particularly for toddlers. The finding of low uptake is informative because it may indicate a greater need for audiologists and interventionists to support and educate families with regards to RM technology. Munoz, Nelson, and Herald (2018) recently published self-report survey data from audiologists that indicated a majority (53%) of audiologists always discussed the benefits of hearing-assistive devices with parents, but fewer audiologists (36%) always discussed how to monitor the function or performance of personal assistive devices. These findings suggest there may be a practice gap related to inconsistent monitoring of RM devices, which could be addressed via inter-professional collaboration among service providers and support for parent education (Munoz et al., 2018).
The frequency of situational use ratings provided valuable information about practices with the RM. In general, families reported using the RM in situations where distance and noise could be an issue, specifically in public and at the playground. These findings mirror results by Moeller et al. (1996), which included 6 CHH who utilized RM systems at home. Parents reported a preference for using the RM system in situations where it provided security, such as stores, parks, or the zoo. Almost 20 years later, with a larger sample and current technology, parents are still inclined to use the RM strategically, particularly in situations where it facilitates child safety and communication from a distance. It appears that parents understand the value of the RM system in these contexts, as the child’s ability to hear better in background noise is evident when using an RM system; however, they may not realize the benefit the child receives in other situations, as indicated by lower frequency ratings. Future investigations may need to address why the RM system appears to be utilized selectively in specific situations when it could benefit the child in other situations as well. Such information may inform us about how parents’ perception of benefit relates to use of RM technology. It may also provide audiologists with insight into best practices for counseling families about when to utilize the RM system, especially for situations where benefit may not be obvious, such as increasing access to caregiver talk (Benitez-Barrera, Angley, & Tharpe, 2018).
With the current data, we were able to identify situations in which the RM was not being used. Parents reported low use ratings for mealtimes, in the car, and shared book reading. Shared book reading is generally done in a quiet environment, with minimal distance between the speaker and the listener. RM use would probably not enhance the audibility of the speaker any further. On the other hand, studies have shown that family meals promote psychosocial health in children (Eisenberg, Olson, Neumark-Sztainer, Story, & Bearinger, 2004). RM use may be difficult in this context because of the practical constraints of trying to feed young children. Additional difficulties include lack of a primary speaker and concerns about damaging the equipment, but if family members are able to pass the RM microphone or place a single microphone in the center of the table, it could provide the child access to a potentially language-rich environment. The availability of microphone arrays that are highly directional can support access to speech from multiple talkers without requiring a pass microphone, making remote microphone use in this situation more feasible than it was with older RM technology. The car is another situation that appears to be underutilized with the RM system, but could be advantageous for the parent and child. The car provides many opportunities for both direct conversation and incidental learning, but distance, background noise, and lack of speechreading cues make it challenging for children to communicate with parents in the car. The car is also a situation in which parents report low HA use due to safety concerns or lack of engagement, particularly for younger children (Walker et al., 2013). Moeller et al. (2007) also reported that consistent HA use in the car was a challenge for families. They examined consistency of HA use across multiple situations in 7 families; two of the families who were able to achieve full-time use in the car also used an RM system to facilitate communication. Thus, utilizing the RM system in the car may encourage better device compliance because the child would feel more engaged in the listening environment. Audiologists who dispense and program RM systems for children may want to discuss these listening contexts with parents, to explain why and how the child will benefit from the RM in different situations. Future research should also address what challenges families face with using the RM system in potentially language-rich environments, and determine ways that family-centered intervention can help to overcome challenges to consistent use.
Although not addressed in the current study, an additional benefit of using the RM system in multiple situations could be the psychological impact on acceptance of the hearing loss and the hearing-assistive technology. RM technology could help parents feel more connected to their child during complex listening situations, such as the car or the playground. Using an RM system in public may increase opportunities for parents to explain the technology to others, which could support the parents’ attitudes towards self-efficacy and commitment to using HAs and personal assistive devices consistently (DesJardin, 2005). There is also the possibility that as children get older, seeing their parents wear a RM device that is connected to their own equipment could enhance the child’s appreciation for having increased access to sound, which may then carryover to continued acceptance of RM technology throughout the school years. It is speculative for us to consider the psychological effects of RM technology on parents and children with hearing loss with the current results, but future research in this area is certainly warranted.
Similar to the Moeller et al. (1996) study, parents reported problems using the RM system related to technology and troubleshooting the devices. While RM technology has advanced to provide additional audibility of speech in complex listening environments, the physical aspects of the devices remain an issue for some families. Audiologists should provide proactive hands-on training so that families feel capable of troubleshooting devices if/when they malfunction. There are also a variety of instructional videos on You Tube related to device management, which may be of use to parents and caregivers following clinic visits.
Not surprisingly, a larger proportion of children had access to RM systems in the schools than for personal use. Half of the children surveyed used a school RM system. This percentage is lower than data reported by Nelson et al. (2013), in which 67% of preschool-age children with hearing loss used personal RM systems and 58% of teachers in deaf/hard of hearing preschool classrooms reported using classroom audio distribution systems. The current results indicated that 80% of children were using ear-level technology (either universal receivers or integrated RM/hearing aid systems) in the preschool setting, whereas results from Nelson et al. indicated teachers were using more of a variety of ear-level and classroom audio distribution systems. Nelson et al. specifically targeted teachers who were providing services in deaf education, with some survey respondents teaching in state schools for the deaf (83%). Thus, it is likely that the study included children with severe-to-profound hearing loss who were being educated in self-contained classrooms for children with hearing loss. The current study focused on children with mild-to-moderately-severe hearing loss who were enrolled in a variety of daycare, public, and specialized preschool programs. Educational preparation of the children’s providers, which may influence uptake and use of RM systems in the classroom, was not examined for the purposes of this study, which may explain the lower percentage of children with RM systems. More research is necessary on what predicts the receipt of RM systems in preschool, including prior family and teacher experience using RM systems, and other child-, family-, and program-related factors.
New technology and equipment may support utilization of RM systems for populations that may have been overlooked for candidacy previously. It should be noted that the data in the current study were collected between 2009 and 2013 and the RM technology worn by these participants may already be considered outdated. For example, microphone/transmitters can now be packaged into one piece instead of two, eliminating the connecting wire and making the technology even smaller and more convenient to use. Additionally, when the questionnaires for this study were administered, it was assumed that the children were using analog FM radio transmission to deliver the signal from the transmitter to the receiver. We did not query parents regarding the type of RM transmission being used. In recent years, digital modulation (DM) technology has been introduced as an alternative to FM systems. DM systems offer concrete advantages in speech recognition over FM technology. The audio bandwidth in DM systems is wider than FM systems, thus providing more access to high frequency information (Wolfe, Morais, Schafer, Agrawal, & Koch, 2015), although the hearing aid may still impose bandwidth restrictions as the transducer (Kimlinger, McCreery, & Lewis, 2015). Digital signal processing also provides better speech recognition in moderate-to-high noise levels compared to FM systems, due to the adaptive gain capacities that are available in DM (Thibodeau, 2014; Wolfe et al., 2013). These improvements may make RM technology even more beneficial to use in the classroom, allowing greater utilization with children who have mild-to-severe hearing loss. Unfortunately, the current results do not capture the use of FM versus DM technology in the preschool setting; future research is needed to investigate the frequency of use and utility of DM systems in the educational preschool setting.
Limitations and Future Directions
This study reported on home and school RM receipt for a group of children who participated in a multi-center, longitudinal study on outcomes of children who are hard of hearing. One limitation in this study is that the children had no additional cognitive, visual, or motor impairments, so the results may not generalize to how RM systems are adopted and used for children with multiple disabilities. Additional research is needed to determine if children with multiple disabilities experience additional challenges using the technology and/or report use and benefit in similar situations.
The conclusions we can draw from survey results on funding, perceived benefit, and problems with the equipment are limited due to a small number of participants who completed the questionnaire and reduced response rates. The specific questions regarding RM use, benefit, and funding were not administered until the second year of data collection, thus restricting the number of responses for some of the OCHL families. We were unable to determine the reason that some parents did not respond to specific questions on benefit and problems. It is possible that the responses were missing due to random reasons (e.g., examiner did not administer the entire RM questionnaire; someone other than a parent brought the child to the research visit). Regardless of the reason for missing data, it should be acknowledged that the reduced response rate further limits the generalizability of the current findings.
Another limitation of the current study is that we did not examine whether RM use led to better language outcomes, which is arguably more important to consider than simply owning an RM. It is beyond the scope of this manuscript to examine how RM receipt or the amount of RM use influences language and listening outcomes. Future studies will include whether amount of RM use influences language outcomes, as it does with HAs (Tomblin, Harrison et al., 2015). Research on the impact of home and preschool RM, intervention services, and family involvement is greatly needed.
Conclusions
The current results indicate that the majority of preschool-age CHH do not receive personal RM systems for home use in early childhood. Approximately half of the children had access to RM technology in the educational setting. There is a need to further examine practices and attitudes surrounding fitting and using RM from an intervention perspective for both the home and educational setting. Many families of young children may be under-served in terms of access to personal RM systems. However, there is a lack of evidence regarding the long-term impact of RM use on language outcomes, which would justify increasing access to these hearing-assistive technologies. Additional high-quality research is needed to determine how RM systems used at home and preschool benefit auditory-linguistic access and spoken-language outcomes of young CHH.
Acknowledgements
This work was supported by National Institutes of Health Grants NIH/NIDCD 5R01DC009560 (co-principal investigators, J. Bruce Tomblin, University of Iowa and Mary Pat Moeller, Boys Town National Research Hospital) and 5R01DC013591 (principal investigator, Ryan W. McCreery, Boys Town National Research Hospital). The content of this project is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Deafness and Other Communication Disorders or the National Institutes of Health. The following people provided support, assistance, and feedback at various points in the project: Dawna Lewis, Mary Pat Moeller, J. Bruce Tomblin, Ryan McCreery, Jacob Oleson, Wendy Fick, and Marlea O’Brien. Special thanks go to the families and children who participated in the research and to the examiners at the University of Iowa, Boys Town National Research Hospital, and the University of North Carolina-Chapel Hill.
Conflicts of Interest and Source of Funding:
The authors have no conflicts of interest to declare. This research was supported by the following grants from the NIH-NIDCD: R01DC009560 and R01DC013591. The authors had full editorial control of this work and manuscript.
Footnotes
1 Additional forms of wireless connectivity include infrared and Bluetooth technology (Atcherson, Childress, & Kennett, 2016). For the purposes of the current paper, we will focus on use of RM systems that utilize frequency modulation or digital modulation to transmit the signal to a listener.
References
- Anderson KL, & Goldstein H (2004). Speech perception benefits of FM and infrared devices to children with hearing aids in a typical classroom. Language, Speech, and Hearing Services in Schools, 35(2), 169–184. [DOI] [PubMed] [Google Scholar]
- Atcherson SR, Childress T, & Warren Kennett S (2016). Assistive hearing and access technologies and auditory-verbal therapy In Estabrooks W, MacIver-Lux K, & Rhoades E (Eds.), Auditory-verbal therapy for young children with hearing loss and their families and the practitioners who guide them (pp. 201–218). San Diego, CA: Plural Publishing. [Google Scholar]
- Benítez-Barrera CR, Angley GP, & Tharpe AM (2018). Remote microphone system use at home: Impact on caregiver talk. Journal of Speech, Language, and Hearing Research, 61(2), 399–409. [DOI] [PubMed] [Google Scholar]
- Benoit R (1989). Home use of FM amplification systems during the early childhood years. Hearing Instruments, 40(3), 8–12. [Google Scholar]
- Blaiser KM, Nelson PB, & Kohnert K (2015). Effect of repeated exposures on word learning in quiet and noise. Communication Disorders Quarterly, 37(1), 25–35. [Google Scholar]
- Bush ML, Hardin B, Rayle C, Lester C, Studts CR, & Shinn JB (2015). Rural barriers to early diagnosis and treatment of infant hearing loss in Appalachia. Otology & Neurotology, 36(1), 93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush ML, Kaufman MR, & McNulty BN (2017). Disparities in access to pediatric hearing health care. Current Opinion in Otolaryngology & Head and Neck Surgery, 25(5), 359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2016). Hearing loss in children: 2016 annual data early hearing detection and intervention (EHDI) program. Retrieved from https://www.cdc.gov/ncbddd/hearingloss/2016-data/09-early-Intervention.html.
- Crandell CC (1993). Speech recognition in noise by children with minimal degrees of sensorineural hearing loss. Ear and Hearing, 14(3), 210–216. [DOI] [PubMed] [Google Scholar]
- Crandell CC, & Smaldino JJ (2000). Classroom acoustics for children with normal hearing and with hearing impairment. Language, Speech, and Hearing Services in Schools, 31(4), 362–370. [DOI] [PubMed] [Google Scholar]
- Davies MG, Yellon L, & Purdy SC (2001). Speech-in-noise perception of children using cochlear implants and FM systems. Australian and New Zealand Journal of Audiology, 23(1), 52–62. [Google Scholar]
- Desjardin JL (2005). Maternal perceptions of self-efficacy and involvement in the auditory development of young children with prelingual deafness. Journal of Early Intervention, 27(3), 193–209. [Google Scholar]
- Eisenberg ME, Olson RE, Neumark-Sztainer D, Story M, & Bearinger LH (2004). Correlations between family meals and psychosocial well-being among adolescents. Archives of Pediatrics & Adolescent Medicine, 158(8), 792–796. [DOI] [PubMed] [Google Scholar]
- Finitzo-Hieber T, & Tillman TW (1978). Room acoustics effects on monosyllabic word discrimination ability for normal and hearing-impaired children. Journal of Speech, Language, and Hearing Research, 21(3), 440–458. [DOI] [PubMed] [Google Scholar]
- Flexer C (1997). Individual and sound-Field FM Systems: Rationale, description, and use. Volta Review, 99(3), 133–162. [Google Scholar]
- Harrison M, Page TA, Oleson J, Spratford M, Berry LU, Peterson B, … & Moeller MP (2016). Factors affecting early services for children who are hard of hearing. Language, Speech, and Hearing Services in Schools, 47(1), 16–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins DB (1984). Comparisons of speech recognition in noise by mildly-to-moderately hearing-impaired children using hearing aids and FM systems. Journal of Speech and Hearing Disorders, 49(4), 409–418. [DOI] [PubMed] [Google Scholar]
- Johnson CE, Stein RL, Broadway A, & Markwalter TS (1997). Minimal High-Frequency Hearing Loss and School-Age Children: Speech Recognition in a Classroom. Language, Speech, and Hearing Services in Schools, 28(1), 77–85. [Google Scholar]
- Kimlinger C, McCreery R, & Lewis D (2015). High-frequency audibility: The effects of audiometric configuration, stimulus type, and device. Journal of the American Academy of Audiology, 26(2), 128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen JB, & Blair JC (2008). The effect of classroom amplification on the signal-to-noise ratio in classrooms while class is in session. Language, Speech, and Hearing Services in Schools, 39(4), 451–460. [DOI] [PubMed] [Google Scholar]
- Madell JR (1992). FM systems as primary amplification for children with profound hearing loss. Ear and Hearing, 13(2), 102–107. [DOI] [PubMed] [Google Scholar]
- Moeller MP, Donaghy KF, Beauchaine KL, Lewis DE, & Stelmachowicz PG (1996). Longitudinal study of FM system use in nonacademic settings: Effects on language development. Ear and Hearing, 17(1), 28–41. [DOI] [PubMed] [Google Scholar]
- Moeller MP, Hoover B, Peterson B, & Stelmachowicz P (2009). Consistency of hearing aid use in infants with early-identified hearing loss. American Journal of Audiology, 18(1), 14–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munoz KF, Nelson L, & Herald K Pediatric Hearing Device Management: Professional Practices for Monitoring Aided Audibility. Journal of Early Hearing Detection and Intervention, 3(1), 2–20. [Google Scholar]
- Nábělek AK, & Pickett J (1974). Reception of consonants in a classroom as affected by monaural and binaural listening, noise, reverberation, and hearing aids. The Journal of the Acoustical Society of America, 56(2), 628–639. [DOI] [PubMed] [Google Scholar]
- Nelson LH, Poole B, & Muñoz K (2013). Preschool teachers’ perception and use of hearing assistive technology in educational settings. Language, Speech, and Hearing Services in Schools, 44(3), 239–251. [DOI] [PubMed] [Google Scholar]
- Schafer EC, & Thibodeau LM (2006). Speech recognition in noise in children with cochlear implants while listening in bilateral, bimodal, and FM-system arrangements. American Journal of Audiology, 15(2), 114–126. [DOI] [PubMed] [Google Scholar]
- Thibodeau L (2010). Benefits of adaptive FM systems on speech recognition in noise for listeners who use hearing aids. American Journal of Audiology, 19(1), 36–45. [DOI] [PubMed] [Google Scholar]
- Thibodeau L (2014). Comparison of speech recognition with adaptive digital and FM remote microphone hearing assistance technology by listeners who use hearing aids. American Journal of Audiology, 23(2), 201–210. [DOI] [PubMed] [Google Scholar]
- Tomblin JB, Harrison M, Ambrose SE, Walker EA, Oleson JJ, & Moeller MP (2015). Language outcomes in young children with mild to severe hearing loss. Ear and Hearing, 36, 76S–91S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin JB, Walker EA, McCreery RW, Arenas RM, Harrison M, & Moeller MP (2015). Outcomes of children with hearing loss: Data collection and methods. Ear and Hearing, 36, 14S–23S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker EA, McCreery RW, Spratford M, Oleson JJ, Van Buren J, Bentler R, … Moeller MP (2015). Trends and predictors of longitudinal hearing aid use for children who are hard of hearing. Ear and Hearing, 36, 38S–47S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker EA, Spratford M, Moeller MP, Oleson J, Ou H, Roush P, & Jacobs S (2013). Predictors of hearing aid use time in children with mild-to-severe hearing loss. Language, Speech, and Hearing Services in Schools, 44(1), 73–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D (2012). The Wechsler Preschool and Primary Scale of Intelligence - Third Edition. Harcourt Assessment. [Google Scholar]
- Wolfe J, Morais M, Schafer E, Agrawal S, & Koch D (2015). Evaluation of speech recognition of cochlear implant recipients using adaptive, digital remote microphone technology and a speech enhancement sound processing algorithm. Journal of the American Academy of Audiology, 26(5), 502–508. [DOI] [PubMed] [Google Scholar]
- Wolfe J, Morais M, Schafer E, Mills E, Mülder HE, Goldbeck F, … Peters BR (2013). Evaluation of speech recognition of cochlear implant recipients using a personal digital adaptive radio frequency system. Journal of the American Academy of Audiology, 24(8), 714–724. [DOI] [PubMed] [Google Scholar]